1. Introduction
Computer-assisted implant surgery was introduced more than 25 years ago with the aim to optimize implant position according to the prosthetic project [
1]. Implant planning supported by cone-beam computed tomography (CBCT) helps preventing intraoperative complications such as mandibular nerve injuries, sinus perforations, fenestrations, or dehiscence [
2]. Guided implantology is made possible using surgical templates that allow implant insertion in the planned position. There are different types of surgical templates, categorized on their stabilization to intraoral structures. Tooth-supported surgical guides are stabilized on remaining teeth, bone-supported guides are anchored to the bone through bone screws or pins, while mucosa-supported templates are positioned on the gingiva [
3]. Stackable guides consist of a fixed base and removable components. This feature simplifies the control of surgical and prosthetic steps. Furthermore, a stackable structure allows to manage hard and soft tissues without remove the fixed base [
4].
An accurate implant placement is crucial in case of immediate loading protocols so that a prefabricated prosthesis can be connected to the implants immediately after the surgery, avoiding intraoperative impressions [
5]. Many errors could lead to deviation added during the computer-aided implant placement sequence. Some of this may arise during the surgery procedure while guide positioning and fixation [
6,
7]. In this regard, stackable surgical guides could aim to improve implant placement and immediate loading accuracy [
8].
One-piece implants combined with a guided insertion show multiple advantages. The absence of internal connection prevents bacterial infiltration and reduces prosthetic complications. Furthermore, a reduction of prosthetic steps is achieved. On the other hand, a precise digital planning, in order to obtain satisfactory primary stability and a correct position of one-piece implants, is mandatory [
9]. In this context, the present case is used to present a newly developed computer-guided protocol characterized by titanium-reinforced stackable surgical guides for one-piece implant placement and subsequent immediate loading.
2. Materials and Methods
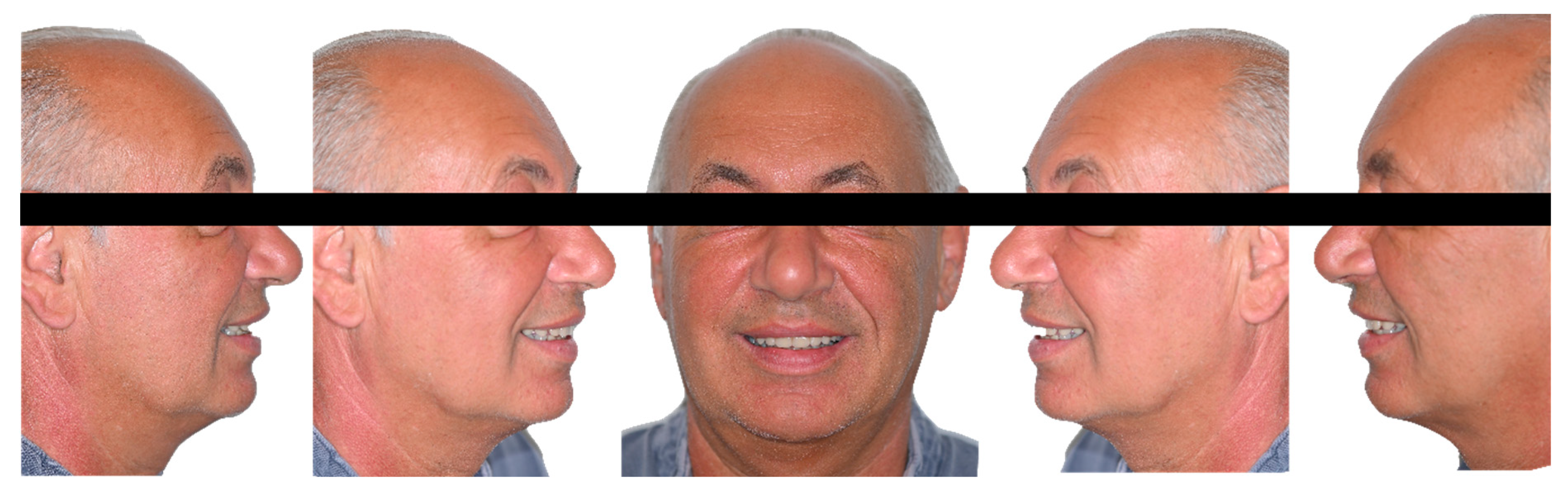
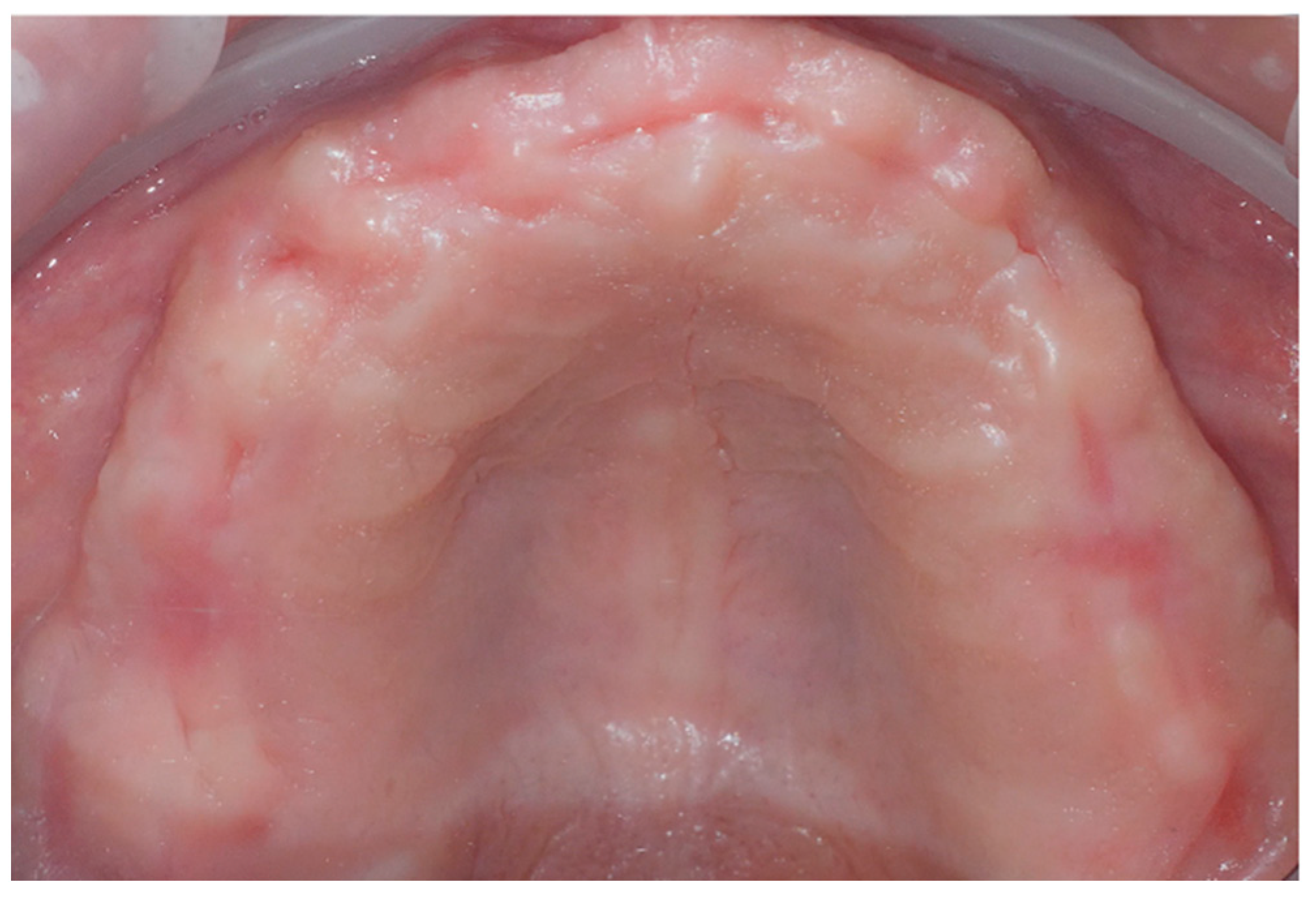
