Introduction
Hepatic hemangiomas are considered vascular malformations. The pathogenesis of these tumors is not completely understood but according to some authors they most likely arise from hyperplasia or hypertrophy of congenital hamartomas. HH are the most frequent benign tumors of the liver. They are usually solitary, small in size and asymptomatic so they are commonly reported as incidental findings in imaging studies. The majority of them have a good prognosis however others can present as large tumors and can be symptomatic, causing abdominal discomfort, hemorrhage, respiratory distress…
Most of them are diagnosed in adulthood, around 30 – 50 years old. They are most frequently found in women, with a female: male ratio of up to 5:1; and they usually grow during pregnancy or after hormonal treatments.
In general, HH are solitary tumors, but in around 40% of the patients multiple lesions can be found. They are diagnosed by: ultrasound, computed tomography scan or Magnetic resonance imaging. Treatment is not necessary except for the cases that present with symptoms caused by enlarged HH. In these cases, surgical resection is recommended.
This report presents an unusual case of a giant HH in which surgical resection to fully remove the tumor was not possible so the patient required orthotopic liver transplantation
Clinical Case
We present the case of a 48 year old male with no previous medical history. The patient was brought to the emergency room complaining of vomiting and pain in the right upper quadrant that had been going on for 8 years. The examination showed a firm mass in the right hypochondrium that extended below the umbilicus. The US reported severe hepatomegaly secondary to giant hypoechoic lesions. The CT-scan and MRI demonstrated a giant HH arising from the right liver and multiple smaller hemangiomas on the left liver.
