Submitted:
14 August 2023
Posted:
15 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
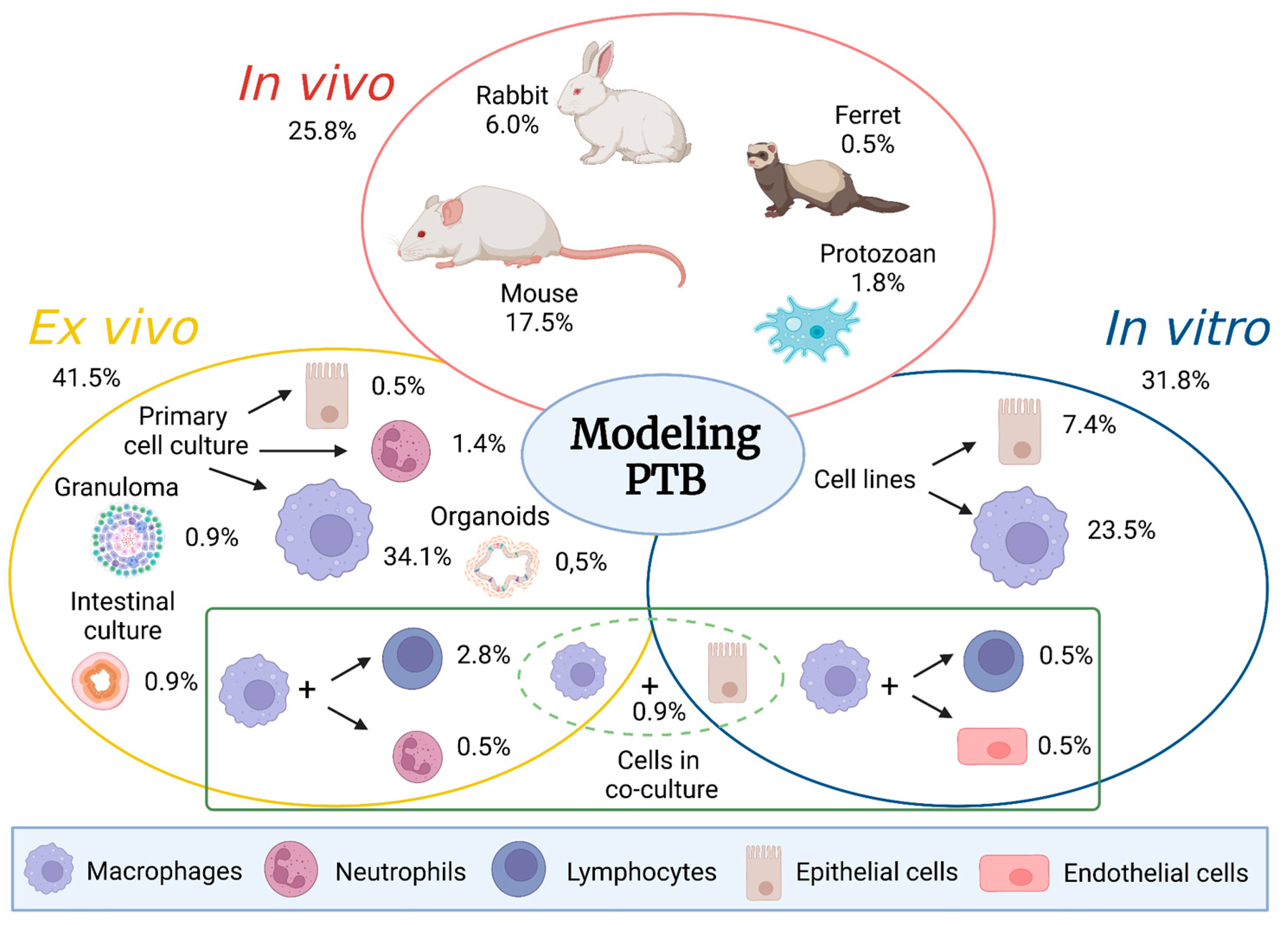
2. In vivo animal models in PTB research
2.1. Mouse model
2.2. Rabbit model
2.3. Ferret model
2.4. Protozoan model
3. From in vivo animal models to ex vivo and in vitro systems
3.1. Ex vivo models
3.1.1. Intestinal models
3.1.2. Immune cell models
Macrophages and monocytes
Granulomas
Neutrophils
3.1.3. Co-cultures of primary cells alone or combined with cell lines
3.1.4. Organoids
3.2. In vitro models
3.2.1. Macrophage cell lines
3.2.2. Epithelial cell lines
3.2.3. Co-culture of cell lines
4. Modeling PTB: future perspectives
4.1. Nematode model
4.2. Organs-on-a-chip
4.3. Precision cut intestinal slices (PCIS)
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Stabel, J.R.; Bannantine, J.P.; Hostetter, J.M. Comparison of sheep, goats, and calves as infection models for Mycobacterium avium subsp. paratuberculosis. Vet. Immunol. Immunopathol. 2020, 225, 110060. [Google Scholar] [CrossRef]
- Hines, M.E., 2nd; Stabel, J.R.; Sweeney, R.W.; Griffin, F.; Talaat, A.M.; Bakker, D.; Benedictus, G.; Davis, W.C.; de Lisle, G.W.; Gardner, I.A.; Juste, R.A.; Kapur, V.; Koets, A.; McNair, J.; Pruitt, G.; Whitlock, R.H. Experimental challenge models for Johne's disease: a review and proposed international guidelines. Vet. Microbiol. 2007, 122, 197–222. [Google Scholar] [CrossRef]
- Talaat, AM. ; Wu; C, Hines, ME2nd. Chapter 16: Experimental animal models of paratuberculosis. In Paratuberculosis: Organism, disease and control, 2nd ed; Marcel A Behr, Karen Stevenson, Vivek Kapur. CABI, Boston, MA, 2020; pp. 213–247. [Google Scholar]
- Cooney, M.A.; Stelle, J.L.; Steinberg, H.; Talaat, A.M. A murine oral model for Mycobacterium avium subsp. paratuberculosis infection and immunomodulation with Lactobacillus casei ATCC 334. Front. Cell. Infect. Microbiol. 2014, 4. [Google Scholar] [CrossRef]
- Veazey, R.S.; Horohov, D.W.; Krahenbuhl, J.L.; Taylor, H.W.; Oliver, J.L. 3rd; Snider, T.G. 3rd.Comparison of the resistance of C57BL/6 and C3H/He mice to infection with Mycobacterium paratuberculosis. Vet. Microbiol. 1995, 47, 79–87. [Google Scholar] [CrossRef]
- Shin, S.J.; Wu, C.; Steinberg, H.; Talaat, A.M. Identification of novel virulence determinants in Mycobacterium paratuberculosis by screening a library of insertional mutants. Infect. Immun. 2006, 74, 3825–33. [Google Scholar] [CrossRef] [PubMed]
- Shao, M.; Cui, N.; Tang, Y.; Chen, F.; Cui, Y.; Dang, G.; Liu, S. A candidate subunit vaccine induces protective immunity against Mycobacterium avium subspecies paratuberculosis in mice. NPJ Vaccines 2023, 8, 72. [Google Scholar] [CrossRef]
- Lee, J.H.; Park, H.T.; Shim, S.; Kim, S.; Woo, S.H.; Kim, D.Y.; Yoo, H.S. Immunopathological mechanisms in the early stage of Mycobacterium avium subsp. paratuberculosis infection via different administration routes in a murine model. PLoS One 2023, 18, e0281880. [Google Scholar] [CrossRef]
- Hussain, T.; Zhao, D.; Ali Shah, S.Z.; Wang, J.; Yue, R.; Liao, Y.; Sabir, N.; Yang, L.; Zhou, X. Responses of Murine Macrophages Infected by Mycobacterium avium subspecies paratuberculosis by Targeting Interleukin-10 and TGF-β-Activated Protein Kinase 1 Binding Protein 2. Front. Immunol. 2018, 8, 915. [Google Scholar] [CrossRef]
- Hussain, T.; Zhao, D.; Shah, S.Z.A.; Sabir, N.; Wang, J.; Liao, Y.; Song, Y.; Dong, H.; Hussain, M.M.; Ni, J.; Yang, L.; Zhou, X. Nilotinib: A Tyrosine Kinase Inhibitor Mediates Resistance to Intracellular Mycobacterium Via Regulating Autophagy. Cells 2019, 8, 506. [Google Scholar] [CrossRef]
- Abdissa, K.; Ruangkiattikul, N.; Ahrend, W.; Nerlich, A.; Beineke, A.; Laarmann, K.; Janze, N.; Lobermeyer, U.; Suwandi, A.; Falk, C.; Schleicher, U.; Weiss, S.; Bogdan, C.; Goethe, R. Relevance of inducible nitric oxide synthase for immune control of Mycobacterium avium subspecies paratuberculosis infection in mice. Virulence 2020, 11, 465–481. [Google Scholar] [CrossRef]
- Harding, H.P. Experimental infection with Mycobacterium johneei. J. Comp. Pathol. Therap. 1957, 67, 37–IN11. [Google Scholar] [CrossRef] [PubMed]
- Mokresh, A.H.; Czuprynski, C.J.; Butler, D.G. A rabbit model for study of Mycobacterium paratuberculosis infection. Infect. Immun. 1989, 57, 3798–3807. [Google Scholar] [CrossRef] [PubMed]
- Mokresh, A.H.; Butler, D.G. Granulomatous enteritis following oral inoculation of newborn rabbits with Mycobacterium paratuberculosis of bovine origin. Can. J. Vet. Res. 1990, 54, 313–319. [Google Scholar]
- Vaughan, J.A.; Lenghaus, C.; Stewart, D.J.; Tizard, M.L.; Michalski, W.P. Development of a Johne’s disease infection model in laboratory rabbits following oral administration of Mycobacterium avium subspecies paratuberculosis. Vet. Microbiol. 2005, 105, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Arrazuria, R.; Molina, E.; Mateo-Adad, M.; Arostegui, I.; Garrido, J.; Juste, R.A.; Elguezabal, N. Effect of various dietary regimens infection on oral challenge with Mycobacterium avium subsp. paratuberculosis in a rabbit model. Res.Vet. Sci. 2015, 101, 80–83. [Google Scholar]
- Beard, P.M.; Rhind, S.M.; Buxton, D.; Daniels, M.J.; Henderson, D.; Pirie, A.; Rudge, K.; Greig, A.; Hutchings, M.R.; Stevenson, K.; Sharp, J.M. Natural paratuberculosis infection in rabbits in Scotland. J. Comp. Pathol. 2001, 124, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Greig, A.; Stevenson, K.; Henderson, D.; Perez, V.; Hughes, V.; Pavlik, I.; Hines, M.E.; McKendrick, I.; Sharp, J.M. Epidemiological study of paratuberculosis in wild rabbits in Scotland. J. Clin. Microbiol. 1999, 37, 1746–1751. [Google Scholar] [CrossRef]
- Francis, J. Infection of laboratory animals with Mycobacterium johnei. J. Comp. Pathol. 1943, 53, 140–150. [Google Scholar] [CrossRef]
- Hirch, A. Infection of hamsters and rabbits with Mycobacterium johnei. J. Comp. Pathol. 1956, 66, 260–269. [Google Scholar] [CrossRef]
- Collins, P.; Matthews, P.R.; McDiarmid, A.; Brown, A. The pathogenicity of Mycobacterium avium and related mycobacteria for experimental animals. J. Med. Microbiol., 1983, 16, 27–35. [Google Scholar] [CrossRef]
- Oyanguren, M.; Molina, E.; Mugica, M.; Badiola, A.; Ladero-Auñon, I.; Elguezabal, N. Probiotic bacteria modulate immune responses to paratuberculosis vaccination. In Proceedings of the 15th International Association for Paratuberculosis Colloquium. Dublin, Ireland, 2022., 12-16 June.
