1. Introduction
The ever-growing emergence of antibiotic resistance associated with tuberculosis (TB) has become a global challenge [
1]. Furthermore, the combination of TB and COVID-19 can cause severe respiratory complications, leading to systemic failure [
2]. According to reports from the World Health Organisation (WHO), TB was estimated to be the leading cause of death from a single infectious agent and the 13th leading cause of death worldwide. However, in 2020 and 2021, it was projected that TB would rank second as a cause of death from a single infectious agent, following the emergence of COVID-19 [
3]. In 2021, it was estimated that approximately 10.6 million individuals worldwide contracted tuberculosis (TB), out of this total, it is estimated that 191,000 deaths occurred specifically due to multidrug-resistant or rifampicin-resistant tuberculosis (MDR/RR-TB) [
4].
For the management of MDR-TB, WHO suggests two-course durations, which are abbreviated as short (9-11 months) and long (18-20 months) treatment regimens [
2,
5]. But the concomitant use of multiple anti-TB medications and lengthy treatment regimens is often met with poor patient adherence, resulting in the emergence of Mycobacterium strains which are resistant to first-line drugs such as isoniazid and rifampicin. Leading to one of the most serious kinds of tuberculosis i.e MDR-TB. This has spurred the necessity of research and development of new drugs to fight against TB [
6,
7]. Albeit, various regulatory bodies are working to overcome the burden of this disease. The USFDA has given expedited approval to bedaquiline (TMC207) in 2012, as a new treatment for drug-resistant TB in adults when there are no other viable options available [
8].
Bedaquiline (BDQ), a diarylquinoline derivative has a unique mechanism of action. The drug specifically targets and deactivates the F1/F0-ATP synthase of MDR strains of
Mycobacterium tuberculosis (M. tb) by binding to its subunit C of ATP synthase enzyme which is responsible for energy production in
M. tb without interfering with the F1/F0-ATP synthase in mammalian cells [
9,
10]. In preclinical and clinical studies, bedaquiline
has shown promising results in treating MDR-TB. These studies involved the use of bedaquiline as a single drug or in combination with other anti-TB drugs (e.g. moxifloxacin and pyrazinamide
). Additionally, some studies utilized a murine model of TB, and the findings support the efficacy of bedaquiline in treating MDR-TB [
11]. In these studies, bedaquiline was administered at a dosage of 400 mg once daily for a period of 2 weeks, followed by 200 mg three times weekly either for 6 or 22 weeks, and showed improved treatment outcomes when compared to existing treatment regimens. Also, bedaquiline regimen led to faster culture conversion (when the bacteria is no longer detectable in the patient's sputum), this suggests that treatment duration with bedaquiline regimens may be shorter compared to other tandard regimens [
12].
Despite this unique anti-TB action of this drug, it is also associated with certain physiochemical limitations. According to the Biopharmaceutical Classification System (BCS), Bedaquiline belongs to the Class II category, as it has exceptionally low solubility in water (0.000193 mg/mL) and high lipophilicity (log P 7.1) [
13], thus making it unsuitable molecule for conventional dosage forms Furthermore, the bedaquiline carries with it several dose-dependent potential adverse effects, such as prolonged QT interval, increased hepatic aminotransferase levels, nausea, vomiting, etc which limiting the use of bedaquiline [
14]. There are several formulation strategies such as reduction in size, complexation, polymorphism, and solid dispersions which overcome the hurdles of dose-dependent adverse effects, solubility, and release rate but they are unable to resolve the bioavailability problems stemming from gastric degradation.
Of late, researchers have found self-nano emulsifying drug delivery systems (SNEDDS) to be the most advantageous lipid-based drug delivery system for circumventing the existing challenges and also gained tremendous popularity due to their advantageous features like small globule size, simplified production process, increased biocompatibility and enhanced stability [
15]. These systems are typically composed of lipid (natural and synthetic oils), surfactants, co-surfactants, and/or co-solvents that spontaneously emulsifies. By pre-dissolving the drug in a mixture of lipids and emulsifying excipients, the disintegration and dissolution steps can be bypassed, which usually hinders the oral absorption of water-insoluble drugs [
16].
The systematic use of design of experiments (DoE) to optimize isotropic systems has become common practice in both industry and academia. The recent approach of "formulation by design" (FbD), based on DoE and quality by design (QbD), provides a rational understanding of the interaction between variables, and helps to select the best formulation with minimal time, effort, and cost compared to the traditional one-factor-at-a-time (OFAT) approach. The FbD methodology involves defining the quality target product profile (QTPP), identification of critical quality attributes (CQAs), critical material attributes (CMAs), and critical process parameters (CPPs) through screening and risk assessment, optimization data analysis using DoE, modeling and optimum search through response surface methodology (RSM) to create the design space, and developing a control strategy for continuous improvement [
17]. The previous experimental studies carried out in various laboratories on diverse nanostructured systems like liquid and S-SNEDDS of carvedilol [
18] and ezetimibe [
19], solid lipid nanoparticles of quercetin [
20], isotretinoin [
21], and liposomes of nimesulide [
22], have vouched the utility of QbD in developing the optimized nanocolloidal formulations.
2. Materials
Bedaquiline fumarate (BDQ-F) (99.5% pure) was obtained as a complimentary sample from Omgene Life Sciences Pvt Ltd. The high-performance liquid chromatography (HPLC) grade solvents, such as Acetonitrile, Methanol, and Ethanol, were procured from Merck Ltd in Mumbai, India. Transcutol-P and Cremophor R EL were acquired from Sigma-Aldrich (Bangalore, India). All other chemicals used in the study were of analytical grade and deionized water was used for all experiments.
3. Methods
3.1. Solubility studies
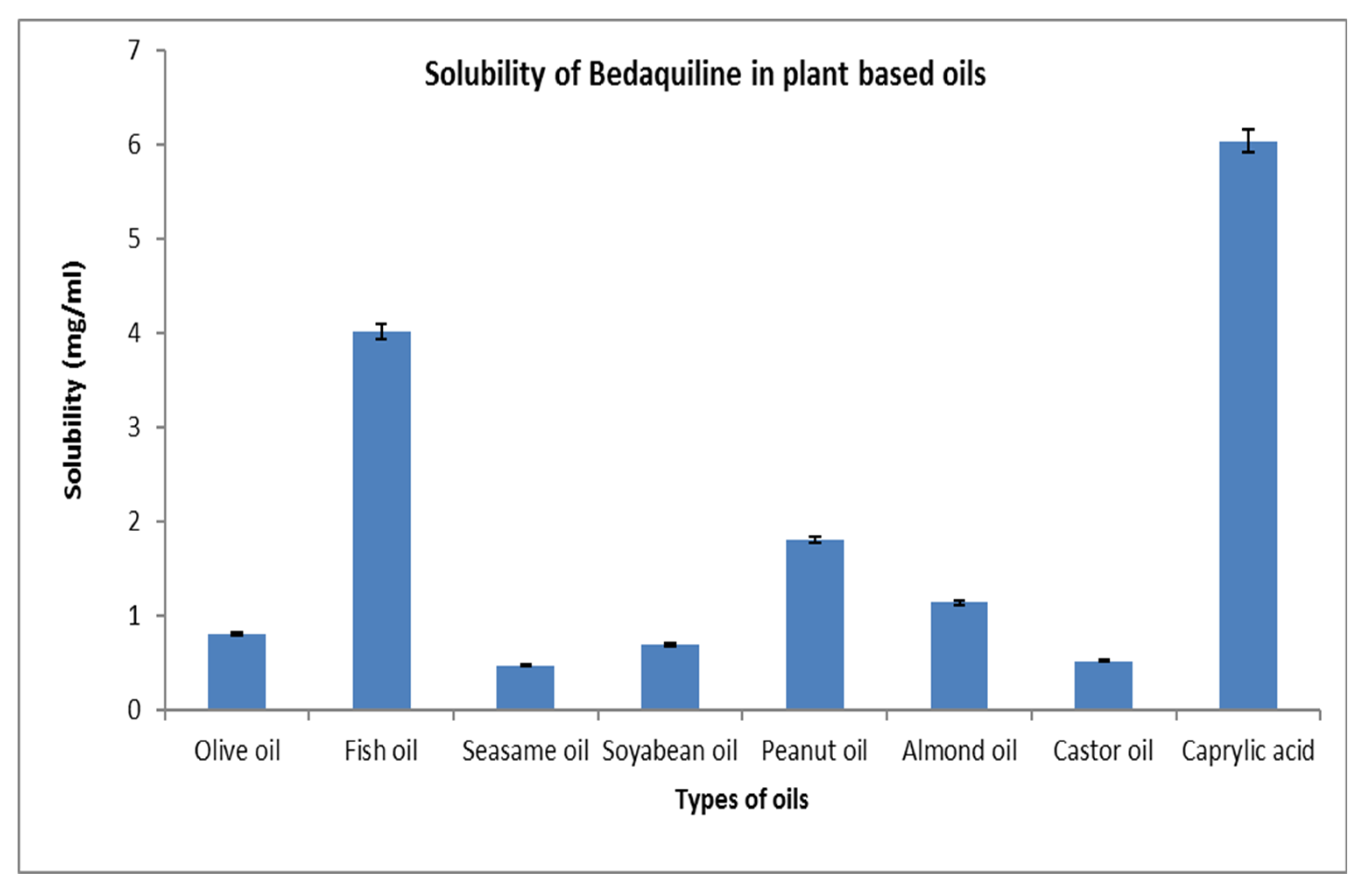
3.1.1. Selection of oil
To determine the solubility of BDQ-F in different oils, the shake flask technique was employed. Excess BDQ-F was added to 2 ml of various oils including olive oil, fish oil, castor oil, sesame oil, soybean oil, peanut oil, almond oil, and caprylic acid. The mixture was vigorously vortexed for 10 minutes to ensure thorough mixing. Subsequently, the samples were incubated for 72 hours in a rotary shaker bath at a controlled temperature of 37 ± 5 °C to attain equilibrium. After the equilibrium period, the samples were centrifuged at 100 rpm for 5 minutes. The resulting supernatant was separated, appropriately diluted, and subjected to analysis to determine the concentrations of BDQ-F [
23].
