2. Case Presentation
An 11-year-old, spayed female mixed breed cat was referred to our hospital with a chief complaint of chronic facial nerve paralysis. She presented with sudden nystagmus and staggering gait 3 months earlier, and a magnetic resonance imaging (MRI) scan was performed at another hospital, which revealed a suspected inflammatory granulation in the right tympanic bulla. A tentative diagnosis of otitis media was made and the patient was started on prednisolone 5 mg/head/day, with no recurrence of nystagmus. However, the dose could not be reduced because withdrawal of prednisolone resulted in decreased vigorous and appetite. The patient experienced a transient right torsional head tilt and narrowing of the right eyelid fissure 2 weeks earlier.
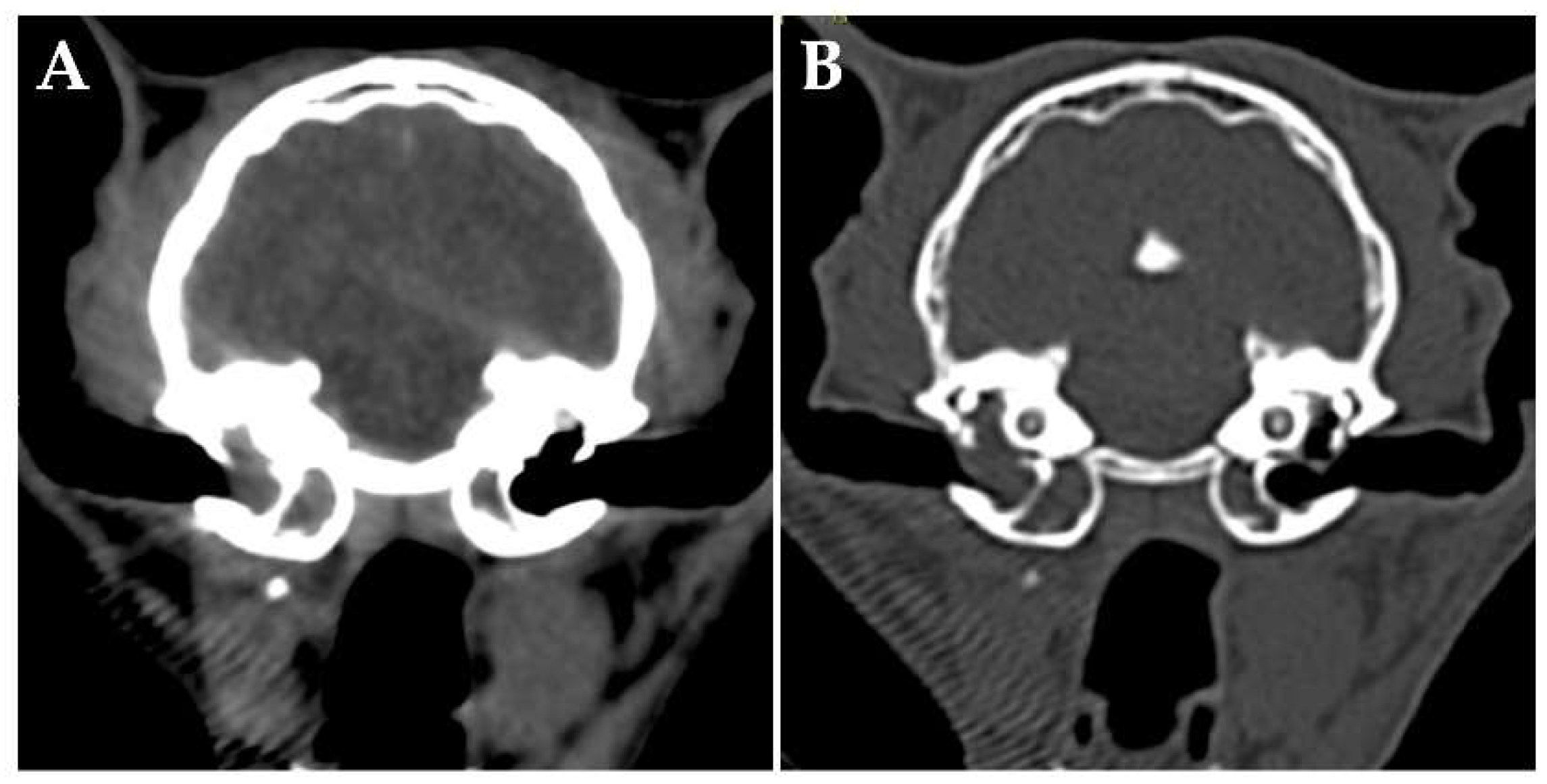
At the time of initial examination, she weighed 3.60 kg and there were no obvious abnormalities in the posture or gait. There was minimal earwax and no enlarged cervical lymph nodes. A cranial neurologic examination was performed, which revealed a disturbance of the right facial nerve and abnormalities of the hypoglossal nerve (narrowing of the right eyelid fissure, loss of right menace reaction, loss of right eyelid reflex, decreased right corneal reflex, decreased right maxillary and