1. Introduction
According to International Diabetes Federation it is estimated that 537 million people worldwide have diabetes, and vast majority of cases are type 2 diabetes (T2D). In addition, there are around 541 million people who have impaired glucose tolerance. It is predicted that by 2045 the number of diabetes cases will reach 783 million. By all accounts, diabetes is certainly one of the fastest-growing global health issues of the 21st century [
1].
According to a recent systematic review, the leading cause of mortality and comorbidity in people with diabetes is cardiovascular disease (CVD), which accounts for 50.3% of all deaths [
2]. It is assessed that in the U.S. around
$37.3 billion per year is spent to treat cardiovascular-related complications associated with diabetes [
3]. A great number of people with type 2 diabetes have cardiometabolic risk factors that can be modified, such as smoking, sedentary lifestyle, dyslipidemia, hypertension, and obesity.
Clinical guidelines recommend an approach to the management of type 2 diabetes that goes beyond simply lowering glucose levels to reduce modifiable cardiometabolic risk factors [4-8].
Treatment should be guided by a person-centered, holistic, multifactorial approach that takes into account individual goals related to glycemic control, body weight, and cardiovascular risk factor management to maintain and improve patient well-being.
It's well established that obesity significantly increases the risk of developing type 2 diabetes and is associated with numerous other psychosocial and medical complications [
9,
10].
According to the American Diabetes Association (ADA), overweight patients with T2D may benefit from modest weight loss (3–7% of baseline weight) in terms of improved glycemic management and cardiovascular risk factor improvement. Greater benefit, including improvement in long-term cardiovascular outcomes and possible remission of disease, results from sustained weight loss greater than 10% of body weight. It is recommended that the potential beneficial effects on body weight be considered when choosing an antihyperglycemic drug. Pharmacological therapy for obesity in these patients is considered effective if the patient loses ≥5% of body weight after 3 months of therapy [
9].
It is especially important to introduce physical activity and a healthy diet in addition to glucose-lowering medication as an effective component of glucose management for people with T2D and obesity.
Over the past decade, a number of clinical trials have been published with results showing that modern therapies, including glucagon-like peptide-1 receptor agonists (GLP-1 RA) and SGLT-2 inhibitors, achieve significant and consistent cardiometabolic benefits [
11].
Semaglutide is the only GLP-1 RA available in both injectable and oral formulation. The efficacy of once-weekly subcutaneously administered semaglutide and once-daily oral semaglutide has been evaluated in the comprehensive clinical trial programs SUSTAIN and PIONEER.
However, to date, no direct comparative studies between injectable and oral semaglutide formulations have been performed. Therefore, the aim of our study was to compare the effectiveness of the two semaglutide formulations in terms of glycemic and body weight control in a real-world setting.
2. Materials and Methods
2.1. Study Design and Population
This was a single-center retrospective observational study conducted at the Rijeka Clinical Hospital Centre. A total of 106 adult (>18 yr.) patients with inadequately controlled type 2 diabetes (HbA1 ≥ 7%) on different oral or basal insulin supported oral therapy were recruited from the diabetes outpatient clinic. All subjects were GLP-1 RA naive and consequently prescribed 0.5 or 1.0 mg once weekly injectable semaglutide (IS) or 7 mg or 14 mg once daily oral semaglutide (OS) for at least 6 months. Glycated hemoglobin (HbA1c), body weight, and body mass index (BMI) were assessed prior to semaglutide administration and after a 6-month follow-up period. The primary endpoint was the change from baseline in HbA1c, and secondary endpoints were the change in body weight and the proportion of participants with a reduction in body weight of ≥ 5% and ≥ 10%, respectively, 6 months after the initiation of semaglutide treatment. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Clinical Hospital Center Rijeka (No: 003-05/20-1/54).
2.2. Data Collection
Data from electronic medical records were retrospectively collected and analyzed from May 2021 to November 2022. Demographic (age, gender) and relevant clinical data [body weight, body height, BMI, HbA1c, comorbidities (arterial hypertension, dyslipidemia, cardio/cerebrovascular disease)] were collected.
2.3. Statistical Analysis
Statistical analysis was performed using Microsoft Excel (Microsoft Office) and MedCalc v12.1.3 (MedCalc Software bvba, Ostend, Belgium). Absolute and relative frequencies, measures of central tendancy, and measures of spread, were used to present the data. The Mann-Whitney test and the χ2-test were used to compare outcomes between groups. Criterion for statistical significance was estimated on p<0.05. All tests were run under 95% confidence interval (CI).
