Submitted:
25 August 2023
Posted:
04 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
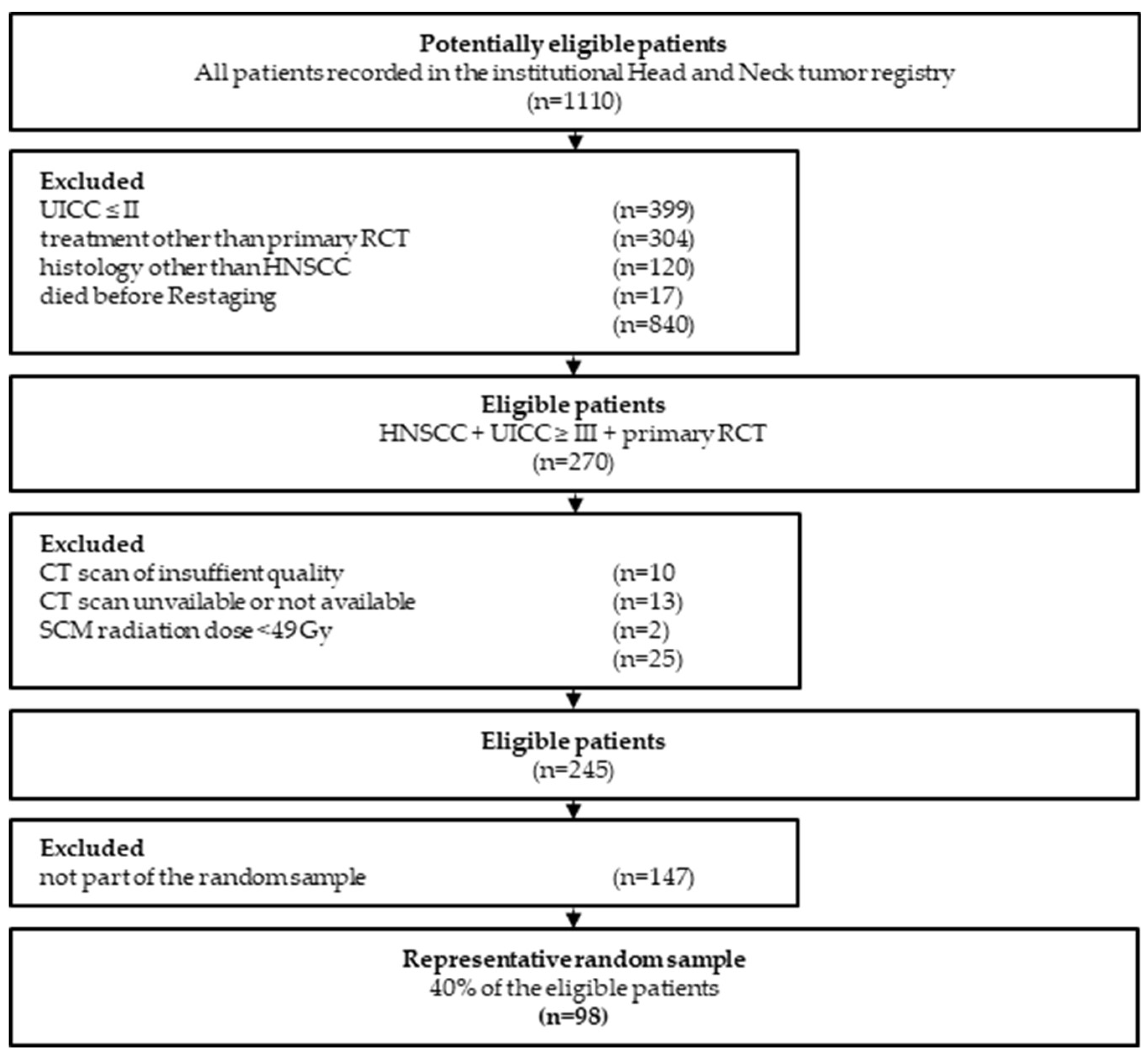
2.1. Study population and additional clinical data
2.2. Clinical data
2.3. CT imaging acquisition
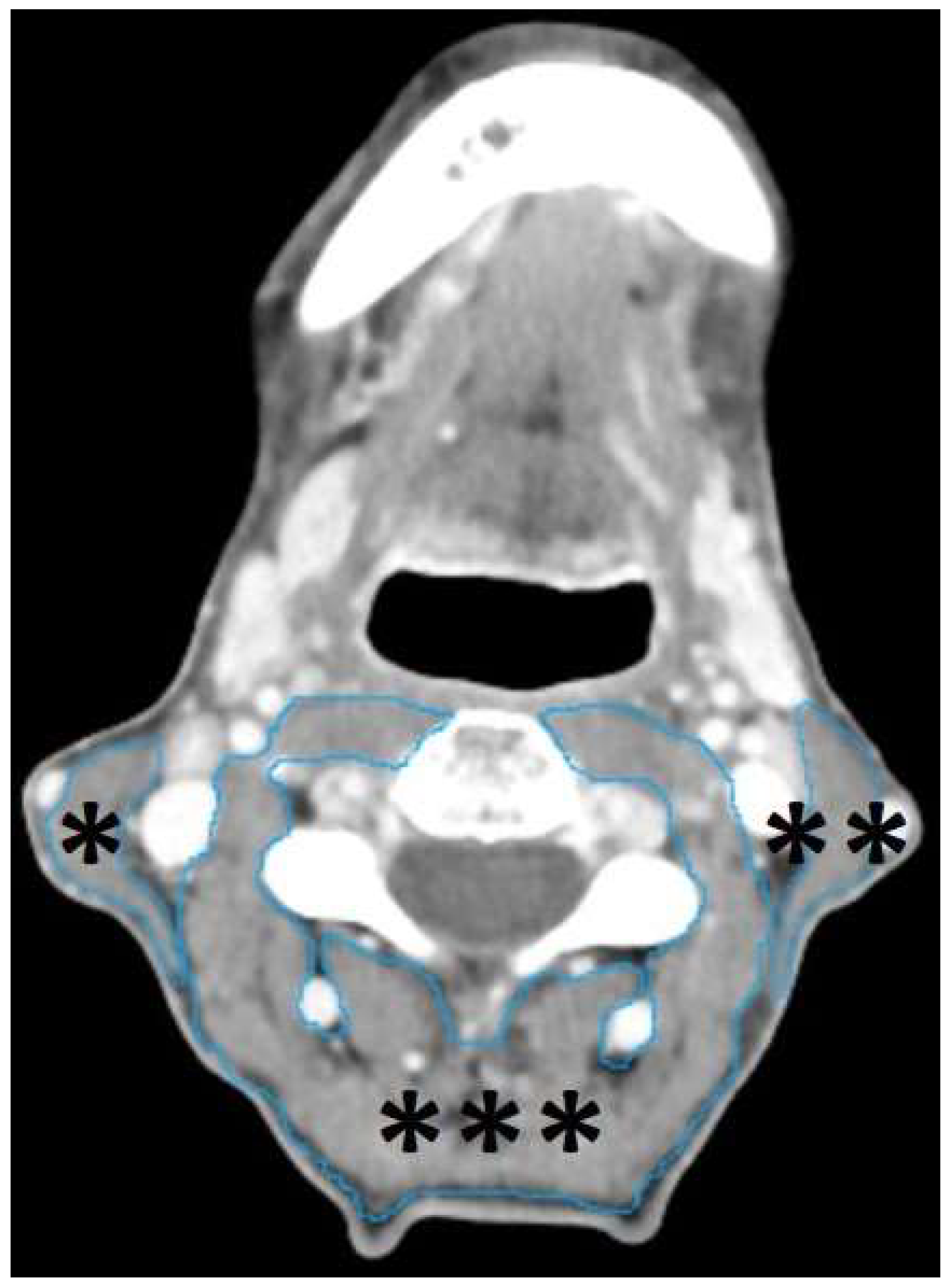
2.4. Segmentation of head-and-neck musculature
2.5. Data analysis
| Radiomic key features | Individual radiomic features |
|---|---|
| Shape features | Short axis diameter1 Long axis diameter1 Volume2 |
| Texture features3 | Entropy Uniformity |
| Intensity features3 | Maximal density Minimal density Mean density Skewness of density Standard deviation of density MPP Uniformity of distribution of positive pixels (UPP) Kurtosis |
2.6. Ethical considerations
3. Results
3.1. Patient population
| Number | Percentages | ||
|---|---|---|---|
| Sex | Male | 73 | 74.5% |
| Female | 25 | 25.5% | |
| Age | ≤50 | 11 | 11.2% |
| 51-60 | 35 | 35.7% | |
| 61-70 | 33 | 33.7% | |
| ≥71 | 19 | 19.4% | |
| Tumor site | Oral cavity | 13 | 13.3% |
| Oropharynx | 46 | 46.9% | |
| Hypopharynx | 20 | 20.4% | |
| Larynx | 15 | 15.3% | |
| Others | 4 | 4.1% | |
| UICC1 truncated | Stage III | 19 | 19.4% |
| Stage IV | 79 | 80.6% | |
| ASA | ASA I/II | 45 | 45.9% |
| ASA III/IV | 53 | 54.1% | |
| Alcohol consumption | < daily | 52 | 53.1% |
| daily | 46 | 46.9% | |
| Smoking habits | < 10 PY | 24 | 24.5% |
| ≥ 10 PY | 74 | 75.5% | |
| BMI-classified | Underweight | 7 | 8.9% |
| Normal weight | 41 | 51.9% | |
| Overweight | 25 | 31.6% | |
| Adipose | 6 | 7.6% | |
| Radiation dose1 | ≤60 Gy | 26 | 26.5% |
| >60 Gy | 72 | 73.5% |
3.2. Primary radiochemotherapy and time intervals
3.3. Variable reduction (principal component analysis)
3.4. Factors influencing pretherapeutic Volume, uniformity and MPP
3.5. Volume, uniformity and MPP before and after therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix
| N | Minimum | Maximum | Mean | Standard deviation | |
| SCMright_Short_Axis | 98 | 4.7 | 24.3 | 14.251 | 3.4045 |
| SCMright_Long_Axis | 98 | 19.5 | 60.9 | 42.026 | 7.5338 |
| SCMright_Volume | 98 | 3.3 | 17.8 | 8.971 | 3.1417 |
| SCMright_Entropy | 98 | 5.5 | 7.3 | 6.489 | 0.3232 |
| SCMright_Kurtosis | 98 | 3.1 | 24.4 | 6.557 | 2.7009 |
