1. Introduction
Nosocomial infections are a serious problem in neonatal intensive care units - they are one of the main causes of morbidity and mortality among neonates. They develop after the 72nd hour of admission and occur in relation to the patient's medical care [
1].
The degree of clinical manifestation can be highly variable, depending on the virulence of pathogens and the host defense mechanisms. The initial symptoms are often non-specific and difficult to differentiate from other non-infectious conditions. They can be predictors of late onset neonatal sepsis (LOS) and, if not recognized on time, can lead to severe complications such as shock and death and, in the long term, to growth retardation, neurodevelopmental impairment and bronchopulmonary dysplasia.
Several clinical and haematological markers are usually considered to diagnose systemic infection, but the correct combination is not clearly defined. In routine practice, total white blood cell count, elevated immature-to-total polymorphonuclear cell ratio, platelet count, acute phase protein (C-reactive protein) are tested, and the gold standard is a positive microbiological culture of biological samples. However, these markers are not sufficiently predictive in the initial phase of systemic neonatal infection and are defined as "late" indicators. Therefore, there is a delay in the diagnosis of affected neonates, which may lead to late initiation of treatment and the above mentioned complications. If antibiotics are started upon suspicion of sepsis without evidence, the disadvantage may be prolonged and unnecessary therapy, selection of resistant microorganisms and increased hospital costs [
2].
2. Materials and Methods
The aim of this study was to determine the potential of early inflammatory markers-procalcitonin (PCT), interleukin 6 (IL-6), interleukin 8 (IL-8) and endocan (ESM-1) - to diagnose late onset sepsis in neonates. Their serum concentrations were assessed and validation criteria for diagnostic tests - sensitivity, specificity, accuracy, positive and negative predictive value- were analyzed. Their diagnostic value was compared with that of C-reactive protein (CRP), immature-to-total polymorphonuclear cell ratio (I:T index), platelet count (PLT) and white blood cells count (WBC).
A prospective clinical-epidemiological study (January, 2022 - January, 2023) was conducted in the Clinic of Neonatology of the University Hospital "Dr. Georgi Stransky", Pleven. The study included preterm and term neonates, with a stay in the neonatal intensive care unit (NICU) exceeding 72 hours. Exclusion criteria were presence of severe congenital anomalies and early postoperative period. The work group consisted of patients with new onset symptoms, suspicious for LOS. We accepted as inclusion criteria the presence of at least three clinical and laboratory indicators and at least one risk factor suggestive of acquired in NICU neonatal infection. (
Table 1).
Later the case group was divided into two subgroups:
Group 1 – symptomatic and infected patients (patients with proven LOS). Diagnoses of clinical sepsis (with negative microbiological result) and septicaemia (with positive microbiological result) were accepted. The evaluation was complex, considering the follow-up haematological investigations in the next 5 days, such as elevated CRP, leukocytosis / leukopenia; results of microbiological samples; evolution of the clinical status, treatment and outcome.
Group 2 – symptomatic but uninfected patients (with no evidence of sepsis during the next 5 days of stay - control paraclinical tests were within reference limits and microbiological samples are negative). Other non-infectious condition or disease could be proven.
In order to analyse the reference ranges of the indicators, a control Group 0 of asymptomatic newborns in stable general condition with hospital stay > 72 h was formed. The taken samples were part of regular follow-up blood tests.
On the day of suspicion of infection, 1.5 - 2 ml of blood was collected from a peripheral vein, the separated serum was stored at -80 °C until analysis.
Concentrations of IL-6, IL-8, PCT, ESM-1 were measured in the laboratory of Medical University, Pleven. Commercial kits based on sandwich ELISA (enzyme-linked immunosorbent assay) were used, respectively: Human IL-6 ELISA Kit, Invitrogen Thermo Fisher Scientific Inc; Human IL-8 ELISA Kit, Invitrogen Thermo Fisher Scientific Inc; Human Procalcitonin ELISA, BioVendor LM; Human Endothelial Cell-Specific Molecule 1 ELISA Kit, CUSABIO TECHNOLOGY LLC. The reaction was performed according to the manufacturer's instructions.
