1. Introduction
Individuals with poor oral hygiene have a higher prevalence of being edentulous and suffering the inconvenience of the daily activities [
1,
2,
3]. The complete denture is one of the most popular treatment modalities to restore esthetics, phonetics, and function [
4,
5]. The complete denture was a standard method to fix the dentition. However, the stability and retention of the denture are always challenging due to the alveolar bone loss over time. After the innovation of the implant support overdenture, the stability of the denture can significantly be improved [
6].
For the implant placement in the maxilla for a removable overdenture, a minimum of four implants is needed for a favorable result. As for the mandible, a minimum of two implants showed a favorable result, although placing four implants showed a slightly better outcome [
7].
The morphology of the bone is considered one of the most crucial factors in implant placement and restoration [
8]. Numerous anatomical and vital structures in the maxilla and the mandible affect and limit the treatment planning and the prosthesis of choice, of these structures that affects the implant placement in the maxilla include: 1) the nasopalatine foramen, which transmits the palatine vessels and nasopalatine nerves. 2) Maxillary Sinus, which is a pyramid shaped cavity bilaterally, it is recommended to avoid membrane perforations. As for the anatomical structures of concern in the mandible, these include: 1) the inferior alveolar canal, which is a branch of the trigeminal nerve, the variation in the position of the canal makes implant placement challenging for the surgeon. 2) mental foramen and nerve, where the mental nerve emerges to supply innervation to the anterior mandible. The location of the mental foramen should be identified prior to implant placement to avoid injury to the nerve. 3) mandibular incisive canal, which is a continuation of the mandibular canal mesial to the mental foramen, patient can feel pain or mild discomfort should they have large incisive nerve canals. Finally, 4) lingual foramen and lateral canals, which are small vascular canals and commonly are in the midline and lateral to the midline. The injury of these minute canals may complicate surgery due to bleeding should larger canals exist [
9]. To aid in detecting these structures and plan the implant procedure in advance, multiple applications can assist with diagnosis, surgical implant planning, and delivery of prostheses, such as a cone-beam computed tomography (CBCT) [
10,
11]. CBCT imaging can generally evaluate the anatomy in multiple angles with reasonable radiation exposure. This is relatively important because the edentulous patients are missing the teeth that can be used as the reference, and it could be challenging to review the critical anatomical structure and plan for the implants [
12,
13,
14].