3. Results
The group of patients administered injectable semaglutide consisted of a total of 53 participants, 30 of whom were men and 23 women, aged 38-78 years. In this group, 10 (18.9%) patients received 0.5 mg of injectable semaglutide, and 43 (81.1%) of them received 1.0 mg. In addition, 12 (22.6%) patients were found to have cardiovascular disease (CVD). In addition to injectable semaglutide, patients also received previously prescribed concomitant therapy, including 48 (90.6%) metformin, 21 (39.6%) SGLT-2i, 11 (20.8%) a sulfonylurea, 3 (5.7%) pioglitazone, and 16 (30.2%) insulin.
The other group of patients who received oral semaglutide consisted of a total of 53 patients, 30 men and 23 women, aged 46-79 years. In this group, 20 (37.7%) patients received an oral semaglutide dose of 7 mg and 14 (62.3%) of them received a dose of 14 mg. CVD was confirmed in 9 (17%) participants in this group. In addition to oral semaglutide, patients in this group also received previously prescribed concomitant therapy, 52 (98.1%) of them metformin, 24 (45.2%) patients SGLT-2i, 13 (24.5%) patients in therapy had a sulfonylurea, 2 (3.8%) patients pioglitazone, and 12 (22.6%) of them insulin.
The demographic and clinical characteristics of the patients (n=106; 56.6% female), who were divided into two groups based on the therapy administered, are shown in
Table 1. There were no statistically significant differences between the oral semaglutide group and the injectable semaglutide group in age and confirmed cardiovascular disease (CVD). There was a significant difference between the doses of the investigational drugs (lower vs. upper dose) between the groups, in favor of the IS group (P=0.014).
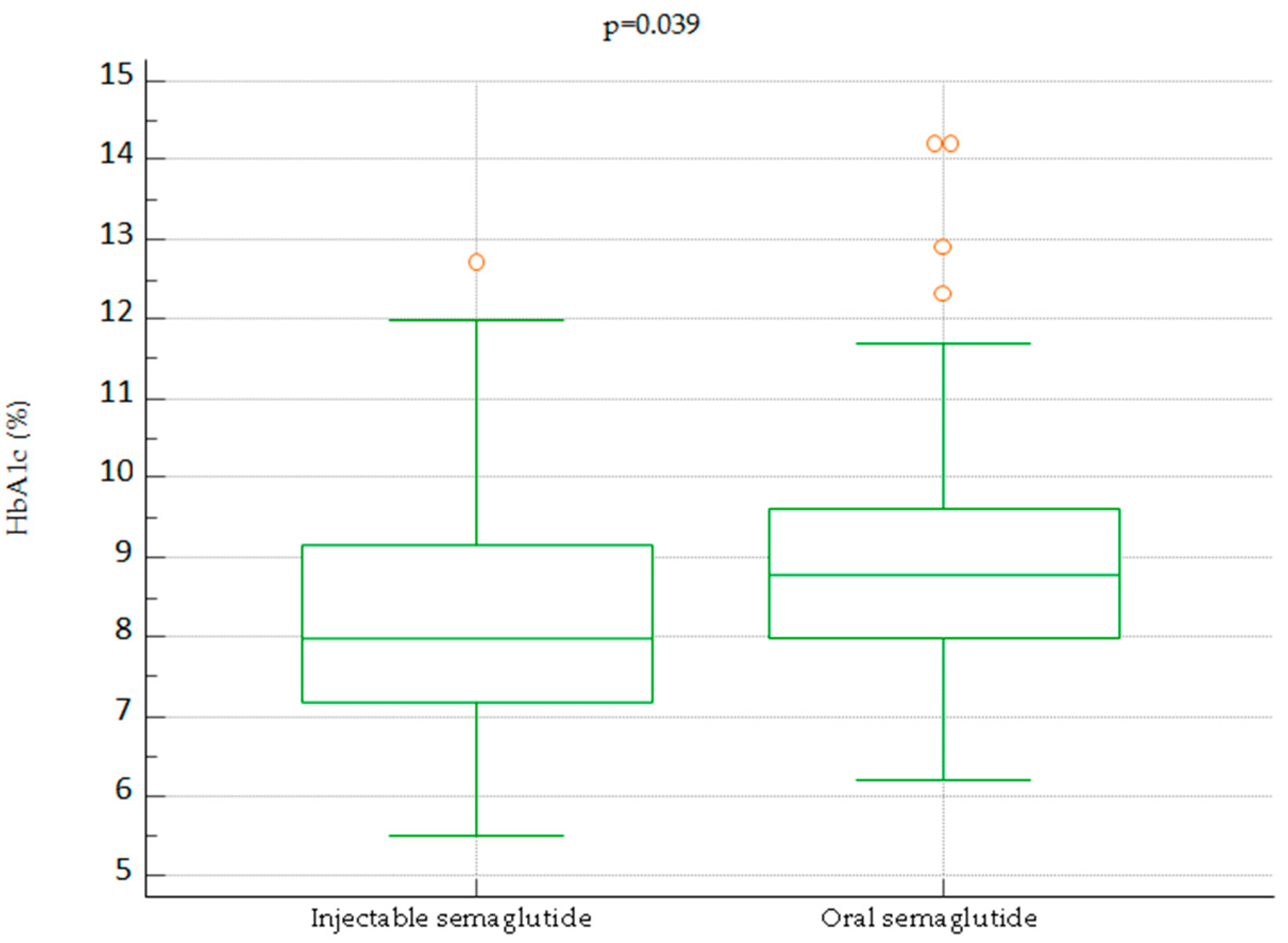
Baseline HbA1c levels are shown in
Figure 1. There was a statistically significant difference in baseline HbA1c values between the injectable semaglutide group and the oral semaglutide group [8.0 (5.5-12.7) versus 8.80 (6.2-14.2) %, P=0.039].
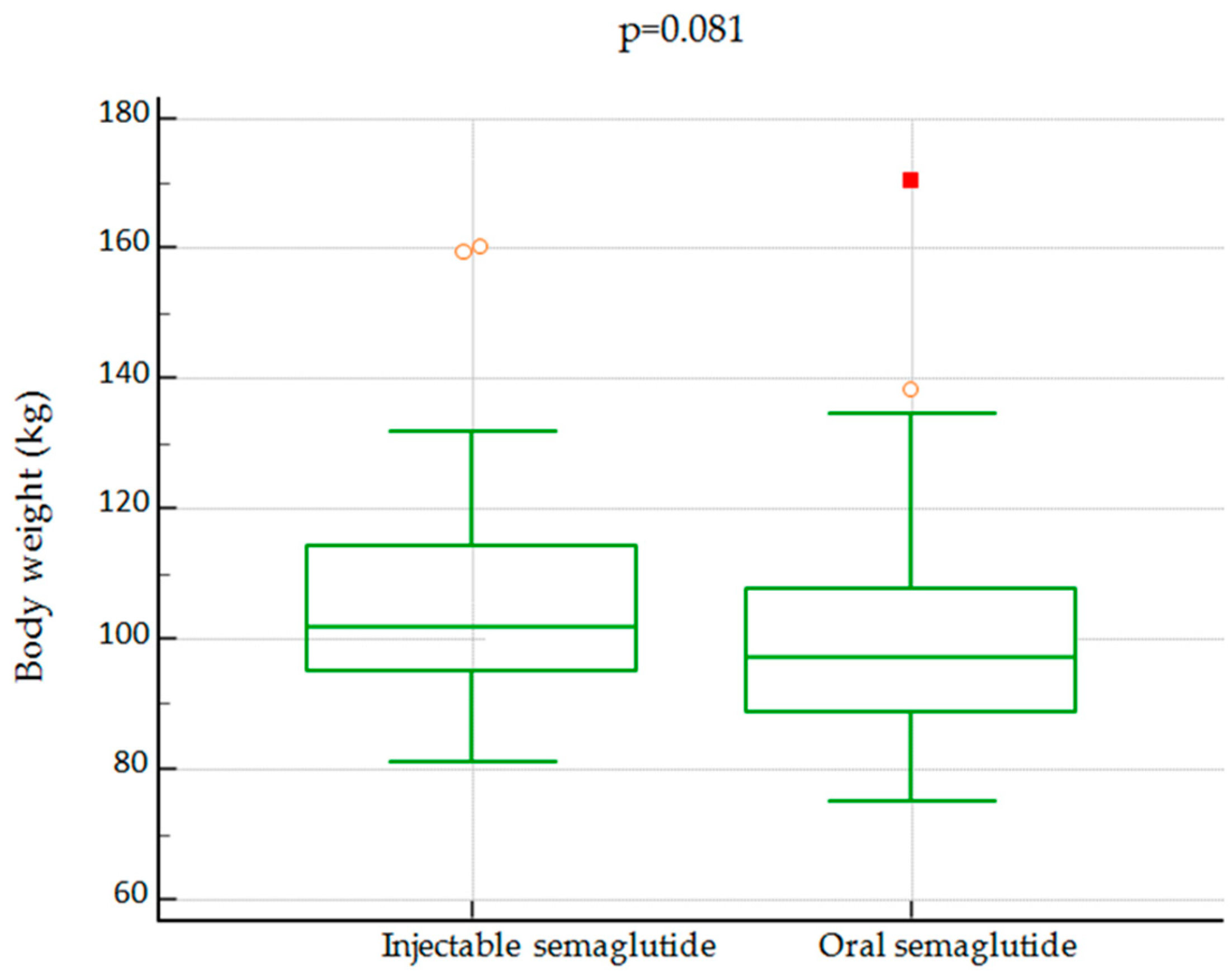
There was no statistically significant difference in terms of baseline body weight between the groups [102.0 ± 5.1 kg vs 97.3 ± 5.9 kg (P=0.081)]
Figure 2.
