Coronary heart disease (CHD) is one of the most important diseases threatening human life at present. About 700,000 people die of CHD in China every year, accounting for about a quarter of all death causes. In the late 1980s, the concept of acute coronary syndrome was put forward in pathological studies of ischemic heart disease, which is defined as a clinical syndrome based on the rupture of coronary atherosclerotic plaque, subsequent thrombosis, and eventually complete or incomplete coronary occlusion [
1,
2,
3]. St-segment elevation acute myocardial infarction is a type of acute myocardial infarction with typical ST-segment elevation electrocardiogram. St-segment elevation acute myocardial infarction has high mortality and many complications, and patients without timely treatment and nursing have a high risk of death in a short period of time [
4,
5,
6]. Percutaneous coronary intervention (PCI) is one of the effective methods for the treatment of ST-segment elevation acute myocardial infarction, mainly by directly dredging the affected vessels, improving the perfusion of myocardial blood flow, and then achieving the purpose of optimizing myocardial blood circulation [
7,
8]. It has been pointed out that percutaneous coronary intervention has a better vascular recanalization rate than thrombolytic therapy. However, percutaneous coronary interventional therapy is an invasive treatment method, and patients may have many complications during the treatment, such as vagal nerve reflex, reperfusion injury, coronary artery spasm, etc., which affect the therapeutic effect of patients [
9,
10,
11]. Therefore, good intraoperative cooperation and nursing are very important. Good intraoperative cooperation and nursing can help doctors to better concentrate during the operation, accelerate the operation efficiency and reduce the possible risks during the operation [
12,
13,
14]. This study investigated the effect of intraoperative coordination and nursing on interventional therapy for PATIENTS with ST-segment elevation myocardial infarction, providing reference for clinical practice.
1. Data and methods
1.1. General Information
A total of 60 patients with ST-segment elevation myocardial infarction treated in our hospital from January 2022 to January 2023 were selected as the research objects. According to different nursing methods, they were divided into routine group (n = 30) and systematic group (n = 30), routine group (n = 20 males and n = 10 females). The average age was (65.17±12.55) years. The lesion locations were left anterior descending branch in 10 cases, right coronary branch in 8 cases and left circumflex branch in 13 cases. The mean time from onset to percutaneous coronary intervention (PCI) was (5.32±2.85)h (1-10h). In system group, there were 22 males and 8 females. The average age was (66.50±9.07) years. The lesion locations were left anterior descending branch in 11 cases, right coronary branch in 6 cases and left circumflex branch in 14 cases. The mean time from onset to percutaneous coronary intervention (PCI) was (5.25±2.69)h (1-10h). The above data conform to the principle of balanced comparability (P > 0.05). See
Table 1.
1.2. Inclusion and exclusion criteria
Inclusion criteria: 1. It met the diagnostic criteria of clinical ST-segment elevation acute myocardial infarction; 2. 2. Coronary angiography was performed; 3. Persistent chest pain that cannot be relieved by nitrates; 4. Sign informed consent. Exclusion criteria :1. Patients with combined malignant tumor; 2. Patients with severe liver and kidney dysfunction; 3. Patients with poor compliance and unable to cooperate.
1.3. methods
Both groups were treated with anticoagulation before percutaneous coronary intervention and intravenous injection of ordinary heparin of 100~120IU/kg. Tirofiban was administered intravenously for 24-36 hours at 0.15μg/(kg·min). The patients were placed in supine position after entering the operating room. After anesthesia, the radial artery or femoral artery was punctured by Sedinger puncture method under digital subtraction angiography. In the conventional group, radial artery puncture was performed in 28 cases and femoral artery puncture in 3 cases. In system group, radial artery puncture was performed in 30 cases and femoral artery puncture in 1 case. Coronary artery stenosis 70% or greater implanted 6 f scabbard, conventional coronary angiography, determine after infarction, vascular, menstruation bellows in coronary angioplasty (PTCA), and appropriate stents, stents implanted 78, residual stenosis < 20%, any imaging showed TIMI the flow within the Ⅲ level, patient condition and hemodynamic stability, the operation is a success. Clopidogrel (75mg/d)+ aspirin (100mg/d) was given postoperative follow-up treatment.On the basis of above the system group add atropine sulfate injection 0.9% sodium chloride 4ml+Atropine sulfate 0.5mg intravenous injection drug batch number 2203305
1.4. Atropine injection combined with nursing intervention
The routine group received routine nursing, including preoperative disinfection, skin preparation, close observation of patients' vital signs, etc., and the occurrence of intraoperative complications were handled by doctors.