Despite the CBCT being of important value in implant surgery, it has become a gold standard in the implant placement protocol. However, many clinicians may have forgotten that the success of the implant surgery is not just the anatomy but also other factors such as the history of periodontitis, other systemic conditions, and the quality of the bone. Relying on the CBCT alone to plan the surgical procedure may lead to unforeseen outcomes such as sinus perforation, buccal bonce dehiscence, or early implant failure. The aim of this study is to evaluate the predictability of using the CBCT alone to plan for implant placement.
2. Materials and Methods
This study is an investigator-initiated, retrospective clinical study was approved by the institutional review board at the University of Pennsylvania. Clinical data, medical history, and the cone-beam computed tomography of edentulous patients are collected. All the patients were planned and received the treatment of implant-supported overdentures in a dental school setting from 2015 to 2020 using an oral health database (AxiUm®, Software, Henry Schein). All patient information was collected without any identifiers, codes, links, or other means of associating the data to the subject’s identity. Demographic variables extracted included age, gender, race, smoking status, diabetes, and health status as classified by the American Society of Anesthesiologists (ASA I, II, III or IV).
Three examiners performed data collection and fabricated the implant treatment plan for implant supported overdenture accordingly without reviewing the clinical records. Inclusion criteria consisted of any edentulous patient who received cone-beam computed tomographies and implant placements for implant support over denture between 2015–2020. Exclusion criteria included dentate or partially dentate patients, implants within the edentulous arch and remaining roots, and patients with reported metabolic bone diseases.
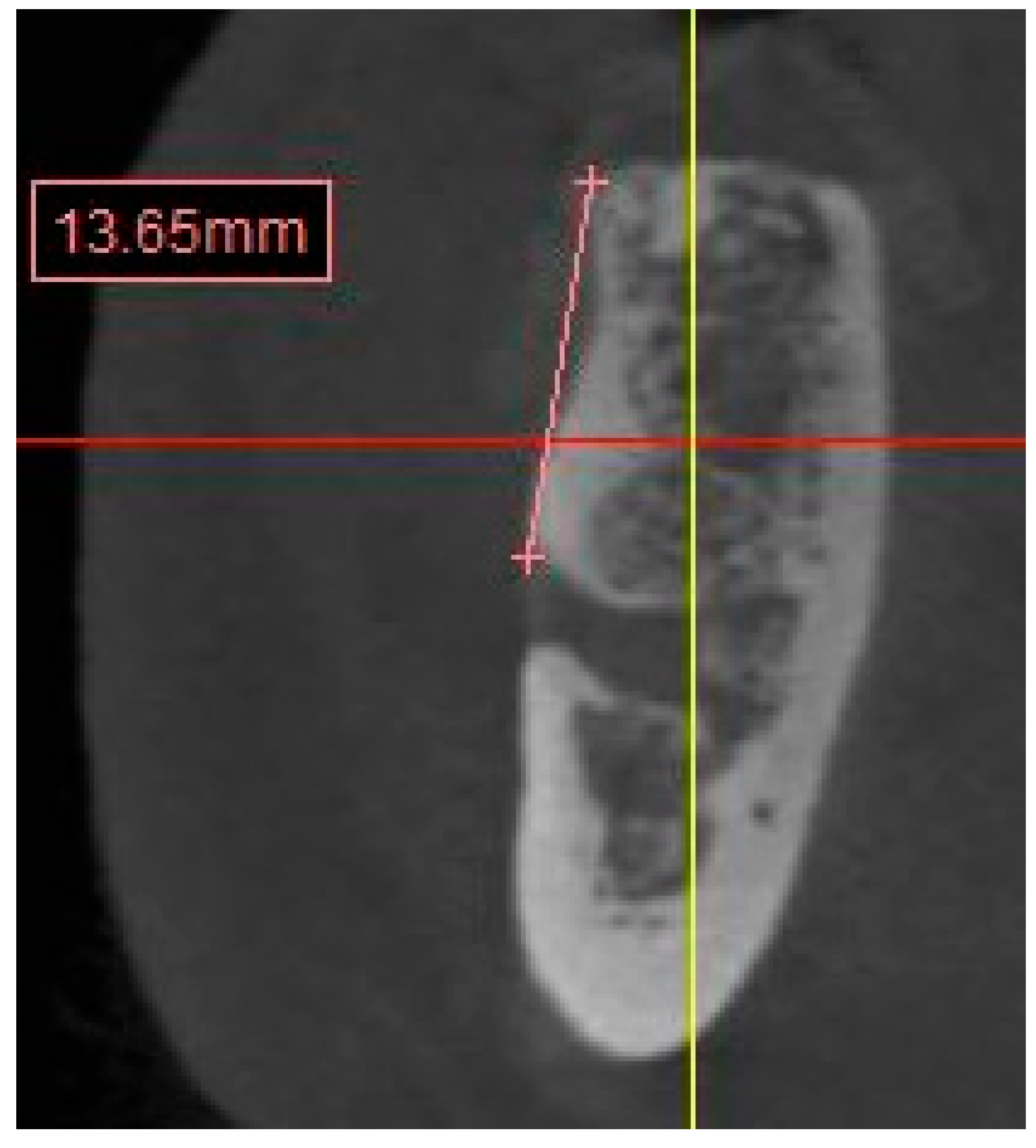
CBCT images were analyzed on Simplant® (Dentsply Sirona, York, PA). Images were reconstructed with slices of 1mm thickness. 12 sites on both maxilla and mandible were measured to evaluate the anatomical structure, such as the width and height of the alveolar ridge and the distance to the anatomical landmarks (sinus floor, mental foramen, and inferior alveolar nerve) as follows:
-
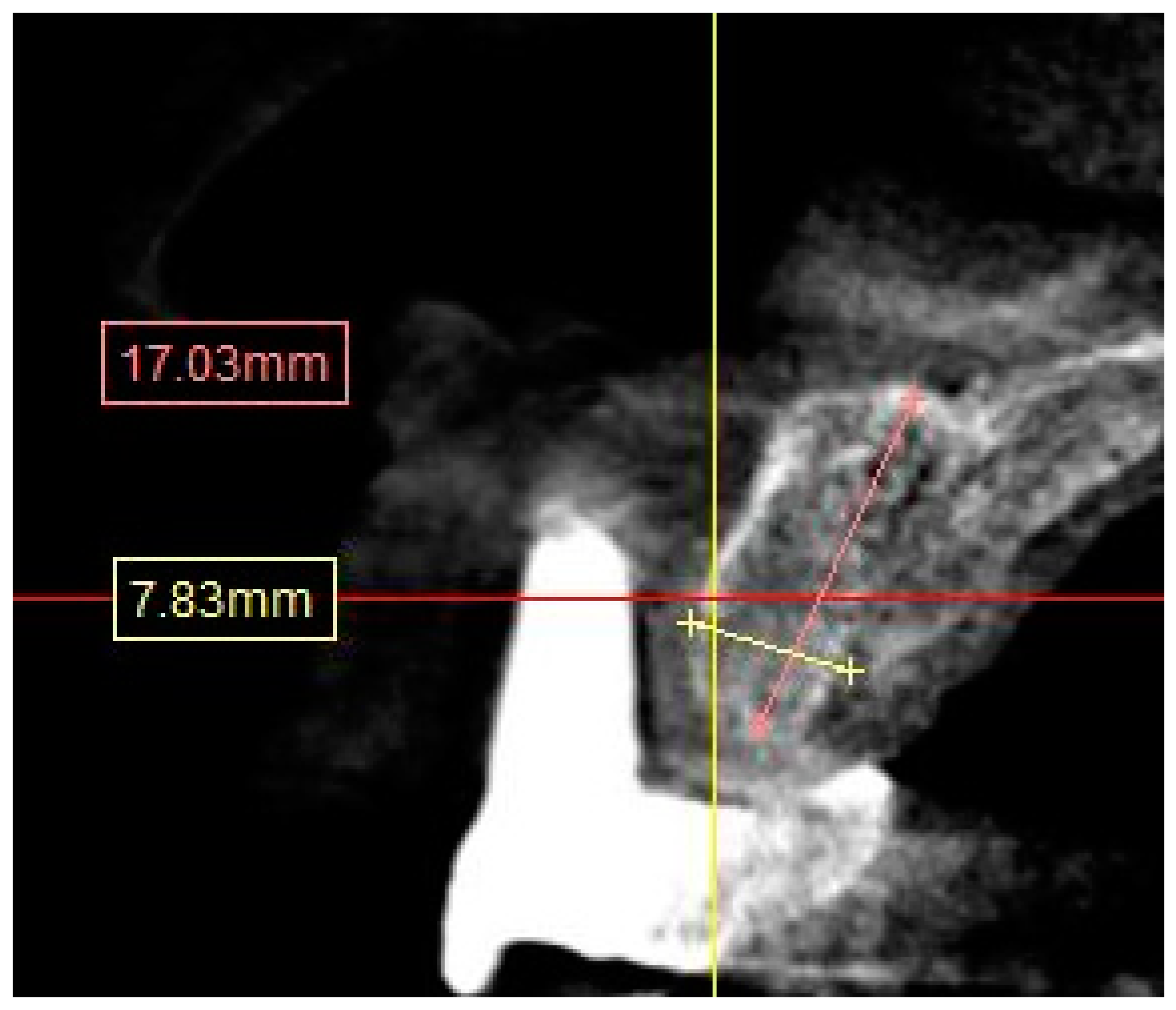
Residual anterior and posterior ridge heights and widths (maxillae and mandible). (
Figure 1)
- ○
Distances were calculated from the crest of the ridge. In case of thin ridge crest, alveoplasty was assumed and measurements were taken from the widest area that would accommodate the implant diameter. The alveoplasty was no more than 5mm. The measurements were taken from the crest if more than 5mm alveoplasty is needed, and the site was noted for grafting.
- ○
The width was calculated 1-2mm apically from the height start point.