Data were entered and processed with the statistical packages IBM SPSS Statistics 25.0. and Office 2021 Excel. A significance level rejecting the null hypothesis was accepted as p<0.05.The following statistical methods are applied: descriptive and graphical analysis, non-parametric Shapiro-Wilk test, Stewart’s T-criterion, non-parametric Mann-Whitney test, ROC curve analysis and multiple binary logistic regression analysis
3. Results
A total of sixty newborns were enrolled, 42 (70%) boys and 18 (30%) girls. The mean gestational age (g.a.) of the study population was 29.75 ± 3.61 gestational weeks (g.w.), ranging between 25 and 40 g.w.
The distribution of study population by groups is presented in
Figure 1.
Microbiological samples were positive only in 66% of the infected patients (14/21). The most common pathogen, responsible for LOS was Gram-negative Klebsiella pneumoniae (7/14, 50%), followed by Gram-positive Staphylococci sp. (3/14, 21%). Less common pathogens were Escherichia coli, Serratia sp., Enterobacter sp.
The comparative analysis of the groups, according to the values of markers PCT, ESM-1, IL-6 and IL-8, and the indicators CRP, I:T index, WBC and PLT revealed that the three groups differed significantly in four of the indicators included in the table, namely PCT, IL-6, I:T index and PLT (
Table 2).
In septic neonates compared to non-septic from Group 0 and 2 the mean serum concentration (ng/mL) of procalcitonin was significantly higher (2.27±3.22 vs. 0.43±0.57, p=0.004 and 0.44±0.58, p=0.005 respectively). Similar correlation was found between the mean IL-6 serum concentration (30.72±53.48) and the other two groups, whose arithmetic means were not different from each other (29.82±104.02 and 5.07±5.39) (
Table 2).
Group 1 had a significantly higher mean I:T index than Group 2 (0.35±0.16 vs. 0.24±0.11, p=0.024), but not higher than controls (0.29±0.21), whose means were not statistically different from those of the other two groups.
For the markers ESM-1, IL-8, CRP and WBC the difference between the main groups was statistically negligible (p>0.005).
The study groups differed significantly in the platelet count. In group 1, they had a significantly lower mean value than that of the controls (265.57±167.86 vs. 384±136.13, p=0.013), but not than that of the symptomatic uninfected patients (321.90±126), which was not statistically different from those of the other two groups.
At the same time, we analyzed the pathological values of WBC and PLT.
Table 3 shows that Group 1 is significantly different from the other two groups in both parameters, which have statistically higher relative proportions in this group. The difference between the percentages of pathological values of platelets and leukocytes in Group 0 and Group 2 is insignificant.