| SCMright_MPP | 98 | 31.6 | 79.2 | 59.880 | 8.3491 |
| SCMright_Density_Max. | 98 | 72 | 234 | 137.21 | 36.768 |
| SCMright_Density_Min. | 98 | -155 | -66 | -105.32 | 17.386 |
| SCMright_Density_Mean | 98 | 23.8 | 77.5 | 51.176 | 10.9033 |
| SCMright_Density_Skewness | 98 | -3.0 | -1.0 | -1.75 | 0.373 |
| SCMright_Density_SD | 98 | 13.9 | 45.3 | 32.183 | 5.9952 |
| SCMright_UPP | 98 | 0.0076 | 0.0298 | 0.016484 | 0.0041614 |
| SCMright_Uniformity | 98 | 0.0078 | 0.0298 | 0.016621 | 0.0040749 |
| SCMleft_Short_Axis | 98 | 5.0 | 27.7 | 14.547 | 3.7930 |
| SCMleft_Long_Axis | 98 | 23.8 | 57.5 | 42.623 | 7.6126 |
| SCMleft_Volume | 98 | 2.9 | 15.7 | 8.930 | 3.0336 |
| SCMleft_Entropy | 98 | 5.5 | 7.3 | 6.494 | 0.3395 |
| SCMleft_Kurtosis | 98 | 2.0 | 14.6 | 6.262 | 2.0012 |
| SCMleft_MPP | 98 | 37.1 | 86.0 | 59.344 | 8.4566 |
| SCMleft_Density M_Axis | 98 | 73 | 200 | 138.57 | 28.363 |
| SCMleft_Density_Min. | 98 | -178 | -48 | -105.65 | 18.427 |
| SCMleft_Density_Mean | 98 | 23.6 | 78.6 | 50.546 | 10.9604 |
| SCMleft_Density_Skewness | 98 | -3.4 | -0.8 | -1.717 | 0.4310 |
| SCMleft_Density SD | 98 | 14.1 | 47.9 | 32.052 | 6.5302 |
| SCMleft_UPP | 98 | 0.0075 | 0.0291 | 0.016344 | 0.0043101 |
| SCMleft_Uniformity | 98 | 0.0078 | 0.0291 | 0.016514 | 0.0042213 |
| PVM_Short_Axig | 98 | 43.7 | 88.9 | 66.209 | 10.0206 |
| PVM_Long _Axis | 98 | 63.3 | 176.3 | 100.281 | 18.8547 |
| PVM_Volume | 98 | 34.4 | 183.9 | 96.452 | 30.1608 |
| PVM_Entropy | 98 | 5.9675 | 7.5142 | 6.959589 | 0.2929190 |
| PVM_Kurtosis | 98 | 1.20 | 32.40 | 7.1407 | 4.72660 |
| PVM_MPP | 98 | 34.9 | 77.2 | 56.324 | 8.6289 |
| PVM_Density_Max. | 98 | 220.0 | 1278.0 | 520.678 | 211.4958 |
| PVM_Density Min. | 98 | -198 | -86 | -127.35 | 19.423 |
| PVM_Density_Mean | 98 | 11.9 | 70.0 | 43.765 | 12.7727 |
| PVM_Density_Skewness | 98 | -2.1 | 3.0 | -0.735 | 0.8544 |
| PVM_Density_SD | 98 | 20.1 | 61.8 | 39.053 | 7.0062 |
| PVM_UPP | 98 | 0.0057 | 0.0235 | 0.011340 | 0.0032782 |
| PVM_Uniformity | 98 | 0.0067 | 0.0235 | 0.011584 | 0.0030456 |
| SCM-rad_Volume | 98 | 3.30 | 17.80 | 8.9992 | 3.15632 |
| SCM-rad_Entropyopy | 98 | 5.45 | 7.28 | 6.4731 | 0.33946 |
| SCM-rad_MPP | 98 | 31.60 | 86.00 | 60.1269 | 8.70200 |
| SCM-rad_Density Mean | 98 | 23.60 | 78.60 | 51.9051 | 11.08669 |
