1. Introduction
Wearable sensing is an emergent technology for the monitoring of human vital signs in various fields such as health, sports and military [
1,
2,
3]. Nowadays, these sensors have gained widespread usage for measuring the vital signs for remote health care. Such sensors provide an opportunity to analyze the subject’s health at their own premises and thus improve the possibility of adaptive medication significantly. Consequently, this has greatly reduced the cost linked with conventional healthcare facilities [
4]. Furthermore, the integration of these sensors into textile fiber and clothes for direct connectivity with the human body is employed for health monitoring [
5]. Such flexible wearable sensors are able to measure several vital signs including body temperature, blood pressure, heart rate, and breathing rate, etc [
6,
7,
8]. Among these vital signs, breathing rate holds particular significance in human physiology, as it contains a wealth of information about a person’s health condition.
Generally, the patients are observed physically to estimate breathing rate by counting the chest expansion and contraction for a short period of time, which may result in a false conclusion about the patient’s health [
9]. Therefore, sensors that can monitor breathing in real-time have the potential to provide important diagnostic and monitoring tools for respiratory diseases, such as asthma, chronic obstructive pulmonary disease (COPD), and sleep apnea [
10]. Furthermore, breathing rate is an important predictor for cardiac arrests as shown in the clinical reports [
11] and [
12]. Likewise, the monitoring of breathing rate is helpful also for the early diagnosis of respiratory illnesses such as Covid-19. In context, an estimation algorithm has been established for the detection of corona virus owing to a correlation between abnormal breathing rate and covid-19 infection, [
13]. Moreover, respiration sensors have also emerged as a valuable tool for monitoring infant health in real time. These sensors facilitate the continuous assessment of respiratory patterns, enabling timely identification of irregularities and facilitating prompt medical intervention [
14,
15]. Respiration sensors are generally classified based on their physical location with re-spect to the subject and employed sensing technique. The literature presents a prevalent categorization into two main types which are contact and contactless sensors [
16,
17,
18]. Contact sensors require physical contact with the subject and can measure parameters such as temperature, humidity, pressure, or gas concentrations. They can be placed on the skin, inside the mouth, nose, or airways. Examples include thermistors, strain gauges, piezo electric sensors, and gas sensors. On the other hand, contactless sensors measure breath parameters without physical contact using optical or electromagnetic principles, detecting variations in light, sound, or electromagnetic waves caused by breathing. Examples include laser spectroscopy, microwave resonators, and acoustic sensors. While contact sensors offer higher accuracy, they can be uncomfortable and affect breathing patterns.
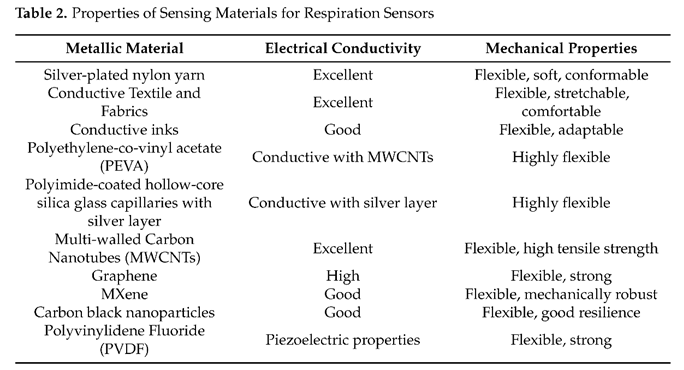
The average respiratory frequency of humans varies across different age groups and typically falls within the range of 10 to 40 breaths per minute. However, the breath monitoring techniques utilize a wide range of frequencies, allowing for their classification based on operational frequencies. Therefore, flexible wearable sensors for breathing can be broadly categorized into high-frequency systems, operating in the microwave range, and relying on changes in electromagnetic properties of surroundings, and low-frequency systems, using passive sensing mechanisms to detect breathing motion. In this review, sensors operating above 10 MHz are classified as high-frequency sensors, while those operating at lower frequencies are categorized as low-frequency sensors, as illustrated in
Figure 1.
This paper aims to provide an in-depth exploration of flexible and wearable sensors for breathing, specifically focusing on the recent techniques according to the operating frequency. Moreover, the materials and fabrication techniques that have been utilized in their development would be discussed. For this review, conference proceedings and full-text articles were selected from a broad search containing diverse foundations and catalogues such as Science Direct, Web of Science, MDPI and IEEE Xplore. Keywords were selected in each source as follows: (Flexible OR textile) AND (wearable AND sensor) AND (respiration OR breathing). The initial search returned 476 results, which were then screened to only include physiological sensors and analyzed to eliminate duplicates, resulting in a final count of 101 studies. All content of the subsequent sections on the sensing techniques, materials, and fabrication techniques are extracted from these studies.
The organization of this paper is as follows.
Section 2 and
Section 3 provide a detailed description of high-frequency and low-frequency respiration sensors. In
Section 4, materials and techniques of respiration sensors are presented and discussed. Finally,
Section 5 summarizes the findings of this study and presents recommendations for future research in this field.
2. High-Frequency Sensors
High-frequency sensors offer unique advantages such as smaller size and wireless communication capabilities, making them suitable for various applications in healthcare and wearable technology. Among these sensors, antenna sensors, RFID/NFC-based sen- sors, metamaterial sensors, and Fiber Bragg Grating (FBG) sensors have emerged as the most promising candidates for high-frequency respiration monitoring. In the following sub- 80 sections, a brief overview of each technique including its operating principle and associated 81 challenges is presented.
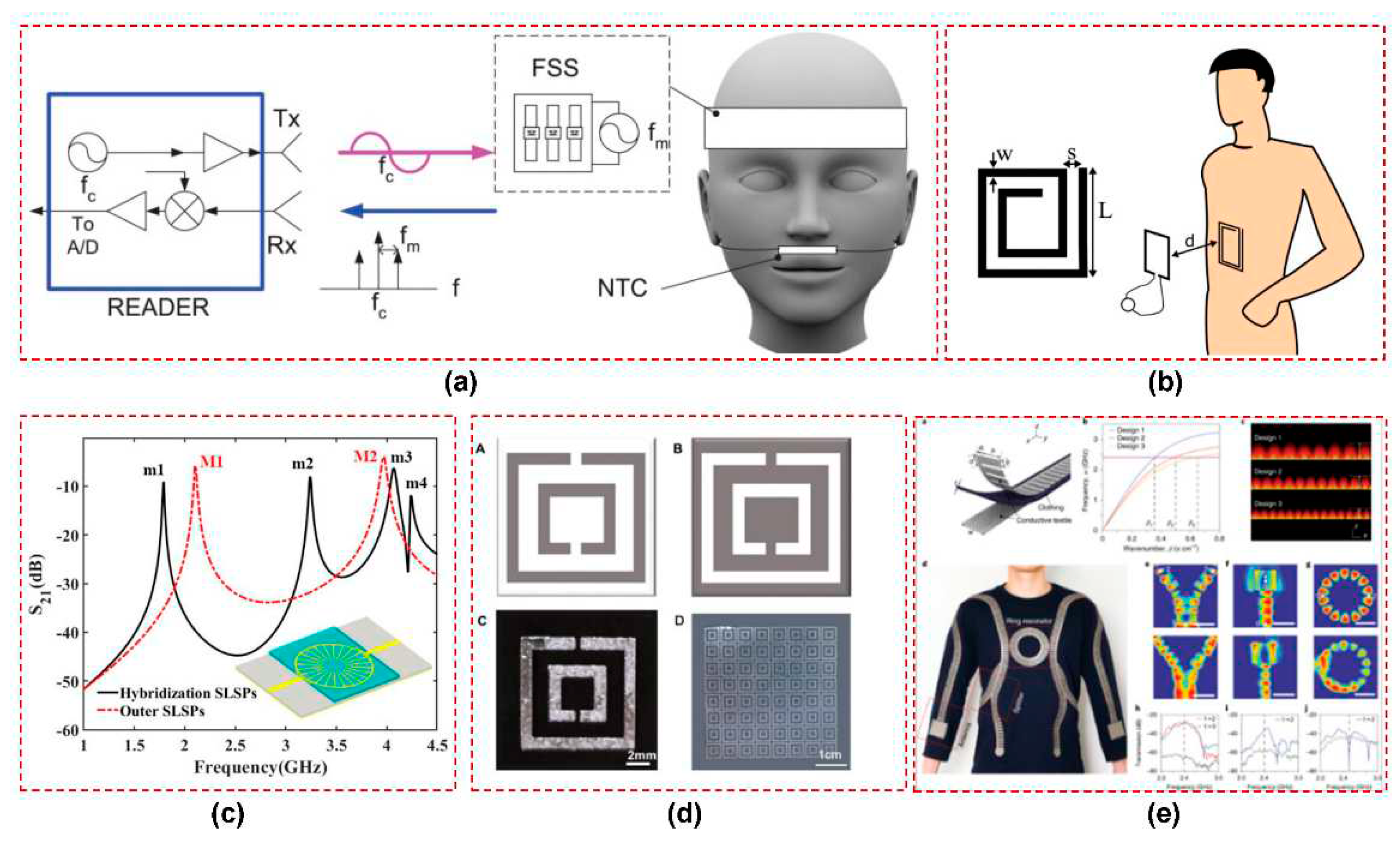
2.1. Antenna Sensors
Antenna sensors have become increasingly prominent in the last few years for the monitoring of vital signs, especially for respiration. The sensing mechanism is primarily based on two factors: chest wall movement and displacement of air volume in the lungs. The movement of the chest wall leads to changes in the physical dimensions of the antenna, while the displacement of air volume alters the dielectric properties in the vicinity of the antenna. Both these effects result in the variation of electrical characteristics of the antenna like its reflection coefficient, resonance frequency, and radiation pattern [
19]. The variations caused by breathing in the reflection coefficient (S11) of antenna sensor can be measured through vector network analyzer (VNA) and then can be processed for estimation of the breath rate and pattern recognition. Of course, this scheme is limited to the laboratory and valid only as a proof of concept. Another more practical method is based on the utilization of a tuned frequency transmitter connected to an antenna sensor and monitoring of the backscatter power intensity or received signal strength indicator (RSSI) at the receiver end. The RSSI varies since the impedance of antenna changes during breathing, therefore, the effective transmitted power also varies accordingly.
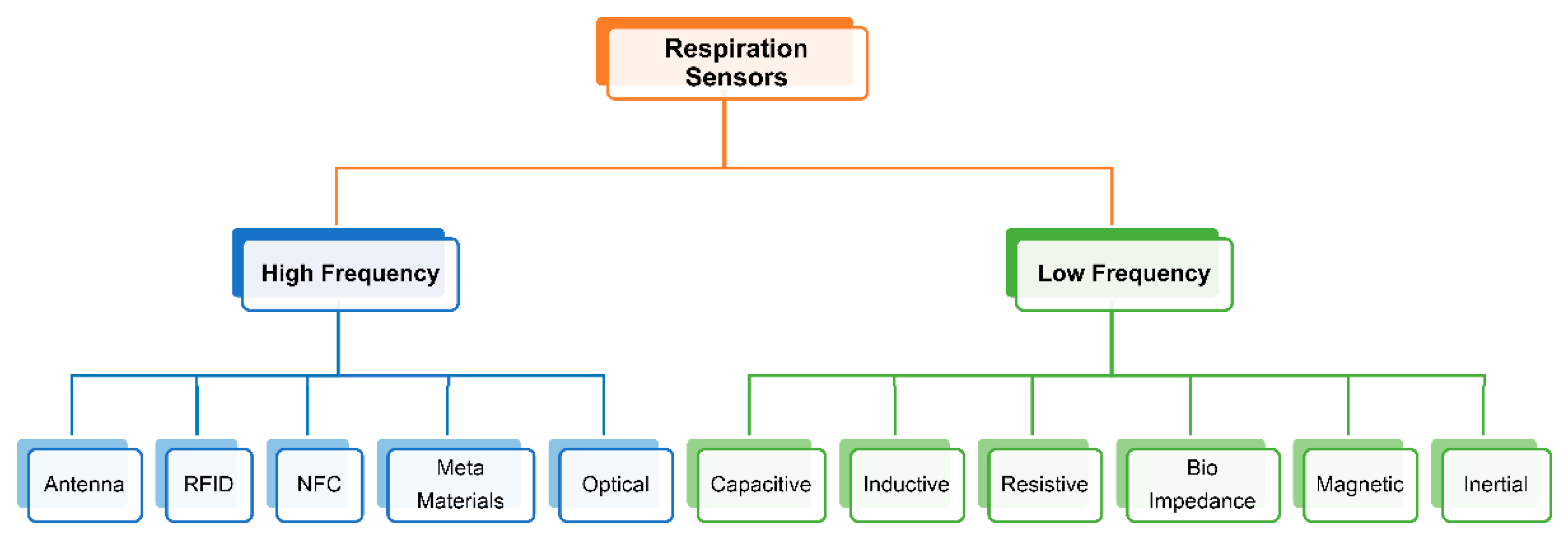
Various types of flexible and wearable antenna-based respiration sensors have been developed for the respiration monitoring. For instance, an embroidered meander dipole antenna-based sensor was integrated into a commercially available T-shirt that detects resonance frequency shifts induced by chest movements during breathing [
20], shown in
Figure 2a. In another study, a wearable strain sensor based on a flexible and sinusoidal dipole antenna is fabricated by utilizing a conductive polymer material [
21], illustrated in
Figure 2b. Similarly, flexible and spiral dipole antennas have been designed using multi-material fibers for the respiration monitoring [
22], as shown in
Figure 2c. Moreover, a low-profile fully textile antenna was used as a passive e-textile respiration sensor that relied on the interaction between human body and antenna to detect changes in dielectric properties induced by breathing [
23]. This antenna was implemented using a conductive fabric on a felt fabric substrate that provides simplicity and compatibility with different textiles, as shown in
Figure 2d.
Different commercial RF platforms such as RFID and Bluetooth have been employed for wireless sensing by utilizing the variations in received signal strength indicator (RSSI). 113 For instance, Patron et al. presented a sensor that employed knitted antennas and inductively coupled RFID tags for comfortable and battery-less monitoring of respiration patterns [
24].
Figure 2e depicts a complete RFID based system for the simultaneous respiration monitoring of multiple persons [
25]. Likewise, some portable wireless communication platforms are presented in [
26,
27] that integrate antennas with Bluetooth modules in wearable T-shirts, shown in
Figure 2f. This enables non-invasive and contactless breath detection with potential applications in medical diagnostics and respiratory condition monitoring. Nevertheless, the development of flexible and wearable antenna sensors is accom-panied by several significant challenges. First, achieving conformity to complex surfaces such as the human body poses a key hurdle. These antennas must be able to adapt and conform to irregular and curved surfaces while maintaining reliable signal reception and transmission. Second, balancing performance and efficiency in a compact and flexible form factor is crucial, since the human body acts as a very lossy medium which absorbs and attenuates electromagnetic signals. This results in decreased antenna efficiency, reduced signal transmission range, and altered radiation patterns. Therefore, wearable antennas need to exhibit high radiation efficiency, wide bandwidth, and reliable communication capabilities by carefully tackling these challenges.
In addition, the safety of subjects is also a crucial aspect to consider in the application of antenna sensors. The compliance with specific absorption rate (SAR) limits is essential to ensure the well-being of users. It can be observed from
Figure 2 that dipole antennas are employed mostly for sensing in the UHF and ISM frequency bands due to their simple geometry and ease of fabrication. However, these antennas radiate a substantial amount of power toward the subject also. Thus, further investigations are required into other antenna types that have better safety features for the end users.
