1. Introduction
The incidence of chronic wounds is positively correlated with age and often associated with chronic diseases. In the United States, approximately 5.7 million people were affected by chronic wounds in 2017, resulting in an estimated annual cost of
$20 billion for their treatment. These chronic wounds significantly impact the quality of life for patients and their families. Patients often experience pain and psychological disorders due to the effects of chronic wounds, leading to social isolation. In some cases, hospitalization may be necessary for long-term treatment or to prevent mortality [
1].
Treating wounds, especially chronic wounds, poses a significant challenge. Despite the availability of various methods ranging from traditional to modern approaches [
2], there is a crucial need to explore and apply new treatment modalities to support existing methods. Low-level laser therapy (LLLT), alternatively referred to as photobiomodulation (PBM), is a medical modality that elicits advantageous clinical effects by stimulating cellular function. LLLT exhibits a distinctive biphasic dose-response relationship, wherein lower light doses frequently engender superior outcomes compared to higher doses. Effective implementation of LLLT necessitates meticulous consideration of numerous parameters, such as wavelength, fluence, irradiance, illumination duration, and timing, as they significantly impact the therapeutic effectiveness of this technique [
3]. Furthermore, it is important to note that LLLT should not be confused with photodynamic therapy, as they are distinct treatment modalities with different mechanisms of action. While LLLT involves stimulating cellular function using low-level laser energy, photodynamic therapy relies on the activation of exogenously administered photosensitizers by light to generate toxic reactive oxygen species (ROS) [
4]. LLLT has been found to stimulate the activity of stem cells, resulting in enhanced tissue healing. This cellular stimulation has been effective in treating a range of dermatological conditions, such as wrinkle reduction, acne scar improvement, hypertrophic scar reduction, burn healing, vitiligo treatment, psoriasis management, and acne control [
5].
Human skin fibroblasts are vital in various wound healing processes. Recent studies have focused on exploring the potential of LED and laser technologies to enhance fibroblast activity and collagen synthesis, aiming to develop a cost-effective and practical approach for wound repair that does not rely on expensive and stationary light systems currently used in therapy. Since fibroblasts play a critical role in wound healing, many published studies on LLLT have investigated its impact on fibroblast cell growth, migration, and collagen production [
6,
7,
8]. Experimental findings have shown that near-infrared (NIR) LED light treatment enhances mitochondrial oxidative metabolism in vitro and accelerates cell and tissue repair in vivo [
9,
10,
11,
12,
13].
LLLT holds promise for enhancing the management of chronic wounds in patients, thus emerging as a valuable treatment modality for healthcare systems in Vietnam and other countries. To provide further evidence of its efficacy, this study aimed to evaluate the effectiveness of LLLT at the cellular level (fibroblast cells) in vitro, specifically focusing on wound development and healing processes.
2. Materials and Methods
The study sample consisted of tissue samples obtained from 10 patients diagnosed with pressure ulcers and 10 patients diagnosed with diabetic foot ulcers who received inpatient treatment at the Vietnam National Institute of Burns. The inclusion criteria were patients aged 18 years and older with stage IV ulcers. Additionally, healthy fibroblast cells derived from the foreskin of children were used as a control group.
2.1. Biopsy for fibroblast cell collection
For optimal biopsy sample suitability, it is crucial to effectively cleanse the biopsy site. Patients are recommended to undergo a thorough full-body shower 24 hours prior to the biopsy procedure. The biopsy site must be carefully cleaned and prepared following the specific instructions provided in the medical guidelines [
14,
15]. The skin surrounding the biopsy site is carefully washed using Microshield medical soap (Schulke, India) and sterile water. Subsequently, the actual biopsy site is treated with Povidone solution (Pharmedic, Vietnam) and thoroughly rinsed with sterilized 0.9% saline solution. Finally, the area is gently dried by blotting, ensuring proper care is taken during the process [
16].
Biopsy procedures were conducted at three distinct locations within each wound: the wound base (Site 1), the wound margin (Site 2), and the surrounding healthy skin (Site 3). Each biopsy specimen, measuring 0.5 × 0.5 cm, encompassed the complete skin thickness, comprising the epidermis, dermis, and subcutaneous tissue [
17]. Immediately following collection, the tissue samples were immersed in Dulbecco’s modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and collagenase. To preserve their integrity, the samples were stored at a temperature of 4 °C until further isolation and subsequent culture of fibroblast cells could be performed [
9].
2.2. Tissue culture, isolation, and preservation of fibroblast cells
The established protocol developed by Freshney [
18] was employed for the isolation and cultivation of fibroblast cells. Initially, the skin samples underwent cleansing with Phosphate Buffered Saline (PBS) solution (Invitrogen, USA) and were subsequently sectioned into 2 mm-sized specimens [
9].
The tissue specimens were placed in a 25 cm
2 Corning cell culture flasks (Corning, USA) containing 5 ml of DMEM culture medium with 10% (FBS) and collagenase. The flask was then incubated under controlled conditions at 37 °C with 5% CO
2 [
19]. Following a 2-day incubation period, an additional 1 ml of culture medium was added to facilitate cell growth. During the culture transition phase, typically lasting 3-5 days, the medium volume was adjusted to reach a total volume of 5 ml. Regular medium changes were conducted every 3-4 days, and the cell population was diligently monitored until achieving at least 50% confluence on the flask surface [
16].
For preservation, fibroblast cells derived from the third passage culture were selected and stored using DMEM storage medium supplemented with 10% dimethyl sulfoxide (DMSO) under cryogenic storage conditions utilizing liquid CO
2 [
16].
2.3. Determining the number, viability, and quality of cells
2.3.1. Counting living cells in the Neubauer counting chamber
The cell quantification for appropriate seeding and assessment of cell proliferation was conducted utilizing a Neubauer counting chamber following the protocol outlined by Bich Phuong et al. [
16]. Cells were stained with a 0.4% trypan blue dye solution and enumerated under a microscope within a unit area of 1 mm
2. The cell density was determined using the formula:
where C denotes the cell density (cells/mL) and n signifies the number of cells counted in the Neubauer counting chamber.
2.3.2. Determining the viability of cultured fibroblast cells
The viability of fibroblast cells at various culture stages was evaluated according to the protocol outlined by Bich Phuong et al. [
16]. A 0.4% Trypan Blue staining solution (Gibco, USA) was utilized for assessing viability. This stain selectively permeates the membranes of impaired (nonviable) cells, resulting in their visualization as blue entities that can be differentiated under microscopic examination [
20].
To perform the cell viability assessment, 1 mL of the cell suspension was transferred to a centrifuge tube, and 50 μL of a 0.4% Trypan Blue stain was added. The mixture was incubated for 5 minutes. Subsequently, the solution was transferred to a hemocytometer and examined under an inverted microscope for the quantification of both the total cell count and the number of cells stained blue, indicating non-viable cells [
16].
The cell viability percentage (%) is calculated using the formula:
2.4. Evaluation of Fibroblasts Proliferation at Wound Sites and the Effect of LLLT on Fibroblasts Proliferation
The proliferation of fibroblasts, specifically wound base fibroblasts, was evaluated using a modified model based on the research conducted by Pansani et al. in 2014 [
21]. The cells from the third generation (G3) were cultured in a 6-well plate (Corning, USA) at a density of 5 × 10
4 cells per well in 2 mL of DMEM supplemented with 10% FBS and 1% AB 1X (Gibco, USA). The cell culture was maintained at 37 °C with 5% CO
2. The number of viable cells, cultured for 24 hours, was determined using the previously described method [
16].
