Submitted:
18 August 2023
Posted:
22 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
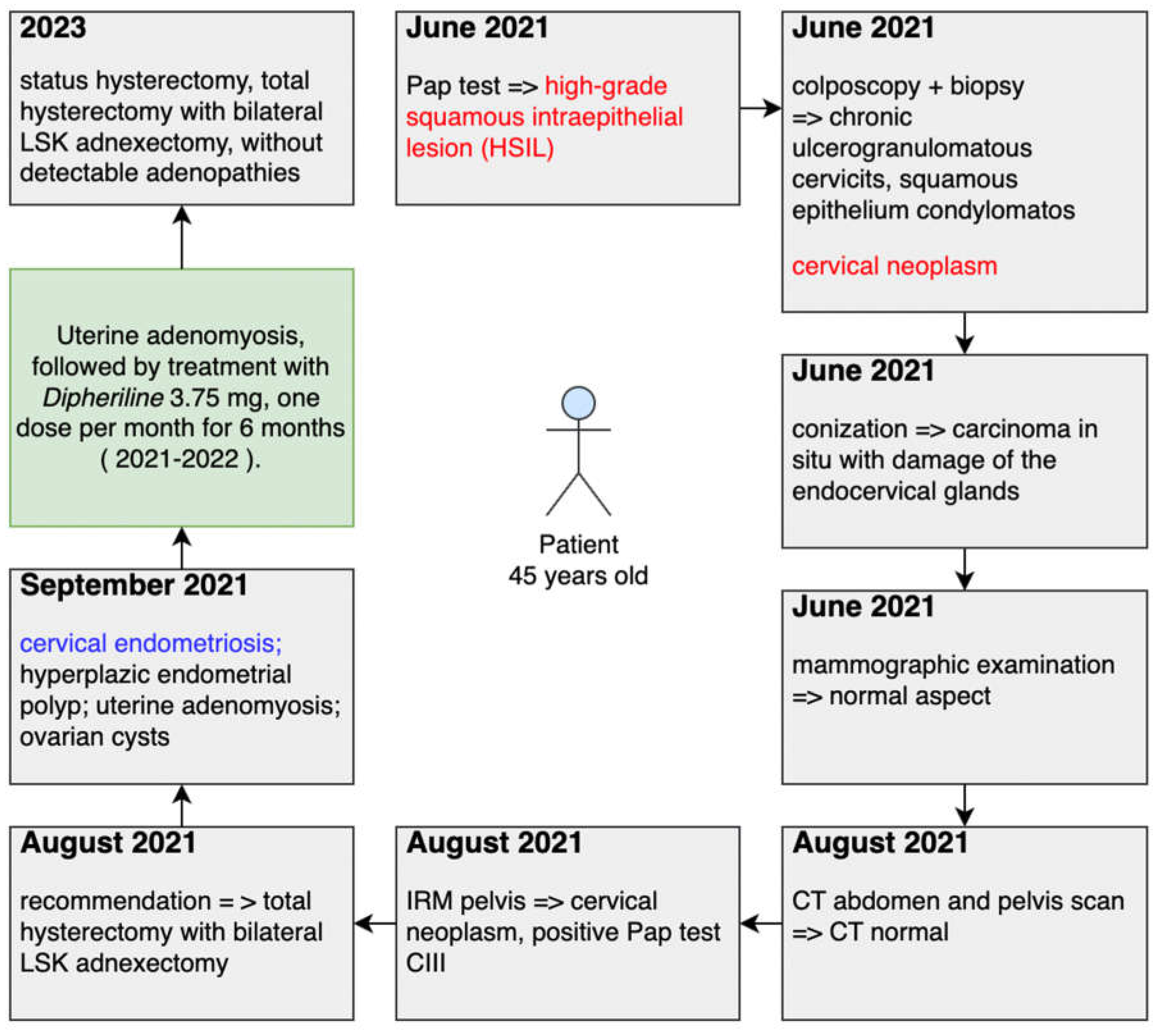
- Total hysterectomy with bilateral LSK adnexectomy
- Post-operative oncological reassessment
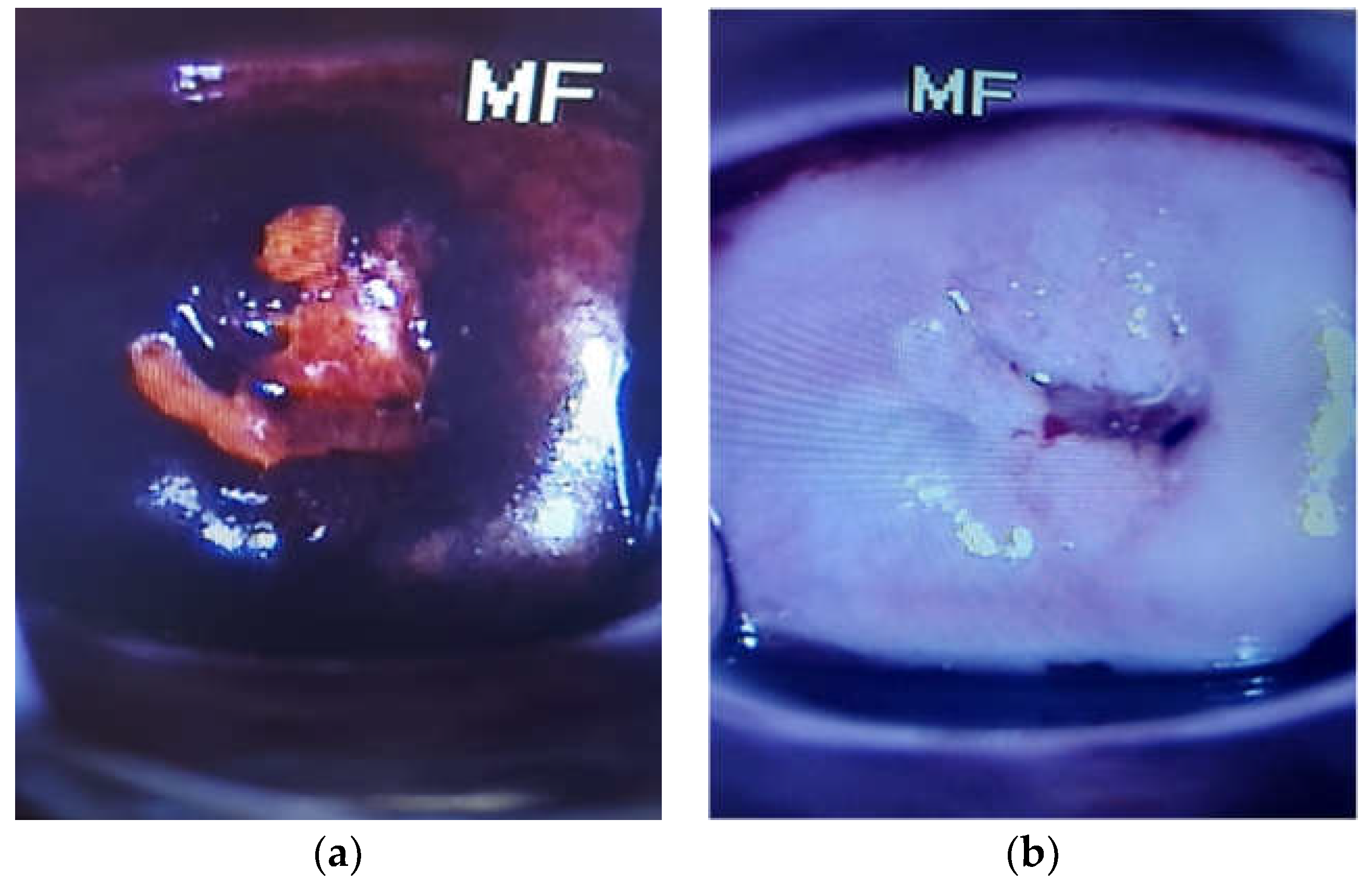
- Cervical size 4.5/3.5/2 cm, with white brown exocervical mucosa, smooth, linear OCE.
- uterine body 5/6.5/4.5 cm. At sectioning, endometrial cavity lined with brown mucosa with brown areas, with a maximum thickness of 0.2 cm; the presence of intracavitary polypoid formation with dimensions of 1.3/0.5/0.1 cm, white-brown, with the implantation base in the isthmic area; white-brown myometer with a beam drawing.
- the right uterine appendix consists of the ovary with dimensions of 2.5/2.2/1.5 cm, with the external surface of the cuneal with a bosselated and the uterine tube with length of 5 cm. At sectioning, non-homogeneous, brown-black appearance, with a cystic with gelatinous, brown-hemorrhagic content; there are present yellow bodies. Paratubar identifies small cystic areas (1.8 cm in diameter).
- the left uterine annex consists of the ovary with dimensions of 3/2.5/1 cm, with the external surface of the cuneal and 4.5 cm long fallopian tube. In the sectioning, a non-homogeneous appearance, brown-tan with multiple cystic areas with gelatinous-green content, the largest with a diameter of 0.9 cm.
- Cervical endometriosis associating non-specific subacute cervicitis lesions.
- Hyperplastic endometrial polyp; uterine adenomyosis.
- Bilateral functional ovarian cysts.
