1. Introduction
Pursuing a more predictable surgical procedure to treat gingival recessions has led to technological advances in recent years. Hence, many therapeutic options are available, including soft tissue tunneling [
1]. This is a widely accepted procedure even though it is a highly sensitive and blind technique. It may cause sulcular epithelium and soft tissue trauma, resulting in less-than-acceptable outcomes. Several tunneling methods were proposed to preserve esthetics, maintain papillary integrity, and prevent relapse and scarring resulting from vertical releasing incisions in keratinized tissue [
2,
3]. Suggestions of new areas for creating tunnel access are available, typically in the alveolar mucosa (apical to the mucogingival junction).
Within this context, in 2011, the Vestibular Incision Subperiosteal Tunnel Access (VISTA) technique [
4] was introduced. It presented a modification for the existing modified-Envelope [
5,
6] and Tunnel technique [
2]. It uses new access through the frenum and creates the subperiosteal tunnel instead of a previous supraperiosteal approach. Thus, a total soft tissue elevation (epithelium, connective tissue, and periosteum) is performed. The tissue is gently raised in the interproximal area and the base of each papilla without any superficial incisions. This tunnel communicates with the intrasulcular area and must be sufficiently elevated (beyond the mucogingival junction and through the gingival sulcus of the respective tooth) to reach a low-tension coronal repositioning of the gingiva. In addition, the original technique also includes a membrane complex (beta-tricalcium phosphate [β-TCP] hydrated with rhPDGF-BB).
Another technique reported in 2012 that also elevates the periosteum (full-thickness flap) is named the Pinhole® Surgical technique (PST) [
7]. This technique performs a hole (around 2-3 mm using specific instruments) in the base of the buccal mucosa, just apical to the recession in case of a single defect; or, in case of multiple recessions, in the interradicular area of two adjacent defect sites. Similar to VISTA, an intrasulcular incision is made, keeping the tip of the interdental papilla intact. A tunneling instrument (transmucosal periosteal elevator) is inserted through the pinhole and used for blunt dissection. The flap is coronal and horizontally extended. The original technique uses collagen stripes placed through the pinhole beneath the tunnel for stabilization.
A similar procedure was preconized by Tuttle et al. (2018) [
8], therefore, changing the connective tissue graft (CTG) by advanced-platelet rich fibrin (A-PRF) (centrifuged to 1300 rpm/8 min) and injectable-PRF (i-PRF) (700 rpm/3 min). It was named Gum Drop Technique (GDT), a minimally invasive and biologically enhanced soft-tissue procedure, which places holes (around 4 for the entire arch) in the gingiva apical to the mucogingival junction (MGJ) using a small soft-tissue piercing instrument. Appropriate instruments are used to create a full-thickness tunnel (subperiosteal access). The tissue is detached and advanced coronally, except for the papillae, which are spared and not detached. The flap is then sutured preferentially 2 mm coronal to the CEJ. Otherwise, as reported in an umbrella review developed by Fernandes et al. (2021) [
9], CTG is yet the gold standard biomaterial for root coverage procedures. However, PRF may be considered a feasible substitute for treating GR defects.
In an attempt to evolute the technique, the periosteum was kept intact, and a supraperiosteal approach was developed [
10]. Then, this tunnel access modification can be a more predictable option. The idea was that a supraperiosteal tunnel approach would permit double vascular surfaces for revascularization for the graft (from the buccal flap/interdental papillae and the underlying periosteum), which is extremely important for the healing process, guaranteeing the nutrient supply and revascularization [
11]. It would result in lesser graft necrosis, scarring, and capillary ingrowth, permitting optimal tissue blending. On this hand, Lee et al. (2015) proposed the Modified-Vestibular Incision Supraperiosteal Tunnel Access (M-VISTA) [
10], working over the principles of minimally invasive surgery. It avoids potential complications with tunneling techniques, such as VISTA incision design, supraperiosteal tunnel access instead of the original subperiosteal approach, and the graft used [
4].
Nevertheless, this technique is limited because the access is only through the frenum area, where the authors proposed a “V-shaped” incision for a simultaneous frenectomy. This fact limits its application only in the anterior region. Otherwise, the difficulty found in thin phenotypes was left aside, which will present high chances of mucosal fenestration. Although M-VISTA has a different approach, it may have an unfavorable post-operative and is restricted to the same area. Within this scenario, this article aimed to introduce a new technique for root coverage (RC), the Mixed-Thickness Tunnel access (MiTT), approaching a full-split design, showing the results of a case series. A simpler technique will be demonstrated step-by-step, along with all details, pros, and cons.
3. Results
A total of 16 patients (7 females and 2 males), with ages ranging from 19 and 43 years, needing RC procedures were initially evaluated. However, it included 9 cases that respected the eligibility criteria (described below). All cases followed the described technique above, adjusting to any particularities. Everyone agreed to return after 7-14 days (suture removal), 180 days, and after 1 year. Then, the MiTT technique was applied. The same surgeons operated and assisted patients (T.M. and N.B.M.S.). Registrations happened between 2018 and 2021 in the clinic of the university (Universidade Católica Portuguesa, Viseu, Portugal).
All surgical procedures were performed with a 15C blade or microblade, inserted intrasulcularly to do the vertical incision in the mucosa, accompanied by all periodontal microsurgical kits and tunnel instruments. The measurements were done using a Periodontal probe (Hu-Friedy Color-Coded Single-End Unc Probe 1-15 1/Each, U.S.A.).
