Submitted:
11 August 2023
Posted:
14 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategry
2.3. Selection of the Studies
2.4. Risk-of-Bias Assessment
- Has the objective of the study been articulated with clarity?
- Does the study design have a clear and detailed outline?
- Are the subject/data’s characteristics and details presented distinctly?
- Does method used to assess the spinal deformity is clearly defined and described?
- Is it the study involving imaging method to diagnose spine deformity?
- Is parameter measured used in the method clearly described?
- Does it use the appropriate numerical methods in data analysis and clearly verified or validated?
- Is it study has clear outcome?
- Is it the study stated the limitations?
- Does the study have a clear conclusion?
3. Results
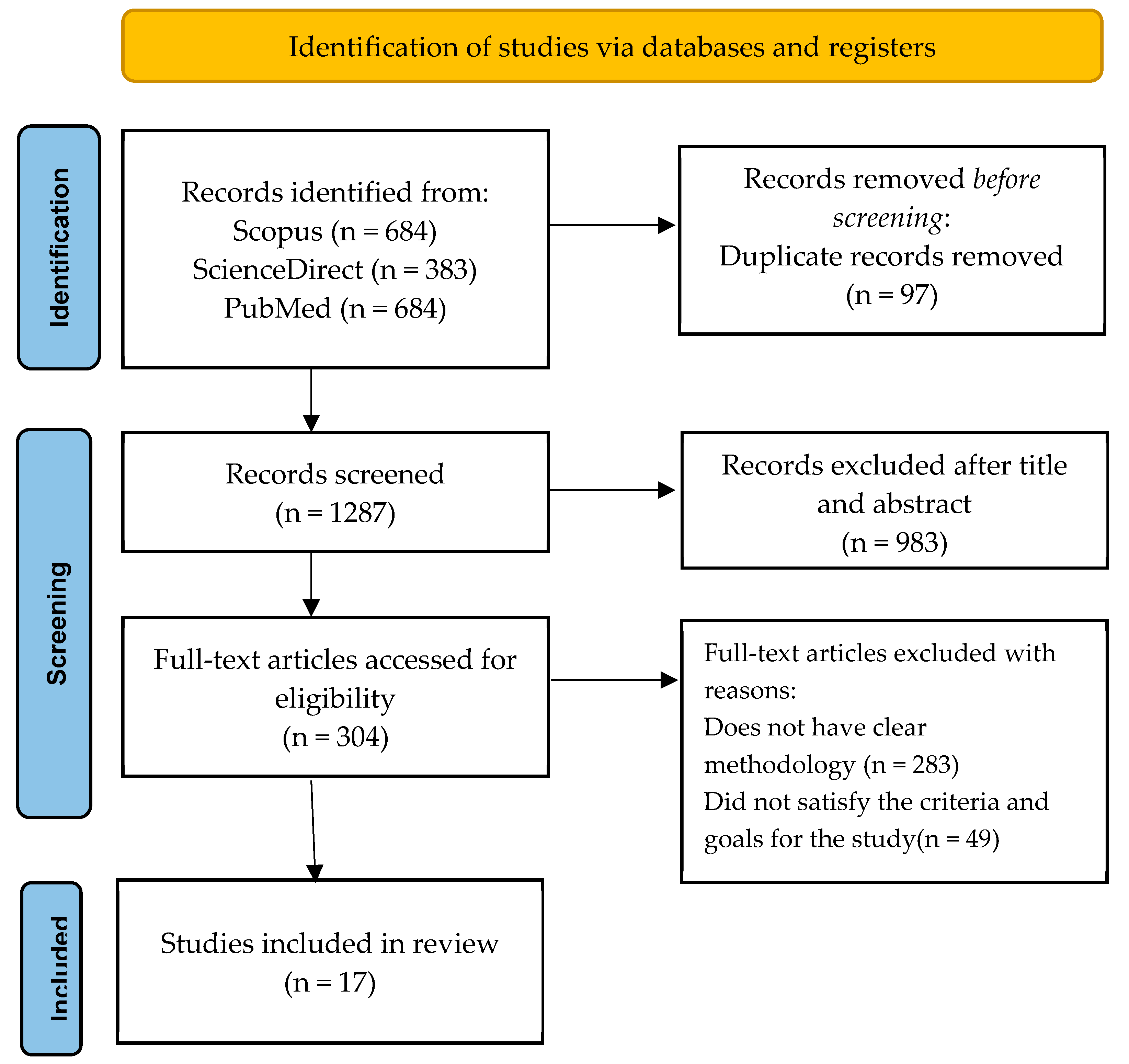
3.1. Primary Search Results.
3.2. Analyzed Data Quality.
3.3. Data Characteristics & Details
3.4. Assessment Methods for Scoliosis Diagnosis.
3.5. Other Variability used in the study.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgement
Conflicts of Interest
References
- C. Adam and G. Dougherty, “Applications of Medical Image Processing in the Diagnosis and Treatment of Spinal Deformity,” 2011, pp. 227–248. [CrossRef]
- “Adolescent Idiopathic Scoliosis: Diagnosis and Management | AAFP.” https://www.aafp.org/pubs/afp/issues/2014/0201/p193.html (accessed Feb. 13, 2023).