mandible perception, and folded tongue). There was no history of seizures. Complete blood count, blood biochemistry, coagulation test, and urinalysis showed no obvious abnormalities. Feline immunodeficiency virus antibody test and feline leukemia virus antigen test were negative (SNAP FIV/FeLV Combo Test; IDEXX Laboratories, Inc., Westbrook, Me, USA). A computed tomography (CT) scan of the head (without anesthesia/without contrast media) was performed to confirm the status of the middle ear, which revealed occupying lesions in the bilateral tympanic bulla (
Figure 1). There were no obvious bony changes and no obvious abnormalities other than the middle ear, including the nasal cavity. The lesions within the tympanic bulla seemed like an effusion or soft tissue, and infection and neoplastic disease were the differential diagnoses.
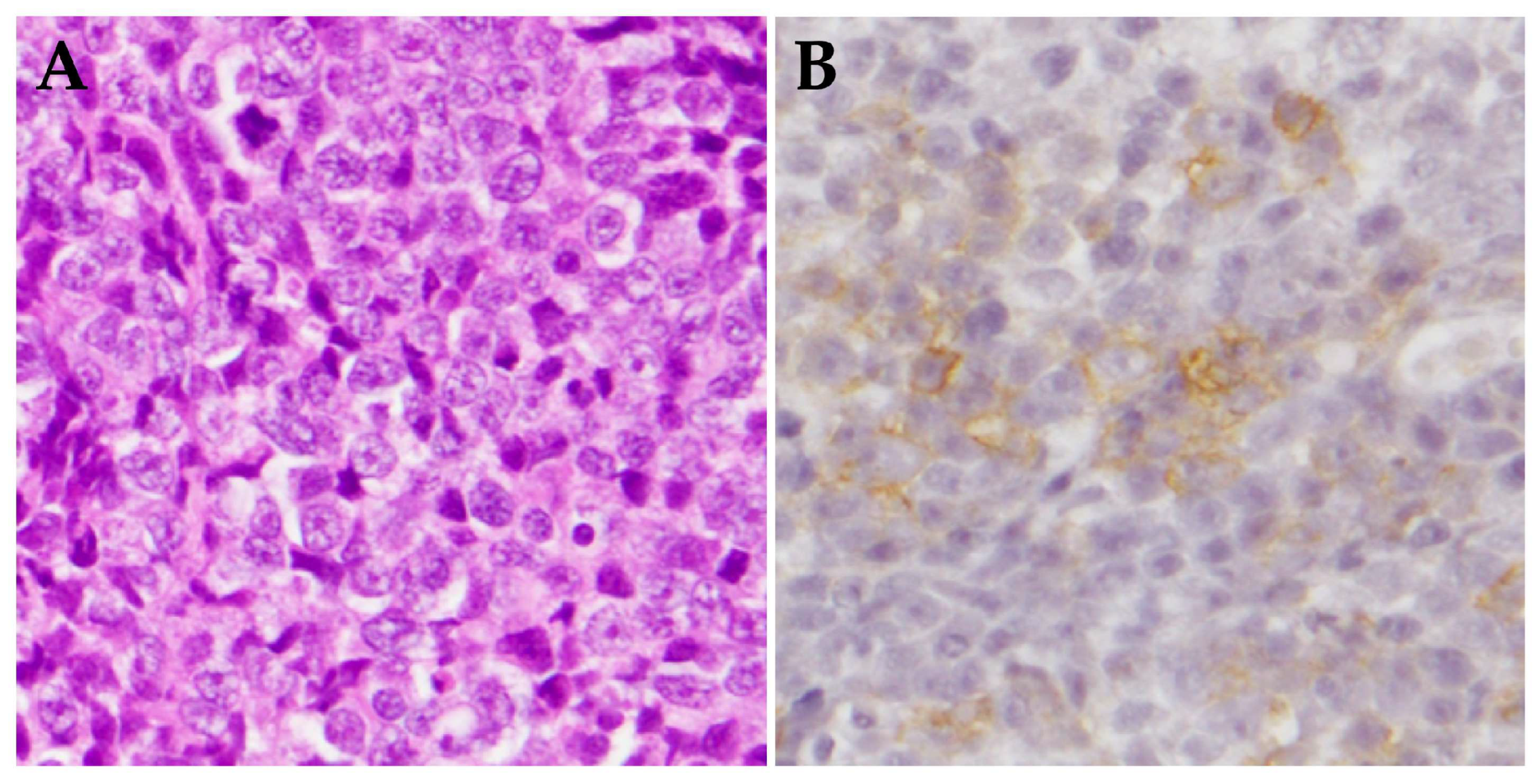
On day 28, the patient's weight had decreased to 3.15 kg, although the condition of her remained the same. The owner reported frequent spills of food, probably due to an abnormality of the hypoglossal nerve. After general anesthesia was administered, the middle ear was examined by video-otoscope. The right tympanic membrane was filled with a cauliflower-shaped mass, and it was difficult to observe the entire tympanic