To assess the impact of low-level laser therapy (LLLT) on fibroblast cell proliferation, the cells were seeded into a 6-well plate and divided into two groups: a control group without laser irradiation and an LLLT group. The LLLT group was further divided into subgroups with varying energy levels (2.5, 3, 3.5, 4, and 5 J/cm2) of 808 nm laser and corresponding irradiation times (60, 48, 42, 36, and 30 seconds). Laser irradiation was administered daily for three consecutive days.
The B-Cure Laser Pro device (Good Energies®, Israel) was utilized for LLLT in the study. The laser employed in the research belonged to the GaAlAs category, which refers to Gallium Aluminum Arsenide and represents a solid-state laser diode. The maximum power output of the laser was 250 mW, ensuring the intensity of the laser irradiation. The wavelength of the laser fell within the infrared range and measured 808 nm, enabling effective penetration into the target tissues. The pulse frequency was set at 13 kHz, indicating the rate at which laser pulses were emitted per second. Furthermore, the laser pulse duration was 26 μs, signifying the duration of each individual laser pulse. To maintain a consistent distance between the laser probe and the sample surface, a distance of 1 cm was maintained throughout the experiments. These specific laser parameters were deliberately selected and implemented to deliver the desired effects of LLLT in the study.
Following the final irradiation, the number of viable cells in both the control group and the LLLT group was determined using the trypan blue staining method described earlier. The cell count was performed at the wound sites and compared with the control group, which did not undergo laser irradiation.
2.5. Statistical analysis
The statistical analysis of the research findings was performed using SPSS 22 statistical software. The cell count was presented as the mean value (±) standard deviation. The non-parametric Mann-Whitney test was employed for data analysis, with a significance level set at p < 0.05 to determine statistical significance.
3. Results
3.1. Culturing of primary fibroblast cells
The results of culturing primary fibroblast cells from various sites, including the wound base (Site 1), the wound margin (Site 2), and the surrounding healthy skin (Site 3) are presented. There was no evidence of bacterial or fungal contamination in any of the three sites, indicating that the cell culture procedure was conducted under aseptic conditions, ensuring the absence of microbial growth. The number of viable fibroblast cell samples remained consistent across all sites, with 20 cell samples observed in each site. This consistency suggests that the primary fibroblast cells were successfully cultured and maintained their viability throughout the entire culturing process. Furthermore, no non-proliferating cell samples were detected in any of the sites, indicating the potential of the fibroblast cell samples to undergo proliferation and division. This characteristic is essential for their vital role in wound healing and tissue regeneration. In summary, the presented data table demonstrates the successful culturing of primary fibroblast cell samples from different sites, with no contamination and a substantial number of viable cells. These findings serve as a solid foundation for further investigations into the behavior and functions of fibroblast cells in the context of wound healing at various sites.
3.2. Culturing and Isolation of Fibroblast Cells across Generations
3.2.1. Growth time and comparison of fibroblast cell generations at different sites for pressure ulcers, diabetic ulcers, and control groups
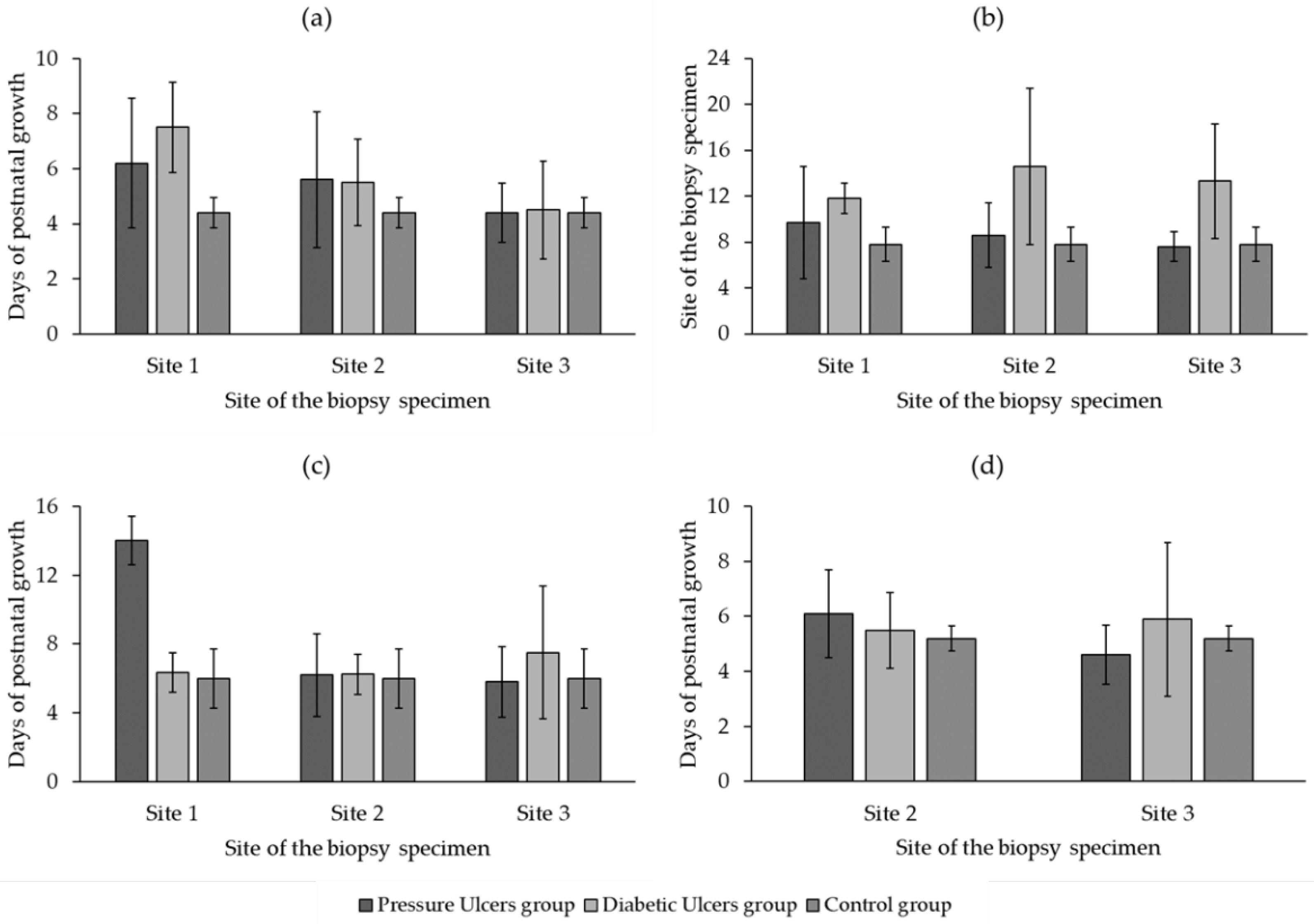
Figure 1a depicts the data pertaining to the initiation phase of fibroblast cell culture. This experiment encompassed three groups: the pressure ulcers group, the diabetic ulcers group, and the control group. The objective was to evaluate fibroblast cell growth at different sites (Site 1, Site 2, and Site 3) over a specific duration, using days as the unit of measurement. In the pressure ulcers group, the mean growth values at Site 1, Site 2, and Site 3 were 6.2 ± 2.35, 5.6 ± 2.46, and 4.4 ± 1.08. The p-values indicated no statistically significant differences between Site 1 and Site 2 (p > 0.05), and between Site 2 and Site 3 (p > 0.05). However, there was a statistically significant difference between Site 1 and Site 3 (p = 0.038). For the diabetic ulcers group, the mean growth values at Site 1, Site 2, and Site 3 were 7.5 ± 1.65, 5.5 ± 1.58, and 4.5 ± 1.78. The p-values indicated a statistically significant difference between Site 1 and Site 2 (p = 0.013), between Site 1 and Site 3 (p = 0.001), but no significant difference between Site 2 and Site 3 (p > 0.05). The p-values comparing the pressure ulcers group to the control group were all greater than 0.05, indicating no significant differences. However, in the comparison between the diabetic ulcers group and the control group, there was a statistically significant difference between Site 1 and the control group (p = 0.007), but no significant differences between Site 2 or Site 3 and the control group (p > 0.05). Overall,
Figure 1a provides an overview of the fibroblast cell culture’s initiation phase at distinct sites. The results underscore variations in cell growth between the pressure ulcers group, the diabetic ulcers group, and the control group. These findings offer valuable insights into the behavior and characteristics of fibroblast cells during the initial phase of cell culture, particularly within the context of wound healing and related conditions.