-
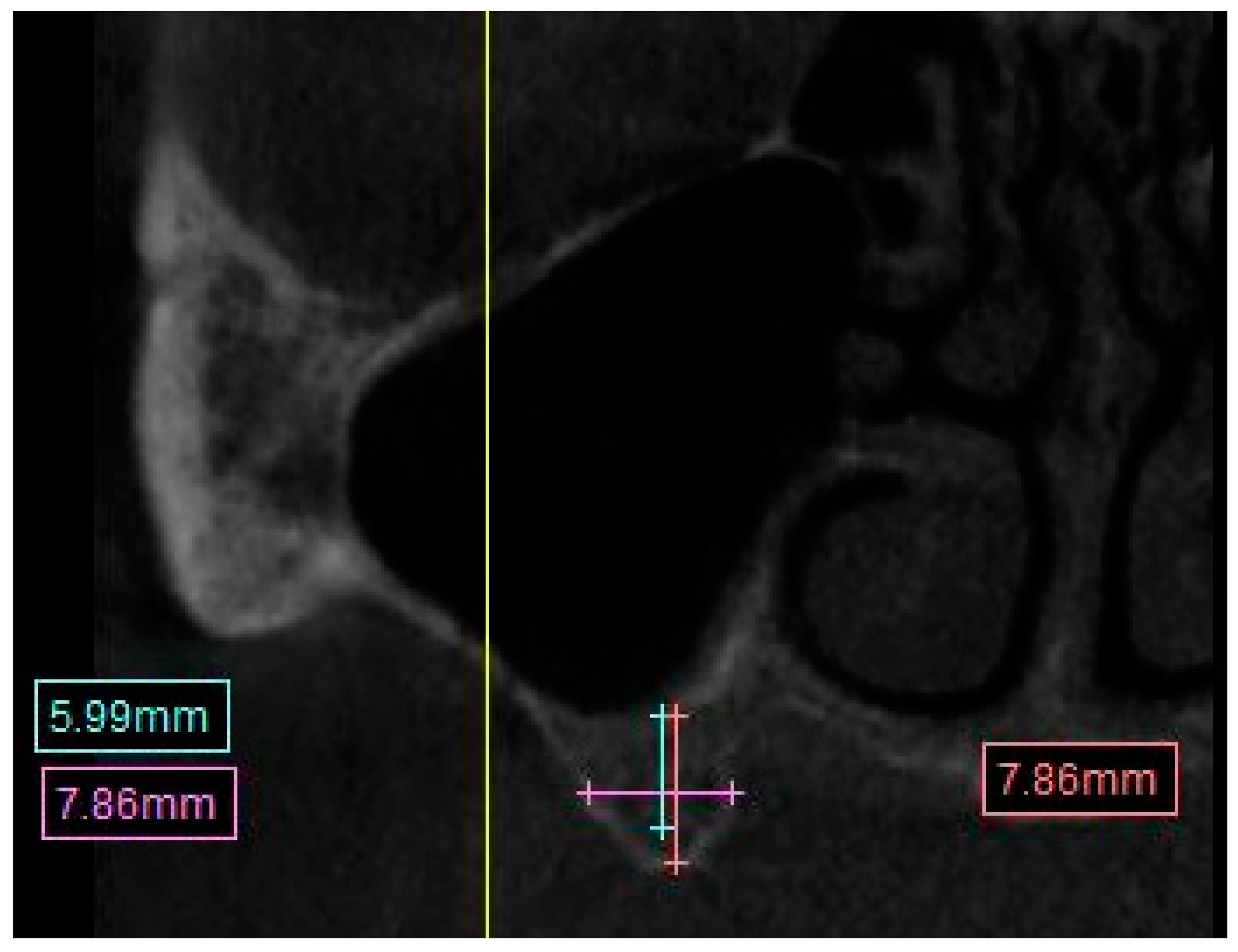
Distance from the crest of maxillary ridge to the floor of the maxillary sinus. (
Figure 2)
- ○
A straight line from the crest of planned molar location to the inferior border of the maxillary sinus.
-
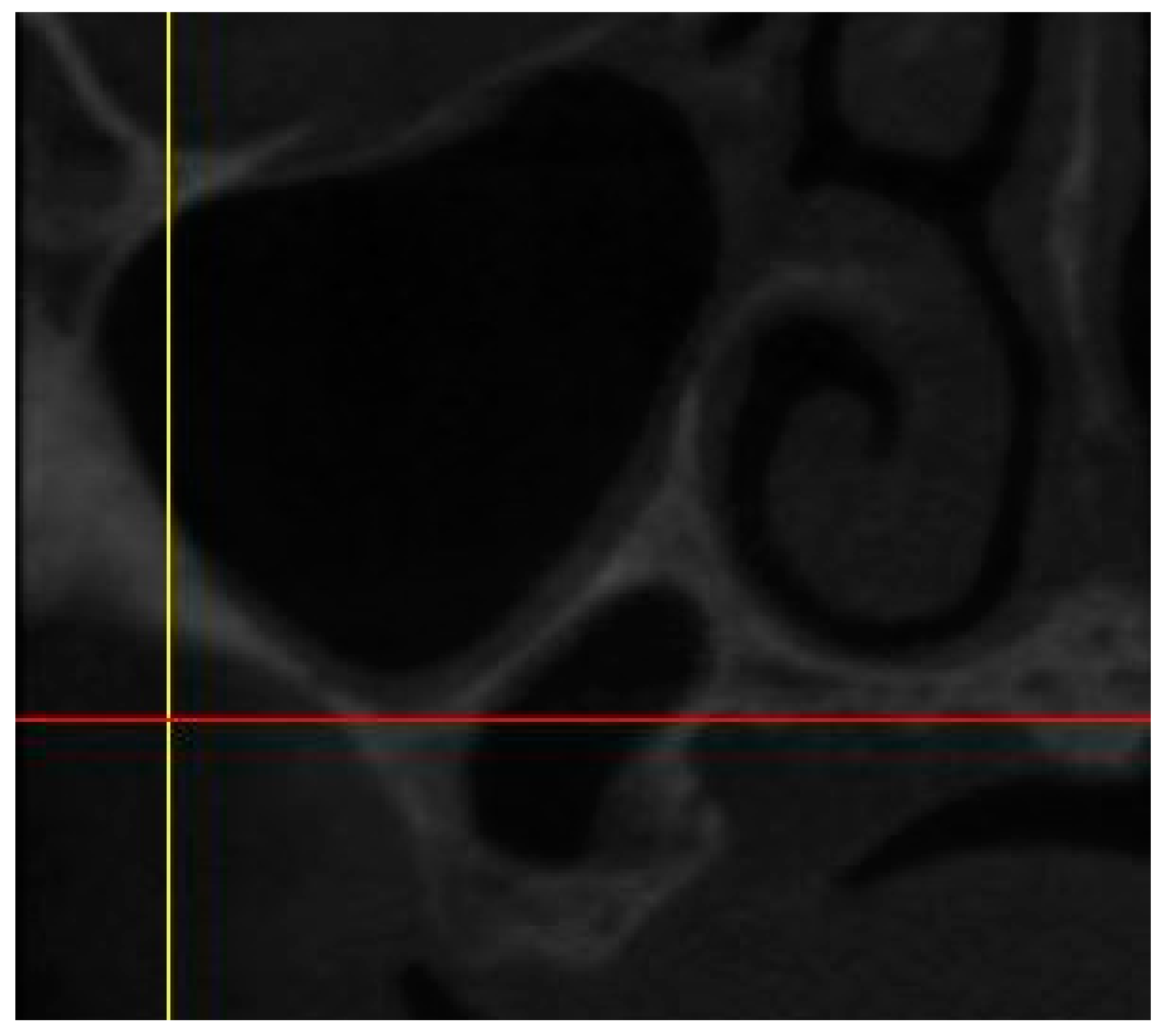
The presence of sinus septum, membrane thickening and/or pathology. (
Figure 3)
- ○
They were noted as Yes/No.