- D. Addai, J. Zarkos, and A. J. Bowey, “Current concepts in the diagnosis and management of adolescent idiopathic scoliosis,” Child’s Nervous System, vol. 36, no. 6, pp. 1111–1119, Jun. 2020. [CrossRef]
- J. J. Kelly et al., “Treatment of adolescent idiopathic scoliosis and evaluation of the adolescent patient,” Curr Orthop Pract, vol. 29, no. 5, pp. 424–429, Sep. 2018. [CrossRef]
- J. P. HORNE, R. FLANNERY, and S. USMAN, “Adolescent Idiopathic Scoliosis: Diagnosis and Management,” Am Fam Physician, vol. 89, no. 3, pp. 193–198, Feb. 2014, Accessed: Feb. 13, 2023. [Online]. Available: https://www.aafp.org/pubs/afp/issues/2014/0201/p193.html.
- D. Addai, J. Zarkos, and A. J. Bowey, “Current concepts in the diagnosis and management of adolescent idiopathic scoliosis”. [CrossRef]
- Karpiel, A. Ziębiński, M. Kluszczyński, and D. Feige, “A survey of methods and technologies used for diagnosis of scoliosis,” Sensors, vol. 21, no. 24. MDPI, Dec. 01, 2021. [CrossRef]
- B. Samuvel, V. Thomas, M. G. Mini, and J. Renjith Kumar, “A mask based segmentation algorithm for automatic measurement of Cobb angle from scoliosis x-ray image,” Proceedings - 2012 International Conference on Advances in Computing and Communications, ICACC 2012, pp. 110–113, 2012. [CrossRef]
- P. Shrestha, A. Singh, R. Garg, I. Sarraf, T. R. Mahesh, and G. Sindhu Madhuri, “Early Stage Detection of Scoliosis Using Machine Learning Algorithms; Early Stage Detection of Scoliosis Using Machine Learning Algorithms,” 2021 International Conference on Forensics, Analytics, Big Data, Security (FABS), vol. 1, 2021. [CrossRef]
- D. Ovadia, “Classification of adolescent idiopathic scoliosis (AIS),” J Child Orthop, vol. 7, no. 1, pp. 25–28, Feb. 2013. [CrossRef]
- L. Scaramuzzo, “Special Issue: ‘Spinal Deformity: Diagnosis, Complication and Treatment in Adolescent Patients,’” J Clin Med, vol. 12, no. 2, p. 525, Jan. 2023. [CrossRef]
- D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman, “METHODS OF SYSTEMATIC REVIEWS AND META-ANALYSIS Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement”. [CrossRef]
- K. Gunasekaran, K. S. Basaruddin, N. A. Muhayudin, and A. R. Sulaiman, “Corrective Mechanism Aftermath Surgical Treatment of Spine Deformity due to Scoliosis: A Systematic Review of Finite Element Studies,” BioMed Research International, vol. 2022. Hindawi Limited, 2022. [CrossRef]
- P. X. Ku, N. A. Abu Osman, and W. A. B. Wan Abas, “Balance control in lower extremity amputees during quiet standing: A systematic review,” Gait and Posture, vol. 39, no. 2. pp. 672–682, Feb. 2014. [CrossRef]
- J. Yang et al., “Development and validation of deep learning algorithms for scoliosis screening using back images,” Commun Biol, vol. 2, no. 1, Dec. 2019. [CrossRef]
- T. Liu et al., “A multi-scale keypoint estimation network with self-supervision for spinal curvature assessment of idiopathic scoliosis from the imperfect dataset,” Artif Intell Med, vol. 125, Mar. 2022. [CrossRef]
- S. Roy, A. T. D. Grünwald, A. Alves-Pinto, and R. Lampe, “Automatic analysis method of 3D images in patients with scoliosis by quantifying asymmetry in transverse contours,” Biocybern Biomed Eng, vol. 40, no. 4, pp. 1486–1498, Oct. 2020. [CrossRef]
- J. Hurtado-Avilés et al., “Validity and Absolute Reliability of the Cobb Angle in Idiopathic Scoliosis with TraumaMeter Software,” Int J Environ Res Public Health, vol. 19, no. 8, Apr. 2022. [CrossRef]