- Arrazuria, R.; Elguezabal, N.; Juste, R.A.; Derakhshani, H.; Khafipour, E. Mycobacterium avium Subspecies paratuberculosis Infection Modifies Gut Microbiota under Different Dietary Conditions in a Rabbit Model. Front Microbiol. 2016, 7, 446. [Google Scholar] [CrossRef] [PubMed]
- Arrazuria, R.; Molina, E.; Garrido, J.M.; Pérez, V.; Juste, R.A.; Elguezabal, N. Vaccination sequence effects on immunological response and tissue bacterial burden in paratuberculosis infection in a rabbit model. Vet Res. 2016, 47, 77. [Google Scholar] [CrossRef]
- Fernández, B. (CONICET-Universidad de Buenos Aires, Ciudad de Buenos Aires, Argentina); Jolly, A. (Universidad de Buenos Aires, Ciudad de Buenos Aires, Argentina). Personal communication, 2023.
- Ladero-Auñon, I.; Molina, E.; Oyanguren, M.; Barriales, D.; Fuertes, M.; Sevilla, I.A.; Luo, L.; Arrazuria, R.; De Buck, J.; Anguita, J.; Elguezabal, N. Oral vaccination stimulates neutrophil functionality and exerts protection in a Mycobacterium avium subsp. paratuberculosis infection model. NPJ Vaccines 2021, 6, 102. [Google Scholar] [CrossRef]
- Arrazuria, R.; Ladero, I.; Molina, E.; Fuertes, M.; Juste, R.; Fernández, M.; Pérez, V.; Garrido, J.; Elguezabal, N. Alternative Vaccination Routes against Paratuberculosis Modulate Local Immune Response and Interference with Tuberculosis Diagnosis in Laboratory Animal Models. Vet. Sci. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Lamont, E.A.; Sreevatsan, S. Paradigm redux–Mycobacterium avium subspecies paratuberculosis-macrophage interactions show clear variations between bovine and human physiological body temperatures. Microb. Pathog. 2010, 48, 143–9. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Jakobsen, I.; Gu, X.; Nei, M. Diversity and evolution of T-cell receptor variable region genes in mammals and birds. Immunogenetics 1999, 50, 301–8. [Google Scholar] [CrossRef]
- Charavaryamath, C.; Gonzalez-Cano, P.; Fries, P.; Gomis, S.; Doig, K.; Scruten, E.; Potter, A.; Napper, S.; Griebel, P.J. Host responses to persistent Mycobacterium avium subspecies paratuberculosis infection in surgically isolated bovine ileal segments. Clin. Vaccine Immunol. 2013, 20, 156–65. [Google Scholar] [CrossRef]
- Krueger, L.A.; Beitz, D.C.; Humphrey, S.B.; Stabel, J.R. Gamma delta T cells are early responders to Mycobacterium avium ssp. paratuberculosis in colostrum-replete Holstein calves. J. Dairy Sci. 2016, 99, 9040–9050. [Google Scholar] [CrossRef]
- Khalifeh, M.S.; Stabel, J.R. Effects of gamma interferon, interleukin-10, and transforming growth factor beta on the survival of Mycobacterium avium subsp. paratuberculosis in monocyte-derived macrophages from naturally infected cattle. Infect. Immun. 2004, 72, 1974–1782. [Google Scholar] [CrossRef] [PubMed]
- Albarrak, S.M.; Waters, W.R.; Stabel, J.R.; Hostetter, J.M. Evaluating the cytokine profile of the WC1+ γδ T cell subset in the ileum of cattle with the subclinical and clinical forms of MAP infection. Vet. Immunol. Immunopathol. 2018, 201, 26–31. [Google Scholar] [CrossRef]
- Ludwig, L.; Egan, R.; Baquero, M.; Mansz, A.; Plattner, B.L. WC1+ and WC1neg γδ T lymphocytes in intestinal mucosa of healthy and Mycobacterium avium subspecies paratuberculosis-infected calves. Vet. Immunol. Immunopathol. 2019, 216, 109919. [Google Scholar] [CrossRef]
- Albrecht, R.A.; Liu, W.C.; Sant, A.J.; Tompkins, S.M.; Pekosz, A.; Meliopoulos, V.; Cherry, S.; Thomas, P.G.; Schultz-Cherry, S. Moving Forward: Recent Developments for the Ferret Biomedical Research Model. mBio 2018, 9, e01113–18. [Google Scholar] [CrossRef] [PubMed]
- Cross, M.L.; Labes, R.E.; Mackintosh, C.G. Oral infection of ferrets with virulent Mycobacterium bovis or Mycobacterium avium: susceptibility, pathogenesis and immune response. J. Comp. Pathol. 2000, 123, 15–21. [Google Scholar] [CrossRef] [PubMed]
- McCallan, L.; Corbett, D.; Andersen, P.L.; Aagaard, C.; McMurray, D.; Barry, C.; Thompson, S.; Strain, S.; McNair, J. A New Experimental Infection Model in Ferrets Based on Aerosolised Mycobacterium bovis. Vet. Med. Int. 2011, 2011, 981410. [Google Scholar] [CrossRef] [PubMed]
- Lugton, I.W.; Wobeser, G.; Morris, R.S.; Caley, P. Epidemiology of Mycobacterium bovis infection in feral ferrets (Mustela furo) in New Zealand: I. Pathology and diagnosis. N. Z. Vet. J. 1997, 45, 140–50. [Google Scholar] [CrossRef]
- Bannantine, J.P.; Gupta, T.; Zinniel, D.K.; Hikal, A.; Quinn, F.D.; Barletta, R.G. Use of a Ferret Model to Test Efficacy and Immunogenicity of Live Attenuated Mycobacterium avium Subspecies paratuberculosis Vaccines. Methods Mol. Biol. 2022, 2411, 95–104. [Google Scholar] [CrossRef]
- Mayer, J.; Marinim, R.P.; Fox, J.G. Biology and Diseases of Ferrets. Lab. Anim. Med. 2015, 2015, 577–622. [Google Scholar] [CrossRef]
- Mura, M.; Bull, T.J.; Evans, H.; Sidi-Boumedine, K.; McMinn, L.; Rhodes, G.; Pickup, R.; Hermon-Taylor, J. Replication and long-term persistence of bovine and human strains of Mycobacterium avium subsp. paratuberculosis within Acanthamoeba polyphaga. Appl. Environ. Microbiol. 2006, 72, 854–9. [Google Scholar] [CrossRef] [PubMed]
- Drancourt, M. Looking at amoebae as a source of mycobacteria. Microb. Pathog. 2014, 77, 119–24. [Google Scholar] [CrossRef]
- Samba-Louaka, A.; Robino, E.; Cochard, T.; Branger, M.; Delafont, V.; Aucher, W.; Wambeke, W.; Bannantine, J.P.; Biet, F.; Héchard, Y. Environmental Mycobacterium avium subsp. paratuberculosis Hosted by Free-Living Amoebae. Front. Cell. Infect. Microbiol. 2018, 8, 28. [Google Scholar] [CrossRef]
- Tenant, R.; Bermudez, L.E. Mycobacterium avium genes upregulated upon infection of Acanthamoeba castellanii demonstrate a common response to the intracellular environment. Curr. Microbiol. 2006, 52, 128–33. [Google Scholar] [CrossRef] [PubMed]
- Dubois, V.; Pawlik, A.; Bories, A.; Le Moigne, V.; Sismeiro, O.; Legendre, R.; Varet, H.; Rodríguez-Ordóñez, M.D.P.; Gaillard, J.L.; Coppée, J.Y.; Brosch, R.; Herrmann, J.L.; Girard-Misguich, F. Mycobacterium abscessus virulence traits unraveled by transcriptomic profiling in amoeba and macrophages. PLoS Pathog. 2019, 15, e1008069. [Google Scholar] [CrossRef]
- Phillips, I.L.; Everman, J.L.; Bermudez, L.E.; Danelishvili, L. Acanthamoeba castellanii as a Screening Tool for Mycobacterium avium Subspecies paratuberculosis Virulence Factors with Relevance in Macrophage Infection. Microorganisms 2020, 8, 1571. [Google Scholar] [CrossRef] [PubMed]
- Randall, K.J.; Turton, J.; Foster, J.R. Explant culture of gastrointestinal tissue: a review of methods and applications. Cell. Biol. Toxicol. 2011, 27, 267–84. [Google Scholar] [CrossRef] [PubMed]
- Karasov, W.H.; Diamond, J.M. A simple method for measuring intestinal nutrient uptake in vitro. J. Comp. Physiol. B. 1983, 152, 105–116. [Google Scholar] [CrossRef]
- Schleig, P.M.; Buergelt, C.D.; Davis, J.K.; Williams, E.; Monif, G.R.; Davidson, M.K. Attachment of Mycobacterium avium subspecies paratuberculosis to bovine intestinal organ cultures: method development and strain differences. Vet. Microbiol. 2005, 108, 271–9. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardóttir, O.G.; Bakke-McKellep, A.M.; Djønne, B.; Evensen, O. Mycobacterium avium subsp. paratuberculosis enters the small intestinal mucosa of goat kids in areas with and without Peyer's patches as demonstrated with the everted sleeve method. Comp. Immunol. Microbiol. Infect. Dis. 2005, 28, 223–30. [Google Scholar] [CrossRef] [PubMed]
- Brand, R.M.; Biswas, N.; Siegel, A.; Myerski, A.; Engstrom, J.; Jeffrey Metter, E.; Brand, R.E.; Cranston, R.D.; McGowan, I. Immunological responsiveness of intestinal tissue explants and mucosal mononuclear cells to ex vivo stimulation. J. Immunol. Methods. 2018, 463, 39–46. [Google Scholar] [CrossRef]
- Li, Z.; You, Q.; Ossa, F.; Mead, P.; Quinton, M.; Karrow, N.A. Assessment of yeast Saccharomyces cerevisiae component binding to Mycobacterium avium subspecies paratuberculosis using bovine epithelial cells. BMC Vet. Res. 2016, 12, 1–10. [Google Scholar] [CrossRef]
- Villena, J.; Aso, H.; Rutten, V.P.M.G.; Takahashi, H.; van Eden, W.; Kitazawa, H. Immunobiotics for the Bovine Host: Their Interaction with Intestinal Epithelial Cells and Their Effect on Antiviral Immunity. Front Immunol. 2018, 9, 326. [Google Scholar] [CrossRef]
- Hostetter, J.; Steadham, E.; Haynes, J.; Bailey, T.; Cheville, N. Phagosomal maturation and intracellular survival of Mycobacterium avium subspecies paratuberculosis in J774 cells. Comp. Immunol. Microbiol. Infect. Dis. 2003, 26, 269–83. [Google Scholar] [CrossRef]
- Kabara, E.; Coussens, P.M. Infection of Primary Bovine Macrophages with Mycobacterium avium Subspecies paratuberculosis Suppresses Host Cell Apoptosis. Front. Microbiol. 2012, 3, 215. [Google Scholar] [CrossRef]
- Langelaar, M.F.; Weber, C.N.; Overdijk, M.B.; Müller, K.E.; Koets, A.P.; Rutten, V.P. Cytokine gene expression profiles of bovine dendritic cells after interaction with Mycobacterium avium ssp. paratuberculosis (M.a.p.), Escherichia coli (E. coli) or recombinant M.a.p. heat shock protein 70. Vet. Immunol. Immunopathol. 2005, 107, 153–61. [Google Scholar] [CrossRef]
- Abdellrazeq, G.S.; Fry, L.M.; Elnaggar, M.M.; Bannantine, J.P.; Schneider, D.A.; Chamberlin, W.M.; Mahmoud, A.H.A.; Park, K.T.; Hulubei, V.; Davis, W.C. Simultaneous cognate epitope recognition by bovine CD4 and CD8 T cells is essential for primary expansion of antigen-specific cytotoxic T-cells following ex vivo stimulation with a candidate Mycobacterium avium subsp. paratuberculosis peptide vaccine. Vaccine 2020, 38, 2016–2025. [Google Scholar] [CrossRef]
- Arteche-Villasol, N.; Benavides, J.; Espinosa, J.; Vallejo, R.; Royo, M.; Ferreras, M.D.C.; Pérez, V.; Gutiérrez-Expósito, D. Optimized in vitro isolation of different subpopulation of immune cells from peripheral blood and comparative techniques for generation of monocyte-derived macrophages in small ruminants. Vet. Immunol. Immunopathol. 2020, 230, 110131. [Google Scholar] [CrossRef]