-
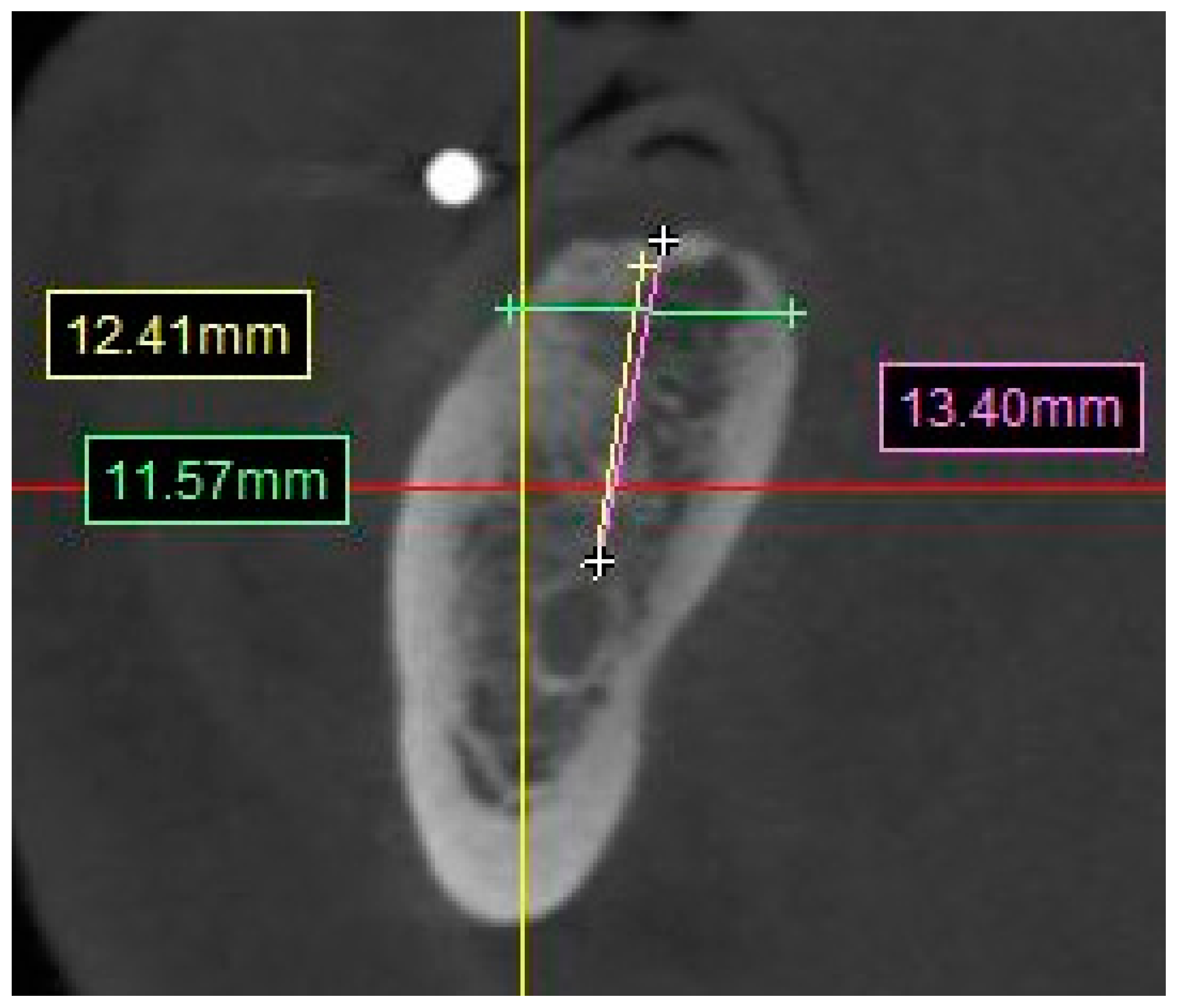
Distance from the posterior mandibular ridge to the inferior alveolar nerve. (
Figure 4)
- ○
A straight line from the crest of the planned molar location to the superior boarder of the inferior alveolar nerve canal.
-
Distance from crest of bone to the mental foramen. (
Figure 5)
- ○
The measurement was taken from the most mesial slice onto which the mental foramen opens inside the oral cavity, the measurement was taken from the most superior boarder of the mental foramen to the edge of the crest in a straight line.
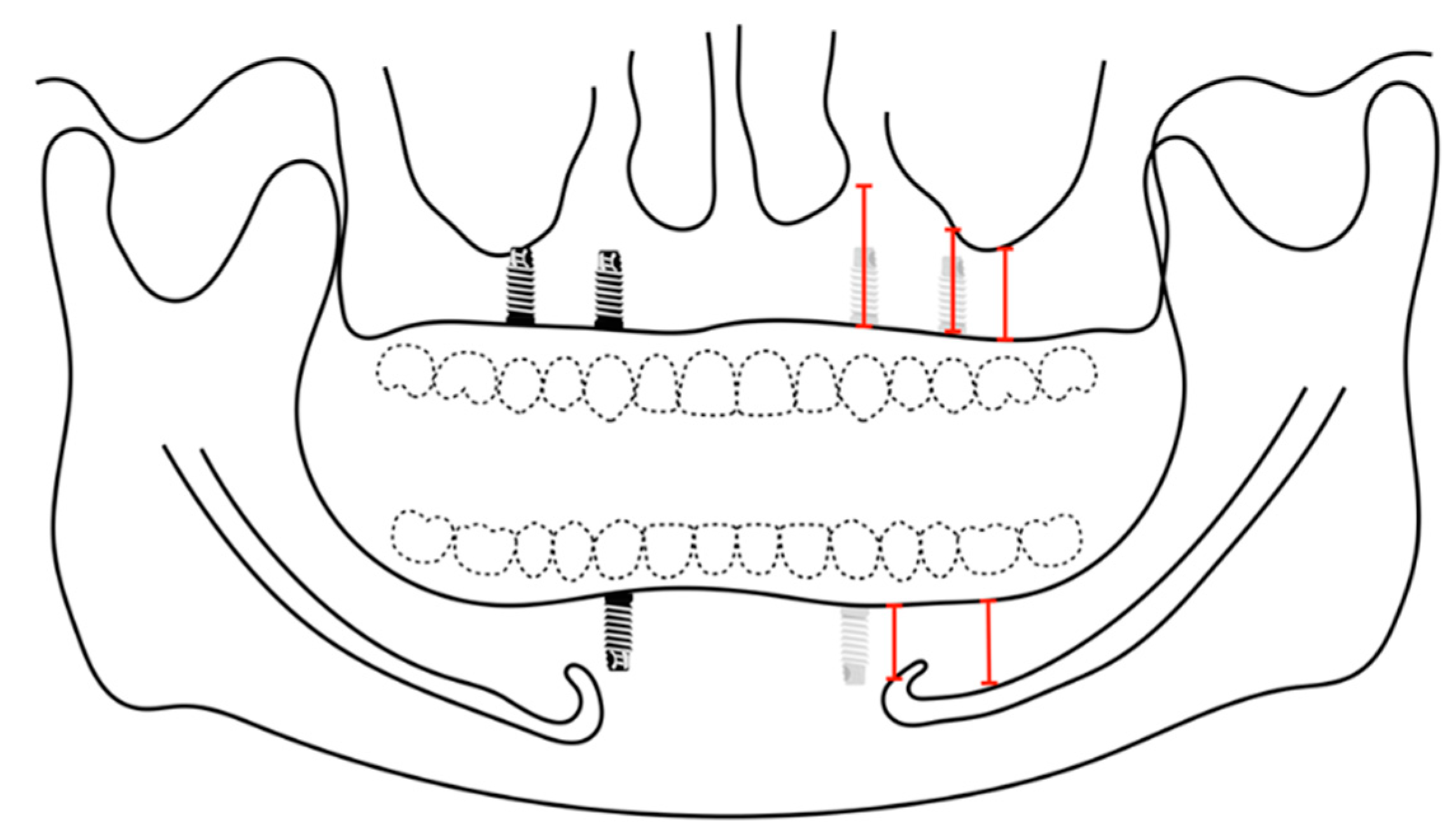
The examiners had digitally measured the alveolar ridges of 4 implant sites in the maxilla and 2 implant sites in the mandible to place implants for an implant-supported removable prosthesis for both maxillary and mandibular arches (
Figure 6). Four implants are planned for the removable prosthesis at the laterals or canines, and the second premolars areas for the maxilla. Two implants at the area of the canine for the mandible. The surgical sites are investigated if they require additional augmentation procedures in advance or afterward, whether guided bone regeneration (GBR) or sinus elevation. Each site at the data collection sheet was given a number, the following numbers were considered and standardized when performing the digital planning:
Placing standard diameter implant size (4.1mm ).
