1. Introduction
In health at a glance 2021, the Organization for Economic Cooperation and Development (OECD) lists life expectancy at birth(LEB) and avoidable mortality as part of the population health system performance indicators for health status [
1].
LEB is a key measure of population health and is often used to evaluate health system performance [
2]. Globally, LEB is continuously increasing, including in Korea. Although LEB indicates the average length of length, it fails to provide any insight into the range of life expectancies. In practice, it has the limitation of not reflecting the differences in LEB between subgroups of the population. Therefore, to fully understand the health of a population, it is important to understand the contribution of subgroups of the population to LEB [
3].
The main goal of a healthcare system is to improve overall health and ensure an equitable distribution of health outcomes across different subgroups. In this regard, gender health inequalities are of considerable importance as they reflect distinctions in social framework, including political and economic establishments and health and social policies [
4]. According to WHO statistics, the gap in LEB between males and females is significant, with females living an average of 5.1 years longer than males globally in 2019 [
5]. The gender gap in LEB may be explainable by biological, behavioral, and social-economic factors [
6,
7]. Given that health systems can enhance the longevity and population health by ensuring timely access to affordable and high-quality healthcare [
9] it is also possible that public health policies and access to quality health care have contributed to the gender gap in LEB because it has been differentially distributed to males and females [
10]. It is therefore important to examine the extent to which health policies and quality of healthcare contribute to the distribution of health outcomes across sociodemographic groups, including males and females.
Avoidable mortality refers to an unnecessary premature death that could be preventable by timely and suitable interventions and effective healthcare policy. It has long been recognized as an indicator of healthcare system performance [
11]. Avoidable mortality can be divided into two distinct categories: preventable and treatable. Preventable mortality is the deaths that can be preventable through appropriate primary healthcare interventions or public health programs. Treatable mortality is defined as deaths that can be avoided through timely and effective medical interventions at the secondary and tertiary healthcare levels [
11]. In South Korea, avoidable mortality continues to decline due to efficient healthcare policies [
12]. South Korea's avoidable mortality rate in 2018 was 144.0 deaths per 100,000 population, which is lower than the OECD average (199.7) and has decreased significantly over 18 years compared to 2000 (344) [
12]. Currently, various health policies are being identified and tried to further reduce avoidable mortality. To do so, it is necessary to understand the impact of different potentially avoidable causes of death on LEB.
Several studies have examined the impact of avoidable mortality on LEB. Avoidable mortality was first applied to population-level studies by Charlton, J et al [
13]. They selected 14 disease groups to identify regional variation in avoidable mortality in England and Wales and found that regional variation in avoidable mortality resulted in significant variation in the quality of healthcare [
13]. The first study to examine trends in avoidable mortality in Korea found that avoidable mortality declined significantly between 1982-1991 (37.4% in 1982 and 24.9% in 1991), especially among males, and cited acute respiratory diseases, malnutrition, pneumonia, and influenza as the leading causes. A follow-up to that study suggested that the reduction in avoidable mortality resulted in improved LEB [
14]. Bahk, J et al. used the UK Office for National Statistics' cause of death list to assess the impact of avoidable mortality on LEB growth from 1998-2017 [
15]. They found that changes in avoidable causes of death contributed more than 50% to the increase in LEB, and that avoidable causes of death such as cerebrovascular disease and traffic accidents were the main causes of the increase in LEB [
15].
This study aims to identify the contribution of age and gender to the change in LEB in Korea over the past two decades and to analyze the impact of avoidable mortality on LEB. The results would provide insights into the causes of the increase in LEB in Korea.