This clinical report is included in an ongoing prospective study conducted in accordance with the ethical principles for medical research involving human subjects outlined in the World Medical Association Declaration of Helsinki as revised in 2008 and was additionally approved by the local ethics committee (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan area 2, registration ID #0002693-U). A 63 years old male patient in good general health (ASA 1) presented with a maxillary complete edentulism rehabilitated with a removable denture (
Figure 1). After discussing the possible therapeutic alternatives with the patient, an implant supported rehabilitation with 6 one-piece implants was proposed. A digital workflow was used to facilitate planning and to accomplish a fully guided implant placement and immediate restoration in a single surgical session. Use of CBCT, photographs, digitalized models, intra-oral scanning, and interactive treatment planning software allowed for accurate surgical planning, fabrication of an innovative design for full-template guidance and management of the provisional milled PMMA (Polymethylmethacrylate) titanium reinforced restoration.
2.1. Surgical planning
Patient presented a correct vertical dimension that was used as a reference during the rehabilitation. Digital 3D scan of the complete removable denture (both the inner and outer parts) worn by the patient and the upper and lower arches was performed. Intraoral and extraoral photographs were taken to create customized virtual diagnostic wax-up designed with dental computer-aided design (CAD) software (exocad DentalCAD, exocad Gmb). (
Figure 1 and
Figure 2).
During the design of the diagnostic waxing, modifications of the complete removable denture were required to achieve optimal esthetic outcomes. A prototype based on the digital waxing was printed allowing an additional intraoral assessment and served as a radiographic stent, being equipped with radiopaque markers (
Figure 3).
CBCT scan was acquired to evaluate the preoperative anatomy of the bone. The standard triangulation language (STL) files obtained from the digital scan were aligned with the digital imaging and communication in medicine (DICOM) data. The superimposition was obtained by means of a best-fit adaptation algorithm that involved matching recognizable surfaces in both STL and DICOM datasets. These markers were recognizable geometric shapes that the software was able to identify in both DICOM and STL files, allowing superimposition of the radiological and digital scans.
