Submitted:
20 August 2023
Posted:
21 August 2023
You are already at the latest version
Abstract
Keywords:
Introduction:
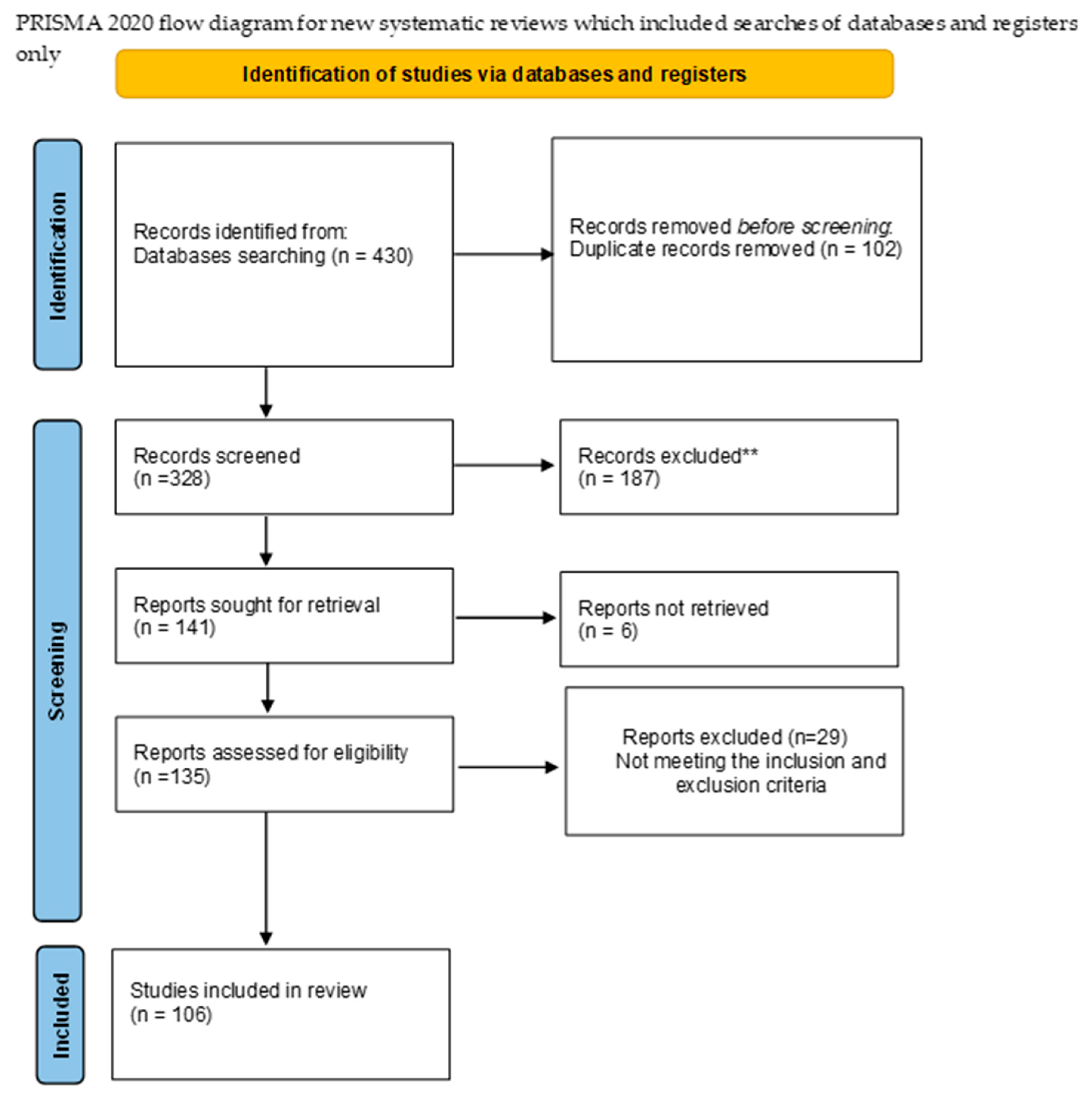
Materials and methods:
Understanding Diabetes:
There are three main types of diabetes:
Effects of diabetes on intimate health:
Erectile Dysfunction: Causes and Symptoms:
Symptoms of ED:
The Interplay of Diabetes and Erectile Dysfunction:
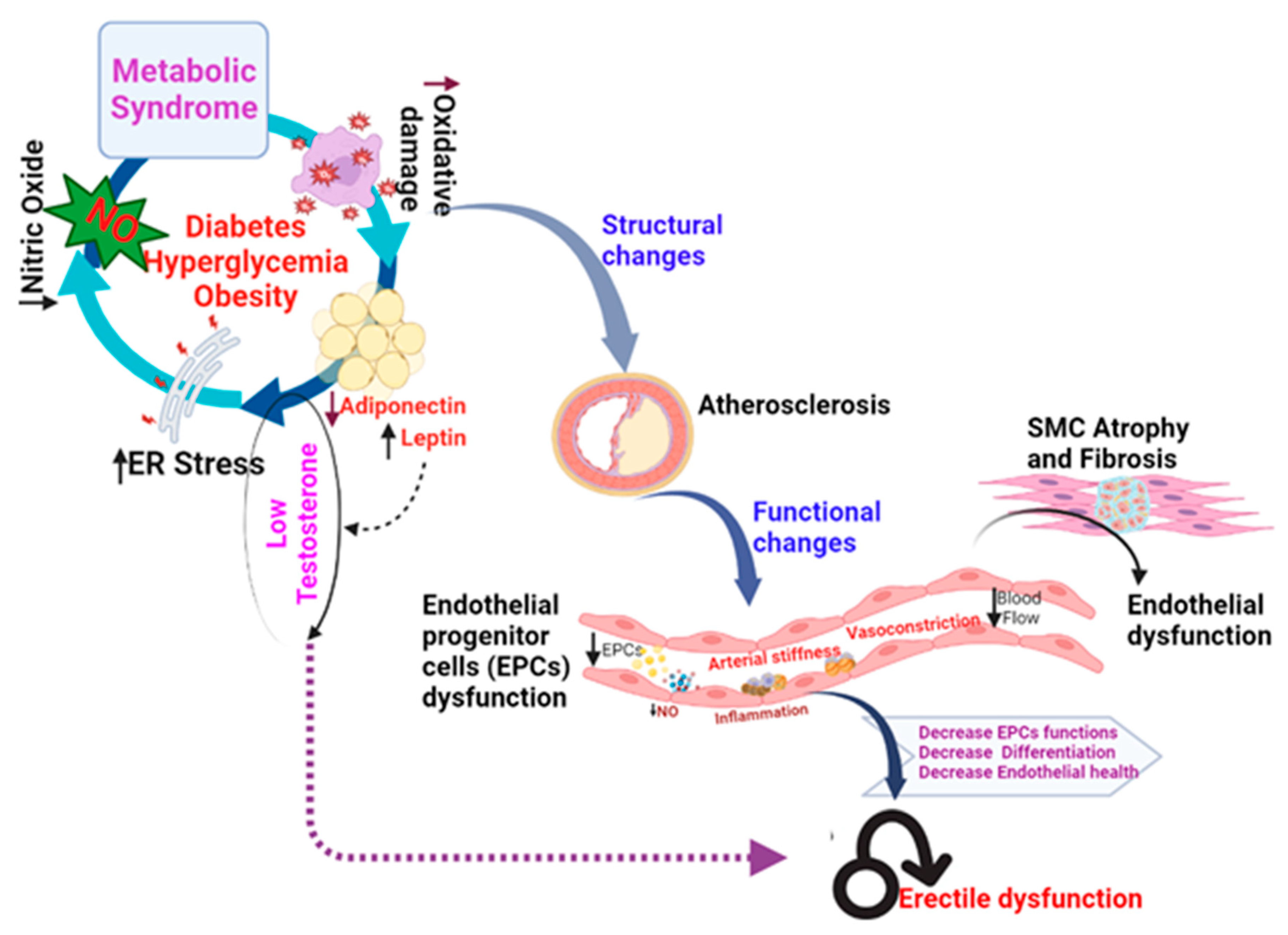
Vascular Damage:
Neural Damage:
Diabetic Peripheral Neuropathy:
Diabetic Autonomic Neuropathy:
Neurotransmitter Imbalance:
Chronic Inflammation:
Oxidative Stress:
Other risk factors that contribute to the ED:
Obesity:
Smoking:
Sedentary Lifestyle:
High Blood Pressure and Cardiovascular Disease:
Psychological Factors:
Strategies for Managing and Preventing Erectile Dysfunction in Diabetic Individuals:
Medications and treatments for ED:
Oral Medications (Phosphodiesterase type 5 inhibitors - PDE5 inhibitors):
Penile Injection:
Vacuum Erection Devices (VEDs):
Intraurethral Suppositories:
Natural Therapies:
Surgical Interventions:
Management of ED in diabetic patient:
Conclusion:
References
- PAHO/WHO and P. A. H. Organization, "Sexual and Reproductive Health," 2002.