2.2. RFID/NFC Sensors
Wireless transmission of sensor data can be achieved through various technologies, including radio-frequency identification (RFID), near field communication (NFC), and Bluetooth. However comparing RFID/NFC technology to Bluetooth, one notable advantage is the potential for batteryless communication. The principle of operation for RFID is backscattering, where the tag receives energy from the reader’s transmission and uses it to send back a reply. In this case, the sensors can derive power from the electromagnetic (EM) field generated by a remote reader.
2.2.1. RFID Sensors
With the advent of the Internet of Things (IoT) era, radio-frequency identification devices (RFID) sensors have gained popularity for wearable sensing. Particularly, passive UHF RFID sensors have been used widely due to their smaller size and no power requirements. These sensors have the advantage of being lightweight and comfortable due to their flexible nature. Typically, RFID systems are utilized for sensing applications in two manners. The first involves the measurement of back-scattered power intensity, while the second entails the transmission of sensor data towards the reader.
For the respiration measurements, the RFID sensors have been mostly used as strain sensors by utilizing the principle of backscattering. In this case, the main sensing element is an antenna which is specially designed according to the impedance of RFID chip and fabricated on a flexible or textile material. When a strain force is applied to an RFID tag, the physical deformation of the embedded antenna causes a shift in its resonance frequency. This results in a variation in the backscattered power (RSSI) transmitted from a passive RFID tag, which can be used as a metric for detecting mechanical deformations. Thus, the RFID-based respiration sensors are designed by correlating the RSSI variation to the mechanical deformation of the RFID antenna. This approach has been demonstrated in various studies for monitoring respiration rate and detecting breathing patterns [
14,
24,
28,
29], as discussed in previous section.
Apart from using RSSI, RFID technology is also utilized to transmit data from other sensors towards the reader. In a study on graphene-based respiration sensing, the AMS SL900A microchip was employed for this purpose [
30]. The SL900A is an Electronic Product Code (EPC) tag that operates in both semi-passive mode (battery-assisted passive) and fully passive mode (without battery) and exhibits power sensitivities of -6.9 dBmW and -15 dBmW in the respective power modes. The EPC chip features a direct connection to the antenna, along with a 10-bit analog-to-digital converter (ADC) capable of controlling two external analog sensors. Additionally, it incorporates an integrated temperature sensor with a programmable dynamic range of -40 to 150°C. This demonstrates that a wearable RFID system with such capabilities enables simultaneous multi-parameter sensing, specifically for humidity and temperature measurements, for subsequent respiration monitoring.
2.2.2. NFC Sensors
NFC is a specific subset of RFID technology that is designed for short-range wireless systems. One significant advantage of NFC over conventional RFID is its ability to facilitate peer-to-peer communication between an NFC-based system and any NFC-enabled smartphone acting as a remote reader. This feature makes NFC technology accessible to individual users and thus expands its potential applications. Similar to RFID, the backscattering technique can be applied to NFC for sensing purposes as well.
An embroidered inductive strain sensor was introduced for respiration sensing that comprises two embroidered planar coils connected in series, and their mutual inductance is influenced by their relative positions [
31]. These coils can serve as antennas for NFC tags modulating the carrier wave from the reader according to the inductance variations of the sensor, which enables wireless extraction of sensing information. Moreover, a NFC based smart bandage incorporating wireless strain and temperature sensors is presented in [
32]. The bandage utilizes a battery-less NFC transponder (RF430FRL152H) as an intermediary between the sensors and a smartphone application. This enables the acquisition and transmission of data from both sensors. The smartphone application can power the system and provide real-time data acquisition from the sensors at a distance of 25 mm. The authors propose potential healthcare applications for the smart bandage, including the assessment of respiratory diseases through its usage as a wearable strain sensor.
Despite the inherent flexibility and lack of power requirements of passive RFID tags, a limitation of these tags is the inclusion of an electronic chip. It limits their large-scale production for wearable applications and renders them susceptible to harsh environmental conditions. Therefore, the future of RFID wearable sensing lies in chipless technology, which is more robust and feasible for production due to the absence of any electronic component [
33].
2.3. Metamaterial Sensors
Electromagnetic metamaterials are man-made materials comprised of structures whose electromagnetic properties are deliberately engineered to offer a range of responses that are difficult or impossible to achieve in naturally occurring materials or composites. The growing popularity of metamaterials in sensing applications is evident from the increasing number of published works utilizing these engineered structures [
34]. In these applications, changes in the resonance frequency or amplitude at resonance are typically used to detect variations in the measured parameter. However, it is worth noting that there are only a small number of studies in the existing literature which employ metamaterials to design flexible and wearable sensors for respiration monitoring.
2.3.1. Frequency Selective Surfaces
Frequency Selective Surfaces (FSS) are two-dimensional planar structures consisting of periodic arrays of sub-wavelength elements. They are designed to selectively transmit or reflect electromagnetic waves based on their frequency. FSSs are widely utilized in the microwave frequency filters, radar absorbing materials (RAMs), and antenna reflectors [
35]. For respiration sensing, a wireless apnea detector is proposed in [
36] that utilizes a passive respiration sensor to measure the changes in airflow temperature during breathing, as shown in
Figure 3a. A transponder based on a modulated FSS is employed that use a backscattered field technique for sensing and is composed of an array of dipoles loaded with varactor diodes. The resistance of thermal sensor changes due to the variations of airflow temperature during breathing which modulates the backscatter response. An algorithm based on peak detection has been used to calculate real-time respiration and apnea intervals. However, this system requires a battery to polarize the FSS and it is rather uncomfortable for the patient due to the many interconnected devices to be worn onto face and head.
Traditional frequency selective surfaces used for sensing present certain limitations in 226 terms of flexibility, as the materials and structures used are rigid. Therefore, liquid metal based technologies [
39] and textile based substrates [
40] are feasible options that can be explored for designing flexible metamaterials for wearable applications, as depicted in
Figure 3d and
Figure 3e.
2.3.2. Spiral Resonator Tag
Planar spiral structures (SRs) are commonly used as lumped inductors in microwave circuits and also serve as a fundamental element for metamaterials [
41]. The inductance of a spiral is determined by its geometry (such as square, circular, or polygonal), number of turns, turn width, and spacing between turns. A breath rate sensor based on an SR tag is illustrated in
Figure 3b that is printed on a thin, flexible textile substrate suitable for wearable applications [
37]. The sensor detects respiratory movement of the abdomen during inspiration and expiration. A microstrip probing loop serves as the reader antenna and measures the variation in the real part of input impedance, caused by the change in the normal distance between the probing loop and the SR tag. Thus, the respiratory rate is 240 obtained by analyzing the amplitude-modulated signal captured by the probe. However, 241 the sensor was employed to experimentally measure the breath rate of a test subject in a quasi-real scenario. Therefore, to enhance the capabilities of the presented sensor, future advancements should focus on transitioning from the quasi-real environment to a fully operational setting by integrating signal acquisition board.
2.3.3. Surface Plasmons Resonators
Spoof localized surface plasmons (LSPs) are electromagnetic modes that are highly confined and can be realized using various techniques such as textured metal surfaces, thin metal layers and conductive textiles [
40,
42,
43]. These modes can be used to design wearable sensors by detecting changes in localized electromagnetic fields. Although, these modes are associated with strong subwavelength confinement, which is a characteristic feature of LSP resonances. However, they also extend into the surrounding space evanescently, enabling interactions for sensing and mode excitation.
Figure 3c shows the structure of a typical spoof LSP resonance sensor with patterned conductive structure.
A wearable textile sensor based on LSP resonances is proposed for vital sign monitoring like breathing and heartbeat in [
44]. The sensor is placed on the chest and excited remotely through a curved dipole antenna. Small movements of the chest during breathing and heartbeat change the resonant frequency of the sensor that is remotely monitored from the excitation source. Moreover, an energy-efficient and secure wireless body sensor network (WBSN) interconnected through radio surface plasmons on metamaterial textiles is introduced [
40]. This conductive fabric has shown a three-times improvement in transmission efficiency compared to conventional radio networks. While, wireless communication remains confined to within 10 cm of the body, ensuring greater privacy and security as well. This textile can be used in conjunction with a range of sensors including respiration sensors for the monitoring of vital signs.
Surface plasmons resonators have generally very high-quality factor since the electric field is confined in very limited space. However, these sensors face challenges in terms of fabrication complexities and sensitivity to the environment. Therefore, further research is needed for their reliable performance in the context of wearable sensing.
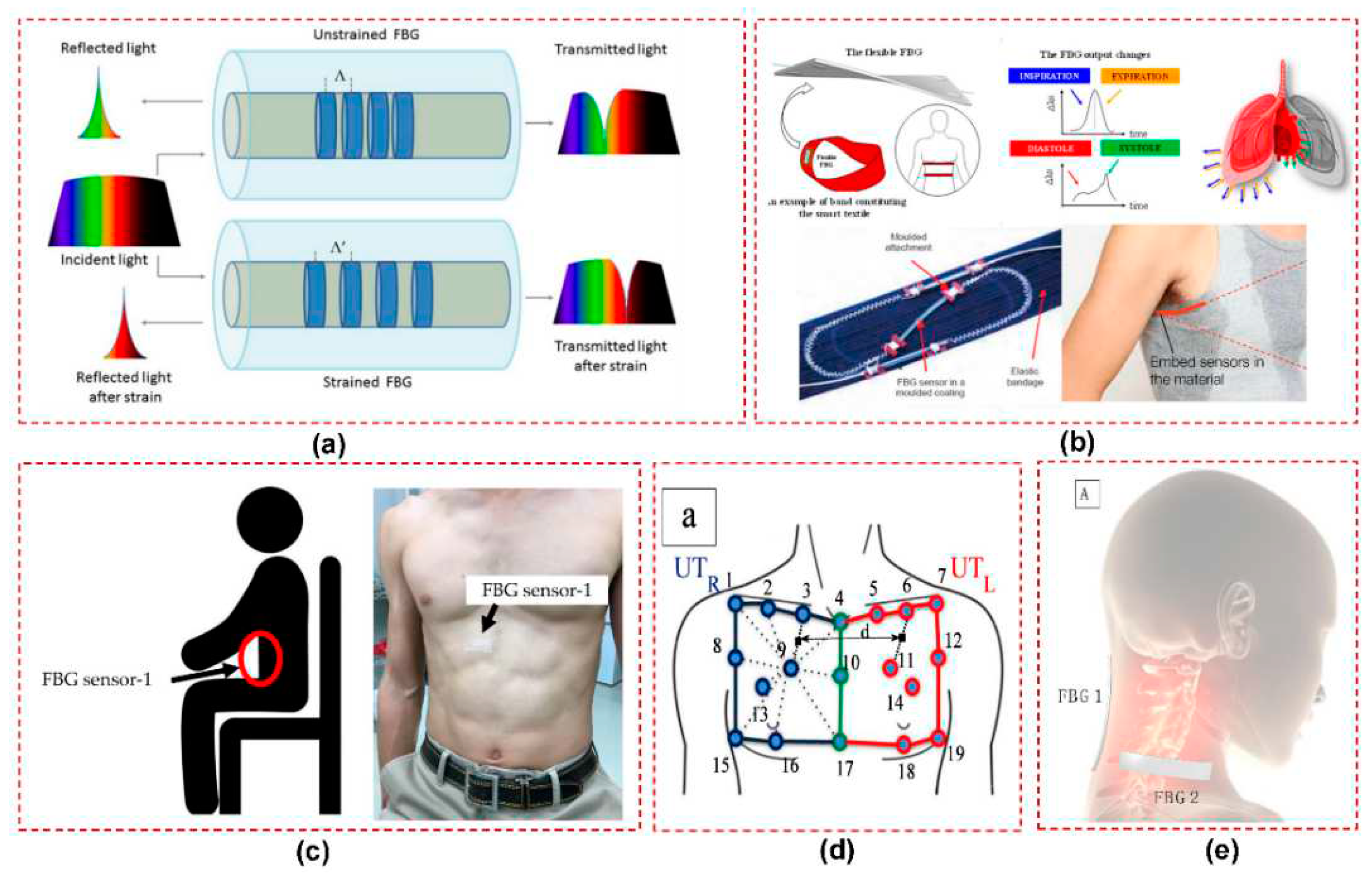
2.4. Fiber Bragg Gratings
Fiber Bragg Grating (FBG) sensors are well-suited for measuring biophysical parameters, including the respiratory behavior of the chest and abdomen regions. These sensors are comprised of fiber optic grating that reflects a specific wavelength of light [
45], as shown in
Figure 4a. When the FBG undergoes strain or displacement caused by breathing, its reflected wavelength has a corresponding shift. This shift is directly proportional to the applied strain or displacement, enabling FBG sensors to accurately measure and monitor breathing patterns. Various applications of FBG sensors are illustrated in
Figure 4b for the monitoring of vital signs including cardiac and respiration activities [
46]. Koyama et. al demonstrated in a study that FBG sensors can efficiently detect respiratory strain on the abdomen, chest, and shoulder region [
47], as shown in
Figure 4c.
FBG sensors are especially advantageous during MRI testing due to their immunity to strong magnetic fields. There is a study that was focused on proposing the design and assessment of an MR-compatible smart textile that utilizes six FBGs [
48]. The objective was to non-intrusively monitor and characterize a patient’s respiration. The chest wall kinematics during breathing was employed to optimize the positioning of FBGs on the textile and to improve their sensitivity in monitoring compartmental volume changes.
Figure 4d illustrates a similar study where the positioning of the FBGs on the textile is led by an optoelectronic system [
49]. Another study evaluated an MR-compatible smart textile with FBG sensors for monitoring respiratory and cardiac activities during apnea and quiet breathing [
50]. The results showed the accurate measurement of respiratory parameters and heart rate are obtained without image artifacts in the MR environment.
Furthermore, elastic belts integrated with optical fibers for monitoring breathing activities were studied in [
51]. The aim was to assess the impact of volunteers’ positions on the breathing patterns detected by the optical fibers. Experiments were conducted using fiber bragg grating sensor arrays to monitor breathing patterns. Two sets of FBG arrays, each comprising five sensors, were placed at specific locations on the body - the abdomen and chest. The diversity technique was employed to enhance detection accuracy. Results showed consistent accuracy for individuals, though variations were observed among the two volunteers. In the same year, a wearable system was proposed by utilizing two fiber bragg grating sensors positioned on the neck to monitor neck movements and breathing [
52], as depicted in
Figure 4e. The system effectively captured flexion-extension, axial rotation, and respiratory frequency parameters with comparable performance to optical reference systems. The estimated mean and breath-by-breath respiratory frequency values exhibited errors 6.09% and 1.90% during quiet breathing and tachypnea, respectively, demonstrating high accuracy. Additionally, a 3D-printed sensor using fiber bragg grating (FBG) technology was introduced for respiratory and heart rate monitoring [
53]. Each sensor was equipped with a single FBG fully encapsulated within a 3D-printable flexible material during printing.
The biggest challenge associated with FBG sensors is that the optical fibers are typically rigid and fragile. Therefore, they need to be encapsulated in some material that can provide protection, flexibility, and biocompatibility to make them suitable for flexible and wearable applications. This encapsulation shields the FBG sensor from external influences, such as moisture, mechanical stress, or bending, which could compromise its performance or cause damage.
3. Low-Frequency Sensors
Various low-frequency sensors have been developed to enable non-invasive and continuous breath monitoring. These sensors are often characterized as simple and passive devices that typically operate at sub-megahertz frequencies and do not require an external power source for their operation. Also, these are relatively straightforward in design and implementation often consisting of basic lumped components designs such as capacitors, resistors, coils, or electrodes. The following section discusses the most commonly used low-frequency techniques for flexible and wearable respiration sensors.