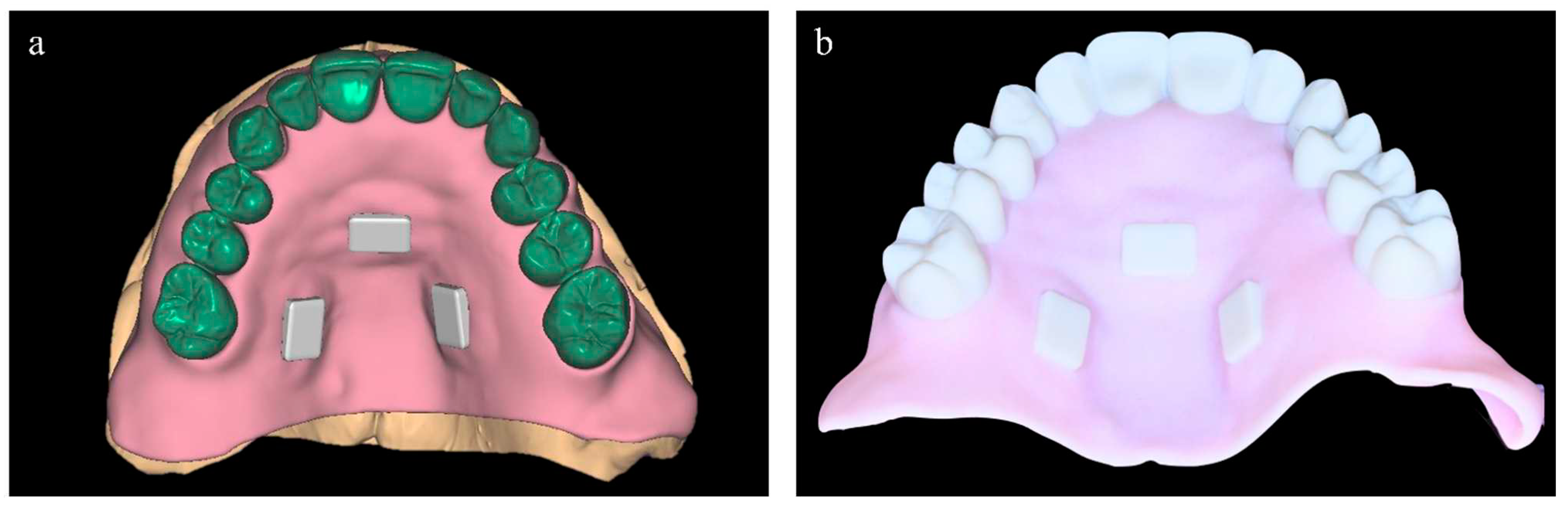
The one-piece implants ideal position was determined by a virtual planning performed by a dedicated software (RealGuide; 3DIEMME, Como, Italy) with the aid of a digital wax-up to perform a prosthetically guided implant placement (
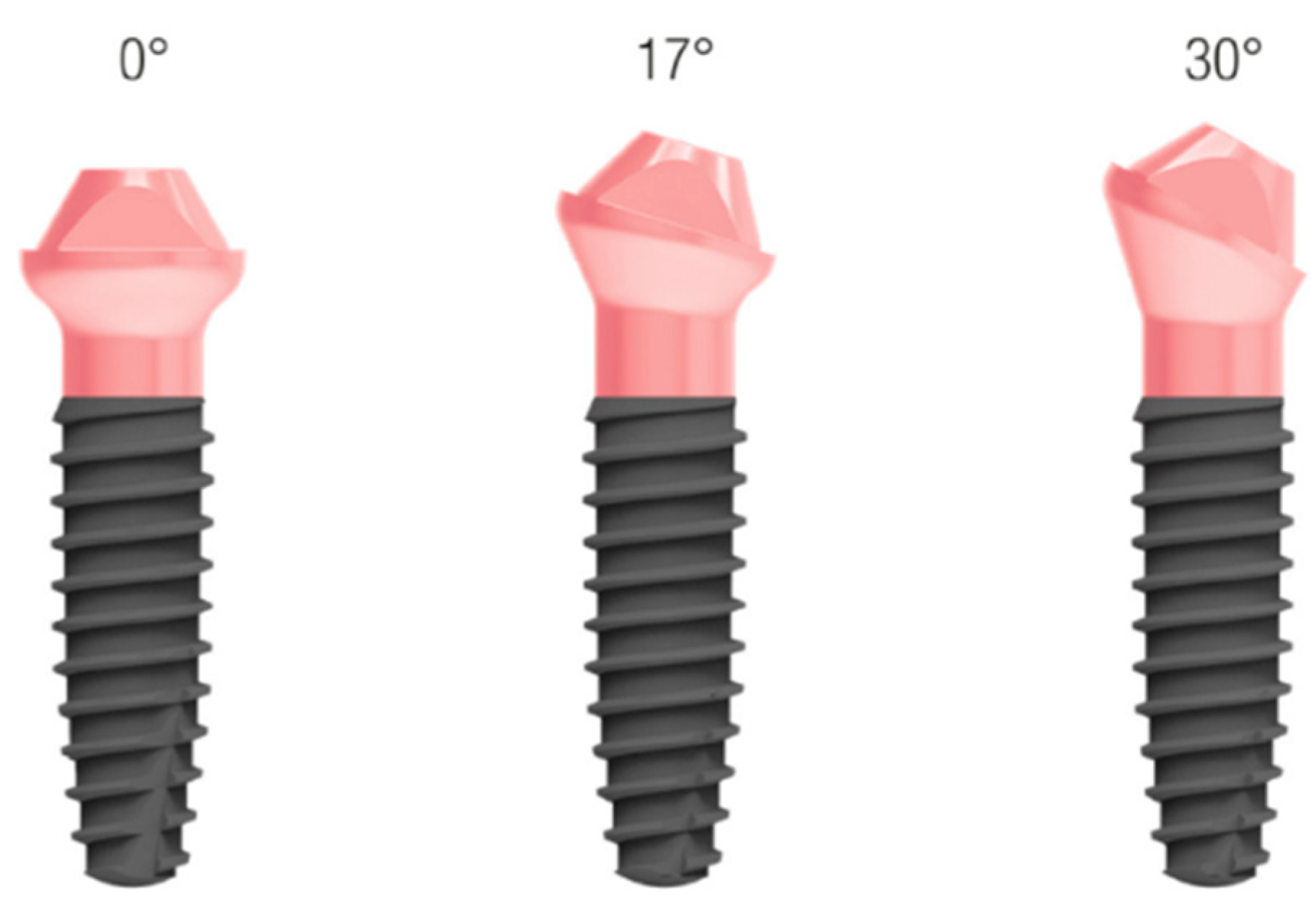
Figure 4). Six pre-angulated one-piece implants (FIXO; Oxy Implant Dental System, Biomec, Colico, Italy) were planned in the maxilla (
Figure 5):
16: Oxy Implant FIXO Short 30° 4x10 mm
14: Oxy Implant FIXO Short 17° 4x10 mm
12: Oxy Implant FIXO Mini 17° 3.5x11,5 mm
22: Oxy Implant FIXO Mini 17° 3,5x13 mm
