1. Introduction
In medicine, the skill of identifying veins in infusions, taking blood is a skill that not all doctors can perform well. Finding a vein is difficult (especially for children, women, and obesity…) [
1] It is not uncommon for cases of vein deviation or rupture of vessels when injected or drawn blood that has adversely affected the patient. The vein retriever process requires the precise operation of people with experience and is not allowed to make mistakes because if taken many times will cause pain and discomfort to the patient [
2].
On the other hand: the problem of breast cancer shows that the incidence of breast cancer is increasing in many parts of the world, especially in transition countries [
3]. Sadly, an estimated 685,000 women lost their lives to breast cancer in 2020, making up 16% of all cancer deaths in women or 1 in every 6 deaths. To address this concerning trend the World Health Organization (WHO) recently initiated the Global Breast Cancer Initiative [
4]. In 2018, Vietnam ranked first in the world in terms of breast cancer incidence with 15,229 new cases and 6,103 deaths. In 2020, there were over 21,555 new cases, including more than 9,345 deaths because of the breast cancer [
5]. Currently, Vietnam annually records about 183,000 new cases of cancer, of which breast cancer accounts for 25.8% of cancers in women, with nearly 22,000 new cases and more than 9,000 deaths [
6]. Notably, often the younger breast cancer patients, the worse the prognosis and the lower the cure rate than the elderly. Epidemiological studies indicated that, the most effective method to increase the cure rate of breast cancer, especially in young people, is screening examination to detect the disease early. While the over 5-year survival rate for the very early stage reaches 98%, for the late stage this rate is only about 10%. This collaborative effort aims to reduce breast cancer mortality by promoting prompt diagnosis, effective treatment, and comprehensive patient management. Currently, there are many advanced diagnostic techniques such as BRCA1/2 gene test, breast ultrasound elastography, 3D mammogram, magnetic resonance imaging (MRI), breast tumor biopsy, ultrasound, computed tomography (CT), etc.
Past studies have indicated that the timely detection and appropriate treatment of breast cancer could significantly decrease mortality rates in the long run [
7]. At present, there is a wide array of clinical approaches employed for the screening and diagnosis of breast cancer. Although mammography is currently the standard screening method for breast cancer, it has limitations. It is less effective for individuals under 40 years old and dense breasts, and it is not sensitive enough to detect small tumors (less than 1 mm, approximately 100,000 cells). Furthermore, it does not provide any information on the potential outcome of the disease [
8,
9]. Contrast-enhanced (CE) digital mammography, on the other hand, offers a more precise diagnosis than mammography and ultrasound for individuals with dense breasts. However, this technique is not widely accessible due to its cost and the high levels radiation involved [
10]. Ultrasound has been utilized as an additional tool for Magnetic resonance imaging (MRI) has the capability to identify small lesions that may not be detectable through mammography it is also costly and has low specificity, potentially leading to overdiagnosis [
9,
10]. Positron emission tomography (PET) is recognized as the most accurate method for visualizing tumor spread or monitoring their response to treatment [
11].
However, the aforementioned methods face challenges when it comes to widespread implementation in early-stage cancer screening due to their limited availability in local medical facilities, high costs, lengthy result turnaround times, and complex processes [
12]. On the other hand, thermal imaging has emerged as an effective method for early detection and diagnosis of breast cancer. In this study, we have focused on the development and testing of the BKA-06 device, which simulates the energy absorption image of cancer (particularly breast cancer and superficial cancers). Through testing on both volunteers and patients, this device has demonstrated rapid and precise results. Additionally, the device also aids in identifying blood vessels during patient treatment, which is crucial for procedures such as blood collection and injection/infusion. It is worth noting that not all medical professionals possess the expertise to accurately identify blood vessels, and misidentification can have detrimental effects on patients, especially children.
2. Materials and Methods
2.1. Research Methods
BKA-06 is based on biomedical physics principles. Analyze and select electronic elements and suitable materials for fabrication equipment.
2.2. Physical Basis and Operating Principle of BKA-06
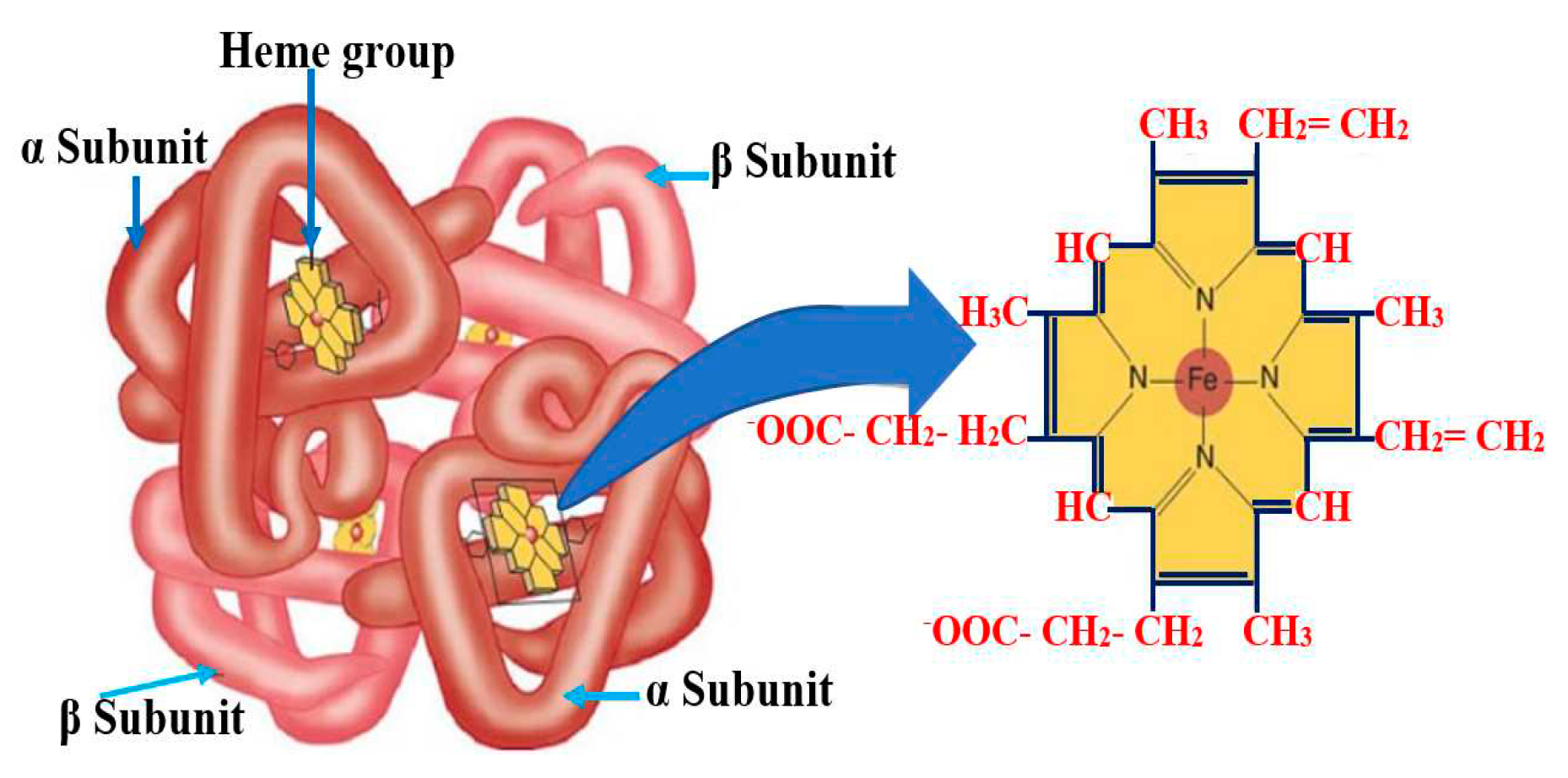
In the composition of red blood cells, there is include hem pigment, the porphyrin type that may combine with metal atoms. Hem in humans is protoporphyrin IX in combination with Fe. Hem has 4 pyrol nucleus linked together by the menten bridge (-CH=). Porphyrin rings are attached to the groups as: metyl (-CH3) at the sites 1, 3, 5, 8; vinyl (-CH=CH2) at the sites 2, 4; propionyl (-CH2 - CH2 - C00H) at the sites 6, 7.
Within heme, the iron atom is attached to the pyrrole nucleus by two symmetrical and two coordinated links, as well as to the protein globin through a histidine residue at the base. These bonds are crucial for the functioning of hemoglobin (Hb) (
Figure 1), as they help to stabilize the structure and allow for the reversible binding of oxygen.
Figure 1.
Chemical formular and structure of Isoleucine and Hemoglobin – the nucleus of red blood cells.
Figure 1.
Chemical formular and structure of Isoleucine and Hemoglobin – the nucleus of red blood cells.
Figure 2.
Absorption spectrum of red blood cells [
13].
Figure 2.
Absorption spectrum of red blood cells [
13].