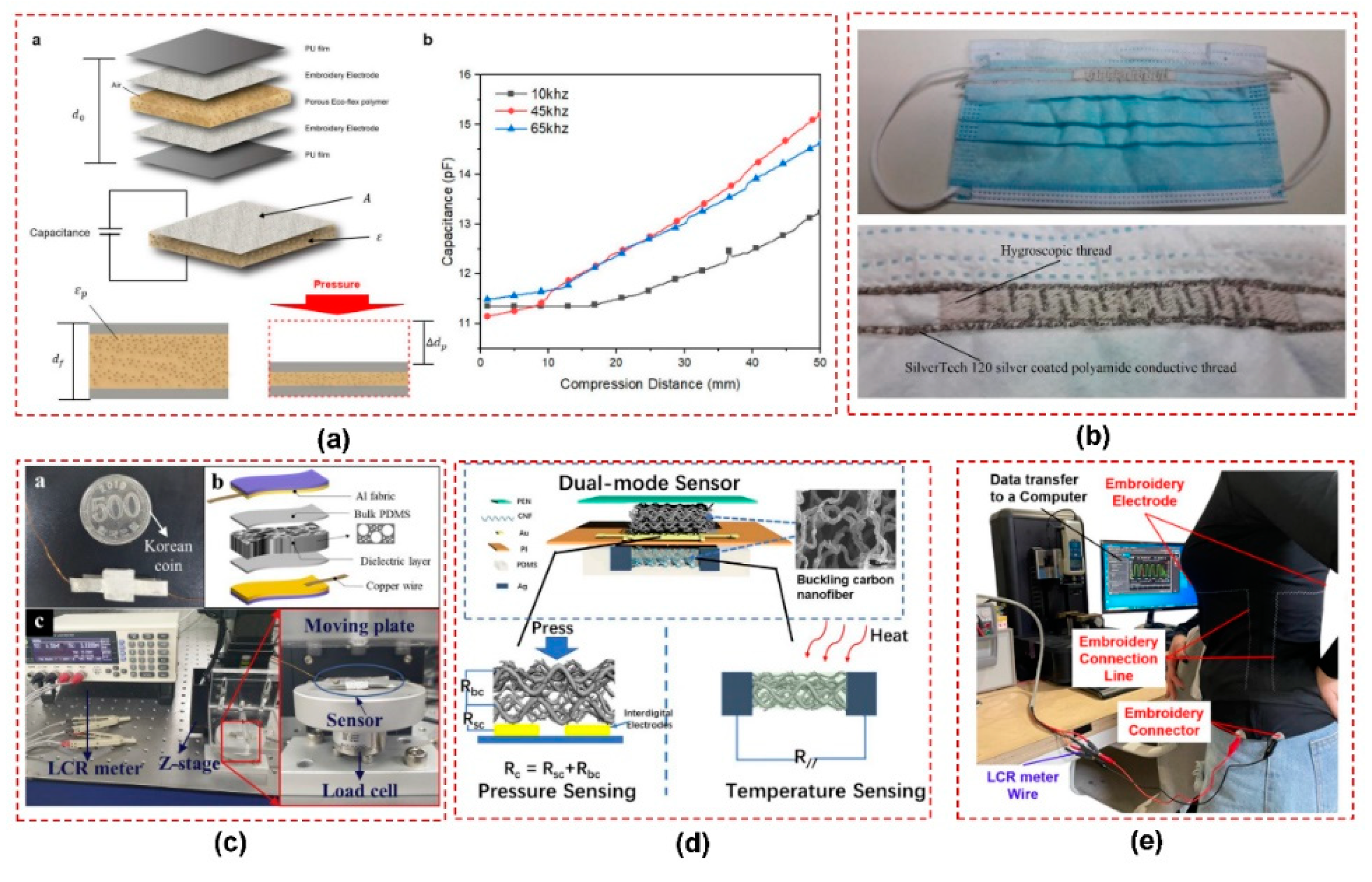
3.1. Capacitive Sensors
Capacitive sensors are a type of flexible wearable sensor that has shown promising scope for monitoring breathing and respiration. The working principle of a capacitive sensor relies on the variation in capacitance due to changes in electrode dimensions, the separation distance between electrodes, or dielectric properties. These changes allow the capacitive sensor to detect physical quantities like strain, pressure, or humidity. Capacitive sensors have been utilized on the human body for detecting breathing in various ways. They can measure chest expansion and contraction during respiration by detecting changes in capacitance. Additionally, these sensors could be employed to detect air humidity from exhaled breath for monitoring respiration. Another approach is to measure the pressure on the abdomen and chest during exhale which can be used to monitor respiratory movements.
The simplicity of capacitive sensor working principle has led researchers to explore various fabrication techniques and materials to improve flexibility and sensitivity for wearable applications. A flexible capacitive sensor has been developed with high sensitivity, a large sensing range, and stability [
54]. The sensor utilizes a micro-structured polydimethylsiloxane (PDMS) film embedded with multi-walled carbon nanotubes as the conductive electrode and a smooth PDMS film as the dielectric layer. The sensor is successfully applied for monitoring arterial pulse waves and breathing. Furthermore, a design of highly-sensitive capacitive sensors is reported for wearable sensing applications, using conductive textile electrodes and polyurethane (PU) foams as the dielectric layer. Unlike previous works that involved complex fabrication processes, this work presents a simple and cost-effective technique using microporous PU foam as the dielectric material [
55]. A compression sensor is illustrated in
Figure 5a where the porous Ecoflex dielectric was placed between embroidered electrodes and changes in capacitance were measured to assess the respiration [
56].
Furthermore, a facemask with inter-digital embroidered capacitor is proposed for respiration monitoring [
57], shown in
Figure 5b. The sensor operates by exploiting the humidity of exhaled air for monitoring respiration. A paper-based wearable screen printed sensor is proposed for respiration monitoring particularly for those patients affected by SARS-CoV-2 [
58]. The sensor utilizes traditional screen printing methods to fabricate interdigitated electrodes composed of multi-walled carbon nanotubes (MWCNTs) and polydimethylsiloxane (PDMS) composite on a paper substrate. The paper substrate functioned as a humidity-sensitive material due to its hygroscopic properties. As a result, the capacitance of the sensor varied in response to the changes in the dielectric constant during inhalation and exhalation. In another study, a flexible paper-based capacitive pressure sensor is fabricated using daily use materials such as paper, polyester conductive tape, and polyimide tape [
59]. The sensor has a wide pressure detection range and also demonstrated successful application in various scenarios, including the nasal respiration analysis. Additionally, a capacitive sensor has been made with co-doped barium titanate dielectric and palladium-silver electrodes in [
60]. Two construction methods, screen-printed and microdispensed, are evaluated. The sensors demonstrate suitable characteristics for respiration monitoring, with the screen-printed sensors chosen for experimentation and prototyping due to their dynamic range.
Similarly, a sensor for wearable electronics has been fabricated using hierarchically porous PDMS composites with a simple and cost-effective method of screen printing [
61], as shown in
Figure 5c. The resulting sensor exhibits a wide pressure measurement range, high sensitivity, and flexibility, making it suitable for various applications in wearable electronics including respiration. Furthermore, a smart face mask with a dual-sensing mode respiration sensor is presented for recognizing multiple respiration patterns [
62]. By incorporating three-dimensional carbon nanofiber mats, the sensor enables simultaneous pressure and temperature sensing, allowing for real-time recognition and accurate monitoring of up to eight respiration patterns, as depicted in
Figure 5d. The mask has potential applications in health monitoring and early detection of breathing-related diseases. Moreover, a fabrication strategy for a multi-functional e-textile based on polypyrrole (PPy) and rose-like silver flower-decorated knitted cotton/spandex fabric (KCSF) is presented in [
63]. It enabled the construction of a capacitive sensor with an ultra-wide working pressure range and high sensitivity. In addition, Ecoflex rubber has been effectively used as a dielectric in capacitive sensors for respiratory measurements. Wearable capacitive pressure sensors were developed for human activity and respiration monitoring, with Ecoflex and silver nanowires serving as the dielectric and electrodes, respectively [
64,
65].
Kang et al. developed a respiration sensor by utilizing a variable parallel-plate capacitive design, incorporating nonwoven fabrics [
66]. The sensor comprised both stretchable and non-stretchable fabric segments that responded to respiratory movements, leading to alterations in sensor length. Moreover, a capacitive sensor was developed based on textiles, designed to be worn around the chest as a belt for respiration rate monitoring [
67]. The sensor utilizes the change in capacitance resulting from the expansion of fabric during respiration, achieving a high precision level in the micrometer range. A zinc-ion hybrid supercapacitor (ZHS) with a double-crosslinked hydrogel electrolyte is developed in [
68] which serves as both an energy storage device and a self-powered sensor for human movement and breathing detection. Moreover, a respiration sensor based on a parallel capacitor embroidered on textiles is proposed [
69]. In this research, a respiration capacitor has been characterized using a silver thread and a porous Ecoflex material simulating lung air. The study then examines actual breathing patterns, including normal breathing, deep breathing, hyperventilation, and apnea, using a clothing-type respiration sensor, as shown in
Figure 5e.
Conversely, capacitive sensors have some limitations when considering their usage in respiration sensing. One limitation is the sensitivity to environmental factors such as humidity and temperature, which can affect the accuracy of the measurements. Additionally, the placement of electrodes on the textile substrate may introduce variability in the signal due to movement or displacement during breathing. Therefore, calibration and compensation techniques are necessary to account for these variations.
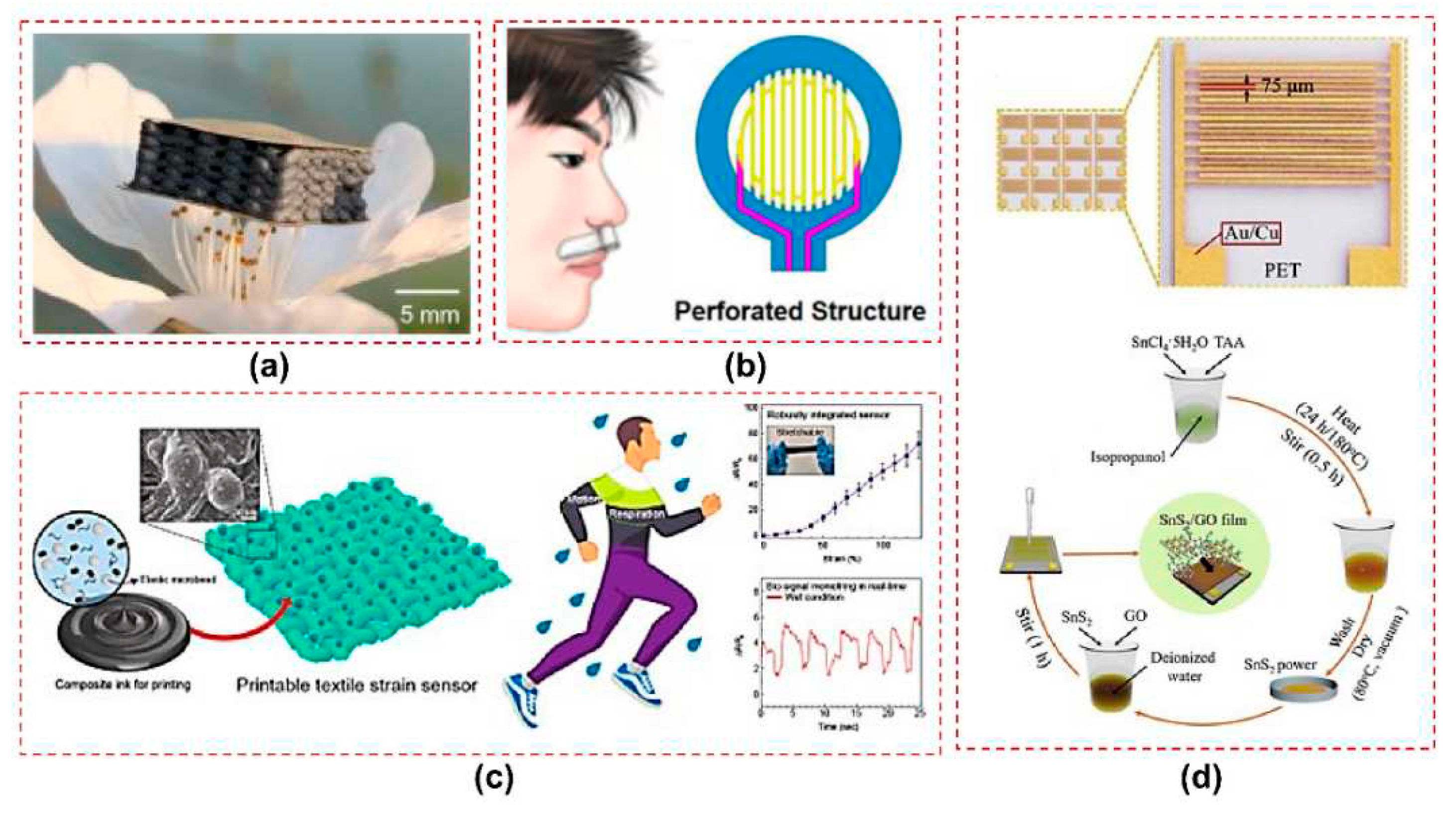
3.2. Resistive Sensors
Resistive sensors for respiration monitoring employ different sensing mechanisms, including strain sensing, temperature sensing, and humidity sensing. Strain sensing involves a flexible material that changes resistance in response to respiratory movements, enabling measurement of respiratory volume or rate. Most strain sensors employ resistive techniques due to the direct proportionality between the resistance of conductive materials and strain. Several hydrogel-based flexible strain sensors with self-healing capabilities and high sensitivity have been proposed for human motion and respiration monitoring [
70,
71]. Furthermore, textile strain sensors have been designed for conductive yarns by combining them with elastic yarns or making them elastic by their coating with carbon-filled silicon [
72,
73]. Moreover, flexible dual parameter sensors are introduced to enhance the functionality of wearable devices, with hierarchical porous structures for fully decoupled pressure and temperature sensing [
74], as shown in
Figure 6a. A flexible and perforated nasal-based respiratory sensing system is introduced in [
75], which has improved airconvection efficiency and thermal sensitivity, as shown in
Figure 6b. Platinum was selected as a sensing material due to its stable physical and chemical properties. Moreover, its resistance-temperature characteristics exhibit excellent linearity and rapid thermal response. A printable wet-resistive textile strain sensors have been introduced in [
76], demonstrating high sensitivity and mechanical durability for robust wearable electronics, as depicted in
Figure 6c. This composite strain sensor was successfully printed on a tracksuit to enable real-time monitoring of respiration and arm motion signals.
Various flexible humidity sensors based on different materials were explored for vital sign monitoring by measuring the impedance. Highly sensitive textile-based humidity sensors employing graphene oxide/Polypyrrole composites have been developed for realtime respiration monitoring [
77,
78]. The field of humidity sensing has seen advancements with printed flexible humidity sensors utilizing cellulose nanofiber-based composites [
79]. A flexible humidity sensor was proposed based on a poly 3D hollow fiber membrane, that exhibits high sensitivity, selectivity, and stability for monitoring physiological activity [
80]. In addition, a graphene oxide-based breath sensor was demonstrated to have high sensitivity to humidity and potential applications in detecting lung cancer and sleep apnea [
81]. Another study focuses on a Coolmax/graphene-oxide functionalized textile humidity sensor with ultrafast response, designed for monitoring human activities [
82]. Furthermore, an ultrasensitive humidity sensing capability was achieved using a tin disulfide/graphene oxide nanoflower composite with an ultrafast response, low hysteresis, and good reversibility, making it promising for wearable applications [
83], as shown in
Figure 6d. Additionally, a few-layer NiPS3 nanosheet-based flexible humidity sensor was developed, offering high selectivity, rapid response, and recovery times for real-time monitoring of respiration and environmental conditions [
84]. Several other flexible and wearable resistive sensors have been designed by employing composites of polymers, carbon, and thermoplastics [
85,
86,
87]. Despite the potential advantages, resistive sensors are susceptible to drift and hysteresis, leading to potential inaccuracies in measurements. Variations in resistance can be introduced by changes in temperature and humidity. In addition, to ensure accurate respiratory monitoring, signal processing techniques are necessary to address noise and extract relevant respiratory information.