| SCM-rad_Uniformity | 98 | 0.01 | 0.03 | 0.0168 | 0.00425 |
| Short _Axis | Long _Axis | Volume | Entropy | Kurtosis | MPP | Density_Max. | Density_Min. | Density_Mean | Density_Skewness | Density_SD | UPP | Uniformity | |
| Short _Axis | 1.00 | 0.11 | 0.45 | -0.12 | 0.12 | 0.06 | 0.00 | 0.04 | 0.13 | -0.12 | -0.16 | 0.10 | 0.09 |
| Long _Axis | 0.11 | 1.00 | 0.72 | -0.09 | 0.12 | -0.03 | 0.04 | -0.04 | 0.01 | -0.13 | -0.07 | 0.10 | 0.10 |
| Volume | 0.45 | 0.72 | 1.00 | -0.12 | 0.13 | -0.06 | -0.03 | -0.07 | -0.01 | -0.16 | -0.12 | 0.12 | 0.11 |
| Entropy | -0.12 | -0.09 | -0.12 | 1.00 | -0.72 | -0.04 | 0.28 | -0.58 | -0.37 | 0.70 | 0.87 | -0.96 | -0.96 |
| Kurtosis | 0.12 | 0.12 | 0.13 | -0.72 | 1.00 | 0.27 | 0.02 | 0.18 | 0.46 | -0.76 | -0.57 | 0.75 | 0.75 |
| MPP | 0.06 | -0.03 | -0.06 | -0.04 | 0.27 | 1.00 | 0.35 | 0.22 | 0.90 | -0.11 | 0.06 | 0.12 | 0.11 |
| Density M _Axis | 0.00 | 0.04 | -0.03 | 0.28 | 0.02 | 0.35 | 1.00 | -0.13 | 0.27 | 0.24 | 0.18 | -0.25 | -0.25 |
| Density Min | 0.04 | -0.04 | -0.07 | -0.58 | 0.18 | 0.22 | -0.13 | 1.00 | 0.47 | -0.01 | -0.68 | 0.48 | 0.47 |
| Density Mean | 0.13 | 0.01 | -0.01 | -0.37 | 0.46 | 0.90 | 0.27 | 0.47 | 1.00 | -0.25 | -0.35 | 0.38 | 0.36 |
| Density Skew | -0.12 | -0.13 | -0.16 | 0.70 | -0.76 | -0.11 | 0.24 | -0.01 | -0.25 | 1.00 | 0.40 | -0.76 | -0.76 |
| Density STD | -0.16 | -0.07 | -0.12 | 0.87 | -0.57 | 0.06 | 0.18 | -0.68 | -0.35 | 0.40 | 1.00 | -0.73 | -0.72 |
| UPP | 0.10 | 0.10 | 0.12 | -0.96 | 0.75 | 0.12 | -0.25 | 0.48 | 0.38 | -0.76 | -0.73 | 1.00 | 1.00 |
| Uniformity | 0.09 | 0.10 | 0.11 | -0.96 | 0.75 | 0.11 | -0.25 | 0.47 | 0.36 | -0.76 | -0.72 | 1.00 | 1.00 |
| Component | Sums of Squared Loadings | % of Variance | Cumulative % |
| Uniformity | 5.3 | 40.8 | 40.8 |
| Intensity | 2.2 | 16.6 | 57.4 |
| Dimension | 2.0 | 15.2 | 72.6 |
| Factor loadings | Uniformity | Intensity | Dimension |
| Entropy | -0.99 | ||
| UPP | 0.97 | ||
| Uniformity | 0.97 | ||
| Density SD | -0.84 | ||
| Kurtosis | 0.77 | ||
| Density Skewness | -0.74 | ||
| Density Min. | 0.57 | ||
| MPP | 0.94 | ||
| Density Mean | 0.41 | 0.88 | |
| Density Max. | -0.31 | 0.62 | |
| Volume | 0.93 | ||
| Long_Axis | 0.82 | ||