bulla. A portion of the mass was sampled with endoscopic forceps. Observation of the left ear canal revealed a thickened tympanic membrane, and the surface of the tympanic membrane was sampled. Histopathological examination revealed that the mass in the right tympanic cavity was diagnosed as a poorly differentiated large B-cell lymphoma (
Figure 2), and the left tympanic membrane was found to have no obvious abnormality.
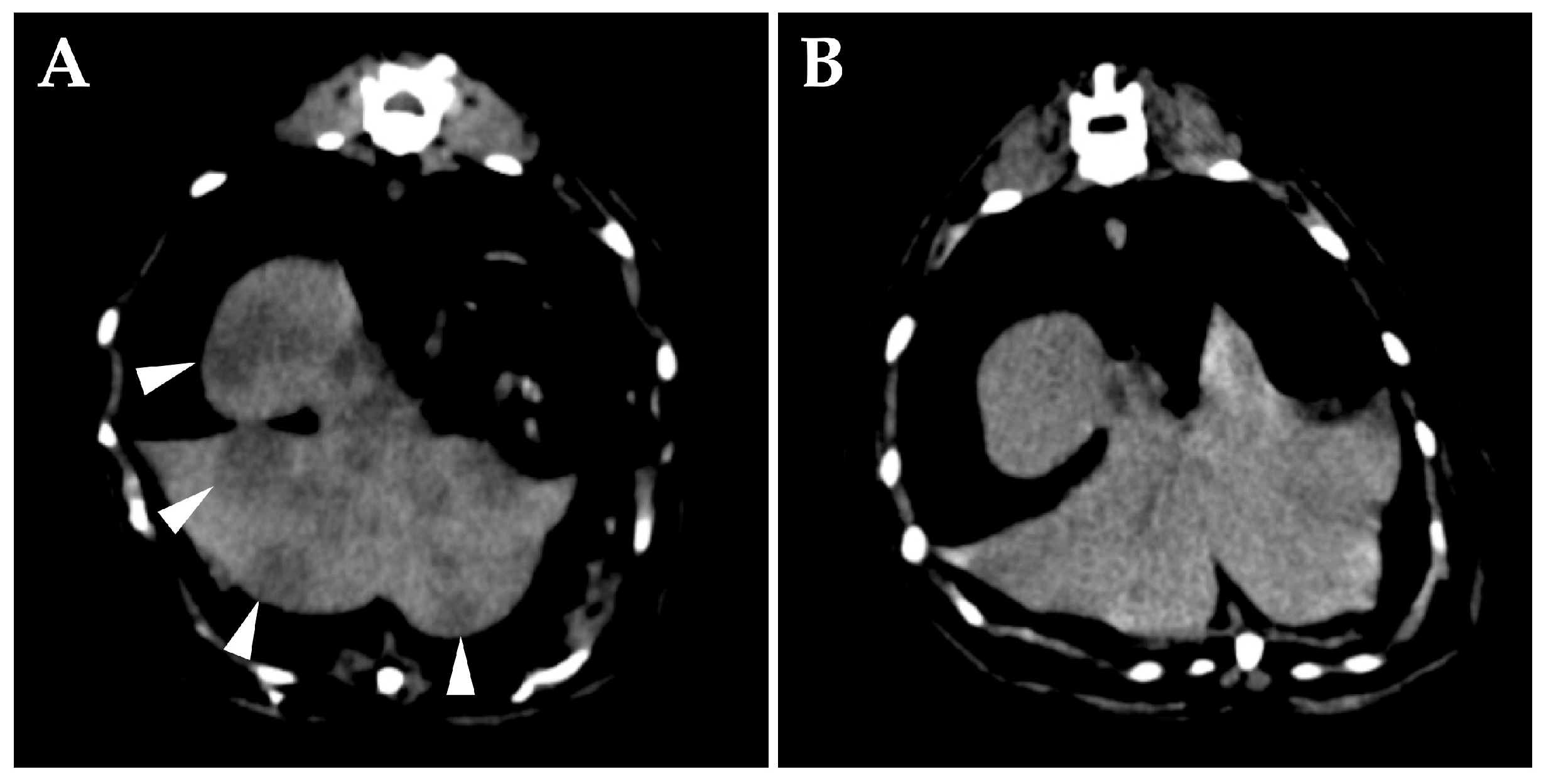
On day 42, a whole-body CT scan (without anesthesia/without contrast media) was performed for clinical staging. The middle ear was unchanged, but diffuse changes were observed in the liver (
Figure 3). Cytology of the liver lesions was not performed. A tentative diagnosis of middle ear lymphoma and hepatic metastasis, namely, clinical stage 4, was made. After discussing the treatment plan with the owner, L-asparaginase 400 KU/kg subcutaneously (Kyowa Kirin, Tokyo, Japan) was administered. Prednisolone was continued at 5 mg/head/day.
On day 56, right eyelid opening had improved. A whole-body CT scan (without anesthesia/without contrast media) was performed, which showed that the dorsolateral lesion of the right tympanic bulla had disappeared, the hepatic lesion was obscured, and the liver swelling had improved. L-asparaginase was evaluated as effective, and a second dose was administered.
On day 68, a multidrug chemotherapy (CHOP protocol) was started [
6]; the patient was treated with vinblastine 1.5 mg/m
2 intravenously (Nippon Kayaku Co., Ltd., Tokyo, Japan), cyclophosphamide 10 mg/kg intravenously (Shionogi Co., Ltd., Osaka, Japan), and doxorubicin 1 mg/kg intravenously (Sandoz K. K., Tokyo, Japan). There were no significant adverse effects in terms of weight change or blood tests, and the protocol was generally carried out as planned, with three postponements of administration due to deterioration of the patient's physical condition, including decreased appetite and dizziness. Considering the nature of the case, the patient was sedated with butorphanol 0.4 mg/kg intramuscularly (Meiji Animal Health Co., Ltd., Tokyo, Japan) each time the catheter needle was placed, and the anticancer drug administration was completed without any problems. The neurological abnormalities were not completely cured, but since there was no increase in liver enzyme levels, the patient was considered to be in remission clinically, and the protocol was continued every other week after the 152nd day. Prednisolone administration at 5 mg/head/day was continued, because the patient's condition worsened when the dose was reduced.