Case 1 was a male RT2 case involving tooth #41, with slight interproximal bone loss and gingival recession (GR) of 6mm (height) x 2.5mm (wide), which achieved the MGJ. No occlusal trauma was detected. The patient reported the use of fixed orthodontic brackets in the past. The MiTT protocol was entirely followed, and the suture was done with a composite in the buccal face of the teeth for coronal positioning. The result was followed for 1 year, achieving 82.25% RC (
Figure 2). A similar case was done in a female but involving tooth #31 with 3mm of GR (RT1), presenting a thin gingival tissue. The patient was scheduled for stitches removal after 7 days and recalled for re-evaluation after 1, 6 months, and 1 year. The result was better than case 1, achieving 100% for RC and improving the tissue thickness (
Figure 3). Case 3 involved one tooth (#41 – RT1). The recession had 1mm, and the anterior region had a thin phenotype. In addition, due to the thin thickness of the soft tissue found, the goal was to improve the thickness and cover the root. After applying the MiTT technique with a central vertical incision in the mucosa and using a de-epithelized CTG, an augmented soft tissue thickness was found with a complete RC (100%) (
Figure 4).
Case 4 presented GR in teeth #31 and #41, respectively, with 3mm and 1mm. The case was approached by applying two vertical incisions instead one in the distal of each involved tooth. The procedure and tissue manipulation happened without an event, and the result showed 100% RC (
Figure 5). Increasing the difficulty of the tissue management level, case 5 (
Figure 6) was done in a single tooth (#43), which was buccally positioned, classified as RT1, presenting 3mm of GR. Case performed yet in the anterior and buccal region of the mandible with one vertical incision. After MiTT, double-crossed suture was made to position the soft tissue coronally and keep it stable. After 7 days and 1 year, 100% for RC was reached, and a significant tissue volume was found. Another case (Case 6) was also done in that same region but with increased difficulty. Following toward the posterior region in the lower arch, 3 teeth had GR (#43-#45), respectively, with 1mm, 2mm, and 1mm. It was also found rotation in the premolars. MiTT was done with one vertical incision in the mesial site, and after 7, 14 days, and 1 year, there was 100% RC with no adverse event, even considering the mental nerve proximity (
Figure 7).
The seventh case (
Figure 8) differed from the rest because it involved an esthetic area in an anterior maxillary region. Even with a gingival RT1 in teeth #12-#22, respectively, with 1mm, 1.5mm, 2mm, and 1.5mm, teeth #11 and #21 presented a wide GR (3mm and 4mm, respectively). The case was conducted without adverse events using two linear vertical incisions on the distal to the central incisors. A buccal suture in the facial region of the teeth was made using composite. An adequate healing process was found after 7 days and 1 year, which was permitted by the tissue stability achieved in soft tissue management. The success rate was 100% for RC.
The 8
th case was a RT2 (
Figure 9), with interproximal attachment loss, involving #32 to #42 (GR of 2mm, 3mm, 3mm, and 1mm, respectively). After explaining that the success rate is reduced in these cases compared to RT1, the patient accepted it and was surgically treated. Before starting the procedure, composites were placed in the interproximal of the teeth to apply the double-crossed suture posteriorly [
14]. De-epithelized CTG was collected from the hard palate, and two distal vertical linear incisions were made. The mixed tunnel was performed, and the graft was inserted through the tunnel. The suture was coronally positioned. After 1 year, the healing was favorable, with 100%, 82.35%, 81.25%, and 58.34%, respectively, success rates reached.
The last patient (9
th) was a RT1 case involving 2 adjacent teeth (#11-#12) in the esthetic region (
Figure 10). The recession height was 1mm and 2mm, respectively. The MiTT surgical steps were followed, and the suture was made with coronal traction of the tunnel, which was held by composites on the buccal face. After 30 days, it observed integration of the CTG with minor dehiscence and redness at the gingival margin. After 1 year, the healing improved, and complete root coverage was reached.
The healing period was uneventful, with no significant inflammation or direct event related to the MiTT technique, as observed in the patient’s post-operative. They presented a unanimous report that the discomfort was lower than expected, mainly because of the donor site, and the result was satisfactory after one intervention. Predictably, the RT2 cases had a generally lower percentual success rate compared with the RT1 cases, which obtained complete root coverage for all samples. Also, an increase was found in the keratinized tissue comparing baseline and 1-year follow-up.
Table 1 shows all data obtained, including details. Only the recession variable had significant results (p > 0.001) after 1 year.
4. Discussion
Gingival recession is the apical migration of the gingival margin, exposing the cementoenamel junction (CEJ) and the root surface [
15]. Root coverage procedures aim to treat that defect. Then, coronally positioned flaps (CAF) and tunnel techniques (TUN) have been proposed, associated or not with the CTG [
6,
16,
17,
18,
19]. Although CAFs, with or without vertical incisions [
20,
21,
22,
23], are the most frequently used technique, TUNs have become popular because of the patients’ increasing esthetic awareness and our understanding of the minimally invasive surgery concept [
24]. Both are adequate procedures for treating localized and multiple GRs defects, with a similar percentual of mean RC, more than 80%, as demonstrated in a systematic study with an extremely high level of heterogeneity [
25]. Likewise, comparing CAF and TUN using an acellular dermal matrix (ADM) in ≥ 3 mm Miller class I or II single GR defects showed no statistically significant results [
26]. Similarly, contrasting the modified-CAF (MCAF), without vertical incisions [
23], to coronally positioned TUN for the treatment of single or multiple Miller class I and II GR defects, both with SCTG [
27,
28,
29], efficient mean RC ranging from 80 to 98%, with no significant results between groups at 6 and 12 months. These findings agree with Toledano-Osorio et al. [
30], who reported no differences between techniques, and with González-Febles et al.’s conclusions [
31], who evaluated TUN versus CAF in combination with a CTG for the treatment of multiple GRs; both groups had similar efficacy in terms of RC; however, TUN demonstrated a higher increase in keratinized tissue (KT), with a milder patient’s surgical experience. On the other hand, another study showed that TUN resulted in thicker gingiva and better clinical outcomes compared to CAF regarding recession reduction and root coverage [
32]. Then, this article aimed to introduce the MiTT technique for RC, a tunnel modification, using a mixed design (full and split, respectively, subperiosteal and supraperiosteal) that was applied in a case series study. Our mean RC was similar to those found in the literature, 100% for RT1 cases and around 80.83% for RT2 patients.