| Short_Axis | 0.54 |
| Dimension-Factor | Uniformity-Factor | Intensity-Factor | Original Volume | Original Uniformity | Original Intensity (MPP) | ||
| Dimension-Factor | r | 1 | 0.08 | 0.017 | 0.937 | 0.165 | 0.018 |
| p | 0.435 | 0.865 | 0.001 | 0.104 | 0.858 | ||
| Uniformity-Factor | r | 1 | 0.268 | 0.075 | 0.966 | 0.317 | |
| p | 0.008 | 0.462 | 0.001 | 0.001 | |||
| Intensity-Factor | r | 1 | -0.074 | 0.228 | 0.963 | ||
| p | 0.468 | 0.024 | 0.001 | ||||
| Original Volume | r | 1 | 0.155 | -0.057 | |||
| p | 0.127 | 0.575 | |||||
| Original Uniformity | r | 1 | 0.284 | ||||
| p | 0.005 | ||||||
| Original Intensity | r | 1 | |||||
| (MPP) | p |
References
- Chow, L.Q.M. Head and Neck Cancer. N Engl J Med. 2020, 382, 60–72. [Google Scholar] [CrossRef]
- Machiels JP; René Leemans C; Golusinski W; Grau C; Licitra L; Gregoire V. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020, 31, 1462–1475. [Google Scholar] [CrossRef]
- Kanno Y; Chen CY; Lee HL; Chiou JF; Chen YJ. Molecular Mechanisms of Chemotherapy Resistance in Head and Neck Cancers. Front Oncol. 2021, 11, 640392. [Google Scholar] [CrossRef] [PubMed]
- Maloney SM; Hoover CA; Morejon-Lasso LV; Prosperi JR. Mechanisms of Taxane Resistance. Cancers (Basel). 2020, 12, 3323. [Google Scholar] [CrossRef]
- Alterio D; Marvaso G; Ferrari A; Volpe S; Orecchia R; Jereczek-Fossa BA. Modern radiotherapy for head and neck cancer. Semin Oncol. 2019, 46, 233–245. [Google Scholar] [CrossRef] [PubMed]
- De Ruysscher D; Niedermann G; Burnet NG; Siva S; Lee AWM; Hegi-Johnson F. Radiotherapy toxicity. Nat Rev Dis Primers. 2019, 5, 13. [Google Scholar] [CrossRef]
- Gujral DM; Nutting CM. Patterns of failure, treatment outcomes and late toxicities of head and neck cancer in the current era of IMRT. Oral Oncol. 2018, 86, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Coppes RP; van der Goot A; Lombaert IM. Stem cell therapy to reduce radiation-induced normal tissue damage. Semin Radiat Oncol. 2009, 19, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Kuhmann C; Weichenhan D; Rehli M; Plass C; Schmezer P; Popanda O. DNA methylation changes in cells regrowing after fractioned ionizing radiation. Radiother Oncol. 2011, 101, 116–121. [Google Scholar] [CrossRef]