Figure 1b illustrates the average growth time of the 1
st generation fibroblasts (G1) at different sites for the pressure ulcers group, diabetic ulcers group, and control group. In the pressure ulcers group, the growth time of the 2nd generation fibroblasts was 9.7 ± 4.9 days at Site 1, 8.6 ± 2.79 days at Site 2, and 7.6 ± 1.27 days at Site 3. However, the p-values for the comparisons between different sites within this group were greater than 0.05. Similarly, the p-values comparing the growth time between the diabetic ulcers group and the control group were less than 0.05 for Site 1 and Site 2, indicating significant differences in growth time between these groups. For Site 3, the p-value was also less than 0.05, indicating a significant difference in growth time between the diabetic ulcers group and the control group.
Figure 1c presents the average growth time of the 2
nd generation fibroblasts (G2) at different sites for each group. Within the pressure ulcers group, the growth time of the 3rd generation fibroblasts was 14 ± 1.41 days at Site 1, 6.2 ± 2.39 days at Site 2, and 5.8 ± 2.04 days at Site 3. The p-values for the comparisons between different sites within this group were 0.028 and 0.031, indicating significant differences in growth time. However, the p-value was greater than 0.05, indicating no significant difference in growth time between Site 2 and Site 3. Similarly, in the diabetic ulcers group, the growth time of the 3rd generation fibroblasts was 6.33 ± 1.15 days at Site 1, 6.25 ± 1.16 days at Site 2, and 7.5 ± 3.86 days at Site 3. The p-values for the comparisons between different sites within this group were all greater than 0.05, indicating no significant differences in growth time. The p-value comparing the growth time between the pressure ulcers group and the control group was 0.044 for Site 1, indicating a significant difference in growth time between these groups. However, for Site 2 and Site 3, the p-values were greater than 0.05, indicating no significant differences in growth time between the pressure ulcers group and the control group. The p-values comparing the growth time between the diabetic ulcers group and the control group were all greater than 0.05, indicating no significant differences in growth time between these groups. Overall, the data presented in
Figure 1c provide insights into the growth time of the 3rd generation fibroblasts at different sites, facilitating comparisons and analysis of growth time differences between the groups.
Figure 1d showcases the growth time of the 3
rd generation fibroblasts (G3) at different sites for each group. Within the pressure ulcers group, no growth was observed at Site 1. The growth time of the 4th generation fibroblasts was 6.1 ± 1.59 days at Site 2 and 4.6 ± 1.07 days at Site 3. The p-value for the comparison between Site 2 and Site 3 was significant (p = 0.038), indicating a notable difference in growth time between these two sites. In the diabetic ulcers group, no growth was observed at Site 1. The growth time of the 4th generation fibroblasts was 5.5 ± 1.38 days at Site 2 and 5.89 ± 2.8 days at Site 3. The p-value for the comparison between Site 2 and Site 3 was not significant (p > 0.05), indicating no substantial difference in growth time between these two sites.