4.1. Evolution of the Tunnel Techniques
Historically, in order to reach the proposed technique (MiTT), the procedure named “envelope” was introduced by Raetzke (1985) [
33], which was associated with a subepithelial connective tissue graft (SCTG) into a partial thickness pouch to cover a single recession without any suture. Sequentially, in 1994, it was introduced the modified envelope technique [
5] treated multiple recessions with a supraperiosteal approach and some modifications, such as papilla mobilization and graft suturing. It pursued conserving the existing gingiva and papillae with minimal surgical trauma to the recipient site and keeping firm fixation of the connective tissue graft over the areas of recession. Both techniques provided a dual vascular supply (internal and external) to improve graft survival. In 1999, Zabalegui et al. [
2] presented the term “tunnel” to describe the preparation of a multi-envelope recipient bed connecting adjacent envelopes, keeping the partial thickness design. Therefore, those techniques did not permit yet coronal movement of the soft tissue, exposing the CTG covering the recessions, which may limit its applicability.
In 2002, Azzi et al. [
34] proposed a full-thickness modification in the abovementioned tunnel to permit coronal movement of the entire gingiva-papillary tunnel apparatus. Thus, the advantage was a large portion of CTG could be covered, avoiding necrosis and achieving a more predictable RC result. This technique was named the modified coronally advanced tunnel (MCAT) technique [
35]. Moreover, to minimize trauma, protect the blood supply, and improve wound healing, the tunnel concept was also applied to the microsurgical approach, but still in a supraperiosteal design, using microblade and appropriate instrumentation [
36].
Classically, tunnel techniques (TUN) utilize the incision-free design and preserve the integrity of the papilla, avoiding any detachment, minimizing the risk of losing papilla height and maximizing the blood supply, avoiding scar formation, and keeping an adequate stabilization of the CTG for optimal wound healing [
24,
33,
36]. Otherwise, TUN is a time-consuming and technique-sensitive procedure with limited visibility and access, with the risk of inadequate positioning of the tunnel flap, which can harm the RC outcome. Furthermore, Zuhr et al. [
24] suggested that single gingival recession defects exceeding 3 mm in height may be unsuitable for a tunneling approach unless a modification is employed. Hence, many surgical changes have been proposed to simplify and improve the technique while retaining elements responsible for the success.
Modifications in the TUN technique have been proposed to improve results and facilitate tissue management. As demonstrated in the introduction section, it is possible to report (VISTA) [
4], PST [
7], GDT [
8], and M-VISTA techniques [
10]. As described, VISTA, PST, and GDT implement periosteal elevation (subperiosteal access), commonly used in Dentistry. Even though those techniques present clinical success and preserve the esthetic, two factors might hinder their development/outcome. Firstly, there may be a higher cost of the treatment due to the biomaterials used except for PRF, which has a low cost for preparation; and the other is the reduced vascularization for the graft, subperiosteal access, which comes only from the gingiva. Otherwise, no scientific evidence shows any significant questions for the subperiosteal access. However, it is essential to highlight that the recipient flap's design contributes to soft graft revascularization and esthetics.
Moreover, the temporal healing sequence at the periosteal-bone interface (PBI) should be considered. After raising the periosteum, the process for new adherence takes at least 12 days for 50% of new insertion and 30 days to obtain 75% of reattachment [
37]. In an experimental study [
37], the authors demonstrated that the control animals (without periosteum elevation or any procedure) had a microscopic normal PBI. After 30 and 90 days of healing, both groups (control and test) had similar results, presenting collagen deposition with minimal cellularity, consistent with an organized scar. As far as a higher number of tissues is raised, a higher inflammatory profile may be found.
On the other hand, M-VISTA [
10] implemented a supraperiosteal approach, providing a dual layer of vascularization for the CTG. This technique is highly complex due to the high risk of fenestration, mainly in thin thickness. Thus, this case series worked on a new approach (MiTT) to provide a more conservative treatment, pursuing to keep a partial design (apical to the MGJ) and full design (coronal to the MGJ). It facilitates detachment, improves vascularization of the tunnel, avoids tissue fenestration and scarring, and keeps papilla and esthetic.
Nine patients were included in this study with 1-year follow-up. Similar data were found by comparing our results (MiTT) to the M-VISTA technique [
10]. RT1 cases achieved complete root coverage and a 100% of success rate. Otherwise, as predicted, RT2-diagnosed patients (2 patients) had lower success rates, with a mean of 80.83%. Moreover, M-VISTA uses a more “aggressive” incision in the labial frenum, which is removed. This fact may impair the esthetic result. Compared to MCAT [
35], when approached GR defects Miller class I and II, complete RC was found at 42% of test (collagen matrix) sites and at 85% of control (CTG) sites, respectively (p < 0.05). The mean RC was statistically significant, with 71% at test sites versus 90% at control sites (p < 0.05). Values are considered lower than those found in this case series. Also, mean KTW measured 2.4 ± 0.7 mm at test sites versus 2.7 ± 0.8 mm at control sites (p > 0.05). The values were also inferior to those found in this case series after 1 year, with a gain of 0.9 ± 0.5mm (final KTW was 4.3 ± 1.4mm). In addition, different from the PST and GDT, which make a perforation/hole in the mucosa, MiTT uses a vertical linear incision to preserve local vascularization better [
38].