Placing narrow-diameter implant (3.3mm).
The surgical site requires horizontal augmentation.
The surgical site requires vertical augmentation.
The surgical site requires vertical augmentation via internal sinus lift.
The surgical site requires horizontal and vertical augmentation.
The surgical site requires short implants (6mm) or vertical augmentation with/or without horizontal augmentation.
After obtaining the measurements and digitally planning the implants, the individual charts were reviewed to correlate the treatment planning in the CBCT with the actual treatment rendered to the patient in the clinic.
To examine the predictability of digital planning, we considered CBCT planning as the covariate. At the same time, whether receiving the planned surgical procedure or not is the outcome of interest, performed the mixed-effects logistic regression for all upper or lower implants to accommodate the situation where some patients have both upper and lower surgical procedures [
15].
3. Results
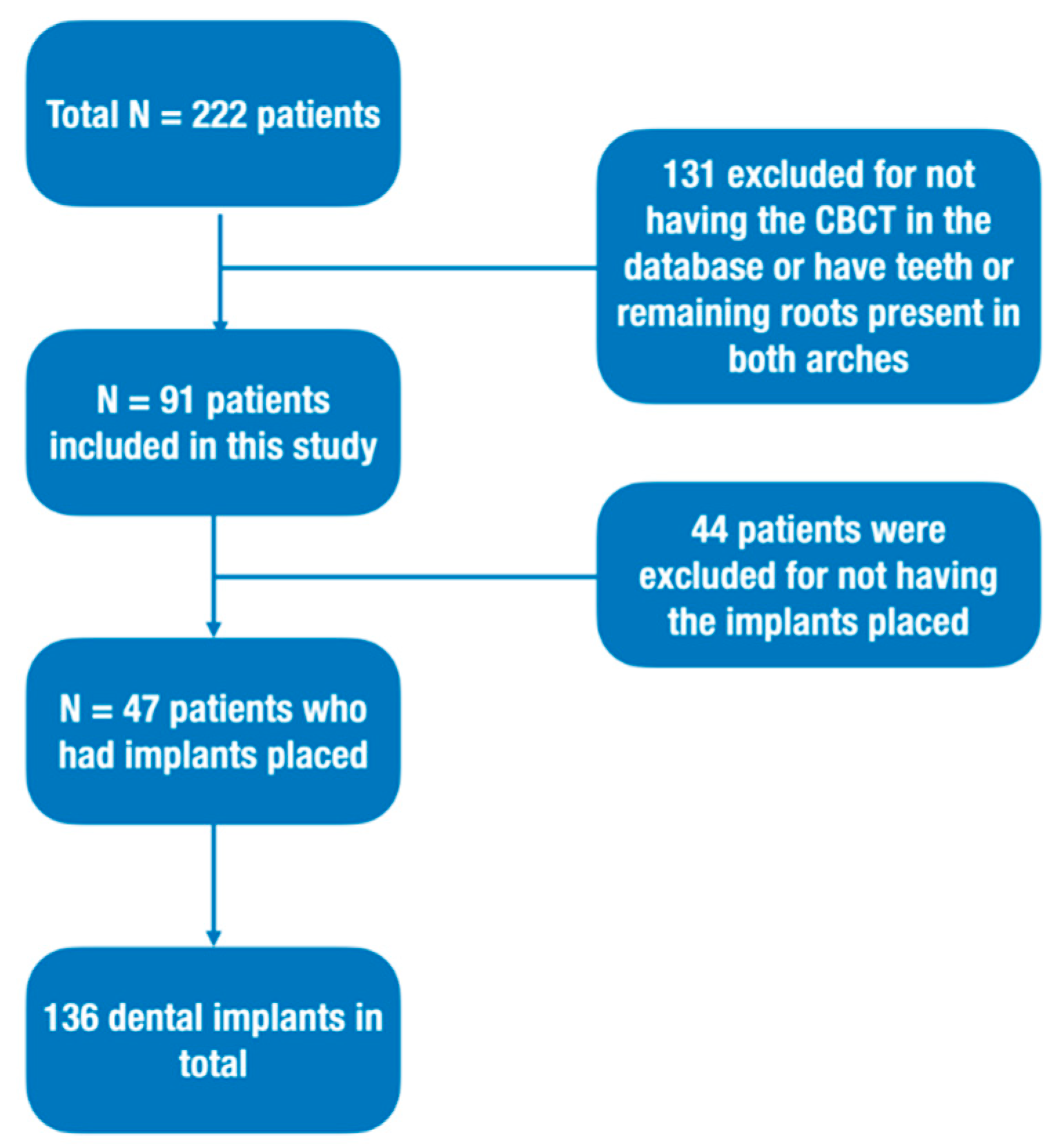
A total of 222 patients were initially evaluated for inclusion in the study. 131 patients were excluded for the missing CBCT data and/or were partial dentated patients. 91 patients’ CBCT files were utilized to digitally plan the implant placement with a mean age of 63.85 years old ±12.66. 55 out of the 91 edentulous patients were males, which correlates to (60.4%) of the total sample, and 36 (39.6%) were females.
In regard to their health history, starting with the American society of anesthesiologists’ classifications, 5 patients out of the 91 (5.5%) were classified as ASA I, 60 (65.9%) were classified as ASA II, 25 (27.5%) were classified as ASA III, and 1 (1.1%) was classified as ASA IV (Fig.12). 48 (52.7%) were smokers and 43 (47.3%) were non-smokers; And regarding diabetes, 16 (17.6%) were diabetic and 75 (82.4%) were non-diabetic.
There were 75 maxillae and 55 mandibles for the 91 patients included in this study, of which 44 (48.6%) had their CBCT scans taken with radiographic guides during the scan.