- A. T. D. Grünwald, S. Roy, and R. Lampe, “Scoliosis assessment tools to reduce follow-up X-rays,” J Orthop Translat, vol. 38, pp. 12–22, Jan. 2023. [CrossRef]
- D. Čelan, B. Jesenšek Papež, P. Poredoš, and J. Možina, “Laser triangulation measurements of scoliotic spine curvatures,” Scoliosis, vol. 10, no. 1, Sep. 2015. [CrossRef]
- J. Dubousset, B. Ilharreborde, and J. C. Le Huec, “Use of EOS imaging for the assessment of scoliosis deformities: Application to postoperative 3D quantitative analysis of the trunk,” European Spine Journal, vol. 23, no. SUPPL. 4, 2014. [CrossRef]
- T. Colombo et al., “Supervised and unsupervised learning to classify scoliosis and healthy subjects based on non-invasive rasterstereography analysis,” PLoS One, vol. 16, no. 12 December, Dec. 2021. [CrossRef]
- Y. Yıldırım, K. Tombak, S. Karaşin, İ. Yüksel, A. H. Nur, and U. Ozsoy, “Assessment of the reliability of hand-held surface scanner in the evaluation of adolescent idiopathic scoliosis,” European Spine Journal, vol. 30, no. 7, pp. 1872–1880, Jul. 2021. [CrossRef]
- S. Rothstock, H.-R. Weiss, D. Krueger, and L. Paul, “Clinical classification of scoliosis patients using machine learning and markerless 3D surface trunk data”. [CrossRef]
- Q. Wang, M. Li, E. H. M. Lou, and M. S. Wong, “Reliability and validity study of clinical ultrasound imaging on lateral curvature of adolescent idiopathic scoliosis,” PLoS One, vol. 10, no. 8, Aug. 2015. [CrossRef]
- Y. P. Zheng et al., “A reliability and validity study for Scolioscan: A radiation-free scoliosis assessment system using 3D ultrasound imaging,” Scoliosis Spinal Disord, vol. 11, no. 1, May 2016. [CrossRef]
- V. Luković, S. Ćuković, D. Milošević, and G. Devedžić, “An ontology-based module of the information system ScolioMedIS for 3D digital diagnosis of adolescent scoliosis,” Comput Methods Programs Biomed, vol. 178, pp. 247–263, Sep. 2019. [CrossRef]
- J. R. L. Navarro, C. T. Candotti, T. S. Furlanetto, V. H. Dutra, M. A. do Amaral, and J. F. Loss, “Validation of a Mathematical Procedure for the Cobb Angle Assessment Based on Photogrammetry,” J Chiropr Med, vol. 18, no. 4, pp. 270–277, Dec. 2019. [CrossRef]
- Sikidar, K. E. C. Vidyasagar, M. Gupta, B. Garg, and D. Kalyanasundaram, “Classification of mild and severe adolescent idiopathic scoliosis (AIS) from healthy subjects via a supervised learning model based on electromyogram and ground reaction force data during gait,” Biocybern Biomed Eng, vol. 42, no. 3, pp. 870–887, Jul. 2022. [CrossRef]
- D. Yang et al., “Semi-automatic method for pre-surgery scoliosis classification on X-ray images using Bending Asymmetry Index,” Int J Comput Assist Radiol Surg, vol. 17, no. 12, pp. 2239–2251, Dec. 2022. [CrossRef]
- P. Główka, W. Politarczyk, P. Janusz, Ł. Woźniak, and T. Kotwicki, “The method for measurement of the three-dimensional scoliosis angle from standard radiographs,” BMC Musculoskelet Disord, vol. 21, no. 1, Jul. 2020. [CrossRef]
- Y. shun Wong et al., “Is Radiation-Free Ultrasound Accurate for Quantitative Assessment of Spinal Deformity in Idiopathic Scoliosis (IS): A Detailed Analysis With EOS Radiography on 952 Patients,” Ultrasound Med Biol, vol. 45, no. 11, pp. 2866–2877, Nov. 2019. [CrossRef]
- Saylor, “Artificial Neural Network for the Estimation of Clinical Parameters from X-rays of Scoliotic Spines,” 2020.
- “Vertebra Segmentation for Spinal Deformity Assessment from X-ray Images - ProQuest.” https://www.proquest.com/docview/2570358625/F320EB77D7BE4628PQ/1?accountid=33397 (accessed Feb. 13, 2023).
