Submitted:
07 August 2023
Posted:
22 August 2023
You are already at the latest version
Abstract

Keywords:
Introduction
Methods
Statistical analysis
Results
Discussion
References
- Group, W.C.R.C.W. World Health Organization cardiovascular disease risk charts: revised modAAels to estimate risk in 21 global regions. Lancet Glob Health 2019, 7, e1332–e1345. [Google Scholar] [CrossRef]
- Bowling, A.; Culliford, L.; Smith, D.; Rowe, G.; Reeves, B.C. What do patients really want? Patients' preferences for treatment for angina. Health Expect 2008, 11, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, L.W.; Hellkamp, A.S.; Leier, C.V.; Sopko, G.; Koelling, T.; Warnica, J.W.; Abraham, W.T.; Kasper, E.K.; Rogers, J.G.; Califf, R.M.; et al. Changing preferences for survival after hospitalization with advanced heart failure. J Am Coll Cardiol 2008, 52, 1702–1708. [Google Scholar] [CrossRef] [PubMed]
- Martin-Fernandez, J.; Polentinos-Castro, E.; del Cura-Gonzalez, M.I.; Ariza-Cardiel, G.; Abraira, V.; Gil-LaCruz, A.I.; Garcia-Perez, S. Willingness to pay for a quality-adjusted life year: an evaluation of attitudes towards risk and preferences. BMC Health Serv Res 2014, 14, 287. [Google Scholar] [CrossRef] [PubMed]
- Meropol, N.J.; Egleston, B.L.; Buzaglo, J.S.; Benson, A.B., 3rd; Cegala, D.J.; Diefenbach, M.A.; Fleisher, L.; Miller, S.M.; Sulmasy, D.P.; Weinfurt, K.P.; et al. Cancer patient preferences for quality and length of life. Cancer 2008, 113, 3459–3466. [Google Scholar] [CrossRef] [PubMed]
- Marta, G.N.; Del Nero, L.G.; Marta, G.N.; Mangabeira, A.; Critchi, G.; Kovacs, M.J.; Silva, J.L.; Saad, E.D. Treatment priorities in oncology: do we want to live longer or better? Clinics (Sao Paulo) 2014, 69, 509–514. [Google Scholar] [CrossRef]
- Rahman, I.A.; Kendall, S. Cardiac surgery in the very elderly: it isn’t all about survival. The British Journal of Cardiology 2020, 27, 3. [Google Scholar] [CrossRef]
- Ruigrok, A.N.; Salimi-Khorshidi, G.; Lai, M.C.; Baron-Cohen, S.; Lombardo, M.V.; Tait, R.J.; Suckling, J. A meta-analysis of sex differences in human brain structure. Neurosci Biobehav Rev 2014, 39, 34–50. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.M.; Chan, C.C.; Leung, A.W.; Fox, P.T.; Gao, J.H. Sex-related differences in neural activity during risk taking: an fMRI study. Cereb Cortex 2009, 19, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.S.; Bechara, A.; de Paula, J.J.; Romano-Silva, M.A.; Correa, H.; Lage, G.M.; Miranda, D.M.; Malloy-Diniz, L.F. Influence of COMT Val(158)Met polymorphism on emotional decision-making: A sex-dependent relationship? Psychiatry Res 2016, 246, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.; Menning, S.; Schelhase, T. Demografische Perspektiven zum Altern und zum Alter. Gesundheitsberichterstattung des Bundes 2009, Gesundheit und Krankheit im Alter, 21-30.