- S. Gruskin, V. Yadav, A. Castellanos-Usigli, G. Khizanishvili, and E. Kismödi, "Sexual health, sexual rights and sexual pleasure: meaningfully engaging the perfect triangle," (in en). [CrossRef]
- "Diabetes Quick Facts | Basics | Diabetes | CDC," 2022-09-21T01:30:51Z 2022.
- M. M. Mohib et al., "Protective role of green tea on diabetic nephropathy—A review," (in en), , 2016. Available online: http://www.editorialmanager.com/cogentbio.
- M. MS et al., "Glucagon Prevents Cytotoxicity Induced by Methylglyoxal in a Rat Neuronal Cell Line Model," Biomolecules, vol. 11, no. 2, 02/15/2021 2021. [CrossRef]
- "CDC Global Health - Infographics - World Diabetes Day," 2020-01-13T03:23:26Z 2020.
- "Diabetes - PAHO/WHO | Pan American Health Organization," 2022.
- M. MS et al., "Glucagon-Like Peptide-1 Receptor Agonist Protects Dorsal Root Ganglion Neurons against Oxidative Insult," Journal of diabetes research, vol. 2019, 02/21/2019 2019. [CrossRef]
- F. Cosentino and G. E. Assenza, "Diabetes and inflammation," (in eng), Herz, vol. 29, no. 8, pp. 749-59, Dec 2004. [CrossRef]
- W. K, K. C, and F. J, "Sexual health and function in women with diabetes," Diabetic medicine : a journal of the British Diabetic Association, vol. 38, no. 11, 2021 Nov 2021. [CrossRef]
- D. Association. "Sex and Diabetes | ADA.". Available online: https://diabetes.org/healthy-living/sexual-health/sex-diabetes.
- R. RC, W. R, S. S, and G. N, "Epidemiology of erectile dysfunction: the role of medical comorbidities and lifestyle factors," The Urologic clinics of North America, vol. 32, no. 4, 2005 Nov 2005. [CrossRef]
- K. Y et al., "High prevalence of erectile dysfunction in diabetes: a systematic review and meta-analysis of 145 studies," Diabetic medicine : a journal of the British Diabetic Association, vol. 34, no. 9, 2017 Sep 2017. [CrossRef]
- T. D, B. DS, S. VK, P. AK, and Y. BK, "Association Between Erectile Dysfunction and Type 2 Diabetes Mellitus," Journal of Nepal Health Research Council, vol. 19, no. 2, 09/06/2021 2021. [CrossRef]
- C. G, G. CB, C. D, G. P, and N. E, "Sexual dysfunction at the onset of type 2 diabetes: the interplay of depression, hormonal and cardiovascular factors," The journal of sexual medicine, vol. 11, no. 8, 2014 Aug 2014. [CrossRef]
- W. X, Y. X, C. Y, W. S, and W. W, "High Prevalence of Erectile Dysfunction in Diabetic Men With Depressive Symptoms: A Meta-Analysis," The journal of sexual medicine, vol. 15, no. 7, 2018 Jul 2018. [CrossRef]
- F. D et al., "Erectile dysfunction in diabetic subjects in Italy. Gruppo Italiano Studio Deficit Erettile nei Diabetici," Diabetes care, vol. 21, no. 11, 1998 Nov 1998. [CrossRef]
- T. CC and P. LH, "Update on diabetes classification," The Medical clinics of North America, vol. 99, no. 1, 2015 Jan 2015. [CrossRef]
- C. A and J. FR, "[Classification of diabetes: an increasing heterogeneity]," Revue medicale suisse, vol. 11, no. 477, 06/03/2015 2015.