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H., J. Ferlay, R.L. Siegel, M. Laversanne, I. Soerjomataram, A. Jemal, and F. Bray. 2021. "Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries." CA Cancer J. Clin. 71: 209–249. [CrossRef]
- Horne, A. W., & Missmer, S. A. 2022. "Pathophysiology, diagnosis, and management of endometriosis." BMJ (Clinical research ed.) 379, e070750. [CrossRef]
- Naqvi, A., MacKintosh, M. L., Derbyshire, A. E., Tsakiroglou, A. M., Walker, T. D. J., McVey, R. J., Bolton, J., Fergie, M., Bagley, S., Ashton, G., Pemberton, P. W., Syed, A. A., Ammori, B. J., Byers, R., & Crosbie, E. J. 2022. "The impact of obesity and bariatric surgery on the immune microenvironment of the endometrium." International journal of obesity (2005) 46(3): 605–612. [CrossRef]
- Wang S, Li XC, Lang JH. 2011. "Cervical endometriosis: clinical character and management experience in a 27-year span." Am J Obstet Gynecol. 205(5):452.e1-5. [CrossRef] [PubMed]
- Seval MM, Cavkaytar S, Atak Z, Guresci S. 2013. "Postcoital bleeding due to cervical endometriosis." BMJ Case Rep. [CrossRef]
- Felix Wu Shun Wong, Chi Eung Danforn Lim, Sonal Karia, Leonardo Santos. 2010. "Cervical endometriosis: Case series and review of literature." The Journal of Obstretics and Gynaecology Research Volume 36, Issue 4, https://doi.org/10.1111/j.1447-0756.2010.01209.x: 916-919. [CrossRef]
- Ata, B.; Ates, U.; Usta, T.; Attar, E. Cervical endometriosis, a case presenting with ıntractable spotting. " MedGenMed. 2005, 7, 64. [Google Scholar] [PubMed]
- Veiga-Ferreira MM, Leiman G, Dunbar F, Margolius KA. 1987. "Cervical endometriosis: facilitated diagnosis by fne needle aspiration cytologic testing." Am J Obstet Gynecol. 157: 849–856. [CrossRef]
- SM., Ismail. 1991 . "Cone biopsy causes cervical endometriosis and tuboendometrioid metaplasia. ." Histopathology. 18: 107–114. [CrossRef]
- Atalay Mert, S., Dilbaz, B., Ercan, E.E. et al. 2023. "A Rare Case of the Cervical Endometriosis and Overview of the Literature." Reprod. Sci. [CrossRef]
- Siddal RS, Mack HC. 1949. "Primary endometriosis of the vaginal portion of the cervix uteri." Am J Obstet Gynecol. 58: 765–769. [CrossRef]
- Swetha P, Nagashree U, Kondammal R. 2020. "A rare presentation of deep infiltrating cervical endometriosis mimicking cervical cancer." Int J Reprod Contracept Obstet Gynecol. 9: 3903–3905. [CrossRef]
- Félix A, Nogales FF, Arias-Stella J. 2010. "Polypoid endometriosis of the uterine cervix with Arias-Stella reaction in a patient taking phytoestrogens." Int J Gynecol Pathol. 29: 185–188. [CrossRef]
- Lundeen SJ, Horwitz CA, Larson CJ, Stanley MW. 2002. "Abnormal cervicovaginal smears due to endometriosis: a continuing problem." Diagn Cytopathol. 26: 35–40. [CrossRef]
- Nawras Zayat, Ariane M Chabanne, Ishola Adeyemo. Cervical endometriosis in pregnancy: A rare cause of bleeding in pregnancy. J Case Rep Images Obstet Gynecol 2023, 9, 75–78. [Google Scholar] [CrossRef]
- Organization, World Health. n.d. "Endometriosis." 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/endometriosis (accessed on 2 August 2023).
- Parasar P, Ozcan P, Terry KL. 2017. "Endometriosis: Epidemiology, Diagnosis and Clinical Management." Curr Obstet Gynecol Rep. 6(1): 34-41. [CrossRef]
- Farland LV, Shah DK, Kvaskoff M, Zondervan K, Missmer SA. 2015. "Epidemiological and Clinical Risk Factors for Endometriosis." In: D’Hooghe T, editor. Biomarkers for Endometriosis. Springer Science.