3.3. Magnetic Induction Sensor
Magnetic Induction (MI) is a non-contact technique used to measure changes in the impedance distribution of an object. It relies on the electromagnetic coupling between a coil and an object in close proximity. Human tissue is also characterized as an electrical medium that is both inhomogeneous and anisotropic in nature. The impedance distribution within the thorax is influenced by physiological activities such as breathing, which can be attributed to various factors including volume changes and displacement of organ boundaries. Currently, three primary categories of flexible inductive sensors are extensively employed: eddy current sensors, mutual-inductive sensors, and self-inductive sensors.
For the eddy current method, the coil is driven by an alternating current, generating a primary alternating magnetic field that penetrates the conductive medium surrounding it, thereby inducing eddy currents within the medium. These eddy currents, in turn, generate a secondary alternating magnetic field that interacts with the primary field, resulting in changes in the coil’s impedance. These changes are directly related to the impedance distribution of the object. When the coil is positioned in front of the thorax, the thorax acts as the object under test, and the coil’s impedance varies in response to the variation in thoracic impedance distribution caused by the movement of the lungs. In a study [
88], a system was introduced for long-term monitoring of respiration and pulse. The system utilizes four non-contact sensors based on magnetic eddy current induction, which are integrated into a shirt, as shown in
Figure 7a. The effectiveness of the system in monitoring respiration and pulse was demonstrated through measurements conducted on healthy volunteers. Similarly, a flexible device is presented for non-contact monitoring of respiration and pulse [
89]. It combines magnetic induction for respiratory monitoring and reflective photoplethysmography (rPPG) for pulse detection, enabling enhanced signal coverage. Sensor signals are processed by a microcontroller and wirelessly transmitted via Bluetooth to a display unit, such as a personal computer or Android device. The device can easily be placed in a shirt or jacket pocket for the monitoring of vital signs.
Inductive sensors can also measure physical quantities, such as displacement and pressure, with high sensitivity by utilizing the principles of mutual inductance. Inductivebased displacement sensors utilize electromagnetic induction to measure and monitor object displacement or position. These sensors generate an alternating magnetic field using a coil, and the movement of the object induces a change in the magnetic field, allowing for displacement measurement. An embroidered inductive strain sensor has been proposed [
31] which is fabricated using off-the-shelf conductive yarns and can be woven onto clothing such as shirts or sweaters. The sensor consists of two embroidered planar coils connected in series, with their mutual inductance affected by their relative positions. The displacement between the coils alters the inductance, enabling the sensor to function as a strain sensor. Moreover, a paper-based self-inductive folding displacement sensor (PSIFS) has been proposed in [
90] which operates on the principle of inductance variation caused by the three-dimensional deformation of a planar inductor coil, as depicted in
Figure 7b. The research focuses on investigating the structural design principles concerning two key aspects of sensitivity and size. The PSIFS has demonstrated the capability to accurately identify and differentiate various breathing states and motion states of human joints.
Magnetic induction sensors in respiration monitoring can be susceptible to measurement errors caused by external electromagnetic interference. It is essential to employ calibration and compensation techniques to mitigate variations in the magnetic field arising from different body positions or environmental factors. Furthermore, careful consideration of the sensor’s design and placement relative to the body is crucial to optimize measurement accuracy.
3.4. Piezoelectric Sensors
Piezoelectric sensors are fabricated using piezoelectric materials, which exhibit an internal polarization phenomenon when subjected to an external force. This phenomenon leads to the appearance of positive and negative charges on the surfaces of the piezoelectric material, resulting in the generation of a piezoelectric potential. Upon removal of the external force, the polarization phenomenon disappears. Thus by detecting variations in the electrical signal, sensors can be designed by using piezoelectric sensors during respiration monitoring.
3.4.1. Piezoelectric Sensors & Generators
Several studies have proposed the use of piezoelectric sensors as part of multifunctional sensing technologies. These studies aim to integrate multiple smart functions into wearable sensors by employing hybrid mechanisms [
91,
92]. In addition, researchers have explored the development of self-powered sensors for portable and wearable devices, aiming to overcome the limitations of operational time, rigid characteristics, and bulky size associated with conventional power sources. For instance, a flexible hybrid nanogenerator is presented that combines a solar cell, a transparent triboelectric nanogenerator, and a piezoelectric nanogenerator [
93].
Similarly, Zhu at el designed a self-powered hybrid electronic skin that combines triboelectric and piezoelectric effects to enable wearable multi-sensing [
94], as shown in
Figure 7c. Moreover, a nanogenerator has been developed and utilized as a flexible active respiratory sensor [
95]. In addition, flexible piezoelectric smart-textile sensor and energy harvester have been developed [
96]. The sensor demonstrates its effectiveness and sensitivity in detecting various activities, such as tiny water droplets, footstep detection, and breathing detection. A nasal-based sensor has been proposed on a thin film of piezoelectric polyvinylidene fluoride (PVDF) for the purpose of monitoring respiratory patterns [
97]. The cantilever beam of the sensor affects by the exhaled air from the nostrils and generates a dynamic voltage signal based on the piezoelectric effect.
3.4.2. Piezoelectric Resonators
Piezoelectric-on-substrate (TPoS) is a specific type of piezoelectrically actuated resonators designed with a piezoelectric layer on top of a substrate layer. The incorporation of the substrate layer enhances power handling capabilities and improves the quality factor of the resonator. For respiratory monitoring applications, it is crucial to have a TPoS resonator that exhibits high sensitivity to changes in respiration flow, as well as a high electromechanical coupling and quality factor.
A wireless sensor utilizing a thin-film piezoelectric-on-substrate (TPoS) resonator has been employed for respiratory monitoring [
98]. The passive wireless sensor comprises an antenna and a resonator, where the resonator detects the respiration profile. The resonator used in this investigation consists of a stack of Molybdenum, Aluminum and Nitride deposited on a diamond substrate. During inhalation and exhalation, TPoS resonators experience two distinct effects. Firstly, the temperature difference between exhaled breath and the resonator induces a frequency shift due to alterations in the elastic properties of the resonator’s constituent materials. Secondly, the condensation of water vapor from exhalation onto the resonator’s surface causes a frequency drift. The TPoS resonator is integrated with an RFID tag’s antenna and respiration monitoring is achieved through back-scattering techniques.
The successful integration of piezoelectric materials into wearable sensors needs meticulous design considerations to ensure mechanical stability and durability. The accuracy of measurements can be compromised by sensor drift and noise, necessitating the implementation of suitable signal-processing techniques. Calibration and compensation methods are imperative to address individual variations and ensure consistent and reliable measurements.
3.5. Bioimpedance Sensors
Bioimpedance sensors for respiration monitoring operate based on the principle of measuring changes in electrical impedance caused by respiratory movements. These sensors typically consist of electrodes that are placed on the skin surface, creating a closed electrical circuit [
99], as shown in
Figure 7d. When the person breathes, the expansion and contraction of the chest or abdomen lead to changes in the thoracic impedance. These changes in impedance are caused by variations in the conductivity and volume of the underlying tissues and organs. Thus, respiratory patterns can be continuously tracked by measuring these impedance variations.
Impedance sensors play a crucial role in breath monitoring, offering a non-invasive and continuous approach to track respiratory patterns and gather valuable health information. Several articles explore the use of such flexible sensors for monitoring physiological activities. For instance, a wearable smart clothing system was proposed, integrating numerous sensors for accurate respiratory rate estimation in homecare monitoring [
101]. Additionally, a portable physiological signal recorder was designed and implemented, achieving a 24-hour operating time and focusing on electrocardiography, bioimpedance, and user activity 5measurements [
102]. Moreover, the development of a wearable monitoring system named Wealthy enabled continuous remote monitoring of electrocardiogram and impedance pneumography signals, along with the discrimination of different breathing patterns using piezoresistive fabric sensors [
72]. Furthermore, a textile sensing system was employed for the simultaneous acquisition of electrocardiogram and impedance pneumography signals using fabric sensors and electrodes [
103].
In addition, a wearable scheme incorporating electrical impedance tomography (EIT) belt was designed with a novel active electrode architecture, high image frame rate, and wide operating bandwidth, enhancing the neonatal thorax monitoring for vital signs [
15]. Moreover, the integration of MEMS stethoscope, ambient noise sensing, ECG, impedance pneumography, and 9-axial actigraphy into a wearable multimodal stethoscope patch allowed for long-term auscultation and high-quality signal acquisition [
104]. Additionally, a high frame rate wearable EIT system utilizing active electrode ASICs was developed, achieving accurate measurement of EIT signals for lung respiration and heart rate monitoring [
105]. Lastly, an energy-efficient and reconfigurable sensor IC was implemented to improve bioimpedance spectroscopy and ECG recording in wearable health devices by enhancing the accuracy of signal measurements [
106].
Bioimpedance measurements are sensitive to electrode placement and contact quality, requiring careful attention to ensure consistent and reliable measurements. Calibration procedures and algorithms are necessary to accurately interpret impedance changes related to respiration and distinguish them from other physiological signals.
3.6. Inertial Sensors
The primary characteristic of respiration involves the movement of air in and out of the lungs, which results from the expansion and contraction of the lungs. The associated ribcage movement can be detected through inertial sensors [
100,
107], as evident from
Figure 7e. These sensors offer versatility and non-obtrusiveness, making them suitable for various applications and providing a reliable and cost-effective method for collecting motion data. A wearable multi-sensor patch was developed for the purpose of detecting and recognizing human breathing patterns [
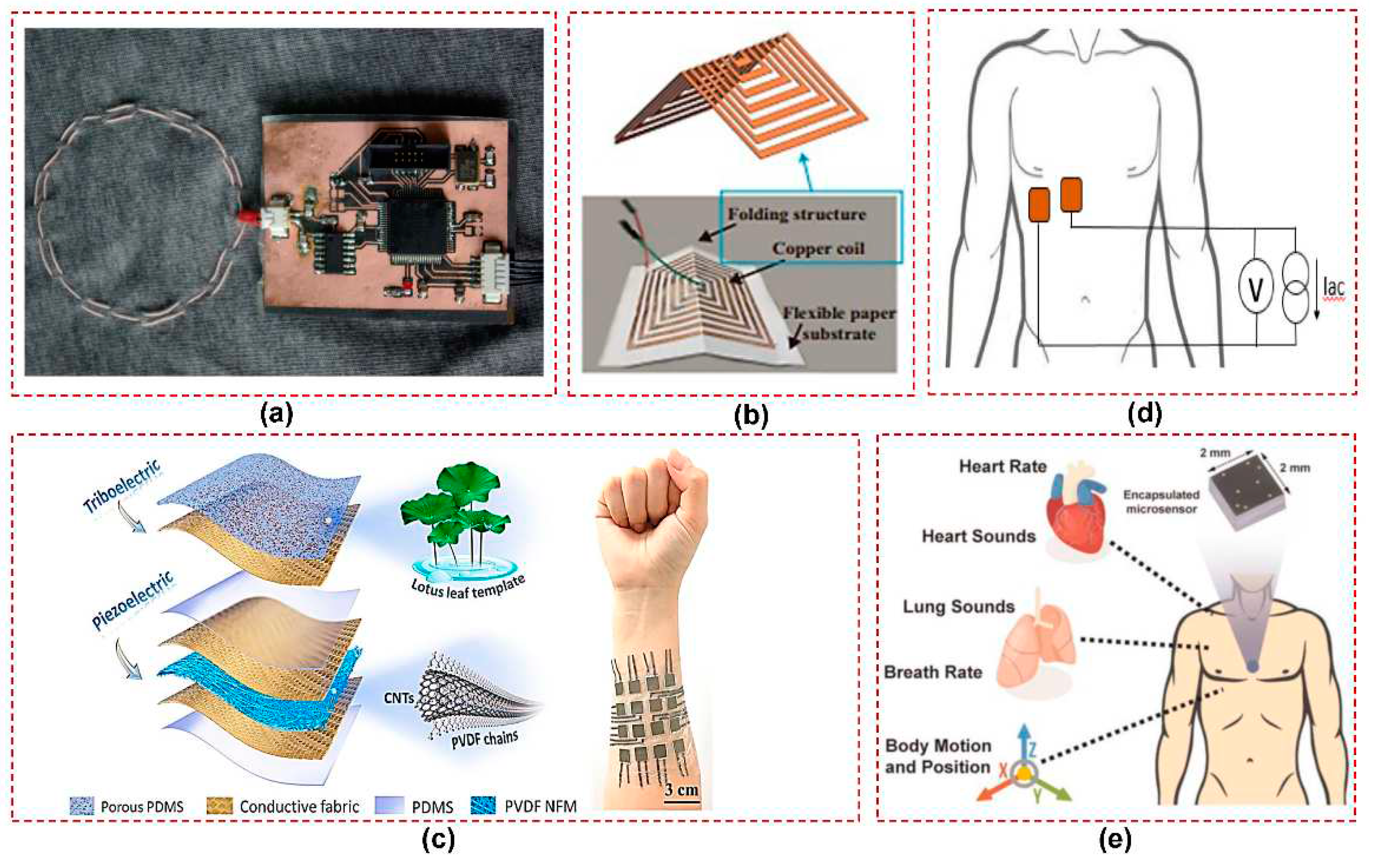
108]. The multi-sensor patch, composed of an accelerometer and a pressure sensor, was shown to accurately measure breathing-related inertial motion and muscle stretch when attached near the diaphragm. Through analysis of different breathing motions, including inhale, exhale, normal breathing, and breath-hold conditions, the breathing frequency and normal breathing rate were determined using the accelerometer and flexible capacitive pressure sensors.
However, mostly inertial measurement units (IMUs) are incorporated for capturing motion data and facilitating activity monitoring in conjuction with other sensors. For instance, the NeoWear system was developed to monitor neonatal vital signs using a sensor belt which comprises a pressure sensor and an Inertial Measurement Unit (IMU) [
109]. The system detects respiration rate and apnea events by analyzing the pressure and movement data of respective sensors. The accuracy of inertia-based methods for detecting body movements can be affected by motion artifacts. In the context of respiration monitoring, motion artifacts can undermine the ability to accurately capture and analyze respiratory patterns, potentially leading to erroneous or incomplete results. Therefore, mitigating and minimizing the impact of motion artifacts is a critical consideration when developing and implementing inertial sensors for respiration monitoring.