On the basis of routine nursing, systematic nursing cooperation was given in the system group. The details are as follows: ① Preoperative preparation: When receiving the notification of percutaneous coronary intervention (PCI), the personnel on duty should be in position as soon as possible. Understand the patient's basic condition and examination indicators, prepare first-aid drugs and conventional coronary angiography and PCI materials, and check whether the instrument is in standby state. The adverse events that are easy to happen during the operation should be prevented and dealt with in advance. After entering the operating room, the patient should do three checks and eight pairs to confirm the operation site and skin preparation. Communicate with the patient, guide the patient how to cooperate with the doctor, explain the possible situation during the operation, calm the patient's emotions. Assist the patient to take the supine position, give the patient oxygen inhalation and ecg monitoring, pay attention to avoid the defibrillation site when connecting the ECG monitoring electrode, so as not to affect the image collection and rescue as the principle. Do a good job of ecg and multifunctional monitoring, to ensure the patient's vein patency. ② Cooperation in interventional surgery: timely delivery of instruments according to the needs of intraoperative physicians to ensure smooth operation. Assist the doctor to complete the puncture. Double check with the doctor after unpacking the balloon stents. Perform all treatments accurately according to condition and doctor's advice. ③ Prevention of intraoperative complications: Arrhythmia: intraoperative possible malignant arrhythmia and thus endanger the patient lives, to closely observe the patient's breathing, heart rate, heart rate, blood pressure, blood oxygen saturation, once found abnormal situation will promptly report to the doctor, when necessary intravenous push note 0.5 ~ 1 mg of atropine or application of temporary pacemaker, immediately came to nurse electric defibrillation, care nurse is responsible for the rescue medication; Amiodarone hydrochloride should be given in the case of ventricular tachycardia. 2. Observation and nursing of precardiac pain: When the coronary artery stent is implanted, the balloon is filled, the coronary artery blood flow is temporarily interrupted, and vascular spasm is easy to occur. Psychological nursing of patients is strengthened, and patients are often asked whether there is chest pain, chest tightness, etc., and informed that this is a normal reaction. For patients with obvious intraoperative pain in the precardiac area filled with balloon, the patient should be asked about the nature of pain, given the relevant explanation of pain and psychological comfort, to eliminate the patient's fear and tension, and given morphine analgesia when necessary. 3. Acute coronary artery occlusion: when acute coronary artery occlusion occurs in timI 0-2 level of anterior coronary artery flow, immediate intravenous administration of antihypertensive drugs, positive inotropic drugs and coronary artery injection of tirofiban hydrochloride, and implantation of stents to cover the damaged intima for patients who cannot be relieved after medication. 4. Vagus reflex: The vagus reflex usually occurs in vascular puncture and postoperative sheath tube removal, and the general clinical manifestations are pallor, nausea and vomiting, dizziness, chest tightness, sweating, decreased blood pressure, slow heart rate, etc. If vomiting occurs, tilt the head to one side and remove foreign bodies in the mouth and nose to prevent suffocation caused by vomit. 1mg atropine was injected intravenously to speed up dripping. For those whose blood pressure could not be raised in time or dropped too much, symptomatic treatment such as hydroxyamine or dopamine was given.
1.5. Evaluation criteria of efficacy
Time of infarct opening and length of hospital stay: recorded by medical staff during operation. Incidence of adverse reactions during PCI: Possible adverse reactions during PCI include ventricular tachycardia, ventricular fibrillation, vagal hypotension and acute coronary artery occlusion. Death during interventional treatment: conditions for clinical declaration of death: ① Complete loss of consciousness of the patient; ② Complete respiratory and heartbeat arrest; ③ The blood pressure continued to be zero, and the above indexes could not be recovered after a period of rescue; ④ The patient has pupil dilation. Determination of treatment success: The criteria for successful treatment were no serious complications, TIMI ⅲ blood flow, stable patient condition and hemodynamics. The criteria of treatment failure were complications, blood flow did not reach TIMI ⅲ, patients' condition did not improve, and hemodynamics did not reach stability. Improvement of heart function: The standard of good improvement of heart function was the heart failure classification of ⅰ - ⅱ set by the New York Heart Association one week after surgery, and the ejection fraction of heart color ultrasound was more than 50%. The criteria for poor improvement in cardiac function were that the patients did not reach the heart failure classification ⅰ - ⅱ set by the New York Heart Association one week after surgery, and the ejection fraction of the heart showed by color ultrasound was less than 50%.