- Anaf, V.; Simon, P.; El Nakadi, I.; Fayt, I.; Simonart, T.; Buxant, F.; et al. Hyperalgesia, nerve infiltration and nerve growth factor expression in deep adenomyotic nodules, peritoneal and ovarian endometriosis. Hum Reprod. 2002, 17, 1895–1900. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Tokushige, N.; Markham, R.; Fraser, I.S. Rich innervation of deep infiltrating endometriosis. Hum Reprod. 2009, 24, 827–834. [Google Scholar] [CrossRef]
- Berkley, K.J.; Rapkin, A.J.; Papka, R.E. The pains of endometriosis. Science 2005, 308, 1587–1589. [Google Scholar] [CrossRef]
- SE, Bulun. Endometriosis. N Engl J Med 2009, 360, 268–79. [Google Scholar] [CrossRef]
- JA, Sampson. Metastatic or embolic endometriosis due to menstrual dissemination of endometrial tissue into the venous circulation. Am J Pathol. 1927, 3, 93–109. [Google Scholar]
- Ferguson BR, Bennington JL, Haber SL. Histochemistry of mucosubstances and histology of mixed mullerian pelvic lymph node glandular inclusions: evidence for histogenesis by mullerian metaplasia of coelomic epithelium. Obstet Gynecol. 1969, 33, 617–625. [Google Scholar]
- Joi, A. SAMPSON, MD. 1927. "METASTATIC OR EMBOLIC ENDOMETRIOSIS, DUE TO THE MENSTRUAL DISSEMINATION OF ENDOMETRIAL TISSUE INTO THE VENOUS CIRCULATION." THE AMERICAN JOURNAL OF PATHOLOGY III, 2.
- Sinaii, N.; Plumb, K.; Cotton, L.; Lambert, A.; Kennedy, S.; Zondervan, K.; Stratton, P. Differences in characteristics among 1,000 women with endometriosis based on extent of disease. Fertil Steril. 2008, 89, 538–545. [Google Scholar] [CrossRef]
- Bloski T, Pierson R. 2008. "Endometriosis and Chronic Pelvic Pain: Unraveling the Mystery Behind this Complex Condition." Nurs Womens Health 12(5): 382-395. Nurs Womens Health. [CrossRef]
- Kitawaki, J.; Kado, N.; Ishihara, H.; Koshiba, H.; Kitaoka, Y.; Honjo, H. Endometriosis: The pathophysiology as an estrogen-dependent disease. Journal of Steroid Biochemistry and Molecular Biology 2002, 83, 149–155. [Google Scholar] [CrossRef]
- Signorello, L.B.; Harlow, B.L.; Cramer, D.W.; Spiegelman, D.; Hill, J.A. Epidemiologic determinants of endometriosis: A hospital-based case-control study. Annals of Epidemiology 1997, 7, 267–741. [Google Scholar] [CrossRef] [PubMed]
- C. , Wellbery. Diagnosis and treatment of endometriosis. American Family Physician. 1999, 60, 1753–1762. [Google Scholar]
- Schenken, R.S. Treatment of human infertility: The special case of endometriosis. Reproductive endocrinology, surgery, and technology 1996, 2, 2121–2140. [Google Scholar]
- Dos Reis, R.M.; Silva De Sa, M.F.; De Moura, M.D.; Nogueira, A.A.; Ribeiro, J.U.; Ramos, E.S.; et al. Familial risk among patients with endometriosis. Journal of Assisted Reproduction and Genetics 1999, 16, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Moen, M.H.; Magnus, P. The familial risk of endometriosis. Acta Obstetricia et Gynecologica Scandinavica 1993, 72, 560–564. [Google Scholar] [CrossRef]
- Sinaii, N.; Cleary, S.D.; Ballweg, M.L.; Nieman, L.K.; Stratton, P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: A survey analysis. Human Reproduction 2002, 17, 2715–2724. [Google Scholar] [CrossRef]
- Bertelsen, L.; Mellemkjaer, L.; Frederiksen, K.; Kjaer, S.K.; Brinton, L.A.; Sakoda, L.C.; et al. Risk for breast cancer among women with endometriosis. International Journal of Cancer 2007, 22, 2693–2697. [Google Scholar] [CrossRef]
- Moini, A.; Salari, E.; Rashidi, H.; et al. Evaluation of the association of endometriosis and mammographic breast density, a cross-sectional study. BMC Women's Health 2022, 22, 81. [Google Scholar] [CrossRef]
- Mounsey, A.L.; Wilgus, A.; Slawson, D.C. Diagnosis and management of endometriosis. American Family Physician 2006, 74, 594–600. [Google Scholar]
- Laganà, A.S.; Garzon, S.; Götte, M.; Viganò, P.; Franchi, M.; Ghezzi, F.; Martin, D.C. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int J Mol Sci. 2019, 20, 5615. [Google Scholar] [CrossRef]
- Vercellini P., Aimi G., De Giorgi O., Maddalena S., Carinelli S., Crosignani P.G. 1998. "Is cystic ovarian endometriosis an asymmetric disease?" Br. J. Obstet. Gynaecol. 105: 1018–1021. [CrossRef]
- ercellini P., Abbiati A., Vigano P., Somigliana E.D., Daguati R., Meroni F., Crosignani P.G. 2007. "Asymmetry in distribution of diaphragmatic endometriotic lesions: Evidence in favour of the menstrual reflux theory." Hum. Reprod. 22: 2359–2367. [CrossRef]
- Jenkins, S.; Olive, D.L.; Haney, A.F. Endometriosis: Pathogenetic implications of the anatomic distribution. Obstet. Gynecol. 1986, 67, 335–338. [Google Scholar] [PubMed]
- Winterhager, E. 2012. "Endometriosis: Science and Practice." Role of Steroid Hormones: Estrogen and Endometriosis; 140–144.