- Nielsen, M.C.; Andersen, M.N.; Møller, H.J. Monocyte isolation techniques significantly impact the phenotype of both isolated monocytes and derived macrophages in vitro. Immunology 2020, 159, 63–74. [Google Scholar] [CrossRef]
- Mitchell, R.M.; Gollnick, N.S.; Sreevatsan, S.; Russell, D.G.; Schukken, Y.H. Quantification of Mycobacterium avium subsp. paratuberculosis (MAP) survival in monocyte-derived macrophages. Vet. Immunol. Immunopathol. 2011, 139, 73–8. [Google Scholar] [CrossRef]
- Mathie, H.A.; Jensen, K.; Stevens, J.M.; Glass, E.J.; Hope, J.C. Quantifying Mycobacterium avium subspecies paratuberculosis infection of bovine monocyte derived macrophages by confocal microscopy. J. Microbiol. Methods. 2020, 168, 105779. [Google Scholar] [CrossRef]
- Bendixen, P.H.; Bloch, B.; Jorgensen, J.B. Lack of intracellular degradation of Mycobacterium paratuberculosis by bovine macrophages infected in vitro and in vivo: light microscopic and electron microscopic observations. Am. J. Vet. Res. 1981, 42, 109–13. [Google Scholar]
- Zurbrick, B.G.; Czuprynski, C.J. Ingestion and intracellular growth of Mycobacterium paratuberculosis within bovine blood monocytes and monocyte-derived macrophages. Infect. Immun. 1987, 55, 1588–93. [Google Scholar] [CrossRef]
- Weiss, D.J.; Evanson, O.A.; Deng, M.; Abrahamsen, M.S. Sequential patterns of gene expression by bovine monocyte-derived macrophages associated with ingestion of mycobacterial organisms. Microb. Pathog. 2004, 37, 215–24. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.J.; Evanson, O.A.; de Souza, C.; Abrahamsen, M.S. A critical role of interleukin-10 in the response of bovine macrophages to infection by Mycobacterium avium subsp paratuberculosis. Am. J. Vet. Res. 2005, 66, 721–6. [Google Scholar] [CrossRef] [PubMed]
- Khalifeh, M.S.; Al-Majali, A.M.; Stabel, J.R. Role of nitric oxide production in dairy cows naturally infected with Mycobacterium avium subsp. paratuberculosis. Vet. Immunol. Immunopathol. 2009, 131, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.D. Blocking the mitogen activated protein kinase-p38 pathway is associated with increase expression of nitric oxide synthase and higher production of nitric oxide by bovine macrophages infected with Mycobacterium avium subsp paratuberculosis. Vet. Immunol. Immunopathol. 2015, 164, 1–9. [Google Scholar] [CrossRef]
- Wherry, T.L.T.; Dassanayake, R.P.; Casas, E.; Mooyottu, S.; Bannantine, J.P.; Stabel, J.R. Exogenous Vitamin D3 Modulates Response of Bovine Macrophages to Mycobacterium avium subsp. paratuberculosis Infection and Is Dependent Upon Stage of Johne's Disease. Front. Cell. Infect. Microbiol. 2022, 11, 773938. [Google Scholar] [CrossRef]
- Jolly, A.; Lompardía, S.; Hajos, S.E.; Mundo, S.L. Evidence of a pro-apoptotic effect of specific antibodies in a bovine macrophage model of infection with Mycobacterium avium subsp. paratuberculosis. Vet. Immunol. Immunopathol. 2016, 169, 47–53. [Google Scholar] [CrossRef]
- Arteche-Villasol, N.; Gutiérrez-Expósito, D.; Vallejo, R.; Espinosa, J.; Elguezabal, N.; Ladero-Auñon, I.; Royo, M.; Del Carmen Ferreras, M.; Benavides, J.; Pérez, V. Early response of monocyte-derived macrophages from vaccinated and non-vaccinated goats against in vitro infection with Mycobacterium avium subsp. paratuberculosis. Vet. Res. 2021, 52, 69. [Google Scholar] [CrossRef]
- Lamont, E.A.; Talaat, A.M.; Coussens, P.M.; Bannantine, J.P.; Grohn, Y.T.; Katani, R.; Li, L.L.; Kapur, V.; Sreevatsan, S. Screening of Mycobacterium avium subsp. paratuberculosis mutants for attenuation in a bovine monocyte-derived macrophage model. Front. Cell. Infect. Microbiol. 2014, 4, 87. [Google Scholar] [CrossRef]
- Rathnaiah, G.; Lamont, E.A.; Harris, N.B.; Fenton, R.J.; Zinniel, D.K.; Liu, X.; Sotos, J.; Feng, Z.; Livneh-Kol, A.; Shpigel, N.Y.; Czuprynski, C.J.; Sreevatsan, S.; Barletta, R.G. Generation and screening of a comprehensive Mycobacterium avium subsp. paratuberculosis transposon mutant bank. Front. Cell. Infect. Microbiol. 2014, 4, 144. [Google Scholar] [CrossRef]
- Gollnick, N.S.; Mitchell, R.M.; Baumgart, M.; Janagama, H.K.; Sreevatsan, S.; Schukken, Y.H. Survival of Mycobacterium avium subsp. paratuberculosis in bovine monocyte-derived macrophages is not affected by host infection status but depends on the infecting bacterial genotype. Vet. Immunol. Immunopathol. 2007, 120, 93–105. [Google Scholar] [CrossRef]
- Koets, A.; Santema, W.; Mertens, H.; Oostenrijk, D.; Keestra, M.; Overdijk, M.; Labouriau, R.; Franken, P.; Frijters, A.; Nielen, M.; Rutten, V. Susceptibility to paratuberculosis infection in cattle is associated with single nucleotide polymorphisms in Toll-like receptor 2 which modulate immune responses against Mycobacterium avium subspecies paratuberculosis. Prev. Vet. Med. 2010, 93, 305–15. [Google Scholar] [CrossRef]
- Badia-Bringué, G.; Canive, M.; Alonso-Hearn, M. Control of Mycobacterium avium subsp. paratuberculosis load within infected bovine monocyte-derived macrophages is associated with host genetics. Front. Immunol. 2023, 14, 1042638. [Google Scholar] [CrossRef] [PubMed]
- Ariel, O.; Brouard, J.S.; Marete, A.; Miglior, F.; Ibeagha-Awemu, E.; Bissonnette, N. Genome-wide association analysis identified both RNA-seq and DNA variants associated to paratuberculosis in Canadian Holstein cattle in vitro experimentally infected macrophages. BMC Genomics 2021, 22, 162. [Google Scholar] [CrossRef]
- Marete, A.; Ariel, O.; Ibeagha-Awemu, E.; Bissonnette, N. Identification of Long Non-coding RNA Isolated From Naturally Infected Macrophages and Associated With Bovine Johne's Disease in Canadian Holstein Using a Combination of Neural Networks and Logistic Regression. Front. Vet. Sci. 2021, 8, 639053. [Google Scholar] [CrossRef]
- Janagama, H.K.; Lamont, E.A.; George, S.; Bannantine, J.P.; Xu, W.W.; Tu, Z.J.; Wells, S.J.; Schefers, J.; Sreevatsan, S. Primary transcriptomes of Mycobacterium avium subsp. paratuberculosis reveal proprietary pathways in tissue and macrophages. BMC Genomics 2010, 11, 561. [Google Scholar] [CrossRef]
- Koets, A.P.; Eda, S.; Sreevatsan, S. The within host dynamics of Mycobacterium avium ssp. paratuberculosis infection in cattle: where time and place matter. Vet. Res., 2015, 46, 61. [Google Scholar] [CrossRef] [PubMed]
- Elkington, P.; Lerm, M.; Kapoor, N.; Mahon, R.; Pienaar, E.; Huh, D.; Kaushal, D.; Schlesinger, L.S. In Vitro Granuloma Models of Tuberculosis: Potential and Challenges. J. Infect. Dis. 2019, 219, 1858–1866. [Google Scholar] [CrossRef]
- Abendaño, N.; Tyukalova, L.; Barandika, J.F.; Balseiro, A.; Sevilla, I.A.; Garrido, J.M.; Juste, R.A.; Alonso-Hearn, M. Mycobacterium avium subsp. paratuberculosis isolates induce in vitro granuloma formation and show successful survival phenotype, common anti-inflammatory and antiapoptotic responses within ovine macrophages regardless of genotype or host of origin. PLoS One 2014, 9, e104238. [Google Scholar] [CrossRef]
- Rice, H.J.; McDaniel, M.M.; Holland, A.; Eda, S. Modelling Bovine Granuloma Formation In Vitro upon Infection with Mycobacterium avium Subspecies paratuberculosis. Vet. Sci. 2019, 6, 80. [Google Scholar] [CrossRef]
- Ganesan, N.; Ronsmans, S.; Vanoirbeek, J.; Hoet, P.H.M. Assessment of Experimental Techniques That Facilitate Human Granuloma Formation in an In Vitro System: A Systematic Review. Cells 2022, 11, 864. [Google Scholar] [CrossRef]
- Lamont, E.A.; Bannantine, J.P.; Armién, A.; Ariyakumar, D.S.; Sreevatsan, S. Identification and characterization of a spore-like morphotype in chronically starved Mycobacterium avium subsp. paratuberculosis cultures. PLoS One 2012, 7, e30648. [Google Scholar] [CrossRef]
- Lugo-Villarino, G.; Hudrisier, D.; Benard, A.; Neyrolles, O. Emerging trends in the formation and function of tuberculosis granulomas. Front. Immunol. 2013, 3, 405. [Google Scholar] [CrossRef]
- Kroon, E.E. Neutrophils: Innate effectors of TB resistance? Front. Immunol. 2018, 9, 2637. [Google Scholar] [CrossRef]
- Hilda, J.N.; Das, S.; Tripathy, S.P.; Hanna, L.E. Role of neutrophils in tuberculosis: a bird’s eye view. Innate Immun. 2020, 26, 240–247. [Google Scholar] [CrossRef]
- Khare, S.; Nunes, J.S.; Figueiredo, J.F.; Lawhon, S.D.; Rossetti, C.A.; Gull, T.; Rice-Ficht, A.C.; Adams, L.G. Early phase morphological lesions and transcriptional responses of bovine ileum infected with Mycobacterium avium subsp. paratuberculosis. Vet. Pathol., 2009, 46, 717–28. [Google Scholar] [CrossRef] [PubMed]
- Trentini, M.M.; de Oliveira, F.M.; Kipnis, A.; Junqueira-Kipnis, A.P. The role of neutrophils in the induction of specific Th1 and Th17 during vaccination against tuberculosis. Front. Microbiol. 2016, 7, 898. [Google Scholar] [CrossRef] [PubMed]
- David, J.; Barkema, H.W.; Guan, L.L.; De Buck, J. Gene-expression profiling of calves 6 and 9 months after inoculation with Mycobacterium avium subspecies paratuberculosis. Vet. Res. 2014, 45, 96. [Google Scholar] [CrossRef]
- Gossner, A.; Watkins, C.; Chianini, F.; Hopkins, J. Pathways and genes associated with immune dysfunction in sheep Paratuberculosis. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef]
- Alonso-Hearn, M.; Canive, M.; Blanco-Vazquez, C.; Torremocha, R.; Balseiro, A.; Amado, J.; Varela-Martinez, E.; Ramos, R.; Jugo, BM.; Casais, R. RNA-Seq analysis of ileocecal valve and peripheral blood from Holstein cattle infected with Mycobacterium avium subsp. paratuberculosis revealed dysregulation of the CXCL8/IL8 signaling pathway. Sci. Rep. 2019, 9, 14845. [Google Scholar]
- Ladero-Auñon, I.; Elguezabal, N. Ladero-Auñon, I.; Elguezabal, N. Neutrophil functional assays. In: Encyclopedia of Infection and Immunity. 1st ed; Nima Razei. Elsevier. 2022, 4 pp 141-152.