Finally, comparing TUN and CAF techniques associated with CTG, both allowed significant recession reduction, reaching clinical outcomes stability after four years. The TUN had increased KTW and gain of gingival thickness. However, both techniques were sufficient to keep the patient satisfied regarding esthetic. Otherwise, the esthetic evaluation done by dentists was more favorable for the TUN technique [
39].
4.2. Pros and Cons for MiTT Technique, and Limitations of the Study
Pros: (1) vertical incision on the buccal or lingual side, permitting to keep a better vascularization of the tissues; (2) it is not mandatory to do an intrasulcular incision once the technique uses the vertical incision for detachment. Therefore, it might be considered; (3) this technique applies full-detachment design in the keratinized gingiva region, which can be one of the most interesting advantages, avoiding the risk of fenestration in case of thin tissue thickness and keeping a better vascularization; (4) reduced risk of post-operative scarring, preserving the esthetic; (5) no use of flap, which brings more predictability for the esthetic result; (6) use of split-detachment design in the region apical to the MGJ improves the tissue mobility, keeping the vascularization; (7) minimal surgical trauma to the recipient area; (8) maintenance of the integrity of the involved papillae, also favoring the esthetic preservation; (9) the MiTT design permits a relatively ease suturing while ensuring firm graft fixation and confinement within the recipient site.
Cons: (1) it is necessary to have KTW remnant to obtain a better outcome; (2) intrasulcular incision can cause some damage in the gingival margin area; (3) the tissue detachment through the vertical incision can present some difficulties to be implemented; (4) shortened vestibule may be challenging to do the procedure; (5) there is a moderate level of technical sensitivity, which will depend on the professional experience/ability.
As limitations, it is possible to consider: even though the tissues are completely stable after 1 year, it is regarded as a short-term evaluation; it is suggested future studies applying the long-term assessment. Using MiTT, a reduced vascularization on the bedside was provided for the CTG due to the full-thickness design (subperiosteal) performed, which did not harm the healing or results. The split design (apical to the MGJ) must be carefully completed, observing the thin alveolar mucosa present, avoiding any perforation. This was a case series study testing a new approach for RC with a limited number of patients. The most significant part of the cases was RT1 and developed in the mandible; even though the soft tissue is thinner in this area, increasing the difficulty, more esthetic cases must be done in the maxilla.
Within the limitation of this case series, Mixed-Thickness Tunnel access (MiTT) can be considered a more straightforward approach for minimally invasive surgical technique, which is a feasible option to treat RC with a high success rate, predictability, and esthetic preservation. MiTT is a technique-sensitive and time-consuming procedure with limited visibility, which is expected due to the full-split design procedure. More studies should be developed to evaluate the technique in the long term and compare MiTT with different approaches.
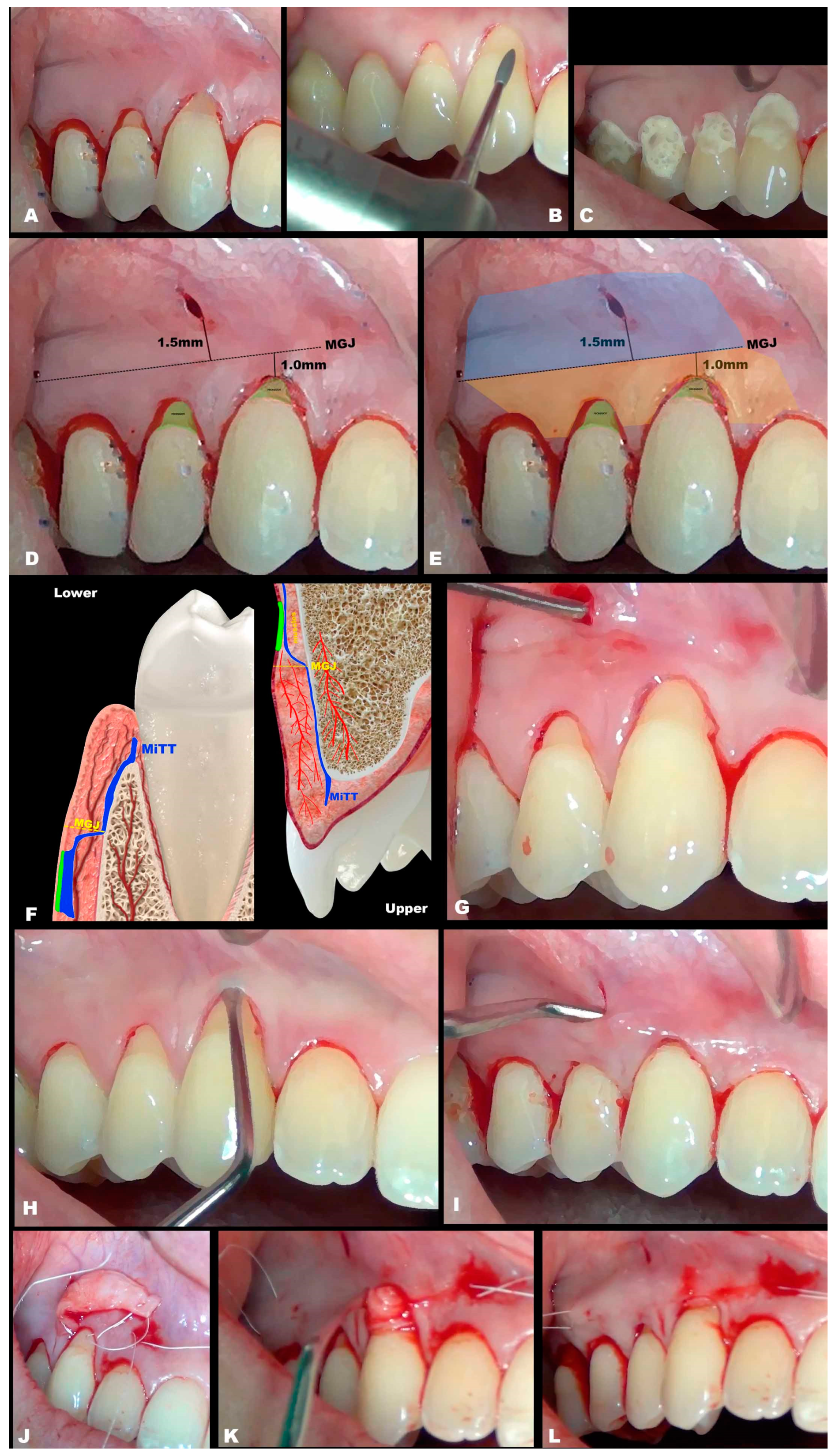
Figure 1.