According to the results in
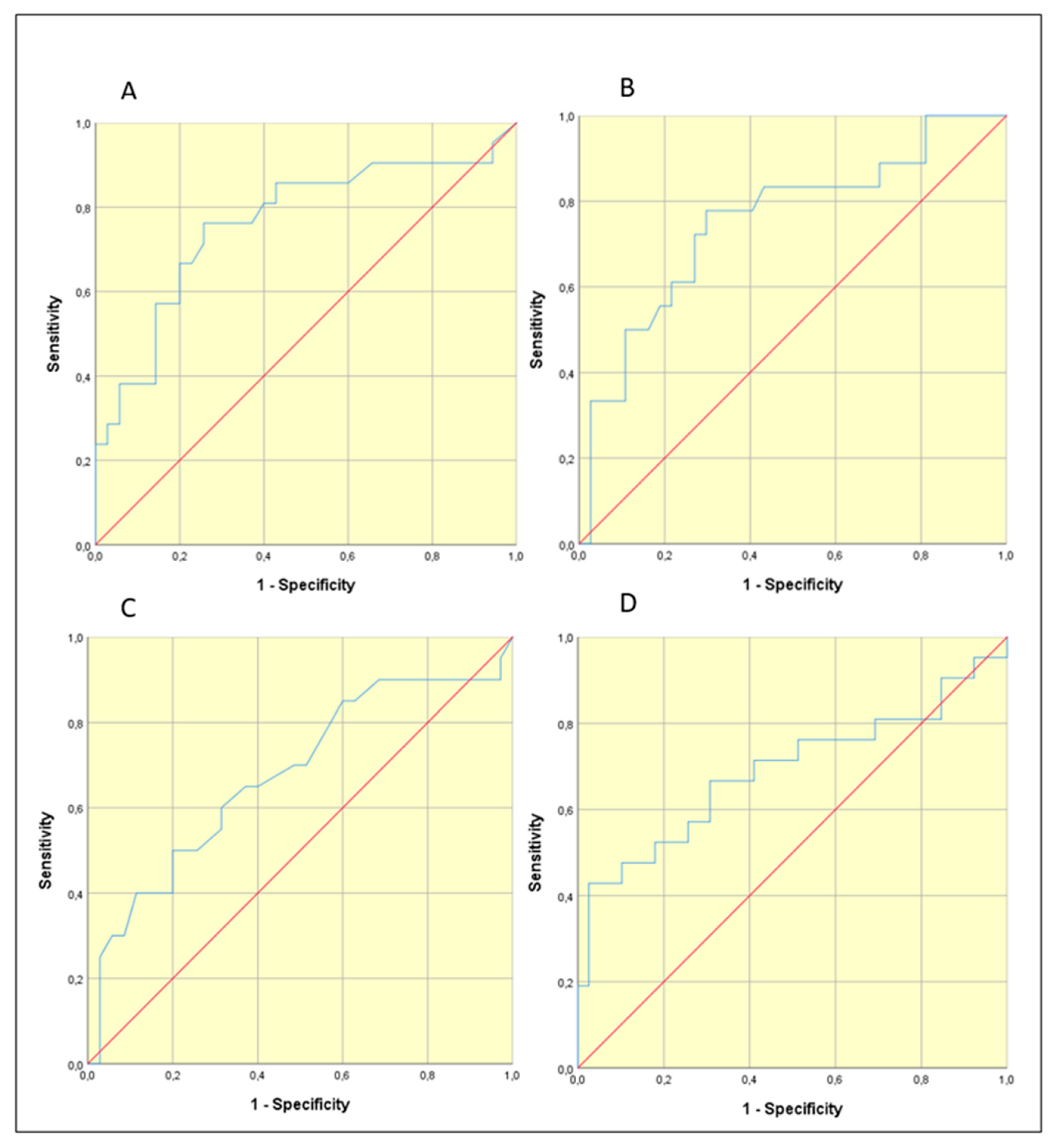
Table 2, we could pool the controls with Group 2 (symptomatic uninfected) when searching for threshold values. To determine whether statistically significant threshold values existed for the markers PCT, ESM-1, IL-6, IL-8, and the indices CRP, I:T index and PLT, ROC curve analysis was applied, distinguishing Group 1 from Groups 0 and 2. From
Figure 2 it is clear that PCT, IL-6, I:T index and PLT have significant threshold values. Their selection was performed according to Youden index = [maximum (sensitivity + specificity-1)]. In addition, the abnormal values of PCT (≥0.5) and I:T index (≥0.25) were also evaluated, as was the combination of the four variables PCT ≥ 0,46 + IL-6 ≥ 4,97 + I:T index ≥ 0,335 + Plt ≤161,5. Multiple binary logistic regression analysis was applied to the combination. The area under the curve is AUC=0.880, p<0.001.
With the established threshold values, an analysis of diagnostic test validation criteria was performed. The results were included in
Table 4.