3.1.2. Selection of surfactant and co-surfactant
Surfactant and co-surfactant selection was done based on the emulsification ability. Various surfactants like tween 80, tween 40, span 80, cremophore, capryol 90, capmul GMO, captex 355, caprol ET, and propylene glycol were screened for their emulsification capability.
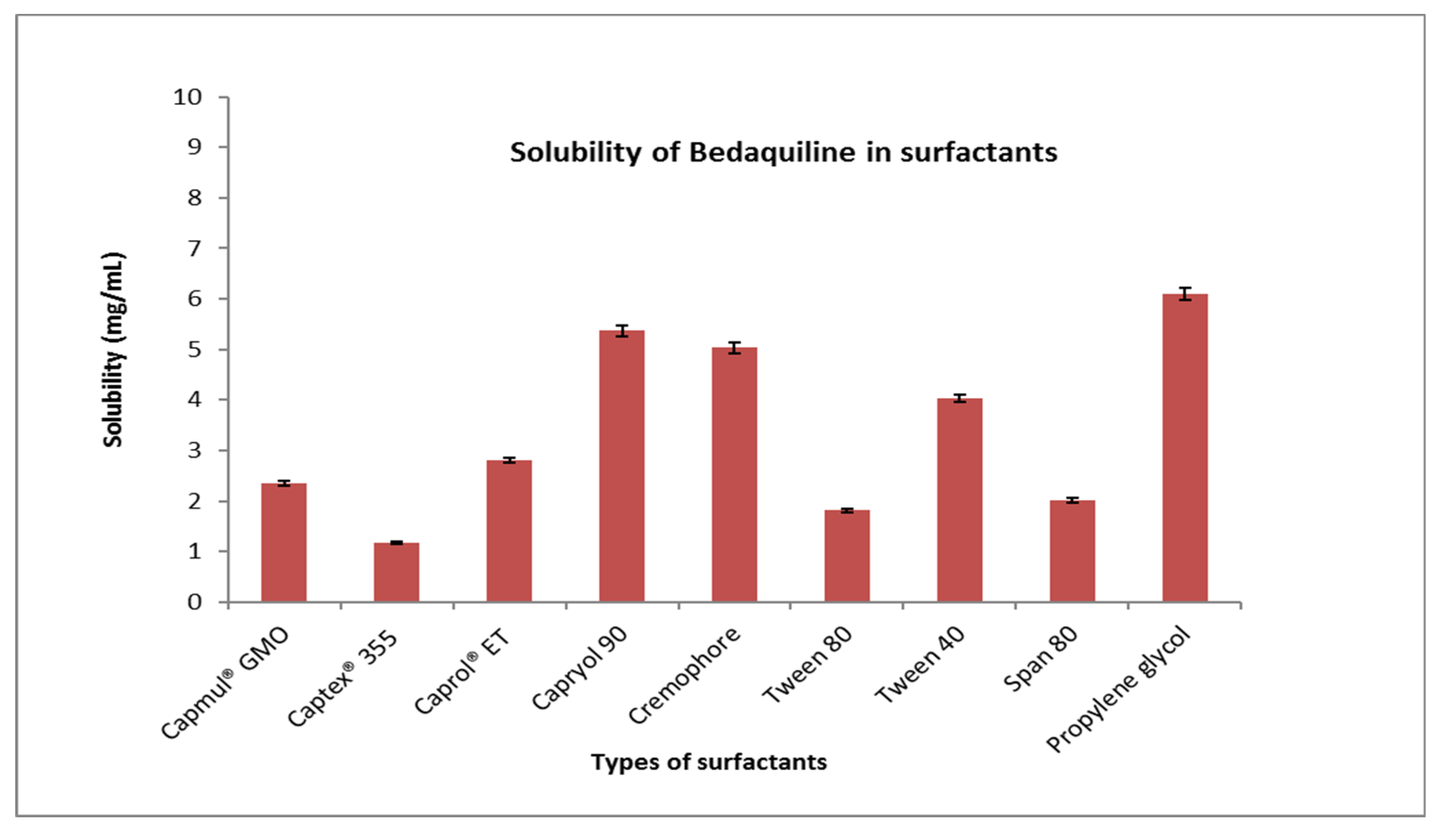
3.2. Pseudo-ternary phase diagram
A pseudoternary phase diagram was built for the SNEDDS development to compute the surfactant: co-surfactant (S
mix) and oil: S
mix ratios. S
mix was taken in the following ratios: 1:0, 1:1, 1:2, 2:1, 3:1, 4:1, 5:1. The oil and S
mix mixtures were then titrated against deionized water. The amount of deionized water was changed at 5% intervals between 5 and 95%. After adding deionized water to the mixture, it was vortexed for 2 to 5 minutes and visually examined for clarity or turbidity, with the results noted on the phase diagram. The S
mix, oil, and deionized water phases of the formulation are represented by the three vertices of the pseudoternary phase diagram. In the pseudoternary phase diagram, the percentage composition of each nanoemulsion was designated as a point, and the area surrounded by these points was measured [
24].
3.3. Quality by design (QbD) approach incorporation
Designing for quality gives value and quality to the final pharmaceutical product. Throughout the formulation development process, it is vital to identify and regulate the critical parameters related to the process and formulation development. The QbD technique entails establishing the quality target product profile (QTPP), identifying critical quality attributes (CQAs), critical material attributes (CMAs), and critical process parameters (CPPs) through screening and risk assessment, optimising data using DoE, and evaluating the results. In
Supplementary File Tables S1 and S2 provides various parameters of QTPP and CQAs for SNEDDs formulation.
3.4. Risk assessment using Ishikawa
A risk assessment approach was developed to detect and estimate the likelihood of drug excipient interactions with various unit functions if there are any risks or failures. The Ishikawa fish-bone diagram was constructed employing Minitab 16 software as shown in
Supplementary File Figure S1.