Another 44 patients were excluded because the implant procedure had not been done. Only 47 patients (55 arches) were included in the study to evaluate the predictability of predicting the implant through CBCT alone. (
Figure 7)
From the total of 91 edentulous patients, the bone volume of the digitally planned implant sites are evaluated. Four implants are planned digitally on the maxilla second premolar, and lateral incisor or canine area positions. The average height of the alveolar bone on the second premolar area is 8.89 mm and 6.78 in width. The average height of the canine area is 14.33 mm and 11.59 in width. The average height of the lateral incisor is 13.82 mm and 5.5 mm in width. Two mandibular implants are planned digitally on the lateral incisor or canine. The average height of the canine area is 13.7 mm and 7.49 in width (
Table 1). The mean distance to the sinus floor is 5.66 mm. There are 31 (41.33%) sinus pathology and/or thickening present such as retentive cyst, and 16 (21.33%) sinus septa found in the total maxillae. 18 (24%) of the second premolars were planned for lateral sinus lift, while 15 (10%) were planned for a vertical sinus lift. The mean distance to the mental foramen from alveolar crest bone is 9.08mm. while for the inferior alveolar nerve, the mean distance from the alveolar crest is 11.19mm (
Table 2).
Statistical Analysis
By using the t-test, the statistical differences between the cases that suggested with/without additional augmentation procedures for the placement of dental implant of the maxillary teeth are found in the continuous covariates: maxillary ridge height (P-value < 0.01), maxillary ridge width (P-value < 0.01), and distance to sinus floor right and left (P-value = 0.01 and < 0.01, respectively), while age, sinus pathology, and sinus septum are insignificant. As for the discrete covariates: gender, ASA classification, smoking, and diabetes, no significant results are detected via the chi-square test. While for the mandible the significant differences between the cases that suggested with/without additional augmentation procedures for the mandibular implants are found in mandibular ridge height (P-value < 0.01), mandibular ridge width (P-value < 0.01), distance to the mental foramen right and left (P-value = 0.01, P-value < 0.01, respectively), and distance to the inferior alveolar nerve right and left (P-value = 0.03, 0.02, respectively); while age, and via the chi-square test, the other demographic variables are not significant.
In the logistic regression model with LASSO regularizations for the maxilla on the suggested surgical procedures (bone augmentation or not) for the maxillary implants, only maxillary ridge height, maxillary ridge width, distance to the sinus floor left, and ASA classification (I&II vs. III&IV) are found significant and selected in the final chosen model. The result shows the expected changes 0.26, 0.14, 0.02, and 0.45 in the log odds of no bone augmentation suggested by the CBCT when 1 unit increment in the covariates (holding all the others constant), respectively. While for the mandible on the suggested surgical procedures (bone augmentation or not) for the lower implants, only lower ridge height, lower ridge width, and distance to the mental foramen left are detected with significant effects 0.29, 1.23, and 0.13 on the log odds of no bone augmentation suggested by the CBCT, respectively.
When evaluating the associations of the mean maxillary bone height with the demographic variables (age, gender, ASA classification, smoking, diabetes), only gender is shown with statistical significance (P-value = 0.01). While for the mean width, gender (P-value < 0.01) and diabetes (P-value = 0.03) are statistically significant. These results indicate that females tend to have smaller average maxillary teeth heights and widths than males, and the diabetes group tend to have higher average upper teeth widths than the non-DM patients in this study. While for the mandible when evaluating the relationships between the mean mandibular bone height/width and the demographic variables (age, gender, ASA classification, smoking, diabetes), no significant results are disclosed.
Predictability of the CBCT Planning for Implant Surgery
75 maxillae in which implant-supported removable prosthesis were treatment planned according to CBCT evaluation, of which 13 arches (17.33%) were able to have implants placed in second premolar areas, canines, or lateral incisor areas without any additional augmentation procedures digitally. A total of 55 arches of mandible implant-supported removable prostheses were treatment planned according to CBCT evaluation, in which 35 arches (63.63%) were able to have implants placed in the canine position without any additional augmentation.
A chart review was conducted to compare the implant position and any need for additional augmentation procedures.
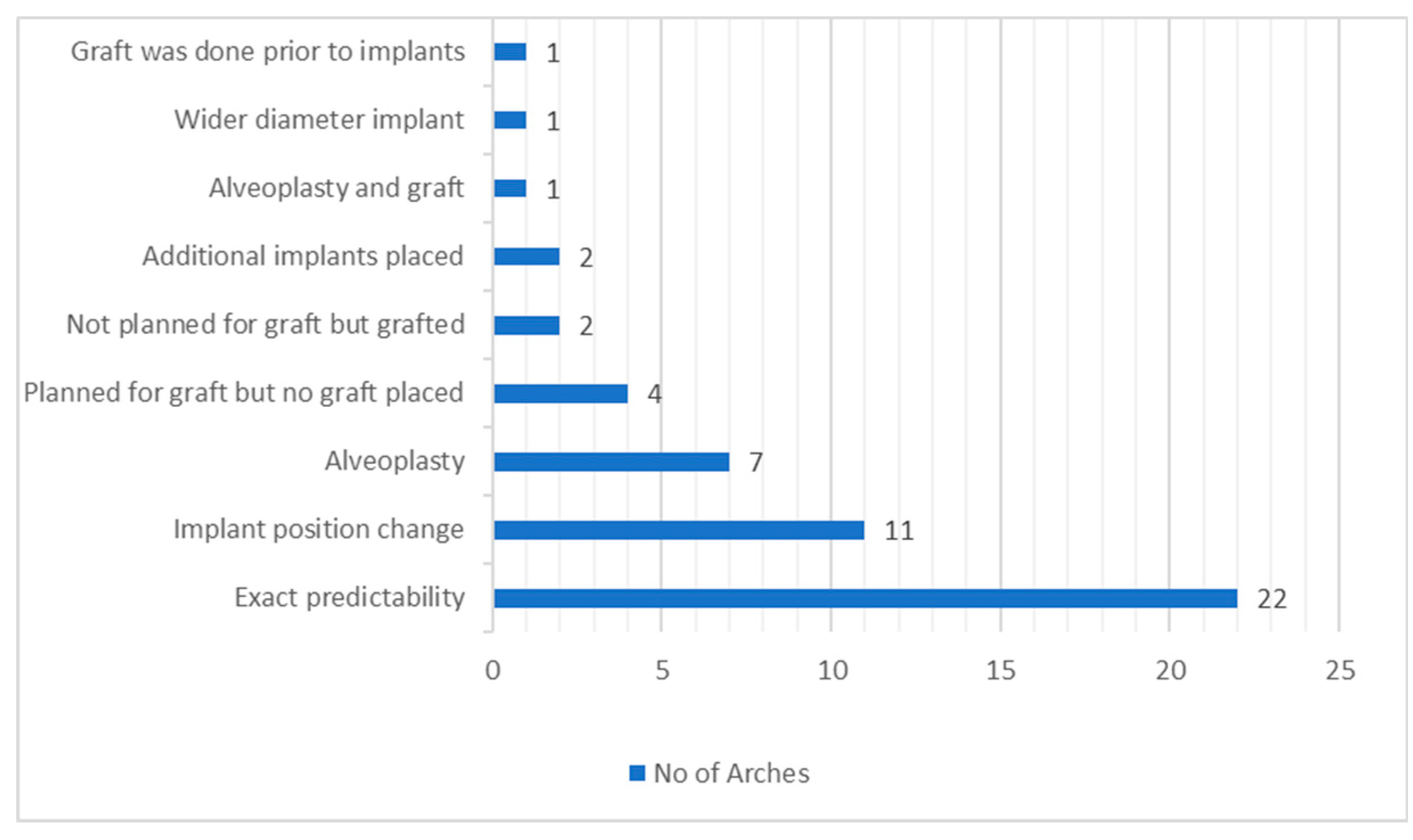
From the 47 patients who had their digital planning compared to clinical treatment, we can appreciate the following variables: (
Figure 8)
22 arches had exact predictability from digital planning.