1.6. Statistical methods
SPSS20.0 was used for data analysis software, measurement data were expressed as (± S), and independent sample T test was used. The counting data were expressed as the number of cases (rate) and X² test was used. The comparison with (P < 0.05) was statistically significant. GraphPad Prism 8 was used as the mapping software.
2. Results
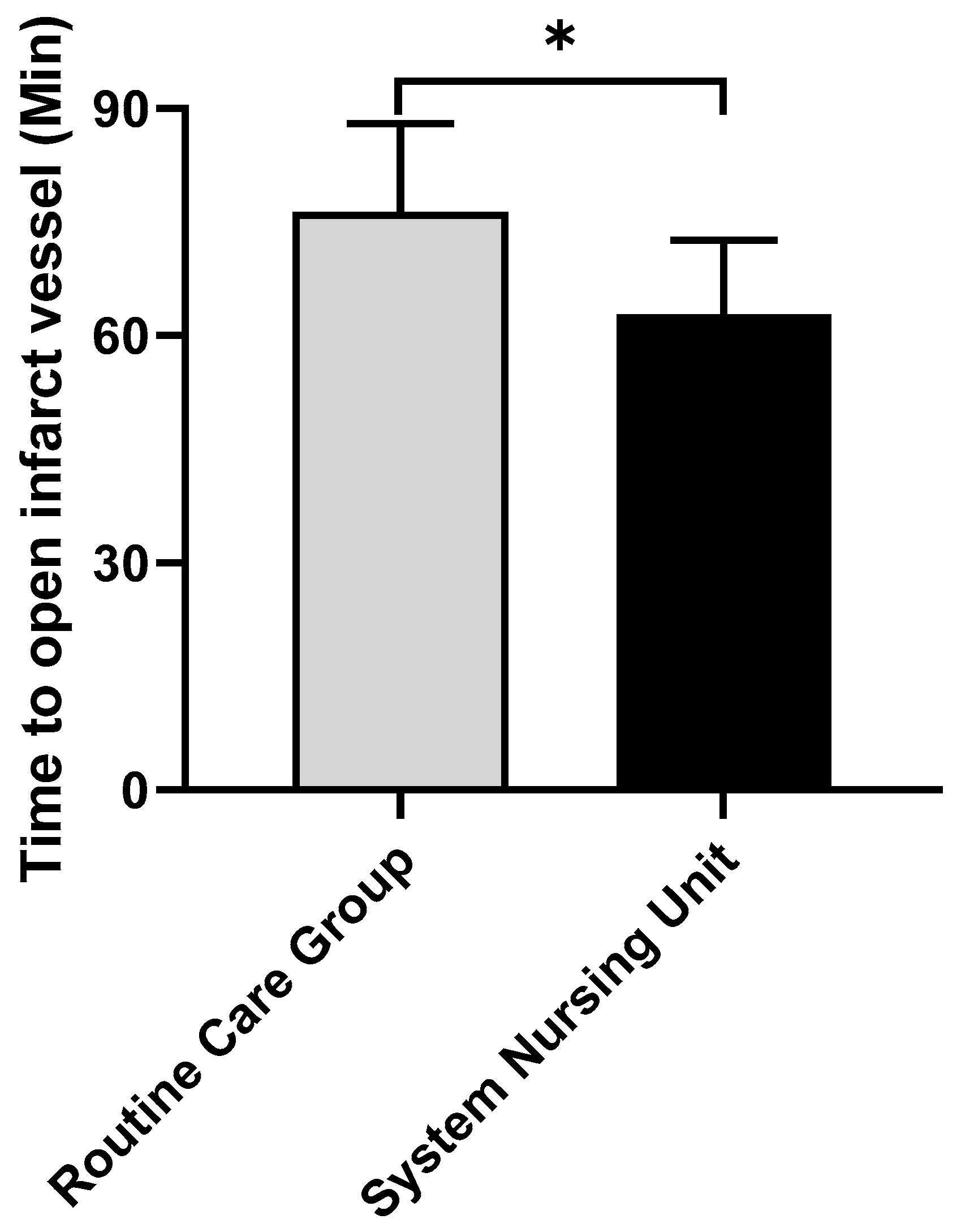
2.1. Comparison of the opening time of infarcted vessels
The opening time of infarct vessel in conventional group was (76.36±11.62) min. The time of infarct vessel opening in the system group was (62.83±9.77) min, which was significantly better than that in the conventional group (P < 0.05), as shown in
Figure 1. (* represents the comparison of time to open infarct vessels between the conventional group and the system group t=4.962, P < 0.001)
2.2. Comparison of the incidence of total adverse reactions during interventional treatment