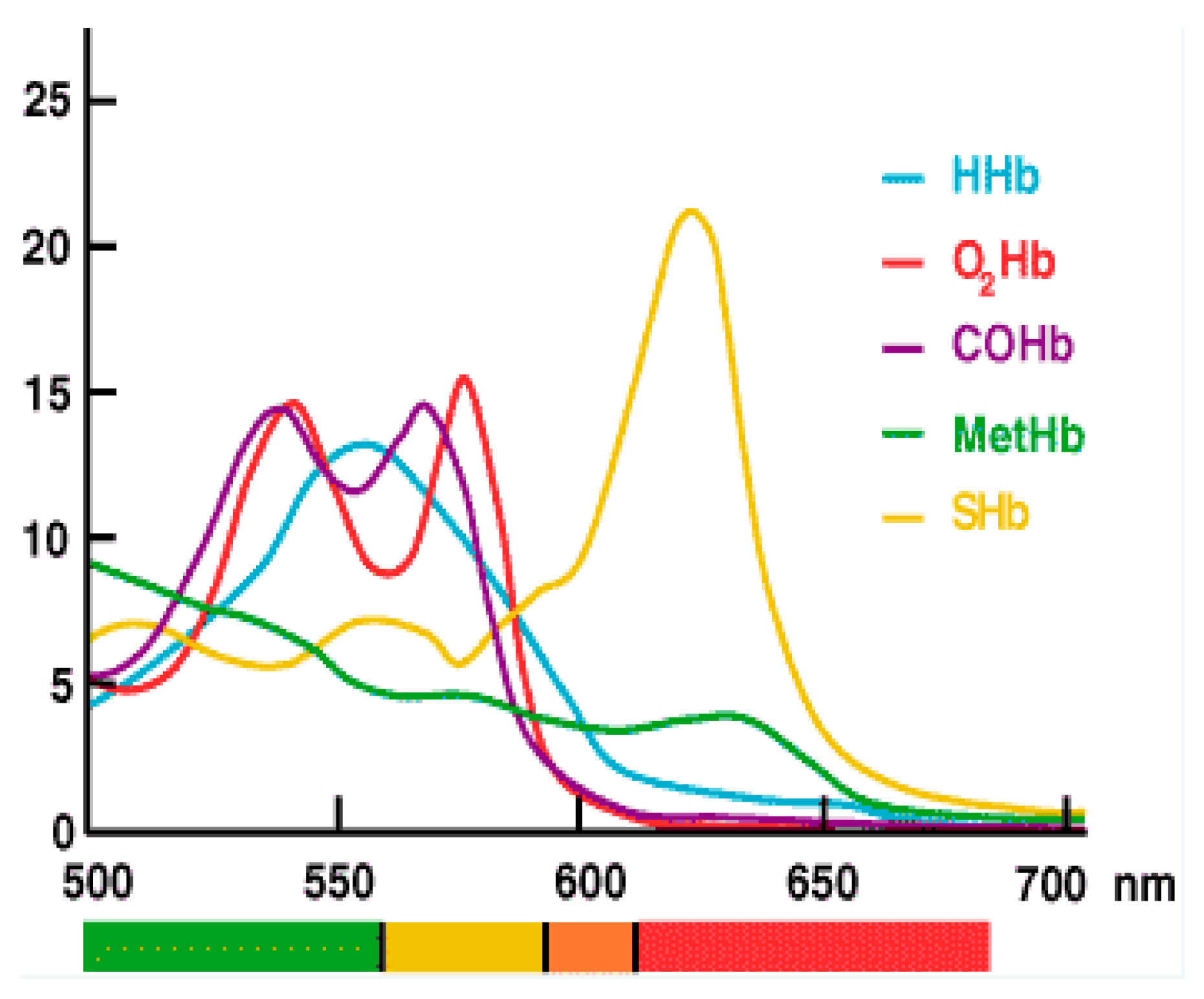
Each Hb molecule consists of four hemes, with one heme containing 1 Fe
++. Spectrometry analysis of blood reveals the maximum absorption spectrum within the 540-700 nm region, with maximum absorbance of SHb component at 622.8 nm [
11]. Human blood with a hematocrit of 10% and oxygen saturation of 98% displays optical properties of 0.210 ± 0.002 mm
-1 for μa, 77.3 ± 0.5 mm
-1 for μs, and 0.994 ± 0.001 for the G factor [
14]. As hematocrit increases up to 50%, there is a linear increase in absorption and a decrease in scattering. Variations in osmosis and wall cutting speed affect all three parameters, while oxygen saturation has a significant impact solely on the absorption coefficient. Measurements of oxidized and de-oxidized blood absorption spectra in the 400-2500 nm wavelength range demonstrate that blood absorption follows that of hemoglobin and water. The scattering factor for λ = 500 nm reduces to approximately 1.7, and the g coefficient is 0.9 higher for the entire wavelength range [
15].
2.3. Techniques
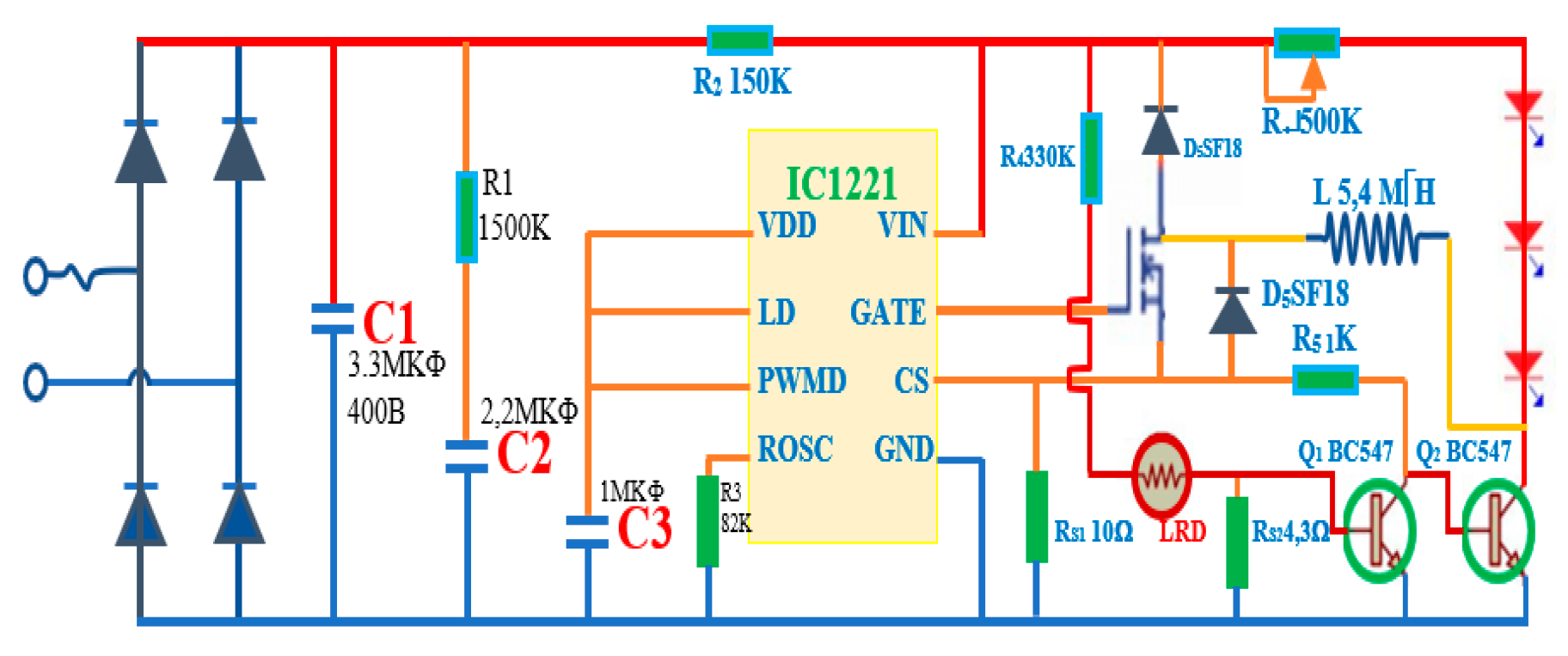
Analysis of circuit components, electronic devices.
Determine the physical parameters of the device by modern measuring devices and reliable devices (Kyoritsu 1052 - Japan, Lux Meter Testo 0500 - the USA, Testo 608-H2-US electronic thermometer, ...).
2.4. Fabrication Design
Component selection: RED LIGHT LED Chip, IC Stable Pressure and Line Stabilization, ...
Line stabilization circuit design for LED:
Figure 3.
Current stabilizer circuit for LED and Sensor.
Figure 3.
Current stabilizer circuit for LED and Sensor.
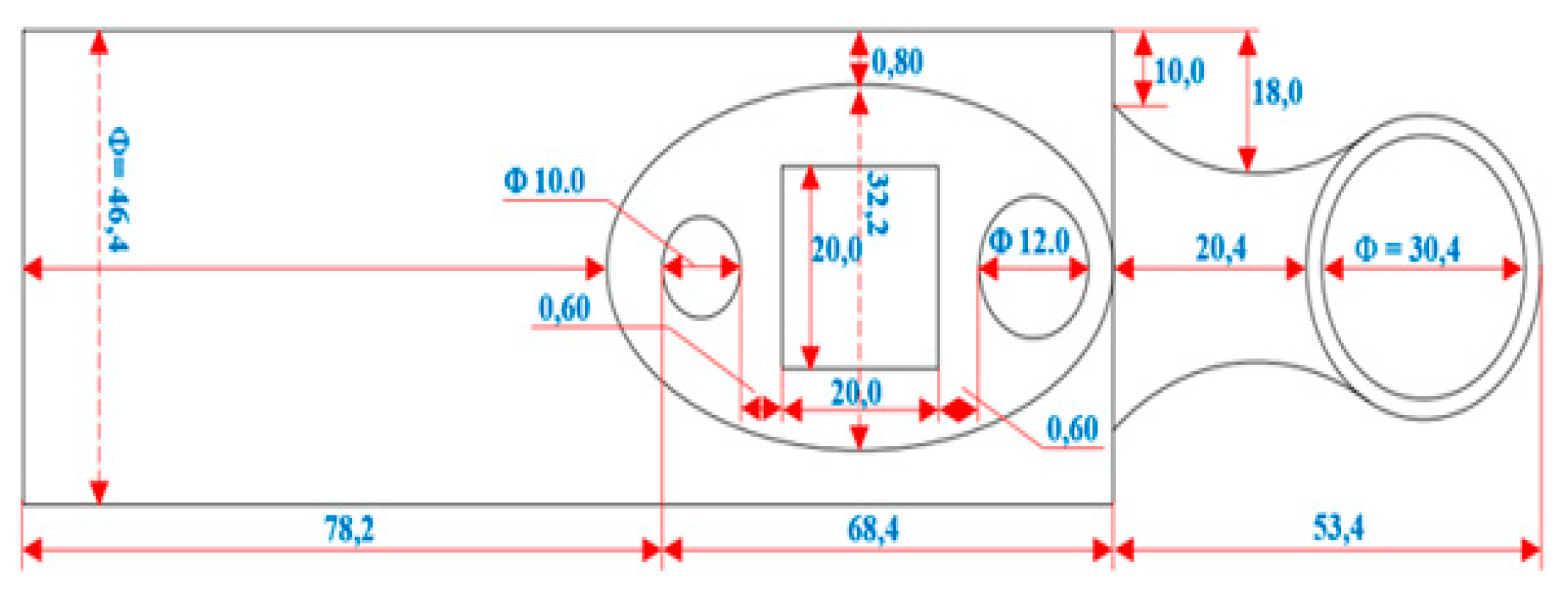
Equipment shell:
Figure 4.
Device shell scheme. Device case: Aluminum; Projector material: Hard plastic; Projector diameter: Φ=32.90 mm; Projector length: 34.50 mm; Device size: 200.00 x38.20 x50.06 mm.
Figure 4.
Device shell scheme. Device case: Aluminum; Projector material: Hard plastic; Projector diameter: Φ=32.90 mm; Projector length: 34.50 mm; Device size: 200.00 x38.20 x50.06 mm.
2.5. Measurement Process
Experiment 1: After designing and testing the elements of the device, the equipment is assembled according to the design scheme, then the basic electrical parameters of the BKA-06 (voltage, current intensity when operating) are measured using a universal meter (Kyoritsu 1052 - Japan) and some other indicators.
Experiment 2: Survey the parameters of BKA-06: measure the brightness intensity on three modes of the device (start, shallow test, deep test) and check the heat increase of the device in the screening area for a period of 1 to 25 minutes.
