1. Introduction
The main cause of mortality and morbidity for adults and elderly worldwide are cardiovascular diseases, primarily due to coronary and non-coronary vascular atherosclerosis. The Framingham Heart Study (FHS), a multigenerational study initiated in 1948, had a major contribution in understanding the causes of coronary disease, stroke, and other cardiovascular pathologies, as well as their prevention strategies. Framingham defined these causes as risk factors for heart disease. Among all these factors, FHS emphasized the major independent elements such as: smoking, arterial hypertension, high total cholesterol and LDL-cholesterol (LDL-c), low HDL-cholesterol (HDL-c), diabetes type II, age, obesity, and a sedentary lifestyle. [
1] In previous years, substantial research was concentrated on the clinical evaluation of these risk factors. However, as time passed, progresses and new discoveries arose in the medical world, and the attention shifted to other screening and diagnostic elements associated with cardiovascular diseases, such as: adipose tissues biomarkers (leptin, resistin, adiponectin), proinflammatorystatusbiomarkers (high sensitive C reactive protein – hsCRP), prothromboticstatusbiomarkers (fibrinogen, plasminogen activator inhibitor-1 – PAI-1), abnormal fat tissue distribution (visceral fat, hepatic steatosis), insulin resistance (IR) and hyperinsulinemia (HI). [
1,
2]Consequently, the metabolic syndrome was defined as a cluster of clinical and biological elements thatprovide patients with a high cardiovascular risk. [
2] Populational studies revealed a doubling of the cardiovascular events risk in individuals with metabolic syndrome, and for non-diabetic patients, the condition increased the risk of developing type II diabetes up to five times. [
2,
4,
5]
In 1999, the World Health Organisation (WHO)first defined the notion of metabolic syndrome, emphasizinghyperglycaemia and insulin resistance as the main pillars of the condition. [
7] Next, came the description formulated by NCEP/ATP III (National Cholesterol Education Programme/Adult Treatment Panel III), published in 2001, and this became the most renowned definition of theentity. [
6]According to the NCEP report, three or more of the following criteria represents the syndrome: 1) waist circumference > 102 cm in men and > 88 cm in women, 2) concentration of triglycerides ≥150 mg/dl (1.7 mmol/l), 3) concentration of HDL-c < 40 mg/dl (1.03 mmol/l) in men and < 50 mg/dl (1.29 mmol/l) in women, 4) systolic blood pressure ≥130 mmHg or a diastolic blood pressure ≥ 85 mmHg, and 5) fasting glucose ≥ 110 mg/dl (≥ 5.6 mmol/l). [
3] However, the International Diabetes Federation (IDF) released new criteria four years later, highlighting central adiposity as a mandatory element for the condition, plus two or more factors: 1) raised levels of triglycerides ≥ 150 mg/dl (1.7 mmol/l) or specific treatment for this lipid abnormality, 2) low concentration of HDL-c < 40 mg/dl (1.03 mmol/l) in men and < 50 mg/dl (1.29 mmol/l) in women or specific treatment, 3) high systolic blood pressure≥ 130 mmHg or high diastolic blood pressure ≥ 85 mmHg, or treatment of previously diagnosed hypertension, and 4) increased concentration of fasting glucose ≥ 100 mg/dl (5.6 mmol/l) or previously diagnosed type II diabetes. [
2,
3]
In 2009, the American Heart Association (AHA) and the National Heart, Lung, and Blood Institute (NHLBI), focusing on the cumulate of risk factors, together with the IDF, which accentuates the role of the waist circumference, attempted to unify all these components. As a result, waist circumference was no longer a mandatory element of thecriteria used to define the metabolic syndrome. [
12]
All these diverse interpretations led to substantial confusion regarding the concept of metabolic syndrome. [
7] Ultimately, the metabolic syndrome is viewed as a pathological cluster of interconnected metabolic risk factors that directly increase the likelihood of developing atherosclerotic coronary diseaseand type II diabetes. [
8]
The underlying causes of metabolic syndrome are complex and involve a combination of genetic, environmental, and lifestyle factors, such as poor diet, sedentary behaviour, and increased weight. The syndrome’s prevalence has been rising globally, coinciding with higher rates of obesity, especially abdominal obesity, and type II diabetes. Augmented insulin resistance, along with old age and central adiposity, represent the main pathophysiological mechanisms which explain the rise in the prevalence of the metabolic syndrome. [
2,
9]
The management of metabolic syndrome mainly involves lifestyle changes. Weight loss, proper nutrition, and adequate physical activity are the fundamental elements of treatment, but medication,according to existing guidelines, might also be prescribed to address specific contributors to the condition, such as high blood pressure or dyslipidaemia. Early detection and intervention are also crucial in lowering the risk of associated cardiovascular complications. [2, 10]
This paper aims to study the correlation between environmental elements, poor lifestyle choices, and the risk of developing metabolic syndrome. We systematically analysed the relation between gender, background, education level, smoker/non-smoker status, physical activity, diet, and the presence of the syndrome. Identifying a specific diet, or certain nutrients, that could reduce the risk of developing this condition, would enhance existing cardiovascular prevention strategies and the prognosis of metabolic syndrome.
2. Materials and Method
A total number of 117 patients were included in the study (53 men, respectively 64 women), with ages between 30 to 79 years old. It was a prospective study, taking place over the course of one year (January 2022 – February 2023) .The participants in the study were selected from among the patients who presented themselves for a cardiological consultation, being addressed by the family doctor.
The study protocol was approved by the ethics committee of Bihor County Clinical Emergency Hospital. Paraclinical investigations, as well as clinical examinations, were performed for every patient.The main parameters of interest were evaluated at the inclusion (T1) : total cholesterol level (TC), blood pressure (BP), triglycerides values (TG), HDL-c, plasma fasting glucose (PFG). All of the measurements were repetead after 6 and 12 month thus creating three time points (T1, T2, T3) for the comparison of the results. Additionally, all the patients filled out a questionnaire regarding their socioeconomic status (age, level of education, occupation), dietary habits, smoking and alcohol consumption, physical activity.