- B. Drerup, “Rasterstereographic measurement of scoliotic deformity,” Scoliosis, vol. 9, no. 1, pp. 1–14, Dec. 2014. [CrossRef]
- Juliene Rodrigues Leite Navarro, B. Nichele da Rosa, and C. Tarragô Candotti, “Anatomical reference marks, evaluation parameters and reproducibility of surface topography for evaluating the adolescent idiopathic scoliosis: a systematic review with meta-analysis,” 2019. [CrossRef]
- V. Kaul, S. Enslin, and S. A. Gross, “History of artificial intelligence in medicine,” Gastrointest Endosc, vol. 92, no. 4, pp. 807–812, Oct. 2020. [CrossRef]
- K. Chen, X. Zhai, K. Sun, H. Wang, C. Yang, and M. Li, “A narrative review of machine learning as promising revolution in clinical practice of scoliosis,” Ann Transl Med, vol. 9, no. 1, p. 67, 2021. [CrossRef]
- S. Patel, “Deep learning models for image segmentation,” Proceedings of the 2021 8th International Conference on Computing for Sustainable Global Development, INDIACom 2021, pp. 149–154, Mar. 2021. [CrossRef]
- Ronneberger, P. Fischer, and T. Brox, “U-net: Convolutional networks for biomedical image segmentation,” Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), vol. 9351, pp. 234–241, 2015. [CrossRef]
- Q. Zhang, Y. Du, Z. Wei, H. Liu, X. Yang, and D. Zhao, “Spine Medical Image Segmentation Based on Deep Learning,” 2021. [CrossRef]
- P. Cheng, Y. Yang, H. Yu, and Y. He, “Automatic vertebrae localization and segmentation in CT with a two-stage Dense-U-Net,” Scientific Reports |, vol. 11, p. 22156, 123AD. [CrossRef]
- W. Weng and X. Zhu, “INet: Convolutional Networks for Biomedical Image Segmentation,” IEEE Access, vol. 9, pp. 16591–16603, 2021. [CrossRef]
| Authors and Year | Questions | Overall Score | Overall (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||
| Dubousset et al. (2014) [21] | 1 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 16/20 | 80.0 | |
| Colombo et al. (2021) [22] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 19/20 | 95.0 | |
| Yang et al. (2019) [15] | 2 | 1 | 2 | 2 | 2 | NA | 1 | 2 | 1 | 1 | 14/18 | 77.8 | |
| Yildirim et al. (2021) [23] | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 0 | 16/20 | 80.0 | |
| Grunwald et al. (2023) [19] | 1 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 16/20 | 80.0 | |
| Rothstock et al. [24] | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 17/20 | 85.0 | |
| Liu et al. (2022) [16] | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 1 | 17/20 | 85.0 | |
| Wang et al. (2015) [25] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 18/20 | 90.0 | |
| Zheng et al. (2016) [26] | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 17/20 | 85.0 | |
| Lukovic et al. (2019) [27] | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 17/20 | 85.0 | |
| Navarro et al. (2019) [28] | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 18/20 | 90.0 | |
| Celan et al. (2015) [20] | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 1 | 14/20 | 70.0 | |
| Yang et al. (2022) [30] | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 18/20 | 90.0 | |
| Sikidar et al. (2022) [29] | 2 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 16/20 | 80.0 | |
| Roy et al. (2020) [17] | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 17/20 | 85.0 | |
| Hurtado-Aviles et al. (2022) [18] | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 17/20 | 85.0 | |
| Glowka et al. (2020) [31] | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 16/20 | 80.0 | |
| Authors | Source of data | Number Subject/ Data |
Gender | Details of Subject/Data |
|---|---|---|---|---|
| Dubousset et al. [21] | Patients | 49 | Male: 4 Female: 45 |
Age: 13 – 17 years old |
| Colombo et al. [22] | Healthy and scoliotic patients |
298 | Male: 135 Female: 163 |
Inclusion criteria: - Age: 14 – 30 years old Male or female Exclusion criteria: - Clinical background of vertebrae pathological condition of vertebrae whether congenital or acquired. Medical history of vertebral fractures and/or vertebral surgery. Disc protrusion/ hernia in any level of the spine diagnosis. Diagnosis of scoliosis is secondary to neurological, rheumatological and/or congenital conditions. AIS diagnosis through X-rays with Cobb angle greater than 45º. Any neurological and/or rheumatological conditions diagnosis. |
| Yang et al. [15] | Labeled images of unclothed backs and standing posterior-anterior X-ray images of spine or ultrasound images from normal and scoliosis patients |
3240 | Male: 1029 Female: 2211 |
Age: 10 - 20 years old Exclusion criteria: - Subjects exhibit nontrue scoliosis (attributed to pain or by leg discrepancy, amongst other factors). Other spine disorders or abnormalities in the back region (such as soft tissue mass, thoracic cage diseases, etc). |