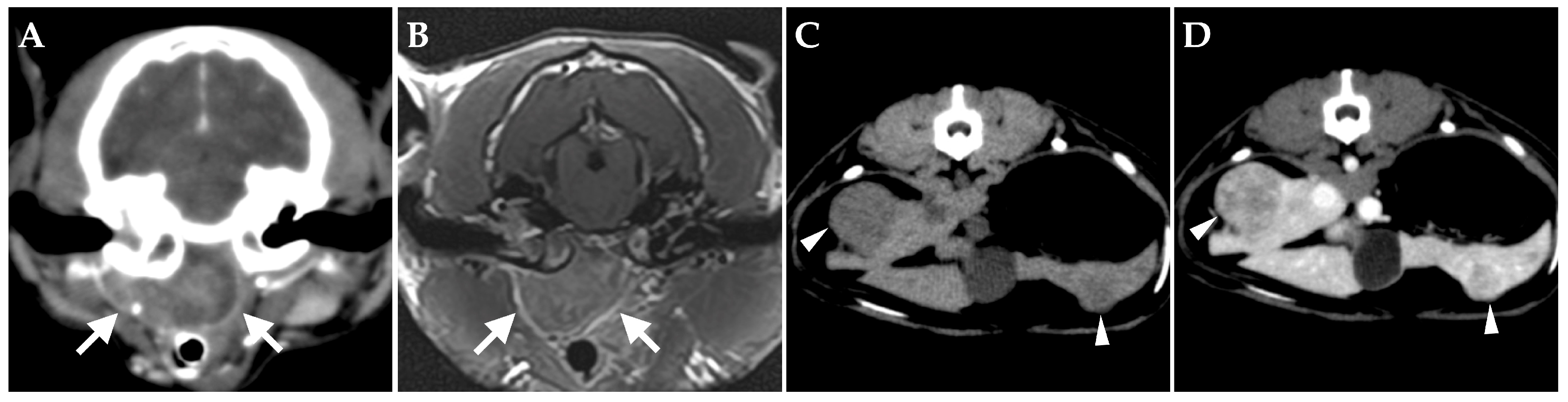
On day 176, the patient had an unstable appetite and nasal obstruction sounds. Intraoral examination revealed a soft palate swelling. Blood tests revealed no particular abnormalities. A contrast-enhanced whole-body CT scan was performed under anesthesia, which revealed unchanged filling of the bilateral tympanic bullas, but no obvious bony abnormalities. A mass lesion with heterogeneously contrast-enhancement was found on the ventral of the right tympanic bulla, which almost completely obstructed the nasopharyngeal region (
Figure 4). The right medial retropharyngeal lymph node was contiguous with the ventral lesion of the tympanic bulla and heterogeneously contrast enhanced. Multiple contrast-enhanced mass lesions were noted in the liver (maximum diameter 18 mm). There were no obvious intrathoracic or intra-abdominal organs abnormalities other than the liver. An MRI scan of the head revealed no obvious meningeal lesions and no obvious abnormal findings in the brain. A tentative diagnosis was made that the lymphoma in the right middle ear had spread to the Eustachian tube and formed a mass in the nasopharyngeal region.
On day 180, L-asparaginase was administered as rescue therapy, but the patient progressively lost appetite due to nasal obstruction, so lomustine 10 mg capsule/head (51 mg/m
2) (Bristol-Myers Squibb, Saint-Laurent, Canada) was administered on day 187 [
7]. Nasal obstruction subsequently improved and appetite was restored, but pupillary asymmetry appeared. On day 201, L-asparaginase was administered, but the pupillary asymmetry did not improve and the patient continued to have unstable appetite, so supportive care was given. As her condition remained relatively stable, L-asparaginase was administered on day 216, cyclophosphamide on day 222, and supportive care was continued. On day 226, the patient developed recurrent nystagmus and generalized seizure, and was treated symptomatically, but died on the 228th day. No postmortem examination was performed.