We analysed the patients’ dietary habits, considering the number of meals per day (≥ 3/day vs < 3/day) and the preference for certain types of food.
Regarding the consumption of lipids, the patients declared:
Concerning meat consumption, the patients were divided into three groups:
no consumption
red meat preference – beef, pork, lamb (rich in saturated fatty acids)
white meat preference – herring, salmon, mackerel, tuna, sardine (rich in unsaturated fatty acids from the omega-3 group) and bird meat (rich in omega-6 fatty acids)
Fresh fruits and vegetables (omega-3, omega-6 and omega-9 acids source) were consumed as following:
Concurrently, the salt intake was also quantified, and the patients were divided as following:
The patients were grouped into 3 categories regarding smoking or alcohol consumption:
With respect to physical activity, we considered individuals as physically active if exercises of moderate intensity were practiced at least 5 times a week, such as 30–60-minute fast walks. Furthermore, patients included in this study were classified into 3 categories based on their education level:
higher education level – postgraduate studies, undergraduate studies, vocational school
medium education level – high school
lower education level – primary education
In this study, cardiovascular prevention strategies were applied. Apart from pharmaceutical therapies, patients were given advice meant to correct the conditions pertaining to the constellation of elements which is the metabolic syndrome. They were included into smoking cessation programs, while withdrawal symptomatology was diminished with the help of nicotine gum, sprays, or patches. On the recommendation of the specialist physician, the patients participated into individualized sport programs, gradually used by each person, while they were also advised on methods for adopting a healthy diet.
To establish the diagnosis of metabolic syndrome, the IDF/AHA/NHLBI (2009) consensus definition we already covered was used. [
3] The exclusion criteria targeted the following categories of patients:
individuals with insufficient data, especially regarding serum levels of PFG, TG, HDL-c, blood pressure, body mass index (BMI);
patients diagnosed with infectious diseases, also the ones diagnosed with hepatitis B or C, liver or renal failure, hepatic cirrhosis, malignant neoplasm;
patients deceased during the study.
The statistical analysis of the data was performed with the Statistica 8.0 .It were performed t-test for numeric variables, chi-square testand cross-tabulation for categorical variables, univariate analysis and multiple regression for independent predictors of metabolic syndrome.
The statistically significant value was considered a value of p˂0.05.
3. Results
The studywas conducted between January 2022 and February 2023. The main characteristics of the patients included into the study are presented in
Table 1.
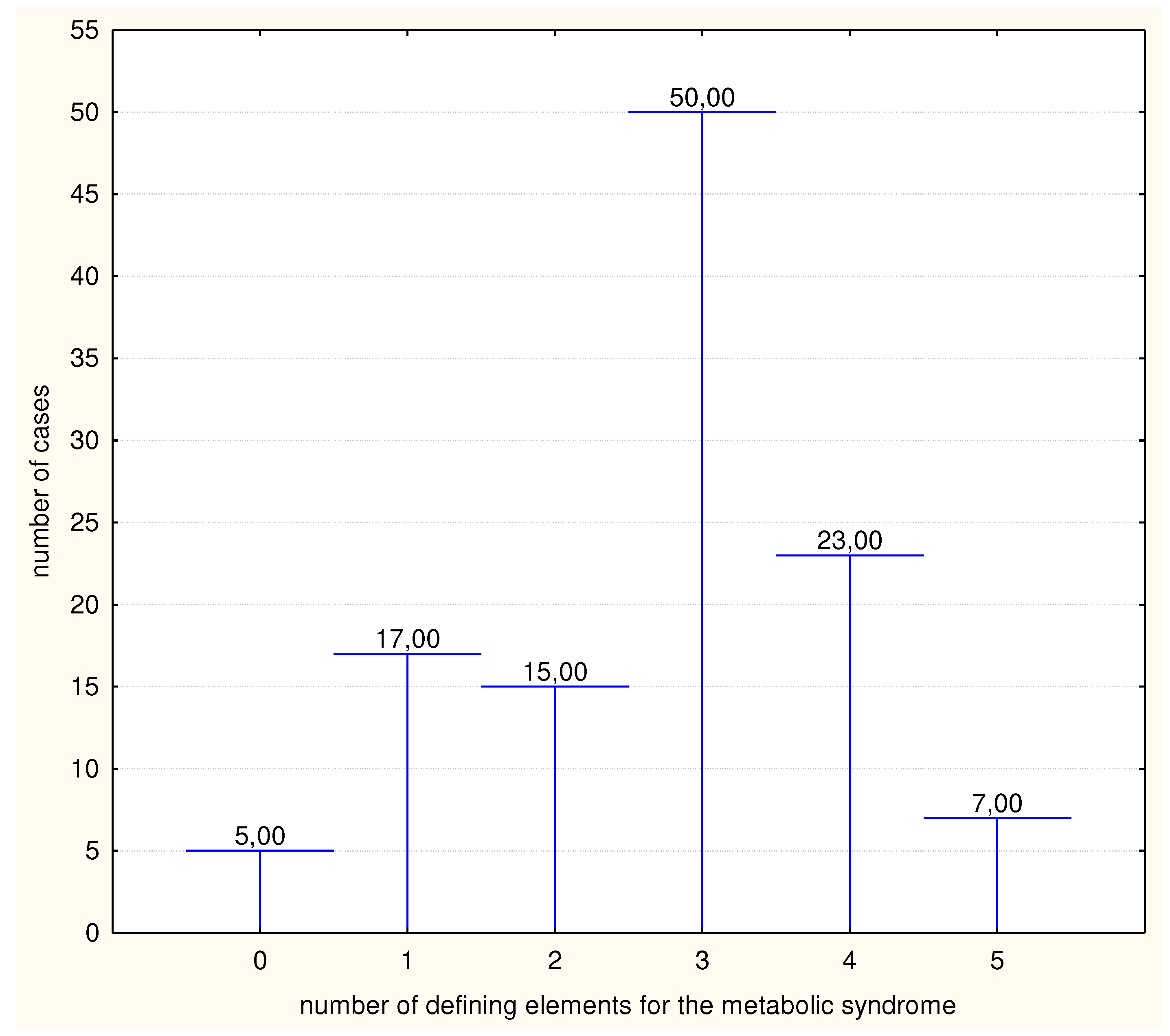
At the start point of the study (T1), our results indicated that the incidence of the metabolic syndrome reached a value of 68.37% in the examined population. (
Figure 1)
Thus, 80 patients presented a minimum of 3 elements of the metabolic syndrome out of 5, while 37 individuals presented two, one, or no factors. Central adiposity seems to be the most prevalent component, present in 76,92% of the participants. The second most common factor was high blood pressure, with an incidence of 70,08 %, while on the opposite pole, high fasting glucose was reported in 33,33% of the cases.