- Lindeboom, J.J.; Coylewright, M.; Etnel, J.R.G.; Nieboer, A.P.; Hartman, J.M.; Takkenberg, J.J.M. Shared Decision Making in the Heart Team: Current Team Attitudes and Review. Struct Heart 2021, 5, 163–167. [Google Scholar] [CrossRef]
| Patients (N) | 1349 |
|---|---|
| Age (years) | 68.49 ± 10.74 |
| Female (%) | 29.28 |
| BMI | 28.62 ± 5.24 |
| EuroScore II (%) | 3.71 ± 5.19 |
| STS Score (%) | 2.16 ± 2.87 |
| NYHA Score | 2.65 ± 0.79 |
| Angina Pectoris – CCSS | 2.00 ± 1.02 |
| Diabetes (%) | 35.80 |
| Hypertension (%) | 89.02 |
| Current smoker (%) | 17.36 |
| Lipid disorder (%) | 64.76 |
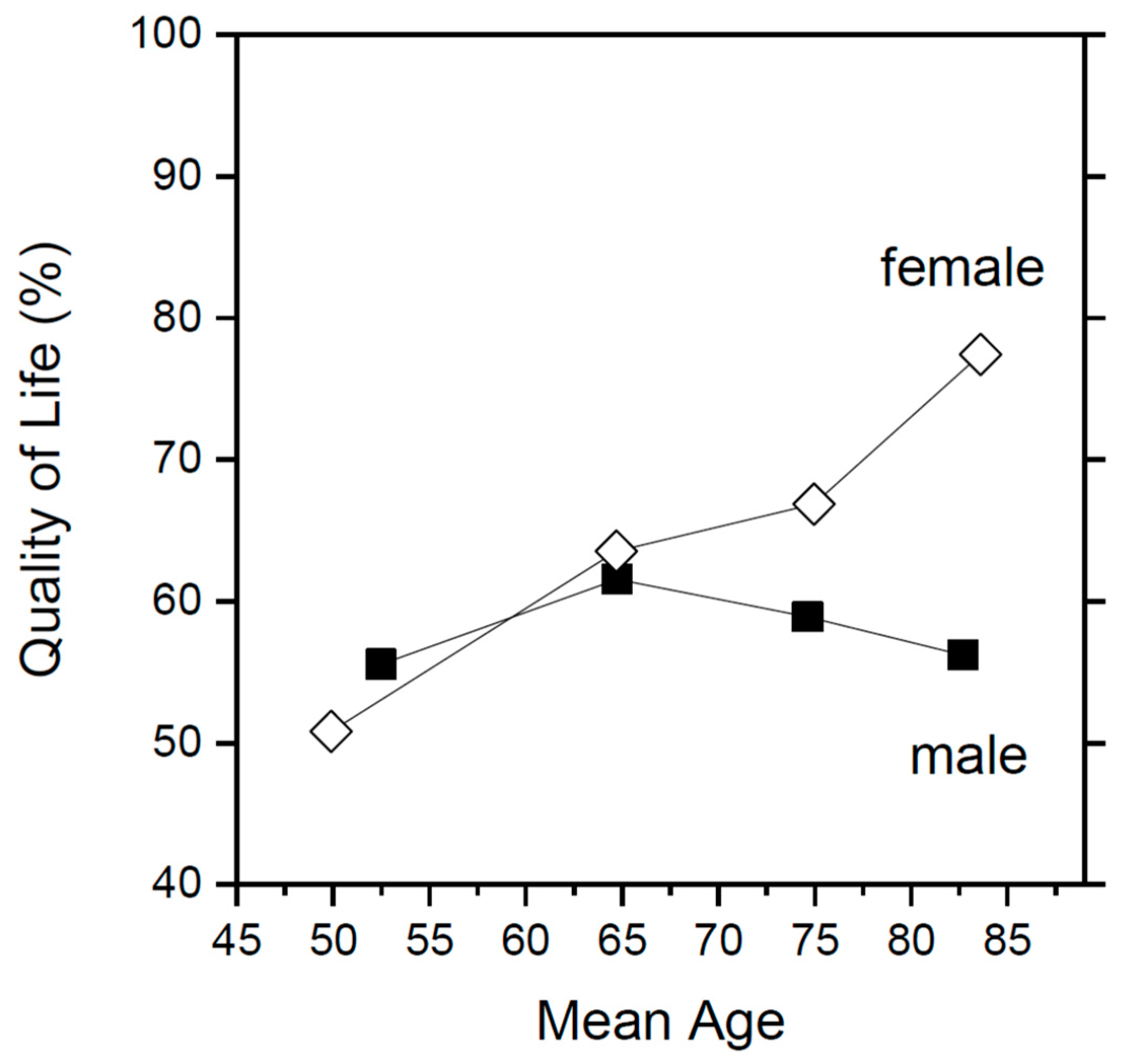
| Males (n=954) | Females (n=395) | Total (n=1349) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age below 60 | 1.00 | 1.00 | 1.000 | ||||||
| Age 60-69 | 1.27 | 0.88 - 1.83 | 0.21 | 1.69 | 0.88 - 3.24 | 0.12 | 1.358 | 0.99 - 1.87 | 0.06 |
| Age 70-79 | 1.14 | 0.80 - 1.62 | 0.46 | 1.97 | 1.09 - 3.56 | 0.03 | 1.335 | 0.99 - 1.80 | 0.06 |
| Age above 80 | 1.02 | 0.63 - 1.64 | 0.95 | 3.32 | 1.52 - 7.23 | 0.003 | 1.482 | 0.99 - 2.21 | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