4. Discussion
Late onset neonatal sepsis is defined as an infection occurring after 72 hours after birth. According to the literature, the incidence ranges from 0.6% to 14% of all neonates admitted to hospital [
3]. Extremely preterm infants are at the highest risk, with a cited incidence of about 34%. Risk factors for LOS include prematurity, prolonged exposure to invasive procedures, delayed enteral feeding, need for surgical intervention, underlying respiratory and cardiac disease.
The three main challenges in the diagnosis of neonatal sepsis are: the myriad of clinical symptoms that can mimic sepsis; false-negative bacterial cultures in cases of so-called culture-negative sepsis; and the need for empiric treatment for a minimum of 24 to 48 hours while cultures are incubated [
4].
The complete blood count with differential count is the most commonly tested laboratory indicator of infection; it is a cheap and easy to perform method. In recourse-limited areas, this may be the only diagnostic tool for neonatal sepsis. This inspired a study in Ethiopia, showing that the mean of total white cell count and platelet count is lower in septic patients. Leucopenia, defined in the study as WBC less than or equal to 12,500/mm3, has a sensitivity of 35.2% and a specificity of 92% in LOS and seems to be more valuable in early-onset sepsis. The sensitivity and specificity of thrombocytopenia (< 145,000/mm3) were 54.1 and 70.4%, respectively [
5]. Low sensitivity and good specificity are often found, considering this indicator as unreliable [
6].
The combination of leucopenia and high I:T ratio (>0.2) shows similar results. Although, they show increased odds of infection (highest odds ratios: 5.38 and 7.97, respectively). In a study by Hornik et al, they have high specificity and negative predictive value and low sensitivity [
7]. They seem to be more useful in eliminating healthy newborns than identifying infected ones. Excellent 100% negative predictive value is reached in a study by Murphy et al with two normal I:T ratio and sterile blood culture. (4) According to our results, patients with LOS have remarkably higher incidence of leucopenia/leukocytosis and thrombocytopenia. Unexpectedly, we found a very good performance of I:T index with specificity of 97% and positive predictive value 80% (for a threshold value ≥ 0.25), which is generally considered a "late" marker of inflammation. The best specificity (97%) and positive predictive value (90%) shows the platelet count parameter.
An acute phase protein that is very often interpreted with complete blood count is C-reactive protein. Usually, it is not positive in the early stage of infection and as we suggested, it did not reach statistically significant values in our study. The peak of its level is after 24 hours, meaning the sensitivity for neonatal sepsis is lowest in the early stage of infection. It rises in serial testing at the 24-48th hour after the onset of symptoms. The specificity and positive predictive value range from 93 to 100%, so it is referred to as a "specific" but "late" marker for neonatal infection [
8].
In contemporary times, there has been considerable scientific exploration of diverse serum inflammatory biomarkers, with the primary objective of unveiling a remarkably sensitive "early" examination method to evaluate instances of inflammation and infection. These biomarkers encompass procalcitonin, interleukin 6, interleukin 8, and endocan (PCT, IL-6, IL-8, endocan / ESM-1). It is hypothesized that their concentrations exhibit augmentation within the initial hours of an inflammatory response. Demonstrating substantial sensitivity and diagnostic significance, these biomarkers hold potential practical utility. Nonetheless, the outcomes of conducted studies frequently lack conclusive evidence, and the establishment of a uniform methodology remains an unresolved endeavor [
9].