- A. N, A. F, B. MJ, M. M, G. F, and K. IJ, "Gestational diabetes insipidus: a review of an underdiagnosed condition," Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC, vol. 32, no. 3, 2010 Mar 2010. [CrossRef]
- C. A and P. F, "Variability of risk factors and diabetes complications," Cardiovascular diabetology, vol. 20, no. 1, 05/07/2021 2021. [CrossRef]
- B. T et al., "Epigenetic basis of diabetic vasculopathy," Frontiers in endocrinology, vol. 13, 12/09/2022 2022. [CrossRef]
- W. PW, D. A. RB, L. D, B. AM, S. H, and K. WB, "Prediction of coronary heart disease using risk factor categories," Circulation, vol. 97, no. 18, 05/12/1998 1998. [CrossRef]
- Sjoholm and T. Nystrom, "Endothelial inflammation in insulin resistance," (in eng), Lancet, vol. 365, no. 9459, pp. 610-2, Feb 12-18 2005. [CrossRef]
- M. HC and M. CA, "Determinants of atherosclerosis in the young. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group," The American journal of cardiology, vol. 82, no. 10B, 11/26/1998 1998. [CrossRef]
- B. V and P. I, "Coronary heart disease risk factors in women," European heart journal, vol. 15, no. 11, 1994 Nov 1994. [CrossRef]
- D. Deshpande, P. AD Deshpande, MPH, is Research Assistant Professor, Division of Health Behavior Research, Department of Medicine, Washington University School of Medicine, St Louis, MO 63110 (USA). At the time of manuscript preparation and submission, Dr Deshpande was Assistant Professor, Department of Community Health, Saint Louis University School of Public Health, St Louis, Missouri., M. Harris-Hayes, P. M Harris-Hayes, DPT, OCS, is Assistant Professor, Program in Physical Therapy, Washington University School of Medicine., M. Schootman, and P. M Schootman, is Associate Professor, Division of Health Behavior Research, Department of Medicine, Washington University School of Medicine., "Epidemiology of Diabetes and Diabetes-Related Complications," Physical Therapy, vol. 88, no. 11, pp. 1254-1264, 2023. [CrossRef]
- S. PH et al., "The effect of diabetes mellitus on prognosis and serial left ventricular function after acute myocardial infarction: contribution of both coronary disease and diastolic left ventricular dysfunction to the adverse prognosis. The MILIS Study Group," Journal of the American College of Cardiology, vol. 14, no. 1, 1989 Jul 1989. [CrossRef]
- B. G et al., "Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study," Diabetologia, vol. 50, no. 5, 2007 May 2007. [CrossRef]
- T. MC, W. AJ, B. OJ, C. ME, and M. TH, "The burden of chronic kidney disease in Australian patients with type 2 diabetes (the NEFRON study)," The Medical journal of Australia, vol. 185, no. 3, 08/07/2006 2006. [CrossRef]
- D. JP, P. HH, H. LG, R. M, R. G, and L. JB, "Renal Dysfunction in the Presence of Normoalbuminuria in Type 2 Diabetes: Results from the DEMAND Study," Cardiorenal medicine, vol. 2, no. 1, 2012 Feb 2012. [CrossRef]
- M. S. Mohiuddin et al., "Glucagon Prevents Cytotoxicity Induced by Methylglyoxal in a Rat Neuronal Cell Line Model," Biomolecules, vol. 11, no. 2, 2021. [CrossRef]
- M. Mohabbulla Mohib et al., "Protective role of green tea on diabetic nephropathy—A review," Cogent Biology, vol. 2, no. 1, p. 1248166, 2016/12/31 2016. [CrossRef]
- M. Motegi et al., "Deficiency of glucagon gene-derived peptides induces peripheral polyneuropathy in mice," Biochem Biophys Res Commun, vol. 532, no. 1, pp. 47-53, 10/29/2020 2020. [CrossRef]
- L. KY, H. WH, L. YB, W. CY, and C. TJ, "Update in the epidemiology, risk factors, screening, and treatment of diabetic retinopathy," Journal of diabetes investigation, vol. 12, no. 8, 2021 Aug 2021. [CrossRef]
- C. N, M. P, and W. TY, "Diabetic retinopathy," Lancet (London, England), vol. 376, no. 9735, 07/10/2010 2010. [CrossRef]
- K. S, "Diabetes and infection: is there a link?--A mini-review," Gerontology, vol. 59, no. 2, 2013 2013. [CrossRef]
- G. H, "[Infection and diabetes]," La Revue de medecine interne, vol. 14, no. 1, 1993 Jan 1993. [CrossRef]
- J. Casqueiro, J. Casqueiro, and C. Alves, "Infections in patients with diabetes mellitus: A review of p... : Indian Journal of Endocrinology and Metabolism," 2023. [CrossRef]
- CDCgov, "Diabetes and Mental Health | CDC," 2023-05-15T09:11:07Z 2023.