Experiment 3: Screening of BKA-06 on the surface of the hands of adults and children.
Experiment 4: Use BKA-06 to identify position on volunteers and breast cancer patients, then test with MRI.
3. Results
3.1. Studies of Basic Parameters of BKA-06
3.1.1. Device Specifications
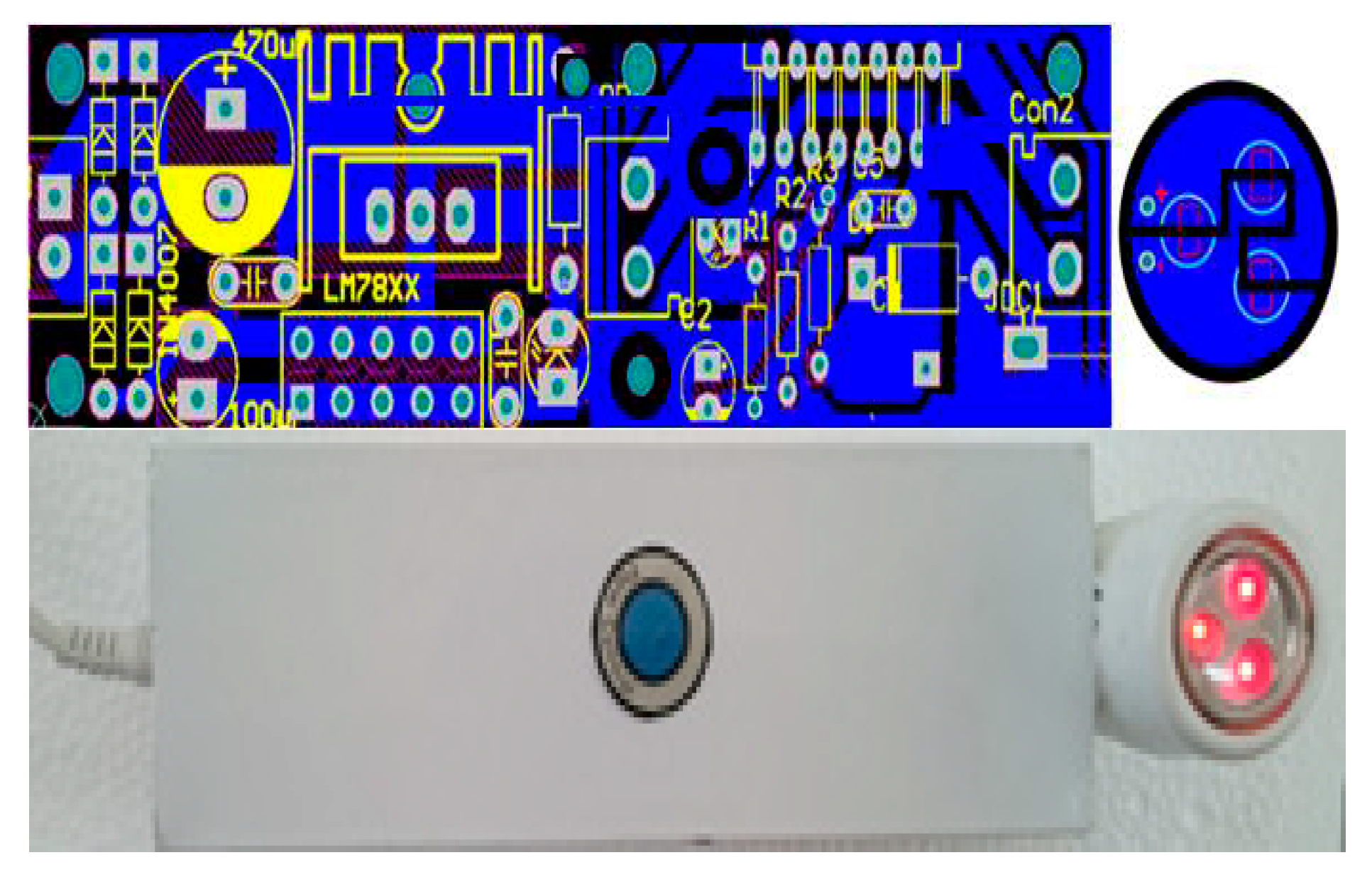
Figure 5.
Printed circuit scheme (above) and BKA-06 (below).
Figure 5.
Printed circuit scheme (above) and BKA-06 (below).
Specifications:
Power supply: 220V ~ 50Hz
Power Consumption: 12.19W
Dimensions: 210.08 x 41.22 x 50.08 mm; Φ 32.92 ± 0.02 mm (use caliper, micrometer)
Weight: 892 g
The ability to penetrate the layers of tissue on the breast is: 15 cm
Device BKA-06 (Early vein detection and breast cancer detection device by energy spectrum) has been licensed by metrology institute - Vietnam Academy (Attached to certificate N0): V11.CN6.300.23
3.1.2. Measure Brightness
Using the Lux Meter (Testo 0500-USA) and Multimeter (kyoritsu 1062- Japan), place the sensor head of the lux meter close to the header of the BKA-06 equipment, measure the brightness intensity in different changing modes.
Table 1.
Result of measuring device power and illuminance.
Table 1.
Result of measuring device power and illuminance.
Amperage
I(A) |
voltage U(V) |
power P(W) |
Lux (lx) |
| 3,02 |
0,75 |
2,27 |
3447 |
| 3,06 |
0,82 |
2,50 |
4157 |
| 3,14 |
0,90 |
2,82 |
5276 |
| 3,26 |
1,00 |
3,25 |
7014 |
| 3,35 |
1,10 |
3,68 |
9013 |
| 3,45 |
1,21 |
4,17 |
11693 |
| 3,55 |
1,33 |
4,73 |
14888 |
| 3,65 |
1,46 |
5,35 |
19234 |
| 3,75 |
1,61 |
6,04 |
24378 |
| 3,85 |
1,77 |
6,81 |
30978 |
| 3,95 |
1,94 |
7,67 |
39268 |
| 4,05 |
2,13 |
8,63 |
49656 |
| 4,15 |
2,33 |
9,69 |
62546 |
| 4,25 |
2,56 |
10,87 |
78768 |
| 4,35 |
2,80 |
12,19 |
98592 |
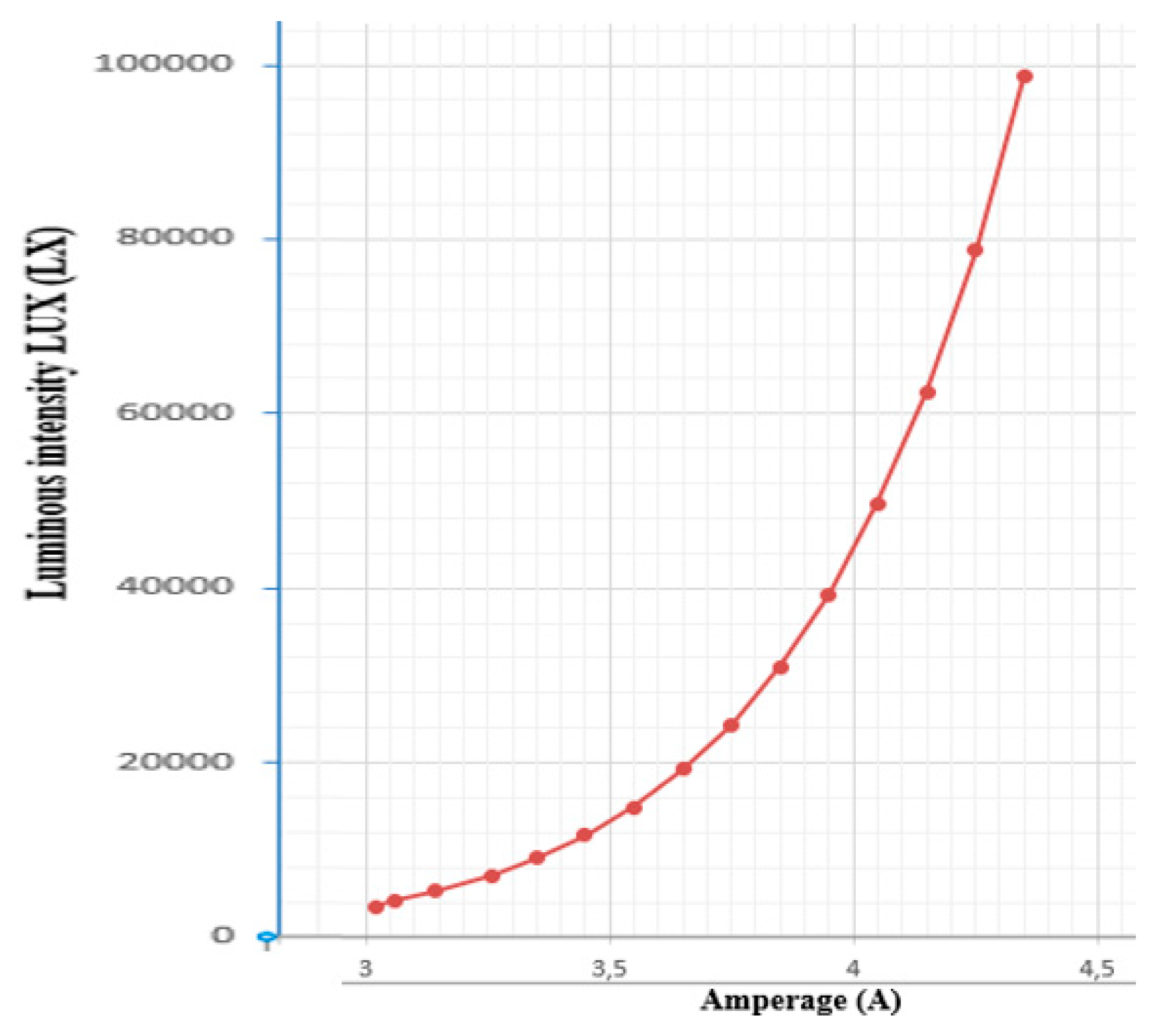
Figure 6.
Relationship between amperage and illuminance.
Figure 6.
Relationship between amperage and illuminance.
The survey results show that the amperage reaches 0.75÷2.80 (A), the maximum power consumption is 12.19W, the illuminance increases from 3,447÷98,592(lx). With illuminance from 3,447 ÷14,888lux, which is bright enough to examine capillaries close to the skin, this mode is suitable for superficial tumor surfacing or vascular endoscopic examination (Figures 7b, 7c). With illuminance from 19,234 to 62,546 lux, suitable for endoscopic examination of tumors, superficial subcutaneous lymph nodes (neck, nasopharynx, breast), this mode has a penetration depth of about 3÷ 7cm (Figure 7a). The illuminance from 62,546÷98,592lux is suitable for endoscopic mode, deep lymph nodes under the skin of the breast 7 ÷ 15 cm are suitable for breast cancer diagnosis.