In the conventional group, there were 1 cases of ventricular fibrillation, 3 cases of ventricular tachycardia, 2 cases of acute coronary artery occlusion, 4 cases of hypotension, and the total rate of adverse reactions was 10 cases (33%). In the systemic group, there were 0 cases of ventricular fibrillation, 1 case of ventricular tachycardia, 1 case of acute coronary artery occlusion, 1 case of hypotension, and 3 cases (10%) of total adverse reactions. The total adr rate in system group was significantly lower than that in conventional group (P < 0.05), as shown in
Table 2.
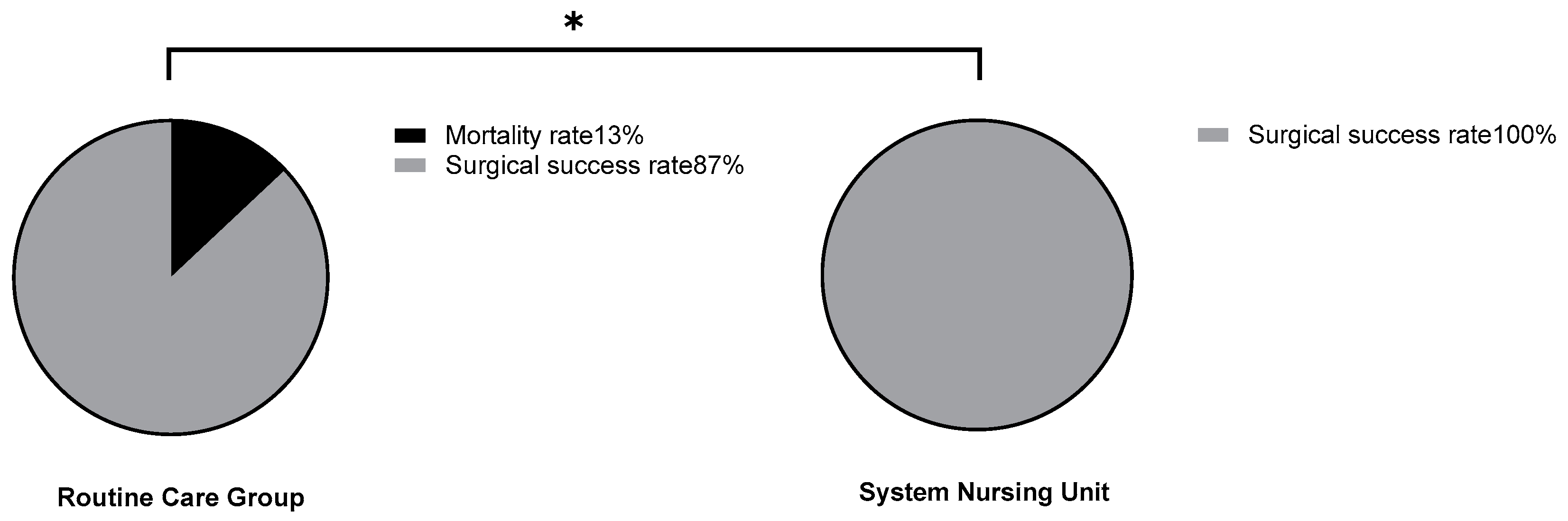
2.3. Comparison of mortality during interventional treatment
In the conventional group, 4 patients died during interventional treatment, with a mortality rate of 13%. In the system group, 0 patients died during interventional treatment, and the mortality rate was 0%. The mortality of routine group was significantly higher than that of system group (P < 0.05), as shown in
Figure 2. (* represents comparison of mortality between the conventional and system groups x²=4.276, P=0.039)
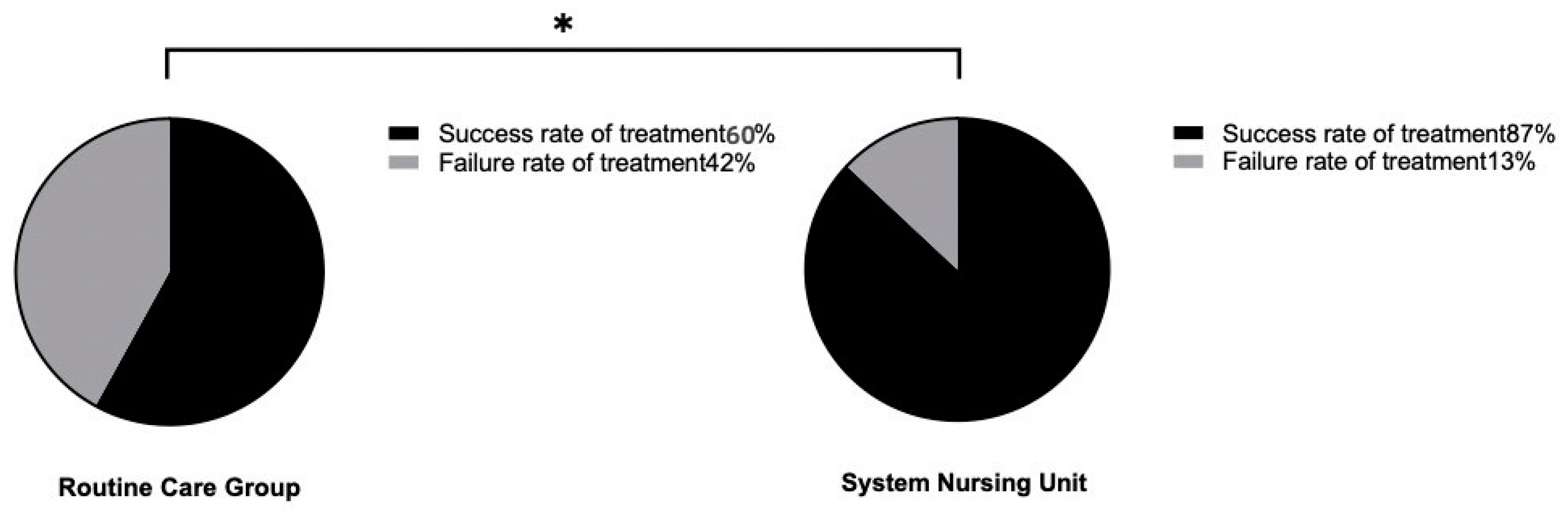
2.4. Comparison of treatment success rate
In the conventional group, 18 cases were successfully treated, and the success rate was 60%. In the systemic group, 26 cases were successfully treated, and the success rate was 87%. The success rate of the system group was significantly higher than that of the conventional group (P < 0.05), as shown in
Figure 3. (* represents the comparison of treatment success rate between the conventional group and the system group x²=5.455, P=0.02)
2.5. Comparison of improvement of cardiac function and length of hospitalization
In the conventional group, 17 patients had good cardiac function improvement, 10 patients had poor cardiac function improvement, and the hospital stay was (7.33±1.21) d. In system group, 25 patients had good cardiac function improvement, 5 patients had poor cardiac function improvement, and the hospital stay was (6.43±1.30) d. The number of patients with improved cardiac function and length of hospital stay in the system group were significantly better than those in the conventional group (P < 0.05), as shown in
Table 3.