- C. Rask-Madsen and G. L. King, "Vascular complications of diabetes: mechanisms of injury and protective factors," (in eng), Cell Metab, vol. 17, no. 1, pp. 20-33, Jan 08 2013. [CrossRef]
- B. MEH, K. EKH, S. RB, S. E, and H. A, "Sexual dysfunction in women with type 1 diabetes in Norway: A qualitative study of women's experiences," Diabetic medicine : a journal of the British Diabetic Association, vol. 39, no. 7, 2022 Jul 2022. [CrossRef]
- S. A and R. U, "Intimacy and women with type 2 diabetes: an exploratory study using focus group interviews," The Diabetes educator, vol. 29, no. 4, 2003 Jul-Aug 2003. [CrossRef]
- L. Mohammed, G. Jha, I. Malasevskaia, H. K. Goud, and A. Hassan, "The Interplay Between Sugar and Yeast Infections: Do Diabetics Have a Greater Predisposition to Develop Oral and Vulvovaginal Candidiasis?," (in en), Cureus, vol. 13, 2021/02/18 2021. [CrossRef]
- A. Bickett and H. Tapp, "Anxiety and diabetes: Innovative approaches to management in primary care," (in en), https://doi.org/10.1177/1535370216657613, research-article 2016-07-06 2016. [CrossRef]
- A.-M. N, P.-B. R, W. H, and S. AV, "Autonomic neuropathy and urologic complications in diabetes," Autonomic neuroscience : basic & clinical, vol. 229, 2020 Dec 2020. [CrossRef]
- D. GL et al., "The effects of diabetes on male fertility and epigenetic regulation during spermatogenesis," Asian journal of andrology, vol. 17, no. 6, 2015 Nov-Dec 2015. [CrossRef]
- S. R and G. H, "Erectile dysfunction," Lancet (London, England), vol. 381, no. 9861, 01/12/2013 2013. [CrossRef]
- F. JF et al., "Combined Transplantation of Mesenchymal Stem Cells and Endothelial Progenitor Cells Restores Cavernous Nerve Injury-Related Erectile Dysfunction," The journal of sexual medicine, vol. 15, no. 3, 2018 Mar 2018. [CrossRef]
- T.-P. D, I. N, R. K, and V. C, "Interactions between erectile dysfunction, cardiovascular disease and cardiovascular drugs," Nature reviews. Cardiology, vol. 19, no. 1, 2022 Jan 2022. [CrossRef]
- R. Ng et al., "Smoking, drinking, diet and physical activity—modifiable lifestyle risk factors and their associations with age to first chronic disease," International Journal of Epidemiology, vol. 49, no. 1, pp. 113-130, 2023. [CrossRef]
- C. M, R. A, B. PS, B. F, and K. A, "Direct actions of adiponectin on changes in reproductive, metabolic, and anti-oxidative enzymes status in the testis of adult mice," General and comparative endocrinology, vol. 279, 08/01/2019 2019. [CrossRef]
- C. M, R. A, B. PS, and K. A, "Protective role of adiponectin against testicular impairment in high-fat diet/streptozotocin-induced type 2 diabetic mice," Biochimie, vol. 168, 2020 Jan 2020. [CrossRef]
- R. Velurajah, O. Brunckhorst, M. Waqar, I. McMullen, and K. Ahmed, "Erectile dysfunction in patients with anxiety disorders: a systematic review," (in En), International Journal of Impotence Research, OriginalPaper vol. 34, no. 2, pp. 177-186, 2021-02-18 2021. [CrossRef]
- @mayoclinic, "Erectile dysfunction - Symptoms and causes," 2023.