a. Schematic drawing presenting two recessions (initial presentation). b. Schematic drawing showing the teeth preparation with Perio Set bur. c. Schematic drawing demonstrating the use of tetracycline 1 minute in the recessions and adjacent tissues. Rinsed sterile saline to wash and dried using cotton pellets. Enamel Matrix Derivative (EMD) was applied to improve regenerative performance. d. Schematic drawing showing the KTW, MGJ, and the suggestive distance from the MGJ to the vertical incision (between 1 and 2mm). e. Schematic drawing showing the first recommended area to work (apical to MGJ), in blue color; and the second region localized coronal to the MGJ, in yellow color. f. The sagittal plane presents schematic designs of the tunnel preparation with MiTT (blue line), keeping the vascularization, and showing the reduced risk of fenestration, for the lower and upper tooth. g. Schematic drawing with the mucosa detachment, with split and superficial approach (see the instrument through the tissue), dividing mucosa from the muscles (deep tissue). h. Schematic drawing showing intrasulcular incisions, which are not mandatory. i. Schematic drawing showing full (subperiosteal) detachment of the soft tissue (instrument deeply positioned), reaching the gingival margin and base of the papilla. j. Schematic drawing showing obtention of the connective tissue graft (CTG), which will be inserted in the site receptor. k. Schematic drawing showing both sides of the CTG already inserted. l. Schematic drawing presenting the CTG in position, using two sutures, one in the mesial and another for the distal. After, through the sutures, the CTG will be positioned 1mm coronal to the cement-enamel junction (CEJ) and stabilized.
Figure 1.
a. Schematic drawing presenting two recessions (initial presentation). b. Schematic drawing showing the teeth preparation with Perio Set bur. c. Schematic drawing demonstrating the use of tetracycline 1 minute in the recessions and adjacent tissues. Rinsed sterile saline to wash and dried using cotton pellets. Enamel Matrix Derivative (EMD) was applied to improve regenerative performance. d. Schematic drawing showing the KTW, MGJ, and the suggestive distance from the MGJ to the vertical incision (between 1 and 2mm). e. Schematic drawing showing the first recommended area to work (apical to MGJ), in blue color; and the second region localized coronal to the MGJ, in yellow color. f. The sagittal plane presents schematic designs of the tunnel preparation with MiTT (blue line), keeping the vascularization, and showing the reduced risk of fenestration, for the lower and upper tooth. g. Schematic drawing with the mucosa detachment, with split and superficial approach (see the instrument through the tissue), dividing mucosa from the muscles (deep tissue). h. Schematic drawing showing intrasulcular incisions, which are not mandatory. i. Schematic drawing showing full (subperiosteal) detachment of the soft tissue (instrument deeply positioned), reaching the gingival margin and base of the papilla. j. Schematic drawing showing obtention of the connective tissue graft (CTG), which will be inserted in the site receptor. k. Schematic drawing showing both sides of the CTG already inserted. l. Schematic drawing presenting the CTG in position, using two sutures, one in the mesial and another for the distal. After, through the sutures, the CTG will be positioned 1mm coronal to the cement-enamel junction (CEJ) and stabilized.