Box plot with comparisons of baseline body weight between IS and OS group.
Figure 2.
Box plot with comparisons of baseline body weight between IS and OS group.
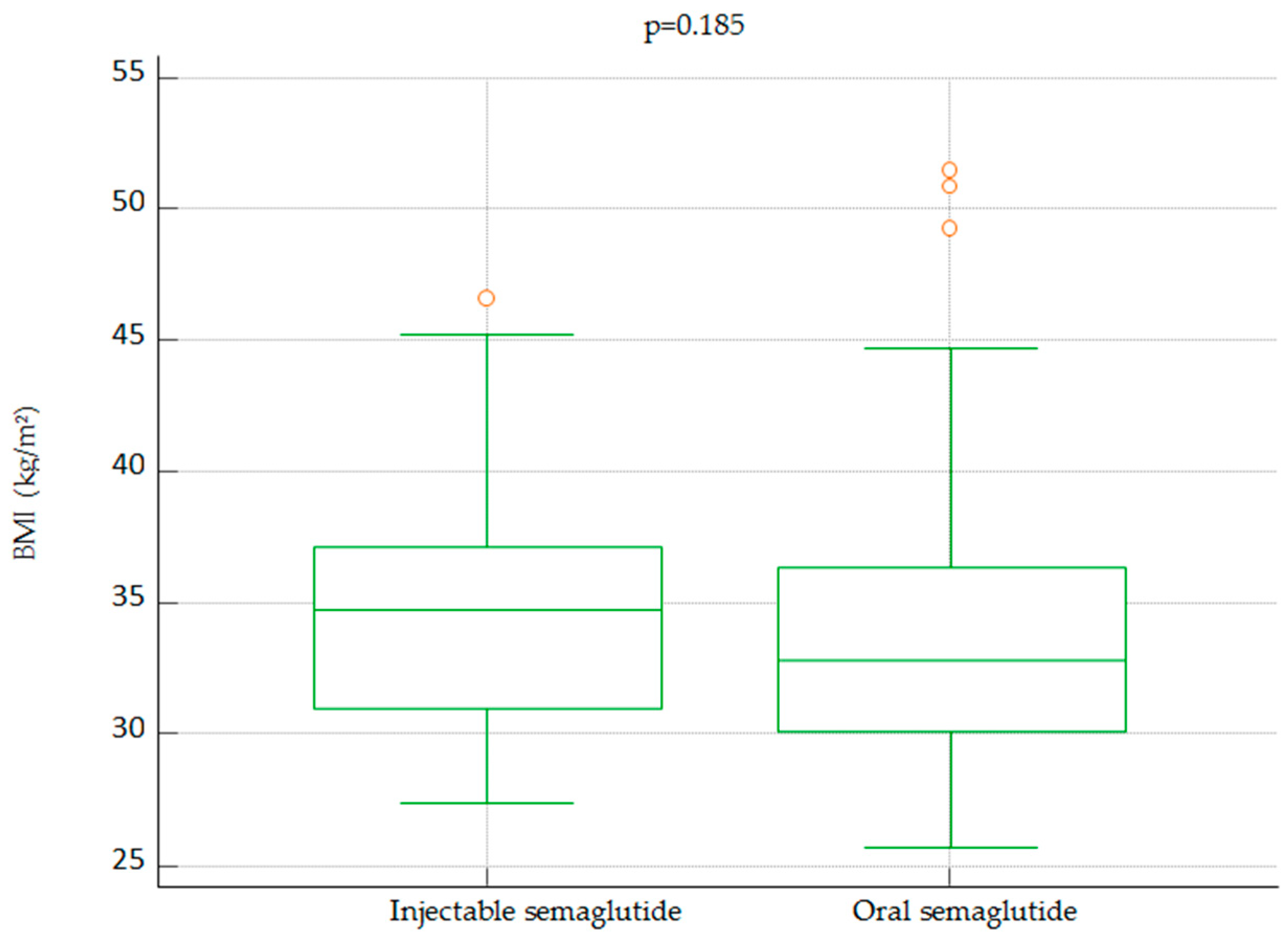
In addition, no statistically significant difference was found between groups in baseline BMI [34.72 (27.41-46.61) vs. 32.87 (25.73-51.45) kg/m2, P=0.185].