- M. I. Maiorino, G. Bellastella, and K. Esposito, "Diabetes and sexual dysfunction: current perspectives," (in English), Diabetes, Metabolic Syndrome and Obesity, vol. 7, pp. 95-105, 2023. [CrossRef]
- F. C, K. A, I. K, D. P, K. M, and D. K, "Microvascular Complications of Type 2 Diabetes Mellitus," Current vascular pharmacology, vol. 18, no. 2, 2020 2020. [CrossRef]
- A. Ponholzer et al., "Is penile atherosclerosis the link between erectile dysfunction and cardiovascular risk? An autopsy study," (in En), International Journal of Impotence Research, OriginalPaper vol. 24, no. 4, pp. 137-140, 2012-03-22 2012. [CrossRef]
- D. W, C. M, P. S, S. HA, and O. L, "Adipocyte CAMK2 deficiency improves obesity-associated glucose intolerance," Molecular metabolism, vol. 53, 2021 Nov 2021. [CrossRef]
- M. DB, C. HC, and K. PJ, "Pharmacologic management of peripheral vascular disease," The Surgical clinics of North America, vol. 78, no. 3, 1998 Jun 1998. [CrossRef]
- M. Choubey. "Growth Hormone and Insulin-like Growth Factor-I: Novel Insights into the Male Reproductive Health." https://scholar.google.com/citations?view_op=view_citation&hl=en&user=-oBBDNsAAAAJ&citation_for_view=-oBBDNsAAAAJ:ye4kPcJQO24C.
- A. Ranjan, M. Choubey, T. Yada, and A. Krishna, "Immunohistochemical localization and possible functions of nesfatin-1 in the testis of mice during pubertal development and sexual maturation," (in En), Journal of Molecular Histology, OriginalPaper vol. 50, no. 6, pp. 533-549, 2019-09-20 2019. [CrossRef]
- V. AM, M. LL, B. C, and F. EL, "Short-term hyperglycemia produces oxidative damage and apoptosis in neurons," FASEB journal : official publication of the Federation of American Societies for Experimental Biology, vol. 19, no. 6, 2005 Apr 2005. [CrossRef]
- F. EL, N. KA, J. TS, and B. DLH, "New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and Pain," Neuron, vol. 93, no. 6, 03/22/2017 2017. [CrossRef]
- S. Akter, M. Choubey, M. M. Mohib, S. Arbee, M. A. T. Sagor, and M. S. Mohiuddin, "Stem Cell Therapy in Diabetic Polyneuropathy: Recent Advancements and Future Directions," (in en), Brain Sciences, Review vol. 13, no. 2, p. 255, 2023-02-02 2023. [CrossRef]
- M. Caitlin W. Hicks, MS Dan Wang, MS B. Gwen Windham, MD, MHS Elizabeth Selvin, PhD, MPH, "Association of Peripheral Neuropathy with Erectile Dysfunction in US Men - The American Journal of Medicine," 2020. [CrossRef]
- F. S et al., "Diabetic peripheral neuropathy and prevalence of erectile dysfunction in Japanese patients aged," International journal of impotence research, vol. 29, no. 1, 2017 Jan 2017. [CrossRef]
- Q. R et al., "Autonomic neuropathy and sexual impotence in diabetic patients: analysis of cardiovascular reflexes," Andrologia, vol. 21, no. 4, 1989 Jul-Aug 1989. [CrossRef]
- S. A, C. M, B. P, and K. A, "Adiponectin and Chemerin: Contrary Adipokines in Regulating Reproduction and Metabolic Disorders," Reproductive sciences (Thousand Oaks, Calif.), vol. 25, no. 10, 2018 Oct 2018. [CrossRef]
- R. Pop-Busui et al., "Cardiovascular Autonomic Neuropathy, Erectile Dysfunction and Lower Urinary Tract Symptoms in Men with Type 1 Diabetes: Findings from the DCCT/EDIC," (in EN), research-article 2015-06 2015. [CrossRef]
- A. KE, "Mechanisms of penile erection and basis for pharmacological treatment of erectile dysfunction," Pharmacological reviews, vol. 63, no. 4, 2011 Dec 2011. [CrossRef]
- M. R. Melis, F. Sanna, and A. Argiolas, "Dopamine, Erectile Function and Male Sexual Behavior from the Past to the Present: A Review," (in en), Brain Sciences, Review vol. 12, no. 7, p. 826, 2022-06-24 2022. [CrossRef]