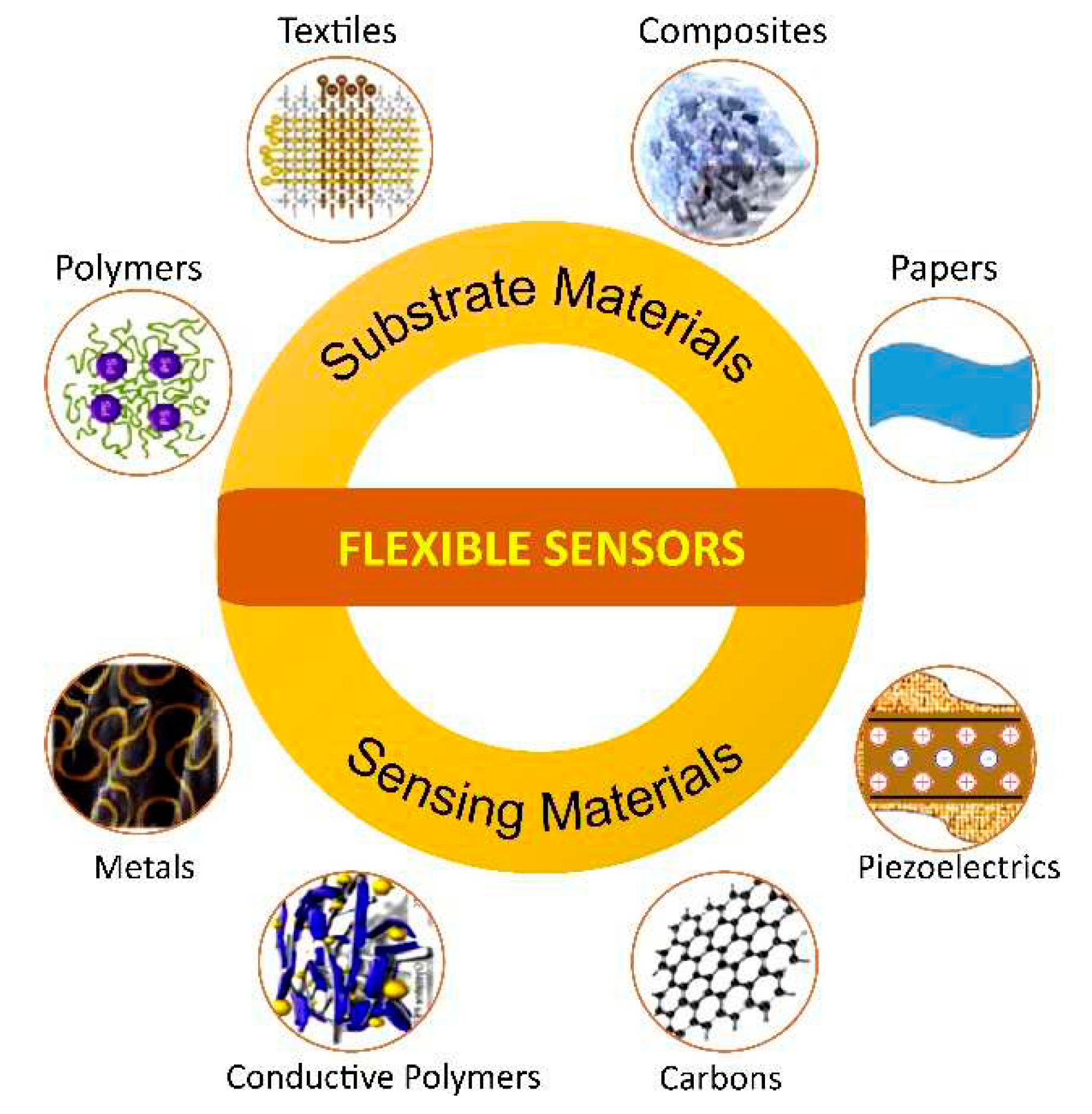
4. Materials and methods for manufacturing respiration sensors
Several materials and techniques have been explored for the fabrication of flexible wearable sensors so far. The fundamental requirement for these sensors is to exhibit improved performance when applied to the human body, while also possessing material flexibility, biocompatibility, and user’s comfort. The sensors primarily comprise two components: the substrate and the sensing elements connected by metallic interconnectors. The subsequent section provide a brief overview of the substrate and sensing materials utilized in the context of respiration sensors, as depicted in
Figure 8.
4.1. Substrate Materials
The substrate selection plays a crucial role in designing wearable sensors, as it is essential for ensuring that the sensor can conform to the body’s contours, withstand movements, and maintain optimal performance, resulting in a satisfactory user experience in wearable sensor technology [
110].
4.1.1. Polymeric Materials
Polymer-based materials have been extensively used as substrates for flexible sensors. These are high weight molecules composed of repeating units and exhibit distinct characteristics based on their internal bonds. Polymers offer tunable chemical, structural, and electrical properties, making them attractive candidates for sensing applications. Several types of polymer-based materials have been used as substrates for flexible wearable respiration sensors. Polydimethylsiloxane (PDMS) is a silicone-based elastomer known for its excellent flexibility, biocompatibility and optical transparency, and it is most commonly used substrate material for wearable sensors [
54,
61]. It has also been used as an encapsulation material for protecting fragile sensors such as FBGs [
53]. In addition, Polyurethane (PU) has also been used for the respiration sensors [
55,
86] as it is softer than PDMS. Polyimide (PI) is another prevalent substrate material for wearable sensors, which has been used for flexible wearable sensing due to its high tensile strength and flexibility [
59,
111,
112]. Furthermore, rubbers such as Ecoflex are employed for breathing applications being a skin-safe substrate material [
64,
65]. These rubbers have modulus similar to that of human skin which enhances their adaptability to the human body.
4.1.2. Textiles and Fabrics
Wearable sensor technologies have witnessed significant advancements in utilizing fabric and textile materials as substrates. These materials offer flexibility, durability, and comfort, making them highly suitable for a wide range of applications. Flexible sensors integrated into textile materials offer comfort, wearability, and ease of use. Several articles focus on the integration of sensors into fabric and textiles, enabling real-time monitoring of vital signs and respiration. For instance, wearable antennas and sensor tags are embroidered or printed on fabric substrates, ensuring unobtrusive and comfortable monitoring experiences [
20,
37]. These materials have been successfully utilized in various applications, such as knitted antennas that utilize wool, lycra, and conductive fabrics to achieve both elasticity and functionality [
14,
24]. Particularly, cotton T-shirts serve as an ideal platform for such applications, providing both comfort and convenience to the subject [
21,
22,
26,
27]. In terms of specific sensing techniques, strain sensors have been fabricated on stretchable fabrics woven with fine yarns [
76], while pressure sensors have utilized knitted cotton/spandex fabric [
63]. Additionally, textile-based sensors have been developed for monitoring respiration through capacitive sensing [
69]. Textile-based capacitive sensors are also fabricated using screen-printed silver ink electrodes on non-stretchable nonwoven textiles, providing flexibility and robustness [
67]. Moreover, fabric-based electrodes [
101] and metamaterial textiles [
40] are employed to facilitate the wearable sensing. Furthermore, some other textile substrates such as nonwoven fabrics [
66] and knitted fabrics [
72] have been explored for cardio-respiratory monitoring. The utilization of fabrics and textiles substrates demonstrates the versatility and potential of integrating sensors and antennas into wearable technologies, enabling the development of comfortable, functional, and personalized smart textiles.
4.1.3. Composites Materials
A variety of composite materials that used different types of materials have been investigated for their applicability in respiration sensors. Thin films of Si/SiO2 multilayer composite serves as the substrate for the piezoelectric respiration sensors [
30,
91]. In another study, co-doped barium titanate has been used for the capacitive respiration sensor as deielectric , which allows the miniaturization and flexibility [
60] . Furthermore, hydrogel composites that are soft and stretchable materials have been employed for the monitoring of vital signs [
70,
71]. A zinc based hydrogel is employed as the dielectric material for the development of a supercapacitor for the self powered sensors [
68]. In addition, a composite material consisting of sodium alginate, polyacrylamide, and gallium is employed for a strain-sensitive hydrogel that could be used in wearable electronic devices [
77].
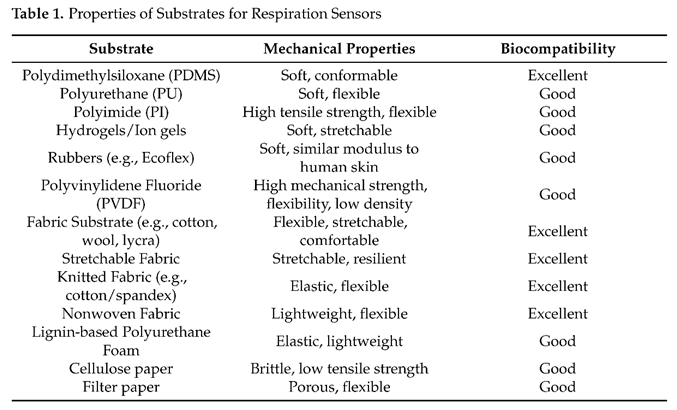
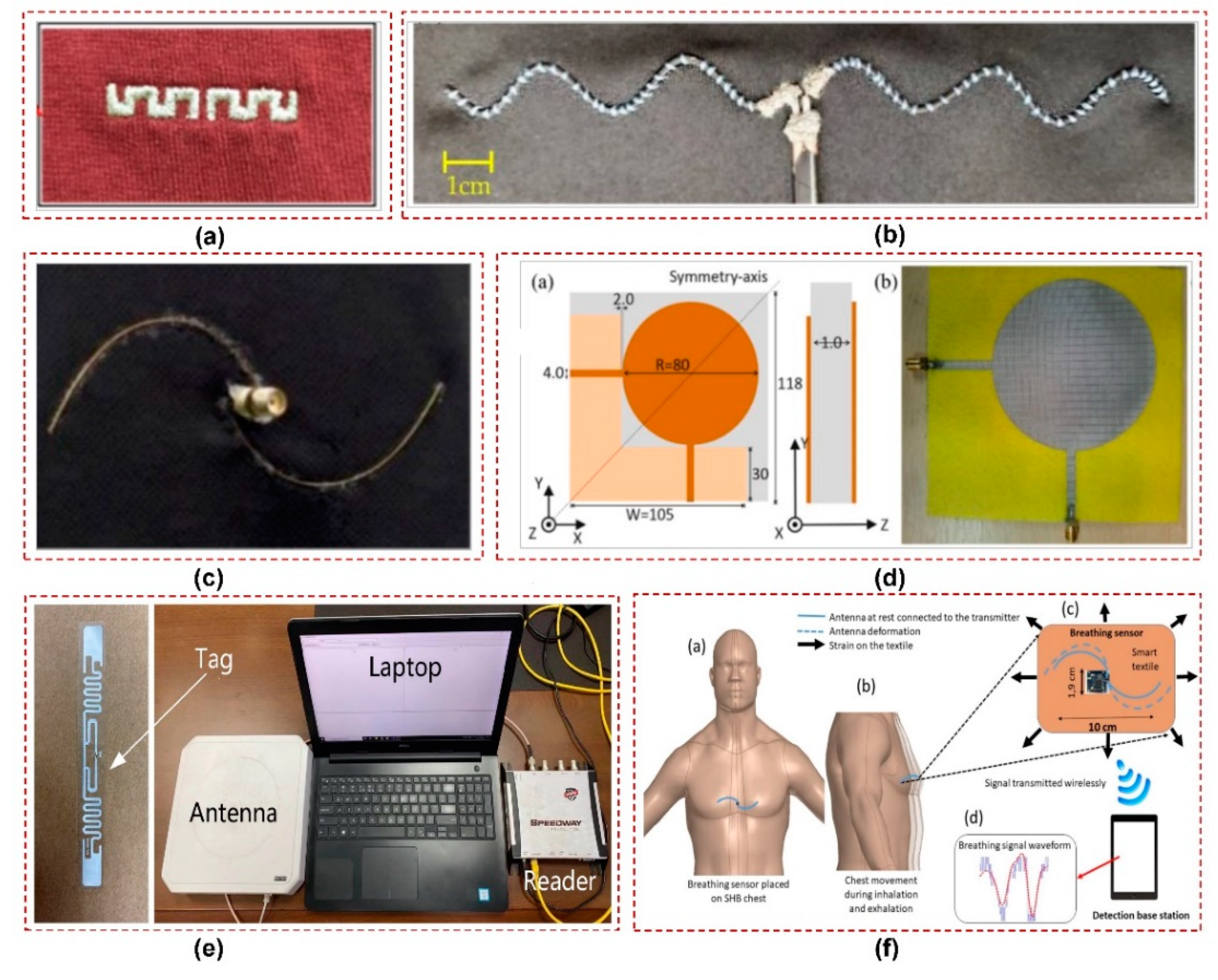
The mechanical and biocompatibility characteristics of commonly used substrate materials are summarized in Table 1.
4.1.4. Paper-Based Materials
Paper substrates have been used in the field of flexible sensing due to their unique properties, such as low cost, flexibility, and ease of fabrication. For instance, a simple and low-cost approach is proposed to fabricate a flexible paper-based capacitive pressure sensor using common materials [
59], where paper is used as a dielectric material and polyester conductive tape as flexible electrodes. Moreover, a noninvasive wearable screen-printed sensor is proposed for human respiration monitoring [
58]using pressure sensing technique. The proposed sensor utilizes multi-walled carbon nanotubes (MWCNTs) and polydimethylsiloxane (PDMS) composites on a paper substrate. Likewise, a paper-based self-inductive folding displacement sensor (PSIFS) was proposed for monitoring human respiration that uses common paper material and copper tape.
4.2. Sensing Materials
Wearable sensors rely on various materials to enable their sensing capabilities and enhance their overall performance. These materials are carefully chosen based on their specific properties and the requirements of the sensor design. The conductivity of surfaces plays a critical role in the operation of various respiration sensors, such as resistive, capacitive, inductive, and antenna-based sensors, etc. since these sensors depend on the surface conductivity to facilitate precise detection and measurements.
4.2.1. Metallic Materials
Metallic materials are used in sensors due to their excellent electrical conductivity, which enables efficient signal transmission and sensing capabilities. For instance, a high-frequency litz wire is integrated into a textile shirt for making a coil for magnetic induction sensor [
88]. Furthermore, the utilization of an ultrathin metal film on a textured metallic disk enables the detection of multipolar spoof localized surface plasmons for breathing monitoring [
42]. Another approach involves a fully embroidered meander dipole antenna-based sensor integrated into a T-shirt, where the conductive part of the antenna sensor is composed of a silver-coated nylon thread [
20]. Similarly, a wearable strain sensor for biomedical monitoring employs a conductive layout knitted with highly conductive silver-coated yarns, resulting in a flexible and conductive fabrics [
24]. Lastly, a wearable sensor for non-contact monitoring of respiratory and heartbeat movements employs conductive textiles as the active sensing material [
44]. The sensor consists of two layers of conductive textiles on a cloth substrate, with a top layer patterned as a disk-like resonator and a bottom layer acting as a ground plane.
In addition, conductive inks and paints have emerged as an effective material for the printing of sensors in the field of wearable technology . These offer numerous advantages, including flexibility, low-cost fabrication, and compatibility with various substrates. Silver conductive ink has been used to create the sensing areas on nonwoven fabrics, enabling seamless integration into everyday clothing for textile-based respiration sensors [
66,
67]. Moreover, composite inks composed of elastomers, carbon particles, and PDMS microbeads have been used for printable textile based strain and humidity sensors, which offer conductivity as well as flexibility [
76,
79]. Besides this, the temperature sensor of a smart bandage is fabricated by forming electrodes with conductive silver paint on a flexible PVC substrate [
32]. Thus, metallic materials play indispensable role in the sensor systems by either contributing to sensing mechanisms or providing interconnects.