| Yildirim et al. [23] | Patients | 42 | Male: 10 Female: 32 |
Age: 10 – 20 years old Caucasian ethnic group Exhibits a double spinal curve with convexity towards the right in thoracic region and convexity towards left in lumbar region. Exclusion criteria: - Gap between the umbilicus-medial malleolus and SIAS-medial malleolus on both right and left side must exceeds one centimeter. |
| Grunwald et al. [19] | Patients | 10 | Male: 5 Female: 5 |
Age: 11-50 years old. Show signs of spinal deformation. Able to stand upright without support. |
| Rothstock et al. [24] | Patients | 50 | NM | Age: 12 – 15 years old. Adolescent idiopathic scoliosis patients and are scheduled to have initial bracing to eliminate any potential artefacts from prior treatments or operations. |
| Liu et al. [16] | X-ray images in anterior-posterior (AP) and lateral (LAT) position | 400 images of 200 patients | NM | Height-width ratios of the image ratio from 1.85 to 2.16. Average image resolution is 3560 x 1740 x 3 pixels and resize into 1024 x 512 x 3 pixels. |
| Wang et al. [25] | Patients | 16 | Female: 16 | Inclusion criteria: Adolescent female. Age: 10-18 years. Cobb angle: 10º - 80º. No previous surgical treatments. MRI examination of the entire spine on the study day without the use of a brace. |
| Zheng et al. [26] | Patients | 49 | Male: 15 Female: 34 |
Age: 11 – 23 years. Exclusion criteria: Have metallic implants. BMI higher than 25 kg/m². Cobb angle larger than 50º. |
| Lukovic et al. [27] | Patients | 35 | Male: 15 Female: 20 |
Age: 11 to 18 years. |
| Navarro et al. [28] | Patients | 61 | NM | Age: 7 – 18 years. Eligibility criteria: Doctors requested to conduct a full-spine radiography. Have ability to maintain an upright position independently. Does not undergo surgical procedure in the spinal region. Absence of spina bifida, sixth lumbar vertebra, or fewer than 12 thoracic vertebrae. |
| Celan et al. [20] | Patients | 275 | Male: 129 Female: 146 |
Age: 16 – 82 years. Distributed into 2 groups which are scoliosis group that has been clinically confirmed scoliosis (28 patients) and control group that has been clinically confirmed physiological spinal curvatures (247 patients). |
| Yang et al. [30] | Patients | 30 | Male: 9 Female: 21 |
- |
| Sikidar et al. [29] | Patients | 16 | All female | Inclusion criteria: Age Range: 12–22 years. Cobb angle: (Healthy controls (HC) < 20º, 20º < Mild scoliosis (MS) < 40º, Severe scoliosis (SS) > 40º). Height range: 130 – 170 cm. Weight range: 25 – 65 kg. Exclusion criteria: Has neurodegenerative disorder such as ataxia, dystonia, Parkinson’s, etc. |
| Roy et al. [17] | Computed Tomography (CT) images |
26 | Male: 14 Female: 12 |
Age: 18 to 86 years. |
| Hurtado-Aviles et al. [18] | X-ray images | 21 | NM | Image resolution is 283.46 pixels/mm and printed in dimension of 350 by 430 mm. |
| Glowka et al. [31] | Patients | 41 | NM | Inclusion criteria: Presence of a main curve either in thoracic or lumbar region. Imaging modalities conducted throughout duration of the hospitalization: High quality plain-standing X-rays (PA and lateral) and thoracic and lumbar spine CT scans conducted as part of the preoperative protocol. Exclusion criteria: Scoliosis type other than the idiopathic, a lack of CT or PA and lateral standing X-ray data, and poor-quality X-rays. |
| Authors | Instrumentation/ Imaging Modality |
Parameters/Landmark Evaluated | Assessment Method of Scoliosis Diagnosis |
Software/ Tools |
|---|---|---|---|---|
| Dubousset et al. [21] | EOS imaging system |
Thoracic: Thoracic volume, mean spinal penetration (SPIm), apical spinal penetration (SPIa) Spinal and Pelvic: T4/T12 kyphosis, L1/S1 lordosis, Cobb angles of different curves; (lumbar, main thoracic, proximal thoracic), apical vertebral rotation (AVR), torsion index of main thoracic curve |
Three-dimensional reconstructions of spine and rib cage from EOS low dose biplanar stereoradiography |
IdefX (version 4.8.4, Arts et Metiers ParisTech) |
| Colombo et al. [22] | Rasterstereography | Rasterstereographic measurements: 40 VRS features including thoracic kyphosis angle, lumbar lordosis angle, lumbar fle´che, cervical fle´che, kyphotic apex |
Supervised and unsupervised machine learning (ML) | Video-Raster-Stereography (VRS), Formetric 4D system |
| Yang et al. [15] | Camera X-ray Ultrasound |
NA | Deep learning algorithms (DLAs): Faster-RCNN and Resnet | MATLAB |
| Yildirim et al. [23] | Hand-held 3D scanner device | Distance, angle, and geometric measurements |
Image processing after 3D scanning (Segmentation and superimposition) and 3D analysis (point to point distance calculation and colored deviation map) |
