Background
Atrial fibrillation (AF) is the most common cardiac arrhythmia, with a worldwide prevalence of ~38 million in 2017, and is associated with high mortality and morbidity rates(1).1 In adjusted models, AF is associated with increased morbidity (especially stroke and heart failure) and mortality(1).From a pathophysiological, epidemiological, diagnostic, and management perspective, the influence of gender on cardiovascular disease has been widely studied and described(2). In this regard, AF is not an exception, showing gender variations.
AF is more frequent in men than in women, with a global annual incidence per year of 77.5 cases per 100,000 population and 48.7 cases per 100,000 population, respectively(3). It is well known that AF has a greater impact on women morbidity and mortality. Compared to those without AF, women with AF have an approximately 3-fold higher risk of suffering a cardiovascular disease (CVD) related event (i.e., hospitalization or death) related to arrhythmia, while men have a 1.8-fold higher risk compared to the general men population(4).
Female sex is an independent risk factor for stroke(5). In the setting of AF, women have up to 1.3-fold higher risk of stroke and systemic embolism compared with men, even if they are treated with non-vitamin K antagonist oral anticoagulants (NOACs), and especially in those older than 75 years(6–8). Some authors have suggested gender-based differences in AF therapy. For example, it has been previously reported that, among patients showing atypical or asymptomatic presentations, conservative treatment is more frequently recommended for women, while rhythm control is more likely to be pursued in men(7,8). Kloosterman et al. reported that men have a greater probability of being treated with electrical cardioversion (ECV) and/or NOAC therapy, while women are more likely to be treated with only ß-blockers or calcium antagonists. Catheter ablation for AF also has been studied, showing that it is a more frequently used strategy in men, despite a similar benefit on quality of life scales between men and women(9). In women, systemic anticoagulation is used less often and, when administered, the therapy may be of lower quality, although the benefits of anticoagulation are higher in women(4,6,8).
Therefore, we carried out a comparison of the medical attention characteristics (main objective), clinical course, morbidity and mortality of patients attended at ED for an AF episode (index episode), stratified by gender.
Material and Methods
Study Design and Population
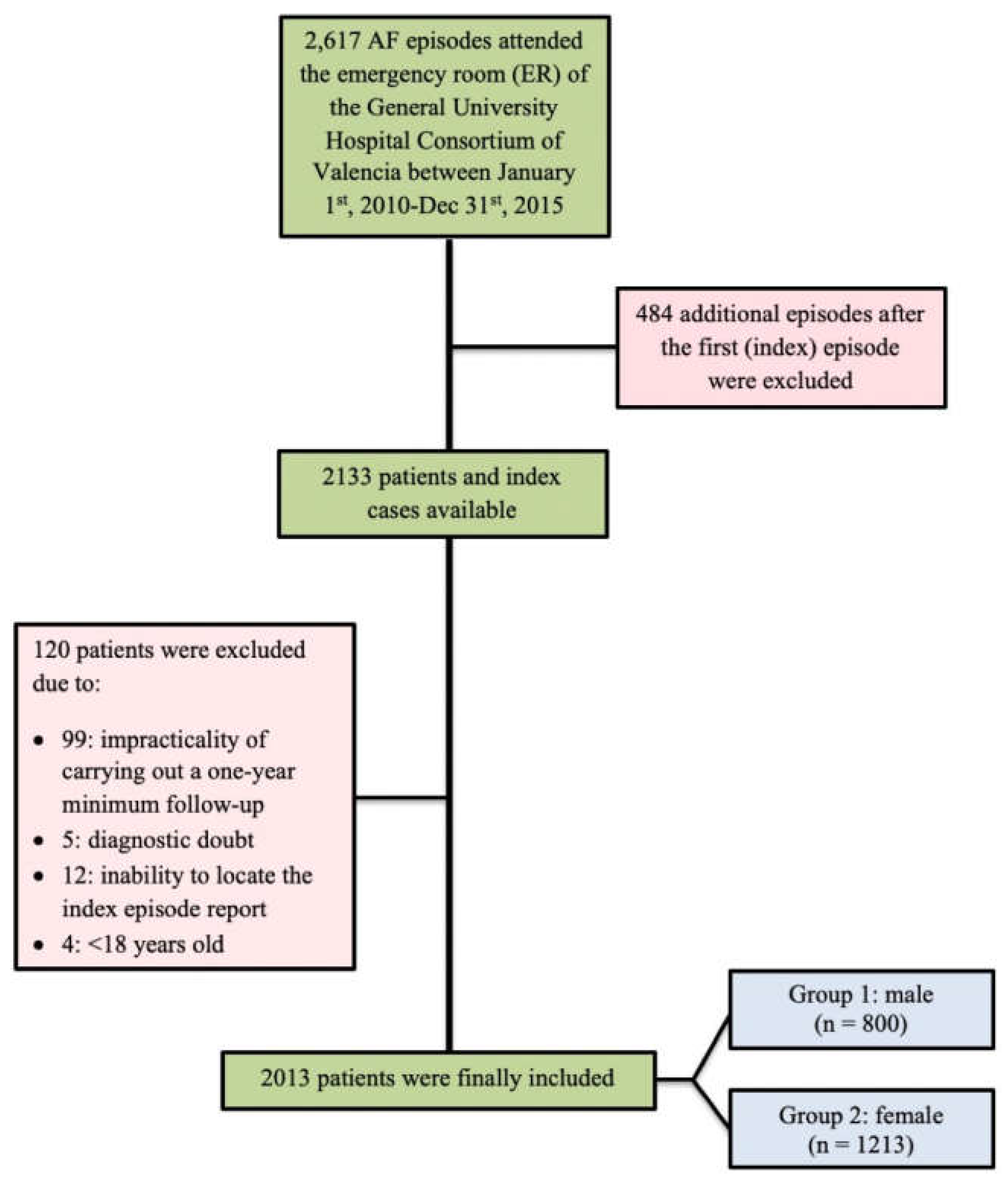
We conducted a retrospective observational study of consecutive patients obtained from a database consisting of 2,617 AF episodes who presented to the emergency department (ED) of the Valencia General University Hospital Consortium (Consorcio Hospital General Universitario de Valencia – CHGUV) with a final diagnosis of AF between January 1, 2010 and December 31, 2015. We captured all AF presentations during the study period. After eliminating repeated episodes and applying the exclusion criteria, a total of 2013 patients were included. Two study groups were finally obtained by dividing the patients according to gender: women and men.
Data from patients over 18 years old who presented with an electrocardiographic (ECG) diagnosis of AF during their admission at the ED were recorded (
Figure 1). Inclusion in the study required at least one-year follow-up. Patients were excluded in case of a mistake in the AF diagnostic, inability to locate the index episode report, further AF episode/s suffered after the AF index episode and follow-up lost were excluded. The work was approved by the Clinical Research Ethics Committee of the CHGUV.
Variables Collected
Age and gender were collected for demographics. Physiological variables included heart rate (HR), blood pressure (BP), oxygen saturation, and left ventricular ejection fraction (LVEF). Likewise, clinical data were collected, including CVD risk factors, previous structural heart disease and other cardiological history, as well as other comorbidities. Characteristics of the index episode, blood test results, clinical presentation (asymptomatic, palpitations, HF, etc.), treatment administered in ED (drugs, cardioversion, etc.), spontaneous conversion to sinus rhythm, assessment by cardiology services, and patient destination after the episode were also collected.