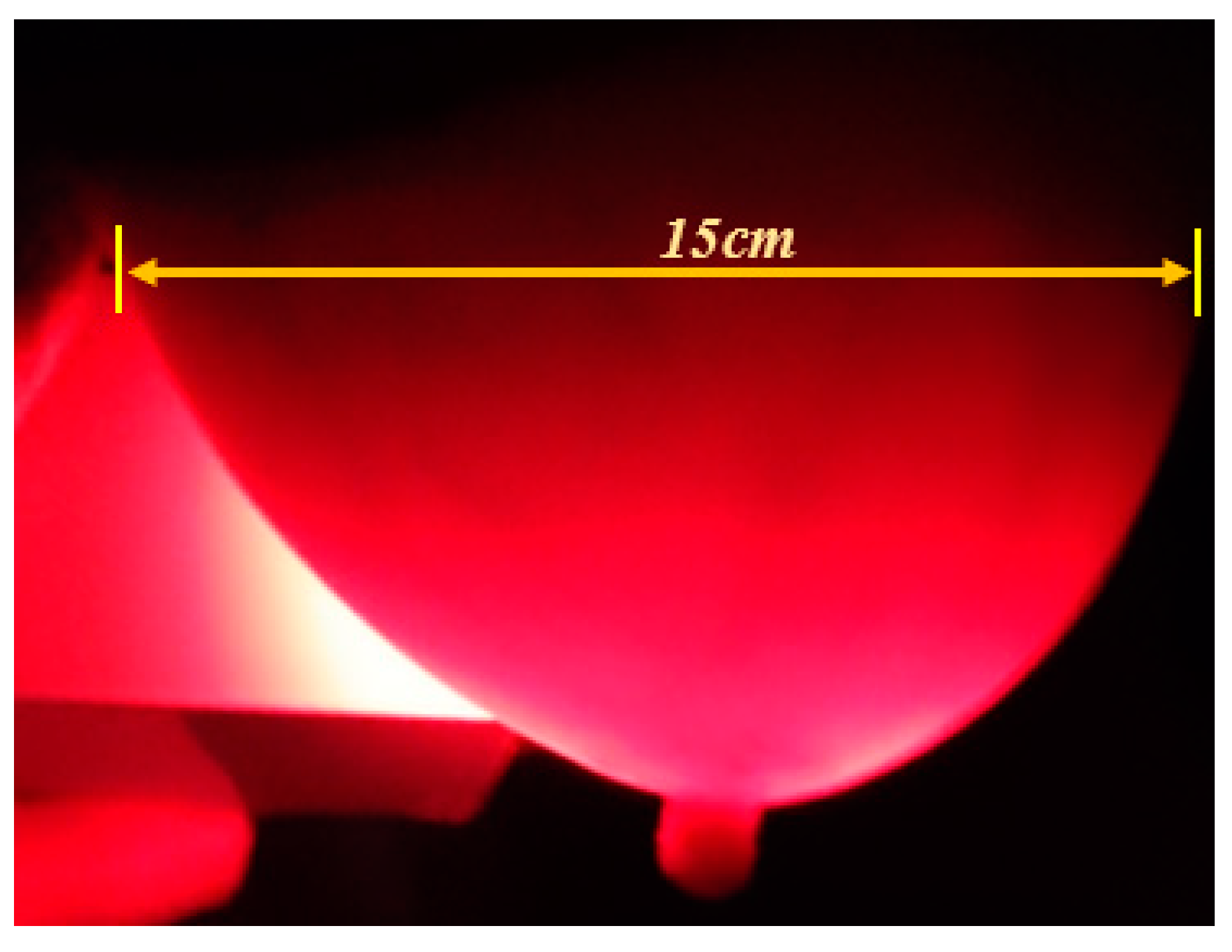
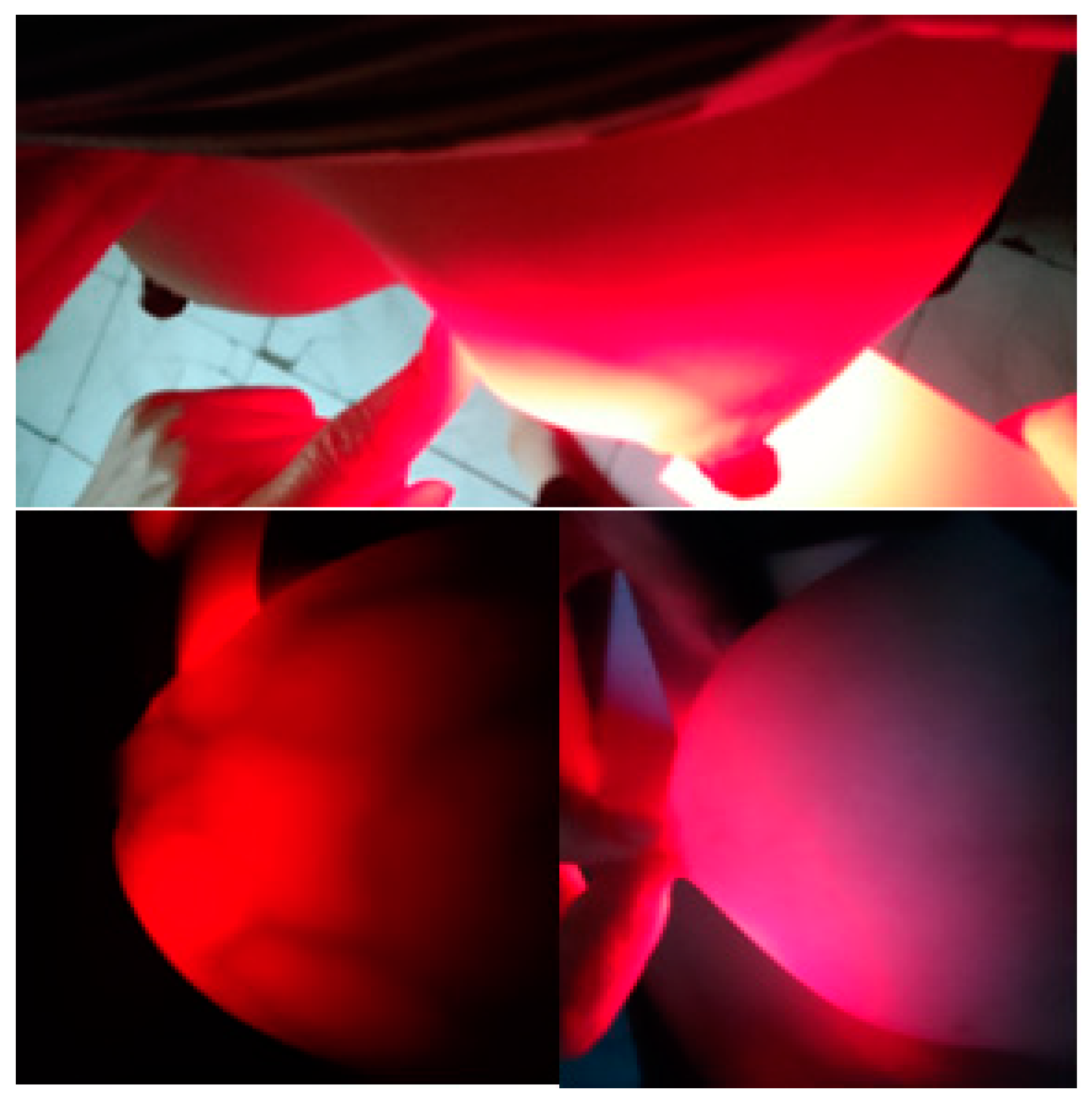
Figure 7a.
BKA-06 equipment image that scans through layers of adult breast tissue.
Figure 7a.
BKA-06 equipment image that scans through layers of adult breast tissue.
