Submitted:
01 September 2023
Posted:
04 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
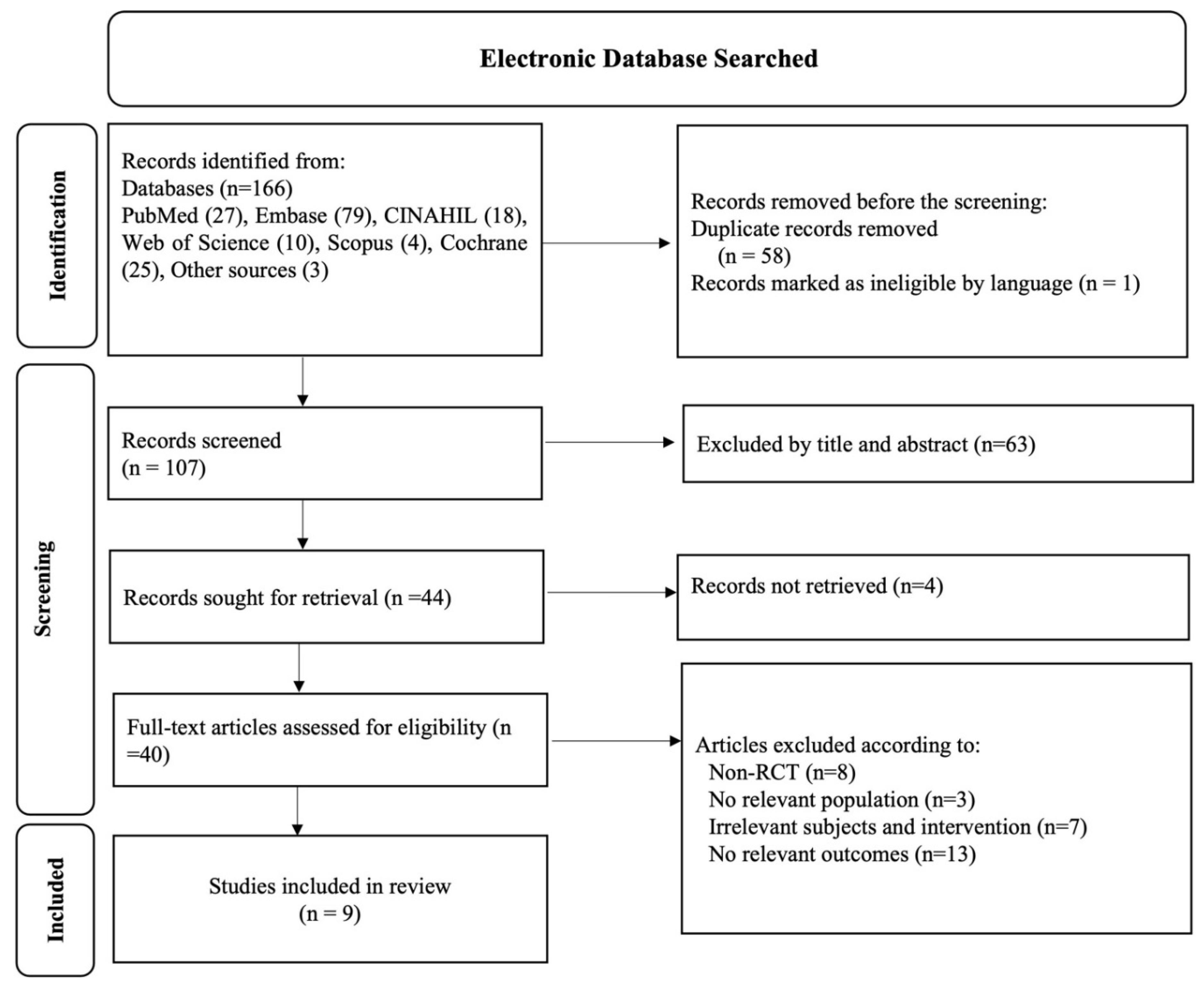
2. Materials and Methods
2.1. Study Participants
2.2. Type of Intervention and Control
2.3. Study Search and Selection
2.4. Outcome Measures
2.5. Data Extraction
3. Results
3.1. Selected Studies
3.2. The effect of omega-3 fatty acids on vasomotor symptoms
3.2. The effect of omega-3 fatty acids on sleep quality
3.4. The effect of omega-3 fatty acids on depression
3.5. Other Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgment
Conflict of Interest
References
- Dalal, P.K.; Agarwal, M. Postmenopausal syndrome. Indian J. Psychiatry 2015, 57, S222. [Google Scholar] [CrossRef] [PubMed]
- Gold, E.B. The timing of the age at which natural menopause occurs. Obstetrics and Gynecology Clinics 2011, 38, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.D.; Haney, E.M.; Humphrey, L.; Miller, J.; Nedrow, A.; Nicolaidis, C.; Vesco, K.K.; Walker, M.; Bougatsos, C.; Nygren, P. Management of menopause-related symptoms. Agency for Healthcare Research and Quality Publication 2005. [Google Scholar]
- Noll, P.R.E.S.; Nascimento, M.G.; Bayer, L.H.C.M.; Zangirolami-Raimundo, J.; Turri, J.A.O.; Noll, M.; Baracat, E.C.; Soares Junior, J.M.; Sorpreso, I.C.E. Changes in Food Consumption in Postmenopausal Women during the COVID-19 Pandemic: A Longitudinal Study. Nutrients 2023, 15, 3494. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C. Epidemiology of women and depression. J. Affect. Disord. 2003, 74, 5–13. [Google Scholar] [CrossRef]
- Kułak-Bejda, A.; Krajewska-Ferishah, K.; Szyszko-Perłowska, A.; Waszkiewicz, N. Risk Assessment of Depression amongst Women during Menopause before and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 20. [Google Scholar] [CrossRef]
- O’Neill, S.; Eden, J. The pathophysiology of menopausal symptoms. Obstetrics, Gynaecology & Reproductive Medicine 2017, 27, 303–310. [Google Scholar]