3.5. Formulation and optimization of SNEDDS using Box Behnken design
Box-Behnken experimental design (BBD) was used to evaluate the critical experimental conditions for the maximum and minimum response. BBD was used to optimize solid-nanoemulsion drug delivery systems (SNEDDS) by studying the effects of variables on size, entrapment efficiency, and drug release. This design helps to eliminate non-significant factors that do not have a significant effect on the response variable, and it can provide an optimized formulation with fewer trials. Consequently, leading to cost and time savings. Furthermore, this design simplifies the experiments by reducing the number of variables that need to be considered [
25]. SNEDDS were created after selecting the surfactant and co-surfactant ratio (S
mix). Using a vortex, an exactly weighed quantity of drug was entirely dissolved in oil. S
mix was slowly added drop by drop to the oil drug combination while constantly swirling to generate uniform formulation. After that, the mixture was sonicated to achieve the desired droplet size. BBD is a more suitable approach for evaluating the effects of formulation variables and the effect on their corresponding variables [
26]. The independent factors were oil, S
mix %, and sonication duration, whereas the dependent variables were droplet size, PdI, and percentage transmittance. The levels of independent variables as well as the constraints of dependent variables are presented in
Table 1. Fourteen runs were generated with two center points with a quadratic polynomial equation.
3.6. Characterization of SNEDDS
3.6.1. Droplet size, PdI, and zeta potential
The average diameter of droplet, PdI and zeta potential was estimated using zeta sizer (Malvern Zetasizer Ver. 7.12, Malvern Instruments). Samples were diluted upto 100 times before analysis at 25°C temperature. Analysis was done in triplicate.
3.6.2. Transmission electron microscopy (TEM)
Morphological analysis of prepared formulation was optimized by Transmission electron microscopy (TEM). To ensure accurate results and avoid any size discrepancies, the sample preparation was performed in a controlled environment free from particles. The procedure involved placing a copper grid on a paraffin sheet using forceps. Subsequently, a diluted sample of BDQ-F loaded SNEDDS was carefully dropped onto the copper grid using a micropipette. The grid, along with the sample, was then immersed in a 2% phosphotungstic acid solution to enhance contrast. Excess fluid was removed by placing the copper grid on Whatman filter paper. After complete drying of the grid, it was subjected to light beam and the morphology of droplets was observed under TEM instrument (CM 200, Philips Briacliff Manor, NY, USA).
3.6.3. Entrapment efficacy
The drug loading efficiency of Bedaquiline fumarate of the optimized formulation was determined by centrifugation method. BDQ-F-SNEDDS were centrifuged at 4000 rpm for 15 minutes. The supernatant was diluted, filtered, and further analyzed using an established high performance liquid chromatography (HPLC) method. Analysis was done in triplicate.
3.6.4. Self-emulsification time
The self-emulsification time of the BDQ-F-SNEDDS was evaluated to confirm its capability to form a stable formulation. The desired outcome of the SNEDDS formulation is that it readily disperses and forms an emulsion when gently mixed with distilled water. Emulsification time was estimated using USP Apparatus II and 0.5 w/v SLS solution with constant stirring. Time taken by the formulation to completely disperse in water was estimated [
17].
3.6.5. Dilution studies
BDQ-F-SNEDDS were subjected to dilution in order to check stability without phase separation. BDQ-F-SNEDDS were diluted to 50, 100, and 200-folds with deionized water and gently shaken. The dilutions were further sonicated for 30 seconds to prevent bubbles and droplet size, PDI and % transmittance were recorded [
27].
3.7. In vitro drug release study
A drug release study was performed using a dialysis membrane. A pre-activated dialysis membrane with a molecular weight cut-off of 12.4 kDa was loaded with 2 ml of optimized BDQ-F-SNEDDS and BDQ-F suspension, respectively. Two separate 100 ml beakers were filled with 48 ml of 0.1N HCl medium. The dialysis membrane containing the BDQ-F-SNEDDS and BDQ-F suspension was placed in the respective beakers filled with the medium. The beakers were then placed on a magnetic stirrer at a temperature of 37°C and a stirring speed of 100 rpm.
Sampling was carried out at specific time intervals (2, 4, 6, 8, 10, and 12 hours) by withdrawing 1 ml of sample at each time point. The withdrawn sample volume was replaced with an equal volume of fresh media to maintain sink conditions. HPLC analysis was performed on the collected samples to determine the drug concentration. The cumulative amount of drug release was calculated based on the analysis results. To ensure reliable data, the experiment was conducted in triplicate for statistical significance [
28].
3.8. Stability studies
The Stability studies performed according to ICH guidelines [
29]. The BDQ-F loaded SNEDDS carriers were subjected to a physical stability study by storing them for the duration of 6 months under both room temperature and accelerated conditions. At predetermined intervals (0, 3, and 6 months), samples were taken from the storage and analyzed for any observable changes in Physical Appearance, droplet size, polydispersity index (PDI), and entrapment efficiency. Additionally, the shelf-life of the optimized BDQ-F-SNEDDS was determined through this analysis [
30]. Stability protocol is provided in
Table S3 as per industry format.
3.9. Cell toxicity studies
The cytotoxicity of both free BDQ-F and optimized BDQ-F-SNEDDS (self-nanoemulsifying drug delivery system) on A549 cells was assessed using the MTT assay. A549 cells were seeded at a density of (5 x 10
3) cells per well in 96-well tissue culture plates and incubated overnight. Subsequently, the cells were treated with varying concentrations (1-100 µg/ml) of the optimized BDQ-F-SNEDDS, placebo, or BDQ-F. Following the treatment, MTT was added to the wells, and the resulting formazan crystals were solubilized using dimethyl sulfoxide. The absorbance of the solution was measured [
31]. The percentage of cytotoxicity, indicating cell viability, was calculated using the provided formula:
3.10. Statistical analysis
The experiments were conducted in triplicate, and the data is presented as mean ± standard deviation (SD), with statistical significance set at p < 0.05. Data analysis was performed using GraphPad Prism® software, version 6.01.
4. Results and discussion
4.1. Solubility study
Maximum solubility of BDQ-F in oils was found in Caprylic acid (6.27±10.9 mg/ml) and among surfactants and co-surfactants propylene glycol and Transcutol-P exhibited highest solubility (6±2.1 mg/ml) as shown in
Figure 1 and
Figure 2. Caprylic acid is medium chain saturated fatty acid and the free fatty acid significantly increase the solubility of drug by showcasing as lipophilic solubilizers [
32]. Propylene glycol is known to reduce the interfacial tension of oil in water [
33]. Transcutol-P has an HLB value of 4.2 and has the ability to permeate GI mucosa by disrupting the lipid bilayer and enhancing the oral bioavailability.
4.2. Pseudoternary phase diagrams
Pseudoternary phase diagrams were created to determine the optimal surfactant: co-surfactant (S
mix) and oil: S
mix ratios for SNEDDS development as shown in
Figure S2. The pink dots represent the nanoemulsion region. It was observed that when 1:0 S
mix ratio was used, nanoemulsion region obtained was almost negligible because propylene glycol was used alone, and sufficient emulsification of oil was not achieved. When co-surfactant was incorporated in S
mix ratio 1:1, the nanoemulsion region increased slightly. On increasing further, the quantity of co-surfactant in S
mix ratio 1:2 no increase in nanoemulsion region was observed. On the other hand, when the concentration of surfactant quantity was increased from 1:1 to 2:1, an increase in nanoemulsion region was observed and 13.7% (v/v) oil was found to be emulsified with 41%v/v of S
mix. On further increasing the quantity of surfactant in S
mix ratio 3:1 ratio there was an appreciable increase in the nanoemulsion region and the maximum amount of oil that could emulsified was found to be 12.9%v/v using 51.6%v/v of S
mix. For the S
mix ratio 4:1 and 5:1 there was no appreciable increase in the nanoemulsion region. Based on the pseudoternary diagrams concentrations of oil, S
mix was taken between range of 10-30 % and 40-60% respectively [
34].