Surgical resection was not an option in this case so he was evaluated by a multi-disciplinary team and placed on the waiting list for a liver transplant. After three months the patient finally received a liver from a matched brain-dead organ donor.
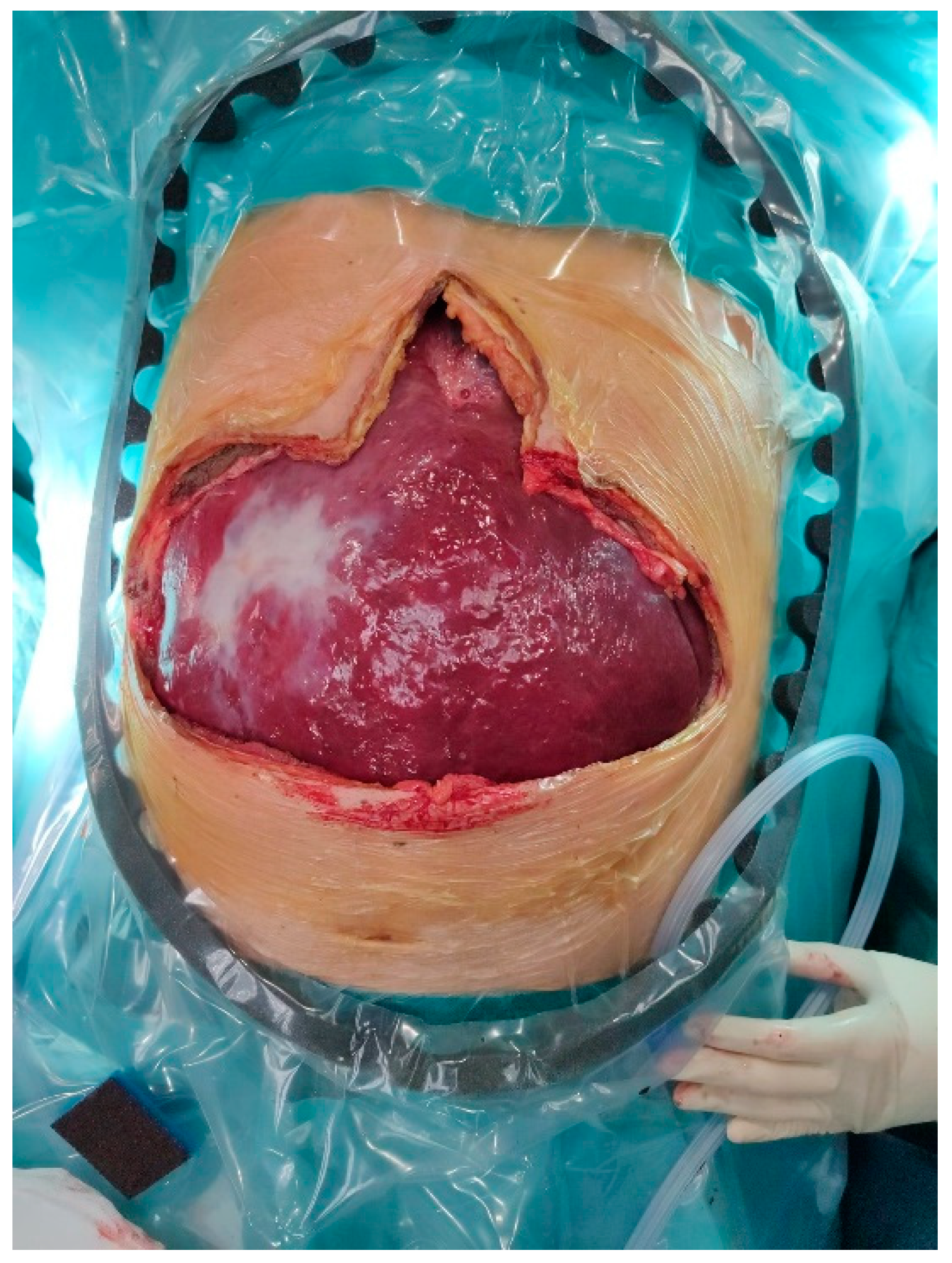
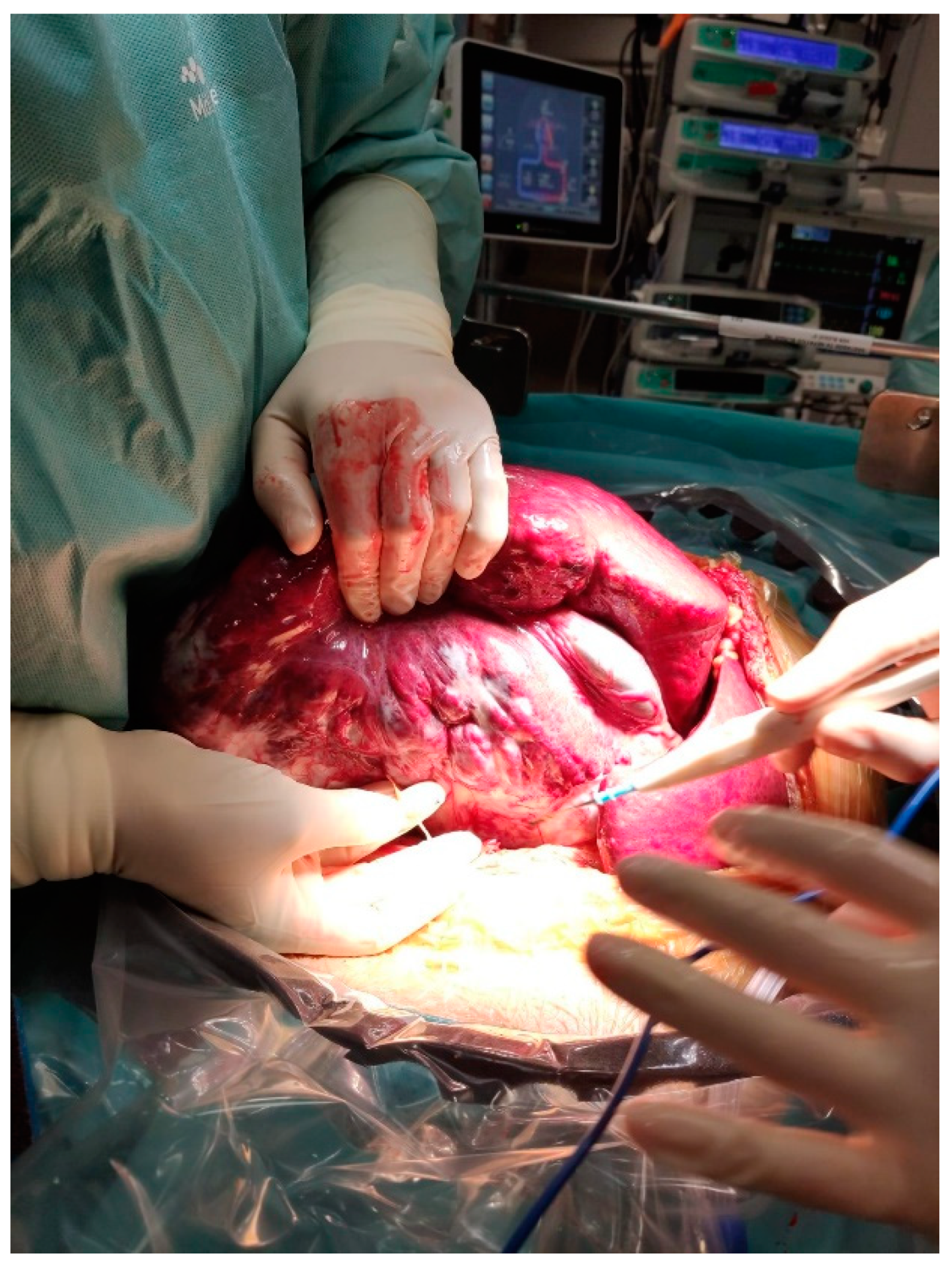
The native liver (
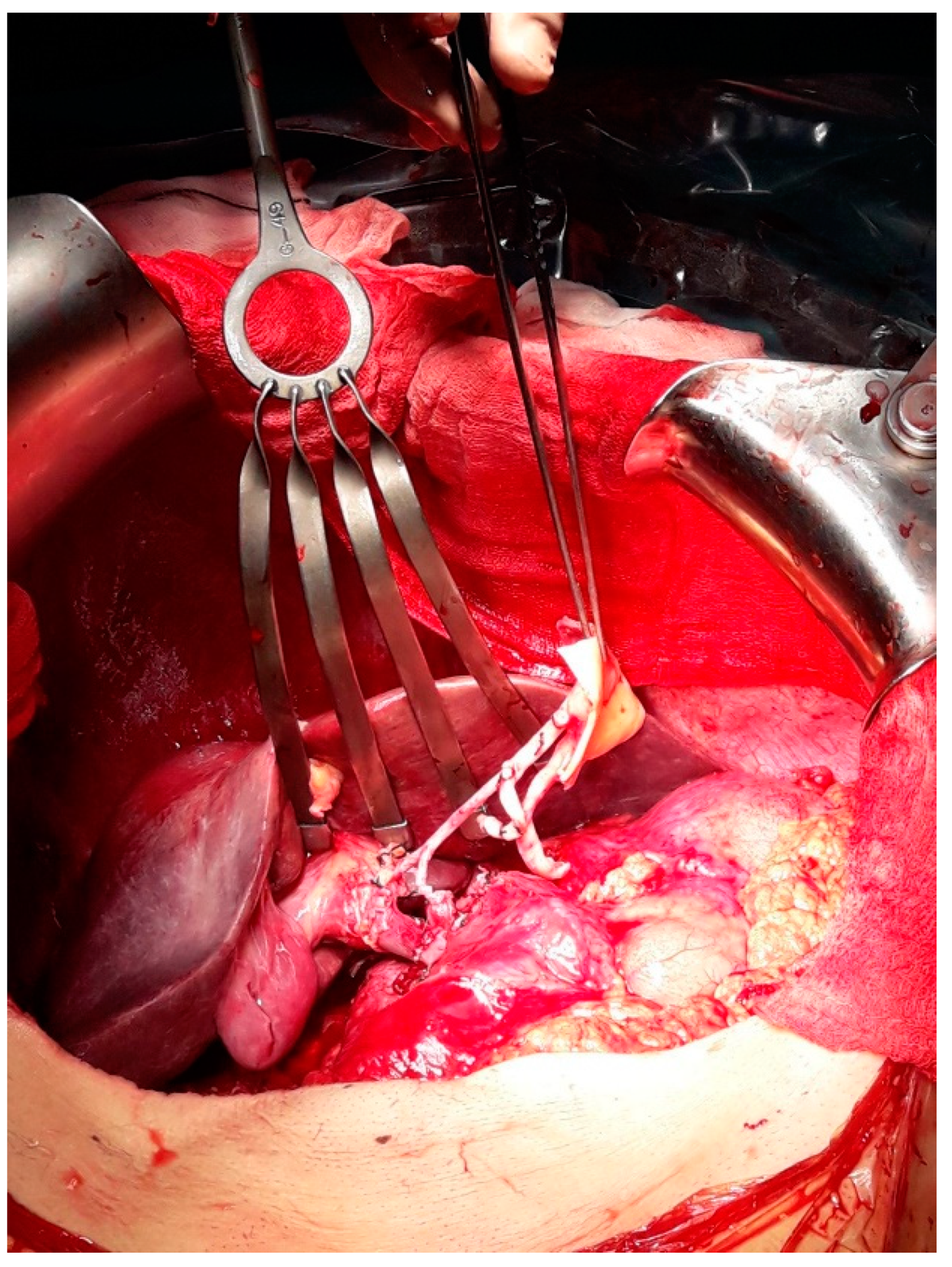
Figure 1) was dissected using a caval-preserving piggy-back (PB) implant technique under a temporary porto-caval shunt (
Figure 2). In this case the surgery was completed without the need of a classic technique nor a veno-venous bypass. He received a transfusion of 8 units of packed red blood cells during the operation. The surgery lasted for 300 min and the patient was transferred to the intensive care unit with no acute complications (
Figure 3). The explanted liver weighed 9 kg. Patient was discarded after 14 days without any medical or surgical complications. The pathology report showed a giant multifocal hemangioma, with a size of 28 x 19 x 15 cms.