Figure 3.
Box plot with comparisons of baseline body mass index between IS and OS group.
Figure 3.
Box plot with comparisons of baseline body mass index between IS and OS group.
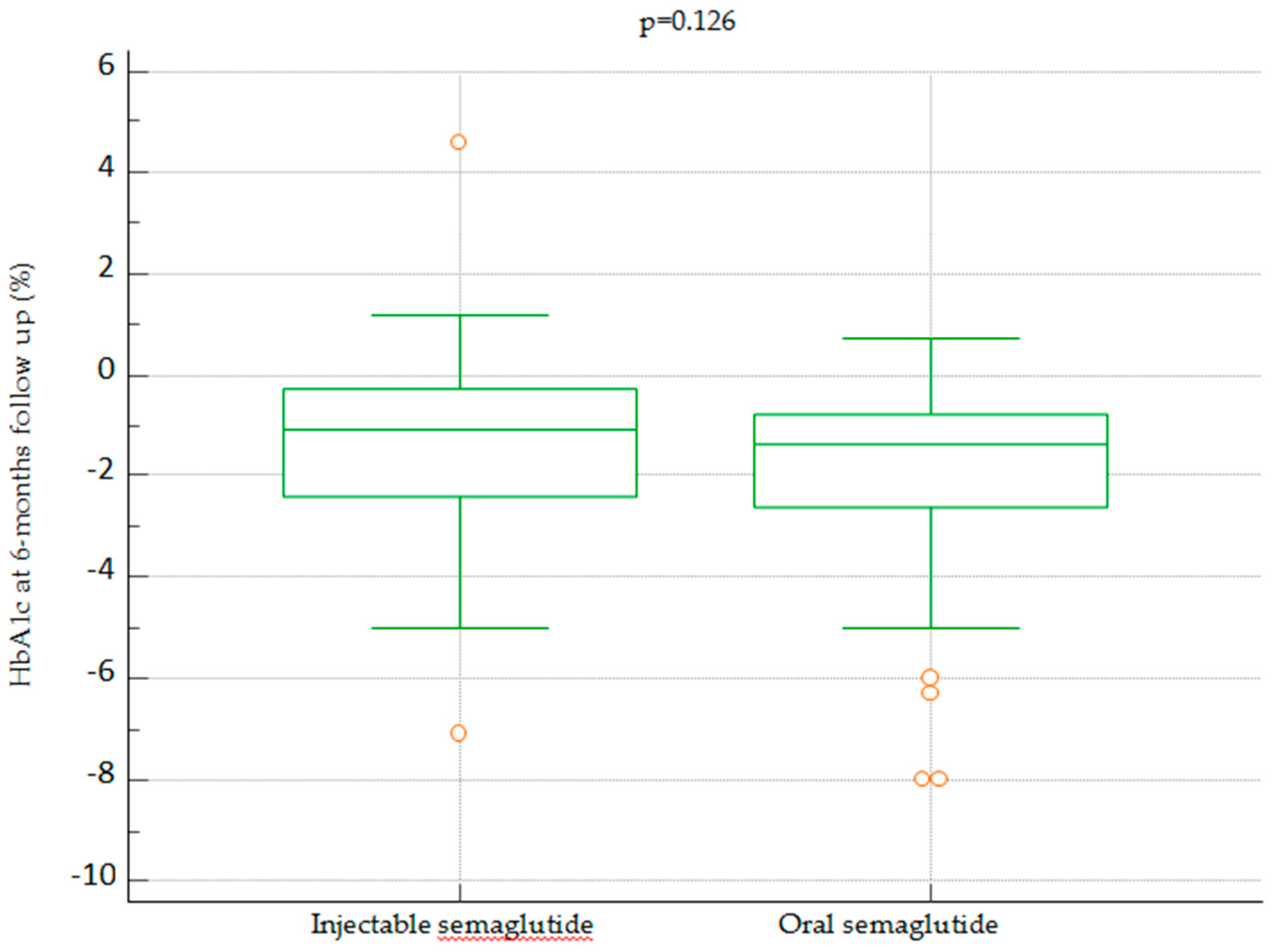
When comparing the efficacy of IS and OS in lowering blood glucose (using HbA1c as a surrogate), no difference was observed between the two formulations at 6 months [-1.10 (-7.10-4.60) vs. -1.40 (-8.0-0.70) %, P=0.126].