Follow-Up
A minimum of one year of follow-up was performed after the index episode by accessing the electronic medical record and/or telephonic call. The following data were collected: all-cause mortality, first arrhythmia-related presentation to ED, first HF-related presentation to ED or hospitalization, first recurrence of AF, minor hemorrhagic events, major hemorrhagic events (defined as gastrointestinal, intracranial, pulmonary, or retroperitoneal bleeding), embolic events, type of embolism (i.e., ischemic stroke, transient ischemic attack [TIA], or peripheral embolism), first CV after the index episode (date and effectiveness), as well as pharmacological treatment administered.
Statistical Analysis
Quantitative variables are expressed as mean ± standard deviation (SD) and qualitative values are presented as percentages. The Chi-square test was used to compare qualitative variables and student's t test was used for quantitative variables. The cumulative event-free survival probability was estimated using the Kaplan-Meier (KM) method and compared using the log rank test and calculating the hazard ratio (HR). A multivariable Cox linear regression analysis for all-cause mortality was performed to test the independent relationship between gender and other clinical variables. Variables were selected based on previous research evidence and the authors' clinical experience. The results of all statistical analyses were considered statistically significant when p<0.05. All data were analyzed using the IBM SPSS statistical package v25.0 or GraphPad Prism v8.0.
Results
Baseline Characteristics of the Study Population
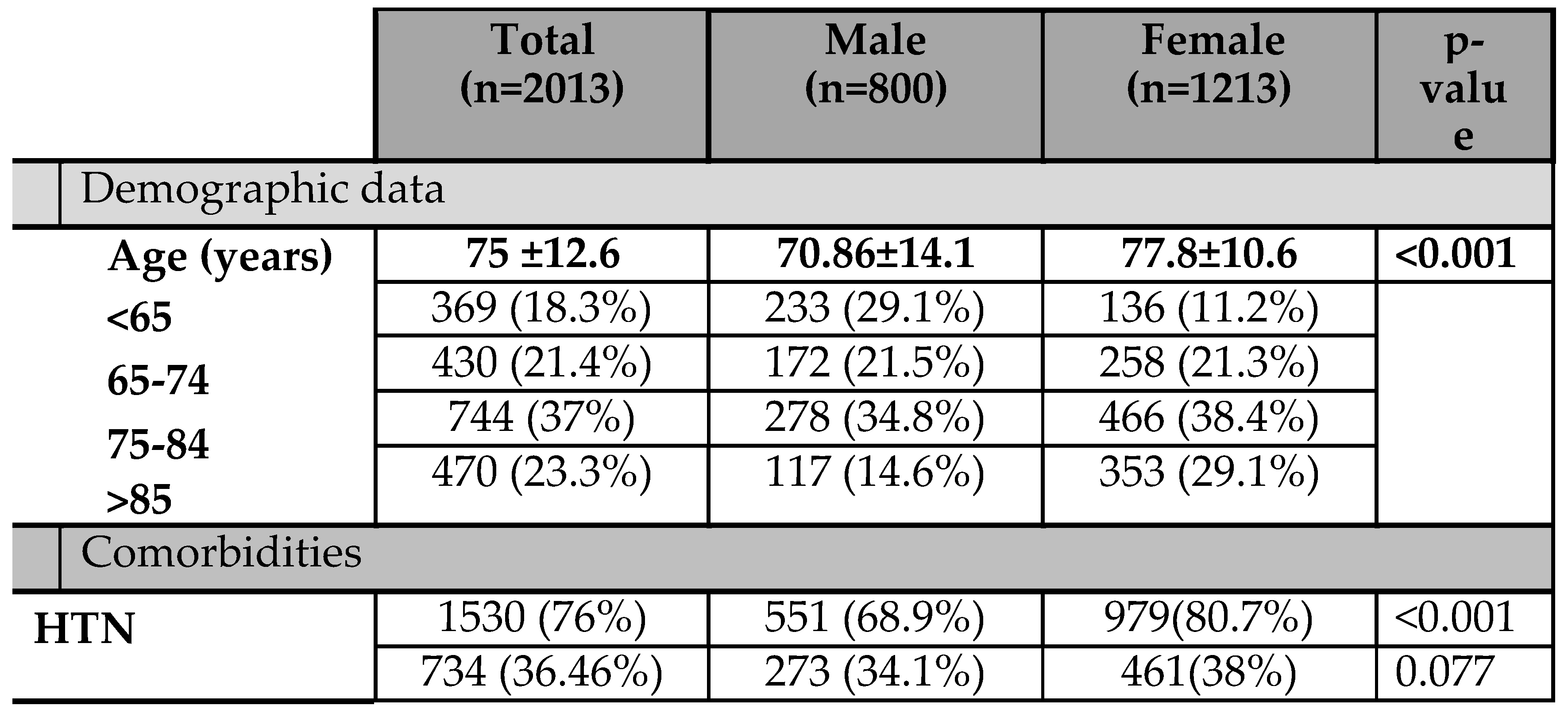
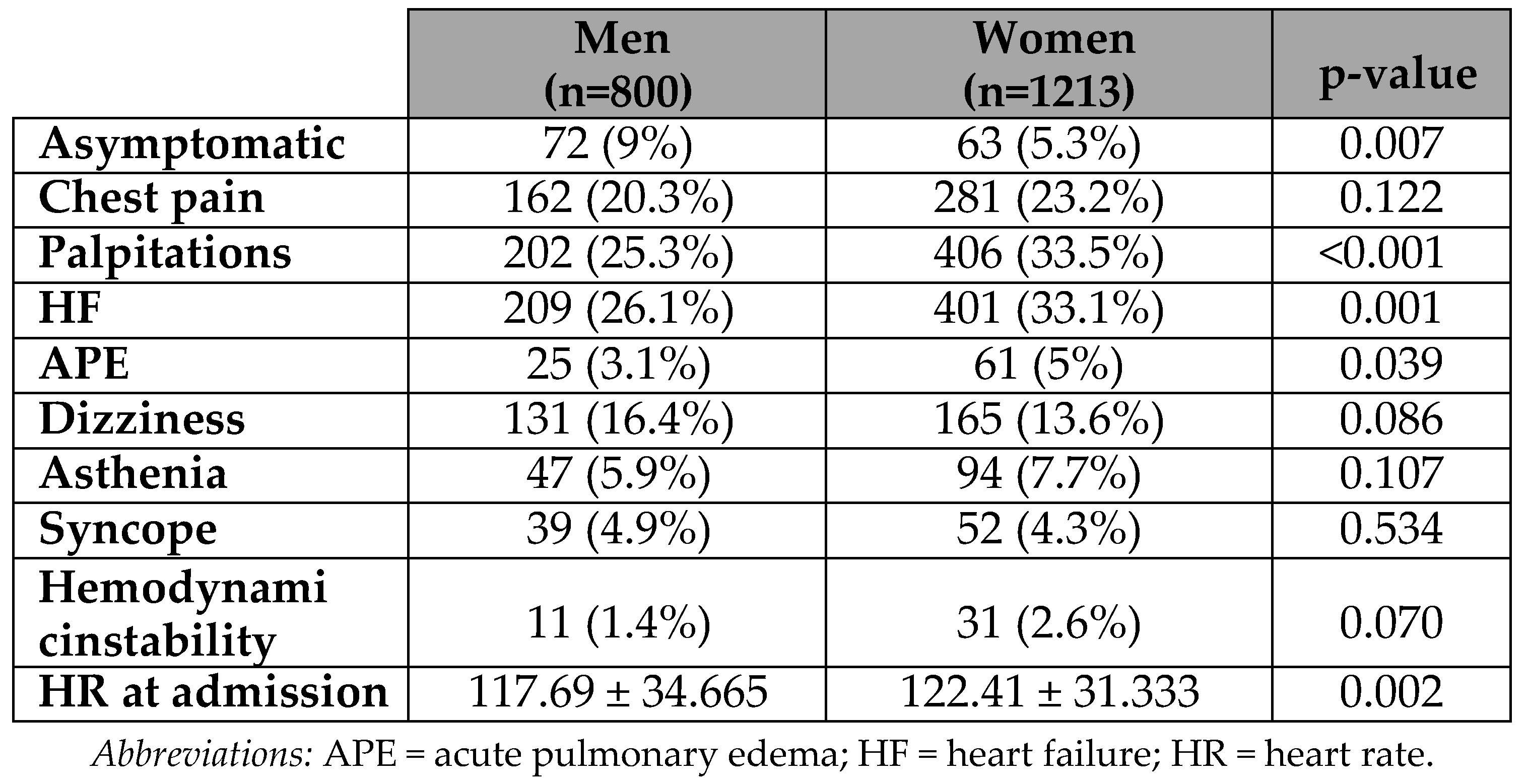
1213 (60.3%) female and 800 (39.7%) male were followed up for a mean period of 3.3±1.5 years. The average age of participants was 75±13 years (60.3% above 75 years; 23% above 85 years). Among the risk factors for CVD, the most frequently observed were hypertension (HTN), dyslipidemia and type 2 diabetes mellitus (T2DM), showing a prevalence of 76%, 39.8% and 36.5%, respectively. The prevalence of smoking and chronic kidney disease (CKD) was low, at approximately 10% for each (
Table 1).