After a 1 year follow up the patient has not presented with any complications and has an adequate function of the graft.
Discusión
HH are defined as liver vascular malformations, however certain authors classify them under benign tumors [
1]. The etiology is not well understood, but it is clear that tumor growth is promoted by hormonal reasons such as pregnancy or hormonal treatments.
The prevalence rate is stated between 0,5% and 20%. They are usually solitary tumors but can also be multicentric and affect both liver lobes. HH are considered giant when the size is above 5 cm although the smaller ones are more common [
1].
Clinically, most of them are asymptomatic and have excellent prognosis, they are usually described as incidental findings on imaging tests. However, bigger HH can produce symptoms caused by the compression of the mass to closer organs. The most common symptoms are: abdominal pain (in particular of the right hypochondrium); nausea, anorexia and early satiety secondary to gastric compression. On examination, only in a few cases hepatomegaly will be present [
1,
2].
Diagnostic imaging exams are needed to make the final diagnosis. Among them CT-scan with intravenous contrast is considered to be the gold standard test for diagnosis [
1] and is key for surgical planning.
The treatment differs depending on the size, location, and number of hemangiomas [
3,
4,
5]. Ranging from simple techniques such as enucleation to complete hepatectomy associating liver transplant, as the case we have presented in this report [
3,
4,
5].
During the decision-making of the case is essential to rely on a multidisciplinary team that includes a hepatobiliary and liver transplant surgeon, a hepatologist and an anesthesiologist. The surgical planning of these type of patients is essential. The risk of bleeding is higher in tumors like this, so physical conditioning and prehabilitation of the patient is critical. The goal is to minimize the risk of intra and post-surgical complications.
In cases where a complete hepatectomy and liver transplant is required it can be performed following a classic technique associating venovenous bypass, to prevent massive bleeding. However, if technically possible caval-preserving piggy-back implant technique under a temporary porto-caval shunt can be safely considered [
6,
7,
8,
9].
Finally, it is crucial to establish a preoperative plan relaying on a multidisciplinary team to minimize the risk of intraoperative and postoperative adverse events that can compromise the patient.
References
- Gandolfi L, Leo P, Solmi L, Vitelli E, Verros G, Colecchia A. Natural history of hepatic haemangiomas: Clinical and ultrasound study. Gut. 1991, 32, 677–680. [CrossRef] [PubMed]
- Díez Redondo P, Velicia Llames R, Caro-Patón A. Giant cavernous hemangiomas of the liver. Rev Esp Enferm Dig. 2004, 96, 665–666, English, Spanish. [CrossRef]
- Alvarez Pérez JA, Baldonedo Cernuda RF, Palacios Fernández E. Hemangioma cavernoso hepático gigante [Giant hepatic cavernous hemangioma]. Rev Esp Enferm Dig. 1994, 85, 403–404, Spanish.
- Farges O, Daradkeh S, Bismuth H. Cavernous hemangiomas of the liver: Are there any indications for resection? World J Surg. 1995, 19, 19–24. [CrossRef] [PubMed]
- Popescu I, Ciurea S, Brasoveanu V, Hrehoret D, Boeti P, Georgescu S, Tulbure D. Liver hemangioma revisited: Current surgical indications, technical aspects, results. Hepatogastroenterology. 2001, 48, 770–776.
- Toro A, Mahfouz AE, Ardiri A, Malaguarnera M, Malaguarnera G, Loria F, Bertino G, Di Carlo I. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann Hepatol. 2014, 13, 327–339. [CrossRef]
- Prodromidou A, Machairas N, Garoufalia Z, Kostakis ID, Tsaparas P, Paspala A, Stamopoulos P, Sotiropoulos GC. Liver Transplantation for Giant Hepatic Hemangioma: A Systematic Review. Transplant Proc. 2019, 51, 440–442. [CrossRef] [PubMed]
- Russo MW, Johnson MW, Fair JH, Brown RS Jr. Orthotopic liver transplantation for giant hepatic hemangioma. Am J Gastroenterol. 1997, 92, 1940–1941.
- Lange UG, Bucher JN, Schoenberg MB, Benzing C, Schmelzle M, Gradistanac T, Strocka S, Hau HM, Bartels M. Orthotopic liver transplantation for giant liver haemangioma: A case report. World J Transplant. 2015, 5, 354–359. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note:
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).