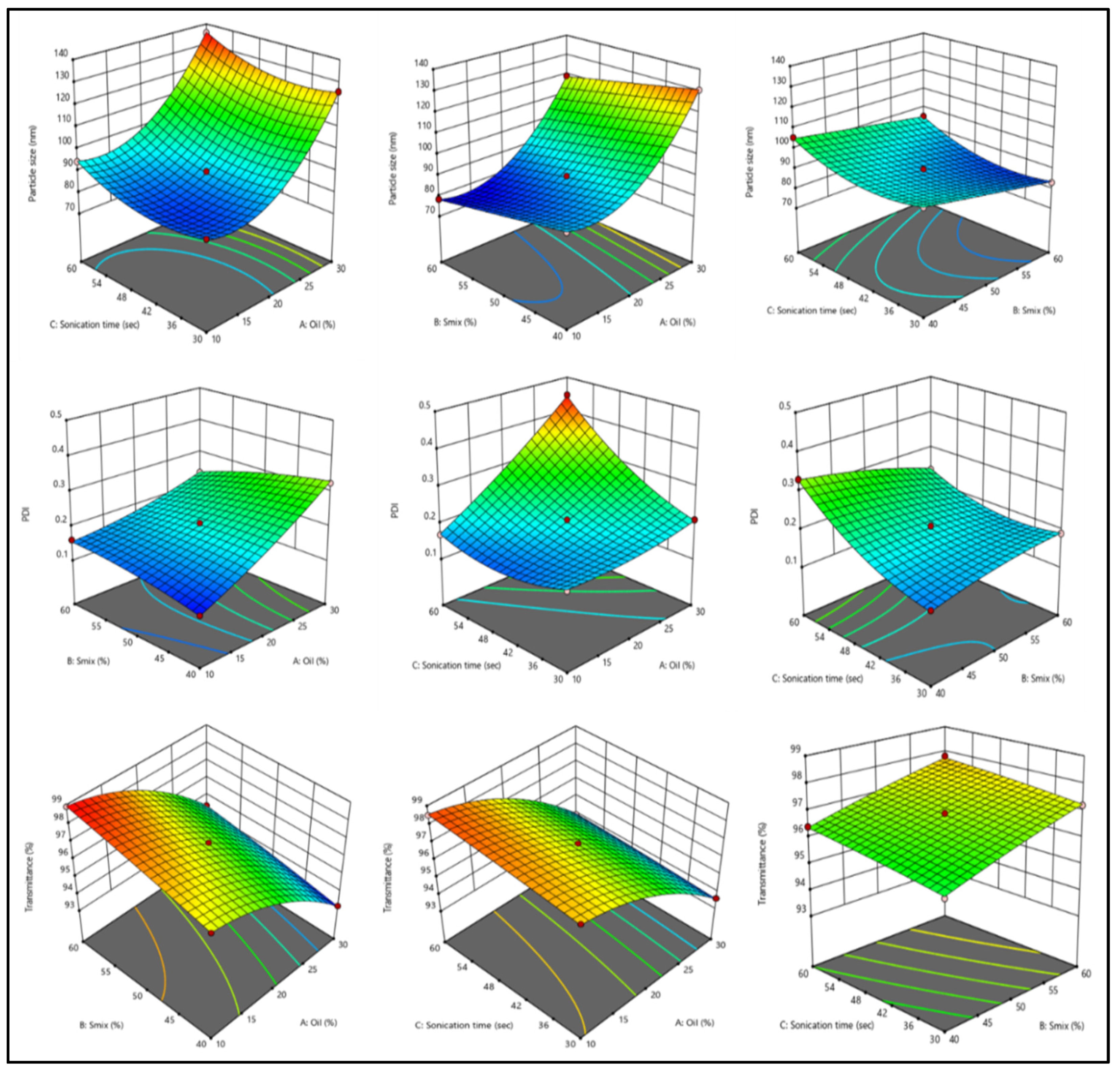
4.3. Optimization using BBD
The final optimization was done using Box-Behnken design using oil, S
mix and sonication time as independent variables and droplet size, PDI, and percentage transmittance as dependent variables. Responses to fourteen runs as shown in
Table S4, were used to determine significant model. Polynomial equations obtained for droplet size, PDI, and transmittance are as follows:
4.3.1. Effect of independent variables on droplet size
Droplet size is an important parameter for the drug release. Smaller droplet size corresponds to larger surface area which in turn leads to more drug release and eventually higher bioavailability. Droplet size increased from 83.1nm to 135.7nm with various variables. Amount of oil has a significant positive effect of droplet size as seen in 3D response curves (
Figure 3). On the contrary S
mix has a negative effect on droplet size. As the concentration of S
mix increases from 40% to 60% droplet size gradually decreases. Larger surfactant concentration decreases the surface tension between oil and aqueous phase leading to smaller droplet size [
35]. Increase in sonication time initially increases the droplet size but further sonication causes aggregation of droplets and increase in size.
4.3.2. Effect of independent variables on PdI
The PDI is an indicator of the homogeneity or uniformity of a formulation. In this study, the effects of different variables on the PDI of BDQ-F-SNEDDS were examined using a polynomial equation. As the concentration of lipid and sonication time increased, the PDI also increased significantly. On the other hand, Smix had an inverse effect on the PDI of BDQ-F-SNEDDS. The PDI values ranged from 0.11 to 0.44, indicating variations in droplet size distribution within the formulation.
4.3.3. Effect of independent variables on transmittance
The percentage transmittance in the runs ranged from 93.1% to 98.9% which is indicative of the transparency of the formulation. Oil percentage has a significant negative impact whereas Smix and Sonication time has a slight positive effect on transmittance. Higher transmittance indicates the transparency and stability of the formulation while lower value shows turbidity and non-homogenous formulation.
4.4. Validation and Point prediction
On the basis of observed values of variables and the constraints applied; software generated a predicted response for optimal formulation and this response was then compared with experimental/observed value. Software generated value comprised of 20% oil, 40% S
mix and 30sec sonication time. Predicted response for droplet size, PDI and Transmittance were 101nm, 0.29, and 98.17 respectively. The observed response was 98.88 nm droplet size, 0.32 PDI and 98.12% transmittance. The predicted and observed values were in good correlation as seen from
Figure S3 establishing the accuracy of BDQ-F-SNEDDS.