The main predictors for metabolic syndrome at T1 were lipids intake and lack of physical activity (p˂0,05).
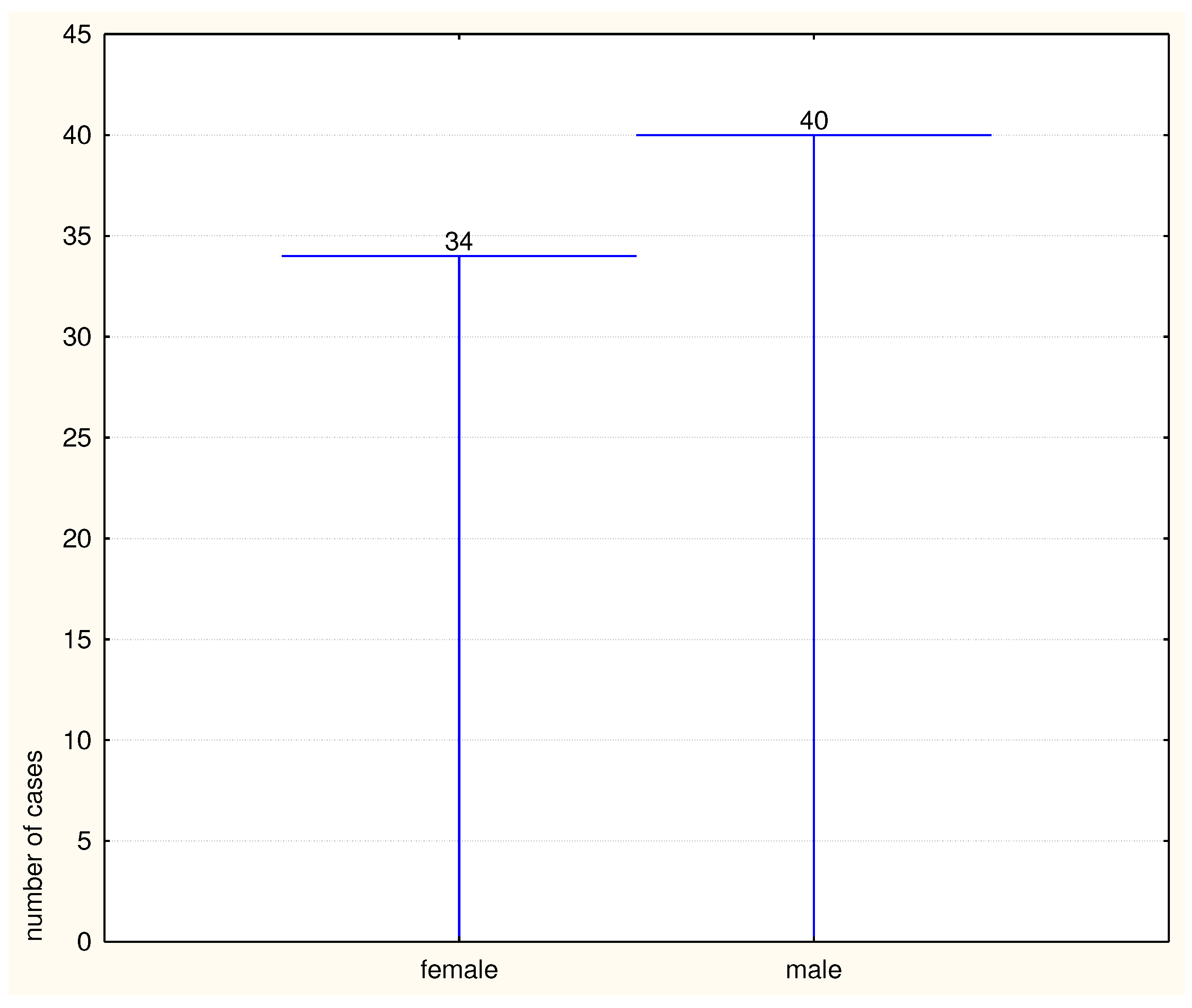
Furthermore, we also determined the incidence of the metabolic syndrome based on gender distribution: females 52,5% (n=42) and 47,5% males (n=38), p=0,73.
When the correlation between age and the incidence of metabolic syndrome was analysed, it has been observed that the distribution by gender was directly proportional with age, the increasing tendency being present in both men and women ( correlation coefficient r=0,24, p=0,009).
A higher education level (vocational training, university, postgraduate studies-
Table 2) was present in 30,7% of patients. Additionally, we were able to confirm that the metabolic syndrome is more prevalent in patients with low or medium level studies, with a notable difference between the two categories (74% vs 52,7% , p=0,0008).
Regarding environment, our data suggest that a rural background may be a predisposing factor of the syndrome, the discrepancies in the ratio also being quite remarkable (78,6% versus 51,10%, p=0,001).