3. Discuss
St-segment elevation acute myocardial infarction is a type of acute myocardial infarction with typical ST-segment elevation electrocardiogram. St-segment elevation acute myocardial infarction has high mortality and many complications. Once patients do not receive timely treatment and nursing, the risk of death in a short period of time is high. Percutaneous coronary intervention (PCI) is one of the effective methods for the treatment of ST-segment elevation acute myocardial infarction. Percutaneous coronary intervention (PCI) can open infarct-related arteries as early as possible, fully and continuously, and effectively inhibit the structural and morphological changes in infarcted and non-infarcted areas. With the characteristics of small trauma and quick postoperative recovery, it is currently recognized as an effective treatment to improve the prognosis of acute myocardial infarction. Some studies have shown that percutaneous coronary intervention has a vascular recervation rate as high as 91%. More and more patients are receiving percutaneous coronary intervention, but for st-segment elevation myocardial infarction patients, whether percutaneous coronary intervention can benefit patients and the extent of benefit is related to the patient's condition on the one hand, and the medical level on the other hand [
15]. The level of medical treatment includes the timing of percutaneous coronary intervention, the experience of doctors and the degree of cooperation of key nursing staff. Nursing cooperation during PCI is the key to successful treatment [
16,
17]. In this study, we compared the time of opening infarct vessels and length of hospital stay in the two groups of patients under different nursing interventions. The results showed that the time of opening infarct vessels and length of hospital stay in the system group were significantly better than those in the conventional group, indicating that intraoperative cooperation and nursing can effectively accelerate the process of surgery and postoperative recovery of patients. The risk of percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction is high, unpredictable emergencies may occur at any time, and intraoperative monitoring is complex and challenging. Medical staff should strengthen the observation of vital signs, prevent the occurrence of complications, timely detect the changes in the condition and give rapid treatment to avoid adverse consequences. In this study, we compared the incidence of total adverse reactions and mortality during interventional treatment between the two groups of patients under different nursing interventions. The results showed that the total adverse reactions rate in the system group was significantly lower than that in the conventional group, and the mortality rate in the system group was significantly lower than that in the conventional group. This indicates that intraoperative cooperation and nursing can effectively reduce the occurrence of adverse reactions during the operation, thus reducing the death situation during the operation, and thus ensuring the life safety of patients. Accepts st-elevation myocardial infarction patients in medical staff to quickly reach the designated position, accurate quickly implement PCI treatment, a study said, at the same time, improve medical and health resources efficiency in good percutaneous coronary artery intervention treatment team, the high quality of intraoperative care coordinates to improve treatment success of percutaneous coronary intervention has a positive role in [
18,
19,
20,
21]. In this study, we compared the treatment success rate of the two groups of patients under different nursing interventions. The results showed that the treatment success rate of the system group was significantly higher than that of the conventional group, indicating that a good interventional treatment team and high-quality intraoperative nursing cooperation can effectively improve the success rate of percutaneous coronary intervention. The improvement of cardiac function is an important indicator of percutaneous coronary intervention. With the transformation of modern medical model and the improvement of people's health awareness, the purpose of treatment is not only to improve the survival rate and prolong the survival time of patients, but also to improve their quality of life. In this study, we compared the improvement of cardiac function between the two groups of patients under different nursing interventions. The number of patients with good cardiac function improvement in the system group was significantly better than that in the conventional group, indicating that intraoperative cooperation and nursing can effectively improve the postoperative cardiac function of patients and improve the quality of life of patients.
In conclusion, rigorous intraoperative cooperation and nursing are important guarantees for patients with ST-segment elevation myocardial infarction, which can effectively reduce the occurrence of adverse reactions during interventional treatment, improve the success rate of treatment, improve the cardiac function of patients, and reduce the death of patients during interventional treatment.
Funding
The authors received no financial support for the research authorship or publication of this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article
References
- Frank, M., C. Sanders, and B.P. Berry, Evaluation and management of ST-segment elevation myocardial infarction in the emergency department. Emerg Med Pract 2021, 23(1), 1–28.