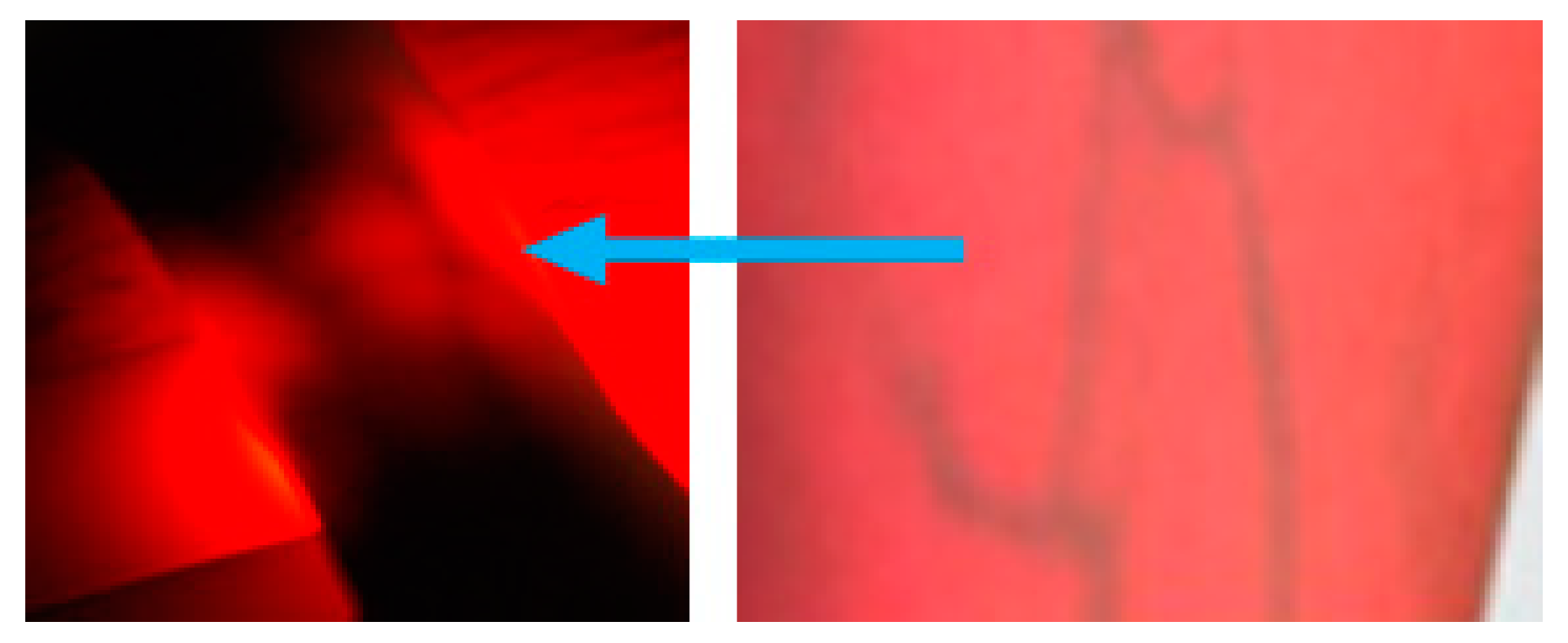
3.2. Vascular Results in Adults and Children
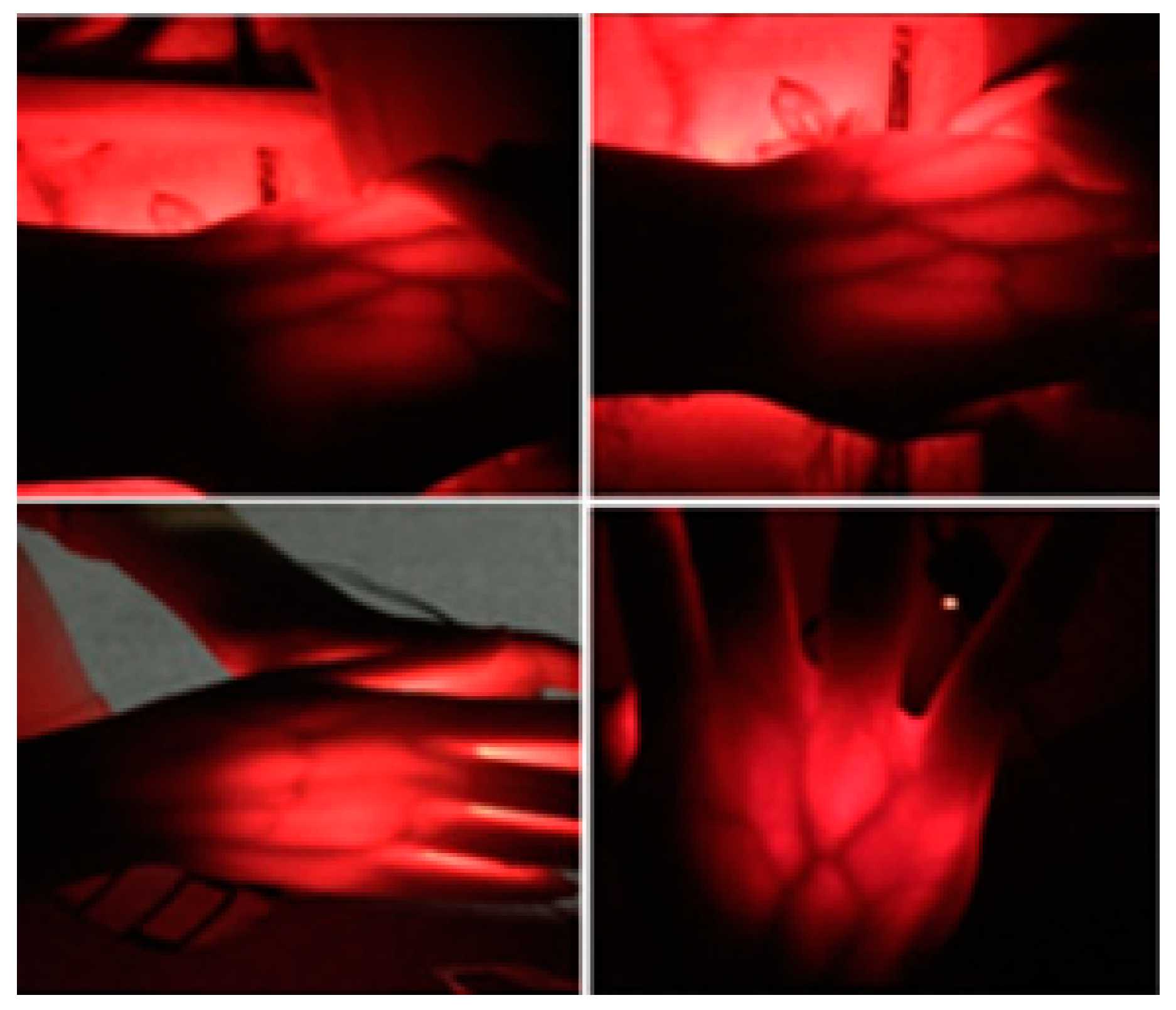
- Angiogram of blood vessels on the hands (on 06 adults) at Figures 7b and 7c.
Figure 7b.
Vascular screening on the surface of an adult's arm using a BKA-06 equipment.
Figure 7b.
Vascular screening on the surface of an adult's arm using a BKA-06 equipment.
Figure 7c.
Vascular screening on an adult's hand using BKA-06 equipment.
Figure 7c.
Vascular screening on an adult's hand using BKA-06 equipment.
Figure 7d.
Vascular screening on the children's hands using BKA-06 equipment.
Figure 7d.
Vascular screening on the children's hands using BKA-06 equipment.
The obtained results show that the images of the blood vessels under the skin are very clear and their positions are easily recognized with the naked eye.
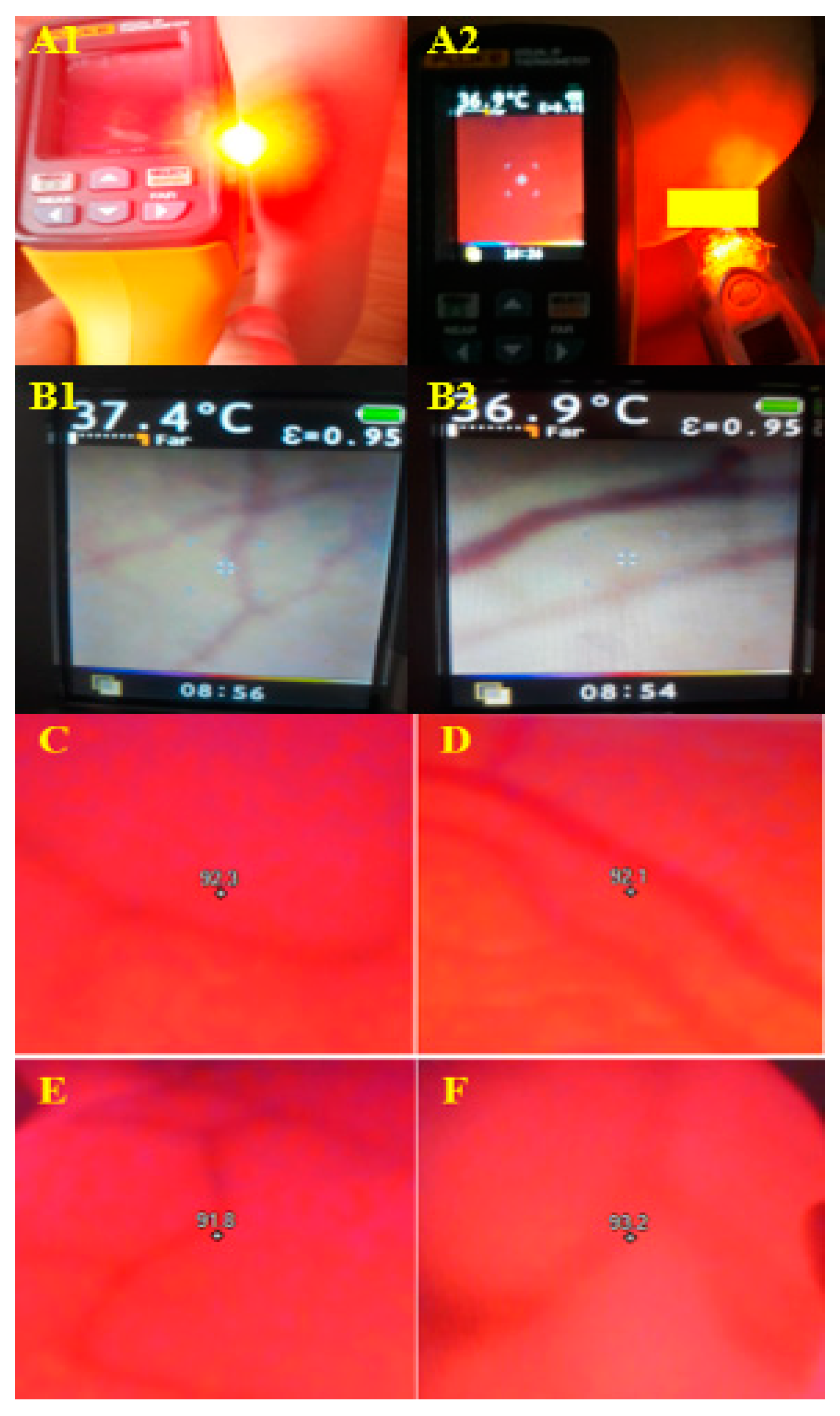
Figure 7e.
The thermal images of blood vessels illuminated by BKA-06 on: (A1, B1, C, D) children's forearm, (A2, B2, E, F) adult's breast.
Figure 7e.
The thermal images of blood vessels illuminated by BKA-06 on: (A1, B1, C, D) children's forearm, (A2, B2, E, F) adult's breast.
The results obtained show that the images of blood vessels under the skin are very clear and easily identifiable with the naked eye when using the BKA-06 device. Because the BKA-06 device heats the area for imaging, the thermal camera also provides clear images of the blood vessel locations. Additionally, for blood vessels located deeper under at 2 cm to 3 cm, heating with the BKA-06 also yields images with clearer contrast of the blood vessels on the thermal camera. The comparison of the images clearly indicates that the contrast of blood vessel images by the BKA-06 is more distinct.
3.3. Breast Test Results on Volunteers and Patients
3.3.1. Volunteers
Volunteers were randomly selected between the ages of 18 and 60 (never had breast cancer tested with any medical devices, no suspicious or conclusive signs of breast cancer). The initial scan results for
Figure 8 and
Figure 9,
Table 3.
Figure 8.
Breast Test Photos of Volunteer Do Kim Huyen.
Figure 8.
Breast Test Photos of Volunteer Do Kim Huyen.
Table 3.
List of volunteers for breast cancer screening (03/04 -28/05/2022).
Table 3.