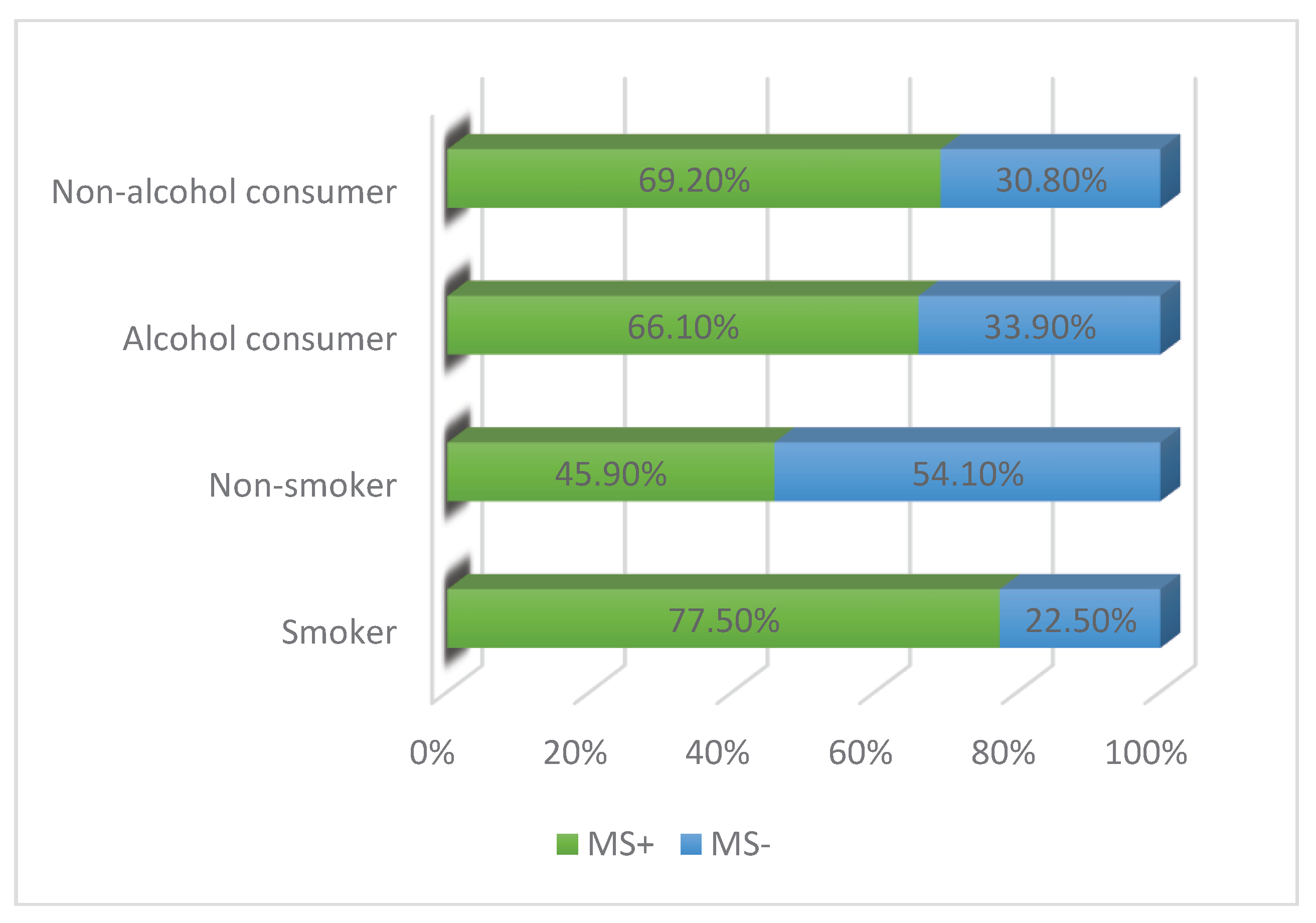
Considering the connection between smoking and the metabolic syndrome, we note that a smoker status represents a considerable risk factor for the condition. Regarding alcohol consumption, our data does not indicate major discrepancies, the link between alcohol and the metabolic entity being even weaker among regular consumers. (
Figure 2)
Furthermore, in terms of alcohol beverages, the results reveal that patients presenting with the metabolic syndrome prefer beer(41%) and wine (33%), over hard liquors (23%).
The relationship between dietary habits and the metabolic syndrome was also analysed, the patients being investigated regarding the number of meals per day ,lipids intake (saturated or trans), meat consumption, salt intake, fresh vegetables and fruit intake and carbonated drinks consumption
We observed thatmetabolic syndrome was more frequent in individuals with a habit of eating under three meals a day. Thus, 30 patients from 41 in total ( 73,2%) that have 2 meals per day were identified with metabolic syndrome (p=0,004) and also 4 patients from 5 patients (80%) who declared to have only one meal/day.
Other significant risk factors we found were the consumption of lipids, saturated and trans, and the preference for red meat. The exclusive intake of white meat seems to be a protective factor against the syndrome (42,5% vs 70,7%, r=0,32, p=0,032). Overall, a diet rich in meat was revealed to favour the appearance of the metabolic syndrome, possibly due to a higher percentage of consumed red meat.
The results of our study also suggest that the consumption of fresh fruits and vegetables has a protective role against the onset of metabolic syndrome, even in conditions of individuals that have unhealthy habits , such as the consumption of salt or carbonated drinks (p=0,036)
Last, but not least, we analysed the correlation between physical activity and the incidence of the metabolic syndrome.Thus, a sedentary lifestyle was proven to be a considerable risk factor for the appearance of the metabolic syndrome.
At the 6 month visit ( visit T2), not every patient was able to follow the recommended prevention schemes. Nevertheless, we can still clearly observe a decrease incidence of metabolic syndrome among the studied population (n=69, 59% ).