11 arches had implant position changed.
7 arches had alveoplasty done. And one arch had alveoplasty and grafting done.
4 arches were planned for grafting, but no graft was placed.
2 arches weren’t planned for grafting but were grafted.
2 arches had implants placed in the additional site rather than mandibular canines.
1 arch received a wider diameter implant than the digital planned.
1 arch had grafting done prior to implant placement surgery.
A total of 47 out of the 91 patients had completed the implant placement in the edentulous ridge clinically, contributing to 55 maxillary and/or mandibular arches. Based on the results of mixed-effects logistic regression model, we observe that the probabilities of having the planned treatments as the digital planning are only 0.57 and 0.38), respectively, for cases that suggested with/without bone augmentation. It is clear that both predictabilities are low since a coin-flipping already has 0.5, implying the CBCT planning for implant placement on the edentulous ridge is not a good index and is insufficient to predict the implant surgical procedures as a solo method. Further information is needed to guide the planning for future surgical procedures. (
Table 3).
4. Discussion
In a review article by Orentlicher et al, he stated that to successfully integrate the cone beam technology and the cone beam-guided surgery, it must be acknowledged that a steep learning curve is required, and that dentists should pursue further continuing education to increase their understanding further for the knowledge of CT scans, their digital and treatment planning software, and the digital workflow. [
16] Guerrero et al. compared the alveolar grafting prediction between panoramic radiograph and CBCT images in 108 partially edentulous patients with 356 implants placed; they found that implant planning with cone-beam computed tomography had a higher prediction and agreement of implant planning versus the panoramic based surgery, and found that the sensitivity and the specificity of CBCT for implant complications were 96.5% and 90.5%, respectively, and for the bone graft augmentation, 95.2% and 96.3%, respectively [
17]. Mello et al investigated the impact of CBCT on implant planning and prediction of final implant size and concluded that cone beam computed tomography improved the prediction of the implant length and improved the accuracy in implant planning [
18]. Necking et al. assessed the reliability of implant placement using a surgical guide after virtual planning with CT data and concluded that cone beam data and surgical guides could be reliable for preoperative planning of implant size, position, and anatomical complications [
19].
The accuracy of CBCT in implant dentistry has also been extensively investigated. Al-Ekrish et al. [
20] found that CBCT was associated with a clinically and statistically significant measurement error of 0.49mm. In a systematic review by Fokas et al [
21] concluded that CBCT can be considered as an appropriate diagnostic tool for planning, but a 2mm safety margin is needed adjacent to anatomic structures. A systematic review by Anter et al [
22] indicated that the average CBCT measurement error ranged from 0.19mm to 1.27mm, they concluded that the evidence is not strong. Conversely, some studies showed that CBCT images underestimate the actual distances. A study by Lascala et al [
23] showed that the measurements were always larger than those for the CBCT images, but only significant for measurements of the internal structures of the skull base. Another study by Komuro et al [
24] showed that CBCT measurements were significantly smaller than model scanners, intra-oral scanner, and electronic caliper control.
Our study demonstrated that the mean maxillary posterior heights and widths were 9.35mm and 6.87mm, respectively, which meant that, on average, the posterior maxilla would require bone grafting for placement of a standard diameter implant or placing a narrow diameter implant to avoid grafting. Similarly, the mean maxillary anterior heights and widths were 14.04mm and 5.69mm, respectively, which means that, on average, the anterior maxilla would require a grafting procedure for placement of implants regardless of its size. As for the mandible, our study shows that the mean mandibular posterior heights and widths were 10.99mm and 8.21mm, respectively, which means that on average, the posterior mandible, in contrast to the maxilla could have implant placement with standard size implants without the need for secondary augmentation procedures. Similarly, the mean mandibular anterior heights and widths were 14.83mm and 7.26mm, respectively, which is also forgiving in placing dental implants without additional procedures. Compared to the clinical treatment, some of the data in our study opted to do alveoplasty to reduce the ridge height and gain width instead of using bone grafting as an option. In a similar study by Fiorellini et al. [
25], where they used CBCT to evaluate bone availability for implant placement and sloped implant design, when they evaluated the ridge dimensions, they found out that in the posterior maxilla the mean buccal bone height was 8.73mm and the mean lingual bone height was 8.52mm and the mean width was 8.06mm, while in the anterior area, the mean buccal bone height was 13.03mm and the mean lingual bone height was 12.37mm, and the mean width was 5.33mm. As for the mandible, posteriorly, the mean alveolar buccal bone height was 10.18mm, the mean alveolar buccal bone height was 11.01, and the mean width was 7.49; And anteriorly, the mean buccal bone height was 13.59mm, the mean lingual height was 13.47mm, and the mean width was 6.9mm. These measurements were remarkably close to the measurements of this study, however, in 60.6% of the site’s implants could be placed, this could be attributed to the placement of single implant rather than four or two implants as a whole. The 39.4% of the site that were not adequate for implant placement, 56.5% of which needed additional guided bone regeneration procedures. Padhye et al. [
26] evaluated 250 CBCTs with a total of 349 edentulous sites; they found that 55.45% of the molar and 54.42% of the premolar maxillary sites had a horizontal ridge width of less than 6mm and concluded that additional augmentation procedures are required in a high percentage of the population in the posterior maxillary site used standard dimension implant.
In the present study,43 of the maxillary molars (57.33%) and eighteen of the maxillary second premolars (24%) required lateral window sinus lifts. In comparison, twenty-six of the maxillary molars (17.33%) and fifteen (10%) of the maxillary second premolars required vertical lifts. Lan et al. [
27] analyzed a total of 100 CBCTs. It concluded that a high percentage of edentulous sites in the posterior maxilla need sinus floor elevation for dental implant placement. Buser et al. [
28] evaluated a total of 122 CBCT scans and found that the bone height decreased from premolar to molar areas, with first and second molar sites showing a bone height of less than 5mm (54.12% and 44.64% respectively). Padhye et al 25 found that 67.83% of the molar and 44.86% of the premolar sites showed a height of less than 8mm. Similarly, Fiorellini et al 24 found that in the 39.4% of the sites that were not adequate for implant placement, 43.5% required sinus augmentation procedures.
5. Conclusions
This retrospective study evaluated the need for additional augmentation procedures for the placement of the dental implant for implant-supported removable prostheses and the predictability of the digital planning alone on the clinical treatment as the primary objective. The low probability suggests that digital planning alone was not predictable, and other factors such as accuracy of the CBCT, bone density, and clinician error should be considered. Due to the limitation of this study and the small sample size, more data is needed in the future to confirm these findings.