Artec studio software, Netfabb Basic software, GraphPad Prism software |
| Grunwald et al. [19] | Body scanner system incorporates both an infrared depth sensor and a RGB video camera. |
Thoracic, lumbar, thoraco-lumbar region. |
Graphical user interface (GUI) of body scanner image analysis tools |
Computer Aided Design (CAD), FEBio software |
| Rothstock et al. [24] | 3D depth sensor | Cobb Angle and Augmented Lehnert-Schroth (ALS) |
Machine learning (ML) | Python 3.1, Artec studio software |
| Liu et al. [16] | 2 plane view X-ray | 3D coordinate of spinal curvature |
A multi-scale keypoint estimation network and a self-supervision module |
Pytorch platform on NVIDIA RTX 2080Ti GPU |
| Wang et al. [25] | Ultrasound MRI |
COL | Measurements Center of laminae (COL) |
Custom developed software |
| Zheng et al. [26] | Scolioscan | Scolioscan angle | 3D ultrasound imaging method: Scolioscan system | Scolioscan |
| Lukovic et al. [27] |
Formetric DIERS raster-stereography scanner and Digital photo camera |
Cobb angle and Spinal curvature |
Ontology-based of the information system ScolioMedIS |
MATLAB |
| Navarro et al. [28] | Digital camera (Sony Cybershot DSC-F717, 5.0 megapixels, 512 Mb of memory, 5x optical zoom and 10x digital zoom) and radiography |
Digital Image-based Postural Assessment (DIPA) angle and Cobb angle |
Photogrammetry and radiographic evaluation |
DIPA software and MATLAB v7.9. |
| Celan et al. [20] | 3D laser profilemeter |
Extreme points in the antero-posterior (AP) and left-right (LR) views |
3D laser-triangulation system | NM |
| Yang et al. [30] | X-ray | Bending Asymmetry Index (BAI) | Semi-automatic X-ray based BAI method. 2 stages involved which are manual annotation and adjustment of pelvis level inclination and automatic generation of BAI values. |
NM |
| Sikidar et al. [29] | SMART DX100 | Electromyogram (EMG) and Ground Reaction Force (GRF) | Supervised learning model | Mokka open-source software (Version 0.6.2, 64 bit, Windows, Biomechanical Toolkit) |
| Roy et al. [17] | Computed Tomography (CT) scans |
Circularity, Difference between the areas located on the left and right of the spinous process (LRAsm) and Difference between the ratios of width/depth on each side of the centroid of the contour (ASR). |
Automatic analysis of 3D structure of human torso by quantifying asymmetry in transverse contours. | MATLAB and 3D slicer software |
| Hurtado-Aviles et al. [18] | X-ray | Cobb angle | Computer-aided measurement system | TraumaMeter software |
| Glowka et al. [31] | Computed Tomography and digitally reconstructed radiographs (DRRs) |
3D scoliosis angle | Measurement of the 3D angles between the upper-end vertebra’s upper endplate (three points coordinate) and lower-end vertebra’s lower endplate (three-points coordinate). |
DeVide Software |
| Authors | Protocol/Design of study | Plane/View | Outcome Measures |
|---|---|---|---|
| Dubousset et al. [21] | Patients in standing position in less than 15 min to obtain their specific 3D spinal reconstruction with the EOS system. Thoracic parameters were computed, and spinal and pelvic parameters were measured during the reconstructions. |
Axial Frontal Sagittal |
Mean pelvic incidence 54.3º (±14) Rotation of axial pelvic ranged between 2º and 6º Spinal parameters (Mean ± standard deviation) Cobb angle of main thoracic (61.2 ± 13º) AVR (19.9 ± 7º) Torsion index 15.8 ± 6 Proximal thoracic Cobb angle (30 ± 11º) Lumbar Cobb angle (42 ± 11º) T4-T12 kyphosis (18 ± 13º) L1-S1 lordosis (53.7 ± 14º) Thoracic parameters (Mean ± standard deviation) Thoracic volume (5056 mm³ ± 869) SPIa (13.3% ± 1.7) SPIm (8.7% ± 1.2) |
| Colombo et al. [22] | Patients maintain a static stance in an upright posture at a predetermined distance from camera for 6 seconds. Data acquisition (sample of pictures) obtained by Formetric 4D system. Then, data were undergone cleaning and normalization before proceeding to machine learning procedure. |
Frontal Sagittal |
Accuracy for unsupervised classifier ML for full set features achieved 61.7% and minimal set features achieved 72.2%. Accuracy for supervised classifier ML for full set features achieved 87.5% and 86.3%. While accuracy of minimal set features achieved 83.7% and 85.5%. |
| Yang et al. [15] | Subjects need to stand naturally, and for data acquisition conducted using multiple cameras. The patient’s back was captured disrobing above hip. Data collected from 3240 patients with images of labeled back and entire spine standing posterior-anterior X-ray images or ultrasound images which were used for training validation dataset. For external validation, 400 images were used for the process. Both training and external validation were performed for three algorithms which are cases with curve ≥ 10º, cases with curve ≥ 20º and curve severity grading. |