- K. A et al., "Insulin resistance in brain alters dopamine turnover and causes behavioral disorders," Proceedings of the National Academy of Sciences of the United States of America, vol. 112, no. 11, 03/17/2015 2015. [CrossRef]
- S. Tsalamandris, "The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives," 2023. [CrossRef]
- M. Y. Donath and S. E. Shoelson, "Type 2 diabetes as an inflammatory disease," (in En), Nature Reviews Immunology, ReviewPaper vol. 11, no. 2, pp. 98-107, 2011-01-14 2011. [CrossRef]
- P. Theofilis et al., "Inflammatory Mechanisms Contributing to Endothelial Dysfunction," (in en), Biomedicines, Review vol. 9, no. 7, p. 781, 2021-07-06 2021. [CrossRef]
- R. Dantzer, "Neuroimmune Interactions: From the Brain to the Immune System and Vice Versa," (in en), https://doi.org/10.1152/physrev.00039.2016, review-article 2017 Dec 20 2017. [CrossRef]
- M. S. Mohiuddin et al., "Glucagon-Like Peptide-1 Receptor Agonist Protects Dorsal Root Ganglion Neurons against Oxidative Insult," (in eng), J Diabetes Res, vol. 2019, p. 9426014, 2019. [CrossRef]
- M. Wronka, J. Krzemińska, E. Młynarska, J. Rysz, and B. Franczyk, "The Influence of Lifestyle and Treatment on Oxidative Stress and Inflammation in Diabetes," (in en), International Journal of Molecular Sciences, Review vol. 23, no. 24, p. 15743, 2022-12-12 2022. [CrossRef]
- Y. P et al., "Liraglutide Ameliorates Erectile Dysfunction via Regulating Oxidative Stress, the RhoA/ROCK Pathway and Autophagy in Diabetes Mellitus," Frontiers in pharmacology, vol. 11, 08/12/2020 2020. [CrossRef]
- R. S et al., "Environmental Factors-Induced Oxidative Stress: Hormonal and Molecular Pathway Disruptions in Hypogonadism and Erectile Dysfunction," Antioxidants (Basel, Switzerland), vol. 10, no. 6, 05/24/2021 2021. [CrossRef]
- M. Taskiran, H. P. H. Department of Urology, Gaziantep 34010, Turkey, K. Dogan, and F. o. M. Department of Urology, Istinye University, Istanbul 34010, Turkey, "The efficacy of systemic inflammatory response and oxidative stress in erectile dysfunction through multi-inflammatory index: a prospective cross-sectional analysis," The Journal of Sexual Medicine, vol. 20, no. 5, pp. 591-596, 2023. [CrossRef]
- S. Y. P. Ki Hak Moon, Yong Woon Kim, "Obesity and Erectile Dysfunction: From Bench to Clinical Implication," World J Mens Health, no. 37(2), pp. 138-147, 2019. [CrossRef]
- d. S. ILL et al., "Hypercaloric Diet Establishes Erectile Dysfunction in Rat: Mechanisms Underlying the Endothelial Damage," Frontiers in physiology, vol. 8, 10/04/2017 2017. [CrossRef]
- F. J, L. M, O. M, B. J, and L. P, "Importance of Different Grades of Abdominal Obesity on Testosterone Level, Erectile Dysfunction, and Clinical Coincidence," American journal of men's health, vol. 11, no. 2, 2017 Mar 2017. [CrossRef]
- J. R. Kovac, Labbate, C., Ramasamy, R., Tang, D. and Lipshultz, L.I. (2015). Effects of cigarette smoking on erectile dysfunction. [CrossRef]
- X. Y, G. H, N. C, R. J, and G.-C. NF, "Effect of long-term passive smoking on erectile function and penile nitric oxide synthase in the rat," The Journal of urology, vol. 157, no. 3, 1997 Mar 1997. [CrossRef]
- X. Guo, M. J. Oldham, M. T. Kleinman, R. F. Phalen, and G. S. Kassab, "Effect of cigarette smoking on nitric oxide, structural, and mechanical properties of mouse arteries," (in en), https://doi.org/10.1152/ajpheart.00376.2006, research-article 2006 Nov 01 2006. [CrossRef]
- G. H, L. CM, G. C, and A. J. K, "Physical Activity to Improve Erectile Function: A Systematic Review of Intervention Studies," Sexual medicine, vol. 6, no. 2, 2018 Jun 2018. [CrossRef]