4. Discussion
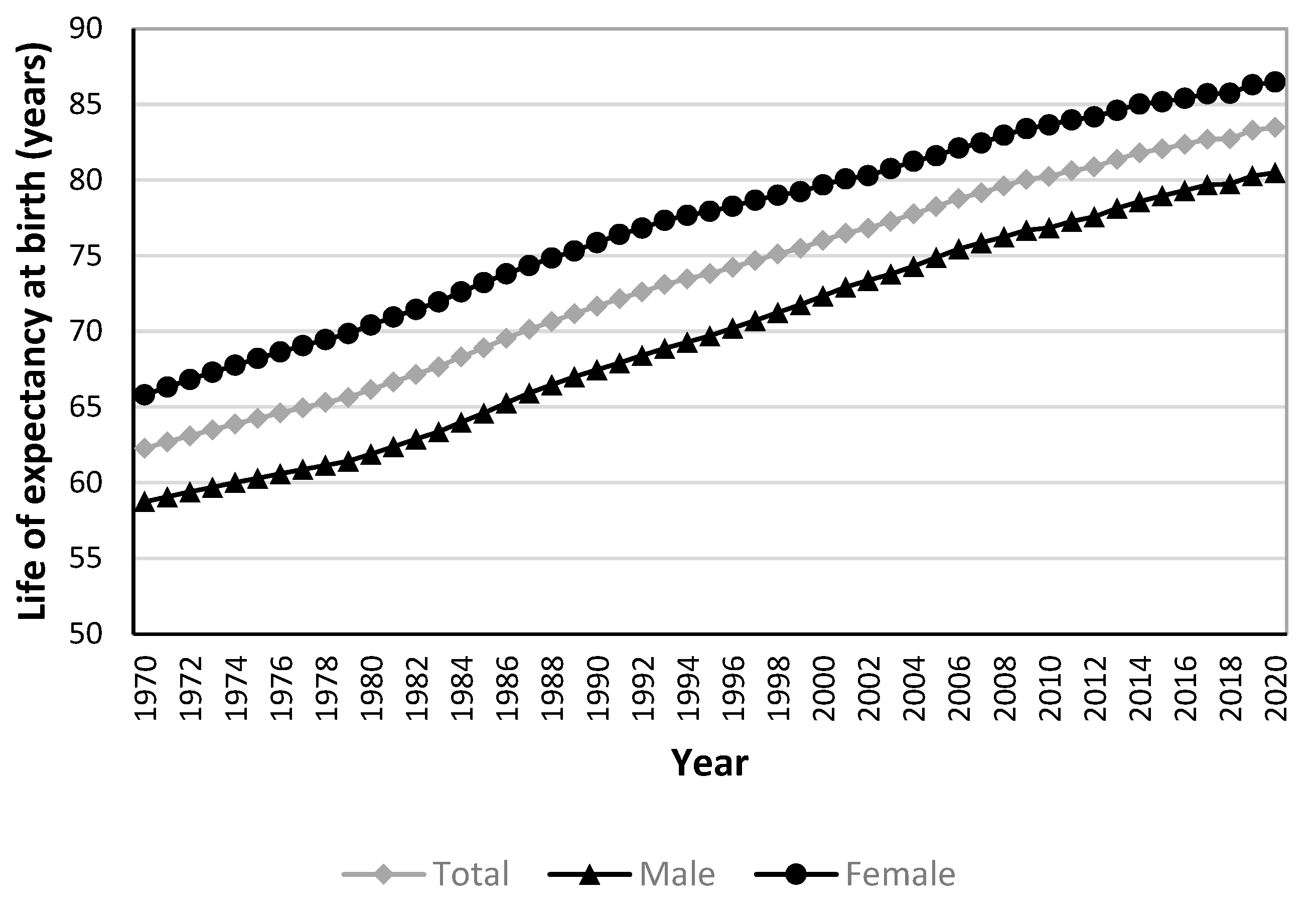
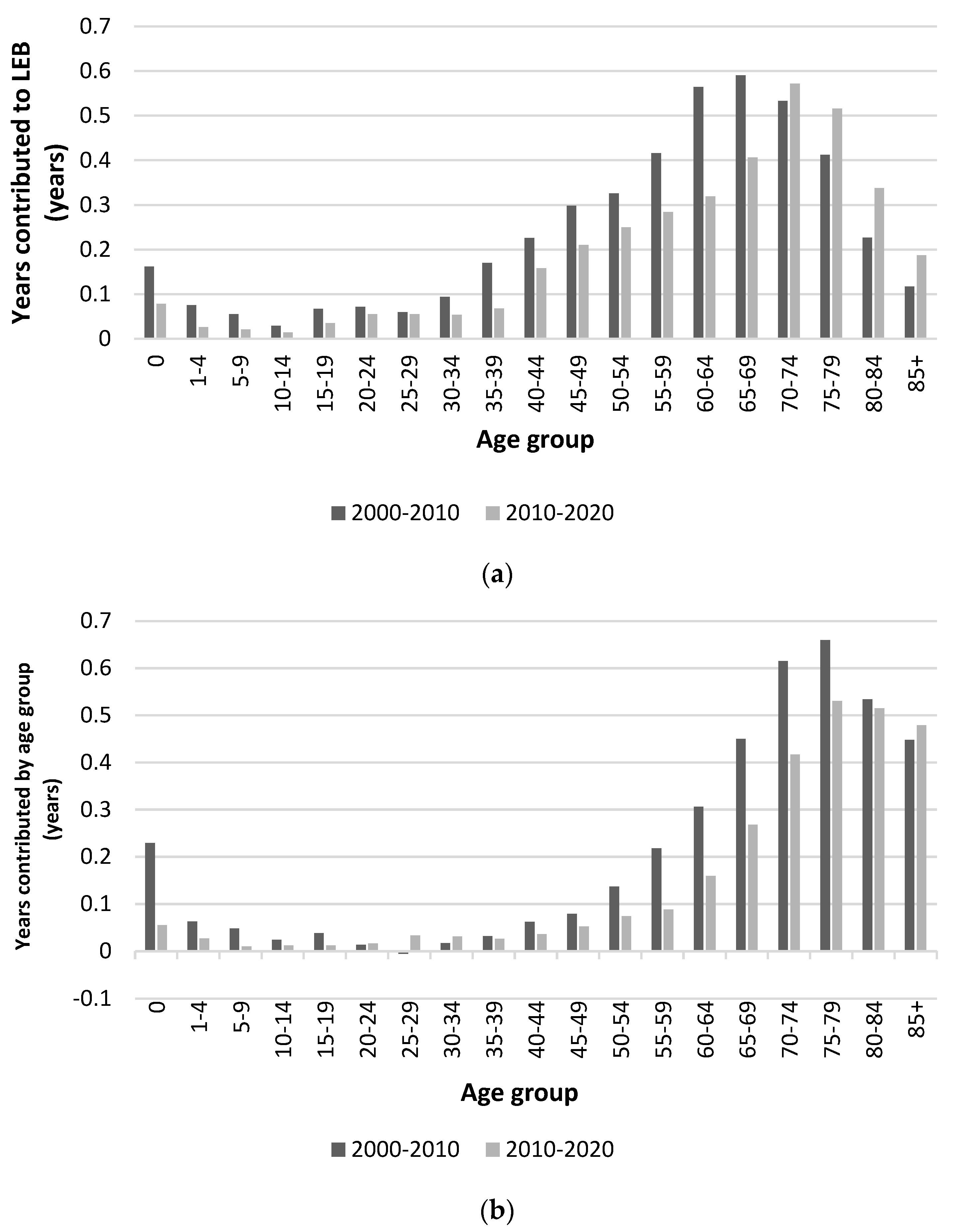
This study analyzed the contribution of differences and changes in mortality by age, gender, and avoidable causes to LEB over the period 2000-2020.
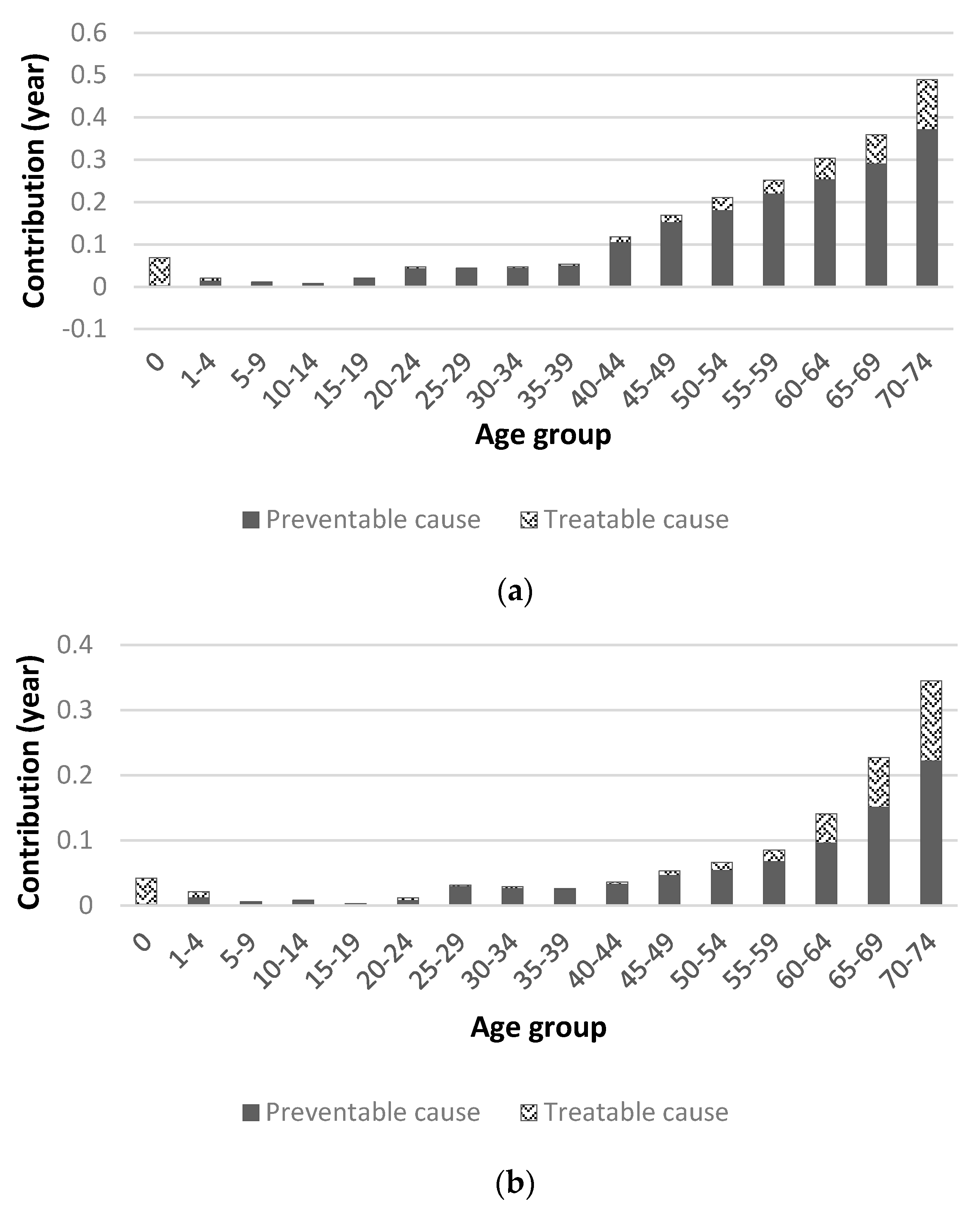
From 2000 to 2020, LEB increased more for males (8.142 years) than for females (6.806 years). The contribution of those aged 65 and older was 45.44% (3.70 years) for males and 71.01% (4.83 years) for females, indicating that a large proportion of the increase in LEB was due to