4.2.2. Carbon based materials
Various types of carbon materials, including carbon nanotubes, graphene, and MXene have been used to fabricate the wearable sensors for respiration sensors. Carbon nanotubes are cylindrical structures made of carbon atoms arranged in a hexagonal lattice with diameters on the scale of nanometer and are classified into two main types: single-walled carbon nanotubes (SWCNTs) and multi-walled carbon nanotubes (MWCNTs). To address the need for cost-effective and non-invasive respiratory monitoring, researchers have explored the use of multi-walled carbon nanotubes (MWCNTs) and polydimethylsiloxane (PDMS) composites [
54,
93,
94]. These materials are utilized in the development of low-cost and reliable wearable sensors for human respiration monitoring. The integration of MWCNTs and PDMS in paper-based sensors offers an alternative solution to existing systems that require direct contact with the body and expensive monitoring equipment [
58]. Furthermore, a biocompatible and lightweight respiration sensor consisting of highly oriented carbon nanotube (HO-CNT) films embedded between polyacrylonitrile (PAN) layers is presented with excellent flexibility and robustness [
113]. Moreover, a combination of lignin-based polyurethane foam and multi-walled carbon nanotubes (MWCNTs) has been used to provide conductivity and large surface area [
86].
Another popular carbon-based material is graphene which is a single layer of carbon atoms arranged in a two-dimensional honeycomb lattice. It is also employed in breath analysis due to its remarkable properties such as biocompatibility, low cost, and ease of functionalization [
30]. In addition, MXene which is a conductive and hydrophilic material belonging to a class of two-dimensional inorganic compounds has been used for respiration sensing. MXene has been integrated into a melamine sponge (MS) structure to create a 3D bifunctional flexible sensor [
78]. This MXene-based sensor exhibits excellent response to pressure and humidity making it a versatile choice for respiration sensing applications. Moreover, to achieve mechanical robustness and high operational stability under dry and wet conditions, researchers have employed composite inks composed of polyurethane elastomer, carbon black nanoparticles, poly(3-hexylthiophene-2,5-diyl) (P3HTs), and PDMS microbeads [
76]. These flexible textile strain sensors offer promising capabilities for integration into wearable applications for breath monitoring.
4.2.3. Conductive Polymers
Conductive polymers have emerged as promising materials for sensor applications due to their unique combination of electrical conductivity, mechanical flexibility, and tunable properties. For instance, a combination of polyethylene-co-vinyl acetate (PEVA) polymer and multi-walled carbon nanotubes (MWCNTs) has been utilized for antenna fabrication [
21] for respiratory strain sensing. Multi-material fibers are another approach for developing respiration sensors. These fibers combine different materials to achieve enhanced performance and functionality in sensing applications. For respiration sensors, polyimide-coated hollow-core silica glass capillaries with a silver layer have been utilized as multi-material fibers [
22,
27], that offers mechanical flexibility of polymers and the conductive properties of the silver. In another study, poly (3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS) polymer, which is a transparent conductive polymer with high ductility, has been proposed to design a flexible strain sensor [
32]. Such conductive polymers can be integrated into antenna designs and other sensing applications to enable accurate respiration monitoring.
The electrical and mechanical characteristics of commonly used sensing materials are summarized in Table 2.
4.2.4. Piezoelectric Materials
Various piezoelectric materials have been employed in sensing for their ability to generate electrical signals in response to mechanical pressure or strain. Materials such as polyvinylidene fluoride (PVDF) film and lead zirconate titanate (PZT) film have been used as sensing materials in respiration sensors. PVDF film is utilized in nasal sensors for noninvasive respiratory monitoring [
114] and is also employed as the piezoelectric material in a self-powered active sensor for respiration monitoring [
115]. A piezoelectric PZT thin film is utilized in a multifunctional wearable device that monitors motion and respiratory frequency [
91]. The development of flexible hybrid nanogenerators has incorporated materials such as fluorinated ethylene propylene (FEP), nanocomposite of barium titanate (BaTiO3) and MWCNTs, enabling energy harvesting and healthcare monitoring [
93]. Moreover, a battery-free electronic skin is proposed that combines PDMS and MWCNTs-doped PVDF for multi-modal sensing [
94]. The PVDF is also extensively utilized in smart textile-based harvesters and sensors for the sake of self-powering and respiratory monitoring [
96].
4.2.5. Optical Fibers
Optical fibers are thin, flexible, and transparent strands made of high-quality glass or plastic materials that can transmit light signals over long distances with minimal loss. These have been extensively utilized in fiber bragg gratings (FBGs) sensors for strain sensing. These sensors, based on the principle of periodic variation in refractive index along an optical fiber, offer unique advantages such as compatibility with magnetic resonance imaging (MRI) and immunity to electromagnetic interference [
48]. The lightweight and small-sized FBG sensors enable their integration into wearable systems, such as elastic belts, ensuring comfort and flexibility for users [
51]. Usually, the FBG sensors need to be encapsulated into flexible materials such as silicone rubbers to enhance their practicality and usability in wearable devices for respiratory rate and heart rate monitoring applications[
52,
53].
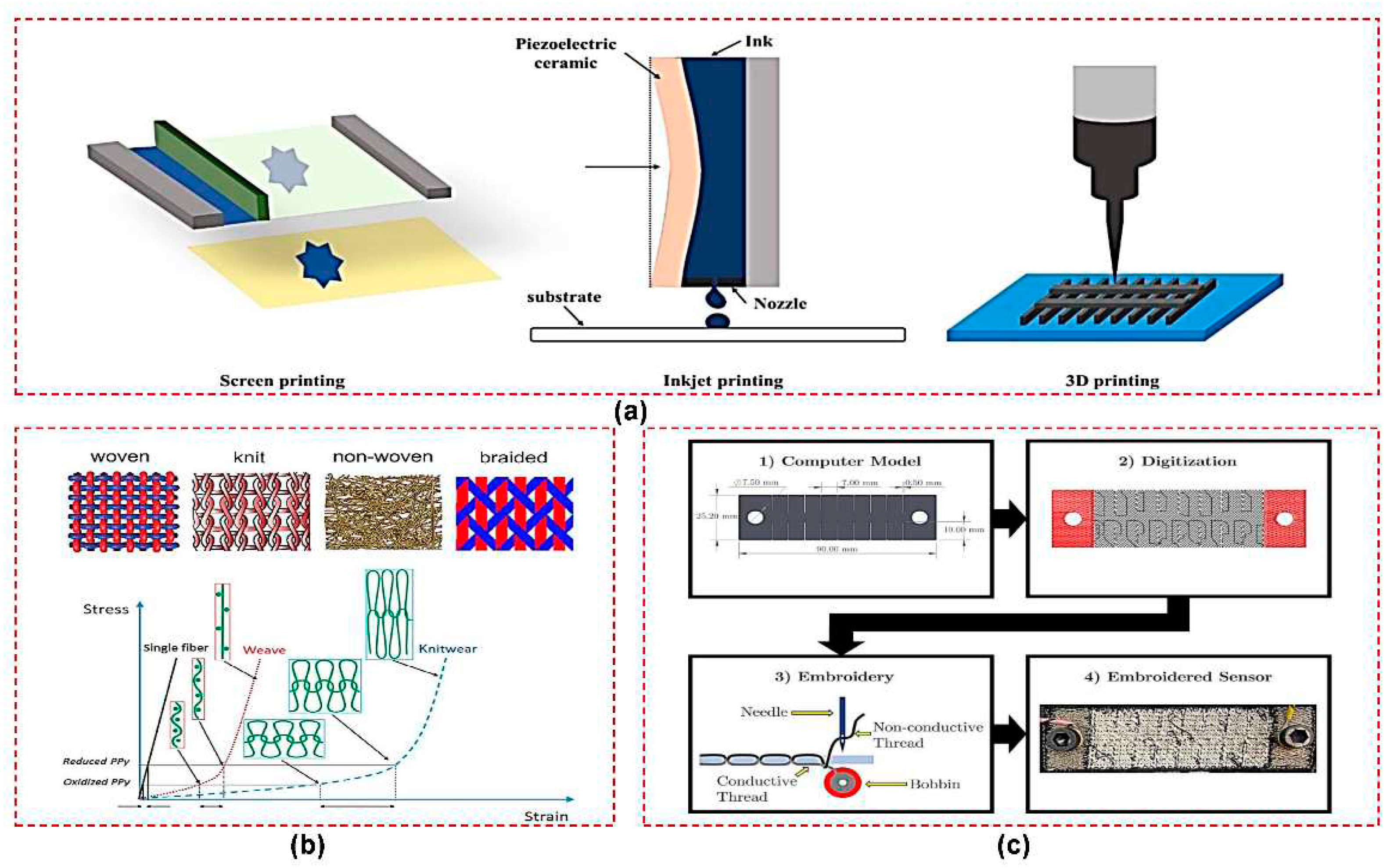
4.3. Fabrication Techniques
Several existing fabrication techniques have been utilized to design functional and reliable sensors for a range of wearable applications. In this review, we summarize common fabrication techniques employed for wearable sensors, focusing on their application in breath monitoring.
4.3.1. Printing
Various printing techniques, including screen printing, inkjet printing, and 3D printing, are employed in the fabrication of wearable sensors, as shown in
Figure 9a. Screen printing is a frequently used technique in the fabrication of wearable sensors. It involves the deposition of conductive inks onto substrates through a mesh screen. This technique enables the creation of sensor electrodes, interconnections, and routing with high precision and repeatability. The use of conductive inks, such as silver or carbon-based inks, ensures good electrical conductivity while maintaining flexibility. Screen printing has been applied in the fabrication of capacitive sensors for respiration monitoring, where the ink is selectively deposited to create electrode patterns on the sensor substrate [
58,
60]. Moreover, screen printing is equally feasible for the non-woven textile and substrates, as demonstrated in [
66,
67]. Similarly, a textile strain sensor is fabricated using the screen printing process, where the composite ink is printed onto the stretchable fabric to create the sensor [
76]. This technique offers the advantage of scalability and cost-effectiveness, making it suitable for large-scale production of wearable sensors.
Other printing techniques such as inkjet printing and 3D printing, are also employed in wearable sensor fabrication. Inkjet printing allows for the precise deposition of functional materials, such as conductive inks or graphene oxide solutions, onto substrates to create sensors with high resolution and customization capabilities. The droplet-based nature of inkjet printing enables the creation of intricate sensor designs and the integration of multiple sensing elements on a single substrate. This technique has been utilized in articles where conductive inkjet printing is employed to fabricate wearable sensors [
36,
37]. On the other hand, 3D printing enables the fabrication of complex sensor structures and the integration of different materials. By layer-by-layer deposition of materials, 3D printing allows for the creation of sensor components with varying mechanical properties and functionalities. This technique has been utilized for the fabrication of various parts of respiration wearable sensors[
53,
74]. Altogether, the printing techniques offer high resolution and design freedom, enabling the development of customized wearable sensors with unique geometries and functionalities.
4.3.2. Knitting
Knitting and weaving techniques are employed in the fabrication of wearable sensors using conductive fibers or yarns. These techniques allow for the integration of conductive elements directly into the textile substrate, enabling seamless and flexible sensors. Conductive fibers or yarns, such as metal-coated fibers or carbon nanotube yarns, are incorporated during the knitting or weaving process to create conductive paths within the textile structure, as depicted in
Figure 9b. For instance, a wearable antenna is fabricated using conductive yarns and knitting techniques [
24], where good conductivity is ensured by using a 99% pure silver-plated nylon yarn with tightly knitted loops. Similarly, a wearable system that integrates fabric sensors, electrodes, and connections, all made using knitting techniques for remote health monitoring is proposed in [
103]. Moreover, the fabrication of a multifunctional e-textile is explained in [
63], which incorporates polypyrrole on a knitted cotton/spandex fabric.
Additionally, CNC knitting machines are employed to seamlessly produce and integrate various components in a single knitting process, including sensors, antennas, conductive fabric, nonconductive fabric, and PCB pocket for a batteryless wearable compression sensor [
14]. Moreover, circular knitting machines are used to design fabric electrodes for respiratory monitoring, enabling accurate measurements of resistance under different conditions [
101]. Furthermore, a combination of knitting technology and coating printing industrial processes is utilized to fabricate knitted and printed sensors for a wearable monitoring system [
72]. The approach of knitting and weaving offers the advantage of simultaneous sensor fabrication and textile production, eliminating the need for additional 847 assembly steps.
4.3.3. Embroidery
Embroidery has been utilized in the fabrication of wearable sensors for various applications, including real-time breath monitoring. In this technique, conductive threads or yarns are embroidered onto the textile substrate to create sensor electrodes and connectors. The electrical conductivity of the threads can be optimized for desired sensor performance by carefully controlling the stitching pattern and density. For instance, an embroidered antenna-based sensor is proposed for real-time breathing monitoring by using a commercial 2-ply conductive yarn [
26]. The layout of the embroidered meander dipole antenna sensor is converted into a digital stitch pattern and embroidered on a commercially available T-shirt using an embroidery machine, as illustrated in
Figure 9c. This system has successfully demonstrated the real-time wireless monitoring of breathing patterns. Similarly, a textile-based, embroidered passive strain and displacement sensor is developed using standard embroidery processes and commercially available conductive yarns [
29]. Lastly, a wearable sensor for detecting respiration is created by embroidering conductive thread onto the fabric to form the electrodes and the connection terminals and circuit [
69]. The integration of conductive elements through embroidery allows for comfortable and unobtrusive sensor placement on clothing or other wearable garments.
Therefore, this technique offers several advantages, including the ability to create flexible and stretchable sensors that can conform to the shape of the human body.
5. Conclusions and Perspectives
The review shows that low-frequency and high-frequency sensors both have been effectively utilized in respiration sensing, offering unique advantages while facing specific challenges. Low-frequency sensors provide direct measurements of respiratory movements with simple designs and wide frequency response. However, challenges exist in terms of hysteresis, electrode-to-skin contact, motion artifacts, and environmental interference. On the other hand, high-frequency sensors offer wireless and contactless operation with communication capabilities. Nevertheless, challenges arise in terms of power consumption, data transmission, and complexity in design. Furthermore, it is learned that a diverse range of materials has been employed in the realm of respiration sensors, ranging from polymers and textiles to metals and carbon-based substances. Obviously, these materials possess both advantages and limitations in the context of specific applications. Therefore, key considerations shall include materials with properties like flexibility and biocompatibility to ensure long-term operation without causing discomfort to the user. Moreover, commonly used fabrication techniques, such as printing, knitting, and embroidery, are discussed and assessed based on factors such as the design resolution of the sensor, manufacturing cost, and their suitability for large-scale production.
In the perspective of future research, high-frequency sensors have emerged as a promising trend in the field of respiration sensors due to their ability to simultaneously sense and communicate breathing information in a compact form factor. In the context, antenna sensors and RFID sensors have shown promise as viable candidates for this purpose. Additional research can focus on enhancing the design of wearable antenna sensors to minimize radiation exposure to users. Furthermore, exploring chipless RFID sensors as an alternative to chip-based RFID can facilitate large-scale production and ensure long-term operation. Moreover, the integration of metamaterial with these existing sensors holds great potential by offering advantages such as tunability and enhanced sensing capabilities. Additionally, flexible metamaterials are very versatile on their own, as these could be used in smart textiles for sensing, shielding, and energy harvesting. Therefore, opportunities for further research lie in the optimization of metamaterial designs and fabrication techniques to enable their seamless integration into wearable devices for diverse sensing applications, including respiration monitoring.
Funding
This work was supported by the Spanish Government-MICINN under Projects TED2021-131209B-I00 and PID2021-124288OB-I00.