- Clayton, A.H.; Ninan, P.T. Depression or menopause? Presentation and management of major depressive disorder in perimenopausal and postmenopausal women. Prim. Care Companion J. Clin. Psychiatry 2010, 12, PCC–08r00747. [Google Scholar] [CrossRef]
- Giannini, A.; Caretto, M.; Genazzani, A.R.; Simoncini, T. Neuroendocrine Changes during Menopausal Transition. Endocrines 2021, 2, 405–416. [Google Scholar] [CrossRef]
- Weber, M.T.; Maki, P.M.; McDermott, M.P. Cognition and mood in perimenopause: A systematic review and meta-analysis. The Journal of Steroid Biochemistry and Molecular Biology 2014, 142, 90–98. [Google Scholar] [CrossRef]
- Mehta, J.; Kling, J.M.; Manson, J.E. Risks, Benefits, and Treatment Modalities of Menopausal Hormone Therapy: Current Concepts. Front. Endocrinol. (Lausanne) 2021, 12, 564781. [Google Scholar] [CrossRef] [PubMed]
- Zailani, H.; Satyanarayanan, S.K.; Liao, W.C.; Liao, H.F.; Huang, S.Y.; Gałecki, P.; Su, K.P.; Chang, J.P. Omega-3 Polyunsaturated Fatty Acids in Managing Comorbid Mood Disorders in Chronic Obstructive Pulmonary Disease (COPD): A Review. J Clin Med 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Thompson, R.L.; Harrison, R.A.; Summerbell, C.D.; Ness, A.R.; Moore, H.J.; Worthington, H.V.; Durrington, P.N.; Higgins, J.P.; Capps, N.E. Risks and benefits of omega 3 fats for mortality, cardiovascular disease, and cancer: systematic review. BMJ 2006, 332, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-K.; Chen, W.-J.; Chang, J.P.-C.; Guu, T.-W.; Hsin, M.-C.; Huang, C.-K.; Mischoulon, D.; Capuron, L.; Su, K.-P. Personalized Medicine of Omega-3 Fatty Acids in Depression Treatment in Obese and Metabolically Dysregulated Patients. Journal of Personalized Medicine 2023, 13, 1003. [Google Scholar] [CrossRef]
- Barnes, P.M.; Bloom, B.; Nahin, R.L. Complementary and alternative medicine use among adults and children: United States, 2007. 2008.