Table 1 also shows gender-based differences in the recorded variables. Women were older than men (77.8±10.6
vs. 70.9±14.1 years). Regarding clinical characteristics, the prevalence of CVD risk factors and other comorbidities was uneven between women and men. Men showed higher prevalence of respiratory diseases, such as chronic obstructive pulmonary disease (COPD) or obstructive sleep apnea (OSA), as well as smoking and alcohol abuse. Specifically, we found significantly higher prevalence rates in men than in women of OSA (5.5%
vs. 2.8%; p=0.002), arteriopathy (7.3%
vs. 3.1%; p<0.001), alcohol abuse (3.6%
vs. 0.2%; p<0.001), smoking (20.3%
vs. 3.4%; p<0.001), history of acute myocardial infarction (10.6%
vs. 6%; p<0.001) and/or ischemic cardiomyopathy, and dilated cardiomyopathy (DCM; 6.1%
vs. 1.8%; p<0.001). In contrast, the prevalence of HTN and obesity were significantly higher in women (80.7%
vs. 68.9%, p<0.001 and 9.6%
vs. 6.9%; p=0.034, respectively). Of note, the prevalence of HF was significantly higher among women (22.3%
vs. 16.3%), as was as the prevalence of mitral valve disease (12.6%
vs. 8.5%). Baseline differences were also translated into prognostic scores differences, with a higher average CHA2DS2-VASc score in women than in men (4.2±1.4
vs.2.7±1.6, p<0.001). No significant difference between the gender was found in anticoagulation therapy or previous ECV.
Gender-Based Clinical Differences at Index Episode
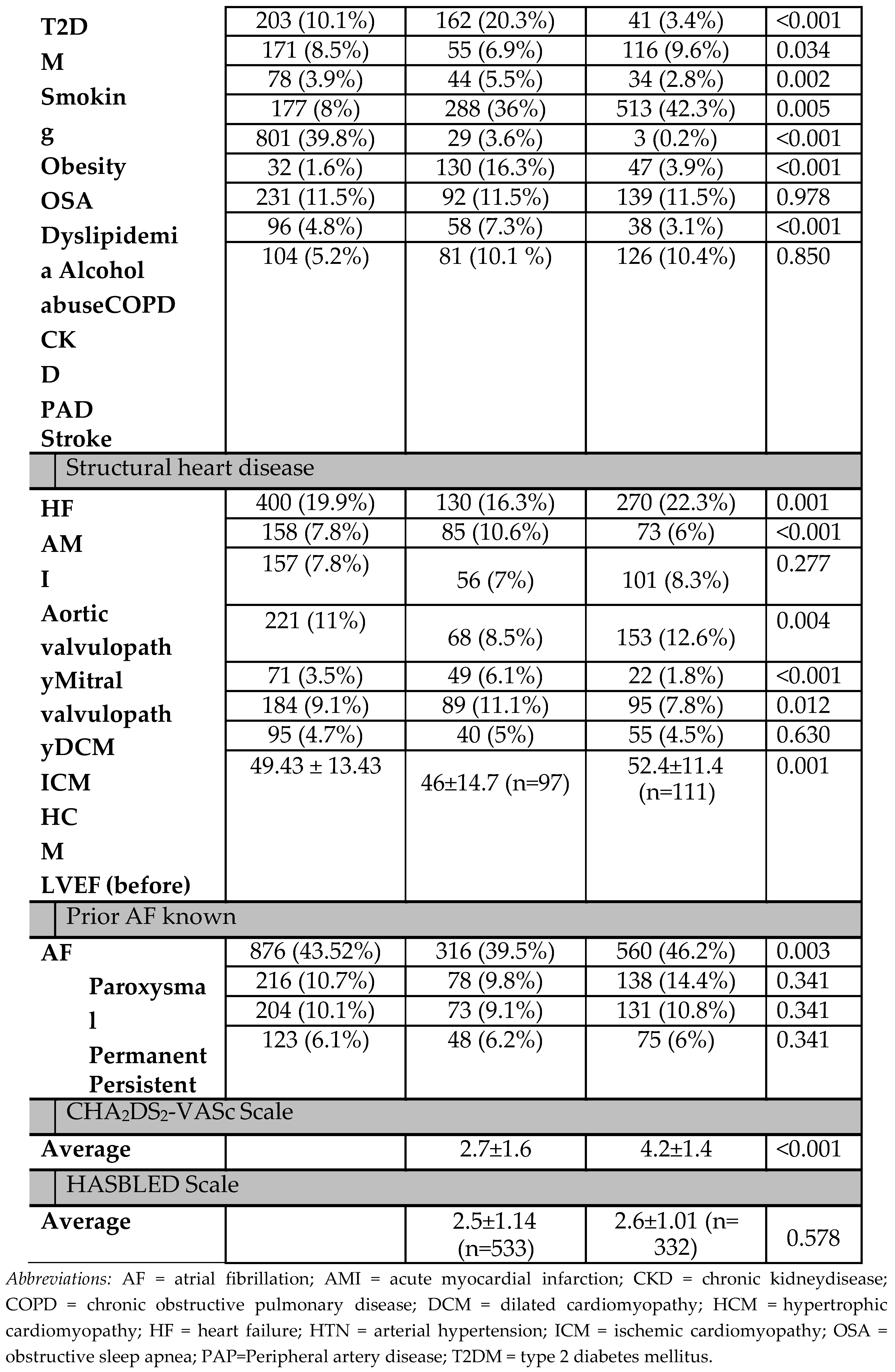
As
Table 2 shows, asymptomatic presentation was more frequent in men, while various symptoms and signs were significantly more frequent in women: palpitations (25.3%
vs. 33.5%; p<0.001), HF (26.1%
vs. 33.1%; p=0.001) and acute pulmonary edema (3.1%
vs. 5%; p=0.039). Although statistical significant difference was also found in HR at admission, 122±31 beats per minute (bpm) in women and 118±35 bpm in men (p=0.002), it was clinically irrelevant.
Healthcare Resources use and Therapeutic Differences
Use of healthcare resources and therapeutic differences were analyzed both during the index episode and during the subsequent follow-up. A significant gender-based difference was found in the proportion of patients being evaluated by the cardiologist during the first episode: 16.6% of male and 11.5% of female were visited by a cardiologist (p=0.05).