Regarding the frequency of the elements defining the metabolic syndrome, central obesity remained in first place, identically to the start of the study, while the last commonly encountered factor was low levels of HDL-col. (
Table 1). Regarding gender distribution in the second point of the study (T2) , males seem to maintain a higher risk in developing the metabolic syndrome compared to women, but not significant (45,3% versus 54,7%, p=0,92).
After 12 months( T3visit) ,final vis) it could be observed an important increase in the prevalence of the metabolic syndrome (74 patients,63,2%).
Regarding the factors pertaining to the metabolic syndrome, central adiposity manifested a progressive increase (54,70%) , while the increased fasting glucose was the least represented element (25,6%). The gender distribution of the metabolic syndrome in indicates a higher risk of the syndrome in men compared to women figure number (
Figure 3) .
At the end of the study, our results indicated a decrease in the prevalence of metabolic syndrome with over 4%, decrease sustained by the lowering prevalence among the masculine gender. The evolution of the prevalence of each element defining the metabolic syndrome is showOver the course of the study, out of the five elements of the metabolic syndrome, a decrease was highlighted for BP, TG and HDL-c levels. Central obesity and high fasting glucose were present at 54,70% of the study population and high blood pressure at 68,9%.
The high value of fasting glucose remains the least observed element of metabolic syndrome (25,6%). The observation is interesting since we expect that among predominantly obese individuals, there is a secondary hyperinsulinemia with an impact on glycemic values. Therefore, we analyzed the predictors for glycemic values recorded in obese patients, and the strongest predictor for normal glycemic values in obese patients was regular physical exercise (p˂0,0001).
4. Discussions
The metabolic syndrome is a public health concern, due to its high and continuously increasing prevalence and incidence, even gaining a pandemic trait in recent years. [
13] The purpose of this work is to evaluate the risk factors involved in the metabolic syndrome, while emphasizing their significant roles in developing cardiovascular complications. We identified nonmodifiable risk factors, such as gender and age, and modifiable elements, referring to low educational levels, rural background, smoking, a diet rich in lipids and poor in fresh vegetables and fruits, as well as a sedentary lifestyle.
The prevalence of metabolic syndrome over the course of the study (January 2022 – February 2023) was 63.3%. Regarding the gender distribution, our data suggests that men present a higher prevalence of the syndrome compared to women (52,5% versus 47,5% males, p=0,73 .
At the second examination, in T2, more than a third of the patients who presented metabolic syndrome at the beginning of the study did not qualify for the condition anymore. Out of the 38 individuals in the control group, 10 patients presented a minimum of 3 elements out of 5, the prevalence of the metabolic syndrome decreasing to 59%. This fact could be attributed to the prevalence decrease with more than 10% in men.
At the end of the study, in T3, our results show a prevalence of 63.2% (74 patients), higher than T2, but lower than T1. Out of the 69 patients who suffered from the syndrome in T2, a total of 11 individuals did not qualify for the condition anymore, while 16 from the 48 cases in the control group continued to present the metabolic criteria. This increase in the total population was due to the rise of the prevalence among the female gender compared to men, 4.6% vs. 3.8%. We also emphasize that the prevalence of the metabolic syndrome among men in T3 was 64%, the exact value of the prevalence among women 12 months prior.
Although these values are similar, we can still report that men have a slightly higher risk of developing the syndrome, numerous other studies, such as SYMFONIE or the SEPHAR study, supporting this claim. [15-16] [18-19] [
25]The data in our paper showcases that the prevalence of the metabolic syndrome among men remained higher along the study, in T3 the discrepancies between genders became almost statistically insignificant.
However, while other papers claim that the prevalence of metabolic syndrome increases in women along with age, reaching a value equal to that of men, if not higher [
14,
17,
22], in our study both genders displayed significant rise in the prevalence along with rising age. The most affected age groups were the 60-69 years old group and the 70-79 years old group, categories where women truly seemed to exhibit an augmented risk. For the rest of the age categories, the incidence and prevalence continued to be higher among men.
Regarding each metabolic factor, central adiposity was the most frequent component, its prevalence decreasing to 52,1% in T2, most probably secondary to the application of measures targeted to weight loss. The fasting glucose presented a similar course, with a decrease of over 9%. Through both pharmaceutical therapies, as well as dietary changes (regular meals, low salt intake, white meat consumption, fresh vegetables and fruits, low consumption of soft drinks), blood pressure was regulated, while the lipidic profile improved. As a result, the prevalence of the other elements decreased with almost 9%, arterial hypertension becoming the most normalized factor, and high fasting glycemia levels were the least frequent (24,7%).
At T3 evaluation, central obesity remained the most prevalent component of the syndrome, with a slight increase of 2%, excepting the prevalence of high blood pressure values that slighly increased with 2% Fasting glucose regained remained the least frequently encountered factor, 25,6%, considering it was the easiest to correct by diet, weight loss and specific treatment. Blood pressure showed a fair reduction, our data reporting a value of 68.9%. As for the lipidic profile, TG increased from 34,18% in T2, to 38,5% in T3 One of the most impressive improvements was the correction of HDL cholesterol values ( from 64,95 at T1 to 42,73% at T3,p˂0,0001).