- H. JL, M. MT, K. M, and A. MA, "Beneficial impact of exercise and obesity interventions on erectile function and its risk factors," The journal of sexual medicine, vol. 6 Suppl 3, 2009 Mar 2009. [CrossRef]
- A. A. de Oliveira, D. o. B. a. C. E. a. S. Laboratory of Vascular Physiology, Florida Institute of Technology, Melbourne, Florida, USA, K. P. Nunes, and D. o. B. a. C. E. a. S. Laboratory of Vascular Physiology, Florida Institute of Technology, Melbourne, Florida, USA, "Hypertension and Erectile Dysfunction: Breaking Down the Challenges," American Journal of Hypertension, vol. 34, no. 2, pp. 134-142, 2023. [CrossRef]
- V. M et al., "Update of the position paper on arterial hypertension and erectile dysfunction," Journal of hypertension, vol. 38, no. 7, 2020 Jul 2020. [CrossRef]
- H.-C. J, B.-G. V, Z. P, and C. A, "Understanding Erectile Dysfunction in Hypertensive Patients: The Need for Good Patient Management," Vascular health and risk management, vol. 28, no. 2, 2001 May 2001. [CrossRef]
- R. RC, "Psychogenic erectile dysfunction. Classification and management," The Urologic clinics of North America, vol. 28, no. 2, 20. [CrossRef]
- S. AD, "Psychologic factors in the multidisciplinary evaluation and treatment of erectile dysfunction," The Urologic clinics of North America, vol. 15, no. 1, 1988 Feb 1988.
- D. H. W. Lau, S. Kommu, F. H. Mumtaz, R. J. Morgan, C. S. Thompson, and D. P. Mikhailidis, "The Management of Phosphodiesterase-5 (PDE5) Inhibitor Failure," Current Vascular Pharmacology, vol. 4, no. 2, pp. 89-93, 2023. [CrossRef]
- A. MH, T. N, and C. S, "Platelet-Rich Plasma Injections for Erectile Dysfunction and Peyronie's Disease: A Systematic Review of Evidence," Sexual medicine reviews, vol. 10, no. 2, 2022 Apr 2022. [CrossRef]
- K. S, C. MC, C. SY, C. H, and R. MR, "Novel Emerging Therapies for Erectile Dysfunction," The world journal of men's health, vol. 39, no. 1, 2021 Jan 2021. [CrossRef]
- L. R, "Review of intraurethral suppositories and iontophoresis therapy for erectile dysfunction," International journal of impotence research, vol. 12 Suppl 4, 2000 Oct 2000. [CrossRef]
- F. M. Md. Ehsan Uddin Talukder, Rashu Barua, Samsad Sultana, Farhana Yesmin, Mohammad Sayedul Islam, Robiul Hasan Bhuiyan, "In vitro Assessment of Cytotoxic Activity of Hybrid Variety of Momordica charantia (Bitter Gourd)," 2023. [CrossRef]
- M. E. U. T. Rashu Barua, Mohammad Sayedul Islam, Farhana Yesmin, Kanchan Chakma, Md Golam Kabir, Robiul Hasan Bhuiyan, "Nutritional Analysis and Phytochemical Evaluation of Bitter Gourd (Momordica Charantia) from Bangladesh," 2020. [CrossRef]
- R. Barua et al., "Antioxidant and Cytotoxic Activity of Crude Flavonoid Fraction from the Fruits of Hybrid Variety of Momordica charantia (Bitter Gourd)," (in en), Journal of Pharmaceutical Research International, pp. 778-786, 2014/02/07 2014. [CrossRef]
- R. Barua et al., "Bioinformatics and Functional Analyses Implicate Potential Roles for EOGT and L-fringe in Pancreatic Cancers," (in en), Molecules, Communication vol. 26, no. 4, p. 882, 2021-02-07 2021. [CrossRef]
- P. V and R. M, "Erectile dysfunction and diabetes: a review of the current evidence-based medicine and a synthesis of the main available therapies," Diabetes & metabolism, vol. 38, no. 1, 2012 Feb 2012. [CrossRef]
- D. Y et al., "Erectile dysfunction, physical activity and physical exercise: Recommendations for clinical practice," Andrologia, vol. 51, no. 5, 2019 Jun 2019. [CrossRef]
- M. DR, B. AL, D. G, E. K, and I. LJ, "Erectile hydraulics: maximizing inflow while minimizing outflow," The journal of sexual medicine, vol. 11, no. 5, 2014 May 2014. 14 May. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