3.2.2. Fibroblast samples cultured over generations for different patient groups and sites
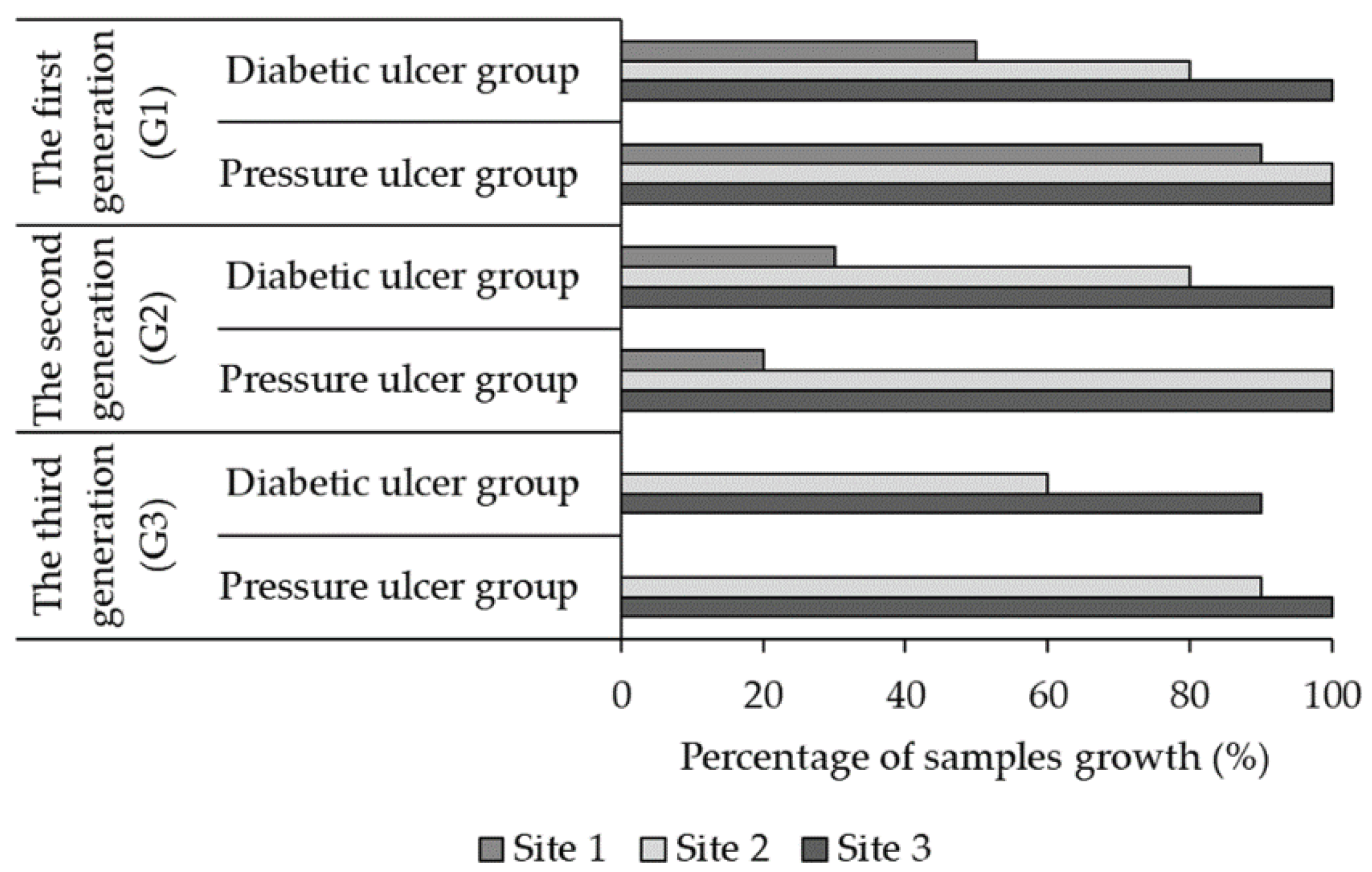
The data presented in
Figure 2 illustrates the percentage of fibroblast samples cultured over generations for different patient groups and sites. The table provides information on the percentage of fibroblast samples cultured at each site over three generations: the first generation (G1), the second generation (G2), and the third generation (G3). In the pressure ulcer group, during the first generation (G1), 90% of the fibroblast samples were cultured at Site 1, while 100% were cultured at both Site 2 and Site 3. For the diabetic ulcer group in the first generation (G1), 50% of the fibroblast samples were cultured at Site 1, 80% at Site 2, and 100% at Site 3. Moving to the second generation (G2), the percentage of fibroblast samples cultured decreased for both patient groups. In the pressure ulcer group, only 20% of the samples were cultured at Site 1, while 100% were cultured at both Site 2 and Site 3. Similarly, in the diabetic ulcer group, 30% of the samples were cultured at Site 1, 80% at Site 2, and 100% at Site 3. In the third generation (G3), no growth was observed for the pressure ulcer group at Site 1. However, 90% of the fibroblast samples were cultured at Site 2, and 100% were cultured at Site 3. For the diabetic ulcer group in the third generation (G3), again, no growth was observed at Site 1, but 60% of the samples were cultured at Site 2, and 90% were cultured at Site 3.
Analyzing the data, it can be observed that the percentage of fibroblast samples cultured generally decreased from the first generation (G1) to the second generation (G2). This trend suggests that there may be a decrease in the proliferation or availability of fibroblast cells for culture in subsequent generations. Additionally, the absence of growth in certain sites in the third generation (G3) for both patient groups indicates potential limitations in the ability of fibroblasts to proliferate at those specific sites. These findings highlight the importance of considering the generation and site-specific differences in fibroblast cell culture when studying wound healing and related conditions. Further investigations into the factors influencing the growth and viability of fibroblast cells over generations are warranted to better understand their behavior and potential implications for tissue regeneration.
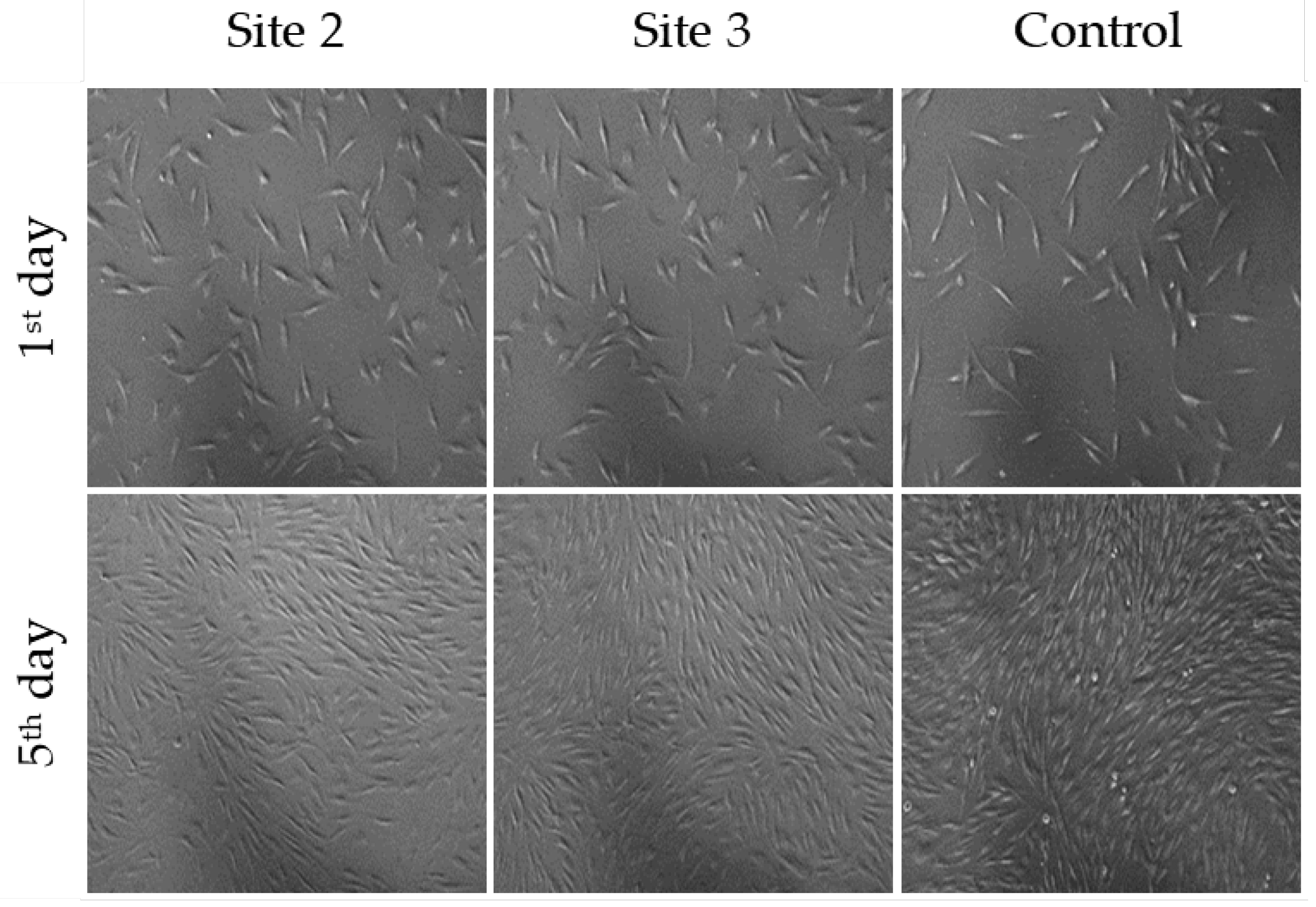
3.2.3. Morphology and growth characteristics of fibroblast cells in the third generation of cell culture
Figure 3 demonstrates the morphology and growth characteristics of fibroblast cells in the third generation of cell culture. The fibroblast cells exhibited a diamond-shaped morphology and adhered to the surface of the culture dish, forming a monolayer. The images presented in
Figure 3 provide visual evidence of the fibroblast cell proliferation and adherence patterns at different time points. It is worth noting that these fibroblast cells were derived from the third generation of fibroblasts cultured from samples taken from Pressure Ulcer Wounds.