- Garratt, K.N., ST-Segment-Elevation Myocardial Infarction Care in America: Celebration and Anxiety. J Am Heart Assoc 2020, 9(11), e016832. [CrossRef] [PubMed]
- Tam, C.F., et al., Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020, 13(4), e006631. [CrossRef] [PubMed]
- Ciofani, J.L., et al., No-reflow phenomenon in ST-segment elevation myocardial infarction: still the Achilles' heel of the interventionalist. Future Cardiol 2021, 17(2), 383–397. [CrossRef]
- Daniels, M.J., et al., Reperfusion of ST-Segment-Elevation Myocardial Infarction in the COVID-19 Era: Business as Usual? Circulation 2020, 141(24), 1948–1950. [CrossRef]
- Frampton, J., et al., Modern Management of ST-Segment Elevation Myocardial Infarction. Curr Probl Cardiol 2020, 45(3), 100393. [CrossRef]
- Ali, Z., et al., Optical coherence tomography-guided coronary stent implantation compared to angiography: a multicentre randomised trial in PCI - design and rationale of ILUMIEN IV: OPTIMAL PCI. EuroIntervention 2021, 16(13), 1092–1099. [CrossRef]
- Atiyeh, B.S., O. Abou Ghanem, and F. Chahine, Microneedling: Percutaneous Collagen Induction (PCI) Therapy for Management of Scars and Photoaged Skin-Scientific Evidence and Review of the Literature. Aesthetic Plast Surg 2021, 45(1), 296–308. [CrossRef]
- Chawla, R., W. Ahamad, and V. Sharma, Techniques to Overcome Difficulty in Device Deliverability to Lesion in Complex PCI. Curr Cardiol Rev 2020, 16(2), 117–124. [CrossRef]
- Ekou, A., et al., Primary PCI in the management of STEMI in sub-Saharan Africa: insights from Abidjan Heart Institute catheterisation laboratory. Cardiovasc J Afr 2020, 31(4), 201–204.
- Feistritzer, H.J. , et al., Multivessel versus culprit-only PCI in STEMI patients with multivessel disease: meta-analysis of randomized controlled trials. Clin Res Cardiol 2020, 109(11), 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Barellini, L., et al., Intraoperative Ultrasound and Oncoplastic Combined Approach: An Additional Tool for the Oncoplastic Surgeon to Obtain Tumor-Free Margins in Breast Conservative Surgery-A 2-Year Single-Center Prospective Study. Clin Breast Cancer 2020, 20(3), e290–e294.
- Blackwood, S.L., et al., Emergency intraoperative vascular surgery consultations at a tertiary academic center. J Vasc Surg 2020, 71(3), 967–978. [CrossRef] [PubMed]
- Fonseca, P., et al., A Bibliometric Analysis of Intraoperative Neuromonitoring in Spine Surgery. World Neurosurg 2021, 154, 3–12. [CrossRef] [PubMed]
- Yerasi, C., et al., Treatment of ST-Segment Elevation Myocardial Infarction During COVID-19 Pandemic. Cardiovasc Revasc Med 2020, 21(8), 1024–1029. [CrossRef] [PubMed]
- Guo, Z., et al., Post-PCI acute heart failure is an independent predictor of long-term mortality in patients with chronic kidney disease. Int J Cardiol 2020, 320, 119–123. [CrossRef]
- Rai, D., et al., Meta-Analysis and Trial Sequential Analysis of Randomized Controlled Trials for Multivessel PCI Versus Culprit Artery Only PCI in STEMI Without Cardiogenic Shock. Curr Probl Cardiol 2021, 46(3), 100646. [CrossRef]
- Privalov, M., et al., First experiences with intraoperative CT in navigated sacroiliac (SI) instrumentation: An analysis of 25 cases and comparison with conventional intraoperative 2D and 3D imaging. Injury 2021, 52(10), 2730–2737. [CrossRef]
- Rigolo, L., et al., Intraoperative Use of Functional MRI for Surgical Decision Making after Limited or Infeasible Electrocortical Stimulation Mapping. J Neuroimaging 2020, 30(2), 184–191. [CrossRef]
- Tsirikos, A.I., et al., Multimodal Intraoperative Spinal Cord Monitoring during Spinal Deformity Surgery: Efficacy, Diagnostic Characteristics, and Algorithm Development. Med Princ Pract 2020, 29(1), 6–17. [CrossRef]
- Zarowski, A., et al., Intraoperative recordings of electromyogenic responses from the human stapedius muscle. Hear Res 2021, 408, 108290. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).