- Mothersill C; Seymour C. Are epigenetic mechanisms involved in radiation-induced bystander effects? Front Genet. 2012, 3, 74. [Google Scholar] [CrossRef]
- Stone HB; Coleman CN; Anscher MS; McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003, 4, 529–536. [Google Scholar] [CrossRef]
- Yarnold J; Brotons MC. Pathogenetic mechanisms in radiation fibrosis. Radiother Oncol. 2010, 97, 149–161. [Google Scholar] [CrossRef]
- Zhou Y; Sheng X; Deng F; Wang H; Shen L; Zeng Y; Ni Q; Zhan S; Zhou X. Radiation-induced muscle fibrosis rat model: establishment and valuation. Radiat Oncol. 2018, 13, 160. [Google Scholar] [CrossRef]
- Baudelet M; Van den Steen L; Tomassen P; Bonte K; Deron P; Huvenne W; Rottey S; De Neve W; Sundahl N; Van Nuffelen G; Duprez F. Very late xerostomia, dysphagia, and neck fibrosis after head and neck radiotherapy. Head Neck. 2019, 41, 3594–3603. [CrossRef] [PubMed]
- Cox JD; Stetz J; Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef]
- Offiah C; Hall E. Post-treatment imaging appearances in head and neck cancer patients. Clin Radiol. 2011, 66, 13–24. [Google Scholar] [CrossRef]
- Saito N; Nadgir RN; Nakahira M; Takahashi M; Uchino A; Kimura F; Truong MT; Sakai O. Posttreatment CT and MR imaging in head and neck cancer: what the radiologist needs to know. Radiographics. 2012, 32, 1261–1282. [Google Scholar] [CrossRef]
- Wen X; Yu X; Cheng W; Li Y; Tian J. Quantitative Evaluation of Shear Wave Elastography on Radiation-Induced Neck Fibrosis in Patients With Nasopharyngeal Carcinoma. Ultrasound Q. 2019, 37, 178–182. [Google Scholar] [CrossRef]
- Bardosi ZR; Dejaco D; Santer M; Kloppenburg M; Mangesius S; Widmann G; Ganswindt U; Rumpold G; Riechelmann H; Freysinger W. Benchmarking Eliminative Radiomic Feature Selection for Head and Neck Lymph Node Classification. Cancers (Basel). 2022, 14, 477. [Google Scholar] [CrossRef] [PubMed]
- Gillies RJ; Kinahan PE; Hricak H. Radiomics: Images Are More than Pictures, They Are Data. Radiology. 2016, 278, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Ridner SH; Dietrich MS; Niermann K; Cmelak A; Mannion K; Murphy B. A Prospective Study of the Lymphedema and Fibrosis Continuum in Patients with Head and Neck Cancer. Lymphat Res Biol. 2016, 14, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Steinbichler TB; Golm L; Dejaco D; Riedl D; Kofler B; Url C; Wolfram D; Riechelmann H. Surgical rescue for persistent head and neck cancer after first-line treatment. Eur Arch Otorhinolaryngol. 2020, 277, 1437–1448. [Google Scholar] [CrossRef] [PubMed]