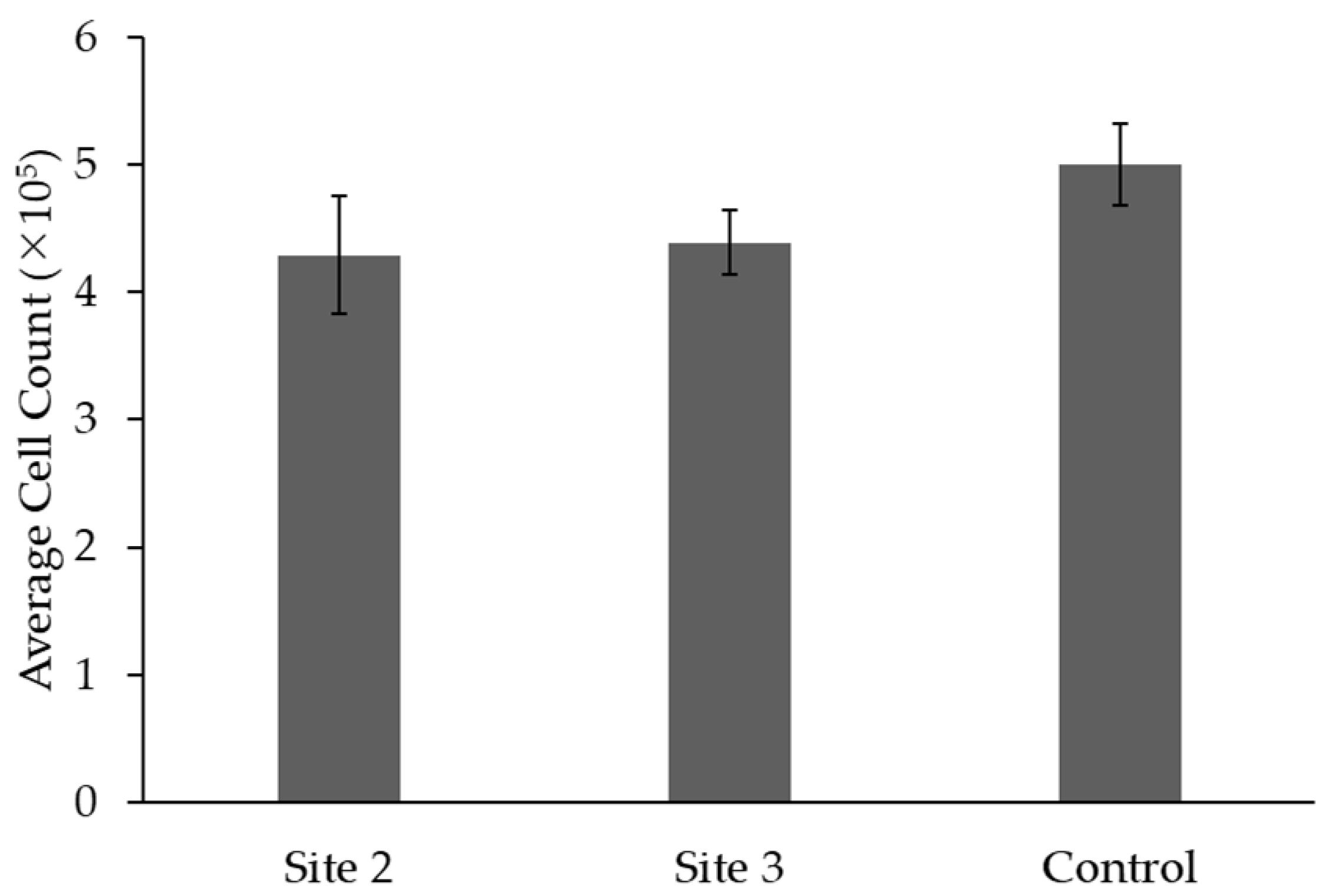
Figure 4 shows the average cell count (×10
5) of cell proliferation in samples from Site 2, Site 3, and the Control group derived from pressure ulcer wounds after 5 days of cultivation in the 3rd generation. The p-value indicates statistical significance when compared to the Control group. The
Figure 4 displays the mean cell count for each site along with the corresponding standard deviation. The average cell count for Site 2 is (4.29 ± 0.46) × 10
5. Similarly, Site 3 has an average cell count of (4.39 ± 0.25) × 10
5, showing slightly higher cell count compared to Site 2. In comparison, the Control group has an average cell count of (5.0 ± 0.32) × 10
5, indicating a slightly higher cell count compared to both Site 2 and Site 3.
The statistical significance is indicated by the p-value being less than 0.05 when compared to the Control group. This suggests that there is a statistically significant difference in cell count between the experimental sites (Site 2 and Site 3) and the Control group.