- Ladero-Auñon, I.; Molina, E.; Holder, A.; Kolakowski, J.; Harris, H.; Urkitza, A.; Anguita, J.; Werling, D.; Elguezabal, N. Bovine Neutrophils Release Extracellular Traps and Cooperate With Macrophages in Mycobacterium avium subsp. paratuberculosis clearance In Vitro. Front. Immunol. 2021, 12, 645304. [Google Scholar] [CrossRef]
- Criado, M.; Pérez, V.; Arteche-Villasol, N.; Elguezabal, N.; Molina, E.; Benavides, J.; Gutiérrez-Expósito, D. Evaluation of the innate immune response of caprine neutrophils against Mycobacterium avium subspecies paratuberculosis in vitro. Vet. Res. 2023, 54, 61. [Google Scholar] [CrossRef] [PubMed]
- Baquero, M.M.; Plattner, B.L. Bovine peripheral blood WC1+ and WC1neg γδ T lymphocytes modulate monocyte-derived macrophage effector functions during in vitro Mycobacterium avium subspecies paratuberculosis infection. Cell. Immunol., 2017, 315, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Pooley, H.B.; Plain, K.M.; Purdie, A.C.; Begg, D.J.; Whittington, R.J.; de Silva, K. Integrated vaccine screening system: using cellular functional capacity in vitro to assess genuine vaccine protectiveness in ruminants. Pathog. Dis. 2018, 76. [Google Scholar] [CrossRef]
- Eshraghisamani, R.; Arrazuria, R.; Luo, L.; De Buck, J. Evaluation of Mycobacterium avium subsp. paratuberculosis isocitrate lyase (IcL) and ABC transporter (BacA) knockout mutants as vaccine candidates. Front. Cell. Infect. Microbiol. 2023, 30, 1149419. [Google Scholar] [CrossRef]
- Lamont, E.A.; O'Grady, S.M.; Davis, W.C.; Eckstein, T.; Sreevatsan, S. Infection with Mycobacterium avium subsp. paratuberculosis results in rapid interleukin-1β release and macrophage transepithelial migration. Infect. Immun. 2012, 80, 3225–35. [Google Scholar] [CrossRef]
- Lamont, E.A.; Xu WW, X.; Sreevatsan, S. Host-Mycobacterium avium subsp. paratuberculosis interactome reveals a novel iron assimilation mechanism linked to nitric oxide stress during early infection. BMC Genomics 2013, 14, 694. [Google Scholar] [CrossRef]
- Hostetter, J.; Zhang, W.; Simutis, F. Mycobacterium avium subspecies paratuberculosis infection of cattle does not diminish peripheral blood-derived macrophage mycobactericidal activity. Immunol. Lett. 2006, 107, 76–9. [Google Scholar] [CrossRef]
- Simutis, F.J.; Jones, D.E.; Hostetter, J.M. Failure of antigen-stimulated gammadelta T cells and CD4+ T cells from sensitized cattle to upregulate nitric oxide and mycobactericidal activity of autologous Mycobacterium avium subsp. paratuberculosis-infected macrophages. Vet. Immunol. Immunopathol. 2007, 116, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Park, K.T.; Allen, A.J.; Bannantine, J.P.; Seo, K.S.; Hamilton, M.J.; Abdellrazeq, G.S.; Rihan, H.M.; Grimm, A.; Davis, W.C. Evaluation of two mutants of Mycobacterium avium subsp. paratuberculosis as candidates for a live attenuated vaccine for Johne's disease. Vaccine 2011, 29, 4709–19. [Google Scholar] [CrossRef]
- Park, K.T.; ElNaggar, M.M.; Abdellrazeq, G.S.; Bannantine, J.P.; Mack, V.; Fry, L.M.; Davis, W.C. Phenotype and Function of CD209+ Bovine Blood Dendritic Cells, Monocyte-Derived-Dendritic Cells and Monocyte-Derived Macrophages. PLoS One 2016, 11, e0165247. [Google Scholar] [CrossRef]
- Abdellrazeq, G.S.; Elnaggar, M.M.; Bannantine, J.P.; Park, K.T.; Souza, C.D.; Backer, B.; Hulubei, V.; Fry, L.M.; Khaliel, S.A.; Torky, H.A.; Schneider, D.A.; Davis, W.C. A Mycobacterium avium subsp. paratuberculosis relA deletion mutant and a 35 kDa major membrane protein elicit development of cytotoxic T lymphocytes with ability to kill intracellular bacteria. Vet. Res. 2018, 49, 53. [Google Scholar] [CrossRef]
- Davis, W.C.; Mahmoud, A.H.; Abdellrazeq, G.S.; Elnaggar, M.M.; Dahl, J.L.; Hulubei, V.; Fry, L.M. Ex vivo Platforms to Study the Primary and Recall Immune Responses to Intracellular Mycobacterial Pathogens and Peptide-Based Vaccines. Front. Vet. Sci. 2022, 9, 878347. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Vries, R.G.; Snippert, H.J.; van de Wetering, M.; Barker, N.; Stange, D.E.; van Es, J.H.; Abo, A.; Kujala, P.; Peters, P.J.; Clevers, H. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature, 2009, 459, 262–5. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Nowak-Imialek, M.; Chen, X.; Chen, D.; Herrmann, D.; Ruan, D.; Chen, A.C.H.; Eckersley-Maslin, M.A.; Ahmad, S.; Lee, Y.L.; Kobayashi, T.; Ryan, D.; Zhong, J.; Zhu, J.; Wu, J.; Lan, G.; Petkov, S.; Yang, J.; Antunes, L.; Campos, L.S.; Fu, B.; Wang, S.; Yong, Y.; Wang, X.; Xue, S.G.; Ge, L.; Liu, Z.; Huang, Y.; Nie, T.; Li, P.; Wu, D.; Pei, D.; Zhang, Y.; Lu, L.; Yang, F.; Kimber, S.J.; Reik, W.; Zou, X.; Shang, Z.; Lai, L.; Surani, A.; Tam, P.P.L.; Ahmed, A.; Yeung, W.S.B.; Teichmann, S.A.; Niemann, H.; Liu, P. Establishment of porcine and human expanded potential stem cells. Nat. Cell. Biol. 2019, 21, 687–699. [Google Scholar] [CrossRef]
- Zhao, L.; Gao, X.; Zheng, Y.; Wang, Z.; Zhao, G.; Ren, J.; Zhang, J.; Wu, J.; Wu, B.; Chen, Y.; Sun, W.; Li, Y.; Su, J.; Ding, Y.; Gao, Y.; Liu, M.; Bai, X.; Sun, L.; Cao, G.; Tang, F.; Bao, S.; Liu, P.; Li, X. Establishment of bovine expanded potential stem cells. Proc. Natl. Acad. Sci. USA. 2021, 118, e2018505118. [Google Scholar] [CrossRef]
- Beumer, J.; Clevers, H. Cell fate specification and differentiation in the adult mammalian intestine. Nat. Rev. Mol. Cell Biol. 2020, 22, 39–53. [Google Scholar] [CrossRef]
- Beaumont, M.; Blanc, F.; Cherbuy, C.; Egidy, G.; Giuffra, E.; Lacroix-Lamandé, S.; Wiedemann, A. Intestinal organoids in farm animals. Vet. Res. 2021, 52, 33. [Google Scholar] [CrossRef]
- Powell, R.H.; Behnke, M.S. WRN conditioned media is sufficient for in vitro propagation of intestinal organoids from large farm and small companion animals. Biol. Open. 2017, 6, 698–705. [Google Scholar] [CrossRef]
- Hamilton, C.A.; Young, R.; Jayaraman, S.; Sehgal, A.; Paxton, E.; Thomson, S.; Katzer, F.; Hope, J.; Innes, E.; Morrison, L.J.; Mabbott, N.A. Development of in vitro enteroids derived from bovine small intestinal crypts. Vet. Res. 2018, 49, 54. [Google Scholar] [CrossRef]
- Alfajaro, M.M.; Kim, J.Y.; Barbé, L.; Cho, E.H.; Park, J.G.; Soliman, M.; Baek, Y.B.; Kang, M.I.; Kim, S.H.; Kim, G.J.; Park, S.I.; Pendu, J.L.; Cho, K.O. Dual Recognition of Sialic Acid and αGal Epitopes by the VP8* Domains of the Bovine Rotavirus G6P[5] WC3 and of Its Mono-reassortant G4P[5] RotaTeq Vaccine Strains. J Virol. 2019, 93, e00941–19. [Google Scholar] [CrossRef]
- Derricott, H.; Luu, L.; Fong, W.Y.; Hartley, C.S.; Johnston, L.J.; Armstrong, S.D.; Randle, N.; Duckworth, C.A.; Campbell, B.J.; Wastling, J.M.; Coombes, J.L. Developing a 3D intestinal epithelium model for livestock species. Cell. Tissue Res. 2019, 375, 409–424. [Google Scholar] [CrossRef]
- Töpfer, E.; Pasotti, A.; Telopoulou, A.; Italiani, P.; Boraschi, D.; Ewart, M.A.; Wilde, C. Bovine colon organoids: From 3D bioprinting to cryopreserved multi-well screening platforms. Toxicol. In Vitro 2019, 61, 104606. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.R.; Yang, H.; Lee, S.I.; Haq, I.; Ock, S.A.; Wi, H.; Lee, H.C.; Lee, P.; Yoo, J.G. Robust Three-Dimensional (3D) Expansion of Bovine Intestinal Organoids: An In Vitro Model as a Potential Alternative to an In Vivo System. Animals (Basel) 2021, 11, 2115. [Google Scholar] [CrossRef]
- Smith, D.; Price, D.R.G.; Burrells, A.; Faber, M.N.; Hildersley, K.A.; Chintoan-Uta, C.; Chapuis, A.F.; Stevens, M.; Stevenson, K.; Burgess, S.T.G.; Innes, E.A.; Nisbet, A.J.; McNeilly, T.N. The Development of Ovine Gastric and Intestinal Organoids for Studying Ruminant Host-Pathogen Interactions. Front. Cell. Infect. Microbiol. 2021, 11, 733811. [Google Scholar] [CrossRef]
- Blake, R.; Jensen, K.; Mabbott, N.; Hope, J.; Stevens, J. The Development of 3D Bovine Intestinal Organoid Derived Models to Investigate Mycobacterium avium ssp paratuberculosis Pathogenesis. Front. Vet. Sci. 2022, 9, 921160. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, J.; Yan, P.; He, L.; Zhang, X.; Wang, X.; Shi, Y.; Deng, L.; Zhang, Z.; Zhao, B. In-depth analysis of the relationship between bovine intestinal organoids and enteroids based on morphology and transcriptome. J. Tissue Eng. Regen. Med. 2022, 16, 1032–1046. [Google Scholar] [CrossRef]
- Noel, G.; Baetz, N.W.; Staab, J.F.; Donowitz, M.; Kovbasnjuk, O.; Pasetti, M.F.; Zachos, N.C. A primary human macrophage-enteroid co-culture model to investigate mucosal gut physiology and host-pathogen interactions. Sci. Rep. 2017, 7, 45270. [Google Scholar] [CrossRef] [PubMed]