- Steinbichler TB; Lichtenecker M; Anegg M; Dejaco D; Kofler B; Schartinger VH; Kasseroler MT; Forthuber B; Posch A; Riechelmann H. Persistent Head and Neck Cancer Following First-Line Treatment. Cancers (Basel). 2018, 10, 421. [Google Scholar] [CrossRef] [PubMed]
- Boyd TS; Harari PM; Tannehill SP; Voytovich MC; Hartig GK; Ford CN; Foote RL; Campbell BH; Schultz CJ. Planned postradiotherapy neck dissection in patients with advanced head and neck cancer. Head Neck. 1998, 20, 132–137. [Google Scholar] [CrossRef]
- Denaro N; Russi EG; Numico G; Pazzaia T; Vitiello R; Merlano MC. The role of neck dissection after radical chemoradiation for locally advanced head and neck cancer: should we move back? Oncology. 2013, 84, 174–185. [Google Scholar] [CrossRef]
- Stenson KM; Haraf DJ; Pelzer H; Recant W; Kies MS; Weichselbaum RR; Vokes EE. The role of cervical lymphadenectomy after aggressive concomitant chemoradiotherapy: the feasibility of selective neck dissection. Arch Otolaryngol Head Neck Surg. 2000, 126, 950–956. [Google Scholar] [CrossRef]
- Lango MN; Andrews GA; Ahmad S; Feigenberg S; Tuluc M; Gaughan J; Ridge JA. Postradiotherapy neck dissection for head and neck squamous cell carcinoma: pattern of pathologic residual carcinoma and prognosis. Head Neck. 2009, 31, 328–337. [CrossRef]
- Moloney EC; Brunner M; Alexander AJ; Clark J. Quantifying fibrosis in head and neck cancer treatment: An overview. Head Neck. 2015, 37, 1225–1231. [Google Scholar] [CrossRef]
- Bourgier C; Auperin A; Rivera S; Boisselier P; Petit B; Lang P; Lassau N; Taourel P; Tetreau R; Azria D; Bourhis J; Deutsch E; Vozenin MC. Pravastatin Reverses Established Radiation-Induced Cutaneous and Subcutaneous Fibrosis in Patients With Head and Neck Cancer: Results of the Biology-Driven Phase 2 Clinical Trial Pravacur. Int J Radiat Oncol Biol Phys. 2019, 104, 365–373. [Google Scholar] [CrossRef]