4.5. Characterization
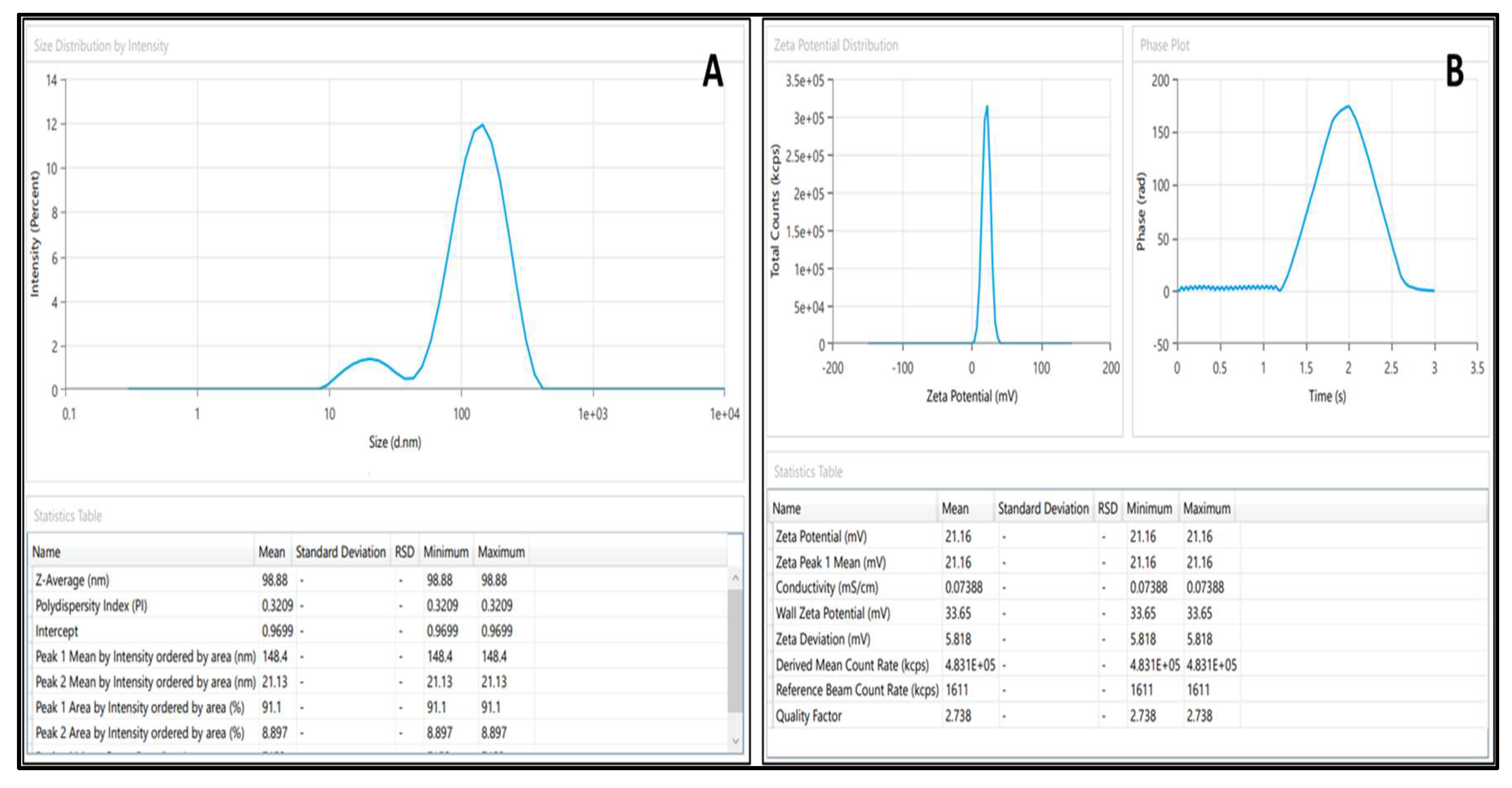
4.5.1. Droplet size and PdI
The droplet size was found to be 98.88±2.1 nm, indicating the average diameter of the droplets in the formulation which is represented in
Figure 4A. The PDI value of 0.3±0.09 suggests a relatively narrow size distribution of the droplets as represented in
Figure 4A.
4.5.2. Zeta potential
BDQ-F-SNEDDS depicted a potential of 21.16±3.4mV as shown in
Figure 4B. The positive zeta potential indicates that the surface charge of droplets is positive [
36]. A formulation is considered stable if the zeta potential is the value is between +30mV and -30mV and no separation or coagulation is seen [
37].
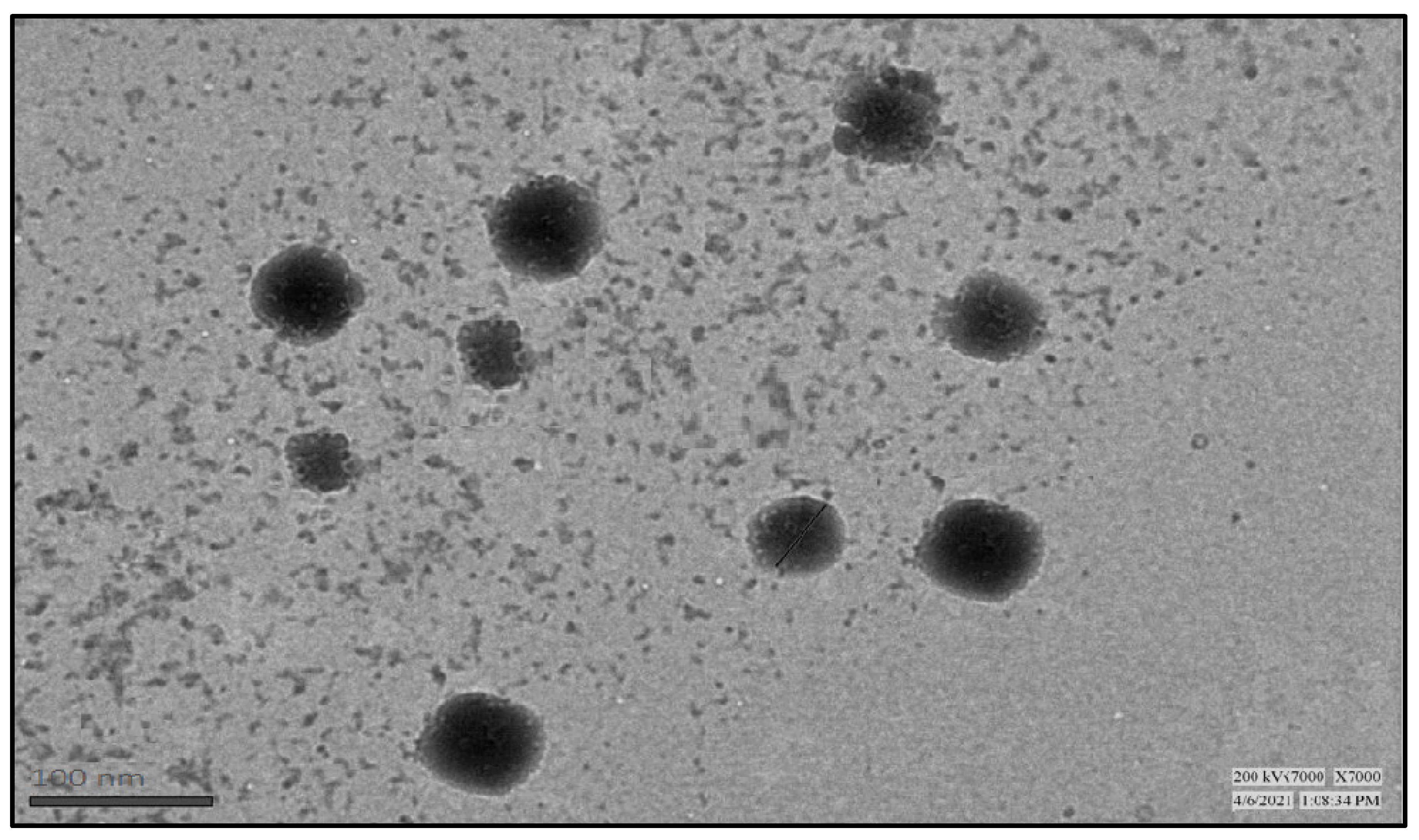
4.5.3. Transmission electron microscopy
TEM image displays visual evidence of spherical-shaped droplets with an average range of size 80 to 100 nm as shown in
Figure 5.
4.5.4. Entrapment efficacy
BDQ-F-SNEDDS exhibited high drug loading efficacy of 81.2±1.3%. This can be attributed to the lipophilic nature of the drug, which enhances its solubility in the oil phase, resulting in a higher entrapment efficacy within the formulation.
4.5.5. Self-emulsification time
BDQ-F-SNEDDS were completely dissolved within 15±3 seconds on gentle agitation which indicates the ability for ease of emulsification. The low emulsification time may be due to reduced interfacial tension by Propylene glycol which causes diffusion of aqueous phase into oil phase [
38]. The sonication time also played a much greater effect on the self-emulsification time. As, a small change in the sonication time can have a significant impact on the time it takes for the SNEDDS to form a nanoemulsion. It could be due the reason, that sonication breaks down the oil droplets into smaller droplets, which makes it easier for them to be dispersed in the aqueous phase. The longer the sonication time, the smaller the oil droplets will be, and the faster the SNEDDS will form a nanoemulsion.