Figure 4.
Change in HbA1c after 6 month of treatment with IS vs OS.
Figure 4.
Change in HbA1c after 6 month of treatment with IS vs OS.
At 6-month follow-up, no significant difference in body weight was observed between the injectable semaglutide group and the oral semaglutide group [-6.50 (-28.0-10.0) vs -5.90 (-45.3-0.2) kg, P=0.714], as shown in
Figure 5.
Participants in both groups, 56.7% in total (n=30), achieved a loss of body mass > 5% (P=1.000). Weight loss > 10% was observed in 20.7% (n=11) of patients on injectable semaglutide and in 15.1% (n=8) of patients on oral semaglutide (P=0.454). No statistically significant difference was observed between the groups.
4. Discussion
GLP-1RAs have been shown to be an effective treatment for patients with type 2 diabetes. Remarkable clinical benefits of GLP-1RAs have been demonstrated, not only in maintaining glycemic control and protecting against hypoglycemia, but also in significant weight loss, lowering blood pressure, and improving lipid profiles [
12].
Moreover, their use has been associated with a reduced risk of major cardiovascular events (MACE), cardiovascular death, nonfatal myocardial infarction, and nonfatal ischemic stroke in patients with T2D [
13].
Semaglutide is the only GLP-1 RA available in both injectable and oral formulation. Impaired absorption of orally administered peptides has been overcome by co-formulation with the absorption enhancer sodium N-(8-[2 hydroxybenzoyl]amino)caprylate (SNAC) which protects semaglutide through local buffering and leads to facilitated absorption across the gastric epithelium [
14,
15].
The first oral formulation of GLP-1RA semaglutide (Rybelsus) was approved by U.S. Food and Drug Administration (FDA) in September 2019 and by European Medicines Agency (EMA) in April 2020 [
16,
17].
Due to the lower bioavailability of oral semaglutide compared to the subcutaneous formulation, a higher dose of 7 mg to 14 mg/day versus 1 mg to 2 mg/week of the subcutaneous formulation is required [
18].
Oral semaglutide is indicated in adults with T2D, as treatment of inadequate glycemic control alongside diet and exercise to improve glycaemia. Starter dose is 3 mg once daily for 30 days, after 30 days dose should be increased to maitenance dosage of 7 mg once daily. In case the maintenance dose of 7 mg after 30 days is not sufficient, the prescriber may increase the dose to 14 mg once daily which is also the maximum currently available daily dose [
17].
Both formulations of semaglutide have been shown to be nearly equally effective in achieving and maintaining glycemic targets, with 66–80% of patricipants administered semaglutide 1.0 mg subcutaneously achieving an HbA1c <7% in SUSTAIN trials, compared with 55–77% of participants treated with oral semaglutide 14 mg throughout the PIONEER study programme [
19]. Moreover, the safety profile of both formulations is highly similar and they have also been associated with significant weight loss and low risk of hypoglycemia [
19].
In a clinical trial conducted by Gibbons et al. (2021.), people with a BMI of 20 - 38 kg/m
2 had less food cravings, had greater control over their diet, and consumed less food at each meal of the day with oral formulation of semaglutide versus placebo [
18].
Semaglutide has shown to be a better option compared to the other GLP-1RA liraglutide, with an average weight loss of 5.8 kg versus 1.9 kg after 30 weeks of treatment [
20].
Given the generally similar efficacy and safety profiles of the two formulations, further considerations may need to be made in selecting the most appropriate formulation. Many patients are reluctant to initiate treatment with injectable medications due to fear of pain during injection and a sense of failure related to disease progression. A possible disadvantage of taking semaglutide orally is that the tablet must be taken on an empty stomach 30 minutes before a meal, drink, or taking other medications to ensure unimpeded absorption [
17].