List of volunteers for breast cancer screening (03/04 -28/05/2022).
| No. |
Full name |
Age |
Phone number |
Code |
| 1 |
Doan Ngoc Bich |
43 |
09835352XX |
CV1 |
| 2 |
Nguyen Kim Chi |
31 |
09048008XX |
CV2 |
| 3 |
Cao Thi Hanh |
28 |
09848714XX |
CV3 |
| 4 |
Pham My Hanh |
41 |
09048008XX |
CV4 |
| 5 |
Do Thi Hinh |
55 |
09155086XX |
CV5 |
| 6 |
Le Thi Hoan |
30 |
019829222XX |
CV6 |
| 7 |
Do Thi Hong |
60 |
09123723XX |
CV7 |
| 8 |
Nguyen Thu Huong |
40 |
09685381XX |
CV8 |
| 9 |
Do Kim Huyen |
65 |
09898389XX |
CV9 |
| 10 |
Trinh Thi Oanh |
40 |
09830519XX |
CV10 |
| 11 |
Nguyen Thuy Quynh |
18 |
012734500XX |
CV11 |
| 12 |
Nguyen Thi Thuy |
42 |
09767644XX |
CV12 |
| 13 |
Doan Thanh Thuy |
36 |
09832868XX |
CV13 |
| 14 |
Do Kieu Trang |
25 |
01635421XX |
CV14 |
| 15 |
Pham Thi My Hanh |
58 |
09836080XX |
CV15 |
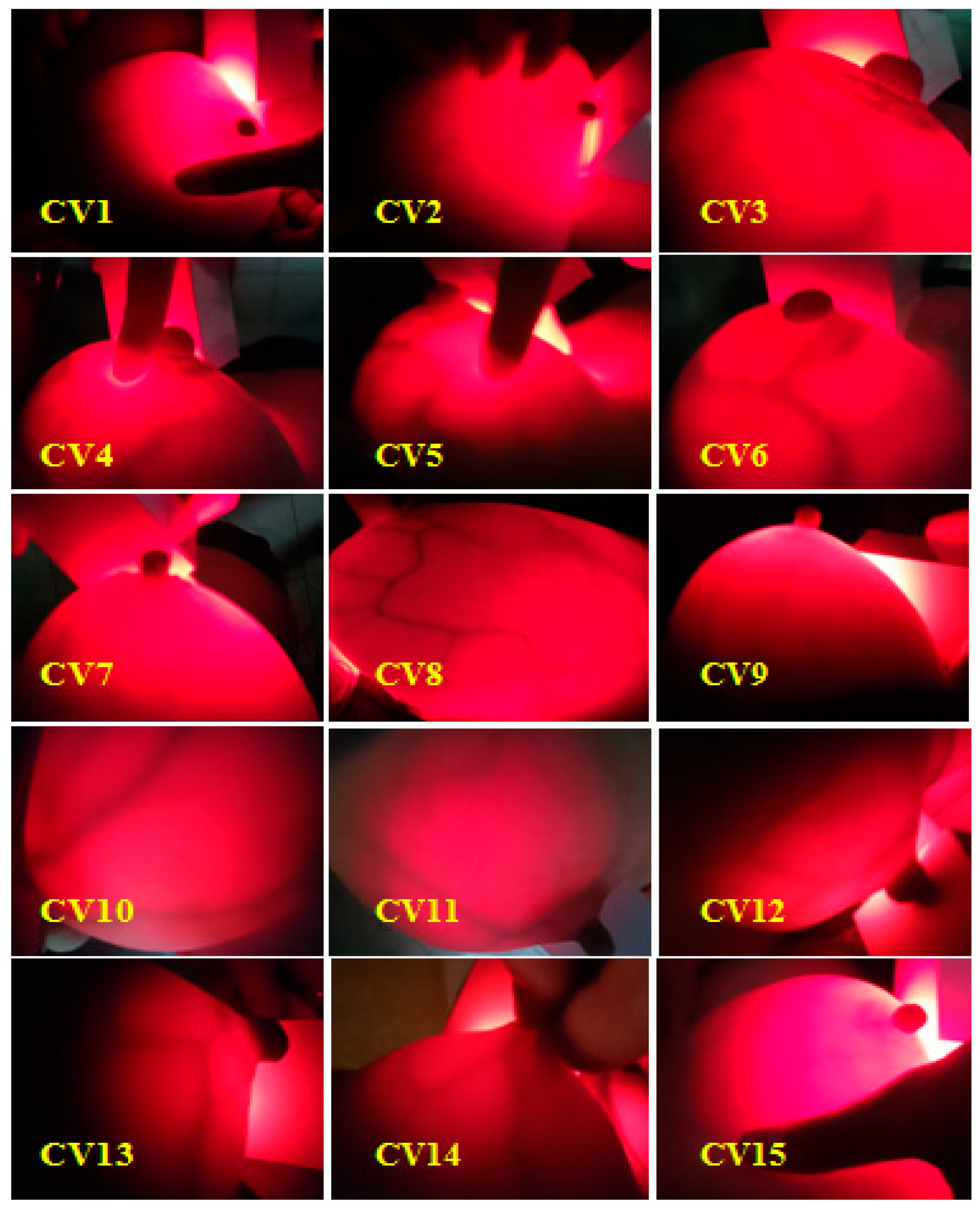
Figure 9.
Summary of breast cancer test results using BKA-06 device.
Figure 9.
Summary of breast cancer test results using BKA-06 device.
Figure 10 clearly shows the non-screening area and the scanning area. At the illuminated are we observe with the eye sees the mammary gland blood vessels with a dark red color, with the appropriate brightness intensity we can observe the layers of breast tissue. Therefore, no need for an infrared camera auxiliary device to connect a computer to simulate the image, we can also see the inside image of the breast when using used equipment.
Figure 10.
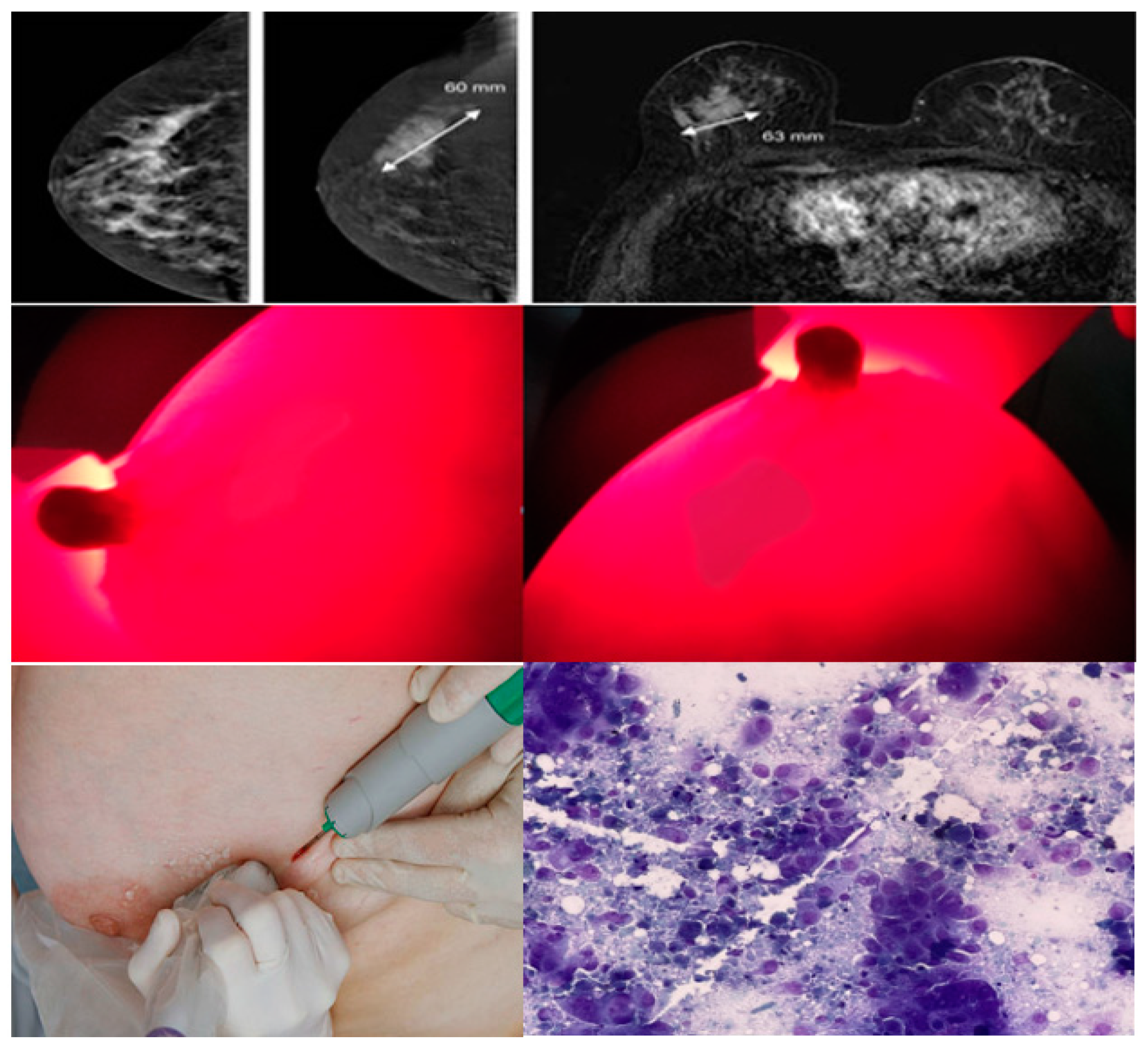
Image MRI scans, BKA-06 and cell biopsies of breast cancer patients Nguyen Thi N.
Figure 10.
Image MRI scans, BKA-06 and cell biopsies of breast cancer patients Nguyen Thi N.
The results of breast cancer screening with the BKA-06 device on 15 volunteers showed quality images, observed with the naked eye, the mammary glands, blood vessels are very clear, no abnormal organization, no lymphoma.
3.3.2. Patient Participation
Twelve (12) patients who took part in the scan had abnormal breast abnormalities. Two MRI patients found to have tumors then had breast cancer scans using BKA-06 devices, the rest were clinically examined suspected that the tumor had an MRI scan (appendix I), conducted a BKA-06 scan, MRI scan and cell biopsies. Result:
+ Patient profile: Nguyen Thi N, 58.
Profile number: 7673/20. Address – Nguyen An Ninh - Hai Ba Trung -Hanoi. Diagnose: Mammary tumor (T), ize 60 x 63mm, middle tumor in the breast (T), non-mobile soft tumor (Δ(t): Left mammary K (T) T
4N
0M
0. GTB UT GDII). The MRI image showed the tumor, location, and size of 60x63 mm of these images taken after the photoreceptor injection and through a computer simulation system. Observing two perpendicular images from the BKA-06 device, we also see that the tumor area is darker than the area around the tumor, especially the border area is very clear, so it is easy to recognize the shape of the tumor's position and size. Because the device has not integrated the computer, the tumor size on the image of BKA-06 is not quantized, but through the naked eye, we also estimate the size of the tumor. The result is in
Figure 10.