These findings support preexisting data, all elements pertaining to the metabolic syndrome increasing the risk of significant cardiovascular disease, such as myocardial infarction, as the INTERHEART study emphasizes. [
17]In the ROMES study, however, stable angina was directly associated with the metabolic syndrome in more circumstances thanacute coronary syndromes. [
18]Another study discusses the correlation between the risk of heart failure (HF) and the metabolic syndrome, arguing whether the condition increasing HF risk independently. [
42] As for arrhythmias, such as atrial fibrillation (AF), it is still obscure if the condition is due to the syndrome as a whole, or the risks of its individual elements. [
43]Other works suggest that certain components of the metabolic syndrome, such as high waist circumference,increase the risk of several organ dysfunctions especially in women. [
15,
20,
23,
44]
When we considered the patients’ backgrounds, we concluded that individuals originating from a rural background, as well as the ones with lower level of studies, were more predisposed to developing the metabolic syndrome, as opposed to higher educated people, or the ones living in urban areas. Both education, as well as background, are two important risk factors, discussed in several specialty works, such as the PURE study. [
19,
24,
26] There was a significant variation of more than 20% between lower educated people, and patients with studies of higher levels suffering from the syndrome, whilst a discrepancy of almost 30% could be observed between the rural and urban population. Thus, we can conclude that the incidence and prevalence of the metabolic syndrome varies by socioeconomic position, but more epidemiological studies are needed to further research this theory.
Two major factors influencing the appearance of the metabolic syndrome were smoking and poor dietary habits. 77.5% of smokers suffered from the metabolic syndrome, while non-smokers developed the condition in only 45.9% of cases. An unbalanced diet, with fewer than three meals a day, proved to be an important risk factor, 78% of people with such diets exhibiting symptoms, while59.7% of individuals with regular meals were affected by this condition. A high intake of saturated fats, originating from red meat, and trans fats, mostly found in junk food, increased the risk of developing the syndrome, with exclusive white meat consumption proving to be a protective factor against the condition.
Another protective factor was the intake of fresh vegetables and fruits, even though the difference in the prevalence is almost insignificant. Despite all this evidence, overall meat consumption enhanced the risk of developing the metabolic syndrome, although this fact could be attributed toa higher intake of red meat, compared to white.
Other patterns related to diet, that may increase the risk of metabolic syndrome, are high salt intake and a considerable consumption of carbonated drinks. In 74.4% of cases, patients who consumed augmented quantities of salt per day suffered from the metabolic syndrome, while only 66.6% of the ones presenting low or no intake, or consumed dietary salt, exhibited signs of the condition. Additionally, the prevalence of metabolic syndrome was higher among individuals who regularly consumed soft drinks (73.1% vs. 60%). The EPIC (European Prospective Investigation into Cancer and Nutrition) cohort brings forth evidence that both artificially and sugar-sweetened soft drinks are associated with all-cause mortality. [10, 36]
Thus, diet plays a vital role in the pathophysiology of the metabolic syndrome. There is clear evidence to support that healthy dietary habits, such as the Mediterranean Diet (MedDiet), which not only facilitates weight loss, but also regulatesplasma glucose and LDL and TG levels, decreasing inflammation and blood pressure, further lowers the risk of metabolic syndrome. [27-29][
31]The PREDIMED study supports the inverse association between cardiovascular risk and adherence to the Mediterranean diet. [
30] Other prevention strategies, such as the Dietary Approach to Stop Hypertension (DASH), or country-specific dietary guidelines, such as Healthy Eating Indices (HEI), serve as alternatives to the MedDiet, being consistently associated with a reduced risk of metabolic syndrome. [
28] [32-34]
In this study, alcohol consumption did not count in the risk factor category. The metabolic syndrome was more frequent in individuals who did not consume alcohol at all, compared to the ones who drank moderate quantities (69.2% vs. 66.1%). The type of beverage also seemed to play a key role in this theory, the majority of patients suffering from the metabolic syndrome preferring wine or beer, while a small part consumed solely hard liquors. However, the concept that moderate alcohol consumption is associated with lower cardiovascular risk, is not supported by several works, which suggest that lower risk for cardiovascular disease outcomes can actually be found in abstainers, any amount of alcohol increasing blood pressure and theBMI, thus further increasing the risk for metabolic syndrome overall. [36, 37, 38]
Concerning physical activity, a sedentary lifestyle played a key role in the pathogenesis of the syndrome. Only 53.3% of patients who consistently remained physically active presented the metabolic syndrome, compared to 76.3% of sedentary individuals. Physical activity should be prescribed and tailored to each individual, according to the guidelines, sports engagement being associated with favourable metabolic health results in numerous studies, while sedentary behaviour is associated with a greater risk for cardiovascular disease. [
36] [39-41]
Another important observation of the study was that obese patients who practice regular physical exercises were less likely to develop diabetes, a fact already known and proven once again by the results of our study.
5. Conclusions
The study confirms that gender and age play significant roles in the prevalence of metabolic syndrome. Men generally have a higher risk compares to women, but both genders exhibit an increased risk with advancing age. Healthcare practitioners should consider these factors when designing preventive strategies and interventions.
The impact of socioeconomic factors, such as education level and background, on the development of metabolic syndrome is highlighted. Individuals with lower education levels and those from rural backgrounds are more susceptible to the condition. Poor lifestyle choices, including smoking, harmful dietary habits, and sedentary behaviour, are major risk factors for metabolic syndrome and require targeted interventions.
The results emphasize the critical role of diet in metabolic syndrome development. A diet rich in saturated and trans fats, low in fresh fruits and vegetables, and high in salt and carbonated drinks significantly increases the risk. Encouraging individuals to adopt and maintain healthier dietary patterns, such as the MedDiet, DASH, or country-specific dietary guidelines, can help in preventing and managing metabolic syndrome.
Regular physical activity remains a key protective factor against metabolic syndrome. Sedentary behaviour is strongly associated with an increased risk, while engaging in regular exercise and moderate-intensity activities can help reduce the likelihood of developing the condition.
The study underscores the importance of early detection and intervention in managing the metabolic syndrome and its associated cardiovascular complications. Implementing lifestyle modifications, such as weight loss, proper nutrition, and increased physical activity, can significantly reduce the risk of metabolic syndrome, and improve overall cardiovascular health.
Healthcare professionals should tailor preventive strategies based on individual risk profiles, considering factors such as age, gender, socioeconomic status, and lifestyle choices. Personalized interventions are essential in addressing the diverse factors contributing to the metabolic syndrome.