- Xin Gao, Jackie Outley, Marc Botteman, James Spalding, James A. Simon, Chris L. Pashos. 2006. "Economic burden of endometriosis." Fertility and Sterility 86 (6): 1561-1572. [CrossRef]
- Toniyan, K.A., E.Y. Gorbacheva, V.V. Boyarintsev, and I.V. Ogneva. 2023. "Endometriosis of the Cervix: A Rare Clinical Case with the Possibility of Comparing the Eutopic and Ectopic Endometrium at the Cellular Level." Int. J. Mol. Sci. 24. [CrossRef]
- Raluca Gabriela SUBA, Ion IONUT, Octavian ENCIU, Bogdan MARINESCU. 2019. "Cervical Endometriosis – Case Report and Review of Literature." Modern Medicine 26, No. 1.
- Junsik Park, Tae-Hee Kim, Hae-Hyeog Lee, Woo Seok Lee, Soo-Ho Chung, Sang-Mo Park. 2011. "Cervical Endometriosis in a Post-menopausal Woman: A Case Report." J Korean Soc Menopause 17, No. 3.
- Phadnis, S.V., Doshi, J.S., Ogunnaike, O. et al. 2005. "Cervical endometriosis: a diagnostic and management dilemma." Arch Gynecol Obstet 272: 289–293. [CrossRef]
- Naho Yokota, MD, MD Hiroshi Yoshida, MD Hideya Sakakibara, MD Yoshiaki Inayama, and MD Fumiki Hirahara. 2008. "A severe vaginal hemorrhage caused by cervical endometriosis." American Journal of Obstetrics & Gynecology. [CrossRef]
- Melin A, Sparen P, Bergqvist A. The risk of cancer and the role of parity among women with endometriosis. Hum Reprod 2007, 22, 3021–3026. [Google Scholar] [CrossRef]
- Brinton LA, Gridley G, Persson I, Baron J, Bergqvist A. Cancer risk after a hospital discharge diagnosis of endometriosis. Am J Obstet Gynecol 1997, 176, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Mingdan Wang, Tongtong Xu, Yue Li, Chen Shi, Lili Jiang, Kuiran Liu. 2022. "Cervical Endometriosis Cyst Complicated with HPV Infection and CIN I:A Case and Review of Literature.
