Submitted:
22 August 2023
Posted:
23 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
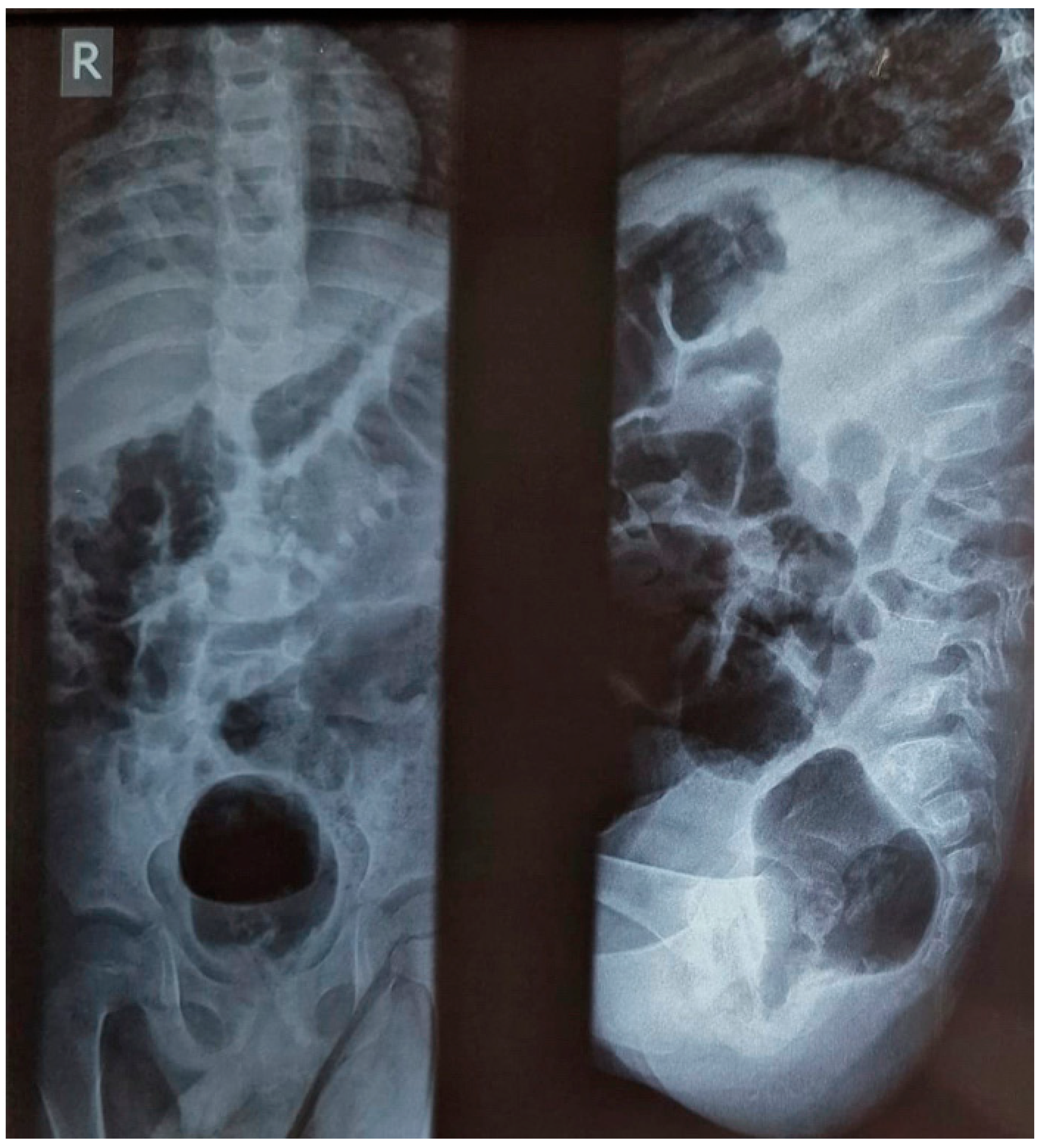
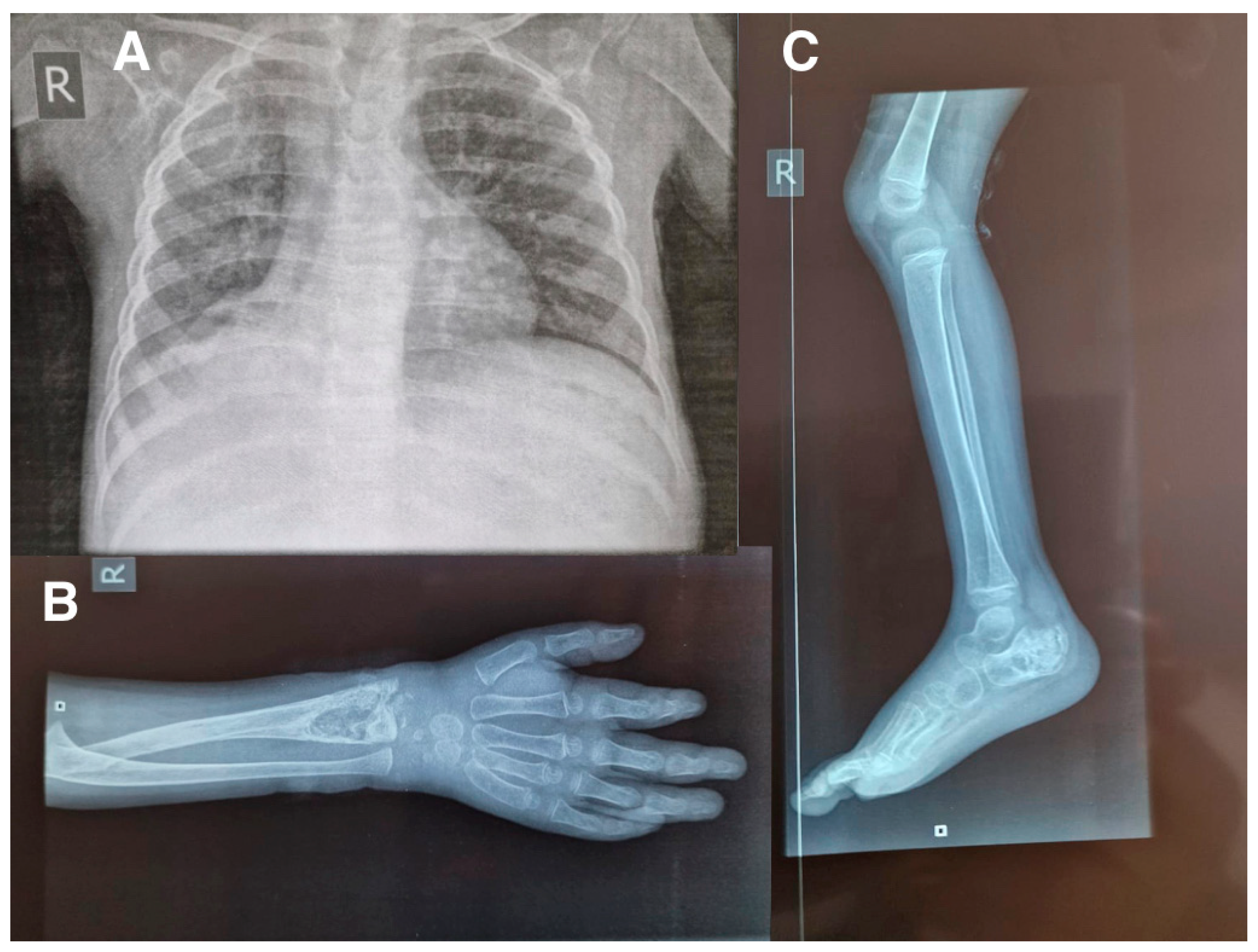
2. Case report
3. Discussion
4. Conclusions
Informed Consent Statement
Conflicts of Interest
References
- Di Gennaro, F.; Pizzol, D.; Cebola, B.; Stubbs, B.; Monno, L.; Saracino, A.; Luchini, C.; Solmi, M.; Segafredo, G.; Putoto, G.; et al. Social determinants of therapy failure and multi drug resistance among people with tuberculosis: A review. Tuberculosis 2017, 103, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, S.; Rekha, B. Pediatric Tuberculosis: Global Overview and Challenges. Clin. Infect. Dis. 2010, 50, S184–S194. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.Y.; Dosa, K.; Fuad, A.; Ibrahim, W.; Alaini, A.; Osman, L.; Albadri, M.; Yassin, M.A.D. Disseminated Tuberculosis among Adult Patients Admitted to Hamad General Hospital, Qatar: A Five Year Hospital Based Study. Mycobact. Dis. 2016, 6. [Google Scholar] [CrossRef]
- Marotta, C.; Gennaro, F.; Pizzol, D.; Madeira, G.; Monno, L.; Saracino, A.; Putoto, G.; Casuccio, A.; Mazzucco, W. The At Risk Child Clinic (ARCC): 3 Years of Health Activities in Support of the Most Vulnerable Children in Beira, Mozambique. Int. J. Environ. Res. Public Heal. 2018, 15, 1350. [Google Scholar] [CrossRef] [PubMed]