- von Elm E; Altman DG; Egger M; Pocock SJ; Gøtzsche PC; Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef]
- Bossuyt PM; Reitsma JB; Bruns DE; Gatsonis CA; Glasziou PP; Irwig L; Lijmer JG; Moher D; Rennie D; de Vet HC; Kressel HY; Rifai N; Golub RM; Altman DG; Hooft L; Korevaar DA; Cohen JF. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Bmj. 2015, 351, h5527. [Google Scholar] [CrossRef]
- Swartz JE; Pothen AJ; Wegner I; Smid EJ; Swart KM; de Bree R; Leenen LP; Grolman W. Feasibility of using head and neck CT imaging to assess skeletal muscle mass in head and neck cancer patients. Oral Oncol. 2016, 62, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Zigon G; Berrino F; Gatta G; Sánchez MJ; van Dijk B; Van Eycken E; Francisci S. Prognoses for head and neck cancers in Europe diagnosed in 1995-1999: a population-based study. Ann Oncol. 2011, 22, 165–174. [Google Scholar] [CrossRef]
- Dejaco D; Steinbichler T; Schartinger VH; Fischer N; Anegg M; Dudas J; Posch A; Widmann G; Riechelmann H. Prognostic value of tumor volume in patients with head and neck squamous cell carcinoma treated with primary surgery. Head Neck. 2018, 40, 728–739. [Google Scholar] [CrossRef]
- Dejaco D; Steinbichler T; Schartinger VH; Fischer N; Anegg M; Dudas J; Posch A; Widmann G; Riechelmann H. Specific growth rates calculated from CTs in patients with head and neck squamous cell carcinoma: a retrospective study performed in Austria. BMJ Open. 2019, 9, e025359. [Google Scholar] [CrossRef] [PubMed]
- Dejaco D; Url C; Schartinger VH; Haug AK; Fischer N; Riedl D; Posch A; Riechelmann H; Widmann G. Approximation of head and neck cancer volumes in contrast enhanced CT. Cancer Imaging. 2015, 15, 16. [Google Scholar] [CrossRef]
- Chamchod S; Fuller CD; Mohamed AS; Grossberg A; Messer JA; Heukelom J; Gunn GB; Kantor ME; Eichelberger H; Garden AS; Rosenthal DI. Quantitative body mass characterization before and after head and neck cancer radiotherapy: A challenge of height-weight formulae using computed tomography measurement. Oral Oncol. 2016, 61, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Choi Y; Ahn KJ; Jang J; Shin NY; Jung SL; Kim BS; Kim MS; Kim YS. Prognostic value of computed tomography-based volumetric body composition analysis in patients with head and neck cancer: Feasibility study. Head Neck. 2020, 42, 2614–2625. [Google Scholar] [CrossRef]