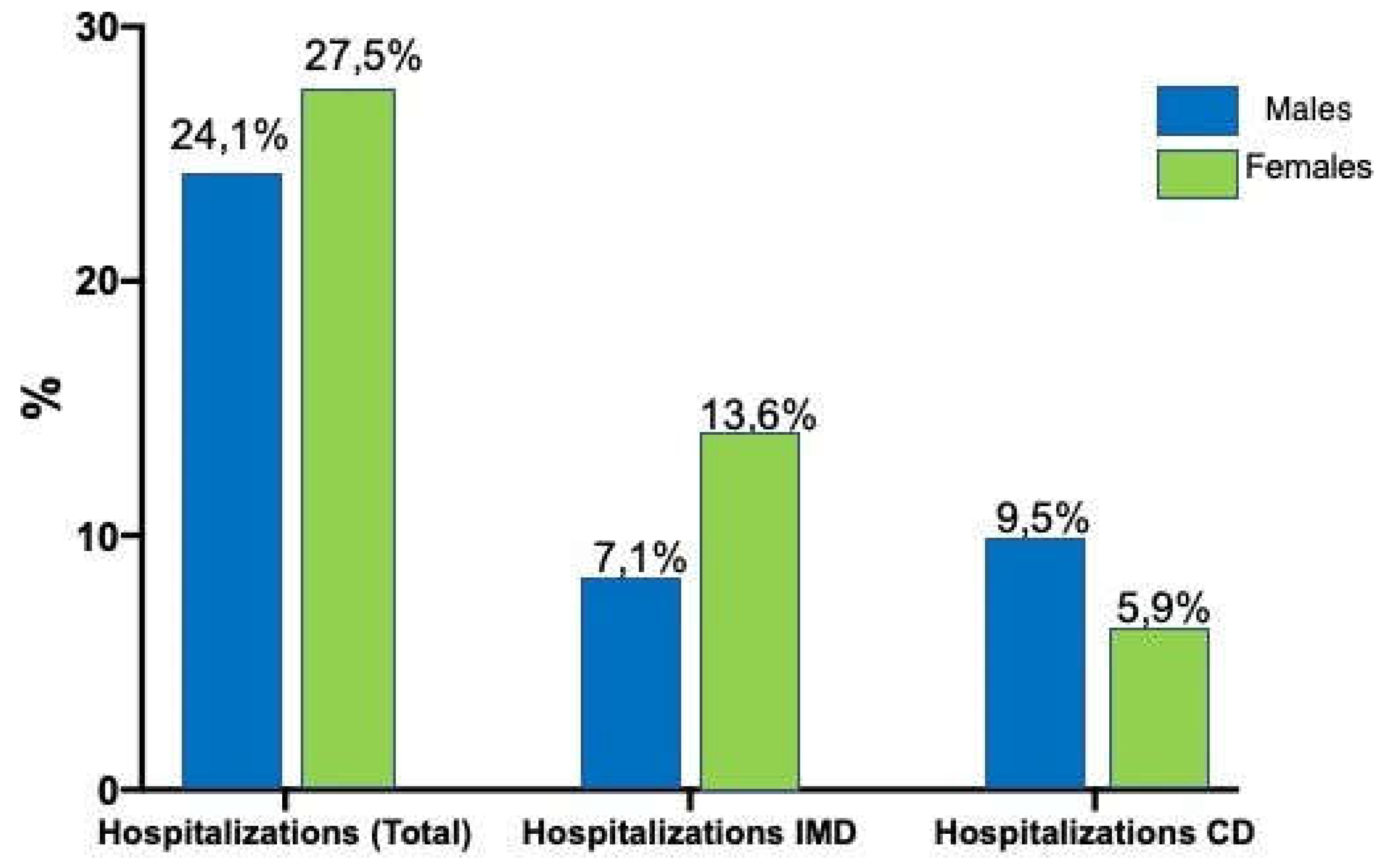
Significant differences were also found in the number of patients transferred to other medical services: 7.1% of men and 13.6% of women (approximately half of those who were admitted to ER) were transferred to internal medicine service (p<0.001), while only 5.9% of women were transferred to the cardiology service versus 9.5% of men (p<0.05) (
Figure 2).
Furthermore, differences were found in the treatment prescribed to prevent cardioembolic events following hospital or ER discharge. Among women, 45.5% were prescribed OACs, an absolute difference of 5.1% more often than men (p<0.05).
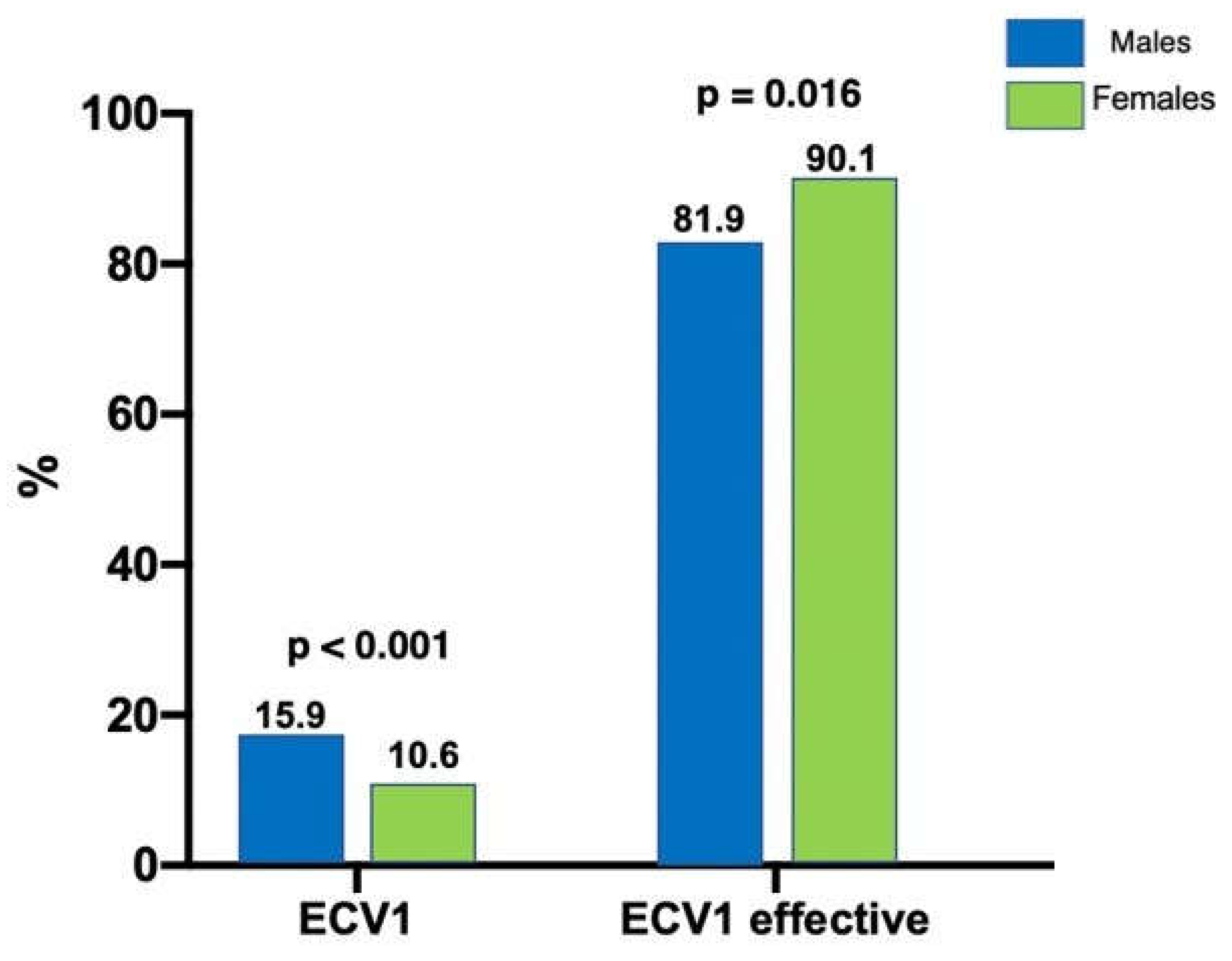
Moreover, we found significant gender differences in the frequency at which ECV was used. During the index episode, men were more frequently treated with ECV (3.4%
vs. 1.2%; p=0.001). During the follow-up period, as
Figure 3 shows, ECV was performed in only 10.6% of women versus 15.9% of men (p<0.001), with a higher recurrence rate after the first ECV in men (23 of 127, 18.12%) than in women (12 of 128, 9.94%; p=0.016).