24: Oxy Implant FIXO Short 17° 4x11,5 mm
26: Oxy Implant FIXO Short 17° 4x8,5 mm
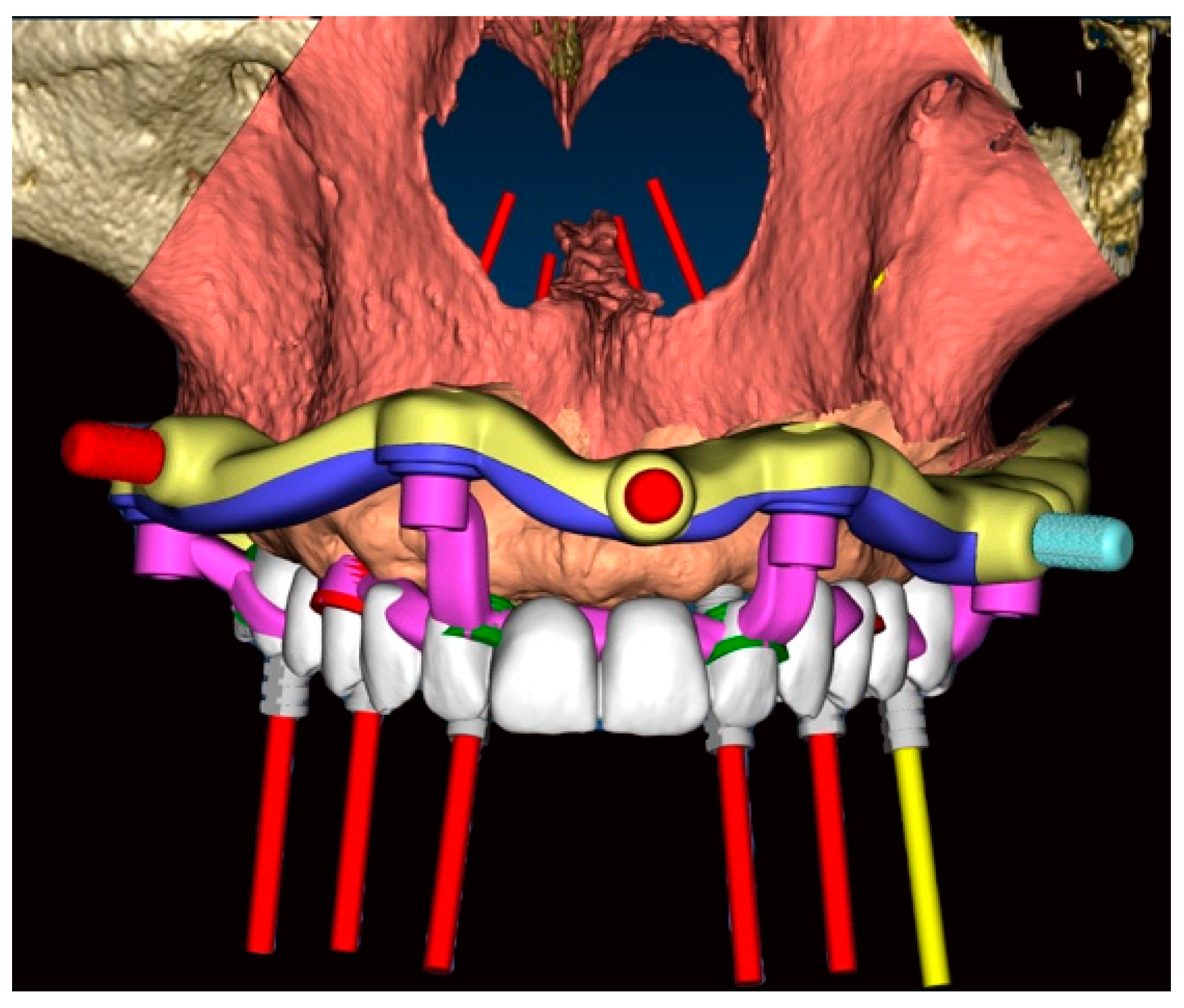
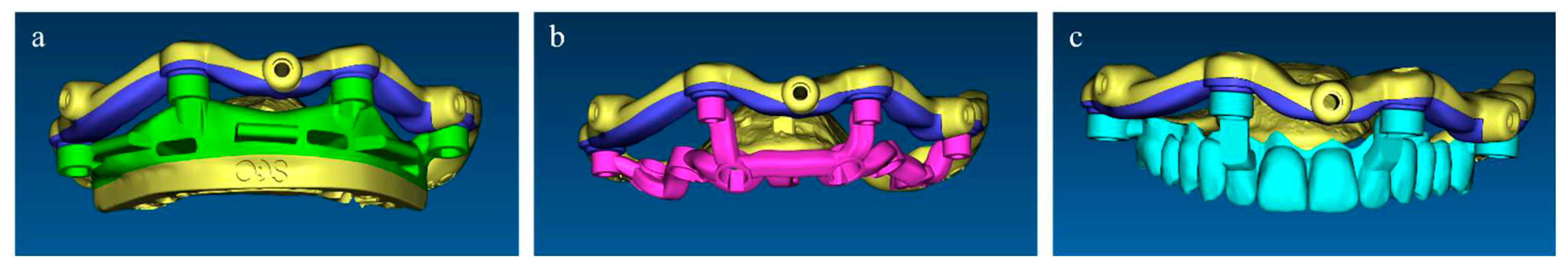
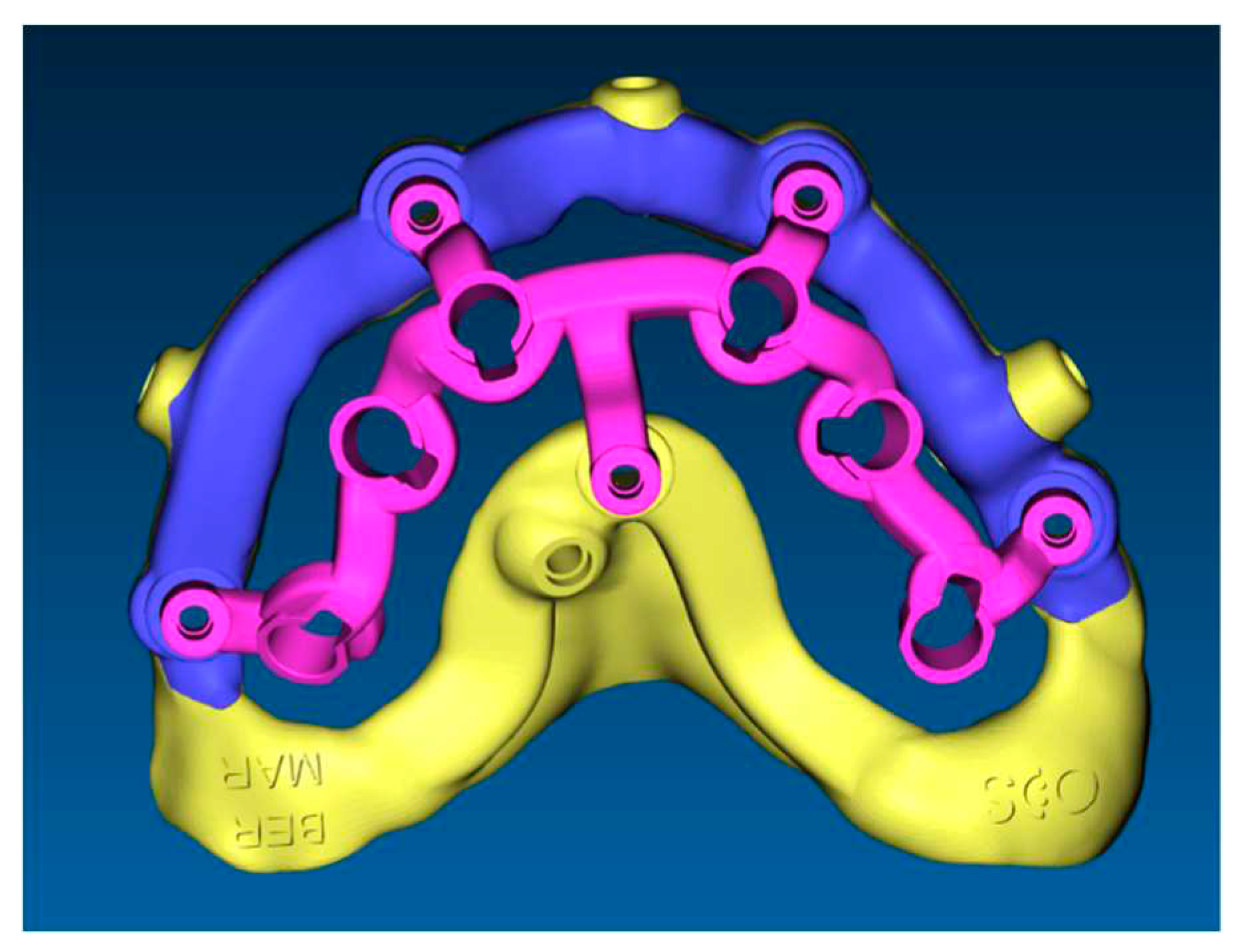
The stackable guide (
Figure 6), fabricated on the basis of the position of the implants in the digital project, was characterized by the following components:
Fixed component or Base Template: printed resin (Clear MED610TM; Stratasys, US) reinforced with milled titanium grade 5 (SINERGIA DISK Ti; Nobil Metal, Bergamo, Italy).
-
Removable components, screwed to the Base Template, consisting of:
Positioning template: printed resin (Clear MED610TM; Stratasys, US)
Implant placement template (
Figure 7): milled titanium grade 5 (SINERGIA DISK Ti; Nobil Metal, Bergamo, Italy)
Provisional Prosthesis: milled PMMA (Multilayer PMMA Disc; Dentsply Sirona, Verona, Italy) and milled titanium grade 5 core (SINERGIA DISK Ti; Nobil Metal, Bergamo, Italy)
A specific miller (XD182; Faimond, Vicenza, Italy) was used for titanium and PMMA in the base template, implant placement template and provisional prosthesis. 3D Printer (J5 DentaJet; Stratasys, US) was used for printed resin in base template and positioning template.