- Findlay M; White K; Stapleton N; Bauer J. Is sarcopenia a predictor of prognosis for patients undergoing radiotherapy for head and neck cancer? A meta-analysis. Clin Nutr. 2021, 40, 1711–1718. [Google Scholar] [CrossRef]
- Grossberg AJ; Chamchod S; Fuller CD; Mohamed AS; Heukelom J; Eichelberger H; Kantor ME; Hutcheson KA; Gunn GB; Garden AS; Frank S; Phan J; Beadle B; Skinner HD; Morrison WH; Rosenthal DI. Association of Body Composition With Survival and Locoregional Control of Radiotherapy-Treated Head and Neck Squamous Cell Carcinoma. JAMA Oncol. 2016, 2, 782–789. [Google Scholar] [CrossRef]
- Platek ME; Myrick E; McCloskey SA; Gupta V; Reid ME; Wilding GE; Cohan D; Arshad H; Rigual NR; Hicks WL Jr; Sullivan M; Warren GW; Singh AK. Pretreatment weight status and weight loss among head and neck cancer patients receiving definitive concurrent chemoradiation therapy: implications for nutrition integrated treatment pathways. Support Care Cancer. 2013, 21, 2825–2833. [CrossRef]
- Santer M; Kloppenburg M; Gottfried TM; Runge A; Schmutzhard J; Vorbach SM; Mangesius J; Riedl D; Mangesius S; Widmann G; Riechelmann H; Dejaco D; Freysinger W. Current Applications of Artificial Intelligence to Classify Cervical Lymph Nodes in Patients with Head and Neck Squamous Cell Carcinoma-A Systematic Review. Cancers (Basel). 2022, 14, 5397. [Google Scholar] [CrossRef] [PubMed]
| Mean (days) |
Minimum (days) |
Maximum (days) |
Standard Deviation (days) |
|
|---|---|---|---|---|
| Imaging interval1 | 148 | 108 | 315 | ±33 |
| Restaging interval2 | 55 | 29 | 229 | ±28 |
| Radiomic key features | Staging-CT (SD) |
Restaging-CT (SD) |
p-value1 | Cohen’s d2 |
|---|---|---|---|---|
| SCM-Volume (ml) | 9.00 (±3.2) | 8.4 (±2.7) | 0.007 | 0.28 |
| SCM-MPP (HU) | 60.1 (±8.7) | 59.7 (±8.1) | 0.664 | 0.04 |
| SCM-Uniformity* | 16.8 (±4.3) | 16.4 (±4.1) | 0.342 | 0.10 |
| PVM –Volume (ml) | 96.5 (±30.2) | 91.9 (±25.8) | 0.007 | 0.28 |
| PVM –MPP (HU) | 56.3 (±8.6) | 58.0 (±8.6) | 0.061 | -0.19 |
| PVM –Uniformity* | 11.6 (±3.1) | 12.0 (±2.8) | 0.058 | -0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