- Appleton, K.M.; Hayward, R.C.; Gunnell, D.; Peters, T.J.; Rogers, P.J.; Kessler, D.; Ness, A.R. Effects of n–3 long-chain polyunsaturated fatty acids on depressed mood: systematic review of published trials. The American journal of clinical nutrition 2006, 84, 1308–1316. [Google Scholar] [CrossRef]
- Chae, M.; Park, K. Association between dietary omega-3 fatty acid intake and depression in postmenopausal women. Nutr. Res. Pract. 2021, 15, 468. [Google Scholar] [CrossRef]
- Hibbeln, J.R.; Linnoila, M.; Umhau, J.C.; Rawlings, R.; George, D.T.; Salem Jr, N. Essential fatty acids predict metabolites of serotonin and dopamine in cerebrospinal fluid among healthy control subjects, and early-and late-onset alcoholics. Biol. Psychiatry 1998, 44, 235–242. [Google Scholar] [CrossRef]
- Carlezon Jr, W.A.; Mague, S.D.; Parow, A.M.; Stoll, A.L.; Cohen, B.M.; Renshaw, P.F. Antidepressant-like effects of uridine and omega-3 fatty acids are potentiated by combined treatment in rats. Biol. Psychiatry 2005, 57, 343–350. [Google Scholar] [CrossRef]
- Ciappolino, V.; Mazzocchi, A.; Enrico, P.; Syrén, M.-L.; Delvecchio, G.; Agostoni, C.; Brambilla, P. N-3 Polyunsatured Fatty Acids in Menopausal Transition: A Systematic Review of Depressive and Cognitive Disorders with Accompanying Vasomotor Symptoms. Int. J. Mol. Sci. 2018, 19, 1849. [Google Scholar] [CrossRef]
- Lucas, M.; Asselin, G.; Mérette, C.; Poulin, M.-J.; Dodin, S. Effects of ethyl-eicosapentaenoic acid omega-3 fatty acid supplementation on hot flashes and quality of life among middle-aged women: a double-blind, placebo-controlled, randomized clinical trial. Menopause 2009, 16, 357–366. [Google Scholar] [CrossRef]
- Cohen, L.S.; Joffe, H.; Guthrie, K.A.; Ensrud, K.E.; Freeman, M.; Carpenter, J.S.; Learman, L.A.; Newton, K.M.; Reed, S.D.; Manson, J.E.; et al. Efficacy of omega-3 for vasomotor symptoms treatment: a randomized controlled trial. Menopause (New York, N.Y.) 2014, 21, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Grigolon, R.B.; Ceolin, G.; Deng, Y.; Bambokian, A.; Koning, E.; Fabe, J.; Lima, M.; Gerchman, F.; Soares, C.N.; Brietzke, E.; et al. Effects of nutritional interventions on the severity of depressive and anxiety symptoms of women in the menopausal transition and menopause: a systematic review, meta-analysis, and meta-regression. Menopause 2023, 30, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Joffe, H.; Crawford, S.L.; Freeman, M.P.; White, D.P.; Bianchi, M.T.; Kim, S.; Economou, N.; Camuso, J.; Hall, J.E.; Cohen, L.S. Independent Contributions of Nocturnal Hot Flashes and Sleep Disturbance to Depression in Estrogen-Deprived Women. J Clin Endocrinol Metab 2016, 101, 3847–3855. [Google Scholar] [CrossRef] [PubMed]
- Lucas, M.; Asselin, G.; Mérette, C.; Poulin, M.-J.; Dodin, S. Ethyl-eicosapentaenoic acid for the treatment of psychological distress and depressive symptoms in middle-aged women: a double-blind, placebo-controlled, randomized clinical trial2. The American Journal of Clinical Nutrition 2009, 89, 641–651. [Google Scholar] [CrossRef]
- Freeman, M.P.; Hibbeln, J.R.; Silver, M.; Hirschberg, A.M.; Wang, B.; Yule, A.M.; Petrillo, L.F.; Pascuillo, E.; Economou, N.I.; Joffe, H.; et al. Omega-3 fatty acids for major depressive disorder associated with the menopausal transition: a preliminary open trial. Menopause 2011, 18, 279–284. [Google Scholar] [CrossRef]