Comparison of Long-Term Adverse Events
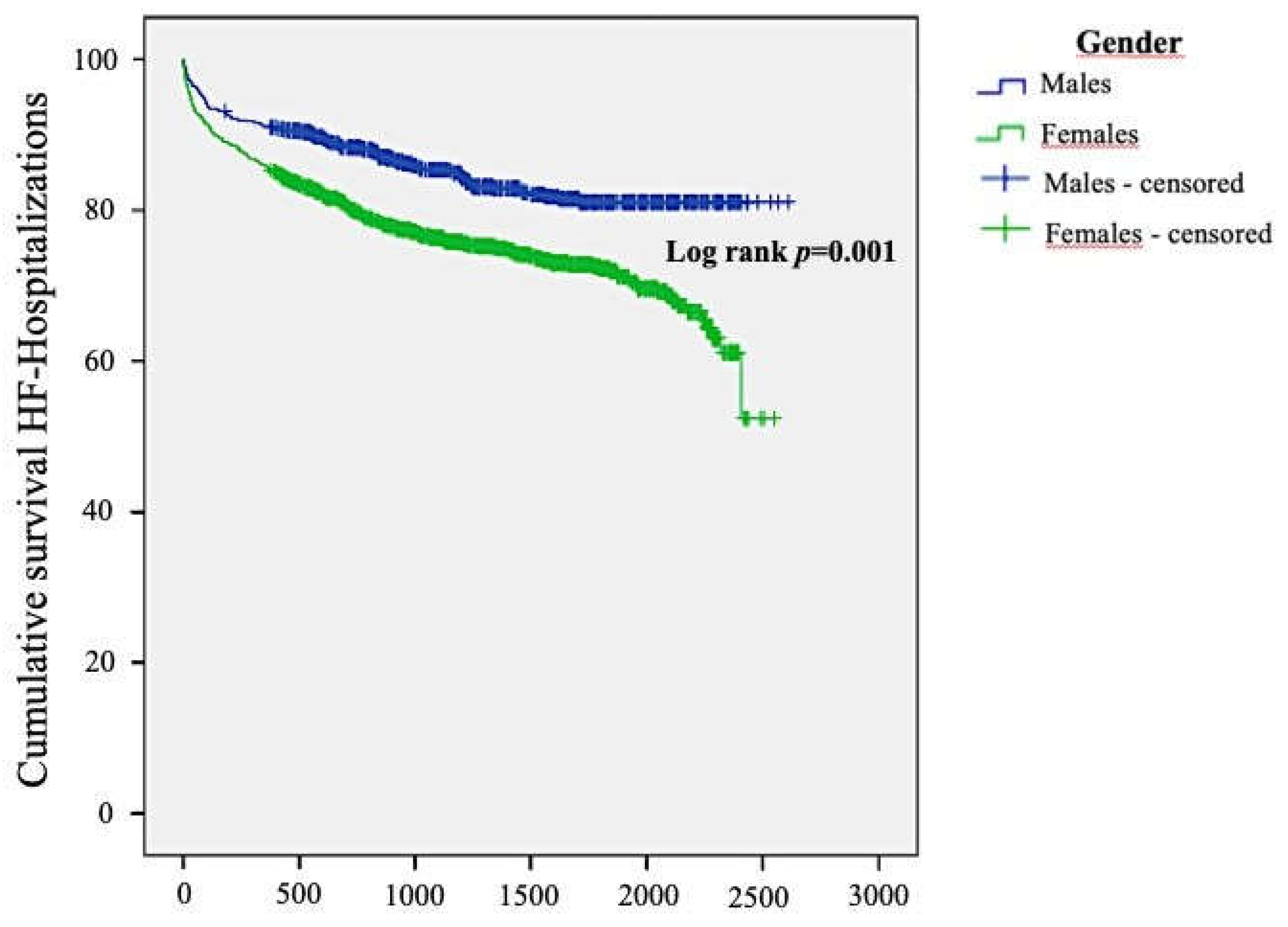
During the follow-up period, significant gender differences were observed in the frequency of HF occurrence. Women were more prone than men to require hospitalization for HF (26.2%
vs. 16.1%; p>0.001). Likewise, women with AF were admitted to the hospital due to HF with a higher frequency than men (33.1%
vs. 26.1%; p=0.001;
Figure 4).
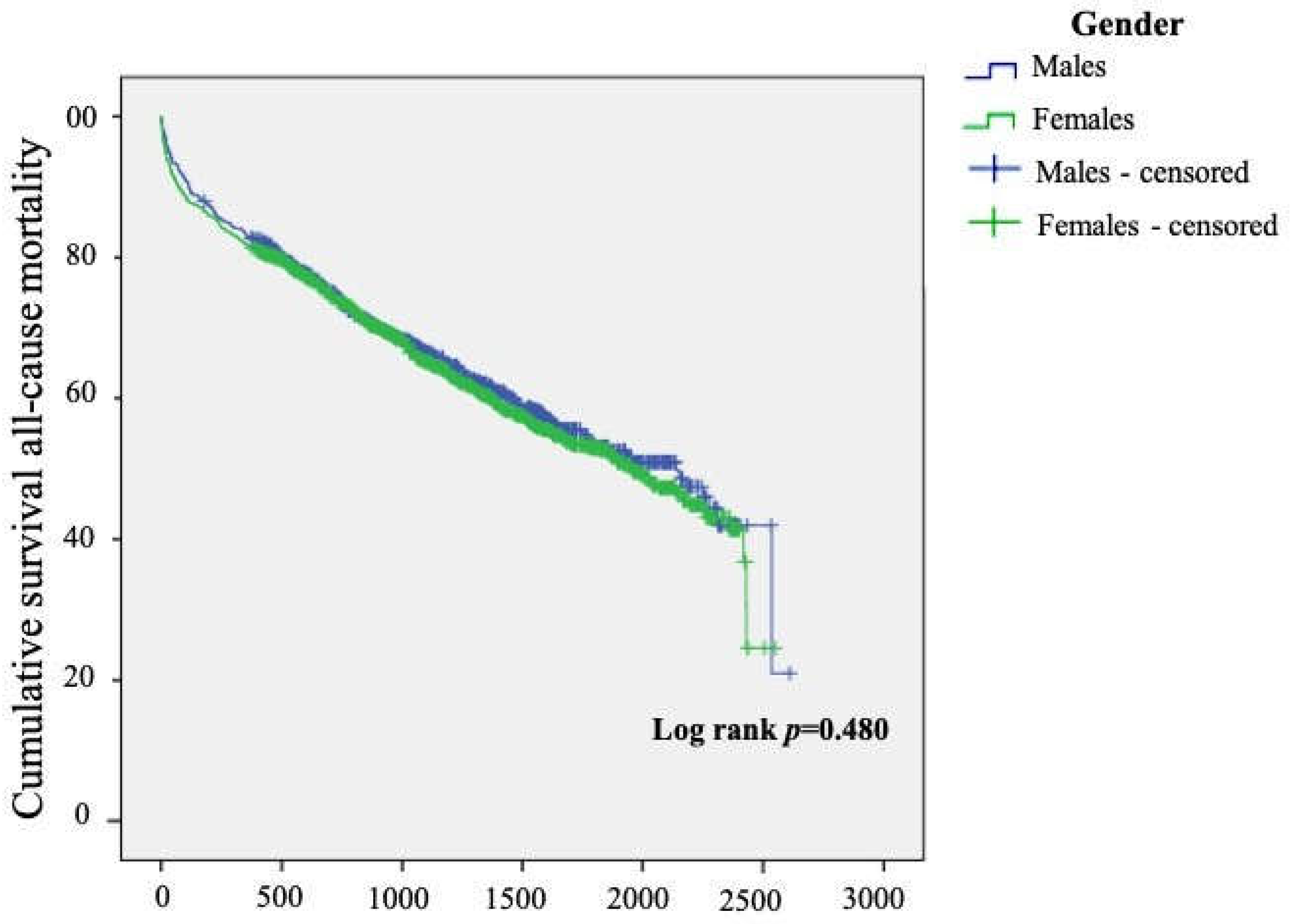
There was no gender difference in the frequency of recurrence of AF (46% vs. 45.7%; p=0.962), nor in mortality (39% vs. 41.6%; p=0.239), incidence of hospitalization (30.3% vs. 32%; p=0.411), emergency care (55.5% vs. 59.1%; p=0.109), ED admissions (27.5% vs. 24.1%; p=0.109), embolism (7.3% vs. 8.6%; p=0.285), or major or minor bleeding (7.8% vs. 5.9%, p=0.094; and 8% vs. 8.1%, p=0.949, respectively).