- Priyanka Bagdi*, and Nithya R. 2021. "Cervical Endometriosis: A Case Report." Research Journal of Pharmaceutical, Biological and Chemical Sciences 12 (2).
- J. W. KWEK, M. W. C. H’NG*, S. H. CHEW and E. H. TAY. 2010. "Florid polypoid endometriosis of the cervix with left uretericobstruction: a mimic of cervical malignancy." Ultrasound Obstet Gynecol 36: 252 – 254. [CrossRef]
- Aleksandra Pečovnik, Simona Šramek Zatler, Uršula Salobir Gajšek, Alenka Repše Fokter. 2021. "Cervical endometriosis – a case report and review of literature ." Slovenian Slovenian Medical Medical JournaJourna l l 91(1–2) : 57–60. [CrossRef]
- Bava SV, Thulasidasan AK, Sreekanth CN, Anto RJ. 2016. "Cervical cancer: a comprehensive approach towards extermination. ." Ann Med. 48: 149-161. [CrossRef]
- Cirstoiu, M.; Munteanu, O. Strategies of preventing ureteral iatrogenic injuries in Obstetrics-Gynecology. " Journal of Medicine and Life 2012, 5, 277–279. [Google Scholar] [PubMed]
- Canfell K, Kim JJ, Brisson M, Keane A, Simms KT, Caruana M, Burger EA, Martin D, Nguyen DTN, Bénard É, Sy S, Regan C, Drolet M, Gingras G, Laprise JF, Torode J, Smith MA, Fidarova E, Trapani D, Bray F, Ilbawi A, Broutet N, Hutubessy R. 2020. "Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries." Lancet 395(10224): 591-603. [CrossRef]
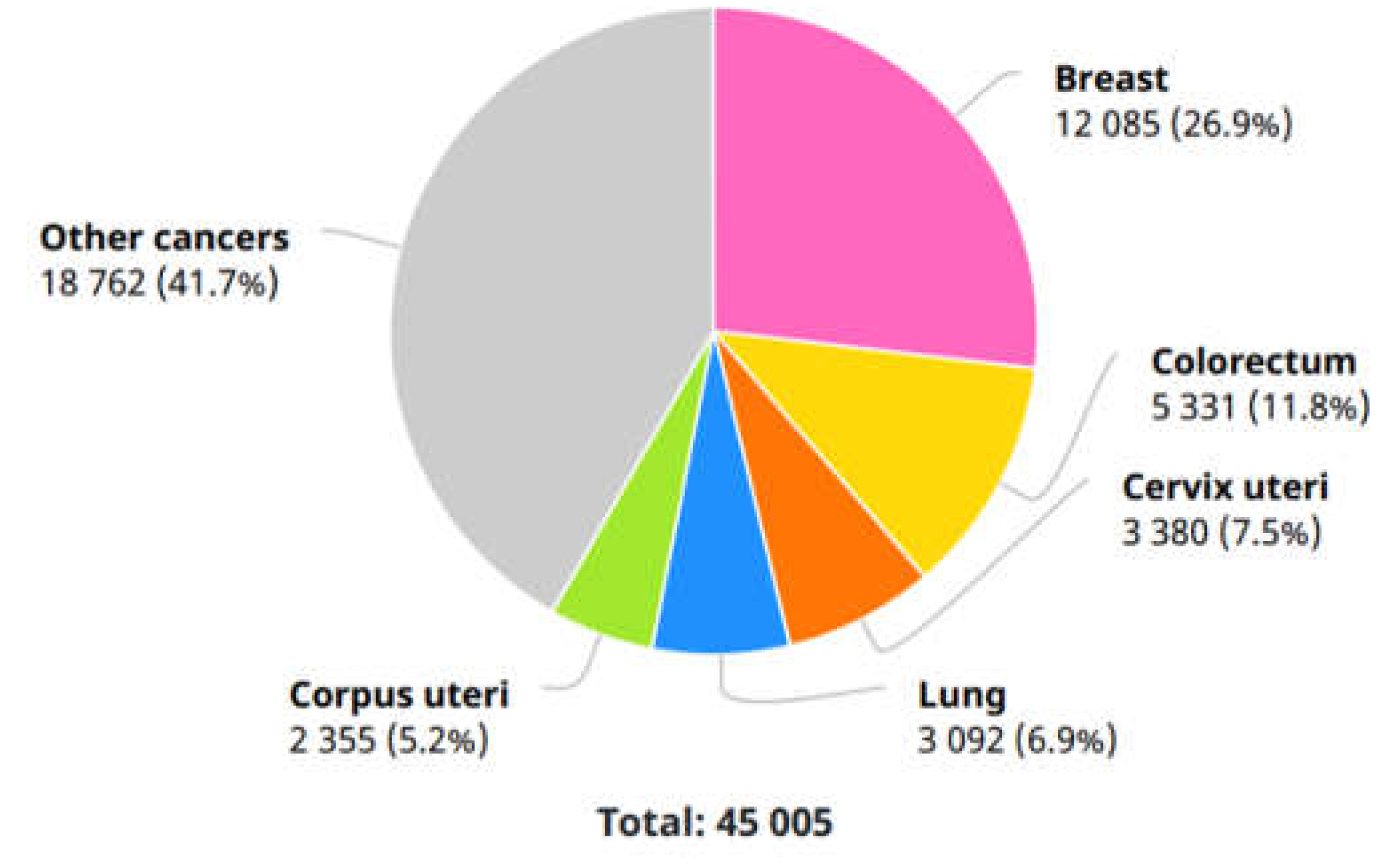
- Deependra Singh, Jerome Vignat, Valentina Lorenzoni, Marzieh Eslahi, Ophira Ginsburg, Beatrice Lauby-Secretan, Marc Arbyn, Partha Basu, Freddie Bray, Salvatore Vaccarella. 2023. "Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative." The Lancent Global Health 11.