- Patrick, R.P.; Ames, B.N. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: Relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. The FASEB Journal 2015, 29, 2207–2222. [Google Scholar] [CrossRef]
- Reed, S.D.; Guthrie, K.A.; Newton, K.M.; Anderson, G.L.; Booth-LaForce, C.; Caan, B.; Carpenter, J.S.; Cohen, L.S.; Dunn, A.L.; Ensrud, K.E.; et al. Menopausal quality of life: RCT of yoga, exercise, and omega-3 supplements. Am. J. Obstet. Gynecol. 2014, 210, 244.e241-211. [Google Scholar] [CrossRef]
- Palacios, S.; Lilue, M.; Mejia, A.; Menendez, C. Omega-3 versus isoflavones in the control of vasomotor symptoms in postmenopausal women. Gynecol. Endocrinol. 2017, 33, 951–957. [Google Scholar] [CrossRef]
- Purzand, B.; Rokhgireh, S.; Shabani Zanjani, M.; Eshraghi, N.; Mohamadianamiri, M.; Esmailzadeh, A.; Alkatout, I.; Gitas, G.; Allahqoli, L. The comparison of the effect of soybean and fish oil on supplementation on menopausal symptoms in postmenopausal women: A randomized, double-blind, placebo-controlled trial. Complement. Ther. Clin. Pract. 2020, 41, 101239. [Google Scholar] [CrossRef]
- G. Ozgoli, R.M., B.Molaei, M. Hajifaraji, H. Soori, S.Najafi. Effect of Eicosapentaenoic acid (EPA) and Docosahexaenoic acid (DHA) Supplementation on Hot Flashes in Menopausal Women: A Randomized, Double - Blind, Placebo- Controlled Clinical Trial. New York Science Journal 2014, 7, 37–42. [Google Scholar]
- Masoumi, S.Z.; Kazemi, F.; Tavakolian, S.; Rahimi, A.; Oshvandi, K.; Soltanian, A.; Shobeiri, F. Effect of citalopram in combination with omega-3 on depression in post-menopausal women: A triple blind randomized controlled trial. Journal of Clinical and Diagnostic Research 2016, 10, QC01–QC05. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, K.A.; Larson, J.C.; Ensrud, K.E.; Anderson, G.L.; Carpenter, J.S.; Freeman, E.W.; Joffe, H.; LaCroix, A.Z.; Manson, J.E.; Morin, C.M.; et al. Effects of Pharmacologic and Nonpharmacologic Interventions on Insomnia Symptoms and Self-reported Sleep Quality in Women With Hot Flashes: A Pooled Analysis of Individual Participant Data From Four MsFLASH Trials. Sleep 2018, 41. [Google Scholar] [CrossRef] [PubMed]
- Freedman, R.R.; Norton, D.; Woodward, S.; Cornélissen, G. Core body temperature and circadian rhythm of hot flashes in menopausal women. J Clin Endocrinol Metab 1995, 80, 2354–2358. [Google Scholar] [CrossRef] [PubMed]
- Rotolo, O.; Zinzi, I.; Veronese, N.; Cisternino, A.M.; Reddavide, R.; Inguaggiato, R.; Leandro, G.; Notarnicola, M.; Tutino, V.; De Nunzio, V.; et al. Women in LOVe: Lacto-Ovo-Vegetarian Diet Rich in Omega-3 Improves Vasomotor Symptoms in Postmenopausal Women. An Exploratory Randomized Controlled Trial. Endocr. Metab. Immune Disord. Drug Targets 2019, 19, 1232–1239. [Google Scholar] [CrossRef]
- Cohen, L.S.; Joffe, H.; Guthrie, K.A.; Ensrud, K.E.; Freeman, M.; Carpenter, J.S.; Learman, L.A.; Newton, K.M.; Reed, S.D.; Manson, J.E.; et al. Efficacy of omega-3 for vasomotor symptoms treatment: A randomized controlled trial. Menopause 2014, 21, 347–354. [Google Scholar] [CrossRef]