Multivariate Analysis of Mortality
Over an average of 3.3±1.5 years months of follow-up, there were 817 deaths, 312 out of 800 men (39%) and 505 out of 1213 women (41.6%).
Figure 5 displays survival over time, stratified by gender.
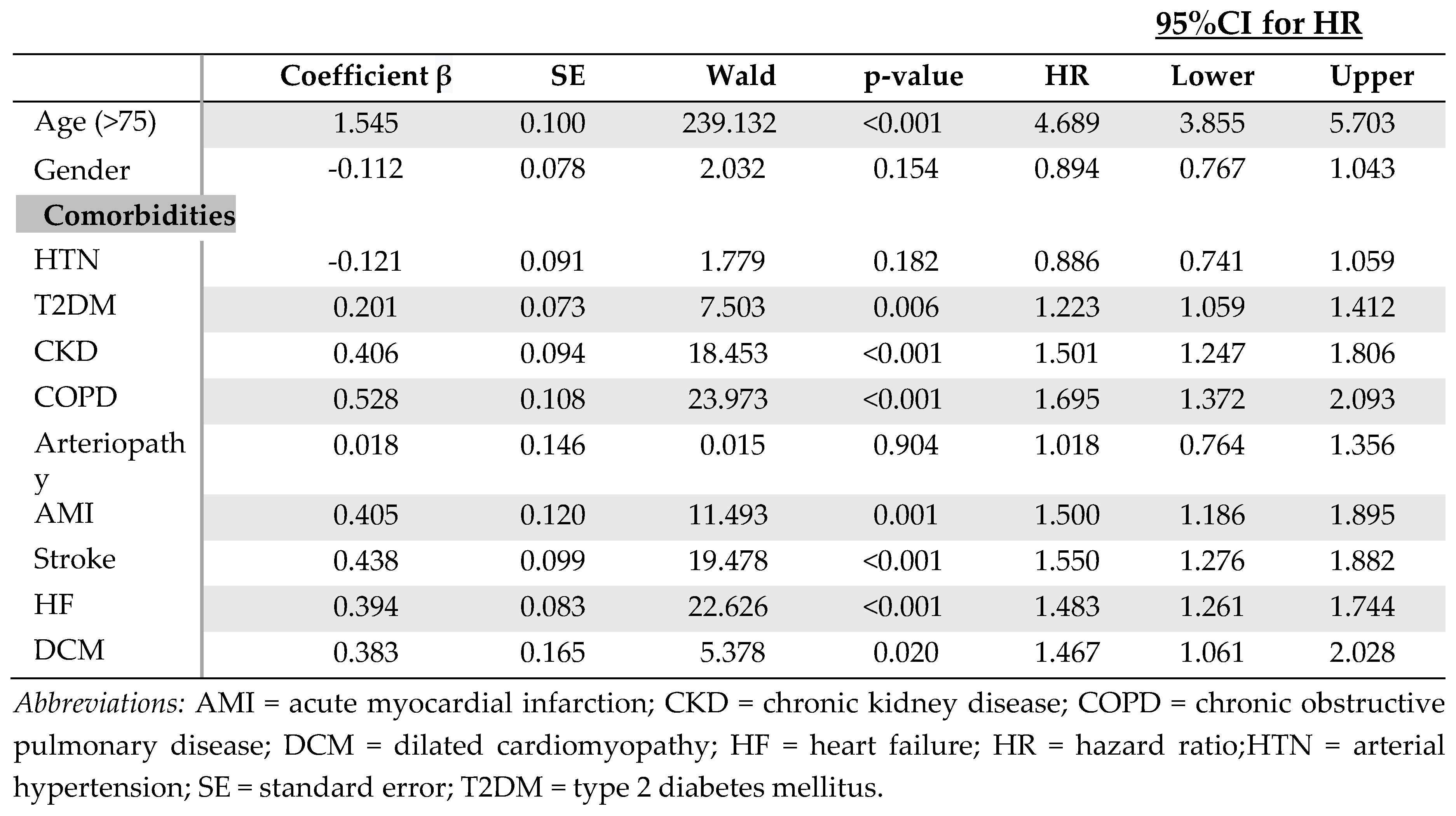
We performed a multivariate analysis to determine whether female gender was an independent risk factor for mortality among patients with AF. Variables included were: age, gender, HTN, T2DM, CKD, COPD, peripheral arteriopathy, acute myocardial infarction (AMI), stroke, HF, and dilated cardiomyopathy (DCM).
Table 3 shows that female gender of patients with AF was not independently associated with any of the risk factors analyzed. However, age and other comorbidities such as T2DM, CKD, COPD, previous AMI, HF, and DCM were independently associated with mortality.
Discussion
Our study shows relevant clinical, use of health resources and prognosis gender-related differences in patients with AF. To highlight, women both experienced more symptomatic AF episodes and received different therapies than did their male counterparts. Likewise, women were less likely to be evaluated by cardiologists in the ER and were less frequently transferred to the cardiology service during their index episode.
In a previous study, in agreement with our findings, Bhave et al.10 reported gender-related differences in health care services provided to AF patients, and concluded that men receive more aggressive care. Specifically, women were less likely to be visited by a cardiologist or electrophysiologist, undergo catheter ablation procedures, or be prescribed oral anticoagulants, rate control drugs, and antiarrhythmic drugs. Thus,
The difference between the study conducted by Bhave et al. (10) and ours was that we analyzed data registered during the acute care in the emergency care setting, while Bhave et al. (10) analyzed the services received after initial AF diagnosis. Hence, our findings reinforce and expand on the evidence provided by Bhave and colleagues. In addition, similarly to our results, Potpara et al. (11) reported that women with AF were more symptomatic than men. This fact was also confirmed by Rienstra et al. (12), who concluded that patients with asymptomatic AF were more often men.