- Bar-Ephraim, Y.E.; Kretzschmar, K.; Clevers, H. Organoids in immunological research. Nat. Rev. Immunol. 2020, 20, 279–293. [Google Scholar] [CrossRef]
- Son, Y.S.; Ki, S.J.; Thanavel, R.; Kim, J.J.; Lee, M.O.; Kim, J.; Jung, C.R.; Han, T.S.; Cho, H.S.; Ryu, C.M.; Kim, S.H.; Park, D.S.; Son, M.Y. Maturation of Human Intestinal Organoids in Vitro Facilitates Colonization by Commensal Lactobacilli by Reinforcing the Mucus Layer. FASEB J. 2020, 34, 9899–9910. [Google Scholar] [CrossRef]
- Puschhof, J.; Pleguezuelos-Manzano, C.; Martinez-Silgado, A.; Akkerman, N.; Saftien, A.; Boot, C.; de Waal, A.; Beumer, J.; Dutta, D.; Heo, I.; Clevers, H. Intestinal organoid cocultures with microbes. Nat. Protoc. 2021, 16, 4633–4649. [Google Scholar] [CrossRef]
- Heo, I.; Dutta, D.; Schaefer, D.A.; Iakobachvili, N.; Artegiani, B.; Sachs, N.; Boonekamp, K.E.; Bowden, G.; Hendrickx, A.P.A.; Willems, R.J.L.; Peters, P.J.; Riggs, M.W.; O'Connor, R.; Clevers, H. Modelling Cryptosporidium infection in human small intestinal and lung organoids. Nat. Microbiol. 2018, 3, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Guzmán-Delgado, N.E.; Carranza-Torres, I.E.; García-Davis, S.; Rivera, G.; Morán-Martínez, J.; Betancourt-Martínez, N.D.; Groothuis, G.M.M.; de Graaf, I.A.M.; Carranza-Rosales, P. Development of a Novel Ex-vivo 3D Model to Screen Amoebicidal Activity on Infected Tissue. Sci. Rep. 2019, 9, 8396. [Google Scholar] [CrossRef] [PubMed]
- Crawford, S.E.; Ramani, S.; Blutt, S.E.; Estes, M.K. Organoids to Dissect Gastrointestinal Virus-Host Interactions: What Have We Learned? Viruses 2021, 13, 999. [Google Scholar] [CrossRef] [PubMed]
- Kotloff, K.L.; Nataro, J.P.; Blackwelder, W.C.; Nasrin, D.; Farag, T.H.; Panchalingam, S.; Wu, Y.; Sow, S.O.; Sur, D.; Breiman, R.F.; Faruque, A.S.; Zaidi, A.K.; Saha, D.; Alonso, P.L.; Tamboura, B.; Sanogo, D.; Onwuchekwa, U.; Manna, B.; Ramamurthy, T.; Kanungo, S.; Ochieng, J.B.; Omore, R.; Oundo, J.O.; Hossain, A.; Das, S.K.; Ahmed, S.; Qureshi, S.; Quadri, F.; Adegbola, R.A.; Antonio, M.; Hossain, M.J.; Akinsola, A.; Mandomando, I.; Nhampossa, T.; Acácio, S.; Biswas, K.; O'Reill, C.E.; Mintz, E.D.; Berkeley, L.Y.; Muhsen, K.; Sommerfelt, H.; Robins-Browne, R.M.; Levine, M.M. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 2013, 382, 209–22. [Google Scholar] [CrossRef]
- Hill, D.R.; Huang, S.; Nagy, M.S.; Yadagiri, V.K.; Fields, C.; Mukherjee, D.; Bons, B.; Dedhia, P.H.; Chin, A.M.; Tsai, Y.H.; Thodla, S.; Schmidt, T.M.; Walk, S.; Young, V.B.; Spence, J.R. Bacterial colonization stimulates a complex physiological response in the immature human intestinal epithelium. Elife 2017, 6, e29132. [Google Scholar] [CrossRef]
- Roodsant, T.; Navis, M.; Aknouch, I.; Renes, I.B.; van Elburg, R.M.; Pajkrt, D.; Wolthers, K.C.; Schultsz, C.; van der Ark, K.C.H.; Sridhar, A.; Muncan, V. A Human 2D Primary Organoid-Derived Epithelial Monolayer Model to Study Host-Pathogen Interaction in the Small Intestine. Front. Cell. Infect. Microbiol. 2020, 10, 272. [Google Scholar] [CrossRef]
- Abuaita, B.H.; Lawrence, A.L.E.; Berger, R.P.; Hill, D.R.; Huang, S.; Yadagiri, V.K.; Bons, B.; Fields, C.; Wobus, C.E.; Spence, J.R.; Young, V.B.; O'Riordan, M.X. Comparative transcriptional profiling of the early host response to infection by typhoidal and non-typhoidal Salmonella serovars in human intestinal organoids. PLoS Pathog. 2021, 17, e100998. [Google Scholar] [CrossRef]
- Co, J.Y.; Margalef-Català, M.; Monack, D.M.; Amieva, M.R. Controlling the polarity of human gastrointestinal organoids to investigate epithelial biology and infectious diseases. Nat Protoc. 2021, 16, 5171–5192. [Google Scholar] [CrossRef]
- Aguirre Garcia, M.; Hillion, K.; Cappelier, J.M.; Neunlist, M.; Mahe, M.M.; Haddad, N. Intestinal Organoids: New Tools to Comprehend the Virulence of Bacterial Foodborne Pathogens. Foods 2022, 11, 108. [Google Scholar] [CrossRef]
- Kawasaki, M.; Goyama, T.; Tachibana, Y.; Nagao, I.; Ambrosini, Y.M. Farm and Companion Animal Organoid Models in Translational Research: A Powerful Tool to Bridge the Gap Between Mice and Humans. Front. Med. Technol. 2022, 4, 895379. [Google Scholar] [CrossRef]
- Hentschel, V.; Seufferlein, T.; Armacki, M. Intestinal organoids in coculture: redefining the boundaries of gut mucosa ex vivo modeling. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 321, G693–G704. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, A.; Pelzer, K.; Sriranganathan, N. The Paratuberculosis Paradigm Examined: A Review of Host Genetic Resistance and Innate Immune Fitness in Mycobacterium avium subsp. paratuberculosis Infection. Front. Vet. Sci. 2021, 8, 721706. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Hearn, M.; Badia-Bringué, G.; Canive, M. Genome-wide association studies for the identification of cattle susceptible and resilient to paratuberculosis. Front. Vet. Sci. 2022, 9, 935133. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardóttir, O.G.; Valheim, M.; Press, C.M. Establishment of Mycobacterium avium subsp. paratuberculosis infection in the intestine of ruminants. Adv. Drug Deliv. Rev. 2004, 56, 819–34. [Google Scholar] [CrossRef]
- Bermudez, L.E.; Petrofsky, M.; Sommer, S.; Barletta, R.G. Peyer's patch-deficient mice demonstrate that Mycobacterium avium subsp. paratuberculosis translocates across the mucosal barrier via both M cells and enterocytes but has inefficient dissemination. Infect. Immun. 2010, 78, 3570–7. [Google Scholar] [CrossRef]
- Ponnusamy, D.; Periasamy, S.; Tripathi, B.N.; Pal, A. Mycobacterium avium subsp. paratuberculosis invades through M cells and enterocytes across ileal and jejunal mucosa of lambs. Res. Vet. Sci. 2013, 94(2), 306–312. [Google Scholar] [CrossRef]
- Golan, L.; Livneh-Kol, A.; Gonen, E.; Yagel, S.; Rosenshine, I.; Shpigel, N.Y. Mycobacterium avium paratuberculosis invades human small-intestinal goblet cells and elicits inflammation. J. Infect. Dis. 2009, 199, 350–4. [Google Scholar] [CrossRef]
- Facciuolo, A.; Gonzalez-Cano, P.; Napper, S.; Griebel, P.J.; Mutharia, L.M. Marked Differences in Mucosal Immune Responses Induced in Ileal versus Jejunal Peyer's Patches to Mycobacterium avium subsp. paratuberculosis Secreted Proteins following Targeted Enteric Infection in Young Calves. PLoS One 2016, 11, e0158747. [Google Scholar] [CrossRef]
- Facciuolo, A.; Lee, A.H.; Gonzalez Cano, P.; Townsend, H.G.G.; Falsafi, R.; Gerdts, V.; Potter, A.; Napper, S.; Hancock, R.E.W.; Mutharia, L.M.; Griebel, P.J. Regional Dichotomy in Enteric Mucosal Immune Responses to a Persistent Mycobacterium avium ssp. paratuberculosis Infection. Front. Immunol. 2020, 11, 1020. [Google Scholar] [CrossRef]
- Ibeagha-Awemu, E.M.; Bissonnette, N.; Do, D.N.; Dudemaine, P.L.; Wang, M.; Facciuolo, A.; Griebel, P. Regionally Distinct Immune and Metabolic Transcriptional Responses in the Bovine Small Intestine and Draining Lymph Nodes During a Subclinical Mycobacterium avium subsp. paratuberculosis Infection. Front. Immunol. 2021, 12, 760931. [Google Scholar] [CrossRef]
- Stabel, J.R.; Stabel, T.J. Immortalization and characterization of bovine peritoneal macrophages transfected with SV40 plasmid DNA. Vet. Immunol. Immunopathol. 1995, 45, 211–20. [Google Scholar] [CrossRef]
- Woo, S.R.; Sotos, J.; Hart, A.P.; Barletta, R.G.; Czuprynski, C.J. Bovine monocytes and a macrophage cell line differ in their ability to phagocytose and support the intracellular survival of Mycobacterium avium subsp. paratuberculosis. Vet. Immunol. Immunopathol. 2006, 110, 109–20. [Google Scholar] [CrossRef]
- Alonso-Hearn, M.; Magombedze, G.; Abendaño, N.; Landin, M.; Juste, R.A. Deciphering the virulence of Mycobacterium avium subsp. paratuberculosis isolates in animal macrophages using mathematical models. J. Theor. Biol. 2019, 468, 82–91. [Google Scholar] [CrossRef]
- Tooker, B.C.; Coussens, P.M. Phagocytosis of M. paratuberculosis fails to activate expression of NADH dehydrogenase and nucleolin-related protein in bovine macrophages. Immunol Lett. 2004, 93, 137–42. [Google Scholar] [CrossRef]
- Abendaño, N.; Sevilla, I.A.; Prieto, J.M.; Garrido, J.M.; Juste, R.A.; Alonso-Hearn, M. Mycobacterium avium subspecies paratuberculosis isolates from sheep and goats show reduced persistence in bovine macrophages than cattle, bison, deer and wild boar strains regardless of genotype. Vet. Microbiol. 2013, 163, 325–34. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Hearn, M.; Abendaño, N.; Ruvira, M.A.; Aznar, R.; Landin, M.; Juste, R.A. Mycobacterium avium subsp. paratuberculosis (Map) Fatty Acids Profile Is Strain-Dependent and Changes Upon Host Macrophages Infection. Front. Cell. Infect. Microbiol. 2017, 7, 89. [Google Scholar] [CrossRef]