Funding
The study was self-funded by the authors and their institution.
References
- Cunha-Cruz, J.; Hujoel, P.; Nadanovsky, P. Secular Trends in Socio-economic Disparities in Edentulism: USA, 1972–2001. J. Dent. Res. 2007, 86, 131–136. [Google Scholar] [CrossRef]
- Douglass, C.W.; Shih, A.; Ostry, L. Will there be a need for complete dentures in the United States in 2020? J. Prosthet. Dent. 2002, 87, 5–8. [Google Scholar] [CrossRef]
- Locker, D. Measuring oral health: a conceptual framework. Community Dent Heal. 1988, 5, 3–18. [Google Scholar]
- Vogel, R.; Smith-Palmer, J.; Valentine, W. Evaluating the Health Economic Implications and Cost-Effectiveness of Dental Implants: A Literature Review. Int. J. Oral Maxillofac. Implant. 2013, 28, 343–356. [Google Scholar] [CrossRef]
- Beikler, T.; Flemmig, T.F. EAO consensus conference: economic evaluation of implant-supported prostheses. Clin. Oral Implant. Res. 2015, 26, 57–63. [Google Scholar] [CrossRef]
- Devlin, H.; Ferguson, M.W. Alveolar ridge resorption and mandibular atrophy. A review of the role of local and systemic factors. Br. Dent. J. 1991, 170, 101–104. [Google Scholar] [CrossRef]
- Kern, J.; Kern, T.; Wolfart, S.; Heussen, N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin. Oral Implant. Res. 2016, 27, 174–195. [Google Scholar] [CrossRef]
- Pietrokovski, J.; Starinsky, R.; Arensburg, B.; Kaffe, I. Morphologic Characteristics of Bony Edentulous Jaws. J. Prosthodont. 2007, 16, 141–147. [Google Scholar] [CrossRef]
- Al-Rawee, R.Y. Anatomy respect in implant dentistry. assortment, location, clinical importance (review article). Journal of Dental Problems and Solutions 2020, 7, 68. [Google Scholar]
- Pauwels, R.; Araki, K.; Siewerdsen, J.H.; Thongvigitmanee, S.S. Technical aspects of dental CBCT: state of the art. Dentomaxillofacial Radiol. 2015, 44, 20140224. [Google Scholar] [CrossRef]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Heal. 2018, 18, 1–16. [Google Scholar] [CrossRef]
- Ganz, S.D. Three-Dimensional Imaging and Guided Surgery for Dental Implants. Dent. Clin. North Am. 2015, 59, 265–290. [Google Scholar] [CrossRef] [PubMed]
- Friedlander-Barenboim, S.; Hamed, W.; Zini, A.; Yarom, N.; Abramovitz, I.; Chweidan, H.; Finkelstein, T.; Almoznino, G. Patterns of Cone-Beam Computed Tomography (CBCT) Utilization by Various Dental Specialties: A 4-Year Retrospective Analysis from a Dental and Maxillofacial Specialty Center. Healthcare 2021, 9, 1042. [Google Scholar] [CrossRef]
- Weiss, R.; Read-Fuller, A. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Dent. J. 2019, 7, 52. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression Shrinkage and Selection Via the Lasso. J. R. Stat. Soc. Ser. B 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Orentlicher, G.; Goldsmith, D.; Abboud, M. Computer-Guided Planning and Placement of Dental Implants. Atlas Oral Maxillofac. Surg. Clin. 2012, 20, 53–79. [Google Scholar] [CrossRef]
- Guerrero, M.E.; Noriega, J.; Jacobs, R. Preoperative implant planning considering alveolar bone grafting needs and complication prediction using panoramic versus CBCT images. Imaging Sci. Dent. 2014, 44, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Pedroso, L.A.d.M.; Garcia, R.R.; Leles, J.L.R.; Leles, C.R.; Silva, M.A.G.S. Impact of cone-beam computed tomography on implant planning and on prediction of implant size. Braz. Oral Res. 2014, 28, 46–53. [Google Scholar] [CrossRef]
- Nickenig, H.-J.; Eitner, S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J. Cranio-Maxillofacial Surg. 2007, 35, 207–211. [Google Scholar] [CrossRef]
- A Al-Ekrish, A.; Ekram, M. A comparative study of the accuracy and reliability of multidetector computed tomography and cone beam computed tomography in the assessment of dental implant site dimensions. Dentomaxillofacial Radiol. 2011, 40, 67–75. [Google Scholar] [CrossRef]
- Fokas, G.; Vaughn, V.M.; Scarfe, W.C.; Bornstein, M.M. Accuracy of linear measurements on CBCT images related to presurgical implant treatment planning: A systematic review. Clin. Oral Implant. Res. 2018, 29, 393–415. [Google Scholar] [CrossRef]
- Anter, E.; Zayet, M.; El-Dessouky, S. Accuracy and precision of cone beam computed tomography in periodontal defects measurement (systematic review). J. Indian Soc. Periodontol. 2016, 20, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Lascala, C.A.; Panella, J.; Marques, M.M. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom). Dentomaxillofacial Radiol. 2004, 33, 291–294. [Google Scholar] [CrossRef]
- Komuro, A.; Yamada, Y.; Uesugi, S.; Terashima, H.; Kimura, M.; Kishimoto, H.; Iida, T.; Sakamoto, K.; Okuda, K.; Kusano, K.; et al. Accuracy and dimensional reproducibility by model scanning, intraoral scanning, and CBCT imaging for digital implant dentistry. Int. J. Implant. Dent. 2021, 7, 1–7. [Google Scholar] [CrossRef]
- Fiorellini, J.; Llobell, A.; Norton, M.; Sarmiento, H.; Chang, Y.-C.; Wada, K. Healed Edentulous Sites: Suitability for Dental Implant Placement, Need for Secondary Procedures, and Contemporary Implant Designs. Int. J. Oral Maxillofac. Implant. 2020, 35, 924–930. [Google Scholar] [CrossRef]
- Padhye, N.M.; Bhatavadekar, N.B. Quantitative Assessment of the Edentulous Posterior Maxilla for Implant Therapy: A Retrospective Cone Beam Computed Tomographic Study. J. Maxillofac. Oral Surg. 2019, 19, 125–130. [Google Scholar] [CrossRef]
- Lan, M.; Zhe, Q.; Xiang, Z.; Wenli, H. [Anatomical presentation of edentulous sites in the posterior maxillary in cone beam computed tomography]. Hua Xi Kou Qiang Yi Xue Za Zhi 2016, 34, 85–90. [Google Scholar] [CrossRef]
- Nunes, L.S.d.S.; Bornstein, M.M.; Sendi, P.; Buser, D. Anatomical characteristics and dimensions of edentulous sites in the posterior maxillae of patients referred for implant therapy. Int. J. Periodontics Restor. Dent. 2013, 33, 337–345. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).