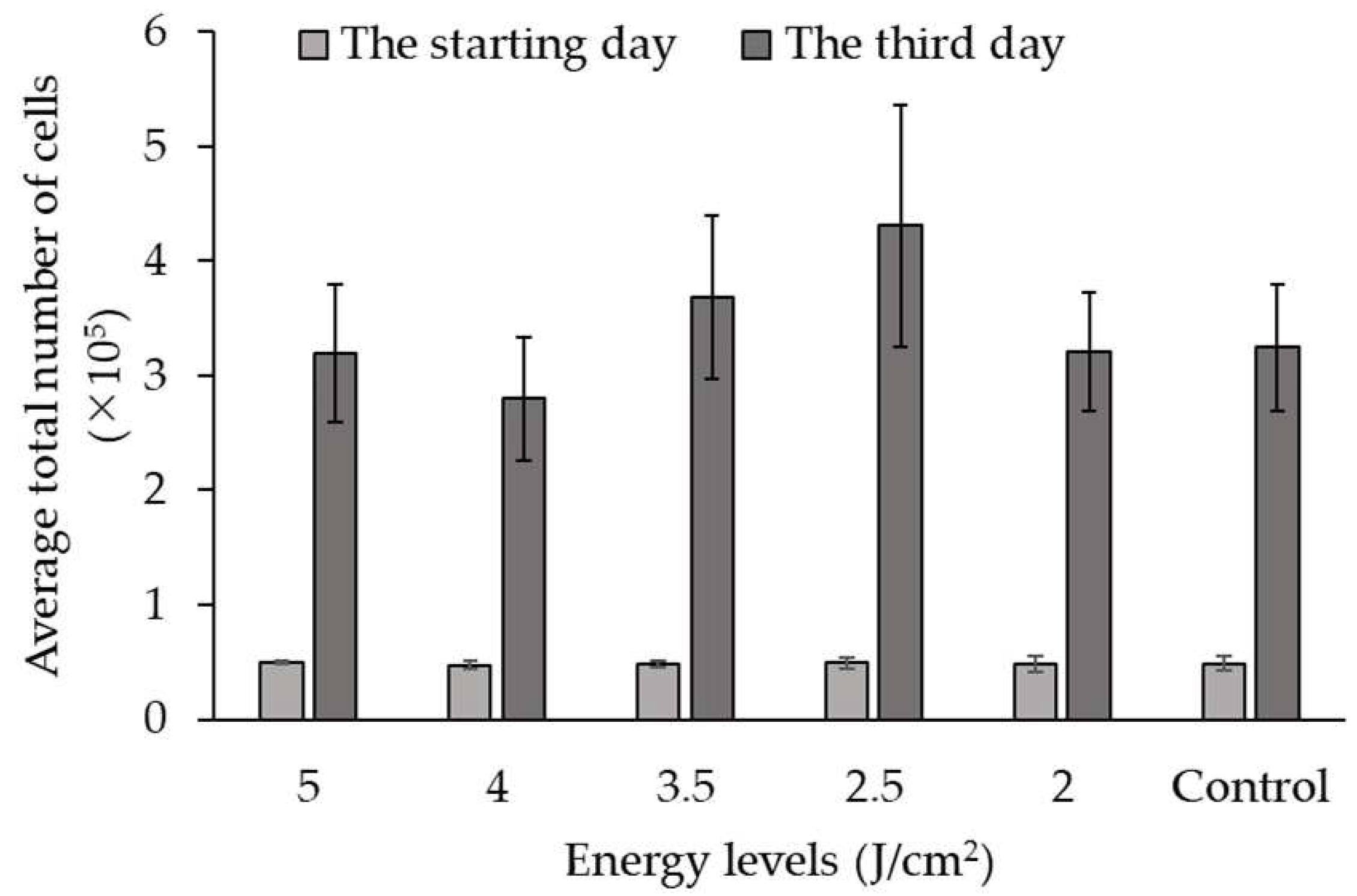
3.3. The Impact of LLLT on Fibroblast Cell Growth
Figure 5 presents the data on the impact of Low-Level Laser Therapy (LLLT) on the growth of fibroblast cells at different energy levels. The experiment involved culturing fibroblast cells and subjecting them to varying levels of energy during LLLT. The growth of fibroblast cells was measured and compared between the different energy levels and a control group (in units of total cells ×10
5).
On the starting day, the average cell counts were relatively similar across all energy levels and the control group, ranging from 0.47 ± 0.04 to 0.50 ± 0.01 × 105 total cells. However, on the third day of culture, significant differences in cell growth were observed among the energy levels. The average cell counts varied across the different energy levels, with values ranging from 2.80 ± 0.54 to 4.31 ± 1.06 × 105 total cells. Statistical analysis using p-values was conducted to compare each energy level with the control group. The p-values indicate the significance of the differences observed.
The analysis revealed that at energy levels of 3, 3.5, and 4 J/cm2, there was a significant increase in cell growth compared to the control group (p < 0.05). At the energy level of 2.5 and 5 J/cm2, although there was an increase in cell growth compared to the control group, the difference was not statistically significant (p < 0.05).
Overall, the data presented in
Figure 3 demonstrate the impact of LLLT on fibroblast cell growth at different energy levels. The results indicate that specific energy levels, such as 4, 3.5, and 3 J/cm
2, can significantly enhance cell growth, while other energy levels may not have a significant effect. It can be concluded that the use of the 3 J/cm
2 energy level in Low-Level Laser Therapy (LLLT) has the most beneficial effect on fibroblast cell growth. This is evident from the significantly higher average cell count observed on the third day of culture compared to the control group. The 3 J/cm
2 energy level during LLLT can positively influence fibroblast cell growth. This provides valuable guidance for selecting an optimal energy level in LLLT to promote fibroblast cell growth, which has implications in tissue engineering and regenerative medicine applications.
4. Discussion
Based on current research, investigations into therapeutic approaches for chronic wounds primarily focus on healthy fibroblast cells due to evidence suggesting reduced proliferation and premature aging in fibroblast cells derived from chronic wounds [
22]. Successful isolation of fibroblast cells from chronic wounds serves as a fundamental basis for experimental studies exploring potential cell-based therapies for managing chronic wounds. Previous research publications have documented the successful isolation of fibroblast cells from venous ulcers, diabetic ulcers, and pressure ulcers [
17,
23,
24]. There are two commonly utilized techniques for tissue sample separation in isolation procedures: purely mechanical techniques and enzyme-based techniques. Purely mechanical techniques are limited in their suitability to certain tissue types and often yield a low quantity of cells. On the other hand, enzyme-based techniques are easier to implement and can result in a higher cell yield, albeit at a higher cost [
18]. In this particular study, 60 biopsy samples were collected from pressure ulcers and diabetic ulcers in 20 patients. Prior to sampling, all tissues were prepared following an established protocol to ensure they were free from infection. The trypan blue method is a straightforward approach used to evaluate cytotoxicity. Nevertheless, this method is not without its limitations. These limitations include potential errors in calculating results for individual samples, challenges in distinguishing between dead cells and stained debris, inconsistencies among operators, and the time and labor-intensive nature of processing multiple samples [
25].
In this study, a total of 60 fibroblast cell samples were examined. Among these samples, only at Site 1 (wound base), the third-generation cell regeneration was not sustained. Fibroblast cells obtained from the surrounding healthy skin (Site 3) and wound margin (Site 2) exhibited no noticeable morphological changes, appearing spindle-shaped and forming a single layer when adhered to the culture dish. Cells from Sites 2 and 3 demonstrated robust proliferative capacity, allowing their isolation up to the third, fourth, and fifth generations. Notably, Brem et al. observed that fibroblast cells isolated from four tissue samples of patients with venous ulcers retained their characteristic phenotype. Fibroblast cells from the surrounding healthy skin displayed the most favorable response, while those from the wound base exhibited an average response, and the cells from the wound margin showed comparatively less development [
17].
Cellular aging is characterized by a decline in growth capacity and morphological alterations. Comparing the proliferation process between Site 2 (wound margin) and Site 3 (surrounding healthy skin) with healthy fibroblast cells revealed no significant differences. However, fibroblast cells derived from chronic wounds exhibited a noticeable deceleration in proliferation compared to healthy fibroblast cells (p < 0.05). The cell count in samples from Sites 2 and 3 was significantly lower than that of the control group (p < 0.05), indicating a slower proliferation rate of fibroblast cells from chronic wounds compared to healthy fibroblast cells. These findings are consistent with seminal studies conducted by Miriam Loots et al., which demonstrated a reduced proliferative capacity of fibroblast cells isolated from type II diabetic ulcers [
23]. Wall et al. also observed decreased proliferation, impaired wound closure ability, and premature aging in fibroblast cells from chronic wounds compared to normal fibroblast cells. Additionally, they highlighted the accumulation of senescent fibroblast cells, accounting for over 15%, in both chronic wounds and non-wounded skin [
24]. Vande Berg and Robson found that fibroblast cells in decubitus ulcers and venous ulcers exhibited reduced proliferation and displayed signs of cellular senescence. Fibroblast cells from decubitus ulcers demonstrated a slower rate of replication compared to normal fibroblast cells as well [
26].