4.5.6. Dilution study
Optimized BDQ-F-SNEDDS were found to be robust at various dilutions. Results shown in
Table 2 depicts that BDQ-F-SNEDDS were stable at different dilutions. When the samples were diluted, slight reduction in droplet size and transmittance was observed. However, the PDI increased as a result of the dilutions.
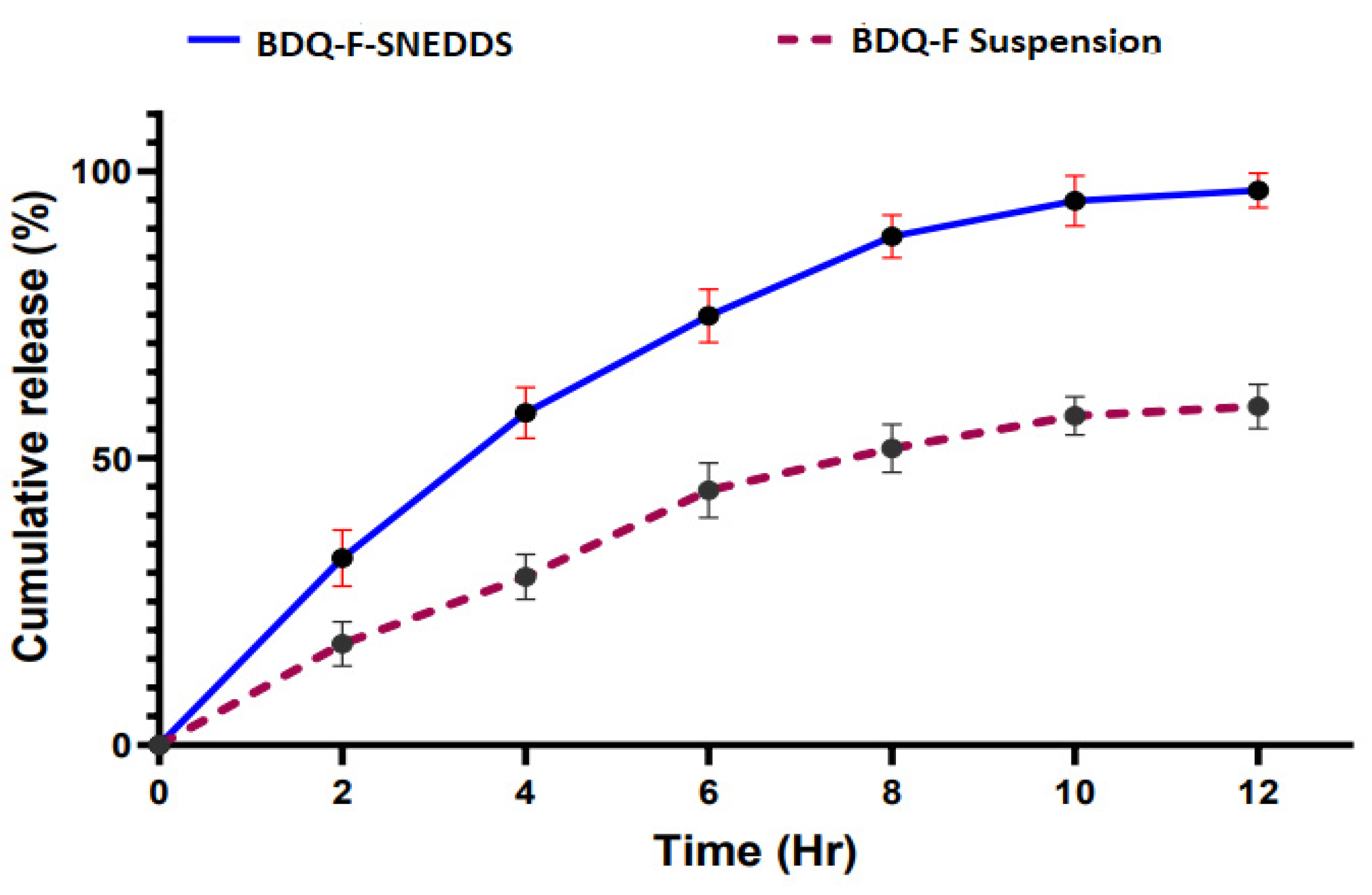
4.5.7. In vitro drug release
Figure 6 illustrates the percentage cumulative drug release (%CDR) of the optimized BDQ-F-SNEDDS and BDQ-F suspension. Within the first 2 hours, BDQ-F-SNEDDS released 27% of the drug, whereas after 12 hours, 93% of the drug was released. In comparison, the suspension only released 55% of the drug. The improved release of drug can be attributed to the rapid formation of a nanoemulsion with nanosize droplets. This suggests that the drug was effectively solubilized in the selected lipid and surfactant components of the formulation [
39].
4.5.8. Stability study
Optimized BDQ-F-SNEDDS were evaluated on the basis of physical appearance, phase separation, caking, droplet size, PDI, and entrapment efficiency as shown in
Table 3. When BDQ-F-SNEDDS were kept at a temperature of 40 ±2 ºC and humidity 75 ±5 % for 6 months no phase separation was observed, and the physical appearance was also clear. Droplet size and PDI increased from 98.88 nm and 103.04nm and 0.34 ± 0.392 to 0.452 ± 0.43 respectively. Droplets tend to coalesce when kept for a longer period resulting in bigger diameter. Entrapment efficiency reduced from 98.3% to 76.2%. Leaking of drug over the period leads to a decrease entrapment efficiency of drug. Optimized BDQ-F-SNEDDS when kept at temperature of 25 ± 2 ºC and humidity of 60 ± 5% droplet size and PdI increased 98.8nm to 106.21nm and 0.34 to 0.48 respectively. Optimized BDQ-F-SNEDDS were stable at both temperatures indicating a robust formulation.
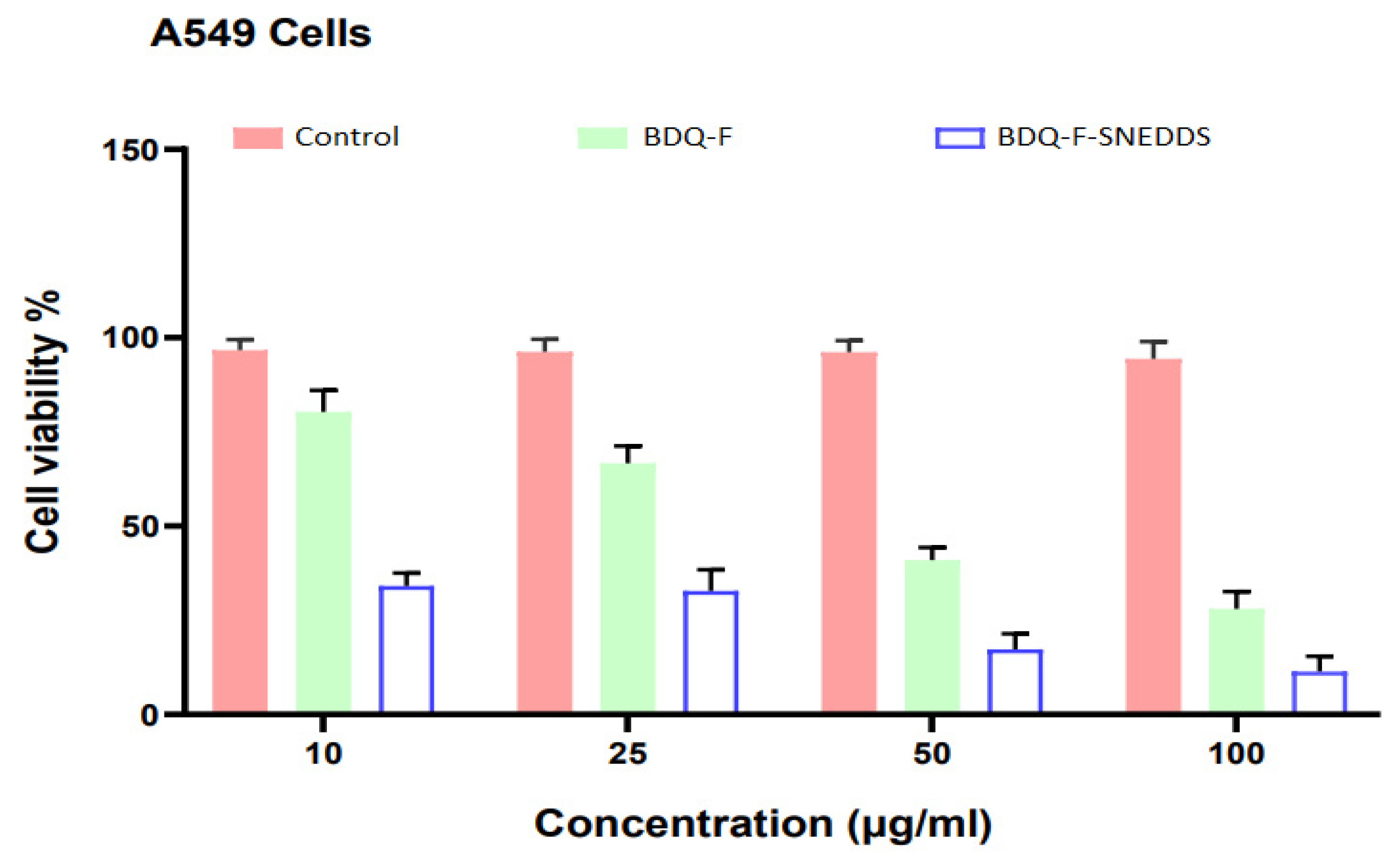
4.5.9. Cell cytotoxicity
The MTT assay was employed to evaluate the cytotoxicity of optimized BDQ-F-SNEDDS, BDQ-F, and a control (placebo) in A549 cells
Figure 7. The IC
50 (the concentration of drug required to inhibit cell growth by 50%) of free BDQ-F was 48.05 ± 1.47 μM. The IC
50 of optimized BDQ-F-SNEDDS was significantly lower, at 17.49 ± 2.38 μM (p < 0.0001). This notable difference could be attributed to the improved solubility of BDQ-F in SNEDDS and the rapid internalization of SNEDDS by cells [
40].