Recently, PCT has been more widely used in the diagnosis of neonatal infections. Procalcitonin is a peptide, produced by monocytes and hepatocytes in response to systemic inflammation and, according to some studies, appears to be more sensitive than CRP in bacterial infections [
10]. Nonspecific, i.e. infection-independent, induction of PCT synthesis can occur after major surgery, multiple trauma and during the early neonatal period, which is why we excluded these newborns from our study [
11]. In neonatal sepsis, its concentrations rise after 4 hours from the proinflammatory effect of bacterial endotoxins, and reach their peak after 6-8 hours, thus rising earlier than CRP [
12]. Its half-life is 25-30 hours and concentrations are not affected by gestational age. Its elevation is independent of calcitonin and is associated with neurotransmission, immunomodulation, vascular control during infection and in the systemic inflammatory response syndrome (SIRS) [
13]. Procalcitonin is usually referred as a highly specific marker for the diagnosis and monitoring of bacterial infections and sepsis, also referring to the severity of the infectious process. In addition, PCT is an indicator of the therapeutic success- a decrease in its plasma levels 24 hours after treatment initiation is connected to favorable therapeutic response [
11]. Its diagnostic profile for systemic bacterial infections and necrotizing enterocolitis has shown to be superior to all other acute phase proteins, with a sensitivity and specificity of 87 to 100%. Bustos et al. performed a prospective observational study of a cohort of 53 neonates with clinically suspected late onset neonatal sepsis. Procalcitonin showed a sensitivity of 88%, a specificity of 71.4%, and a negative predictive value of 87% [
14].
In Bulgaria, there are only few neonatal centers that routinely test PCT levels. Semi-quantitative immunochromatographic study of procalcitonin in neonates with generalized bacterial infection was carried out in 2001 by Georgieva et al. [
15]. Eighty-seven neonates were studied - 30 with early and late sepsis, 8 with late sepsis and 49 controls. A sensitivity of 63% and specificity of 100% were demonstrated for values above 2 ng/mL.
In our study, at a threshold value > 0.46 ng/mL, PCT showed a sensitivity of 76%, a specificity of 74%, and a negative predictive value of 84%, which are close to those cited in the literature. This proves the necessity to be implemented in the basic septic screening.
Another group of biomarkers that have been evaluated for the diagnosis of neonatal sepsis are the interleukins. Interleukin 6 is an important cytokine of the host's early immune response. A review of studies, conducted from 1990 to 2020 shows that IL-6 is the biomarker that has been studied more than any other interleukin in newborns [
16]. Different threshold values have been proposed, and as this value increases, specificity increases at the expense of sensitivity. In most studies, the results are extremely promising. The mean (30.72) and threshold (≥27.5) steady-state values found in our study are similar to those of Adib et al. [
17], who reported sensitivity, specificity, positive and negative predictive values for IL-6 with a threshold value of 30 pg/mL 78%, 95%, 100% and 87% respectively for the diagnosis of neonatal sepsis. For PCT and IL-6, patients in Group 1 have a significantly higher mean compared to the other two groups, whose means are not statistically different from each other. The obtained results demonstrate comparable sensitivity and negative predictive value, albeit at the cost of reduced specificity and negative predictive value. Among the various novel markers investigated in this study, interleukin-6 (IL-6) exhibited the most favorable sensitivity (78%) and negative predictive value (84%).
In the early stage of neonatal bacterial infection, IL-8 levels are also increased. In a study by Boskabadi et al., they showed that serum IL-8 concentration in infants with confirmed sepsis was significantly higher than in healthy infants before blood culture positivity. Also, the serum level of this marker in deceased infants with sepsis was much higher than that of surviving infants. The sensitivity, specificity, positive predictive value and negative predictive value for IL-8 were 95%, 10%, 97% and 10% respectively and for CRP was 83%, 86%, 83% and 69% respectively. The cutoff value of IL8 was above 60 pg/mL [
17,
18].
In the group of symptomatic infected infants the mean IL-8 value was 141.98 pg/mL. The serum concentrations of the marker, measured by the described methodology in our study varied within a very wide range, both in the demonstrably ill and in the other two groups of uninfected children. The comparative analysis between the three main groups on the IL-8 value proved that the difference was statistically insignificant.