- Buskwofie A, David-West G, Clare CA. 2020. "A Review of Cervical Cancer: Incidence and Disparities." J Natl Med Assoc. 112(2): 229-232. [CrossRef] [PubMed]
- Vu M, Yu J, Awolude OA, Chuang L. 2018. "Cervical cancer worldwide." Curr Probl Cancer 42(5): 457-465. [CrossRef]
- Tsikouras, P.; Zervoudis, S.; Manav, B.; Tomara, E.; Iatrakis, G.; Romanidis, C.; Bothou, A.; Galazios, G. Cervical cancer: screening, diagnosis and staging. J BUON. 2016, 21, 320–325. [Google Scholar] [PubMed]
- Chiorean, DM, MI Mitranovici, MC Muresan, CF Buicu, R Moraru, L Moraru, TC Cotoi, et al. 2023. "The Approach of Artificial Intelligence in Neuroendocrine Carcinomas of the Breast: A Next Step towards Precision Pathology?-A Case Report and Review of the Literature." Medicina 59: 672. [CrossRef]
- Melinda-Ildiko Mitranovici, Diana Maria Chiorean, Sabin Gligore Turdean, Maria Cezara Muresan, Corneliu-Florin Buicu, Raluca Moraru, Liviu Moraru, Titiana Cornelia Cotoi, Havva Serap Toru, Adrian Apostol, Claudiu Marginean, Ion Petre, Ioan Emilian Oala, V. 2023. "A Rare Case of Malignant Ovarian Germ Cell Tumor: Dysgerminoma and Seminoma in the Same Patient." Reports 6, (14). [CrossRef]
- Ion Petre, Flavia Barna, Daniela Gurgus, Laurentiu Cezar Tomescu, Adrian Apostol, Izabella Petre, Cristian Furau, Miruna Lucia Năchescu, Anca Bordianu. 2023. "Analysis of the Healthcare System in Romania: A Brief Review." Healthcare 11(14), 2069. [CrossRef]
- MI, Mitranovici, Chiorean DM, Muresan MC, Buicu CF, Moraru R, Moraru L, Cotoi TC, et al. 2022. "Diagnosis and Management of Dysgerminomas with a Brief Summary of Primitive Germ Cell Tumors." Diagnostics 12, 3105. [CrossRef]
- MI Mitranovici, DM Chiorean, AH Sabău, IG Cocuz, AC Tinca, MC Mărginean, MC Popelea, T Irimia, R Moraru, C Mărginean, ML Craina, Izabella Petre, Elena Silvia Bernad, Ion Petre, Ovidiu Simion Cotoi. 2022. "An Interesting Image of Transmural Migration of a Levonorgestrel-Releasing Intrauterine Device (LNg-IUD)." Diagnostics 12(9), 2227. [CrossRef]
- odrin Dan Nicolae Ilea, Lucia Georgeta Daina, Simona Bungau, Delia Mirela Tit, Diana Uivarosan , Lavinia Moleriu, Ion Petre, Constantin Bungau, Izabella Petre. 2020. "Sustainable Management, Instable Legislation Regarding Wages, and Employee Satisfaction/Motivation in Two Romanian Hospitals." Sustainability 12(3), 909. [CrossRef]
- Perkins RB, Wentzensen N, Guido RS, Schiffman M. 2023. "Cervical Cancer Screening: A Review." JAMA 330(6): 547-558. [CrossRef]
- Marwah N, Garg M, Singh S, Sethi D, Sen RJIJOA. 2012. "Research BM Unusual form of squamous cell carcinoma of the cervix extending in situ into the endometrium: three case reports and review of literature." International Journal of Applied and Basic Medical Research 2: 139–141. [CrossRef]
- Hashiguchi M, Kai K, Nishiyama S, Nakao Y, Yokoyama M, Aishima S. 2018. "Clear cell carcinoma of the uterine cervix presented as a submucosal tumor arising in a background of cervical endometriosis." International Journal of Gynecological Pathology 37: 88–92. [CrossRef]
- Saavalainen L, Lassus H, But A, Tiitinen A, Härkki P, Gissler M, Pukkala E, Heikinheimo O. 2018. "Risk of gynecologic cancer according to the type of endometriosis." Obstetrics & Gynecology 131: 1095–1102. [CrossRef]
- Symonds, D.A.; Reed, T.P.; Didolkar, S.M.; Graham, R.R. AGUS in cervical endometriosis. J Reprod Med. 1997, 42, 39–43. [Google Scholar]
- Szyfelbein, W.M.; Baker, P.M.; Bell, D.A. Superficial endometriosis of the cervix: a source of abnormal glandular cells on cervicovaginal smears. Diagn Cytopathol. 2004, 30, 88–91. [Google Scholar] [CrossRef]
- Hanau, C.A.; Begley, N.; Bibbo, M. Cervical endometriosis: a potential pitfall in the evaluation of glandular cells in cervical smears. Diagn Cytopathol. 1997, 16, 274–280. [Google Scholar] [CrossRef]
- Walker, J.L.; Manetta, A.; Mannel, R.S.; Berman, M.L.; DiSaia, P.J. The influence of endometriosis on the staging of cervical cancer. Obstet Gynecol. 1990, 75, 543–545. [Google Scholar]
- Jörg B. Engel, Stefan Heuer, Sabine Segerer, Stephan Rauthe, Johannes Dietl, Arnd Hönig. 2011. "Cervical endometriosis associated with malignant pleural mesothelioma mimicking cervical cancer—Occam’s razor or the “third man”." Fertility and Sterility Volume 95. [CrossRef]
|
Study Ref. |
Total patients |
Age |
Additional information |
Gynecological anamnesis |
Total Pregnancy |
Pregnancy Delivery |
Diagnosis | Treatment |
| [13] 2023* | 1 | 38 | pelvic pain and menstrual irregularity, with endometrioma and adenomyosis, confirmed by histopathological evaluation of the specimen; a hearing impairment; divorce |