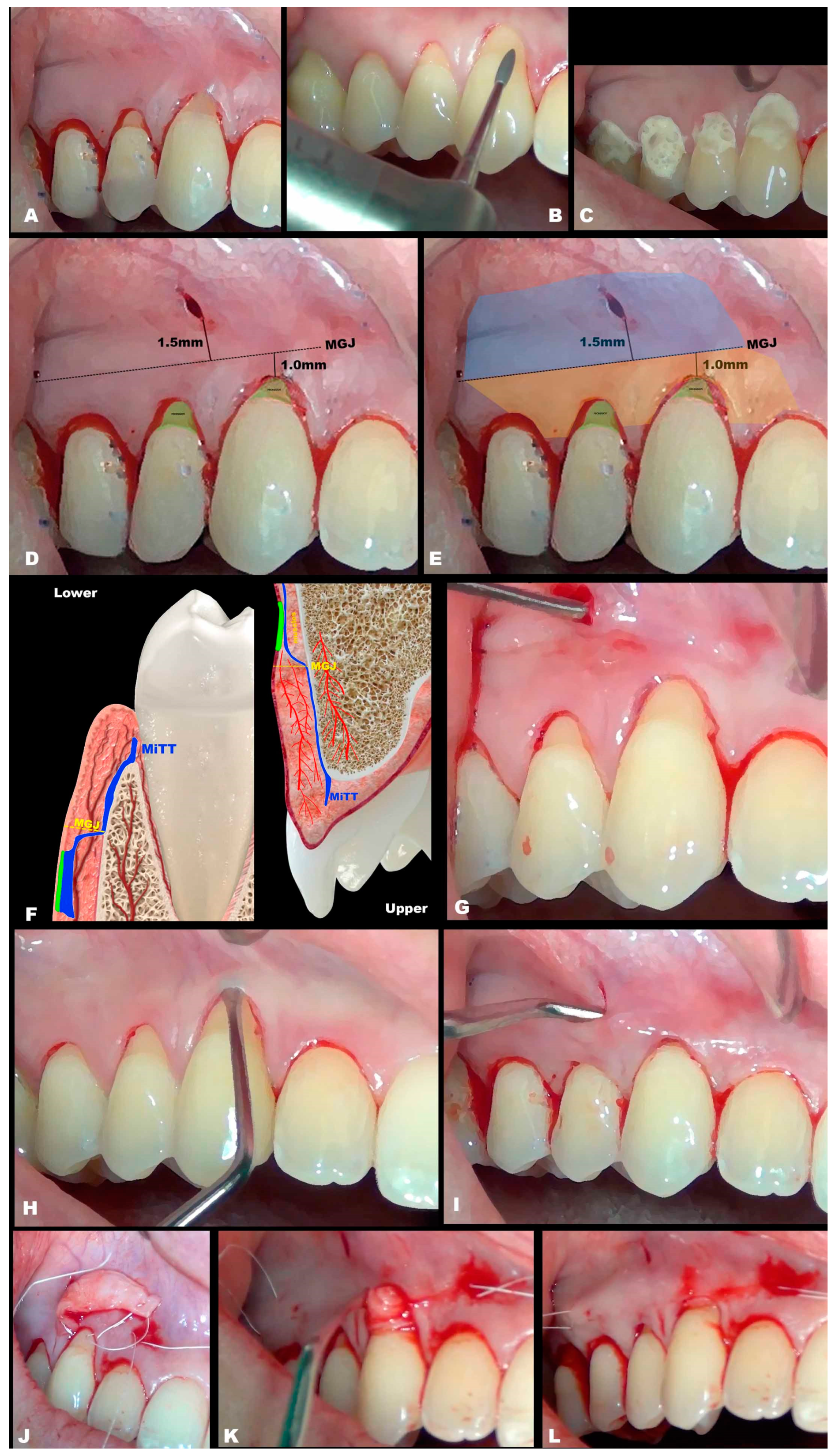
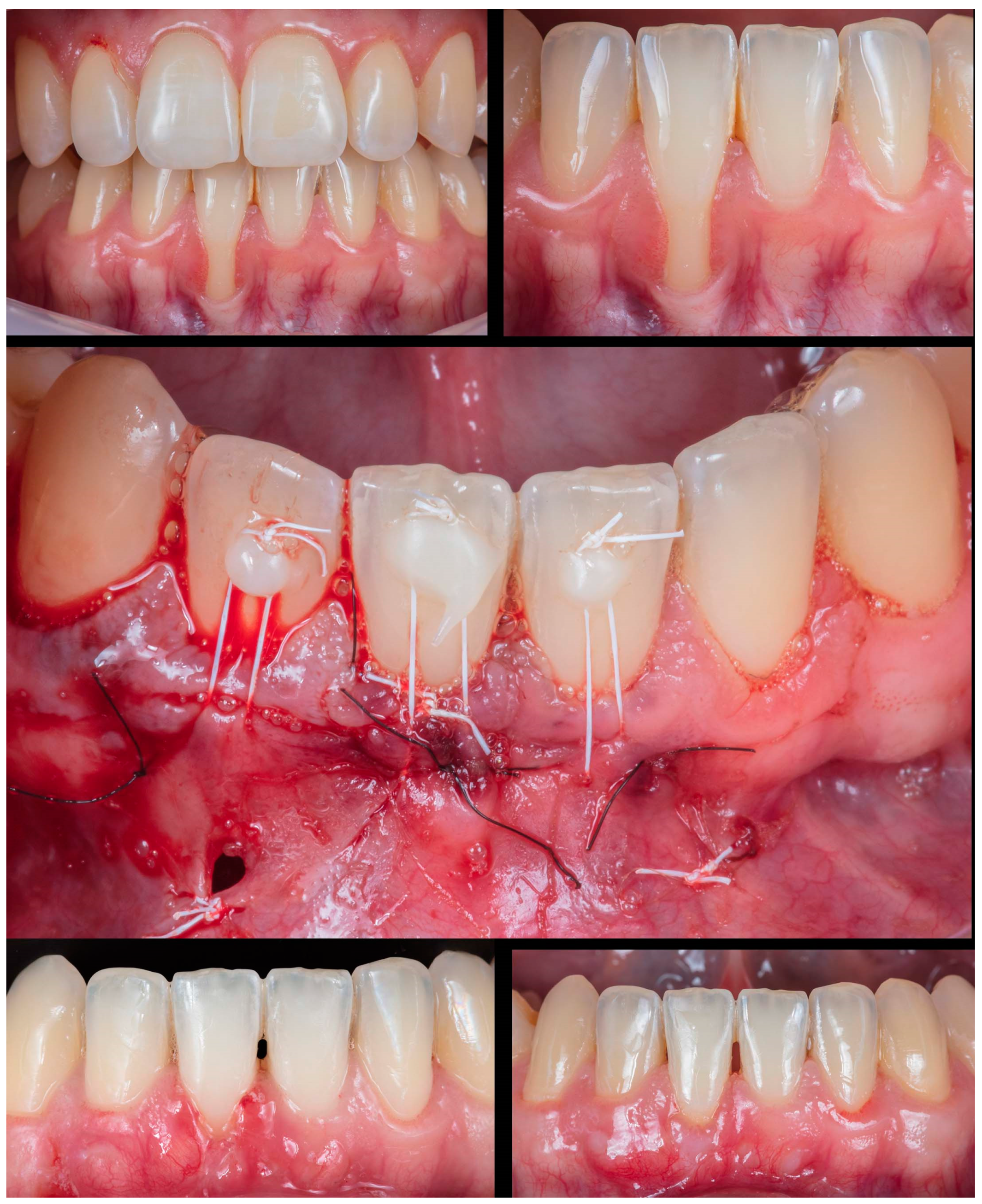
Figure 2.