changes in mortality in the 65 and older age group. From this, it can be concluded that the 65+ age group contributed the most to the increase in LEB in Korea since 2000, especially in the 70-74 age group for males and 75-79 age group for females.
In recent years, the contribution of the younger age groups to the increase in LEB has been declining, while the contribution of the middle-aged and older age groups has been increasing. This is consistent with a study that found that changes in mortality at age 65 and older had the largest impact on LEB between 2000-2013 [
19], and the previous study that found that the most significant contribution to LEB gains over the 30-year period from 1985-2015 was at ages 55-64 for males and 65-74 for females [
19]. It is also consistent with findings in Germany that the largest contribution to LEB over 40 years was made by those aged 65 and older (2.9 years for males and 4.0 years for females) [
20] and in Sweden that the largest contribution was made by those aged 65 and older (2.3 years for males and 1.37 years for females) between 1997-2014 [
21].
The gender gap in LEB at each period was highest for those aged 60-64 in 2000 (0.959 years), 70-74 in 2010 (0.952 years), and 75-79 in 2020 (0.862 years). In 2000 and 2010, the gender gap in LEB was highest at ages 65-74 and decreased thereafter, while in 2020, the gender gap in LEB increased until ages 75-84. The gender gap in LEB shifts to older age group, which is consistent with previous studies [
19].
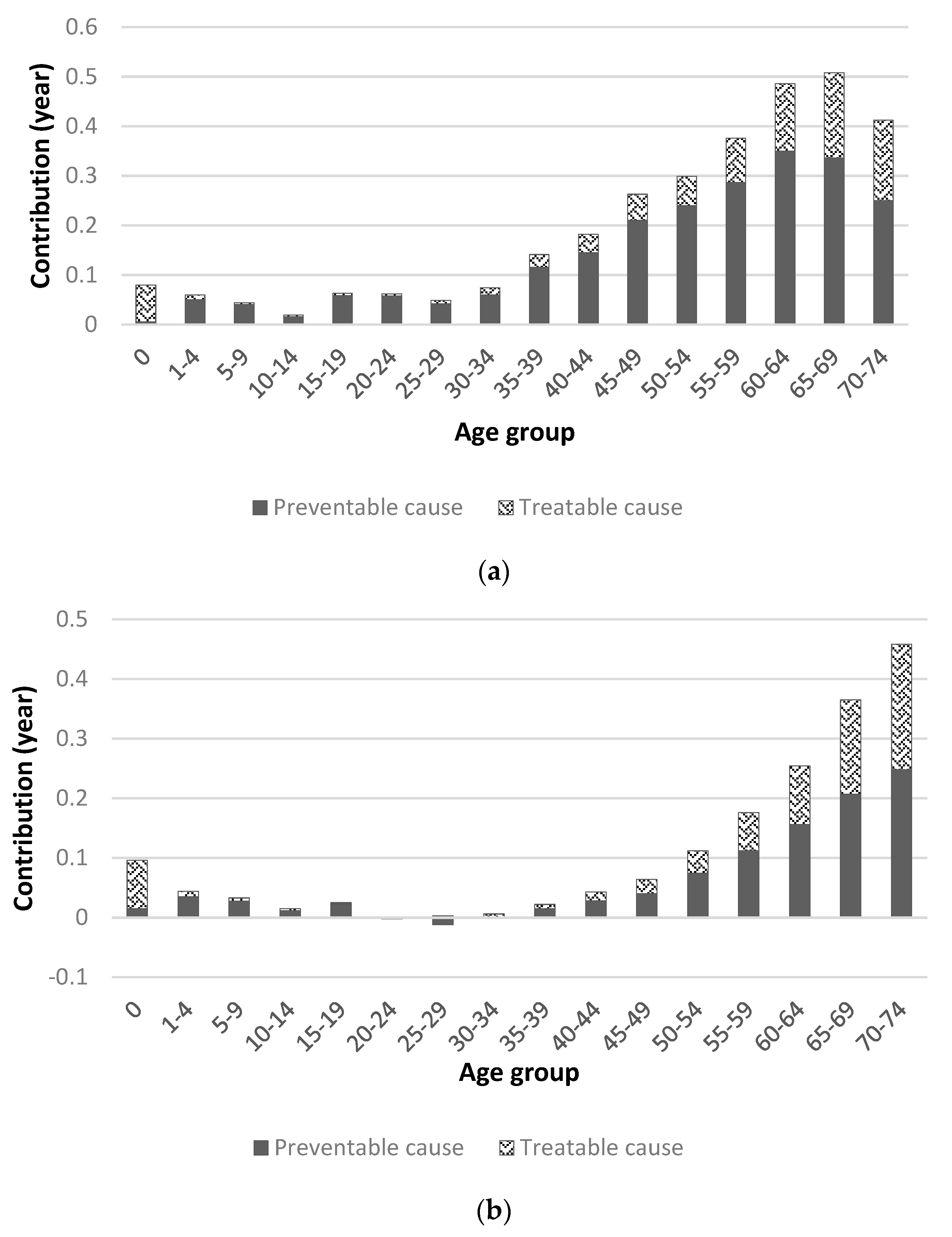
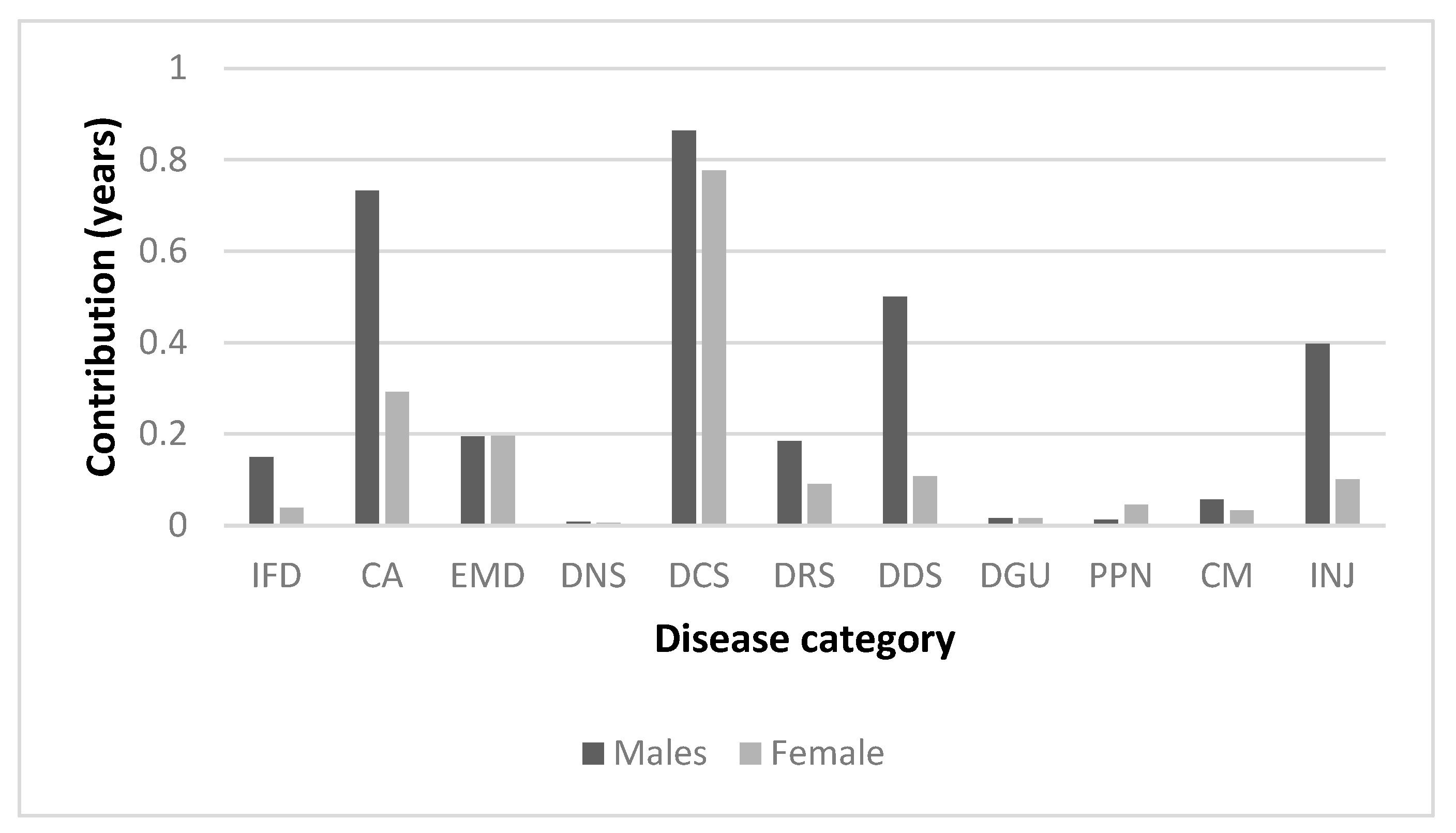
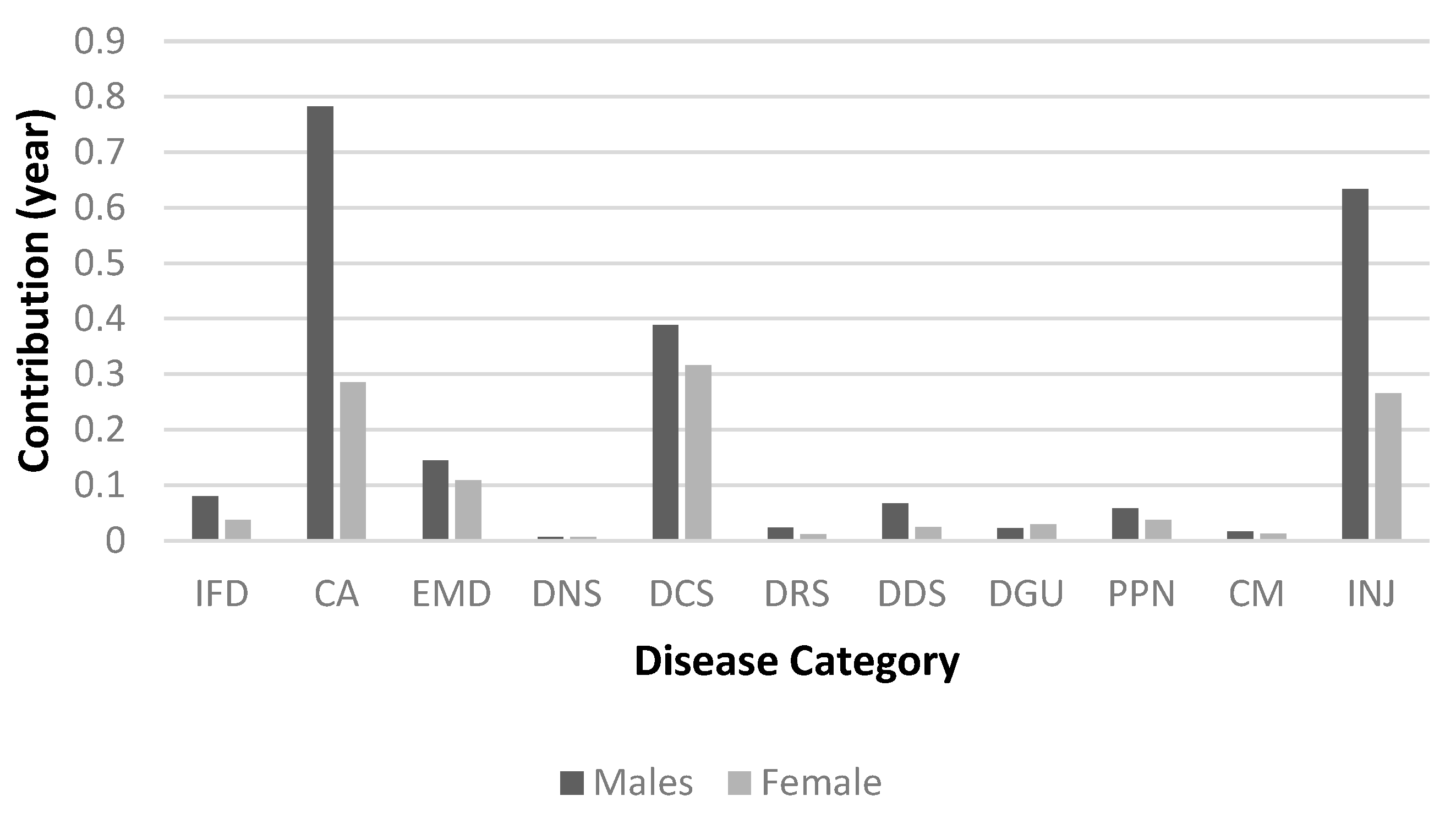
The contribution of avoidable mortality to LEB from 2000 to 2020 is 57.3% (4.285 years), which is not directly comparable to other studies due to the different list of avoidable causes of death and study period. The increase in LEB due to avoidable mortality is higher for males (5.338 years) compared to females (2.833 years), which can be explained by the increase in LEB being higher for males (8.142 years) compared to females (6.806 years). The age-specific contribution of avoidable mortality is higher in the 65+ age group, which is likely due to the higher contribution of LEB gains in the 65+ age group.