2.2. Surgery
The base template connected with screws to the mucosa-supported positioning template was placed in the oral cavity. The proper seating of the mucosa-supported template was achieved through the occlusion with the teeth of the opposite arch (
Figure 4). After proper seating of the positioning stent, verified by inspection holes, the connected base template was stabilized by means of screwed anchor pins to the bone buccally and palatally. The mucosa-supported positioning template was removed, while the base template anchored to the bone was left in place until the procedure was completed. In order to preserve the width of the keratinized gingiva, elevation of a mucoperiosteal flap was performed. (
Figure 8).
The implant stent, completely made of milled titanium grade 5, was then screwed to the base template and computer-guided insertion of one-piece implants (FIXO; Oxy Implant Dental System, Biomec, Colico, Italy) was performed. In the posterior regions, to avoid grafting procedures, tilted implants at 17° or 30° were placed. In order to obtain the correct position, one-piece implants were inserted in the bone with an appropriate implant mounter. This specific mounter is able to compensate for implant angulation during insertion. To verify the correct position of inserted implant, this specific mounter presented a notch that had to match with the corresponding notch positioned in the surgical template sleeve as planned (
Figure 7). Once the two notches matched, the implants were properly seated, and both the implant mounters and the implant template were unscrewed from the base template. All implants were positioned with an insertion torque ≥ 35 ncm. 6/0 polyglycolic acid sutures were used.
2.3. Prosthetic Restoration
The provisional abutments of correct height, as set according to the virtual waxing, were connected to the fixtures. The interim prosthesis was screwed to the base template. Such prosthesis was made of PMMA reinforced with a metal framework, designed and fabricated according to the diagnostic waxing. The interim prosthesis was relined intraorally to the provisional abutments with a self-polymerizing composite resin (RelyX Ultimate; 3M Italia, Milano, Italy) (
Figure 8).
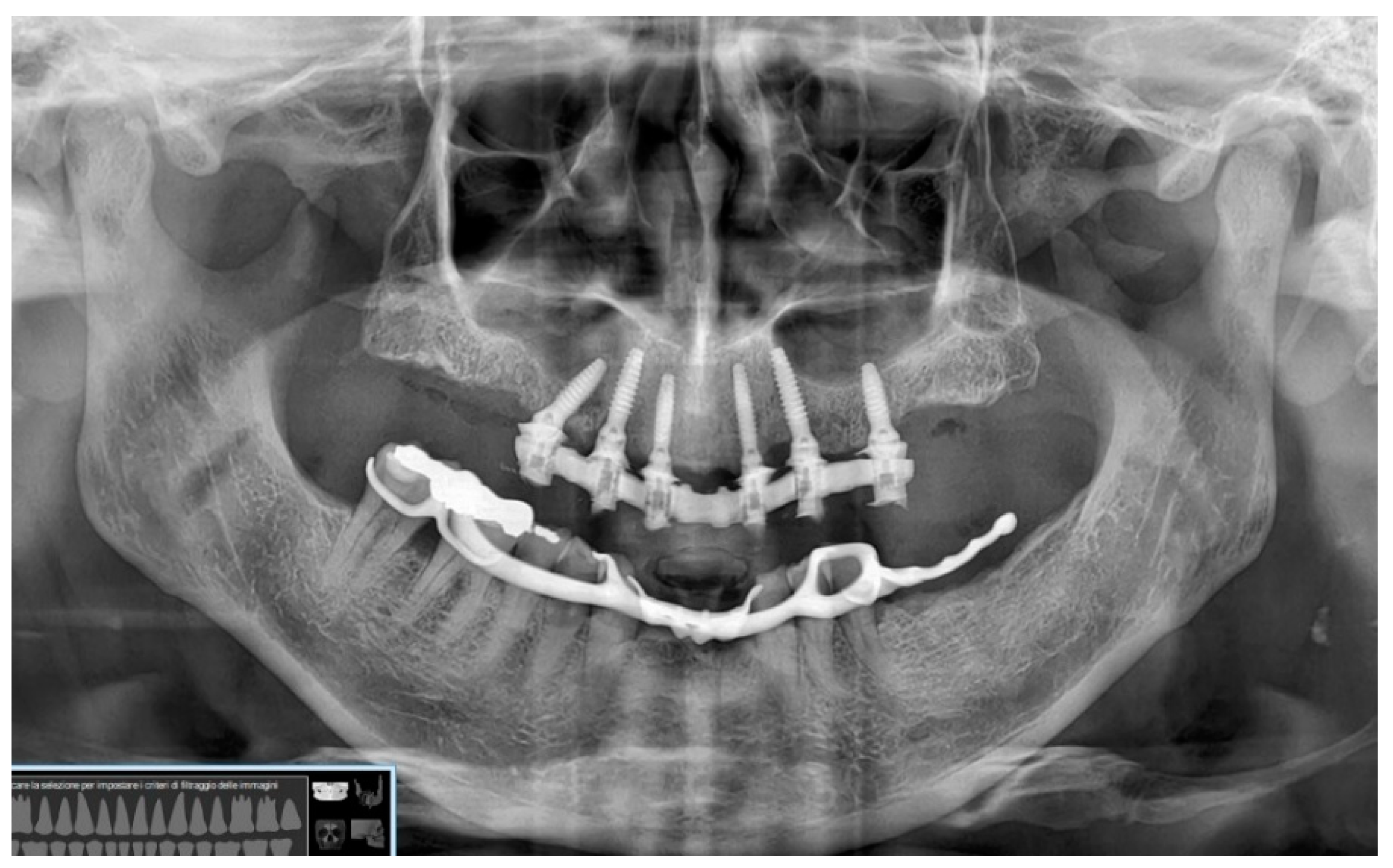
After extraoral prosthetic adjustments and polishing, the access holes to the prosthetic screws of the interim abutments were closed with a photopolymerizable nano-hybrid composite (Tetric EvoFlow; Ivoclar Vivadent, Bolzano, Italy). Occlusal check refinements were done to achieve proper distribution of mastication forces. Post-surgery orthopantomografy was performed for radiological assessment (
Figure 9).