Case 1 shows initial pictures of the GR defect (#41); immediate post-operative; and the healing period of 1 month and 6 months.
Figure 2.
Case 1 shows initial pictures of the GR defect (#41); immediate post-operative; and the healing period of 1 month and 6 months.
Figure 3.
Case 2 shows initial pictures of the GR defect (#31); and the healing period after 1 month and 1 year.
Figure 3.
Case 2 shows initial pictures of the GR defect (#31); and the healing period after 1 month and 1 year.
Figure 4.
Case 3 shows initial pictures of the GR defect (#41) and thin phenotype present; CTG over the receptor site and one vertical incision to apply MiTT; and the healing period after 6 months.
Figure 4.
Case 3 shows initial pictures of the GR defect (#41) and thin phenotype present; CTG over the receptor site and one vertical incision to apply MiTT; and the healing period after 6 months.
Figure 5.
Case 4 shows initial pictures of the GR defect (#41 and #31) and thin phenotype present; CTG over the receptor site with 2 distal vertical incisions to apply MiTT; suture performed; and the healing period after 6 months.
Figure 5.
Case 4 shows initial pictures of the GR defect (#41 and #31) and thin phenotype present; CTG over the receptor site with 2 distal vertical incisions to apply MiTT; suture performed; and the healing period after 6 months.
Figure 6.
Case 5 shows initial pictures of the GR defect (#43); a picture showing the final aspect immediately after surgery (double-crossed suture); and the healing period after 1 and 1 year.
Figure 6.
Case 5 shows initial pictures of the GR defect (#43); a picture showing the final aspect immediately after surgery (double-crossed suture); and the healing period after 1 and 1 year.
Figure 7.
Case 6 shows initial pictures of the multiple GR defects (#43-#45); a picture showing the final aspect immediately after surgery (double-crossed suture); and the healing period after 1 and 6 months.
Figure 7.
Case 6 shows initial pictures of the multiple GR defects (#43-#45); a picture showing the final aspect immediately after surgery (double-crossed suture); and the healing period after 1 and 6 months.
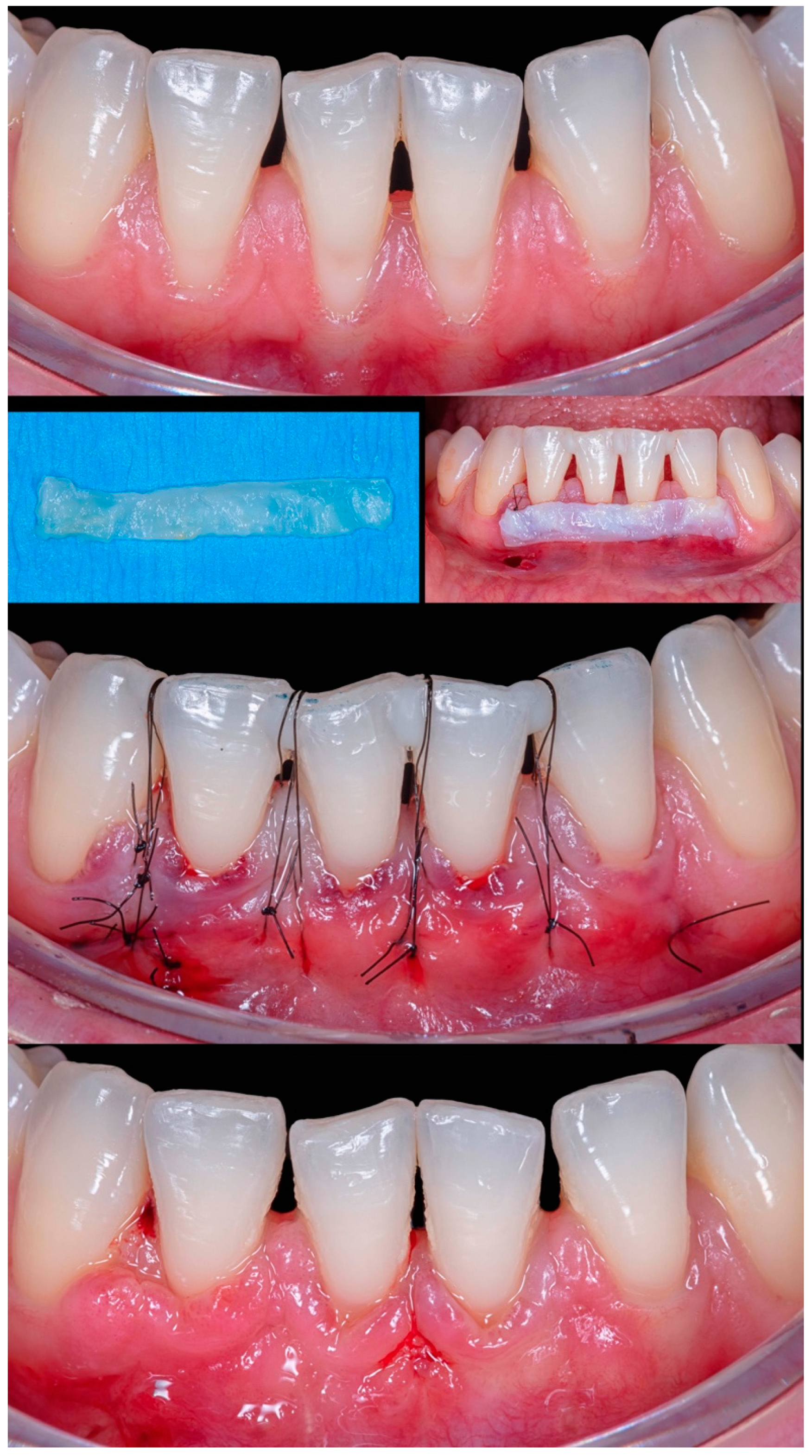
Figure 8.