- Mundo, S.L.; Fontanals, A.M.; García, M.; Durrieu, M.; Alvarez, E.; Gentilini, E.R.; Hajos, S.E. Bovine IgG1 antibodies against Mycobacterium avium subsp. paratuberculosis protein p34-cx improve association of bacteria and macrophages. Vet Res. 2008, 39, 6. [Google Scholar] [CrossRef]
- Jolly, A.; Colavecchia, S.B.; Fernández, B.; Fernández, E.; Mundo, S.L. Antibodies Induced by Lipoarabinomannan in Bovines: Characterization and Effects on the Interaction between Mycobacterium avium subsp. paratuberculosis and Macrophages In Vitro. Vet. Med. Int. 2011, 2011, 258479. [Google Scholar] [CrossRef] [PubMed]
- Everman, J.L.; Bermudez, L.E. Antibodies against invasive phenotype-specific antigens increase Mycobacterium avium subspecies paratuberculosis translocation across a polarized epithelial cell model and enhance killing by bovine macrophages. Front. Cell. Infect. Microbiol. 2015, 5, 58. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Kang, H.; You, Q.; Ossa, F.; Mead, P.; Quinton, M.; Karrow, N.A. In vitro bioassessment of the immunomodulatory activity of Saccharomyces cerevisiae components using bovine macrophages and Mycobacterium avium ssp. paratuberculosis. J. Dairy Sci. 2018, 101, 6271–6286. [Google Scholar] [CrossRef] [PubMed]
- Kuehnel, M.P.; Goethe, R.; Habermann, A.; Mueller, E.; Rohde, M.; Griffiths, G.; Valentin-Weigand, P. Characterization of the intracellular survival of Mycobacterium avium ssp. paratuberculosis: phagosomal pH and fusogenicity in J774 macrophages compared with other mycobacteria. Cell. Microbiol. 2001, 3, 551–66. [Google Scholar] [CrossRef]
- Raschke, W.C.; Baird, S.; Ralph, P.; Nakoinz, I. Functional macrophage cell lines transformed by Abelson leukemia virus. Cell. 1978, 15, 261–7. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Levis, W.R.; Quinn, M.R.; Park, S.Y.; Schuller-Levis, G.B. Regulation of nitric oxide induced by mycobacterial lipoarabinomannan in murine macrophages: effects of interferon-beta and taurine-chloramine. Int. J. Lepr. Other Mycobact. Dis. 2000, 68, 444–51. [Google Scholar]
- Means, T.K.; Jones, B.W.; Schromm, A.B.; Shurtleff, B.A.; Smith, J.A.; Keane, J.; Golenbock, D.T.; Vogel, S.N.; Fenton, M.J. Differential effects of a Toll-like receptor antagonist on Mycobacterium tuberculosis-induced macrophage responses. J. Immunol. 2001, 166, 4074–82. [Google Scholar] [CrossRef]
- Bohsali, A.; Abdalla, H.; Velmurugan, K.; Briken, V. The non-pathogenic mycobacteria M. smegmatis and M. fortuitum induce rapid host cell apoptosis via a caspase-3 and TNF dependent pathway. BMC Microbiol. 2010, 10, 237. [Google Scholar] [CrossRef]
- Helguera-Repetto, A.C.; Chacon-Salinas, R.; Cerna-Cortes, J.F.; Rivera-Gutierrez, S.; Ortiz-Navarrete, V.; Estrada-Garcia, I.; Gonzalez-y-Merchand, J.A. Differential macrophage response to slow- and fast-growing pathogenic mycobacteria. Biomed. Res. Int. 2014, 2014, 916521. [Google Scholar] [CrossRef]
- Fu, Y.R.; Gao, K.S.; Ji, R.; Yi, Z.J. Differential transcriptional response in macrophages infected with cell wall deficient versus normal Mycobacterium tuberculosis. Int. J. Biol. Sci. 2015, 11, 22–30. [Google Scholar] [CrossRef]
- Taka, S.; Gazouli, M.; Sotirakoglou, K.; Liandris, E.; Andreadou, M.; Triantaphyllopoulos, K.; Ikonomopoulos, J. Functional analysis of 3'UTR polymorphisms in the caprine SLC11A1 gene and its association with the Mycobacterium avium subsp. paratuberculosis infection. Vet. Immunol. Immunopathol. 2015, 167, 75–9. [Google Scholar] [CrossRef]
- Thirunavukkarasu, S.; Plain, K.M.; Purdie, A.C.; Whittington, R.J.; de Silva, K. IFN-γ fails to overcome inhibition of selected macrophage activation events in response to pathogenic mycobacteria. PLoS One. 2017, 12, e0176400. [Google Scholar] [CrossRef] [PubMed]
- Barletta, R.G.; Bannantine, J.P.; Stabel, J.R.; Muthukrishnan, E.; Anderson, D.K.; Dutta, E.; Manthena, V.; Hanafy, M.; Zinniel, D.K. Mycobacterium avium subsp. paratuberculosis Candidate Vaccine Strains Are Pro-apoptotic in RAW 264.7 Murine Macrophages. Vaccines (Basel). 2023, 11, 1085. [Google Scholar] [CrossRef] [PubMed]
- Zur Lage, S.; Goethe, R.; Darji, A.; Valentin-Weigand, P.; Weiss, S. Activation of macrophages and interference with CD4+ T-cell stimulation by Mycobacterium avium subspecies paratuberculosis and Mycobacterium avium subspecies avium. Immunology 2003, 108, 62–9. [Google Scholar] [CrossRef]
- Ghosh, P.; Wu, C.W.; Talaat, A.M. Key role for the alternative sigma factor, SigH, in the intracellular life of Mycobacterium avium subsp. paratuberculosis during macrophage stress. Infect. Immun. 2013, 81, 2242–57. [Google Scholar] [CrossRef]
- Hostetter, J.M.; Steadham, E.M.; Haynes, J.S.; Bailey, T.B.; Cheville, N.F. Cytokine effects on maturation of the phagosomes containing Mycobacterium avium subspecies paratuberculosis in J774 cells. FEMS Immunol. Med. Microbiol. 2002, 34, 127–34. [Google Scholar] [CrossRef]
- Cirone, K.M.; Lahiri, P.; Holani, R.; Tan, Y.L.; Arrazuria, R.; De Buck, J.; Barkema, H.W.; Cobo, E.R. Synthetic cathelicidin LL-37 reduces Mycobacterium avium subsp. paratuberculosis internalization and pro-inflammatory cytokines in macrophages. Cell. Tissue Res. 2020, 379, 207–217. [Google Scholar] [CrossRef]
- Chanput, W.; Mes, J.J.; Wichers, H.J. THP-1 cell line: an in vitro cell model for immune modulation approach. Int. Immunopharmacol. 2014, 23, 37–45. [Google Scholar] [CrossRef]
- Cossu, A.; Sechi, L.A.; Zanetti, S.; Rosu, V. Gene expression profiling of Mycobacterium avium subsp. paratuberculosis in simulated multi-stress conditions and within THP-1 cells reveals a new kind of interactive intramacrophage behaviour. BMC Microbiol. 2012, 12, 87. [Google Scholar] [CrossRef]
- Shin, M.; Shin, S.W.; Jung, M.; Park, H.; Park, H.; Yoo, H.S. Host gene expression for Mycobacterium avium subsp. paratuberculosis infection in human THP-1 macrophages. Pathog. Dis. 2015, 73. [Google Scholar] [CrossRef]
- Mostoufi-Afshar, S.; Tabatabaei, M.; Ghahramani Seno, M.M. Mycobacterium avium subsp. paratuberculosis induces differential cytosine methylation at miR-21 transcription start site region. Iran. J. Vet. Res. (IVJR) 2018, 19, 262–269. [Google Scholar]
- Park, H.T.; Park, W.B.; Kim, S.; Lim, J.S.; Nah, G.; Yoo, H.S. Revealing immune responses in the Mycobacterium avium subsp. paratuberculosis-infected THP-1 cells using single cell RNA-sequencing. PLoS One. 2021, 16, e0254194. [Google Scholar] [CrossRef]
- Park, H.T.; Lee, S.M.; Ko, S.; Kim, S.; Park, H.E.; Shin, M.K.; Kim, D.; Yoo, H.S. Delineating transcriptional crosstalk between Mycobacterium avium subsp. paratuberculosis and human THP-1 cells at the early stage of infection via dual RNA-seq analysis. Vet Res. 2022, 53, 71. [Google Scholar] [CrossRef]
- Borrmann, E.; Möbius, P.; Diller, R.; Köhler, H. Divergent cytokine responses of macrophages to Mycobacterium avium subsp. paratuberculosis strains of Types II and III in a standardized in vitro model. Vet. Microbiol. 2011, 152, 101–11. [Google Scholar] [CrossRef]
- Motamedi Boroojeni, A.; Derakhshandeh, A.; Haghkhah, M.; Jalali, S.A.H.; Eraghi, V.A. A Novel Approach to Deliver a Mycobacterium avium subsp. paratuberculosis Antigen in Eukaryotic Cells. Mol. Biotechnol. 2019, 61, 506–512. [Google Scholar] [CrossRef]
- Wang, J.; Wang, Z.; Yao, Y.; Wu, J.; Tang, X.; Gu, T.; Li, G. The fibroblast growth factor-2 arrests Mycobacterium avium sp. paratuberculosis growth and immunomodulates host response in macrophages. Tuberculosis (Edinb). 2015, 95, 505–14. [Google Scholar] [CrossRef]
- Momotani, E.; Whipple, D.L.; Thiermann, A.B.; Cheville, N.F. Role of M cells and macrophages in the entrance of Mycobacterium paratuberculosis into domes of ileal Peyer's patches in calves. Vet. Pathol. 1988, 25, 131–7. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Hearn, M.; Patel, D.; Danelishvili, L.; Meunier-Goddik, L.; Bermudez, L.E. The Mycobacterium avium subsp. paratuberculosis MAP3464 gene encodes an oxidoreductase involved in invasion of bovine epithelial cells through the activation of host cell Cdc42. Infect. Immun. 2008, 76, 170–8. [Google Scholar] [CrossRef]