- Didel, S.; Purohit, A.; Vyas, V.; Kumar, P. Disseminated tuberculosis in children—a difficult diagnose depends on how far we can go. BMJ Case Rep. 2020, 13, e237192. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, M.; Nordholm, A.-C.; Ssekyanzi, B.; Byamukama, O.; Orikiriza, P.; Tusabe, T.; Nyehangane, D.; Taremwa, I.M.; Turyashemererwa, E.; Wobudeya, E.; et al. Mortality and Cause of Death in Children With Presumptive Disseminated Tuberculosis. Pediatrics 2023, 151. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Mohan, A.; Sharma, A. Miliary tuberculosis: A new look at an old foe. J. Clin. Tuberc. Other Mycobact. Dis. 2016, 3, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Pizzol, D.; Veronese, N.; Marotta, C.; Di Gennaro, F.; Moiane, J.; Chhaganlal, K.; Monno, L.; Putoto, G.; Mazzucco, W.; Saracino, A. Predictors of therapy failure in newly diagnosed pulmonary tuberculosis cases in Beira, Mozambique. BMC Res. Notes 2018, 11, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Segala, F.V.; Papagni, R.; Cotugno, S.; De Vita, E.; Susini, M.C.; Filippi, V.; Tulone, O.; Facci, E.; Lattanzio, R.; Marotta, C.; et al. Stool Xpert MTB/RIF as a possible diagnostic alternative to sputum in Africa: a systematic review and meta-analysis. Front. Public Heal. 2023, 11, 1117709. [Google Scholar] [CrossRef] [PubMed]