Frontal | Performance of DLAs was measured by accuracy, sensitivity, and specificity which the results as below: - Algorithm 1: Accuracy=75%, Sensitivity=80.67%, Specificity=58% Algorithm 2: Accuracy=87%, Sensitivity=84%, Specificity=90% Algorithm 3: Accuracy=55% |
| Yildirim et al. [23] | Patients’ back surface scanned with 3D hand-held scanner in three distinct positions (P1: stand with arms hanging at the sides, P2: stand with arms extended, P3: bend forward). Patients required to stabilize their body position as much as possible while maintaining normal breathing. Distance patients with scanner adjusted according to the distance indicator in Artec Studio software and 3D surfaces of the patients acquired. |
Frontal | The RMS and Cobb values in the thoracic were observed to have a significant correlation coefficency (r) (P1 = 0.80,P2 = 0.76, P3 = 0.71) and lumbar region (P1 = 0.56, P2 = 0.65, P3 = 0.63); |
| Grunwald et al. [19] | Patients need to maintain static and vertical stance while their arms slightly abducted in front of the scanner. The scanning duration took no more than 10 seconds. |
Coronal Transverse Sagittal |
Correlation coefficients of ρs>0.87 indicates strong correlation between Cobb angle and lateral deviation, between Cobb angle and rotation of the vertebrae. Parameters have potential to offer supplementary information. |
| Rothstock et al. [24] | Patients need to be positioned in vertical stance with their arms slightly extended away laterally from the torso on an electronic tumtable for full torso 360º 3D scanning. Reconstruction of 3D trunk surface was done by 3D software for data acquisition. Data analysis and classification were performed in term radiographic analysis and 3D surface topography. |
Coronal Transverse Sagittal |
Accuracy classification for curve severity = 90%. Accuracy classification for ALS = 50 – 72%. |
| Liu et al. [16] | Data acquisition of 400 full spine radiography images in anterior and lateral views from 200 patients. The dataset image resized and partitioned into two sets, training set (340 images) and validation set (60 images). Conventional augmentation method applied to the dataset. (Add gaussian noise and rotated up to 10 degrees randomly). |
Anterior-posterior and lateral | Average precision, AP= 81.5 AP with regarding both AP and LAT views. Pearson correlation coefficient (ρ) = 0.925. Statistical significance test: p-value = 0.02134. Null hypothesis states that there is no significant difference in the AP between proposed method and the average outcome of the other established method. Requires verification in real-world scenario. |
| Wang et al. [25] | Ultrasound scan was performed with following parameters: a frequency of 2.5MHz, an 18 cm penetration depth, gain 10%. Patients’ backs palpated and marked from C7 to S1 using a water-soluble marker for the scanning process. The patient laying on the scanning couch in supine position and received a total of 6 scans that evaluated by 2 raters which each rater with 3 scans. |
Coronal | Has significant intra- and inter-rater reliability to measure the coronal curvatures. (Both with ICC, (2, K) > 0.9, p < 0.05) There is no significant difference (p<0.05) found of COL method in ultrasound during measurement of coronal curvature at supine position. Bland-Altman method evinced an accord between these two methods, and it was found that Pearson’s correlation coefficient (r) has a high value (r>0.9, p<0.05). |
| Zheng et al. [26] | Subjects stands in front of the Scolioscan according to the locations of the four supporters at the scanner. Subjects scanned using the Scolioscan probe along the screening region. |
Coronal | Scolioscan angle measurement shows a remarkably commendable intra-rater and intra- operator reliability with ICC larger than 0.94 and 0.88 respectively.The angles measurement between Scolioscan angle and Cobb angle provide moderate to string associations with R2 greater than 0.72 for both thoracic and lumbar regions. It was observed that Scolioscan angle tends to slightly underestimate the extent of spinal deformity compared to Cobb angle. |
| Lukovic et al. [27] | System developed with the aid of an ontology – based module that implement four fundamental steps which are specification, conceptualization, formalization and implementation. |
Frontal Sagittal |
The system has capacity to classify spinal curvatures and produce statistical markers about spinal curvatures frequency, degree progression and Lenke classification system. |