We also find unsatisfactory results for endocan. This is a new biomarker, being studied in terms of late neonatal sepsis. The mean value in symptomatic infected patients was 163.52 ng/mL. The level in all patients was relatively low and without large variations, compared to results from other authors. The difference between the three groups was not statistically significant and no significant threshold value could be found. It could not be interpreted in terms of diagnostic marker validation criteria.
Our results for endocan are not consistent with those found in the literature, but reports to date are scarce. It is a proteoglycan, secreted by endothelial cells and is suggested to play a role in the pathogenesis of sepsis. An increase in its expression leads to endothelial activation and neovascularization, which are prominent pathophysiological changes associated with inflammation [
19].
In a study by Buyuktiryaki et al., CRP, IL-6 and endocan levels were measured in a total of 102 preterm infants. Overall, while all three biomarkers showed "good performance" in differentiating between sepsis and healthy controls, area under the curve (AUC) values in the groups with proven sepsis showed a more significant value for endocan. Further, serial measurements showed that there was no significant difference in CRP and IL-6 levels between the proven and presumed sepsis groups, while endocan levels were significantly higher [
20]. Overall, the endocan was found to show a specificity of 94% and a sensitivity of 94.2% [
21].
So far, the best combination of markers for predicting late-onset neonatal sepsis with highest level of validation criteria has not been found. Well-known to many clinicians is the neonatal calculator for early-onset sepsis (Kaiser Neonatal Sepsis Calculator), combining maternal risk factors and infant’s clinical presentation [
22]. Similar diagnostic tool for LOS has not yet been approved. Some proposals have been made, such as a Sepsis Prediction Score by Sofouli et al. This is a retrospective study in Greece on 120 newborns with suspected sepsis, combining eight clinical and laboratory parameters such as temperature instability, feeding volume decrease, platelet count < 150 000/mm3, changes in blood glucose, CRP > 1 mg/dL, circulatory and respiratory deterioration. The scoring model was then validated prospectively on 145 infants [
23]. The results were again inconclusive as a lot of septic infants reached very low scores.
We conclude that some interesting findings from our analysis can contribute to the development of a more precise LOS scoring system. The combination of PCT + IL-6 + I:T index demonstrated high precision (78%); the same was the result for platelets and the four parameter combination PCT + IL-6 + I:T + PLT. Best sensitivity (94%) and negative predictive value (95%) we reach in binary logistic model with 4 variables. These conclusions can be useful in future research on a bigger cohort.
5. Conclusions
The introduction into routine practice of indicators such as PCT and IL-6 may provide an opportunity for timely diagnosis, optimization of the therapeutic approach and reduction of complications from nosocomial infections. The I:T index and platelet count can be relied upon, especially when interpreted together with PCT and IL-6. According to our results, ESM-1 and IL-8 are not reliable markers of late neonatal sepsis. More studies are needed on a larger cohort of newborns as well as on other early biomarkers of inflammation.
Supplementary Materials
The following supporting information can be downloaded at:
Preprints.org.
Author Contributions
Conceptualization, P.G. and V.A.; methodology, A.B.; software, Z.Y.; validation, P.G. and V.A.; formal analysis, Z.Y.; investigation, P.G.; resources, P.G..; data curation, A.B, Z.Y.; writing—original draft preparation, P.G. ; writing—review and editing, V.A.; visualization, A.B.; supervision, V.A.; project administration, V.A.; funding acquisition, P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Medical university Pleven, grant number D3/2023.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Medical university Pleven.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing not applicable. No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- el Manouni el Hassani, S., et al., Risk Factors for Late-Onset Sepsis in Preterm Infants: A Multicenter Case-Control Study. Neonatology, 2019. 116(1): p. 42-51.
- Wynn, J.L., Defining neonatal sepsis. Curr Opin Pediatr, 2016. 28(2): p. 135-40.
- Dong, Y. and C.P. Speer, Late-onset neonatal sepsis:Recent developments. Archives of Disease in Childhood: Fetal and Neonatal Edition, 2015. 100(3): p. F257-F263.