3. Discussion
The purpose of the present technical note was to introduce an innovative approach in computer-guided implantology consisting of stackable templates sequentially used to improve the predictability of the workflow in combination with one-piece implants. In this respect, accuracy of guided surgery plays a crucial role. Different surgical guides have been developed depending on the supporting tissue, generally bone, mucosa, or residual teeth. Dental and mucosal-supported guides are more precise than bone-supported stents because inaccuracies in the 3D examination and segmentation or irregular bone anatomy can significantly alter the position of the latter and therefore the precision of implant placement [
3,
10,
11].
Conventional protocols involve the use of an initial tooth- or mucosa-supported guide that is preliminarily used to create the holes for the bone pins. The stent is then removed, remaining teeth are eventually extracted, and a second implant template is stabilized with fixation pins inserted into the holes made with the previous guide [
5]. Sequential removal and insertion of pins may lead to variations in the holes direction due to the elastic rebound of the bone. This fact can dislocate the surgical stents, which may assume a position different from that planned, leading to linear and angular deviations [
12]. To overcome such a drawback, the above-described method contemplated the fixation of a base template that was left in situ during the entire procedure. In this way, errors in repositioning the subsequent templates were minimized. Furthermore, in this protocol pins were replaced by a new version of screwed pins, improving the stability of the system. These pins presented a 1.5 mm thread in the terminal portion, allowing proper adaptation of the base template to the underneath tissues. It should also be noted that a fixed reference helps the operator to switch the templates rapidly, so that surgical and prosthetic times are reduced.
The material used to fabricate the stackable templates in this protocol is another aspect to be considered. Conventional PMMA guides may suffer deformation or fracture during implant site preparation. To solve this issue, the base template was reinforced with titanium while full titanium for the implant insertion guide (
Figure 6). Titanium enhances stiffness to reduce the risk of deformation and fracture during the drilling sequence.
Another limitation of conventional protocols using closed stents is the inability to cool properly the drills with saline while preparing the implant site. This can lead to an increase in bone temperature with potential impairment of the healing process [
13]. This likely results in the formation of scar tissue and consequent fibrointegration of the implant [
14]. Conversely, stackable guides were designed open, allowing direct cooling of the drills during implant bed preparation.
The quantity and stability of hard and soft tissues play a key role in the long-term success of the rehabilitation [
15]. In conventional guided implantology, surgical stents often reduce the visibility of the entire surgical field. Moreover, the bulky aspect of traditional stent does not allow the management of the future peri-implant tissues [
16]. In the protocol herein described, the slim and open design of the base template offered an excellent view of the surgical area and allowed the intraoperative management of underneath tissues [
17,
18]. In terms of hard tissue management, one-piece implants did not require the use of a bone profiler, which is normally used to create space for prosthetic components in two-piece fixtures. This resulted in greater bone preservation, also thanks to the reduced thickness of the implant neck made possible by the lack of an internal connection and a prosthetic screw [
9]. In this matter, the absence of an implant-abutment connection also avoids the bacterial infiltration that has been observed in two-piece implants, thereby reducing the likelihood of developing biological complications in the follow-up [
19]. Furthermore, one-piece implants reduce the risk of complications referred to the prosthetic screw. This screw characterized by a diameter of 1.8 mm reduces the risk of fracture. When required, a resective guide could be connected to the base template, allowing guided osteoplasty previously planned in the software according to the digital waxing. Another advantage related to the use of this stackable templates is the possibility to manage soft tissues as well. This aspect was particularly important in those sites characterized by suboptimal soft tissue thickness.
The one-piece implants inserted according to the described protocol achieved a minimum insertion torque of 35 Ncm. In the posterior regions tilted implants at 17° or 30° were placed to avoid grafting procedures. Through digital planning, notches were realized on the surgical guides so that the axis of the abutment corresponded to the axis of interim prosthesis access holes. Concerning prosthetic advantages, the use of stackable components ensured a more precise position of the temporary restoration during the relining procedures. The interim prosthesis was screwed to the base template in order to replicate as more accurately as possible the position of the framework according to the digital project. Intraoperative impressions were avoided, and the positioning of the prosthesis was not solely dependent on the occlusal key. It is also worth noting that the increased level of precision achieved by connecting the provisional restoration to the base template allowed reducing the space between the titanium framework and the temporary abutments. Interestingly, no interferences were observed between the prosthesis and the temporary abutments, demonstrating a good level of correspondence of the position of the implant with respect to the digital project. A limitation may be represented by the operator experience in both planning surgical and prosthetic phases. In addition, the deviation between the planned and achieved implant position remains, currently, an unsolved issue. For this reason, the screwed interim prosthesis placement still remains inaccurate and unpredictable.
4. Conclusions
The use of stackable templates combined with one-piece implants showed excellent optimal aesthetic and functional results in full-arch maxillary computer-guided rehabilitation. Digital planning and the use of stackable templates associated to one-piece implants allowed simplification and acceleration of surgical and prosthetic steps respecting at the same time biological, surgical and prosthetic aspects.
Author Contributions
M.B. and M.M., conceptualization; M.M. and P.P.P., formal analysis; M.M. and P.P.P., investigation and methodology; F.E.S. and M.T., writing original draft; C.M. and P.P.P. writing—review and editing; M.B. and C.M., project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Italian Ministry of Health—current research IRCCS.