Our study is the first direct comparison between the two semaglutide formulations in a real-world setting showing equal effectiveness of oral and injectable semaglutide in terms of glycemic control and weight loss after 6 months of treatment.
However, since this is a single-centre retrospective observational study; the findings should be interpreted accordingly. It was conducted on a relatively small sample of respondents. Also, due to aforementioned study design, the researchers had no control over exposures and interventions or absolute medication adherence. Likewise, there is the possibility of various confounding effects, such as background therapy and comorbidities. Nonetheless, our results have shown that orally administered semaglutide may be as effective an option for improving glycemic target attainment and supporting weight loss in adults with T2D as the injectable formulation, particularly in patients who are reluctant to take injectable medications.
5. Conclusions
In a real-world setting, oral semaglutide as add-on therapy to ongoing antihyperglycemic treatment in patients with inadequately controlled type 2 diabetes who had not previously received GLP-1 RA demonstrated the same effectiveness as injectable semaglutide in terms of glycemic control and weight loss after 6 months of treatment. Considering the almost equal effect, the oral formulation of semaglutide could make it easier for patients to use since there is no injection burden.
Author Contributions
S.K. and A.B. - conception and design, data acquisition and analysis, review and editing; I.B. - data acquisition; N. M. - original draft preparation; D. R. – supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Clinical Hospital Center Rijeka (No: 003-05/20-1/54).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
Sanja Klobučar is the vice president of the Croatian Society for Diabetes and Metabolic Disorders of the Croatian Medical Association and the vice president of the Croatian Society for Obesity of the Croatian Medical Association. She serves as an Executive Committee member of the Croatian Endocrine Society. She has served as principal investigator or co-investigator in clinical trials of Eli Lilly, MSD, Novo Nordisk, and Sanofi Aventis. She has received honoraria for speaking or advisory board engagements and consulting fees from Abbott, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Lifescan—Johnson & Johnson, Novartis, Novo Nordisk, MSD, Merck Sharp & Dohme, Mylan, Pliva, and Sanofi Aventis. Dario Raheli´c is the director of the Vuk Vrhovac University Clinic for Diabetes, Endocrinology, and Metabolic Diseases at Merkur University Hospital, Zagreb, Croatia. He is the president of the Croatian Society for Diabetes and Metabolic Disorders of the Croatian Medical Association. He serves as an Executive Committee member of the Croatian Endocrine Society, Croatian Society for Obesity, and Croatian Society for Endocrine Oncology. He was a board member and secretary of IDF Europe, and the chair of the IDF Young Leaders in Diabetes (YLD) Program. He has served as an Executive Committee member of the Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes (EASD), and currently, he serves as an Executive Committee member of the Diabetes and Cardiovascular Disease Study Group of EASD. He has served as a principal investigator or co-investigator in clinical trials for AstraZeneca, Eli Lilly, MSD, Novo Nordisk, Sanofi Aventis, Solvay, and Trophos. He has received honoraria for speaking or advisory board engagements and consulting fees from Abbott, Amgen, AstraZeneca, Bauerfeund, Bayer, Boehringer Ingelheim, Eli Lilly, Lifescan—Johnson & Johnson, Novartis, Novo Nordisk, MSD, Mylan, Pfizer, Pliva, Roche, Salvus, Sanofi Aventis, and Takeda. The other authors declare no conflict of interest.
References
- Sun, H., Saeedi, P., Karuranga, S., Pinkepank, M., Ogurtsova, K., Duncan, B. B., Stein, C., Basit, A., Chan, J. C. N., Mbanya, J. C., Pavkov, M. E., Ramachandaran, A., Wild, S. H., James, S., Herman, W. H., Zhang, P., Bommer, C., Kuo, S., Boyko, E. J., & Magliano, D. J. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022, 183, 109119. [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 2018, 17, 1-19. [CrossRef]
- American Diabetes Association Economic Costs of Diabetes in the U.s. in 2017. Diabetes Care 2018, 41, 917–928.
- King, D.E.; Mainous, A.G., 3rd; Buchanan, T.A.; Pearson, W.S. C-Reactive Protein and Glycemic Control in Adults with Diabetes. Diabetes Care 2003, 26, 1535–1539.