Some studies suggest that estrogens reduce AF prevalence in premenopausal women, not only through decreasing overall CVD risk associated with a better lipid profile, but also by inducing prolongation of the atrial action potential(13). In men, higher testosterone levels seem to elicit the opposite effects, including leading to more fibrotic and proarrhythmic myocardial remodeling(14). On the other hand, when comparing older patients of both sexes, this hormonal benefit disappears progressively and other comorbidities develop higher prevalence. This could predispose older women to AF and other clinical repercussions, such as left ventricle hypertrophy, diastolic HF, and valve disease(14).14
In our study, ECV was less frequently performed for women. This finding concurs with Andrade el al.(4) and Kloosterman et al.(9),9 who reported in previous studies that ECV was more frequently used in men. Likewise, Alegret et al.(15) also reported that gender was an important determinant to decide the treatment for managing patients with AF (i.e., rhythm control strategy or rate control only) in 67 Spanish hospitals during the last decade. These authors observed a lower percentage of women undergoing ECV, and this difference was particularly significant among older asymptomatic patients. Kloosterman and colleagues(9) described demographic and clinical gender-related differences similar to ours. Women had a higher mean age and comorbidities, particularly HF, and some works have reported a slight higher recurrences rate after ECV in women (16,17)which might influence the under-treatment of women with moderate-to-high risk and the underuse of ECV among women(15,18), as we observed in the present study. Likewise, the lower prevalence of symptomatic women with AF might also be a possible explanation for these gender-variations in ECV use(15). Although ECV and/or rhythm control certainly are not contraindicated in elderly women, female gender does increase the risk of complications (e.g., thromboembolism) following ECV of acute AF (duration <48 h), especially in patients aged >75 years and time to ECV exceeding 12 hours(19). Although the prognostic impact of the choice of strategy (rhythm vs. rate control) remains controversial, better symptomatic control and quality of life have been described with the rhythm control strategy(20).
Despite a slightly longer hospital stay and a higher rate of minor bleeding among women, the post-CV improvement in quality of life and cognitive status found on various scales was similar in between the two genders.(4,9) To highlight, unlike what has been reported (16,17), we found that scheduled cardioversions during follow-up had lower recurrence rates in women than in men. which should support efforts for a more generalized use in females, as opposed to what we have observed (see below).
We also found a higher rate of hospital admission for HF in women with AF during the follow-up period. Although they did not evaluate long-term HF admissions, Piccini et al.(8) described a similar frequency difference between the gender in the occurrence of new HF during follow-up. Although it was not statistically significant, O’Neal et al.19(21) also reported a numerically increased risk of hospitalization in women with AF. Undoubtedly, the higher mean age of the women in our population may have influenced our findings, as well as the higher baseline rates of HF among women. However, this might alternatively be explained by the gender-related differences in therapy received(22). In this regard, Bhave et al.(10)10 also reported less aggressive management and therapy of AF in women, which might ultimately influence disease evolution with poorer results. In addition, Cheng and Kong (7) found gender- based differences in the efficacy of medical management of patients with AF. Compared with men, women who were not anticoagulated had greater thromboembolic risk but benefited from greater risk reduction when systemically anticoagulated.
We found no significant gender-related difference in mortality among these patients with AF. Marijon et al.(23) investigated which factors were associated with mortality and several specific causes of death, finding neutral results regarding the influence of gender. Moreover, Potpara et al.(11) did not find any significant difference between men and women patients in terms of all- cause mortality, CVD death, or sudden cardiac death. Other studies, however, associated female gender with higher mortality rates in patients with AF (7,10,22,24–26). The clinical guideline of the European Society of Cardiology states that, while men with AF have a mortality 1.5 times higher than men without AF, similarly afflicted women have a mortality 2 times that of their counterparts without AF(24). However, these differences decreased markedly when the study was carried out in developed countries, a difference which must also be considered in our study(3). In contrast, Piccini et al.(8) found higher mortality from all causes in men AF patients.
The higher mortality in women described by other studies may be due to the higher embolic risk in women, since mortality differences decrease in effectively anticoagulated populations. This difference in all-cause mortality decreases significantly, as we also observed in our study, and the main cause of death becomes CVD death(23). Finally, we must be aware that the results of higher mortality observed in some studies, especially those carried out in less economically developed areas or the greater rate of HF, a surrogate of mortality found in ours, may not reflect biologic sex-related differences in mortality, but rather gender-related differences in health care delivery. Being alert to these iniquities should facilitate to take measures to correct them.
Study Limitations
Our data may be subjected to information biases due to varying levels of detail of the clinical reports or some information omitted in the clinical history. Of note, if it was appropriate according to the antecedent diagnosis dates, we completed the collection of baseline information during the follow-up period. Regarding mortality, there were baseline differences in the characteristics and comorbidities of both groups that could affect the prognosis. To eliminate the effects of confounders, a multivariate analysis was carried out, confirming that gender did not independently impact mortality rates in our population, but HF, more frequent in women, did it. The fact that all patients were enrolled from the ER could be considered a source of selection bias. However, the sample was representative of the population.
Although the data relates to patients with AF between 2010 and 2015, our perception is current practice and treatment strategies of AF have scarcely varied compared to the years of study, however this remain to be confirmed in future studies without the distortions imposed by the COVID pandemic. Finally, other treatments aimed at rhythm control, such as AF catheter ablation, were not evaluated.
Conclusions
There are significant gender-related differences in patients with AF. Although we did not find a significant independent gender-related difference in mortality in these patients, female gender increased the risk of admission for HF, a surrogate of mortality, in the long-term follow-up of patients with AF. Also, women differed in several unfavorable baseline characteristics compared to men, mainly in terms of age and greater CHA2DS2-VASc score, and more frequently present with symptomatic AF. In spite of these adverse profile, there were marked healthcare differences according to gender, such as women being less likely to receive a cardiology consultation or to be transferred to the cardiology department. ECV also was used less frequently in women, both in the ER and during follow-up, notwithstanding its better result in the latter.
Finally, all of our findings related to the use of health resources and treatment strategies would point to the fact that differences in HF may be more related to a gender bias than a sex one. Increasing recognition of these gender differences may help clinicians improve both the acute and chronic management of AF.
Author Contributions
Aurelio Quesada, Javier Quesada-Ocete and Fabian Sanchis-Gomar: Conceptualization, Meth- odology, Validation, Formal analysis, Investigation, Data curation, Writing-original draft, Writing review & editing, Visualization, Supervision, Project administration. Víctor del Moral-Ronda, Blanca Quesada-Ocete Javier Jiménez-Bello: Conceptualization, Methodology, Investigation, In- vestigation, Resources. Ricardo Rubini-Costa: Methodology, Formal analysis, Investigation. Fer- nando de la Guía-Galipienso and Ricardo Rubini-Puig: Methodology, Writing-review & editing. Carl J. Lavie and Daniel P. Morin: Writing-review & editing.
Acknowledgements
Fabian Sanchis-Gomar is supported by a postdoctoral contract granted by “Subprograma Atracció de Talent - Contractes Postdoctorals de la Universitat de València”.