an enlarged and fixed cervix, and the gynecological examination was extremely painful for the patient. Pap smear normal Transvaginal ultrasonography |
NS | NS | anechoic cyst in the left adnexal area endocervical curettage the surgical specimens of endometrial sampling and endocervical curettage were found to be secretory endometrium. The presence of focal adenomyosis and 3 leiomyomas that were<2 cm using magnetic resonance imaging (MRI) A lobulated cyst in the left ovary hysteroscopy and cervical biopsy - Hysteroscopic biopsies as proliferative endometrium - cervical punch biopsy => cervical endometriosis pelvic infection endometriotic cyst and nonspecific salpingitis hypertensive very low chance of achieving pregnancy. Requested definitive surgery, including the removal of the right ovary and the uterus. a uterus with adenomyosis and cervical endometriosis |
2 mg/ day of dienogest (Visanne, Bayer Germany). antibiotics for pelvic infection treatment for hypertensive |
| [46], 2023 | 1 | 46 | stable clinical condition with no clinical, microbiological or laboratory evidence of infection, encephalopathy, renal failure, comorbidities including heart failure or pulmonary disease, malignancy, diabetes mellitus | the duration of the menstrual cycle—28 days, regularly, the duration of menstruation—4–5 days, average, painful | 1 | operative delivery (caesarean section) |
First: an endometrial polyp | |
| [50] 2022 | 1 | 27 | vaginal bleeding for 3 months | NS | NS | positive for HPV31, 53, and 56 and complicated with CIN I the rotten flesh-like tissue in the cervical posterior lip tumor was found during surgery |
GnRH | |
| [51] 2021 | 1 | 32 | extracyclic and contact bleeding and cervical erythroplakia regularly participated in the screening program for early detection of cervical cancer (ZORA) |
NS | NS | high-grade squamous intraepithelial lesion (HSIL; CIN3); endometriosis in the cervical transition zone |
||
| [53] 2019 | 1 | 24 | no history of cervical interventions; no family history of endometriosis |
nulliparous and suffered dysmenorrhea 7-VAS, chronic pelvic pain 3-VAS, without dyspareunia | First: cervical dysplasia primary infertility. Final: cervical endometriosis and vaginal endometriotic nodule |
laparoscopic surgery |
||
| [54] 2011 | 1 | 54 | post-menopause; menopause state three years ago without hormone therapy; Pap smear showed reactive cellular changes with inflammation and human papillomavirus (HPV) deoxyribonucleic acid (DNA) Chip test was negative; generally well, weighed 74.9 kg and not pale; underwent laparoscopy assisted vaginal hysterectomy on June 14, 2011 |
2 | full term vaginal deliveries | First: huge myoma uteri Final: Microscopically, both endometrial glands and stroma present at the cervical stroma. Pathologic findings indicate that there was endometriosis at cervix, atrophy at endometrium, and leiomyoma at myometrium |
||
| [55] 2010 | 1 | 48 | nulliparous Chinese woman subtotal hysterectomy and left salpingo-oophorectomy for uterine adenomyosis and left ovarian endometriotic cyst | heavy vaginal bleeding | 4.0-cm heterogeneous cervical mass with internal vascularity and irregular polypoid extension into the left parametrium and causing left hydroureter, suspicious for cervical tumor; an enlarged cervical stump was found with a polypoid mass in the cervical canal; polypoid lesion with histological features of polypoid endometriosis |
|||
| [56] 2008 | 1 | 37 | regular menstrual periods and heavy dysmenorrhea | 0 | regular menstrual periods and heavy dysmenorrhea regular menstrual periods and heavy dysmenorrhea | |||
|
[57] 2005 |
1 | 49 | Pelvic Pain, Intermenstrual bleeding | 2 | Laparoscopy: Endometriosis on the right utero-sacral ligament | Past: LLETZ(large loop excision of the transformation zone) | ||
| 1 | 51 | Citology: Persistent Borderline smears | Pelvic Pain, Postcoital Bleeding | 3 | Laparoscopy: Normal | Past: Nil | ||
| 1 | 43 | Pelvic Pain, Postcoital Bleeding | 3 | Laparoscopy: Endometriosis in the pouch of douglas | Past: LLETZ;Previous cervical cautery | |||
| 1 | 46 | Mild tomoderatedyskaryosis | Intermenstrual Bleeding,Post-coital Bleeding | 2 | Laparoscopy: Endometriosis on both utero-sacral ligaments | Past: LLETZ;Previous Cervical Cryocautery | ||
| 1 | 36 | Persistent borderline smears | Intermenstrual Bleeding | 3 | Laparoscopy: Normal | Past: LLETZ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