- Di Gennaro F, Cotugno S, Fasano M, Ricciardi A, Ronga L, Lattanzio R, Grimaldi A, Bavaro DF, Ciarallo M, Garzone S, De Iaco G, Guido G, Fiore JR, Brindicci G, Santoro CR, Sica S, Iacovazzi TL, Santantonio TA, Saracino A. High risk of unsuccessful treatment outcome in migrant population with tuberculosis: Data from three Italian hospitals. Front Public Health. 2023 Jan 10;10:1024474.
- Di Gennaro F, Marotta C, Antunes M, Pizzol D. Diabetes in active tuberculosis in low-income countries: to test or to take care? Lancet Glob Health. 2019 Jun;7(6):e707.

| Parameter | Admission | 2 days after | 5 days after |
|---|---|---|---|
| WBC | 13.3x103/uL | 15.04x103/uL | 14.17x103/uL |
| LYM | 5.8 (43.7%) | 5.5 (37%) | 6.36 (44.9%) |
| NEUT | 6.5 (48.7%) | 7.9 (52.5%) | 5.88 (41.4%) |
| RBC | 4.77x106/uL | 4.62x106/uL | 4.72x106/uL |
| HGB | 7.5g/dl | 7.4g/dl | 7.7g/dl |
| MCV | 57.9 fL | 54.1fL | 54.2fL |
| MCH | 15.7 pg | 16.0pg | 16.3pg |
| MCHC | 27.2g/dl | 29.6g/dl | 30.1g/dl |
| PLT | 1000x103/uL | 944x103/uL | 1030x103/uL |
| Na | 133 mEq/L | NR | 132.9 mEq/L |
| K | 4.37 mEq/L | NR | 5.44 mEq/L |
| Cl | 98 mEq/L | NR | 98 mEq/L |
| Creatinine | 20.3 umol/L | NR | 22.33 umol/L |
| ALT | 16.54 U/L | NR | 26 U/L |
| AST | 31.33 U/L | NR | 43 U/L |
| Urea | 3.01 mg/dL | NR | 2.47 mg/dL |
| Glucose | 4.86 mmol/L | NR | 3.5 mmol/L |
| ESR | 51mm/h | NR | NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