5. Conclusion
Optimized BDQ-F-SNEDDS were formulated using Design of Experiments (DoE), with Caprylic acid as the lipid and Transcutol P and Propylene glycol as the surfactant/cosurfactant system, forming an interfacial film around the oil globules. The prepared SNEDDS underwent evaluation for various parameters including droplet size, PDI, and percent transmittance. Key Quality Target Product Profiles (QTPPs) and CQAs were identified to ensure a robust formulation. Risk assessment was performed using an Ishikawa Fishbone diagram. Optimization of BDQ-F-SNEDDS was accomplished using the Box Behnken design, resulting in an optimized formulation with small droplet size and low PdI, indicating stability and robustness. Transmission Electron Microscopy (TEM) images exhibited spherical shape and a distinct boundary, suggesting high entrapment efficiency.
Results from in vitro drug release studies have indicated that optimized BDQ-F-SNEDDS displayed greater concentrations of drug release compared to the suspension form. This suggests that the optimized BDQ-F-SNEDDS formulation effectively releases the drug in higher concentrations.
Cell cytotoxicity studies conducted on A549 cells revealed enhanced cellular internalization of BDQ-F-SNEDDS, which may be correlated with improved permeability. The lipophilic oil globules in SNEDDS could potentially enable its penetration through bacterial biofilms, thereby enhancing the effectiveness against resistant strains of bacteria. Furthermore, stability studies indicated that BDQ-F-SNEDDS remained stable at both 40 ± 2 ºC and 25 ± 2 ºC for up to 6 months.
The advantages of SNEDDS include its smaller globule size, which facilitates improved drug delivery. Furthermore, it also offers potential benefits for the long-term treatment of multidrug-resistant tuberculosis (MDR-TB) by extending the circulation time of the drug and providing a controlled release pattern. These characteristics hold promise for reducing the dose frequency of administration and enhancing patient compliance.
In summary, BDQ-F-SNEDDS presents a promising strategy for drug delivery that requires further exploration to optimize the treatment protocol for multidrug-resistant tuberculosis (MDR-TB) by decreasing the frequency of dosing and treatment duration. However, it is important to conduct additional research to fully understand the intricate in vivo disposition and pharmacodynamics in animal models.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org.
Author Contributions
Rao Nargis Jahan: conceptualization, methodology and writing-original draft; Pavitra Solanki: visualization; Md. Sayeed Akhtar: data curation and formal analysis; Zafar Khan: visualization; Mohd. Aqil: formal analysis and investigation; Farhan J. Ahmad: Supervision; Yasmin Sultana: supervision, evaluation and final draft.
Funding
Author received financial assistance from Hamdard National Fellowship (HNF).
Data Availability Statement
The article holds the data within its contents.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research at King Khalid University for funding this work through Large Groups (Project under grant number (RGP.2/207/44).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Global tuberculosis report 2020 2020. Available from: https://www.who.int/publications/i/item/9789240013131.
- Ndjeka N, Schnippel K, Master I, Meintjes G, Maartens G, Romero R, et al. High treatment success rate for multidrug-resistant and extensively drug-resistant tuberculosis using a bedaquiline-containing treatment regimen. 2018;52(6). [CrossRef]
- Zhou L, Yang L, Tilton S, Wang JJJops. Development of a high throughput equilibrium solubility assay using miniaturized shake-flask method in early drug discovery. 2007;96(11):3052-71. [CrossRef]
- WHO. WHO Coronavirus (COVID-19) Dashboard. Available from: https://covid19.who.int/.