Case 7 shows initial pictures of the GR defects (#12-#22); a picture showing the final aspect immediately after surgery; and the healing period after 14 days and 1 year.
Figure 8.
Case 7 shows initial pictures of the GR defects (#12-#22); a picture showing the final aspect immediately after surgery; and the healing period after 14 days and 1 year.
Figure 9.
Case 8 shows initial pictures of the multiple GR defects (#42-#32) and thin phenotype present; CTG over the receptor site and two vertical incisions at the distal to apply MiTT; a picture showing the final aspect immediately after surgery; and the healing period after 1 month.
Figure 9.
Case 8 shows initial pictures of the multiple GR defects (#42-#32) and thin phenotype present; CTG over the receptor site and two vertical incisions at the distal to apply MiTT; a picture showing the final aspect immediately after surgery; and the healing period after 1 month.
Figure 10.
Case 9 shows initial pictures of the GR defects (#12-#13); CTG already positioned through the vertical linear incision; a picture showing the final aspect immediately after surgery; and the healing period after 6 months.
Figure 10.
Case 9 shows initial pictures of the GR defects (#12-#13); CTG already positioned through the vertical linear incision; a picture showing the final aspect immediately after surgery; and the healing period after 6 months.
Table 1.
Clinical information from the included cases. Data from baseline and after 1 year.
Table 1.
Clinical information from the included cases. Data from baseline and after 1 year.
| |
Classification |
Gender |
Tooth/teeth with REC |
Initial REC height (mm) |
Initial REC width (mm) |
Initial PD (mm) |
Initial KTW (mm) |
Final REC height (mm) |
Final PD (mm) |
Final KTW (mm) |
Success rate (%) |
p-value |
| |
|
|
|
baseline |
6-month follow-up |
|
| Case 1 |
RT2 |
M |
41 |
6.2 |
2.5 |
1.0 |
.3 |
1.1 |
2.0 |
4.3 |
82.25 |
REC:
p < 0.0001
PD:
p = 0.2771
KTW:
p = 0.1013
|
| Case 2 |
RT1 |
F |
31 |
3.3 |
1.7 |
.5 |
.3 |
none |
1.0 |
3.7 |
100 |
| Case 3 |
RT1 |
F |
41 |
1.2 |
2.1 |
1.0 |
3.3 |
none |
.5 |
7.3 |
100 |
| Case 4 |
RT1 |
F |
41 / 31 |
1.4 / 1.2 |
2.1 / 1.8 |
1.0 / .5 |
3.1 / 2.9 |
none |
1.0 / .5 |
3.7 / 4.0 |
100 (for all) |
| Case 5 |
RT1 |
M |
43 |
1.5 |
2.3 |
1.0 |
1.3 |
none |
1.5 |
4.4 |
100 |
| Case 6 |
RT1 |
F |
43 / 44 / 45 |
1.2 / 2.1 / 1.4 |
2.6 / 3.1 / 2.8 |
2.0 / 1.5 / 1.0 |
3.0 / 3.8 / 3.8 |
none |
1.5 / 1.0 / 1.0 |
2.1 / 2.8 / 5.3 |
100 (for all) |
| Case 7 |
RT1 |
F |
12 / 11 / 21 / 22 |
1.1 / 1.5 / 2.4 / 1.5 |
1.5 / 3 / 4 / 2 |
1.0 / 2.0 / 1.5 / 2.0 |
5.4 / 5.0 / 6.3 / 6.9 |
none |
1.0 / 2.5 / 2.5 / 1.5 |
4.3 / 5.7 / 6.0 / 6.3 |
100 (for all) |
| Case 8 |
RT2 |
F |
42 / 41 / 31 / 32 |
2.2 / 3.4 / 3.2 / 1.2 |
2.3 / 2.5 / 3 / 2.7 |
.5 / .5 / .5 / 1.0 |
2.4 / 1.9 / 1.5 / 3.5 |
0 / 0.6 / 0.6 / 0.5 |
1.5 / 1.0 / 1.0 / 1.0 |
3.6 / 2.9 / 2.1 / 3.3 |
100 / 82.35 / 81.25 / 58.34 |
| Case 9 |
RT1 |
F |
12 / 13 |
1.3 / 2.1 |
2.2 / 2.3 |
1.5 / 2.0 |
4.4 / 5.3 |
none |
2.5 / 1.5 |
4.6 / 5.2 |
100 (for all) |