- Pott, J.; Basler, T.; Duerr, C.U.; Rohde, M.; Goethe, R.; Hornef, M.W. Internalization-dependent recognition of Mycobacterium avium ssp. paratuberculosis by intestinal epithelial cells. Cell. Microbiol. 2009, 11, 1802–15. [Google Scholar] [CrossRef]
- Miyazawa, K.; Hondo, T.; Kanaya, T.; Tanaka, S.; Takakura, I.; Itani, W.; Rose, M.T.; Kitazawa, H.; Yamaguchi, T.; Aso, H. Characterization of newly established bovine intestinal epithelial cell line. Histochem. Cell. Biol. 2010, 133, 125–34. [Google Scholar] [CrossRef]
- Chiba, E.; Villena, J.; Hosoya, S.; Takanashi, N.; Shimazu, T.; Aso, H.; Tohno, M.; Suda, Y.; Kawai, Y.; Saito, T.; Miyazawa, K.; He, F.; Kitazawa, H. A newly established bovine intestinal epithelial cell line is effective for in vitro screening of potential antiviral immunobiotic microorganisms for cattle. Res Vet Sci. 2012, 93, 688–94. [Google Scholar] [CrossRef] [PubMed]
- Takanashi, N.; Tomosada, Y.; Villena, J.; Murata, K.; Takahashi, T.; Chiba, E.; Tohno, M.; Shimazu, T.; Aso, H.; Suda, Y.; Ikegami, S.; Itoh, H.; Kawai, Y.; Saito, T.; Alvarez, S.; Kitazawa, H. Advanced application of bovine intestinal epithelial cell line for evaluating regulatory effect of lactobacilli against heat-killed enterotoxigenic Escherichia coli-mediated inflammation. BMC Microbiol. 2013, 13, 54. [Google Scholar] [CrossRef]
- Kobayashi, H.; Kanmani, P.; Ishizuka, T.; Miyazaki, A.; Soma, J.; Albarracin, L.; Suda, Y.; Nochi, T.; Aso, H.; Iwabuchi, N.; Xiao, J.Z.; Saito, T.; Villena, J.; Kitazawa, H. Development of an in vitro immunobiotic evaluation system against rotavirus infection in bovine intestinal epitheliocytes. Benef. Microbes. 2017, 8, 309–321. [Google Scholar] [CrossRef]
- Zhan, K.; Lin, M.; Liu, M.M.; Sui, Y.N.; Zhao, G.Q. Establishment of primary bovine intestinal epithelial cell culture and clone method. In Vitro Cell. Dev. Biol. Anim. 2017, 53, 54–57. [Google Scholar] [CrossRef]
- Katwal, P.; Thomas, M.; Uprety, T.; Hildreth, M.B.; Kaushik, R.S. Development and biochemical and immunological characterization of early passage and immortalized bovine intestinal epithelial cell lines from the ileum of a young calf. Cytotechnology 2019, 71, 127–148. [Google Scholar] [CrossRef]
- Katwal, P.; Uprety, T.; Okda, F.; Antony, L.; Thomas, M.; Chase, C.; Diel, D.G.; Nelson, E.; Young, A.; Li, F.; Scaria, J.; Kaushik, R.S. Characterization of bovine ileal epithelial cell line for lectin binding, susceptibility to enteric pathogens, and TLR mediated immune responses. Comp. Immunol. Microbiol. Infect. Dis. 2021, 74, 101581. [Google Scholar] [CrossRef]
- Kernéis, S.; Bogdanova, A.; Kraehenbuhl, J.P.; Pringault, E. Conversion by Peyer's patch lymphocytes of human enterocytes into M cells that transport bacteria. Science 1997, 277, 949–52. [Google Scholar] [CrossRef]
- El Bahi, S.; Caliot, E.; Bens, M.; Bogdanova, A.; Kernéis, S.; Kahn, A.; Vandewalle, A.; Pringault, E. Lymphoepithelial interactions trigger specific regulation of gene expression in the M cell-containing follicle-associated epithelium of Peyer's patches. J. Immunol. 2002, 168, 3713–20. [Google Scholar] [CrossRef]
- Nair, V.R.; Franco, L.H.; Zacharia, V.M.; Khan, H.S.; Stamm, C.E.; You, W.; Marciano, D.K.; Yagita, H.; Levine, B.; Shiloh, M.U. Microfold Cells Actively Translocate Mycobacterium tuberculosis to Initiate Infection. Cell. Rep. 2016, 6, 1253–1258. [Google Scholar] [CrossRef]
- Bannantine, J.P.; Huntley, J.F.J.; Miltner, E.; Stabel, J.R.; Bermudez, L.E. The Mycobacterium avium subsp. paratuberculosis 35 kDa protein plays a role in invasion of bovine epithelial cells. Microbiology 2003, 149, 2061–2069. [Google Scholar] [CrossRef]
- Patel, D.; Danelishvili, L.; Yamazaki, Y.; Alonso, M.; Paustian, M.L.; Bannantine, J.P.; Meunier-Goddik, L.; Bermudez, L.E. The ability of Mycobacterium avium subsp. paratuberculosis to enter bovine epithelial cells is influenced by preexposure to a hyperosmolar environment and intracellular passage in bovine mammary epithelial cells. Infect. Immun. 2006, 74, 2849–55. [Google Scholar] [CrossRef]
- Alonso-Hearn, M.; Eckstein, T.M.; Sommer, S.; Bermudez, L.E. A Mycobacterium avium subsp. paratuberculosis LuxR regulates cell envelope and virulence. Innate Immun. 2010, 16, 235–47. [Google Scholar] [CrossRef]
- Everman, J.L.; Danelishvili, L.; Flores, L.G.; Bermudez, L.E. MAP1203 Promotes Mycobacterium avium Subspecies paratuberculosis Binding and Invasion to Bovine Epithelial Cells. Front. Cell. Infect. Microbiol. 2018, 8, 217. [Google Scholar] [CrossRef]
- Everman, J.L.; Eckstein, T.M.; Roussey, J.; Coussens, P.; Bannantine, J.P.; Bermudez, L.E. Characterization of the inflammatory phenotype of Mycobacterium avium subspecies paratuberculosis using a novel cell culture passage model. Microbiology (Reading). 2015, 161, 1420–1434. [Google Scholar] [CrossRef]
- Sweeney, R.W.; Whitlock, R.H.; Rosenberger, A.E. Mycobacterium paratuberculosis isolated from fetuses of infected cows not manifesting signs of the disease. Am. J. Vet. Res. 1992, 53, 477–80. [Google Scholar] [PubMed]
- Thompson, B.R.; Clark, R.G.; Mackintosh, C.G. Intra-uterine transmission of Mycobacterium avium subsp paratuberculosis in subclinically affected red deer (Cervus elaphus). N. Z. Vet. J. 2007, 55, 308–13. [Google Scholar] [CrossRef]
- Kugadas, A.; Lamont, E.A.; Bannantine, J.P.; Shoyama, F.M.; Brenner, E.; Janagama, H.K.; Sreevatsan, S. A Mycobacterium avium subsp. paratuberculosis Predicted Serine Protease Is Associated with Acid Stress and Intraphagosomal Survival. Front. Cell. Infect. Microbiol. 2016, 6, 85. [Google Scholar] [CrossRef]
- Schwarz, D.G.G.; Shoyama, F.M.; Oliveira, L.L.; Sreevatsan, S.; Moreira, M.A.S. Rapid baso-apical translocation of Mycobacterium avium ssp. paratuberculosis in mammary epithelial cells in the presence of Escherichia coli. J. Dairy Sci. 2018, 101, 6287–6295. [Google Scholar] [CrossRef] [PubMed]
- Pena, J.L.; Gonçalves Schwarz, D.G.; Willian de Lima Brasil, A.; Licursi de Oliveira, L.; Albuquerque Caldeira, J.L.; Scatamburlo Moreira, M.A. Differences in the coinfective process of Staphylococcus aureus and Streptococcus agalactiae in bovine mammary epithelial cells infected by Mycobacterium avium subsp. paratuberculosis. Microb Pathog. 2020, 149, 104476. [Google Scholar] [CrossRef] [PubMed]
- Shandilya, U.K.; Wu, X.; McAllister, C.; Mutharia, L.; Karrow, N.A. Role of Toll-Like Receptor 4 in Mycobacterium avium subsp. paratuberculosis Infection of Bovine Mammary Epithelial (MAC-T) Cells In Vitro. Microbiol Spectr. 2023, 11, e0439322. [Google Scholar] [CrossRef]
- Shandilya, U.K.; Wu, X.; McAllister, C.; Mutharia, L.; Karrow, N.A. Impact of Mycobacterium avium subsp. paratuberculosis infection on bovine IL10RA knockout mammary epithelial (MAC-T) cells. In Vitro Cell Dev Biol Anim. 2023, 59, 214–223. [Google Scholar] [CrossRef]
- Phillips, I.L.; Danelishvili, L.; Bermudez, L.E. Macrophage Proteome Analysis at Different Stages of Mycobacterium avium Subspecies paratuberculosis Infection Reveals a Mechanism of Pathogen Dissemination. Proteomes 2021, 9, 20. [Google Scholar] [CrossRef]
- Engelmann, I.; Pujol, N. Innate immunity in C. elegans. Adv. Exp. Med. Biol. 2010, 708, 105–21. [Google Scholar] [CrossRef]
- Komura, T.; Yasui, C.; Miyamoto, H.; Nishikawa, Y. Caenorhabditis elegans as an alternative model host for legionella pneumophila, and protective effects of Bifidobacterium infantis. Appl. Environ. Microbiol. 2010, 76, 4105–8. [Google Scholar] [CrossRef] [PubMed]
- Everman, J.L.; Ziaie, N.R.; Bechler, J.; Bermudez, L.E. Establishing Caenorhabditis elegans as a model for Mycobacterium avium subspecies hominissuis infection and intestinal colonization. Biol. Open. 2015, 4, 1330–5. [Google Scholar] [CrossRef]
- Bermudez, L.E.; Rose, S.J.; Everman, J.L.; Ziaie, N.R. Establishment of a Host-to-Host Transmission Model for Mycobacterium avium subsp. hominissuis Using Caenorhabditis elegans and Identification of Colonization-Associated Genes. Front. Cell. Infect. Microbiol. 2018, 8, 123. [Google Scholar] [CrossRef] [PubMed]
- Viri, V.; Arveiler, M.; Lehnert, T.; Gijs, M.A.M. An In Vivo Microfluidic Study of Bacterial Load Dynamics and Absorption in the C. elegans Intestine. Micromachines (Basel) 2021, 12, 832. [Google Scholar] [CrossRef]
- Mallo, G.V.; Kurz, C.L.; Couillault, C.; Pujol, N.; Granjeaud, S.; Kohara, Y.; Ewbank, J.J. Inducible antibacterial defense system in C. elegans. Curr. Biol. 2002, 12, 1209–14. [Google Scholar] [CrossRef]