3. Discussion
This case demonstrated the following two points. Prednisolone alone was highly effective in primary feline middle ear lymphoma, and the CHOP protocol was also effective. Feline primary middle ear lymphoma should be carefully monitored for metastasis to the liver. The occurrence of feline middle ear lymphoma is rare, and all previously reported cases have died within a short period of time, so little is known about the pathogenesis [
3,
4,
5]. It is not known whether the course of this case is typical, and more cases should be accumulated in the future.
Prednisolone was effective in this case of lymphoma. The patient was very stable on 5 mg/head/day (equivalent to 1.5-2.2 mg/kg/day), worsened when the dose of prednisolone was reduced, and recovered when the dose was restored. When feline extranodal lymphoma was treated with prednisolone alone, it was reported to be effective in 7 out of 10 cats [
2]. Prednisolone may also be highly effective in lymphoma of the middle ear. However, because of the high efficacy of prednisolone, the use of prednisolone as a symptomatic treatment before diagnosis may result in delaying the diagnosis of the tumor. If clinical signs related to the middle ear improve with prednisolone, lymphoma may need to be included in the differential diagnosis and a further examination should be suggested.
The patient was evaluated as having responded well to medical treatment, as she had been clinically well for 4 months after initiating the multidrug chemotherapy. Lomusitine used as a rescue agent also had a short-term effect. However, the patient had been on prednisolone for 5 months prior to initiation of combination chemotherapy, which may have induced multidrug resistance, resulting in the reduction of the effectiveness of anticancer drugs. If the patient had started multidrug chemotherapy without the long-term use of prednisolone, an even longer remission might have been achieved. Among feline patients with extranodal lymphoma treated with multidrug chemotherapy and achieving complete remission, those who used prednisolone before chemotherapy were reported to have significantly shorter survival time [
2]. In addition, studies with feline lymphoma cells have suggested that the efficacy of doxorubicin and vincristine is reduced, i.e., multidrug resistance may be induced, after the use of prednisolone [
8]. Ideally, multidrug chemotherapy should be initiated as early as possible, minimizing the duration of treatment with prednisolone alone. In previous case reports, brain invasion was observed in the early stages of the disease [
3,
4], and brain infiltration was finally suspected in this case as well. The use of anticancer agents that penetrate the blood-brain barrier may also be useful.
In this case, hepatic metastasis was suspected at the time the beginning of the treatment, so multidrug chemotherapy was selected. Radiotherapy might have been effective if the diagnosis had been made at clinical stage 1, in a localized state. In cases of intranasal lymphoma, which has a relatively high incidence as extranodal lymphoma and in the absence of distant metastasis, long-term remission can be achieved with radiotherapy of the nasal lesions alone [
9]. Primary middle ear lymphoma can also be expected to be curable if diagnosed at clinical stage 1 and radiotherapy can be administered.
In this case, we found that the liver may be the predilection site of metastasis of the primary lymphoma of the middle ear. Although we did not perform cytologic examination of the liver because we could not obtain the owner's consent, it is highly probable that the hepatic lesions in this case were metastatic lesion of the lymphoma, since the diffuse changes in the liver temporarily disappeared after administration of L-asparaginase. Hepatic involvement was also present on day 176, although there was no elevation of hepatic enzyme during follow-up. Santagostino et al. also found hepatic metastases at autopsy [
4], and hepatic metastases may be common in lymphoma of middle ear. Although the mechanism is unknown, renal metastases are known to be common in nasal lymphoma [
9]. In feline extranodal lymphoma, follow-up should be based on knowledge of the pathophysiologic characteristics of each primary site.
The occurrence of feline primary middle ear lymphoma is very rare; given the common finding of middle ear effusion on CT scan [
10], it is even possible that an undiagnosed middle ear lymphoma may exist. Although biopsy of the middle ear is relatively difficult, in cats presenting with prednisolone-responsive middle ear-related symptoms, biopsy of the middle ear should be aggressively suggested to owners.
The immunophenotype of this case was large B cell. Previous cases were T cell [
4,
5], non-B, non-T cell [
3], all of which were large cell-type. Lymphoma is known to have an immunophenotype and cell morphology that are related to prognosis [
1]. Further accumulation of patients with middle ear lymphoma is needed to characterize this type of extranodal lymphoma.