In this study, the contribution to LEB gains was higher for avoidable mortality than for treatable mortality for both males and females, which is consistent with previous studies [
14]. This suggests that preventable mortality needs to be further reduced. There was also a higher contribution from preventable mortality in males compared to females, which was likely due to liver disease (cirrhosis and fibrosis), stomach cancer and lung cancer. These causes of death are associated with higher mortality rates in males than in females and are thought to be caused by alcohol consumption and smoking habits, which contribute to liver disease (cirrhosis and fibrosis). It has also been argued that the lower rate of change in preventable mortality in females compared to males may be due to an increase in breast cancer mortality [
14].
Alcohol consumption in Korea has not decreased over the past two decades and the downward trend in hepatitis B virus infection may have contributed to the decrease in mortality from alcohol-related diseases and malignant neoplasms of the liver [
22]. Although the prevalence of smoking among men in Korea has decreased significantly from 60.9% in 2001 to 34% in 2020, the prevalence among women is very low (6.6% in 2020) and has increased slightly compared to 2001 (5.2%). Since the 2000s, the prevalence of smoking has decreased significantly due to the impact of government anti-smoking policies and changes in social awareness and is almost comparable to the average prevalence in OECD countries. Gender disparities in lifestyle behaviors, including smoking and alcohol consumption, are likely to be an important factor in the difference in LEB between males and females [
23].
The present study could suggest the factors that influenced the decline in preventable mortality in two aspects.
First, a significant contributor to preventable mortality is vaccination. Vaccines are one of the greatest achievements of biomedical science and public health, contributing to the reduction of acute and chronic infectious diseases. Studies in the United States have shown that vaccination has reduced deaths by more than 99% for diphtheria, mumps, pertussis, and tetanus [
24]. Polio, measles, and rubella viruses have been eliminated, and smallpox has been eradicated globally. Reductions in cases and deaths of most vaccine-preventable diseases, including hepatitis A, acute hepatitis B, Hib, and chickenpox, have been shown to be greater than 80%. In Korea, immunization rates are estimated to be high due to state support for essential immunizations for children. According to data from Statistics Korea in 2020 (National Childhood Immunization Rate Status), the immunization rate of nine vaccines surveyed was over 90%. The vaccination target is also gradually expanding, and in the case of HPV vaccination, state support is expanding from the current 12-year-olds to female adolescents aged 13-17 and low-income women aged 18-26. Immunization against human papillomavirus infection aims to prevent cervical, oropharyngeal, and anal and genital cancers. It can be said that infection prevention policies and immunizations have led to a decrease in infectious diseases and a decrease in avoidable mortality.
Second, Korea has implemented the National Health Promotion Act of 1995, which aims to improve the health of the people by creating conditions for practicing healthy living, and has implemented health promotion projects through health education, disease prevention, nutrition improvement, and healthy living practices. Changes in lifestyle appear to have contributed to the decline in preventable mortality. The development of non-communicable diseases, the world's leading cause of death, is influenced by lifestyle. Smoking, physical inactivity, unhealthy diet, obesity, and other lifestyle behaviors (such as alcohol consumption) are associated with the development of diseases such as cancer, heart disease, stroke, and diabetes [
25], and are factors in reducing preventable mortality.
The higher the number of healthy lifestyle factors among the above five lifestyle factors, the lower the mortality rate, especially when four healthy lifestyle factors are practiced [
25,
26], and when at least three are practiced, it can be considered to have a healthy lifestyle [
27]. Therefore, it is thought that time and motivation are needed to continuously promote health promotion projects for lifestyle improvement to the entire population so that it can become a habit.
In present study, cerebrovascular disease and transport accidents were the factors that influenced the increase in LEB from avoidable mortality in both males and females. Cerebrovascular disease contributed 0.942 years of LEB for males and 0.823 years of LEB for females. This is consistent with studies in Europe[
28], Korea [
15] and elsewhere that show that changes in the mortality of circulatory diseases are a major factor affecting LEB.