Studying fibroblast cells derived from chronic wounds provides a foundation for investigating experimental interventions, such as Low-Level Laser Therapy (LLLT), for wound treatment. Numerous studies have demonstrated the effectiveness of LLLT in promoting wound healing, with outcomes dependent on the dosage and wavelength employed [
27,
28,
29]. In this study, we applied laser irradiation (808 nm) at various energy levels to fibroblast cells, aiming to determine the optimal dosage that stimulates the potential biological effects of LLLT on fibroblast proliferation. The results revealed a significant increase in cell count following LLLT treatment with dosages of 2.5, 3, and 3.5 J/cm
2, with the 3 J/cm
2 dosage yielding the most favorable outcome (p < 0.05). These findings align with previous research by Basso and colleagues [
30,
31,
32], which explored the impact of LLLT on the proliferation and migration of gingival fibroblast cells in humans and identified the optimal energy dosage as 3 J/cm². A comprehensive review of cell culture studies conducted by AlGhamdi et al. [
33] further supported these findings, demonstrating that LLLT at energy levels ranging from 0.5 to 4.0 J/cm2 enhanced the proliferation rate of various cell lines. Kreisler et al. [
34] also observed an increase in fibroblast cell proliferation in vitro following direct and continuous Low-Level Laser Therapy (LLLT) irradiation. Similarly, Ma et al. [
35] demonstrated that irradiation of healthy fibroblast cells with an 830 nm laser wavelength promoted both cell proliferation and collagen synthesis. These findings are consistent with previous investigations highlighting the beneficial effects of LLLT on cells through the upregulation of growth factor expression [
31,
36].
5. Conclusions
In chronic wounds and diabetic ulcer ulcers, fibroblasts can be isolated at the edge of the wound and healthy skin without changing its morphology during cultivation. However, the proliferation and migration rate of fibroblasts in chronic wounds wounds is lower than in healthy individuals. Low-power laser (808 nm) with an energy level of 3 J/cm2 does not change cell morphology and stimulates proliferation and migration of fibroblasts samples derived from chronic wounds patients.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org, Figure S1: Fibroblast Cell Cultures under LLLT Influence.
Author Contributions
Conceptualization, M.H.P., B.P.N.T.; Data curation, P.B.N.T., V.H.D., T.H.N.; Formal analysis, M.H.P., B.P.N.T.; Investigation, P.B.N.T., V.H.D.; Methodology, P.B.N.T., V.H.D.; Writing—original draft, M.H.P., B.P.N.T.; Writing—review & editing, M.H.P., B.P.N.T., V.H.D., T.H.N.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of VIETNAM NATIONAL INSTITUTE OF BURNS and HO CHI MINH CITY HOSPITAL OF REHABILITATION AND OCCUPATIONAL DISEASE (Code: 1237/QD-HCQY).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We acknowledge the cooperation and support of outpatients, and collaborators at the Vietnam National Institute of Burns for the time and effort they devoted to the study. We also thank you for the support from Ho Chi Minh city Hospital of Rehabilitation and Occupational Disease.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alam, W.; Hasson, J.; Reed, M. Clinical approach to chronic wound management in older adults. Journal of the American Geriatrics Society 2021, 69, 2327–2334. [Google Scholar] [CrossRef] [PubMed]
- Addis, R.; Cruciani, S.; Santaniello, S.; Bellu, E.; Sarais, G.; Ventura, C.; Maioli, M.; Pintore, G. Fibroblast Proliferation and Migration in Wound Healing by Phytochemicals: Evidence for a Novel Synergic Outcome. International Journal of Medical Sciences 2020, 17, 1030–1042. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.-Y.; Carroll, J.D.; Hamblin, M.R. The Nuts and Bolts of Low-level Laser (Light) Therapy. Annals of Biomedical Engineering 2012, 40, 516–533. [Google Scholar] [CrossRef] [PubMed]
- Freitas, L.F.d.; Hamblin, M.R. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE Journal of Selected Topics in Quantum Electronics 2016, 22, 348–364. [Google Scholar] [CrossRef] [PubMed]
- Santos, C.M.d.; Rocha, R.B.d.; Hazime, F.A.; Cardoso, V.S. A Systematic Review and Meta-Analysis of the Effects of Low-Level Laser Therapy in the Treatment of Diabetic Foot Ulcers. The International Journal of Lower Extremity Wounds 2020, 20, 198–207. [Google Scholar] [CrossRef]
- Oliveira, D.A.A.P.; De Oliveira, R.F.; Magini, M.; Zangaro, R.A.; Soares, C.P. Assessment of Cytoskeleton and Endoplasmic Reticulum of Fibroblast Cells Subjected to Low-Level Laser Therapy and Low-Intensity Pulsed Ultrasound. Photomedicine and Laser Surgery 2009, 27, 461–466. [Google Scholar] [CrossRef]
- Hsieh, Y.-L.; Cheng, Y.-J.; Huang, F.-C.; Yang, C.-C. The Fluence Effects of Low-Level Laser Therapy on Inflammation, Fibroblast-Like Synoviocytes, and Synovial Apoptosis in Rats with Adjuvant-Induced Arthritis. Photomedicine and Laser Surgery 2014, 32, 669–677. [Google Scholar] [CrossRef]
- Amorim, F.C.M.; Arisawa, E.Â.L.; Sant’anna, L.B.; Rodrigues, A.B.M.; Costa, D.R.J.R.L.-A.d.E. Preclinical study of experimental burns treated with photobiomodulation and Human Amniotic Membrane, both isolated and associated. Rev Lat Am Enfermagem 2023, 31, e3726. [Google Scholar] [CrossRef]
- Yang, T.-S.; Nguyen, L.-T.-H.; Hsiao, Y.-C.; Pan, L.-C.; Chang, C.-J. Biophotonic Effects of Low-Level Laser Therapy at Different Wavelengths for Potential Wound Healing. Photonics 2022, 9, 591. [Google Scholar] [CrossRef]
- Erdle, B.J.; Brouxhon, S.; Kaplan, M.; Vanbuskirk, J.; Pentland, A.P. Effects of Continuous-Wave (670-nm) Red Light on Wound Healing. Dermatologic Surgery 2008, 34, 320–325. [Google Scholar] [CrossRef]
- Corazza, A.V.; Jorge, J.; Kurachi, C.; Bagnato, V.S. Photobiomodulation on the Angiogenesis of Skin Wounds in Rats Using Different Light Sources. Photomedicine and Laser Surgery 2007, 25, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Dall Agnol, M.A.; Nicolau, R.A.; de Lima, C.J.; Munin, E. Comparative analysis of coherent light action (laser) versus non-coherent light (light-emitting diode) for tissue repair in diabetic rats. Lasers in Medical Science 2009, 24, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Trelles, M.A.; Allones, I. Red light-emitting diode (LED) therapy accelerates wound healing post-blepharoplasty and periocular laser ablative resurfacing. Journal of Cosmetic and Laser Therapy 2006, 8, 39–42. [Google Scholar] [CrossRef]