- McGurnaghan, S.; Blackbourn, L.A.K.; Mocevic, E.; Haagen Panton, U.; McCrimmon, R.J.; Sattar, N.; Wild, S.; Colhoun, H.M. Cardiovascular Disease Prevalence and Risk Factor Prevalence in Type 2 Diabetes: A Contemporary Analysis. Diabet. Med. 2019, 36, 718–725. [CrossRef]
- CDC Coronavirus Disease 2019. Available online: https://www.cdc.gov/chronicdisease/. (accessed on 5 April 2023).
- American Heart Association. Available online: https://www.heart.org/. (accessed on 20 March 2023).
- Grant, P.J.; Cosentino, F. The 2019 ESC Guidelines on Diabetes, Pre-Diabetes, and Cardiovascular Diseases Developed in Collaboration with the EASD: New Features and the ‘Ten Commandments’ of the 2019 Guidelines Are Discussed by Professor Peter J. Grant and Professor Francesco Cosentino, the Task Force Chairmen. Eur. Heart J. 2019, 40, 3215–3217.
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46, S128–S139. [CrossRef]
- Narayan, K.M.V.; Boyle, J.P.; Thompson, T.J.; Gregg, E.W.; Williamson, D.F. Effect of BMI on Lifetime Risk for Diabetes in the U.S. Diabetes Care 2007, 30, 1562–1566. [CrossRef]
- Sharma A, Verma S. Mechanisms by Which Glucagon-Like-Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter-2 Inhibitors Reduce Cardiovascular Risk in Adults With Type 2 Diabetes Mellitus. Can J Diabetes. 2020;44(1):93-102. [CrossRef]
- Lyseng-Williamson, K.A. Glucagon-like Peptide-1 Receptor Agonists in Type-2 Diabetes: Their Uses and Differential Features. Clin Drug Invest 2019, 39, 805–819. [CrossRef]
- Lin, D.S.-H.; Lee, J.-K.; Chen, W.-J. Major Adverse Cardiovascular and Limb Events in Patients with Diabetes Treated with GLP-1 Receptor Agonists vs DPP-4 Inhibitors. Diabetologia 2021, 64, 1949–1962. [CrossRef]
- Buckley, S.T.; Bækdal, T.A.; Vegge, A.; Maarbjerg, S.J.; Pyke, C.; Ahnfelt-Rønne, J.; Madsen, K.G.; Schéele, S.G.; Alanentalo, T.; Kirk, R.K.; et al. Transcellular Stomach Absorption of a Derivatized Glucagon-like Peptide-1 Receptor Agonist. Sci. Transl. Med. 2018, 10, eaar7047. [CrossRef]
- Andersen, A.; Knop, F.K.; Vilsbøll, T. A Pharmacological and Clinical Overview of Oral Semaglutide for the Treatment of Type 2 Diabetes. Drugs 2021, 81, 1003–1030. [CrossRef]
- HIGHLIGHTS OF PRESCRIBING INFORMATION These Highlights Do Not Include All the Information Needed to Use RYBELSUS ® Safely and Effectively. See Full Prescribing Information for RYBELSUS. RYBELSUS (Semaglutide) Tablets, for Oral Use Initial U.S. Approval: 2017 WARNING: RISK OF THYROID C-CELL TUMORS See Full Prescribing Information for Complete Boxed Warning. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf (accessed on 15 March 2023).
- Rybelsus. Summary of product characteristics. Available online: https://www.ema.europa.eu/en/documents/productinformation/rybelsus-epar-product-information_en.pdf (accessed on 15 March 2023).
- Gibbons, C.; Blundell, J.; Tetens Hoff, S.; Dahl, K.; Bauer, R.; Baekdal, T. Effects of Oral Semaglutide on Energy Intake, Food Preference, Appetite, Control of Eating and Body Weight in Subjects with Type 2 Diabetes. Diabetes Obes. Metab. 2021, 23, 581–588.
- Meier, J.J. Efficacy of Semaglutide in a Subcutaneous and an Oral Formulation. Front. Endocrinol. (Lausanne) 2021, 12. [CrossRef]
- Capehorn, M.S.; Catarig, A.-M.; Furberg, J.K.; Janez, A.; Price, H.C.; Tadayon, S.; Vergès, B.; Marre, M. Efficacy and Safety of Once-Weekly Semaglutide 1.0 Mg vs Once-Daily Liraglutide 1.2 Mg as Add-on to 1–3 Oral Antidiabetic Drugs in Subjects with Type 2 Diabetes (SUSTAIN 10). Diabetes Metab. 2020, 46, 100–109.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).