- Shaver, J.L.; Woods, N.F. Sleep and menopause: a narrative review. Menopause 2015, 22, 899–915. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Stone, K.L.; Blackwell, T.L.; Sawaya, G.F.; Tagliaferri, M.; Diem, S.J.; Grady, D. Frequency and severity of hot flashes and sleep disturbance in postmenopausal women with hot flashes. Menopause 2009, 16, 286–292. [Google Scholar] [CrossRef]
- Ohayon, M.M. Severe hot flashes are associated with chronic insomnia. Arch. Intern. Med. 2006, 166, 1262–1268. [Google Scholar] [CrossRef]
- Jahangard, L.; Sadeghi, A.; Ahmadpanah, M.; Holsboer-Trachsler, E.; Sadeghi Bahmani, D.; Haghighi, M.; Brand, S. Influence of adjuvant omega-3-polyunsaturated fatty acids on depression, sleep, and emotion regulation among outpatients with major depressive disorders - Results from a double-blind, randomized and placebo-controlled clinical trial. J. Psychiatr. Res. 2018, 107, 48–56. [Google Scholar] [CrossRef]
- Yokoi-Shimizu, K.; Yanagimoto, K.; Hayamizu, K. Effect of Docosahexaenoic Acid and Eicosapentaenoic Acid Supplementation on Sleep Quality in Healthy Subjects: A Randomized, Double-Blinded, Placebo-Controlled Trial. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Kessler, R.C.; McGonagle, K.A.; Swartz, M.; Blazer, D.G.; Nelson, C.B. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J. Affect. Disord. 1993, 29, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Judd, F.K.; Hickey, M.; Bryant, C. Depression and midlife: are we overpathologising the menopause? J. Affect. Disord. 2012, 136, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Su, K.P. Nutrition, psychoneuroimmunology and depression: the therapeutic implications of omega-3 fatty acids in interferon-α-induced depression. Biomedicine (Taipei) 2015, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, R.M. Long-term side effects of SSRIs: sexual dysfunction and weight gain. J. Clin. Psychiatry 2003, 64 Suppl 18, 20–24. [Google Scholar]
- Nemets, B.; Stahl, Z.; Belmaker, R.H. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am. J. Psychiatry 2002, 159, 477–479. [Google Scholar] [CrossRef]
- Peet, M.; Horrobin, D.F. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch. Gen. Psychiatry 2002, 59, 913–919. [Google Scholar] [CrossRef]
- Su, K.P.; Huang, S.Y.; Chiu, C.C.; Shen, W.W. Omega-3 fatty acids in major depressive disorder. A preliminary double-blind, placebo-controlled trial. Eur. Neuropsychopharmacol. 2003, 13, 267–271. [Google Scholar] [CrossRef]
- Yang, B.; Lin, L.; Bazinet, Richard P. ; Chien, Y.-C.; Chang, Jane P.-C.; Satyanarayanan, Senthil K.; Su, H.; Su, K.-P. Clinical Efficacy and Biological Regulations of ω–3 PUFA-Derived Endocannabinoids in Major Depressive Disorder. Psychother. Psychosom. 2019, 88, 215–224. [Google Scholar] [CrossRef]
- Matthews, K.A.; Bromberger, J.T. Does the menopausal transition affect health-related quality of life? Am. J. Med. 2005, 118 Suppl 12B, 25–36. [Google Scholar] [CrossRef]
| Authors & Year | Study Design | Participants, No. | Intervention | Duration | Vasomotor Symptoms | Sleep Quality | Depression | Other Outcomes |
|---|---|---|---|---|---|---|---|---|
| [32] | Triple-Blind Randomized Controlled Trial | Menopause women, n=60; Intervention group, n=30; Control group, n=30 |