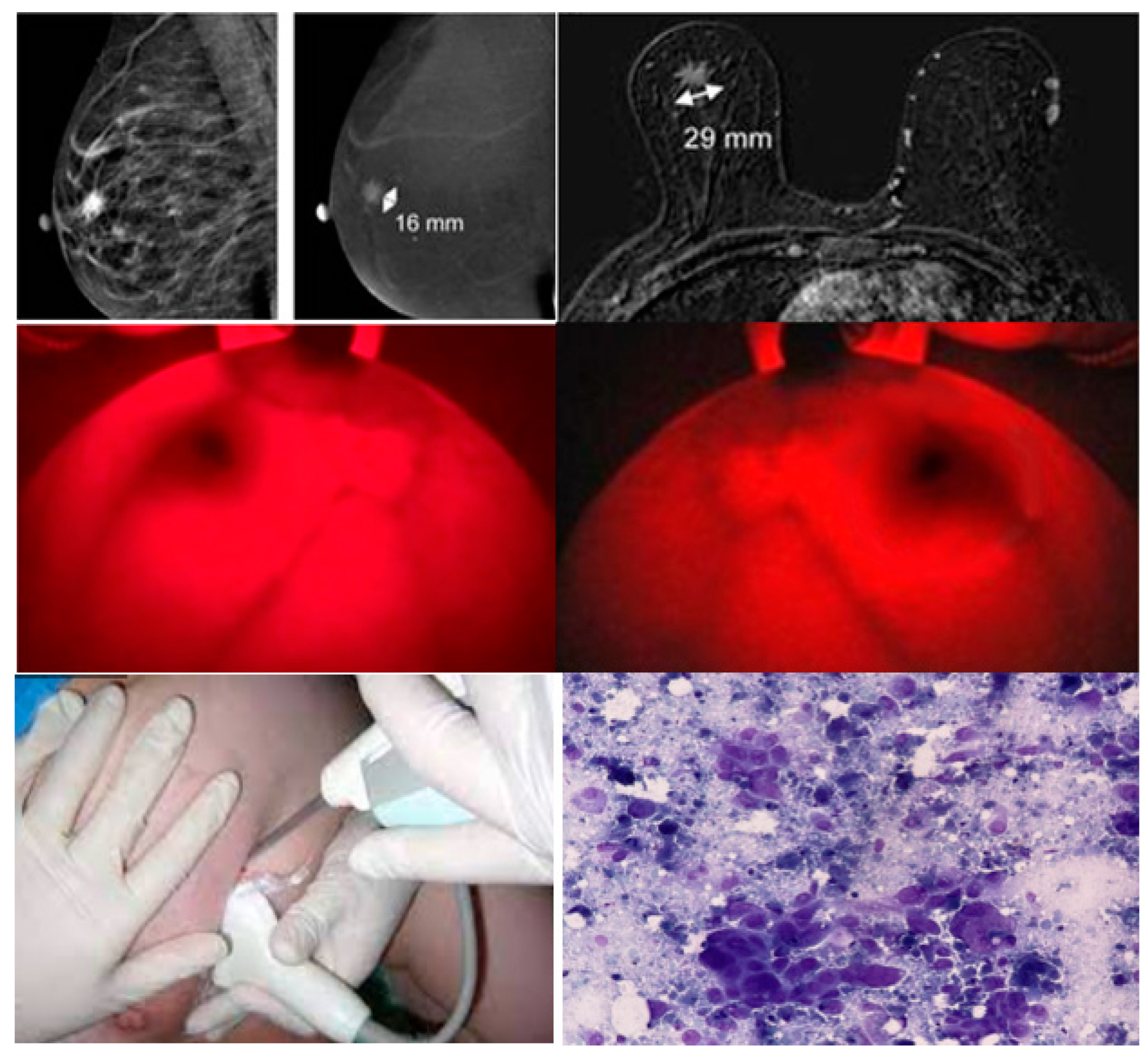
+ Patient profile: Vu Thi L, 64. Profile number: 7692/20. Address - Nghèn Town, Cam Loc, Ha Tinh. Diagnose: Mammary tumor (T), size 16 x 29mm, Inner protrusive bottom (T), I am probably not mobile (Δ (t): Left mammary gland (T) T4N0M0. GTB UT GDII). Results of MRI scans, BKA-06 and cell biopsies in Figure 11.
Figure 12.
Image MRI scans, BKA-06 and cell biopsies of breast cancer patients Vu Thị L.
Figure 12.
Image MRI scans, BKA-06 and cell biopsies of breast cancer patients Vu Thị L.
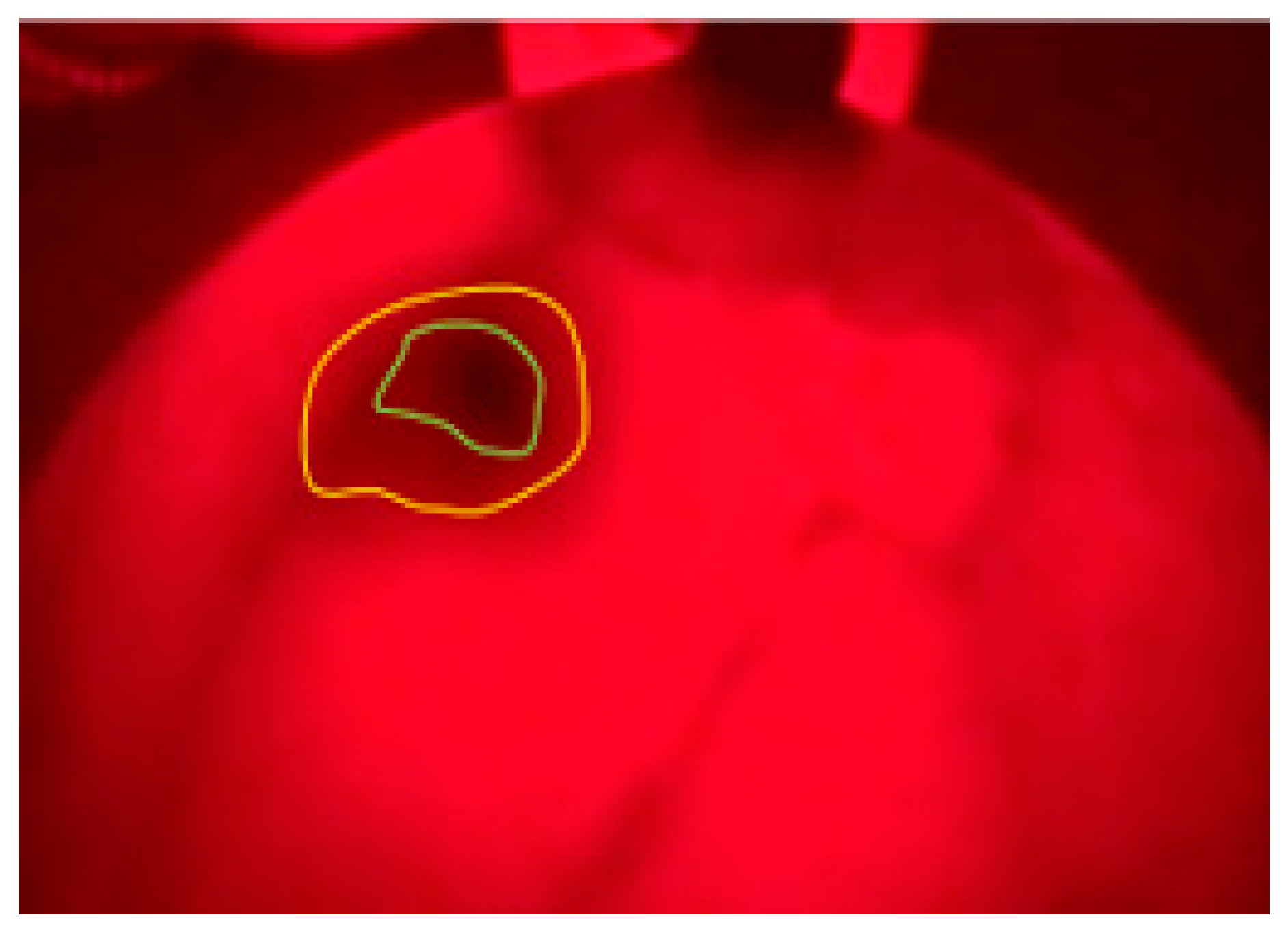
Similar to patient Nguyen Thu N, the images were taken on the disease give clearer and darker images (it may be because one patient has a different type, solid lymph nodes according to the results of clinical examination) we observe the depth of the tumor, the area around the tumor (yellow vinculum) develops many capillary organizations so it is darker than the middle area tumor center (blue vinculum
Figure 13). Cell biopsy results showed melanoma. The results on the MRI show the location and size of the tumor (16x29 mm).
Figure 13.
BKA-06 image of patient Vu Thi M.
Figure 13.
BKA-06 image of patient Vu Thi M.
The results of BKA-06, MRI and cell biopsies are summarized in
Table 4, Figure 14. Observation on the images taken on BKA-06 shows that the location and size of the tumor is very clear and shallow. depth or same cell density
Table 4.
List of breast cancer test patients (04/2022 - /12/2022).
Table 4.
List of breast cancer test patients (04/2022 - /12/2022).