- Cantey, J.B. and J.H. Lee, Biomarkers for the Diagnosis of Neonatal Sepsis. 2021, W.B. Saunders. p. 215-227.
- Worku, M., et al., Role of complete blood cell count parameters in the diagnosis of neonatal sepsis. BMC Pediatrics, 2022. 22(1): p. 1-9.
- Sharma, D., et al., Biomarkers for diagnosis of neonatal sepsis : a literature review. 2017. 7058(November).
- Hornik, C.P., et al., Use of the complete blood cell count in late-onset neonatal sepsis. Pediatric Infectious Disease Journal, 2012. 31(8): p. 803-807.
- Shah, B.A. and J.F. Padbury, Neonatal sepsis an old problem with new insights. Virulence, 2014. 5(1): p. 163-171.
- Gude, S.S., et al., Biomarkers of neonatal sepsis: From being mere numbers to becoming guiding diagnostics. Cureus, 2022. 14(3).
- Eschborn, S. and J.-H. Weitkamp, Procalcitonin versus C-reactive protein: review of kinetics and performance for diagnosis of neonatal sepsis. Journal of Perinatology, 2019. 39(7): p. 893-903.
- Atanasova V, R.R.H.A., Procalcitonin: an innovative marker for bacterial infections. Biochemical, immunological and clinical aspects (chapter 1)tle. Clinical application of immunological investigations" (International immunological journal for clinicians. 3(1):153-1.
- Ng, P.C. and H.S. Lam, Biomarkers for Late-Onset Neonatal Sepsis: Cytokines and Beyond. Clinics in Perinatology, 2010. 37(3): p. 599-610.
- Mitchell, E., Serum calcitonin gene-related peptide concentrations in the horse and their relationship to the Systemic Inflammatory response. 2006, Virginia Tech.
- Raúl Bustos, B. and C. Heriberto Araneda, Procalcitonina para el diagnóstico de la sepsis tardía en recién nacidos de muy bajo peso de nacimiento. Revista Chilena de Infectologia, 2012. 29(5): p. 511-516.
- Georgieva R, H.E., Dyankova D Diagnostic value of semi-quantitive testing of serum procalcitonin in newborns with generalized bacterial infections. . Pediatrics, 2001(4): p. 28-31.
- Eichberger, J. and B. Resch, Reliability of interleukin-6 alone and in combination for diagnosis of early onset neonatal sepsis: systematic review. Frontiers in Pediatrics, 2022. 10: p. 840778.
- Boskabadi, H. and M. Zakerihamidi, Evaluate the diagnosis of neonatal sepsis by measuring interleukins: A systematic review. Pediatrics and Neonatology, 2018. 59(4): p. 329-338.
- Boskabadi, H., et al., Serum interleukin 8 level as a diagnostic marker in late neonatal sepsis. Iranian Journal of Pediatrics, 2010. 20(1): p. 41-47.
- Bechard, D., et al., Characterization of the secreted form of endothelial-cell-specific molecule 1 by specific monoclonal antibodies. Journal of Vascular Research, 2000. 37(5): p. 417-425.
- Kali, A. and K.S. Rathan Shetty, Endocan: A novel circulating proteoglycan. Indian Journal of Pharmacology, 2014. 46(6): p. 579-583.
- Buyuktiryaki, M., et al., Can Endocan Predict Late-Onset Neonatal Sepsis? Journal of Pediatric Infectious Diseases, 2019. 14(3): p. 96-102.
- Kuzniewicz, M.W., et al., Development and implementation of an early-onset sepsis calculator to guide antibiotic management in late preterm and term neonates. Joint Commission Journal on Quality and Patient Safety, 2016. 42(5): p. 232-239.
- Sofouli, G.A., et al., Early Diagnosis of Late-Onset Neonatal Sepsis Using a Sepsis Prediction Score. Microorganisms, 2023. 11(2).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).