- Chávez, V.; Mohri-Shiomi, A.; Maadani, A.; Vega, L.A.; Garsin, D.A. Oxidative stress enzymes are required for DAF-16-mediated immunity due to generation of reactive oxygen species by Caenorhabditis elegans. Genetics 2007, 176, 1567–77. [Google Scholar] [CrossRef]
- Galbadage, T.; Shepherd, T.F.; Cirillo, S.L.; Gumienny, T.L.; Cirillo, J.D. The Caenorhabditis elegans p,8 MAPK Gene plays a key role in protection from mycobacteria. Microbiologyopen 2016, 5, 436–52. [Google Scholar] [CrossRef]
- Sutton, K.M.; Orr, B.; Hope, J.; Jensen, S.R.; Vervelde, L. Establishment of bovine 3D enteroid-derived 2D monolayers. Vet. Res. 2022, 53, 15. [Google Scholar] [CrossRef] [PubMed]
- Candarlioglu, P.L.; Dal Negro, G.; Hughes, D.; Balkwill, F.; Harris, K.; Screen, H.; Morgan, H.; David, R.; Beken, S.; Guenat, O.; Rowan, W.; Amour, A. Organ-on-a-chip: current gaps and future directions. Biochem. Soc. Trans. 2022, 50, 665–673. [Google Scholar] [CrossRef]
- Csukovich, G.; Pratscher, B.; Burgener, I.A. The World of Organoids: Gastrointestinal Disease Modelling in the Age of 3R and One Health with Specific Relevance to Dogs and Cats. Animals (Basel) 2022, 2, 2461. [Google Scholar] [CrossRef]
- Xian, C.; Zhang, J.; Zhao, S.; Guang Li, X. Gut-on-a-chip for disease models. J. Tissue. Engineer. 2023, 14, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Baddal, B.; Marrazzo, P. Refining Host-Pathogen Interactions: Organ-on-Chip Side of the Coin. Pathogens. 2021, 10, 203. [Google Scholar] [CrossRef]
- Pimenta, J.; Ribeiro, R.; Almeida, R.; Costa, P.F.; da Silva, M.A.; Pereira, B. Organ-on-Chip Approaches for Intestinal 3D In Vitro Modeling. Cell. Mol. Gastroenterol. Hepatol. 2022, 13, 351–367. [Google Scholar] [CrossRef] [PubMed]
- Morsink, MAJ. ; Willemen, NGA.; Leijten, J.; Bansal, R.; Shin, S.R. Immune organs and immune cells on a chip: an overview of biomedical applications. Micromachines, 2020, 11, 849. [Google Scholar] [CrossRef]
- Majorova, D.; Atkins, E.; Martineau, H.; Vokral, I.; Oosterhuis, D.; Olinga, P.; Wren, B.; Cuccui, J.; Dirk Werling, D. Use of Precision-Cut Tissue Slices as a Translational Model to Study Host-Pathogen Interaction. Front. Vet. Sci. 2021, 8, 686088. [Google Scholar] [CrossRef]
- Li, M.; de Graaf, I.A.M.; Groothuis, G.M.M. Precision-cut intestinal slices: alternative model for drug transport, metabolism, and toxicology research. Expert. Opin. Drug. Metab. Toxicol. 2016, 12, 175–90. [Google Scholar] [CrossRef] [PubMed]
- de Kanter, R.; Tuin, A.; van de Kerkhof, E.; Martignoni, M.; Draaisma, A.L.; de Jager, M.H.; de Graaf, I.A.; Meijer, D.K.; Groothuis, G.M. A new technique for preparing precision-cut slices from small intestine and colon for drug biotransformation studies. J. Pharmacol. Toxicol. Methods. 2005, 51, 65–72. [Google Scholar] [CrossRef]
- Molina-Torres, C.A.; Flores-Castillo, O.N.; Carranza-Torres, I.E.; Guzmán-Delgado, N.E.; Viveros-Valdez, E.; Vera-Cabrera, L.; Ocampo-Candiani, J.; Verde-Star, J.; Castro-Garza, J.; Carranza-Rosales, P. Ex vivo infection of murine precision-cut lung tissue slices with Mycobacterium abscessus: a model to study antimycobacterial agents. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 52. [Google Scholar] [CrossRef]
- Remot, A.; Carreras, F.; Coupé, A.; Doz-Deblauwe, É.; Boschiroli, M.L.; Browne, J.A.; Marquant, Q.; Descamps, D.; Archer, F.; Aseffa, A.; Germon, P.; Gordon, S.V.; Winter, N. Mycobacterial Infection of Precision-Cut Lung Slices Reveals Type 1 Interferon Pathway Is Locally Induced by Mycobacterium bovis but Not M. tuberculosis in a Cattle Breed. Front. Vet. Sci. 2021, 8. [Google Scholar] [CrossRef]
- Punyadarsaniya, D.; Winter, C.; Mork, A.K.; Amiri, M.; Naim, H.Y.; Rautenschlein, S.; Herrler, G. Precision-cut intestinal slices as a culture system to analyze the infection of differentiated intestinal epithelial cells by avian influenza viruses. J. Virol. Methods. 2015, 212, 71–75. [Google Scholar] [CrossRef]
- Krimmling, T.; Beineke, A.; Schwegmann-Weßels, C. Infection of porcine precision cut intestinal slices by transmissible gastroenteritis coronavirus demonstrates the importance of the spike protein for enterotropism of different virus strains. Vet. Microbiol. 2017, 205, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Martinec, O.; Huliciak, M.; Staud, F.; Cecka, F.; Vokral, I.; Cerveny, L. Anti-HIV and Anti-Hepatitis C Virus Drugs Inhibit P-Glycoprotein Efflux Activity in Caco-2 Cells and Precision-Cut Rat and Human Intestinal Slices. Antimicrob. Agents. Chemother. 2019, 63, e00910–19. [Google Scholar] [CrossRef] [PubMed]
| Age at challenge | Infective strain source | Infective dose (dose number) |
Study end-point w.p.i. |
Evidence of infection %* | Experiment objective |
Reference |
|---|---|---|---|---|---|---|
| 4-5 w | Rabbit /hamster |
1.6-5.6 mg (7) | 4-40 | 6-50 | Pathogenesis | [20] |
| 1-2 d | Cattle | 7x106 CFU (5-10) | 32-40 | 43 | Pathogenesis | [13] |
| 1-2 d | Cattle | 3.6x108 CFU (1) | 2-36 | 38 | Pathogenesis | [14] |
| 1-2 d | Cattle | 2.6x108 CFU (1) | 2-36 | 100 | Pathogenesis | [14] |
| 3 m | Cattle | 5x108 CFU (3) | 104-128 | 50 | Pathogenesis | [15] |
| 2 w | Cattle | 1x108 CFU (3) | 8-84 | 19 | Pathogenesis | [15] |
| 8 w | Cattle K10 | 1x109 CFU (3) | 16-20 | 40-87 | Diet evaluation | [16] |
| 16 w | Cattle K10 | 4x108 CFU (3) | 20 | 80 | MAP infection and diet effect on microbiota | [23] |
| 16 w/ 30 w |
Cattle K10 | 4x108 CFU (6) | 20 | 100 | MAP infection and diet effect on microbiota | [23] |
| 12 w | Cattle K10 | 4x108 CFU (3) | 25 | 80 | Vaccination sequence efficacy | [24] |
| 13 w | Cattle K10 | 1x109 CFU (3) | 24-25 | 80 | Vaccination routes | [27] |
| 13-14 w | Cattle NK-764 | 3x108 CFU (3) | 19 | 60 | Vaccination efficacy and trained immunity | [26] |
| 15 w | Cattle NK-832 | 3x108 CFU (3) | 12 | 100 | Effect of vaccination and probiotics and trained immunity | [22] |
| 8-11 w | Cattle | 1x109 CFU (3) | 21 | 100 | Effect of passively transferred antibodies | [25] |
| Models | Reported application* P D V T |
References | Main limitations | Scientific potential | |
|---|---|---|---|---|---|
|
In vivo non-ruminant animal models |
Mouse | ✓ ✓ ✓ | [4,5,6,7,8,9,10,11] | Lack of development of clinical signs | Great amount of immunological reagents Well defined model Initial vaccine screening platform |
| Rabbit | ✓ ✓ ✓ ✓ | [13,14,15,16,20,22,23,24,25,26,27] | Scarcity of immunological reagents | Clinical outcome closely resembling ruminant PTB | |
| Ferret | ✓ ✓ | [39] | Scarcity of immunological reagents Carnivore diet Outbred nature of the model |
Strain virulence factor research | |
| Protozoa | ✓ | [41,43,46] | Unicellular organism | Strain virulence factor research | |
| Ex vivo models | Intestinal | ✓ ✓ | [49,50,52] | Difficult to manage No standardized protocols available |
Early stage pathogenesis |
| Immune cells: macrophages/ monocytes |
✓ ✓ ✓ | [33,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,78] | High variability between donors and lower reproducibility | Strain virulence factor research Host genetics MAP-host interaction at receptor-ligand level |
|
| Granulomas | ✓ ✓ | [81,82] | Limited growth potential Not all granuloma cell types included |
Early stage pathogenesis Initial vaccine screening platform |
|
| Immune cells: neutrophils | ✓ ✓ | [26,93,94,95] | Role in PTB not fully understood Short life span cells Inability to cryopreserve or expand them in vitro |
Early stage host-pathogen interaction | |
| Co-cultures of primary cells | ✓ ✓ | [57,94,96,97,98,99,100,101,102,103,104,105,106] | Limited growth potential High variability between donors |
Dissection of cross-talk between key cell types in upon MAP infection Initial vaccine screening platform |
|
| Organoids | ✓ | [119] | No standardized protocols available | Early stage pathogenesis | |
| In vitro models | Macrophage cell lines | ✓ ✓ ✓ | [54,55,69,145,146,147,148,149,150,151,152,153,154,155,163,165,166] | Genetically transformed cells Lower or different response in relation to primary cells |
Strain virulence factor research MAP-host interaction at receptor-ligand level |
| Epithelial cell lines | ✓ ✓ ✓ | [139,179,180,191,192,193,194,195,198,199,200,201,202] | Only to study initial interactions as they are not the target cells | MAP intestinal invasion (cellular and molecular level), early pathogenesis and therapy | |
| Co-culture of cell lines | ✓ | [165,203] | Simple and controllable set up | Early stage pathogenesis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