The results emphasize the need for further research in understanding the metabolic syndrome and its risk factors. Additionally, public health initiatives should focus on raising awareness about metabolic syndrome, its consequences, and the benefits of adopting a healthy lifestyle to prevent its occurrence.
References
- Mahmood, S.S.; Levy, D.; Vasan, R.S.; Wang, T.J. The Framingham Heart Study and the epidemiology of cardiovascular disease: A historical perspective. Lancet 2014, 383, 999–1008. [Google Scholar] [CrossRef]
- Jurcut, R. Factorii de risccardiovasculari. In Mic Tratat de Cardiologie, 2nd ed.; Ginghina, C., Ed.; Editura Academiei: Bucuresti, Romania, 2017; pp. 175–189. [Google Scholar]
- Ford, E.S. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care 2005, 28, 2745–2749. [Google Scholar] [CrossRef]
- Lakka, H.-M. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002, 288, 2709. [Google Scholar] [CrossRef]
- Hanson, R.L.; Imperatore, G.; Bennett, P.H.; Knowler, W.C. Components of the “metabolic syndrome” and incidence of type 2 diabetes. Diabetes 2002, 51, 3120–3127. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA J. Am. Med. Assoc. 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Hwang, I.-C.; Kim, K.-K.; Jee, S.-H.; Kang, H.-C. Comparison of predictability of cardiovascular events between each metabolic component in patients with metabolic syndrome based on the revised National Cholesterol Education Program Criteria. Yonsei Med. J. 2011, 52, 220. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C.J. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Forceon Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heartfederation; International Atherosclerosis Society; and International Association for the Study of Obesity. Obes. Metab. 2010, 7, 63–65. [Google Scholar]
- Enzi, G.; Gasparo, M.; Biondetti, P.; Fiore, D.; Semisa, M.; Zurlo, F. Subcutaneous and visceral fat distribution according to sex, age, and overweight, evaluated by computed tomography. Am. J. Clin. Nutr. 1986, 44, 739–746. [Google Scholar] [CrossRef]
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Yamagishi, K.; Iso, H. The criteria for metabolic syndrome and the National Health Screening and education system in Japan. Epidemiol. Health 2017, 39, e2017003. [Google Scholar] [CrossRef]
- Scuteri, A.; Laurent, S.; Cucca, F.; Cockcroft, J.; Cunha, P.G.; Mañas, L.R.; Raso, F.U.; Muiesan, M.L.; Ryliškytė, L.; Rietzschel, E.; et al. Metabolic syndrome across Europe: Different clusters of risk factors. Eur. J. Prev. Cardiol. 2014, 22, 486–491. [Google Scholar] [CrossRef]
- Pucci, G.; Alcidi, R.; Tap, L.; Battista, F.; Mattace-Raso, F.; Schillaci, G. Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in Metabolic syndrome: A review of the literature. Pharmacol. Res. 2017, 120, 34–42. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Lehmkuhl, E.; Mahmoodzadeh, S. Gender aspects of the role of the metabolic syndrome as a risk factor for cardiovascular disease. Gender Med. 2007, 4, S162–S177. [Google Scholar] [CrossRef]
- Pannier, B.; Thomas, F.; Eschwège, E.; Bean, K.; Benetos, A.; Leocmach, Y.; Danchin, N.; Guize, L. Cardiovascular risk markers associated with the metabolic syndrome in a large French population: The symfonie study. Diabetes Amp Metab. 2006, 32, 467–474. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the Interheart Study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Matei, C.; Pop, I.; Jurcut, R.; et al. ROmanianmulticentric study of the prevalence of metabolic syndrome--ROMES. Hellenic J Cardiol. 2008, 49, 303–309. [Google Scholar]
- Walli-Attaei, M.; Joseph, P.; Rosengren, A.; Chow, C.K.; Rangarajan, S.; Lear, S.A.; AlHabib, K.F.; Davletov, K.; Dans, A.; Lanas, F.; et al. Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (pure): A prospective cohort study. Lancet 2020, 396, 97–109. [Google Scholar] [CrossRef]
- Beltrán-Sánchez, H.; Harhay, M.O.; Harhay, M.M.; McElligott, S. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999–2010. J. Am. Coll. Cardiol. 2013, 62, 697–703. [Google Scholar] [CrossRef]
- Rapsomaniki, E.; Timmis, A.; George, J.; Pujades-Rodriguez, M.; Shah, A.D.; Denaxas, S.; White, I.R.; Caulfield, M.J.; Deanfield, J.E.; Smeeth, L.; et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, Healthy Life-years lost, and age-specific associations in 1·25 million people. Lancet 2014, 383, 1899–1911. [Google Scholar] [CrossRef]
- Hiramatsu, Y.; Ide, H.; Furui, Y. Differences in the components of metabolic syndrome by age and sex: A cross-sectional and longitudinal analysis of a cohort of middle-aged and older Japanese adults. BMC Geriatr. 2023, 23, 438. [Google Scholar] [CrossRef] [PubMed]
- Ramezankhani, A.; Azizi, F.; Hadaegh, F. Gender differences in changes in metabolic syndrome status and its components and risk of cardiovascular disease: A longitudinal cohort study. Cardiovasc. Diabetol. 2022, 21, 227. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.-F.; Yeh, Y.-P.; Hsiu-Hsi Chen, T.; Luh, D.-L. Sex differences in the change of exercise behavior leading to incident metabolic syndrome reduction: A community-based prospective study. Prev. Med. Rep. 2023, 31, 102076. [Google Scholar] [CrossRef] [PubMed]