| Number |
Full name |
Age |
Encrypted image |
| 1 |
Hoang Thi Thuy Ch |
25 |
UHV1 – MRI1 |
| 2 |
Dang Thu B |
67 |
UHV1 – MRI2 |
| 3 |
Doan Thi D |
45 |
UHV3 – MRI3 |
| 4 |
Hoang Thi H |
65 |
UHV4– MRI4 |
| 5 |
Le Thi To H |
45 |
UHV5– MRI5 |
| 6 |
Nguyen Thi H |
58 |
UHV6– MRI6 |
| 7 |
Vu Thi L |
64 |
UHV7– MRI7 |
| 8 |
Le Thi L |
52 |
UHV8– MRI8 |
| 9 |
Vu Thi Kim O |
46 |
UHV9– MRI9 |
| 10 |
Nguyen Thi Q |
43 |
UHV10– MRI10 |
| 11 |
Ta Thi Thanh Th |
59 |
UHV11– MRI11 |
| 12 |
Pham Thi Y |
58 |
UHV12– MRI12 |
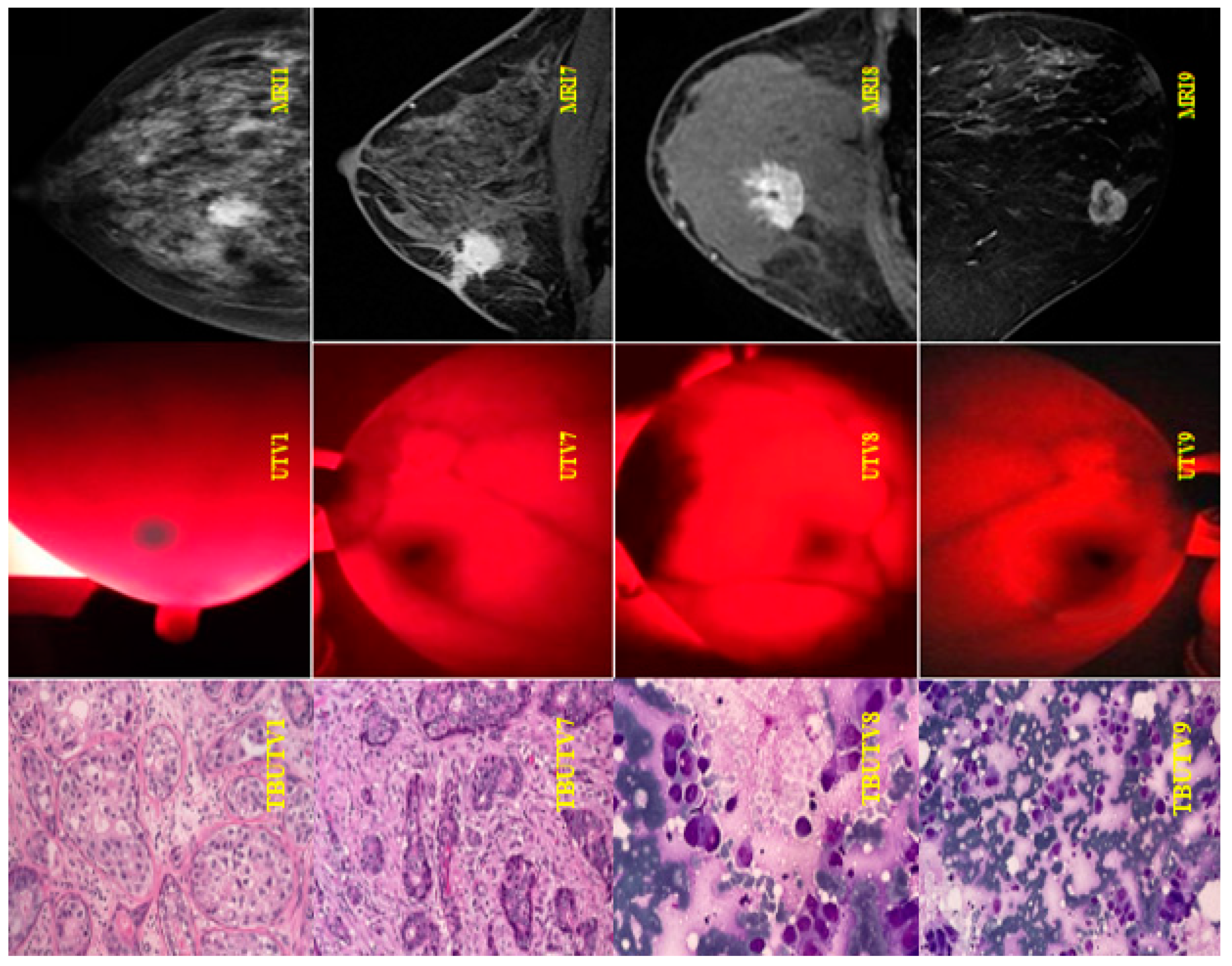
The results of MRI scans, BKA-06 and cell biopsies showed the summary on
Table 4,
Figure 15. Observations on the images taken on the BKA-06 show that the location and size of the tumor are very clear the depth or density of cells and the internal environment in and out of the typical tumor in patients UHV1, UHV7, UHV8, UHV9. On the other hand, breast MRI images on the upper patients also show the location and size of the tumor for the same result as BKA-06. The advantage is that the penetrating image compared to the black and white image on the MRI is recommended to observe the tumor boundary area.
Figure 15.
Image of MRI scans, BKA-06 and cell biopsies of breast cancer patients.
Figure 15.
Image of MRI scans, BKA-06 and cell biopsies of breast cancer patients.
4. Discussions
The BKA-06 device takes 2D, 3D images of the screening area on the body. Visually observing with the naked eye into the image, we can have seen some of the structures inside the skin that are layer-by-layer vascular systems in depth [
16,
17,
18]. For breast tumors, it is also close to the location, size, and invasive areas around the tumor.
The device has the advantage of simple structure, easy to use, clear images can be observed with the naked eyes. The area of light emitted in the red area of the spectrum is not harmful to the eyes or skin, because infrared lights are used in the treatment of skin diseases in the cosmetic industry and other areas in health.
The initial results of the successful manufacture of BKA-06 and some potential results can upgrade to create new essential products for the medical industry, improving the quality of infusions and blood draws.
BKA-06 is specialized for a blood angiogram of shallow tumors. There are outstanding advantages when it comes to breast scans compared to CT scan or MRI methods: Without photovoltaic injections, the 3÷5minutes scan time (CT scan, MRI 25÷30 minutes) costs an estimated 7 ÷ 9 million so if the cost of a test is negligible compared to the MRI (2.3 ÷ 2.8 million / 1 degree), The patient can take a selfie and easy to see their result, easy-to-use.
BKA-06 has not been able to capture internal organs, deeper locations, bone organizations, that can be taken by MRI or CT scans
The thesis successfully designed BKA-06 and initially achieved some good results that can upgrade to create new essential products for the medical industry, improve diagnostic methods for medical facilities on domestic and international.
Imaging method based on the principle of energy absorption of the mass is a new method in diagnostic imaging, both in the world and in Vietnam, so this study could help to access and update in research and application in other industries. The subject's BKA-06 device also expected superior applications with other diagnostic methods. The BKA-06 device also expected to have applications that are superior to reality.
5. Conclusions
In short, we successfully designed and fabricated equipment (BKA-06) with basic specifications: Power Consumption of 12.19W, size of 210.08 x 41.22 x 50.08 mm; Φ 32.92 ± 0.02 mm; weight of 892 g. The device is of capability to penetrate the layers of tissue on the breast up to 15 cm. BKA-06 does not burn on the screening part, emits red light (the main wavelength of 633nm is healthy radiation, does not cause side effects), there are three screening modes, maximum brightness intensity 98238 lux, inspection time 3 ÷ 5 minutes, the image is close to the naked eye. Surveyed safety specifications when using the device in various modes (starting, shallow test, and deep test mode) in venipuncture, as well as breast scan examination. We have successful tested on volunteers and patients gives very good initial results: XCS observations identifies blood vessels, tumors in the breast, and surrounding organizations very clearly to determine the location, size of the tumor, the area around the tumor directly without surgery or other diagnostic methods. A parallel examination on the MRI and cell biopsies with reliable results.
Author Contributions
Conceptualization, H.T.M and D.D.L; methodology H.T.M; software, D.Q.N; validation, H.T.M and H.P.N.T.; formal analysis H.P.N.T.; investigation, H.P.N.T..; resources, D.Q.N; data curation, D.Q.N.; writing—original draft preparation H.T.M and D.D.L; writing—review and editing, H.T.M and D.D.L; visualization, H.T.M and D.D.L; supervision, H.T.M and D.D.L; project administration, H.T.M and D.D.L; funding acquisition, H.T.M. All authors have read and agreed to the published version of the manuscript.” Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding
This research was funded by Vietnam Ministry of Education and Training, grant number: B2021-BKA-06.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Duong Thi Tuan, Anh. ""Assessment of the actual situation of performing intravenous injection procedures by nurses in construction hospitals." (2011), trang 6-11, 13-20.
- Dang Thi Thanh, Thuy. ““Knowledge, skills to practice safe injection and some related factors of students at Kon Tum medical secondary school in 2016.” (2016), trang 12-14.
- E. Heer, A. Harper, N. Escandor, H. Sung, V. McCormack, M.M. Fidler-Benaoudia, Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study, The Lancet. Global health, 8 (2020) e1027-e1037. [CrossRef]
- B.O. Anderson, A.M. Ilbawi, E. Fidarova, E. Weiderpass, L. Stevens, M. Abdel-Wahab, B. Mikkelsen, The Global Breast Cancer Initiative: a strategic collaboration to strengthen health care for non-communicable diseases, The Lancet. Oncology, 22 (2021) 578-581. [CrossRef]
- F. Bray, J. Ferlay, I. Soerjomataram, R.L. Siegel, L.A. Torre, A. Jemal, Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries, CA: a cancer journal for clinicians, 68 (2018) 394-424. [CrossRef]
- A. Migowski, Early detection of breast cancer and the interpretation of results of survival studies, Ciencia & saude coletiva, 20 (2015) 1309.
- Breast cancer. Early detection and prompt treatment are critical, Mayo Clinic health letter (English ed.), Suppl (2001) 1-8.
- T. Onega, L.E. Goldman, R.L. Walker, D.L. Miglioretti, D.S. Buist, S. Taplin, B.M. Geller, D.A. Hill, R. Smith-Bindman, Facility Mammography Volume in Relation to Breast Cancer Screening Outcomes, Journal of medical screening, 23 (2016) 31-37. [CrossRef]
- T.C. Lewis, V.J. Pizzitola, M.E. Giurescu, W.G. Eversman, R. Lorans, K.A. Robinson, B.K. Patel, Contrast-enhanced Digital Mammography: A Single-Institution Experience of the First 208 Cases, The breast journal, 23 (2017) 67-76. [CrossRef]
- A.M. Hassan, M. El-Shenawee, Review of electromagnetic techniques for breast cancer detection, IEEE reviews in biomedical engineering, 4 (2011) 103-118. [CrossRef]
- P. Xu, Y. Peng, M. Sun, X. Yang, SU-E-I-81: Targeting of HER2-Expressing Tumors with Dual PET-MR Imaging Probes, Medical Physics, 42 (2015) 3260-3260. [CrossRef]
- J.M. Poneros, S. Brand, B.E. Bouma, G.J. Tearney, C.C. Compton, N.S. Nishioka, Diagnosis of specialized intestinal metaplasia by optical coherence tomography, Gastroenterology, 120 (2001) 7-12. [CrossRef]
- Higgins, C. (2005). Hemoglobin and its measurement. Hemoglobin.
- F. Chandra, A. Wahyudianto, M. Yasin, Design of vein finder with multi tuning wavelength using RGB LED, Journal of Physics: Conference Series, 853 (2017) 012019. [CrossRef]
- D. Grosenick, H. Rinneberg, R. Cubeddu, P. Taroni, Review of optical breast imaging and spectroscopy, Journal of Biomedical Optics, 21 (2016) 091311. [CrossRef]
- Delvo, Elaine D. "Implementa, on of Near--Infrared Technology (AccuVein AV--400®) To Facilitate Successful PIV Cannula, on.".
- Wang, Y.; Bower, B.A.; Izatt, J.A.; Tan, O.; Huang, D.(2008), “Retinalblood flow measurement by circumpapillary Fourier domain Doppler optical coherence tomography”. J. Biomed. Opt, 13. pp. 202-208. [CrossRef]
- International Journal Of Engineering, Education And Technology (ARDIJEET), ISSN 2320-883X, VOLUME
2 ISSUE 1, 01/01/2014 b/ British Journal of Anaesthesia 110 (6): 966–71 (2013) Advance Access publication 5
February 2013. doi: 10.1093 /bja/aet003 4. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).