| Navarro et al. [28] | Photogrammetry method: Patients subjected to a photographic register in orthostatic posture and has the same position as the radiograph method for the upper and lower limbs. The spinous process of the C7, T2, T4, T6, T8, T10, T12, l2, l4 and S2 vertebrae were marked using double-sided tape on to indicates as reference anatomic landmarks. Radiologic method: Patients assumed in a relaxed orthostatic posture with the trunk pressed against the grid and keep the upper limbs at the side of the body and the feet while radiologist obtained the full-spine radiographs. Inspiratory apnea maintained during the process of the radiograph. |
Coronal for photogrammetry and anteroposterior for radiography |
Thoracic, lumbar, and thoracolumbar scoliotic curve topographies were used to categorise the analyses. All the areas of the spine had high correlations (ranging from 0.72 to 0.81) and significant correlation coefficients (between 0.75 and 0.88). The mean difference was quite near to zero, while the root-mean-square error ranged from 5 to 11 degrees. The area under the curve, which ranged between 95% and 99 percent, was outstanding and noteworthy. |
| Celan et al. [20] | Patients in upright standing position and lean against to a foam affixed to the wall during the measurements. Arms were allowed to hang freely near body while hold their breath. |
Transversal Frontal |
The distances between the extreme points of the spine in the AP view were found to marginally different between the groups (p = 0.1), however the distances between the LR extreme points observed to have a greater significant difference in the scoliosis group compared to the control group (p < 0.001). The quotient LR/AP was determined to be statistically different in both groups (p < 0.001). Thus, this indicates that the method is proficient enough to differentiate between scoliotic and healthy subjects based on statistically differences. |
| Yang et al. [30] | Patients undergone X-ray scanning in three adopted postures which are anterior-posterior (AP) supine, left and right bending. |
Coronal | Between BAI and S-Cobb, the correlation value was R² = 0.730 (p 0.05). Out of 30 patients, 1 case was proven to have be incorrectly diagnosed while using the Lenke classification before and has now been corrected. All scoliotic curve types were correctly identified. |
| Sikidar et al. [29] | Dataset was obtained while the subjects in static pose (standing), and approximately 2 to 6 trials were captured during gait (walking) per subject, contingent on the subject’s level of comfort. Placement of markers adopted from Helen Hayes protocol at sampling frequency of 500 Hz. |
NA | The classification accuracy for SS, MS and HC group was 90.6%. The proposed model has capability detection of AIS in early stages and can be utilized by medical professionals to strategize treatments and remedical measures. |
| Roy et al. [17] | Data collected from the study conducted by the radiology department and underwent analysis of CT images. |
Sagittal Coronal Transverse |
Patients with thoracic scoliosis have larger value for both LRAsm and ASR which the degree of asymmetry was more pronounced in thoracic than in the lumbar region. Lumbar scoliosis patients have smaller value for both LRAsm and ASR which the asymmetry being less pronounced in thoracic than in the lumbar region. Circularity factor does not provide any indications of scoliosis-related asymmetries. |
| Hurtado-Aviles et al. [18] | X ray images collected from a digital image repository. |
Coronal | Utilization of the software TraumaMeter (Mean bias error (MBE) = 1.8º, Standard deviation (SD) = 0.65º) depicts a lower intra- observer measurement error compared to the conventional manual Cobb angle (MBE = 2.31º, SD = 0.83º). The MBE value of the inter-group (expert and novice) distributions differs significantly when using TraumaMeter or the manual method. The use of the software leads to reduction in the difference in error between the novice and expert observers in a statistically significant way. |
| Glowka et al. [31] | The study consists of four steps which are: - 1) 3D scoliosis angle calculation of computed tomography (CT). 2) 3D scoliosis angle calculation of digitally reconstructed radiographs (DRRs). 3) 3D scoliosis angle calculations comparison of CT versus DRRs. 4) Reproducibility and reliability evaluation of the proposed method of X-rays (PA and lateral). |
Posterior- anterior (PA) and lateral |
The 3D-angle measurements obtained with DRRs and CT (p > 0.05) were not significant different. However, a significant difference was found between the 3D-scoliosis angle and the Cobb angle measurements performed based on the X-rays. 3D angle measurements had high reproducibility and reliability value. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