- Greenwood, J.D.; Merry, S.P.; Boswell, C.L. Skin Biopsy Techniques. Primary Care: Clinics in Office Practice 2022, 49, 1–22. [Google Scholar] [CrossRef]
- Manchanda, M.; Torres, M.; Inuossa, F.; Bansal, R.; Kumar, R.; Hunt, M.; Wheelock, C.E.; Bachar-Wikstrom, E.; Wikstrom, J.D. Metabolic Reprogramming and Reliance in Human Skin Wound Healing. Journal of Investigative Dermatology 2023. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.B.P.; Dinh, V.H.; Nguyen, N.T.; Nguyen, N.L.; Nguyen, T.H. In Vitro Assessment of The Effect of Low Level Laser Therapy on the Proliferation and Migration of Fibroblasts Derived from Patients with Chronic Wounds. Vietnam Medical Journal 2023, 525, 230–235. [Google Scholar] [CrossRef]
- Brem, H.; Golinko, M.S.; Stojadinovic, O.; Kodra, A.; Diegelmann, R.F.; Vukelic, S.; Entero, H.; Coppock, D.L.; Tomic-Canic, M. Primary cultured fibroblasts derived from patients with chronic wounds: A methodology to produce human cell lines and test putative growth factor therapy such as GMCSF. Journal of Translational Medicine 2008, 6, 75. [Google Scholar] [CrossRef]
- Freshney, R.I. Culture of animal cells: A manual of basic technique and specialized applications; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Roberts, W.G.; Berns, M.W. In vitro photosensitization I. Cellular uptake and subcellular localization of mono-L-aspartyl chlorin e6, chloro-aluminum sulfonated phthalocyanine, and photofrin II. Lasers in Surgery and Medicine 1989, 9, 90–101. [Google Scholar] [CrossRef]
- Kaltenbach, J.P.; Kaltenbach, M.H.; Lyons, W.B. Nigrosin as a dye for differentiating live and dead ascites cells. Experimental Cell Research 1958, 15, 112–117. [Google Scholar] [CrossRef]
- Pansani, T.N.; Basso, F.G.; Turirioni, A.P.S.; Kurachi, C.; Hebling, J.; de Souza Costa, C.A. Effects of low-level laser therapy on the proliferation and apoptosis of gingival fibroblasts treated with zoledronic acid. International Journal of Oral and Maxillofacial Surgery 2014, 43, 1030–1034. [Google Scholar] [CrossRef]
- desJardins-Park, H.E.; Foster, D.S.; Longaker, M.T. Fibroblasts and wound healing: An update. Regenerative Medicine 2018, 13, 491–495. [Google Scholar] [CrossRef]
- Loots, M.A.M.; Lamme, E.N.; Mekkes, J.R.; Bos, J.D.; Middelkoop, E. Cultured fibroblasts from chronic diabetic wounds on the lower extremity (non-insulin-dependent diabetes mellitus) show disturbed proliferation. Archives of Dermatological Research 1999, 291, 93–99. [Google Scholar] [CrossRef]
- Wall, I.B.; Moseley, R.; Baird, D.M.; Kipling, D.; Giles, P.; Laffafian, I.; Price, P.E.; Thomas, D.W.; Stephens, P. Fibroblast Dysfunction Is a Key Factor in the Non-Healing of Chronic Venous Leg Ulcers. Journal of Investigative Dermatology 2008, 128, 2526–2540. [Google Scholar] [CrossRef]
- Gupta, R.; Rajpoot, K.; Tekade, M.; Sharma, M.C.; Tekade, R.K. Chapter 7—Methods and models for in vitro toxicity. In Pharmacokinetics and Toxicokinetic Considerations; Tekade, R.K., Ed.; Academic Press: Cambridge, MA, USA, 2022; Volume 2, pp. 145–174. [Google Scholar]
- Vande Berg, J.S.; Rose, M.A.; Haywood-Reid, P.L.; Rudolph, R.; Payne, W.G.; Robson, M.C. Cultured pressure ulcer fibroblasts show replicative senescence with elevated production of plasmin, plasminogen activator inhibitor-1, and transforming growth factor-β1. Wound Repair and Regeneration 2005, 13, 76–83. [Google Scholar] [CrossRef]
- Gupta, A.; Keshri, G.K.; Yadav, A.; Gola, S.; Chauhan, S.; Salhan, A.K.; Bala Singh, S. Superpulsed (Ga-As, 904 nm) low-level laser therapy (LLLT) attenuates inflammatory response and enhances healing of burn wounds. Journal of Biophotonics 2015, 8, 489–501. [Google Scholar] [CrossRef]
- Wanitphakdeedecha, R.; Iamphonrat, T.; Phothong, W.; Eimpunth, S.; Manuskiatti, W. Local and systemic effects of low-level light therapy with light-emitting diodes to improve erythema after fractional ablative skin resurfacing: A controlled study. Lasers in Medical Science 2019, 34, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Nilforoushzadeh, M.A.; Kazemi khoo, N.; Zareh, S.; Mokmeli, S.; Dahmardehei, M.; Vaghardoost, R.; Momeni, M.; Ansari, F. An Open-Label Study of Low-Level Laser Therapy Followed by Autologous Fibroblast Transplantation for Healing Grade 3 Burn Wounds in Diabetic Patients. Journal of Lasers in Medical Sciences 2019, 10, S7–S12. [Google Scholar] [CrossRef]
- Basso, F.G.; Soares, D.G.; de Souza Costa, C.A.; Hebling, J. Low-level laser therapy in 3D cell culture model using gingival fibroblasts. Lasers in Medical Science 2016, 31, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Peplow, P.V.; Chung, T.-Y.; Baxter, G.D. Laser Photobiomodulation of Proliferation of Cells in Culture: A Review of Human and Animal Studies. Photomedicine and Laser Surgery 2010, 28, S-3–S-40. [Google Scholar] [CrossRef] [PubMed]
- Basso, F.G.; Pansani, T.N.; Turrioni, A.P.S.; Bagnato, V.S.; Hebling, J.; de Souza Costa, C.A. In Vitro Wound Healing Improvement by Low-Level Laser Therapy Application in Cultured Gingival Fibroblasts. International Journal of Dentistry 2012, 2012, 719452. [Google Scholar] [CrossRef]
- AlGhamdi, K.M.; Kumar, A.; Moussa, N.A. Low-level laser therapy: A useful technique for enhancing the proliferation of various cultured cells. Lasers in Medical Science 2012, 27, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Kreisler, M.; Christoffers, A.B.; Al-Haj, H.; Willershausen, B.; d’Hoedt, B. Low level 809-nm diode laser-induced in vitro stimulation of the proliferation of human gingival fibroblasts. Lasers in Surgery and Medicine 2002, 30, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Yang, J.-P.; Tan, R.K.; Lee, H.-W.; Han, S.-K. Effect of Low-Level Laser Therapy on Proliferation and Collagen Synthesis of Human Fibroblasts in Vitro. J Wound Manag Res 2018, 14, 1–6. [Google Scholar] [CrossRef]
- Woodruff, L.D.; Bounkeo, J.M.; Brannon, W.M.; Dawes, K.S.; Barham, C.D.; Waddell, D.L.; Enwemeka, C.S. The Efficacy of Laser Therapy in Wound Repair: A Meta-Analysis of the Literature. Photomedicine and Laser Surgery 2004, 22, 241–247. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).