Intervention group: 20 mg citalopram and 1g of omega-3 PUFAs per day Placebo group: 20 mg citalopram along with a placebo per day |
4 weeks | -------- | -------- | BDI-II (p < 0.001) |
------ |
| [33] | Double-blind placebo-controlled, RCT | Postmenopausal women, n=188 Intervention group, n=; 95 Control group, n= 93 |
Intervention group: 1.8 g omega-3 fatty acids per day Placebo group: 3 capsules per day containing olive oil |
12 weeks | -------- | PSQ-I (0.0933) ISI = (0.729) |
------ | ------ |
| [22] | Double-Blind, Randomized Clinical Trial | Menopause women, n=355; Intervention group, n=177; Placebo group, n=178 |
Intervention group: 615 mg omega-3 PUFAs (EPA= 425 mg, DHA=100 mg) 3 capsules per day Placebo group: 3 capsules per day containing olive oil |
12 weeks | VMS frequency = (p=0.283) | PSQ-I (0.0933) ISI = (0.729) |
PHQ-8 (0.097) GAD-7 = (0.191 ) |
No Adverse Effect |
| [25] | Double-blind placebo-controlled, RCT | Menopause women, n=120; Intervention group, n=59; Placebo group, n=61 |
Intervention group: 500 mg omega-3 PUFAs (EPA= 350 mg and DHA= 50 mg in ethyl esters form) / day Placebo group: 500 mg capsule containing sunflower oil per day 0.2% of regular fish oil (18% EPA/12% DHA) 3 times daily |
8 weeks | ------- | ----- | PGWB (p = 0.034) HSCL-D-20 (p = 0.040) HAM-D-21 (p = 0.030) |
------ |
| [21] | Double-blind placebo-controlled, RCT | Menopause women, n=120; Intervention group, n=59; Placebo group, n=61 |
Intervention group: 500 mg omega-3 PUFAs (EPA= 350 mg and DHA= 50 mg in ethyl esters form) / day Placebo group: 500 mg capsule containing sunflower oil per day 0.2% of regular fish oil (18% EPA/12% DHA) 3 times daily |
8 weeks | HF and night sweats Frequency (p= 0.005) and Intensity (0.64) |
------ | ------- | MENQOL (p=0.2) No Adverse Effect |
| [28] | Randomized control trial | Menopause women, n=355; Intervention group, n=177; Placebo group, n=178 |
Intervention group: Omega-3 supplement contained 425 mg ethyl EPA, 100 mg DHA acid per day Placebo group: 90 mg placebo containing olive oil per day |
12 weeks | VMS frequency = (p=0.06) | PSQ-I (0.0933) ISI = (0.729) PSS = (0.08) |
PHQ-8 (0.097) GAD-7 = (0.191 ) |
MENQOL = (0.12) |
| [29] | Randomized, Prospective, Two-Arm Study | Menopause women, n=76; Omega-3 group, n=40; Isoflavone group, n=36 |
Intervention group: omega-3 PUFAs (425 mg of omega-3/capsule), 2 capsules per day Placebo group: Soybean isoflavones (54.4 mg of isoflavones/ tablet), 2 tablets per day |
16 weeks | VMS Frequency and HF (p < .001) |
----- | ------ | No Adverse Effect |
| [30] | Double-Blind, Placebo-Controlled, Randomized Clinical Trial | Menopause women, n=180; Soy group, n=60; Omega-3 group, n=60; Placebo group, n=60 |
Intervention group: 1000 mg Omega-rex soft gel Soygan 500 mg capsule Placebo group: placebo |
3 months | MRS (p = 0.03) |
----- | ----- | No Adverse Effect |
| [31] | Double-blind, randomized controlled clinical trial | Menopause women, n=68; Omega-3 group, n=38; Control, n=38 |
Intervention group: 300 mg (contain EPA=120 mg and DHA= 180 mg) per day Placebo group: Placebo containing paraffin |
8 weeks | HF frequency (p=0.003) but no intensity (p=0.2) | ----- | ------- | No Adverse Effect |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