References
- Lippi, G.; Sanchis-Gomar, F.; Cervellin, G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int. J. Stroke 2020, 16, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V.; Oertelt-Prigione, S.; Prescott, E.; Franconi, F.; Gerdts, E.; Foryst-Ludwig, A.; Maas, A.H.; Kautzky-Willer, A.; Knappe-Wegner, D.; Kintscher, U.; et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur. Hear. J. 2015, 37, 24–34. [Google Scholar] [CrossRef]
- Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 2014, 129, 837–847. [CrossRef] [PubMed]
- Andrade, J.G.; Deyell, M.W.; Lee, A.Y.; Macle, L. Sex Differences in Atrial Fibrillation. Can. J. Cardiol. 2018, 34, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Albert, C.M.; Andreotti, F.; Badimon, L.; Van Gelder, I.C.; Hylek, E.M.; Cove, C.L. Female sex as an independent risk factor for stroke in atrial fibrillation: Possible mechanisms. Thromb. Haemost. 2014, 112, 385–391. [Google Scholar] [CrossRef]
- Arnson Y, Hoshen M, Berliner Senderey A, Reges O, Balicer R, Leibowitz M, et al. Comparing Management and Outcomes in Men and Women With Nonvalvular Atrial Fibrillation: Data From a Population-Based Cohort. JACC Clin Electrophysiol. 2018, 4, 604–614.
- Cheng, E.Y.; Kong, M.H. Gender Differences of Thromboembolic Events in Atrial Fibrillation. Am. J. Cardiol. 2015, 117, 1021–1027. [Google Scholar] [CrossRef]
- Piccini JP, Simon DN, Steinberg BA, Thomas L, Allen LA, Fonarow GC, et al. Differences in Clinical and Functional Outcomes of Atrial Fibrillation in Women and Men: Two-Year Results From the ORBIT-AF Registry. JAMA Cardiol. 2016, 1, 282–291. [CrossRef]
- Chua, W.; Fabritz, L.; Al-Khalidi, H.R.; Schotten, U.; Nielsen, J.C.; Piccini, J.P.; Di Biase, L.; Todd, D.; Mont, L.; Van Gelder, I.C.; et al. Sex differences in catheter ablation of atrial fibrillation: results from AXAFA-AFNET 5. Eur. 2020, 22, 1026–1035. [Google Scholar] [CrossRef]
- Bhave, P.D.; Lu, X.; Girotra, S.; Kamel, H.; Sarrazin, M.S.V. Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Hear. Rhythm. 2015, 12, 1406–1412. [Google Scholar] [CrossRef]
- Potpara, T.S.; Marinkovic, J.M.; Polovina, M.M.; Stankovic, G.R.; Seferovic, P.M.; Ostojic, M.C.; Lip, G.Y. Gender-related differences in presentation, treatment and long-term outcome in patients with first-diagnosed atrial fibrillation and structurally normal heart: The Belgrade atrial fibrillation study. Int. J. Cardiol. 2012, 161, 39–44. [Google Scholar] [CrossRef]
- Rienstra, M.; Vermond, R.A.; Crijns, H.J.; Tijssen, J.G.; Van Gelder, I.C. Asymptomatic persistent atrial fibrillation and outcome: Results of the RACE study. Hear. Rhythm. 2014, 11, 939–945. [Google Scholar] [CrossRef] [PubMed]
- Bhupathy, P.; Haines, C.D.; Leinwand, L.A. Influence of Sex Hormones and Phytoestrogens on Heart Disease in Men and Women. Women's Heal. 2010, 6, 77–95. [Google Scholar] [CrossRef] [PubMed]
- E Odening, K.; Deiß, S.; Dilling-Boer, D.; Didenko, M.; Eriksson, U.; Nedios, S.; Ng, F.S.; Luque, I.R.; Borque, P.S.; Vernooy, K.; et al. Mechanisms of sex differences in atrial fibrillation: role of hormones and differences in electrophysiology, structure, function, and remodelling. Eur. 2018, 21, 366–376. [Google Scholar] [CrossRef] [PubMed]
- Alegret, J.M.; Viñolas, X.; Martínez-Rubio, A.; Pedrote, A.; Beiras, X.; García-Sacristán, J.F.; Crespo-Mancebo, F.; Ruiz-Mateas, F. Gender Differences in Patients with Atrial Fibrillation Undergoing Electrical Cardioversion. J. Women's Heal. 2015, 24, 466–470. [Google Scholar] [CrossRef]
- Gurevitz, O.T.; Varadachari, C.J.; Ammash, N.M.; Malouf, J.F.; Rosales, A.G.; Herges, R.M.; Bruce, C.J.; Somers, V.K.; Hammill, S.C.; Gersh, B.J.; et al. The effect of patient sex on recurrence of atrial fibrillation following successful direct current cardioversion. Am. Hear. J. 2006, 152, 155–e9. [Google Scholar] [CrossRef]
- Grönberg, T.; Hartikainen, J.E.K.; Nuotio, I.; Biancari, F.; Vasankari, T.; Nikkinen, M.; Ylitalo, A.; Airaksinen, K.E.J. Can We Predict the Failure of Electrical Cardioversion of Acute Atrial Fibrillation? The FinCV Study. Pacing Clin. Electrophysiol. 2014, 38, 368–375. [Google Scholar] [CrossRef]
- Kostopoulou, A.; Zeljko, H.M.; Bogossian, H.; Ciudin, R.; Costa, F.; Heijman, J.; Kochhaeuser, S.; Manola, S.; Scherr, D.; Sohal, M.; et al. Atrial fibrillation-related stroke in women: Evidence and inequalities in epidemiology, mechanisms, clinical presentation, and management. Clin. Cardiol. 2019, 43, 14–23. [Google Scholar] [CrossRef]
- Bah, A.; Nuotio, I.; Grönberg, T.; Ylitalo, A.; Airaksinen, K.E.J.; Hartikainen, J.E.K. Sex, age, and time to cardioversion. Risk factors for cardioversion of acute atrial fibrillation from the FinCV study. Ann. Med. 2016, 49, 254–259. [Google Scholar] [CrossRef]
- Gleason, K.T.; Himmelfarb, C.R.D.; Ford, D.E.; Lehmann, H.; Samuel, L.; Jain, S.; Naccarelli, G.; Aggarwal, V.; Nazarian, S. Association of sex and atrial fibrillation therapies with patient-reported outcomes. Hear. 2019, 105, 1642–1648. [Google Scholar] [CrossRef]
- O'Neal, W.T.; Sandesara, P.; Hammadah, M.; Venkatesh, S.; Samman-Tahhan, A.; Kelli, H.M.; Soliman, E.Z. Gender Differences in the Risk of Adverse Outcomes in Patients With Atrial Fibrillation and Heart Failure With Preserved Ejection Fraction. Am. J. Cardiol. 2017, 119, 1785–1790. [Google Scholar] [CrossRef] [PubMed]
- Kassim, N.A.; Althouse, A.D.; Qin, D.; Leef, G.; Saba, S. Gender differences in management and clinical outcomes of atrial fibrillation patients. J. Cardiol. 2016, 69, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Marijon, E.; Le Heuzey, J.-Y.; Connolly, S.; Yang, S.; Pogue, J.; Brueckmann, M.; Eikelboom, J.; Themeles, E.; Ezekowitz, M.; Wallentin, L.; et al. Response to Letter Regarding Article, “Causes of Death and Influencing Factors in Patients With Atrial Fibrillation: A Competing-Risk Analysis From the Randomized Evaluation of Long-Term Anticoagulant Therapy Study”. Circulation 2014, 130, e85. [Google Scholar] [CrossRef]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; Hart, C.L.; Hole, D.J.; McMurray, J.J. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am. J. Med. 2002, 113, 359–364. [Google Scholar] [CrossRef]
- Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 1998, 98, 946–952. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).