The age-standardized mortality rate for cerebrovascular disease in Korea decreased from 89.8 per 100,000 in 2000 to 20.1 in 2020, which is lower than the average for OECD countries (63.5 in 2018) [
12]. The global rate of cerebrovascular disease deaths in Korea is also decreasing, which may have contributed to the decrease in avoidable mortality. The decline in stroke mortality, a type of cerebrovascular disease, can be attributed to quality improvement efforts. The Acute Stroke Adequacy Evaluation System was launched by the Korea Health Insurance Review and Assessment Service in 2006, and the Ministry of Health and Welfare has been operating regional cardiovascular disease centers since 2008. In addition, the Cardiovascular Disease Act was enacted in 2016, which comprehensively establishes and implements policies for the prevention, treatment, rehabilitation, and research of cardiovascular diseases. In addition, the decrease in the prevalence of hypertension, the increase in the treatment rate for hypertension, and the expansion of medical access through the National Health Insurance Program have contributed to the decrease in cerebrovascular disease mortality [
22].
Among avoidable causes, the decrease in transportation accidents contributed to the improvement in LEB for both males and females. It increased LEB by 0.768 years for males and 0.324 years for females. Korea's transport accident rate decreased from 21.8 deaths per 100,000 people in 2000 to 5.9 deaths per 100,000 people in 2020, which is still the highest among major OECD countries. This decrease in traffic accident fatality rate can be attributed to seat belt use, walking environment improvement projects, expansion of traffic surveillance cameras, increased fines, stricter penalties for drunk driving, and road safety education programs.
In this study, suicide (intentional self-harm) was found to be the leading cause of decreased LEB in both men and women. Korea's suicide rate (per 100,000 population) was 23.0 ('17), the highest among OECD countries and 2.1 times higher than the OECD average (11.2). Over the 20-year period 2000-2020, the increase in mortality from suicide was the largest contributor to the decline in LEB. Suicide mortality has now surpassed deaths from diabetes, hypertensive disease, and liver disease, and the need to address rising suicide mortality cannot be overemphasized. Since 2000, suicide rates have continued to increase, reaching a peak in 2011, and have been declining since then. This can be explained by the fact that in this study, suicide was analyzed as a negative contributor to LEB in the period 2000-2010, whereas in the period 2010-2020 it was analyzed as a positive contributor.
In 2020, the suicide rate was three times higher for men than for women and increased with age, peaking in the 80+ age group. Suicide rates have been reported to increase during economic crises in different countries[
29,
30,
31], and the impact of changes in the economy, employment, and other socioeconomic factors on suicide rates may have been greater in men in recent decades [
32].
Pneumonia was the cause of death that contributed to the decrease in LEB among males. Infectious disease mortality rates for pneumonia and influenza are known to fluctuate from year to year, but in any given year, pneumonia mortality accounts for 30% of all respiratory causes of death in the OECD [
33]. Pneumonia is a common cause of death in the elderly [
34], and the resurgence of pneumonia is likely since Korea is the fastest aging country in the world [
35]. In the future, pneumococcal and influenza immunization rates should be increased, and the prescription of antibiotics should be used more wisely [
36]. Strategies to reduce the volume and pathogenicity of aspirated material are needed, especially in the elderly, because swallowing disorders and cough reflex disorders in the presence of cerebrovascular disease increase the risk of pneumonia [
34].
Breast cancer was found to be the cause of decreased LEB among females. Breast cancer is the most common malignancy among Korean women and is a multifactorial complex disease in which many factors are involved in the development of the disease, including family history and genetic predisposition, internal environmental factors such as hormonal and reproductive factors, drugs, personal illness and lifestyle, and external environmental factors such as diet, occupational exposure, and environmental hormones. A woman's age can be seen as a major factor contributing to the increased risk of breast cancer because many risk factors for breast cancer can accumulate and increase with age, and exposure to female sex hormones also accumulates with age [
37]. However, while the frequency of breast cancer increases with age in Western women, it increases until the early 50s in Korea and then gradually decreases after that. According to OECD statistics, the five-year survival rate for breast cancer in Korea from 2010-2014 was 86.6%, which is slightly higher than the OECD average of 84.5%. Primary prevention of breast cancer can be considered as reducing exposure to female hormones and improving lifestyle. Secondary prevention is early detection, and women aged 40 and older are encouraged to have a mammogram every two years. Early detection and treatment of breast cancer can reduce mortality, and higher national cancer screening rates have been shown to reduce curable mortality [
38]. It has also been reported that breast cancers detected by screening often have a better prognosis and tend to have lower mortality rates than cancers diagnosed after symptoms have developed, emphasizing the effectiveness and importance of breast cancer screening.
The present study suggests that the causes of death that contributed to the decline in LEB during the period 2000-2020 were suicide (both genders), pneumonia (males), and breast cancer (females), and that improving avoidable causes of death, especially preventable causes, can contribute to increasing LEB.
Korea is one of the OECD countries with the highest projected LEB at age 65 [
35], and reductions in avoidable mortality have contributed significantly to the increase in LEB among the elderly. There is still room for improvement in avoidable mortality, and health policies to reduce treatable and preventable mortality should continue.