- Dorobantu, M.; Darabont, R.O.; Badila, E.; Ghiorghe, S. Prevalence, awareness, treatment, and control of hypertension in Romania: Results of the SEPHAR study. Int. J. Hypertens. 2010, 2010, 1–6. [Google Scholar] [CrossRef]
- Hoveling, L.A.; Liefbroer, A.C.; Bültmann, U.; Smidt, N. Understanding socioeconomic differences in incident metabolic syndrome among adults: What is the mediating role of health behaviours? Prev. Med. 2021, 148, 106537. [Google Scholar] [CrossRef]
- Shen, J.; Wilmot, K.A.; Ghasemzadeh, N.; Molloy, D.L.; Burkman, G.; Mekonnen, G.; Gongora, M.C.; Quyyumi, A.A.; Sperling, L.S. Mediterranean dietary patterns and Cardiovascular Health. Annu. Rev. Nutr. 2015, 35, 425–449. [Google Scholar] [CrossRef]
- Farooqui, A.A.; Farooqui, T. Effect of Mediterranean diet components on type 2 diabetes and metabolic syndrome. Role Mediterr. Diet Brain Neurodegener. Dis. 2018, 209–222. [Google Scholar] [CrossRef]
- Harrison, S.; Couture, P.; Lamarche, B. Diet quality, saturated fat and metabolic syndrome. Nutrients 2020, 12, 3232. [Google Scholar] [CrossRef]
- Babio, N.; Toledo, E.; Estruch, R.; Ros, E.; Martínez-González, M.A.; Castañer, O.; Bulló, M.; Corella, D.; Arós, F.; Gómez-Gracia, E.; et al. Mediterranean diets and metabolic syndrome status in the PREDIMED randomized trial. CMAJ 2014, 186, E649–E657. [Google Scholar] [CrossRef]
- Bendall, C.L.; Mayr, H.L.; Opie, R.S.; Bes-Rastrollo, M.; Itsiopoulos, C.; Thomas, C.J. Central obesity and the Mediterranean diet: A systematic review of intervention trials. Crit. Rev. Food Sci. Nutr. 2018, 58, 3070–3084. [Google Scholar] [CrossRef]
- Hu, E.A.; Steffen, L.M.; Coresh, J.; Appel, L.J.; Rebholz, C.M. Adherence to the Healthy Eating Index-2015 and Other Dietary Patterns May Reduce Risk of Cardiovascular Disease, Cardiovascular Mortality, and All-Cause Mortality. J. Nutr. 2020, 150, 312–321. [Google Scholar] [CrossRef]
- Appel, L.J.; Champagne, C.M.; Harsha, D.W.; Cooper, L.S.; Obarzanek, E.; Elmer, P.J.; Stevens, V.J.; Vollmer, W.M.; Lin, P.H.; Svetkey, L.P.; et al. Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. JAMA 2003, 289, 2083–2093. [Google Scholar] [PubMed]
- National Heart Lung and Blood Institute. DASH Eating Plan; National Heart Lung and Blood Institute: Bethesda, MD, USA, 2020. [Google Scholar]
- Rodríguez-Monforte, M.; Sánchez, E.; Barrio, F.; Costa, B.; Flores-Mateo, G. Metabolic syndrome and dietary patterns: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2016, 56, 925–947. [Google Scholar] [CrossRef]
- Mullee, A.; Romaguera, D.; Pearson-Stuttard, J.; Viallon, V.; Stepien, M.; Freisling, H.; Fagherazzi, G.; Mancini, F.R.; Boutron-Ruault, M.C.; et al. Association Between Soft Drink Consumption an d Mortality in 10 European Countries. JAMA Intern. Med. 2019, 179, 14791490. [Google Scholar] [CrossRef] [PubMed]
- Millwood, I.Y.; Walters, R.G.; Mei, X.W.; Guo, Y.; Yang, L.; Bian, Z.; Bennett, D.A.; Chen, Y.; Dong, C.; Hu, R.; et al. China Kadoorie Biobank Collaborative Group. Conventional and genetic evidence on alcohol and vascular disease aetiology: A prospective study of 500 000 men and women in China. Lancet 2019, 393, 18311842. [Google Scholar] [CrossRef]
- Holmes, M.V.; Dale, C.E.; Zuccolo, L.; Silverwood, R.J.; Guo, Y.; Ye, Z.; Prieto-Merino, D.; Dehghan, A.; Trompet, S.; Wong, A.; et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014, 349, g4164. [Google Scholar] [CrossRef] [PubMed]
- Cleven, L.; Dziuba, A.; Krell-Roesch, J.; Schmidt, S.C.; Bös, K.; Jekauc, D.; Woll, A. Longitudinal associations between physical activity and five risk factors of metabolic syndrome in middle-aged adults in Germany. Diabetol. Metab. Syndr. 2023, 15, 82. [Google Scholar] [CrossRef]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. 2018 Physical Activity Guidelines Advisory Committee. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med. Sci. Sports Exerc. 2019, 51, 12701281. [Google Scholar]
- Powell, K.E.; King, A.C.; Buchner, D.M.; Campbell, W.W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J. Phys. Act. Health 2018, 111, 1–11. [Google Scholar] [CrossRef]
- Gargiulo, P.; Marsico, F.; Renga, F.; Dell’Aversana, S.; Esposito, I.; Marciano, C.; Dellegrottaglie, S.; Perrone-Filardi, P.; Paolillo, S. The metabolic syndrome in heart failure: Insights to specific mechanisms. Heart Fail. Rev. 2019, 25, 1–7. [Google Scholar] [CrossRef]
- Georgakopoulos, C.; Vlachopoulos, C.; Lazaros, G.; Tousoulis, D. Biomarkers of atrial fibrillation in metabolic syndrome. Curr. Med. Chem. 2019, 26, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Mendrick, D.L.; Diehl, A.M.; Topor, L.S.; Dietert, R.R.; Will, Y.; La Merrill, M.A.; Bouret, S.; Varma, V.; Hastings, K.L.; Schug, T.T.; Emeigh Hart, S.G.; Burleson, F.G. Metabolic syndrome and associated diseases: From the bench to the clinic. Toxicol. Sci. 2017, 162, 36–42. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).