References
- Koncar, V. 1—Introduction to Smart Textiles and Their Applications. In Smart textiles and their applications; Elsevier: Amsterdam, The Netherlands, 2016; pp. 1–8. ISBN 978-0-08-100574-3. [Google Scholar]
- Morris, D.; Schazmann, B.; Wu, Y.; Coyle, S.; Brady, S.; Hayes, J.; Slater, C.; Fay, C.; Lau, K.T.; Wallace, G.; et al. Wearable sensors for monitoring sports performance and training. In Proceedings of the 2008 5th International Summer School and Symposium on Medical Devices and Biosensors. IEEE; 2008; pp. 121–124. [Google Scholar]
- Nayak, R.; Wang, L.; Padhye, R. Electronic textiles for military personnel. In Electronic Textiles; Elsevier, 2015; pp. 239–256. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Kluge, F.; Gaßner, H.; Hannink, J.; Pasluosta, C.; Klucken, J.; Eskofier, B.M. Towards Mobile Gait Analysis: Concurrent Validity and Test-Retest Reliability of an Inertial Measurement System for the Assessment of Spatio-Temporal Gait Parameters. Sensors 2017, 17, 1522. [Google Scholar] [CrossRef] [PubMed]
- Kinkeldei, T.; Zysset, C.; Cherenack, K.; Troster, G. A textile integrated sensor system for monitoring humidity and temperature. In Proceedings of the 2011 16th International Solid-State Sensors, Actuators and Microsystems Conference, Beijing, China, 5–9 June 2011; pp. 1156–1159. [Google Scholar] [CrossRef]
- Pantelopoulos, A.; Bourbakis, N.G. A Survey on Wearable Sensor-Based Systems for Health Monitoring and Prognosis. IEEE Trans. Syst. Man Cybern. Part C Appl. Rev. 2010, 40, 1–12. [Google Scholar] [CrossRef]
- Nemati, E.; Deen, M.J.; Mondal, T. A wireless wearable ECG sensor for long-term applications. IEEE Commun. Mag. 2012, 50, 36–43. [Google Scholar] [CrossRef]
- L’her, E.; N’guyen, Q.-T.; Pateau, V.; Bodenes, L.; Lellouche, F. Photoplethysmographic determination of the respiratory rate in acutely ill patients: validation of a new algorithm and implementation into a biomedical device. Ann. Intensiv. Care 2019, 9, 11. [Google Scholar] [CrossRef]
- Ebell, M.H. Predicting pneumonia in adults with respiratory illness. Am. Fam. Physician 2007, 76. [Google Scholar]
- Churpek, M.M.; Yuen, T.C.; Huber, M.T.; Park, S.Y.; Hall, J.B.; Edelson, D.P. Predicting Cardiac Arrest on the Wards: A Nested Case-Control Study. Chest 2012, 141, 1170–1176. [Google Scholar] [CrossRef]
- Mochizuki, K.; Shintani, R.; Mori, K.; Sato, T.; Sakaguchi, O.; Takeshige, K.; Nitta, K.; Imamura, H. Importance of respiratory rate for the prediction of clinical deterioration after emergency department discharge: a single-center, case-control study. Acute Med. Surg. 2016, 4, 172–178. [Google Scholar] [CrossRef]
- Miller, D.J.; Capodilupo, J.V.; Lastella, M.; Sargent, C.; Roach, G.D.; Lee, V.H.; Capodilupo, E.R. Analyzing changes in respiratory rate to predict the risk of COVID-19 infection. PLOS ONE 2020, 15, e0243693. [Google Scholar] [CrossRef]
- Tajin, A.S.; Amanatides, C.E.; Dion, G.; Dandekar, K.R. Passive UHF RFID-Based Knitted Wearable Compression Sensor. IEEE Internet Things J. 2021, 8, 13763–13773. [Google Scholar] [CrossRef]
- Wu, Y.; Jiang, D.; Bardill, A.; Bayford, R.; Demosthenous, A. A 122 fps, 1 MHz Bandwidth Multi-Frequency Wearable EIT Belt Featuring Novel Active Electrode Architecture for Neonatal Thorax Vital Sign Monitoring. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Nicolò, A.; Presti, D.L.; Sacchetti, M.; Silvestri, S.; Schena, E. Contact-Based Methods for Measuring Respiratory Rate. Sensors 2019, 19, 908. [Google Scholar] [CrossRef]
- Ali, M.; Elsayed, A.; Mendez, A.; Savaria, Y.; Sawan, M. Contact and Remote Breathing Rate Monitoring Techniques: A Review. IEEE Sensors J. 2021, 21, 14569–14586. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Nicolo, A.; Sacchetti, M.; Schena, E. Contactless Methods For Measuring Respiratory Rate: A Review. IEEE Sensors J. 2020, 21, 12821–12839. [Google Scholar] [CrossRef]
- Bansal, R. Antenna theory; analysis and design. Proc. IEEE 1984, 72, 989–990. [Google Scholar] [CrossRef]
- El Gharbi, M.; Fernández-García, R.; Gil, I. Embroidered wearable Antenna-based sensor for Real-Time breath monitoring. Measurement 2022, 195. [Google Scholar] [CrossRef]
- Measurement, 195, 111080,.
- Ahadi, M.; Roudjane, M.; Dugas, M.-A.; Miled, A.; Messaddeq, Y. Wearable Sensor Based on Flexible Sinusoidal Antenna for Strain Sensing Applications. Sensors 2022, 22, 4069. [Google Scholar] [CrossRef]
- Guay, P.; Gorgutsa, S.; LaRochelle, S.; Messaddeq, Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors 2017, 17, 1050. [Google Scholar] [CrossRef]
- Wagih, M.; Malik, O.; Weddell, A.S.; Beeby, S. E-Textile Breathing Sensor Using Fully Textile Wearable Antennas. Engineering Proceedings 2022, 15, 9. [Google Scholar] [CrossRef]
- Patron, D.; Mongan, W.; Kurzweg, T.P.; Fontecchio, A.; Dion, G.; Anday, E.K.; Dandekar, K.R. On the Use of Knitted Antennas and Inductively Coupled RFID Tags for Wearable Applications. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 1047–1057. [Google Scholar] [CrossRef]
- Zang, C.; Zhang, C.; Zhang, M.; Niu, Q. An RFID-Based Method for Multi-Person Respiratory Monitoring. Sensors 2022, 22, 6166. [Google Scholar] [CrossRef] [PubMed]
- El Gharbi, M.; Fernández-García, R.; Gil, I. Wireless Communication Platform Based on an Embroidered Antenna-Sensor for Real-Time Breathing Detection. Sensors 2022, 22, 8667. [Google Scholar] [CrossRef] [PubMed]
- Roudjane, M.; Bellemare-Rousseau, S.; Khalil, M.; Gorgutsa, S.; Miled, A.; Messaddeq, Y. A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection. Sensors 2018, 18, 973. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Gil, I.; Fernandez-Garcia, R. Electro-Textile UHF-RFID Compression Sensor for Health-Caring Applications. IEEE Sensors J. 2022, 22, 12332–12338. [Google Scholar] [CrossRef]
- Liu, Y.; Yu, M.; Xia, B.; Wang, S.; Wang, M.; Chen, M.; Dai, S.; Wang, T.; Ye, T.T. E-Textile Battery-Less Displacement and Strain Sensor for Human Activities Tracking. IEEE Internet Things J. 2021, 8, 16486–16497. [Google Scholar] [CrossRef]
- Caccami, M.C.; Mulla, M.Y.S.; Di Natale, C.; Marrocco, G. Wireless monitoring of breath by means of a graphene oxide-based radiofrequency identification wearable sensor. In Proceedings of the 2017 11th European Conference on Antennas and Propagation, EUCAP; 2017. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, M.; Yu, M.; Xia, B.; Ye, T. Embroidered Inductive Strain Sensor for Wearable Applications’. In Proceedings of the 2020 IEEE International Conference on Pervasive Computing and Communications Workshops, PerCom Workshops; 2020. [Google Scholar]
- Escobedo, P.; Bhattacharjee, M.; Nikbakhtnasrabadi, F.; Dahiya, R. Smart Bandage With Wireless Strain and Temperature Sensors and Batteryless NFC Tag. IEEE Internet Things J. 2021, 8, 5093–5100. [Google Scholar] [CrossRef]
- Behera, S.K. Chipless RFID Sensors for Wearable Applications: A Review. IEEE Sensors J. 2021, 22, 1105–1120. [Google Scholar] [CrossRef]
- Chen, T.; Li, S.; Sun, H. Metamaterials Application in Sensing. Sensors 2012, 12, 2742–2765. [Google Scholar] [CrossRef]
- Munk, B.A. Frequency selective surfaces: theory and design. Wiley-Interscience: New York.
- Milici, S.; Lorenzo, J.; Lazaro, A.; Villarino, R.; Girbau, D. Wireless Breathing Sensor Based on Wearable Modulated Frequency Selective Surface. IEEE Sensors J. 2016, 17, 1285–1292. [Google Scholar] [CrossRef]
- Elgeziry, M.; Costa, F.; Tognetti, A.; Genovesi, S. Wearable Textile-Based Sensor Tag for Breath Rate Measurement. IEEE Sensors J. 2022, 22, 22610–22619. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, J.; Gao, H.; Fu, X.; Bao, D.; Cui, T.J. Mixed-Resolution High-Q Sensor Based on Hybridized Spoof Localized Surface Plasmons. Front. Phys. 2022, 10. [Google Scholar] [CrossRef]
- Ren, Y.; Sun, X.; Liu, J. Advances in Liquid Metal-Enabled Flexible and Wearable Sensors. Micromachines 2020, 11, 200. [Google Scholar] [CrossRef] [PubMed]
- Elgeziry, M.; Costa, F.; Genovesi, S. Design Guidelines for Sensors Based on Spiral Resonators. Sensors 2022, 22, 2071. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Cui, T.J. Ultrathin plasmonic metamaterial for spoof localized surface plasmons. Laser Photon- Rev. 2013, 8, 137–145. [Google Scholar] [CrossRef]
- Pors, A.; Moreno, E.; Martin-Moreno, L.; Pendry, J.; Garcia-Vidal, F. Localized spoof plasmons arise while texturing closed surfaces. Phys Rev Lett 108. [CrossRef]
- Yang, X.; Tian, X.; Ho, J. Wearable Radio-frequency Plasmonic Resonance Sensor for Non-contact Vital Sign Monitoring’. In Proceedings of the 2021 IEEE International Symposium on Antennas and Propagation and North American Radio Science Meeting; pp. 1261–1262.
- Massaroni, C.; Saccomandi, P.; Schena, E. Medical Smart Textiles Based on Fiber Optic Technology: An Overview. J. Funct. Biomater. 2015, 6, 204–221. [Google Scholar] [CrossRef]
- Mayoral, C.P.; Gutiérrez, J.G.; Pérez, J.L.C.; Treviño, M.V.; Velasco, I.B.G.; Cruz, P.A.H.; Rosas, R.T.; Carrillo, L.T.; Ríos, J.A.; Apreza, E.L.; et al. Fiber Optic Sensors for Vital Signs Monitoring. A Review of Its Practicality in the Health Field. Biosensors 2021, 11, 58. [Google Scholar] [CrossRef]
- Koyama, S.; Fujimoto, A.; Yasuda, Y.; Satou, Y. Verification of the Propagation Range of Respiratory Strain Using Signal Waveform Measured by FBG Sensors. Sensors 2020, 20, 7076. [Google Scholar] [CrossRef]
- Massaroni, C.; Saccomandi, P.; Formica, D.; Presti, D.L.; Caponero, M.A.; Di Tomaso, G.; Giurazza, F.; Muto, M.; Schena, E. Design and Feasibility Assessment of a Magnetic Resonance-Compatible Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring. IEEE Sensors J. 2016, 16, 8103–8110. [Google Scholar] [CrossRef]
- Ciocchetti, M.; Massaroni, C.; Saccomandi, P.; Caponero, M.A.; Polimadei, A.; Formica, D.; Schena, E. Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring: Design and Preliminary Trials. Biosensors 2015, 5, 602–615. [Google Scholar] [CrossRef]
- Presti, D. Respiratory and cardiac rates monitoring during MR examination by a sensorized smart textile’. In Proceedings of the I2MTC 2017 - 2017 IEEE International Instrumentation and Measurement Technology Conference.
- Issatayeva, A.; Beisenova, A.; Tosi, D.; Molardi, C. Fiber-Optic Based Smart Textiles for Real-Time Monitoring of Breathing Rate. Sensors 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Presti, D.L.; Carnevale, A.; D’abbraccio, J.; Massari, L.; Massaroni, C.; Sabbadini, R.; Zaltieri, M.; Di Tocco, J.; Bravi, M.; Miccinilli, S.; et al. A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers. Sensors 2020, 20, 536. [Google Scholar] [CrossRef] [PubMed]
- Tavares, C.; Teichmann, D.; Kuhn, A.; Leonhardt, S.; Walter, M. Respiratory and heart rate monitoring using an FBG 3D-printed wearable system. Biomed Opt Express 13. [CrossRef]
- Chen, Y.; Zhang, P.; Li, Y.; Zhang, K.; Su, J.; Huang, L. Flexible capacitive pressure sensor based on multi-walled carbon nanotubes microstructure electrodes. J. Phys. D Appl. Phys. 2021, 54, 155101. [Google Scholar] [CrossRef]
- Rohit, A.; Kaya, S. Flexible Multi-Modal Capacitive Sensors with Polyurethane Foam Dielectrics for Wearables. In Proceedings of the 2021 IEEE International Flexible Electronics Technology Conference, IFETC 2021; 2021. [Google Scholar] [CrossRef]
- Kim, J.; Kim, J. Classification of Breathing Signals According to Human Motions by Combining 1D Convolutional Neural Network and Embroidered Textile Sensor. Sensors 2023, 23, 5736. [Google Scholar] [CrossRef]
- Simic´, M.; Stavrakis, A.K.; Sinha, A.; Premcˇevski, V.; Markoski, B.; Stojanovic´, G.M. Portable respiration monitoring system with an embroidered capacitive facemask sensor. Biosensors 2022, 12, 339. [Google Scholar] [CrossRef]
- Thiyagarajan, K.; Rajini, G.K.; Maji, D. Flexible, Highly Sensitive Paper-Based Screen Printed MWCNT/PDMS Composite Breath Sensor for Human Respiration Monitoring. IEEE Sensors J. 2020, 21, 13985–13995. [Google Scholar] [CrossRef]
- Duan, Z.; Jiang, Y.; Huang, Q.; Yuan, Z.; Zhao, Q.; Wang, S.; Zhang, Y.; Tai, H. A do-it-yourself approach to achieving a flexible pressure sensor using daily use materials. J. Mater. Chem. C 2021, 9, 13659–13667. [Google Scholar] [CrossRef]
- Small, I.K.; Jovanov, E.; Rolin, T.D. Monitoring of Respiration by Means of an Additively Manufactured Barium Titanate-based Hygroscopic Sensor. 2019 SoutheastCon 2019, 1–5. [Google Scholar] [CrossRef]
- Hwang, J.; Kim, Y.; Yang, H.; Oh, J.H. Fabrication of hierarchically porous structured PDMS composites and their application as a flexible capacitive pressure sensor. Compos. Part B: Eng. 2021, 211, 108607. [Google Scholar] [CrossRef]
- Pang, Z.; Zhao, Y.; Luo, N.; Chen, D.; Chen, M. Flexible pressure and temperature dual-mode sensor based on buckling carbon nanofibers for respiration pattern recognition. Sci. Rep. 2022, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Liu, Z.; Zhang, L.; Li, K.; Zhang, S.; Xu, H.; Mao, Z.; Zhang, H.; Chen, J.; Pan, G. Multifunctional polypyrrole and rose-like silver flower-decorated E-textile with outstanding pressure/strain sensing and energy storage performance. Chem. Eng. J. 2021, 427, 130823. [Google Scholar] [CrossRef]
- Park, S.W.; Das, P.S.; Chhetry, A.; Park, J.Y. A Flexible Capacitive Pressure Sensor for Wearable Respiration Monitoring System. IEEE Sensors J. 2017, 17, 1–1. [Google Scholar] [CrossRef]
- Yao, S.; Zhu, Y. Wearable multifunctional sensors using printed stretchable conductors made of silver nanowires. Nanoscale 2013, 6, 2345–2352. [Google Scholar] [CrossRef]
- Kang, T.H. Sensors on textile substrates for home-based healthcare monitoring’. In Proceedings of the 1st Transdisciplinary Conference on Distributed Diagnosis and Home Healthcare, 2006. D2H2. IEEE; pp. 5–7. [Google Scholar]
- Merritt, C.R.; Nagle, H.T.; Grant, E. Textile-Based Capacitive Sensors for Respiration Monitoring. IEEE Sensors J. 2008, 9, 71–78. [Google Scholar] [CrossRef]
- Wen, X.; Jiang, K.; Zhang, H.; Huang, H.; Yang, L.; Zhou, Z.; Weng, Q. Flexible and Wearable Zinc-Ion Hybrid Supercapacitor Based on Double-Crosslinked Hydrogel for Self-Powered Sensor Application. Materials 2022, 15, 1767. [Google Scholar] [CrossRef]
- Kim, J.; Truong, T.; Kim, J. Development of Embroidery-Type Sensor Capable of Detecting Respiration Using the Capacitive Method’. Polymers 15. [CrossRef]
- Xia, S.; Song, S.; Jia, F.; Gao, G. A flexible, adhesive and self-healable hydrogel-based wearable strain sensor for human motion and physiological signal monitoring. J. Mater. Chem. B 2019, 7, 4638–4648. [Google Scholar] [CrossRef]
- Ling, Q.; Ke, T.; Liu, W.; Ren, Z.; Zhao, L.; Gu, H. Tough, Repeatedly Adhesive, Cyclic Compression-Stable, and Conductive Dual-Network Hydrogel Sensors for Human Health Monitoring. Ind Eng Chem Res, 18373, 18383. [Google Scholar] [CrossRef]
- Taccini, N.; Loriga, G.; Pacelli, M.; Paradiso, R. Wearable monitoring system for chronic cardio-respiratory diseases’. In Proceedings of the Proceedings of the 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS’08 - ‘Personalized Healthcare through Technology’, p.; pp. 3690–3693.