Institutional Review Board Statement
The study was conducted in accordance with the fundamental principles of the 1975 Helsinki Declaration on clinical analysis involving human subjects, as revised in 2008, and was additionally approved by the local ethics committee of the Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico (Milan area 2) in relation to digital workflows (#0002693-U). All patients involved in the present study signed an informed consent form for participation.
Informed Consent Statement
Informed consent was obtained from the subject involved in the study.
Data Availability Statement
Data are available in the article itself.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Negreiros WM, Hamilton A, Gallucci GO. A completely digital workflow for the transition from a failed dentition to interim complete-arch fixed implant-supported prostheses: A clinical report. J Prosthet Dent. 2022;127(4):527-32. [CrossRef]
- Verstreken K, Van Cleynenbreugel J, Marchal G, Naert I, Suetens P, van Steenberghe D. Computer-assisted planning of oral implant surgery: a three-dimensional approach. Int J Oral Maxillofac Implants. 1996;11(6):806-10.
- Gargallo-Albiol J, Barootchi S, Salomó-Coll O, Wang HL. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann Anat. 2019;225:1-10. [CrossRef]
- Li J, Chen Z, Chan HL, Sinjab K, Yu H, Wang HL. Does flap opening or not influence the accuracy of semi-guided implant placement in partially edentulous sites? Clin Implant Dent Relat Res. 2019;21(6):1253-61. [CrossRef]
- Lopes A, Maló P, de Araújo Nobre M, Sánchez-Fernández E, Gravito I. The NobelGuide(®) All-on-4(®) Treatment Concept for Rehabilitation of Edentulous Jaws: A Retrospective Report on the 7-Years Clinical and 5-Years Radiographic Outcomes. Clin Implant Dent Relat Res. 2017;19(2):233-44. [CrossRef]
- Beretta M, Poli PP, Maiorana C. Accuracy of computer-aided template-guided oral implant placement: a prospective clinical study. J Periodontal Implant Sci. 2014;44(4):184-93. [CrossRef]
- Eftekhar Ashtiani R, Ghasemi Z, Nami M, Mighani F, Namdari M. Accuracy of static digital surgical guides for dental implants based on the guide system: A systematic review. J Stomatol Oral Maxillofac Surg. 2021;122(6):600-7. [CrossRef]
- García-Sala Bonmati F, Pérez-Barquero JA, Ilzarbe Ripoll LM, Labaig Rueda C, Fernandez-Estevan L, Revilla-León M. An additively manufactured, magnetically retained, and stackable implant surgical guide: A dental technique. J Prosthet Dent. 2022. [CrossRef]
- Beretta M, Manfredini M, Poli PP, Tansella S, Maiorana C. Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up. Prosthesis (Basel, Switzerland). 2022;4(2):202-12. [CrossRef]
- El Kholy K, Lazarin R, Janner SFM, Faerber K, Buser R, Buser D. Influence of surgical guide support and implant site location on accuracy of static Computer-Assisted Implant Surgery. Clin Oral Implants Res. 2019;30(11):1067-75. [CrossRef]
- Chmielewski K, Ryncarz W, Yüksel O, Goncalves P, Baek KW, Cok S, et al. Image analysis of immediate full-arch prosthetic rehabilitations guided by a digital workflow: assessment of the discrepancy between planning and execution. Int J Implant Dent. 2019;5(1):26. [CrossRef]
- Choi K, Kuhn JL, Ciarelli MJ, Goldstein SA. The elastic moduli of human subchondral, trabecular, and cortical bone tissue and the size-dependency of cortical bone modulus. J Biomech. 1990;23(11):1103-13. [CrossRef]
- Boa K, Barrak I, Varga E, Jr., Joob-Fancsaly A, Varga E, Piffko J. Intraosseous generation of heat during guided surgical drilling: an ex vivo study of the effect of the temperature of the irrigating fluid. Br J Oral Maxillofac Surg. 2016;54(8):904-8. [CrossRef]
- Eriksson A, editor Heat-induced bone tissue injury : an in vivo investigation of heat tolerance of bone tissue and temperature rise in the drilling of cortical bone1984.
- Farronato D, Pasini PM, Orsina AA, Manfredini M, Azzi L, Farronato M. Correlation between Buccal Bone Thickness at Implant Placement in Healed Sites and Buccal Soft Tissue Maturation Pattern: A Prospective Three-Year Study. Materials (Basel). 2020;13(3). [CrossRef]
- Liu YF, Wu JL, Zhang JX, Peng W, Liao WQ. Numerical and Experimental Analyses on the Temperature Distribution in the Dental Implant Preparation Area when Using a Surgical Guide. J Prosthodont. 2018;27(1):42-51. [CrossRef]
- Tomasi C, Donati M, Cecchinato D, Szathvary I, Corrà E, Lindhe J. Effect of socket grafting with deproteinized bone mineral: An RCT on dimensional alterations after 6 months. Clin Oral Implants Res. 2018;29(5):435-42. [CrossRef]
- Beretta M, Maiorana C, Manfredini M, Signorino F, Poli PP, Vinci R. Marginal Bone Resorption Around Dental Implants Placed in Alveolar Socket Preserved Sites: A 5 Years Follow-up Study. J Maxillofac Oral Surg. 2021;20(3):381-8. [CrossRef]
- Gamper FB, Benic GI, Sanz-Martin I, Asgeirsson AG, Hämmerle CHF, Thoma DS. Randomized controlled clinical trial comparing one-piece and two-piece dental implants supporting fixed and removable dental prostheses: 4- to 6-year observations. Clin Oral Implants Res. 2017;28(12):1553-9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).