- Lange C, Dheda K, Chesov D, Mandalakas AM, Udwadia Z, Horsburgh CR. Management of drug-resistant tuberculosis. The Lancet. 2019;394(10202):953-66. [CrossRef]
- Rawal T, Butani S. Combating tuberculosis infection: a forbidding challenge. Indian Journal of Pharmaceutical Sciences. 2016;78(1):8. [CrossRef]
- Ginsberg AM, Spigelman M. Challenges in tuberculosis drug research and development. Nature medicine. 2007;13(3):290-4. [CrossRef]
- Cox E, Laessig K. FDA approval of bedaquiline—the benefit–risk balance for drug-resistant tuberculosis. New England Journal of Medicine. 2014;371(8):689-91. [CrossRef]
- Chahine EB, Karaoui LR, Mansour HJAoP. Bedaquiline: a novel diarylquinoline for multidrug-resistant tuberculosis. 2014;48(1):107-15. [CrossRef]
- Guo H, Courbon GM, Bueler SA, Mai J, Liu J, Rubinstein JL. Structure of mycobacterial ATP synthase with the TB drug bedaquiline. bioRxiv. 2020:2020.08.06.225375. [CrossRef]
- Ibrahim M, Andries K, Lounis N, Chauffour A, Truffot-Pernot C, Jarlier V, et al. Synergistic Activity of R207910 Combined with Pyrazinamide against Murine Tuberculosis. Antimicrobial Agents and Chemotherapy. 2007;51(3):1011-5. [CrossRef]
- Diacon AH, Donald PR, Pym A, Grobusch M, Patientia RF, Mahanyele R, et al. Randomized Pilot Trial of Eight Weeks of Bedaquiline (TMC207) Treatment for Multidrug-Resistant Tuberculosis: Long-Term Outcome, Tolerability, and Effect on Emergence of Drug Resistance. Antimicrobial Agents and Chemotherapy. 2012;56(6):3271-6. [CrossRef]
- Gomes MJ, Martins S, Ferreira D, Segundo MA, Reis S. Lipid nanoparticles for topical and transdermal application for alopecia treatment: development, physicochemical characterization, and in vitro release and penetration studies. International journal of nanomedicine. 2014;9:1231. [CrossRef]
- Kakkar AK, Dahiya N. Bedaquiline for the treatment of resistant tuberculosis: promises and pitfalls. Tuberculosis. 2014;94(4):357-62. [CrossRef]
- Singh B, Bandopadhyay S, Kapil R, Singh R, Katare OP. Self-emulsifying drug delivery systems (SEDDS): formulation development, characterization, and applications. Critical Reviews™ in Therapeutic Drug Carrier Systems. 2009;26(5). [CrossRef]
- Mu H, Holm R, Müllertz A. Lipid-based formulations for oral administration of poorly water-soluble drugs. International journal of pharmaceutics. 2013;453(1):215-24. [CrossRef]
- Beg S, Sandhu PS, Batra RS, Khurana RK, Singh B. QbD-based systematic development of novel optimized solid self-nanoemulsifying drug delivery systems (SNEDDS) of lovastatin with enhanced biopharmaceutical performance. Drug Delivery. 2015 2015/08/18;22(6):765-84. [CrossRef]
- Singh B, Singh R, Bandyopadhyay S, Kapil R, Garg B. Optimized nanoemulsifying systems with enhanced bioavailability of carvedilol. Colloids and Surfaces B: Biointerfaces. 2013 2013/01/01/;101:465-74. [CrossRef]
- Bandyopadhyay S, Katare OP, Singh B. Optimized self nano-emulsifying systems of ezetimibe with enhanced bioavailability potential using long chain and medium chain triglycerides. Colloids and Surfaces B: Biointerfaces. 2012 2012/12/01/;100:50-61. [CrossRef]
- Dhawan S, Kapil R, Singh B. Formulation development and systematic optimization of solid lipid nanoparticles of quercetin for improved brain delivery. Journal of Pharmacy and Pharmacology. 2011;63(3):342-51. [CrossRef]
- Raza K, Singh B, Singal P, Wadhwa S, Katare OP. Systematically optimized biocompatible isotretinoin-loaded solid lipid nanoparticles (SLNs) for topical treatment of acne. Colloids and Surfaces B: Biointerfaces. 2013 2013/05/01/;105:67-74. [CrossRef]
- Singh B, Mehta G, Kumar R, Bhatia A, Ahuja N, Katare O. Design, development and optimization of nimesulide-loaded liposomal systems for topical application. Current drug delivery. 2005;2(2):143-53. [CrossRef]
- Zhou L, Yang L, Tilton S, Wang J. Development of a high throughput equilibrium solubility assay using miniaturized shake-flask method in early drug discovery. Journal of pharmaceutical sciences. 2007;96(11):3052-71. [CrossRef]
- Czajkowska-Kośnik A, Szekalska M, Amelian A, Szymańska E, Winnicka K. Development and Evaluation of Liquid and Solid Self-Emulsifying Drug Delivery Systems for Atorvastatin. Molecules. 2015;20(12):21010-22. PubMed PMID: doi:10.3390/molecules201219745. [CrossRef]
- Joseph E, Reddi S, Rinwa V, Balwani G, Saha R. DoE based Olanzapine loaded poly-caprolactone nanoparticles decreases extrapyramidal effects in rodent model. International journal of pharmaceutics. 2018 Apr 25;541(1-2):198-205. PubMed PMID: 29474898. Epub 2018/02/24. eng. [CrossRef]
- Yadav P, Rastogi V, Verma A. Application of Box–Behnken design and desirability function in the development and optimization of self-nanoemulsifying drug delivery system for enhanced dissolution of ezetimibe. Future Journal of Pharmaceutical Sciences. 2020 2020/03/02;6(1):7. [CrossRef]
- Syukri Y, Martien R, Lukitaningsih E, Nugroho AE. Novel Self-Nano Emulsifying Drug Delivery System (SNEDDS) of andrographolide isolated from Andrographis paniculata Nees: characterization, in-vitro and in-vivo assessment. Journal of Drug Delivery Science and Technology. 2018;47:514-20. [CrossRef]
- Balakumar K, Raghavan CV, selvan NT, prasad RH, Abdu S. Self nanoemulsifying drug delivery system (SNEDDS) of rosuvastatin calcium: design, formulation, bioavailability and pharmacokinetic evaluation. Colloids and surfaces B, Biointerfaces. 2013 Dec 1;112:337-43. PubMed PMID: 24012665. Epub 2013/09/10. eng. [CrossRef]
- Chinchole A, Poul B, Panchal C, Chavan D. A review on stability guidelines by ICH and USFDA guidelines for new formulation and dosage form. PharmaTutor. 2014;2(8):32-53.
- Singh SK, Dadhania P, Vuddanda PR, Jain A, Velaga S, Singh S. Intranasal delivery of asenapine loaded nanostructured lipid carriers: formulation, characterization, pharmacokinetic and behavioural assessment. RSC Advances. 2016;6(3):2032-45. [CrossRef]
- Patil SM, Sawant SS, Kunda NK. Pulmonary delivery of bedaquiline-loaded cubosomes for non-small cell lung cancer (NSCLC) treatment. Drug Delivery to the Lungs. 2021;32.
- Shahba AA-W, Mohsin K, Alanazi FK, Abdel-Rahman SI. Optimization of self-nanoemulsifying formulations for weakly basic lipophilic drugs: role of acidification and experimental design. Brazilian Journal of Pharmaceutical Sciences. 2016;52:653-67. [CrossRef]
- Solans C, Izquierdo P, Nolla J, Azemar N, Garcia-Celma MJ. Nano-emulsions. Current Opinion in Colloid & Interface Science. 2005 2005/10/01/;10(3):102-10. [CrossRef]
- Limbani MD, Patel L. Studies on drug solubilization and role of lipid vehicle in pseudo ternary phase diagram in formulation development of SNEDDS containing poorly water soluble drug. Int J Pharm Sci Rev Res. 2016;40(2):228-37.
- Marasini N, Yan YD, Poudel BK, Choi HG, Yong CS, Kim JO. Development and Optimization of Self-Nanoemulsifying Drug Delivery System with Enhanced Bioavailability by Box–Behnken Design and Desirability Function. Journal of Pharmaceutical Sciences. 2012 2012/12/01/;101(12):4584-96. [CrossRef]
- Shanmugam S, Baskaran R, Balakrishnan P, Thapa P, Yong CS, Yoo BK. Solid self-nanoemulsifying drug delivery system (S-SNEDDS) containing phosphatidylcholine for enhanced bioavailability of highly lipophilic bioactive carotenoid lutein. European Journal of Pharmaceutics and Biopharmaceutics. 2011;79(2):250-7. [CrossRef]
- Rodríguez-Rodríguez R, Espinosa-Andrews H, Morales-Hernández N, Lobato-Calleros C, Vernon-Carter EJ. Mesquite gum/chitosan insoluble complexes: relationship between the water state and viscoelastic properties. Journal of Dispersion Science and Technology. 2019 2019/09/02;40(9):1345-52. [CrossRef]
- Nasr A, Gardouh A, Ghorab M. Novel Solid Self-Nanoemulsifying Drug Delivery System (S-SNEDDS) for Oral Delivery of Olmesartan Medoxomil: Design, Formulation, Pharmacokinetic and Bioavailability Evaluation. Pharmaceutics. 2016 Jun 27;8(3). PubMed PMID: 27355963. Pubmed Central PMCID: PMC5039439. Epub 2016/06/30. eng. [CrossRef]
- Alhakamy NA, Aldawsari HM, Hosny KM, Ahmad J, Akhter S, Kammoun AK, et al. Formulation design and pharmacokinetic evaluation of docosahexaenoic acid containing self-nanoemulsifying drug delivery system for oral administration. Nanomaterials and Nanotechnology. 2020;10:1847980420950988. [CrossRef]
- Shukla SK, Kulkarni NS, Farrales P, Kanabar DD, Parvathaneni V, Kunda NK, et al. Sorafenib Loaded Inhalable Polymeric Nanocarriers against Non-Small Cell Lung Cancer. Pharmaceutical research. 2020 Mar 12;37(3):67. PubMed PMID: 32166411. Epub 2020/03/14. eng. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).