- Brendgen, R.; Nolden, R.; Simon, J.; Junge, T.; Zöll, K.; Schwarz-Pfeiffer, A. Textile Strain Sensor Enhancement by Coating Metal Yarns with Carbon-Filled Silicone. Polymers 2022, 14, 2525. [Google Scholar] [CrossRef]
- Yin, Y.; Wang, Y.; Li, H.; Xu, J.; Zhang, C.; Li, X.; Cao, J.; Feng, H.; Zhu, G. A flexible dual parameter sensor with hierarchical porous structure for fully decoupled pressure–temperature sensing. Chem. Eng. J. 2021, 430, 133158. [Google Scholar] [CrossRef]
- Cao, L.; Zhang, Z.; Li, J.; Wang, Z.; Ren, Y.; Wang, Q.; Huang, D.; Li, Z. A Low-Cost Flexible Perforated Respiratory Sensor Based on Platinum for Continuous Respiratory Monitoring. Micromachines 2022, 13, 1743. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Choi, J.Y.; Yoo, E.S.; Lim, D.Y.; Lee, J.Y.; Kim, J.K.; Pang, C. Printable wet-resistive textile strain sensors using bead-blended composite ink for robustly integrative wearable electronics. Compos. Part B: Eng. 2021, 210, 108674. [Google Scholar] [CrossRef]
- Cao, Q.; Shu, Z.; Zhang, T.; Ji, W.; Chen, J.; Wei, Y. Highly Elastic, Sensitive, Stretchable, and Skin-Inspired Conductive Sodium Alginate/Polyacrylamide/Gallium Composite Hydrogel with Toughness as a Flexible Strain Sensor’. Biomacromolecules 23, 2603–2613. [CrossRef] [PubMed]
- Xu, Y. A super water-resistant MXene sponge flexible sensor for bifunctional sensing of physical and chemical stimuli. Lab Chip, 23, 485–494. [CrossRef]
- Tachibana, S.; Wang, Y.-F.; Sekine, T.; Takeda, Y.; Hong, J.; Yoshida, A.; Abe, M.; Miura, R.; Watanabe, Y.; Kumaki, D.; et al. A Printed Flexible Humidity Sensor with High Sensitivity and Fast Response Using a Cellulose Nanofiber/Carbon Black Composite. ACS Appl. Mater. Interfaces 2022, 14, 5721–5728. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Chen, H.; Yang, M.; Li, Y. Facile fabrication of poly (diallyldimethyl ammonium chloride)/Ti3C2Tx/poly (vinylidene fluoride) 3D hollow fiber membrane flexible humidity sensor and its application in the monitoring of health-related physiological activity’. Sens Actuators B Chem, 374. Online].
- Al-Hamry, A.; Panzardi, E.; Mugnaini, M.; Kanoun, O. Human Breathing Monitoring by Graphene Oxide Based Sensors. 2021, 97–107. [Google Scholar] [CrossRef]
- Xu, L.; Zhai, H.; Chen, X.; Liu, Y.; Wang, M.; Liu, Z.; Umar, M.; Ji, C.; Chen, Z.; Jin, L.; et al. Coolmax/graphene-oxide functionalized textile humidity sensor with ultrafast response for human activities monitoring. Chem. Eng. J. 2021, 412, 128639. [Google Scholar] [CrossRef]
- Zhang, D.; Zong, X.; Wu, Z. Fabrication of tin disulfide/graphene oxide nanoflower on flexible substrate for ultrasensitive humidity sensing with ultralow hysteresis and good reversibility. Sensors Actuators B: Chem. 2019, 287, 398–407. [Google Scholar] [CrossRef]
- Jenjeti, R.; Kumar, R.; Sampath, S. Two-dimensional, few-layer NiPS3 for flexible humidity sensor with high selectivity’. J Mater Chem A Mater, 7, 14545–14551. [CrossRef]
- Maita, F.; Piccialli, V.; Pensa, F.; Scatto, M.; Ruggeri, M.; Maiolo, L. Application of Unconditioned Nanostructured Thermoplastic-Based Strain Gauge Sensor in Wearable Electronics. IEEE Sensors J. 2022, 22, 24019–24026. [Google Scholar] [CrossRef]
- Wang, F.; Ma, X.; Wu, J.; Chao, Y.; Xiao, P.; Zhu, J.; Chen, J. Flexible, recyclable and sensitive piezoresistive sensors enabled by lignin polyurethane-based conductive foam. Mater. Adv. 2022, 4, 586–595. [Google Scholar] [CrossRef]
- Deb, M.; Chen, M.-Y.; Chang, P.-Y.; Li, P.-H.; Chan, M.-J.; Tian, Y.-C.; Yeh, P.-H.; Soppera, O.; Zan, H.-W. SnO2-Based Ultra-Flexible Humidity/Respiratory Sensor for Analysis of Human Breath. Biosensors 2023, 13, 81. [Google Scholar] [CrossRef]
- Teichmann, D.; Kuhn, A.; Leonhardt, S.; Walter, M. The MAIN Shirt: A Textile-Integrated Magnetic Induction Sensor Array. Sensors 2014, 14, 1039–1056. [Google Scholar] [CrossRef] [PubMed]
- Teichmann, D.; Matteis, D.; Bartelt, T.; Walter, M.; Leonhardt, S. A bendable and wearable cardiorespiratory monitoring device fusing two noncontact sensor principles. IEEE J Biomed Health Inform, 19, 784–793. [CrossRef]
- Zhu, J.; Jia, Y.; Li, M.; Zhou, Z.; Chen, Y.; Liu, Q.; Yang, X. A paper-based self-inductive folding displacement sensor for human respiration and motion signals measurement. npj Flex. Electron. 2022, 6, 1–11. [Google Scholar] [CrossRef]
- Wang, Q.; Ruan, T.; Xu, Q.; Yang, B.; Liu, J. Wearable multifunctional piezoelectric MEMS device for motion monitoring, health warning, and earphone. Nano Energy 2021, 89, 106324. [Google Scholar] [CrossRef]
- Zeng, X.; Deng, H.-T.; Wen, D.-L.; Li, Y.-Y.; Xu, L.; Zhang, X.-S. Wearable Multi-Functional Sensing Technology for Healthcare Smart Detection. Micromachines 2022, 13, 254. [Google Scholar] [CrossRef]
- Lee, T.; Kim, I.; Kim, D. Flexible Hybrid Nanogenerator for Self-Powered Weather and Healthcare Monitoring Sensor. Adv. Electron. Mater. 2021, 7, 2100785. [Google Scholar] [CrossRef]
- Electron Mater, 7. Electron Mater, 7.
- Zhu, M.; Lou, M.; Yu, J.; Li, Z.; Ding, B. Energy autonomous hybrid electronic skin with multi-modal sensing capabilities. Nano Energy 2020, 78, 105208. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, S.; Jin, Y.M.; Ouyang, H.; Zou, Y.; Wang, X.X.; Xie, L.X.; Li, Z. Flexible piezoelectric nanogenerator in wearable self-powered active sensor for respiration and healthcare monitoring. Semicond. Sci. Technol. 2017, 32, 064004. [Google Scholar] [CrossRef]
- Hossain, I.Z.; Khan, A.; Hossain, G. A Piezoelectric Smart Textile for Energy Harvesting and Wearable Self-Powered Sensors. Energies 2022, 15, 5541. [Google Scholar] [CrossRef]
- Manjunatha, G.R.; Rajanna, K.; Mahapatra, D.R.; Nayak, M.M.; Krishnaswamy, U.M.; Srinivasa, R. Polyvinylidene fluoride film based nasal sensor to monitor human respiration pattern: An initial clinical study. J. Clin. Monit. Comput. 2013, 27, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Moradian, S.; Abdolvand, R. MEMS-based passive wireless respiration profile sensor. In Proceedings of the 2016 IEEE SEN-SORS, Orlando, FL, USA, 30 October–3 November 2016; Institute of Electrical and Electronics Engineers (IEEE): Los Alamitos, CA, USA, 2016; pp. 1–3. [Google Scholar]
- Aqueveque, P.; Gómez, B.; Monsalve, E.; Germany, E.; Ortega-Bastidas, P.; Dubo, S.; Pino, E.J. Simple Wireless Impedance Pneumography System for Unobtrusive Sensing of Respiration. Sensors 2020, 20, 5228. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, M.H.; Berkvens, R.; Weyn, M. Chest-Worn Inertial Sensors: A Survey of Applications and Methods. Sensors 2021, 21, 2875, Respiratory Rate Estimation by Using ECG, Impedance, and Motion Sensing in Smart Clothing’. J Med Biol Eng, 37, 826–842. [Google Scholar] [CrossRef]
- Vuorela, T.; Seppa, V.-P.; Vanhala, J.; Hyttinen, J. Design and Implementation of a Portable Long-Term Physiological Signal Recorder. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 718–725. [Google Scholar] [CrossRef]
- Loriga, G.; Taccini, N.; De Rossi, D.; Paradiso, R. Textile Sensing Interfaces for Cardiopulmonary Signs Monitoring. 2005, 7349–7352. [Google Scholar] [CrossRef]
- Klum, M.; Leib, F.; Oberschelp, C.; Martens, D.; Pielmus, A.-G.; Tigges, T.; Penzel, T.; Orglmeister, R. Wearable Multimodal Stethoscope Patch for Wireless Biosignal Acquisition and Long-Term Auscultation. 2019, 5781–5785. [Google Scholar] [CrossRef]
- Wu, Y.; Jiang, D.; Bardill, A.; de Gelidi, S.; Bayford, R.; Demosthenous, A. A High Frame Rate Wearable EIT System Using Active Electrode ASICs for Lung Respiration and Heart Rate Monitoring. IEEE Trans. Circuits Syst. I: Regul. Pap. 2018, 65, 3810–3820. [Google Scholar] [CrossRef]
- Xu, J.; Harpe, P.; Van Hoof, C. An Energy-Efficient and Reconfigurable Sensor IC for Bio-Impedance Spectroscopy and ECG Recording. IEEE J. Emerg. Sel. Top. Circuits Syst. 2018, 8, 616–626. [Google Scholar] [CrossRef]
- De Fazio, R.; Stabile, M.; De Vittorio, M.; Velázquez, R.; Visconti, P. An Overview of Wearable Piezoresistive and Inertial Sensors for Respiration Rate Monitoring. Electronics 2021, 10, 2178. [Google Scholar] [CrossRef]
- Das, P.S.; Ahmed, H.E.U.; Motaghedi, F.; Lester, N.J.; Khalil, A.; Al Janaideh, M.; Anees, S.; Carmichael, T.B.; Bain, A.R.; Rondeau-Gagné, S.; et al. A Wearable Multisensor Patch for Breathing Pattern Recognition. IEEE Sensors J. 2023, 23, 10924–10934. [Google Scholar] [CrossRef]
- Cay, G. NeoWear: An IoT-connected e-textile wearable for neonatal medical monitoring. Pervasive Mob Comput, 86. [CrossRef]
- Hassan, M.; Abbas, G.; Li, N.; Afzal, A.; Haider, Z.; Ahmed, S.; Xu, X.; Pan, C.; Peng, Z. Significance of Flexible Substrates for Wearable and Implantable Devices: Recent Advances and Perspectives. Adv. Mater. Technol. 2021, 7, 2100773. [Google Scholar] [CrossRef]
- Jiang, T.; Zhong, J.; Liang, J.; Wu, Y.; Li, Z.; Wang, X.; Lin, L.; Qian, X. Wearable Airflow Sensor for Nasal Symmetric Evaluation and Respiration Monitoring. In Proceedings of the Proceedings of IEEE Sensors 2019, 1–4. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, P.; Li, Y.; Zheng, R.; Ding, G.; Xiao, Q.; Su, K.; Yin, S.; Yang, Z. A Wearable Ultrathin Flexible Sensor Inserted Into Nasal Cavity for Precise Sleep Respiratory Monitoring. IEEE Trans. Electron Devices 2021, 68, 4090–4097. [Google Scholar] [CrossRef]
- Nguyen, T. A Wearable, Bending-Insensitive Respiration Sensor Using Highly Oriented Carbon Nanotube Film’. IEEE Sens J, 21, 7308–7315. [CrossRef]
- Manjunatha, G.R.; Rajanna, K.; Mahapatra, D.R.; Nayak, M.M.; Krishnaswamy, U.M.; Srinivasa, R. Polyvinylidene fluoride film based nasal sensor to monitor human respiration pattern: An initial clinical study. J. Clin. Monit. Comput. 2013, 27, 647–657. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, S.; Jin, Y.; Ouyang, H.; Zou, Y.; Wang, X.; Xie, L.; Li, Z. Flexible Piezoelectric Nanogenerator for Wearable Self-powered Respiration Active Sensor and Healthcare Monitoring. Materials Research Express 2019. [Google Scholar] [CrossRef]
- Yuan, Y.; Liu, B.; Li, H.; Li, M.; Song, Y.; Wang, R.; Wang, T.; Zhang, H. Flexible Wearable Sensors in Medical Monitoring. Biosensors 2022, 12, 1069. [Google Scholar] [CrossRef]
- Wu, S. An Overview of Hierarchical Design of Textile-Based Sensor in Wearable Electronics. Crystals 2022, 12, 555. [Google Scholar] [CrossRef]
- Alfaro, J.G.C.; Trejos, A.L. Design and Fabrication of Embroidered Textile Strain Sensors: An Alternative to Stitch-Based Strain Sensors. Sensors 2023, 23, 1503. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).