Submitted:
04 September 2023
Posted:
04 September 2023
You are already at the latest version
Abstract
Keywords:
Introduction
The neuroscience of criminal behavior
Schizophrenia as a segmental progeria
Schizophrenia outcome studies - Kraepelin was right!
The molecular basis of SCZ and dementia: Tau protein loss of function
bvFTD: from insight to acquired psychopathy
Neuropathological basis of bvFTD
Dementia in PLWS, potential biomarkers
Chronic Traumatic Encephalopathy
Interventions: receptor-independent antipsychotic treatments (RIATs)
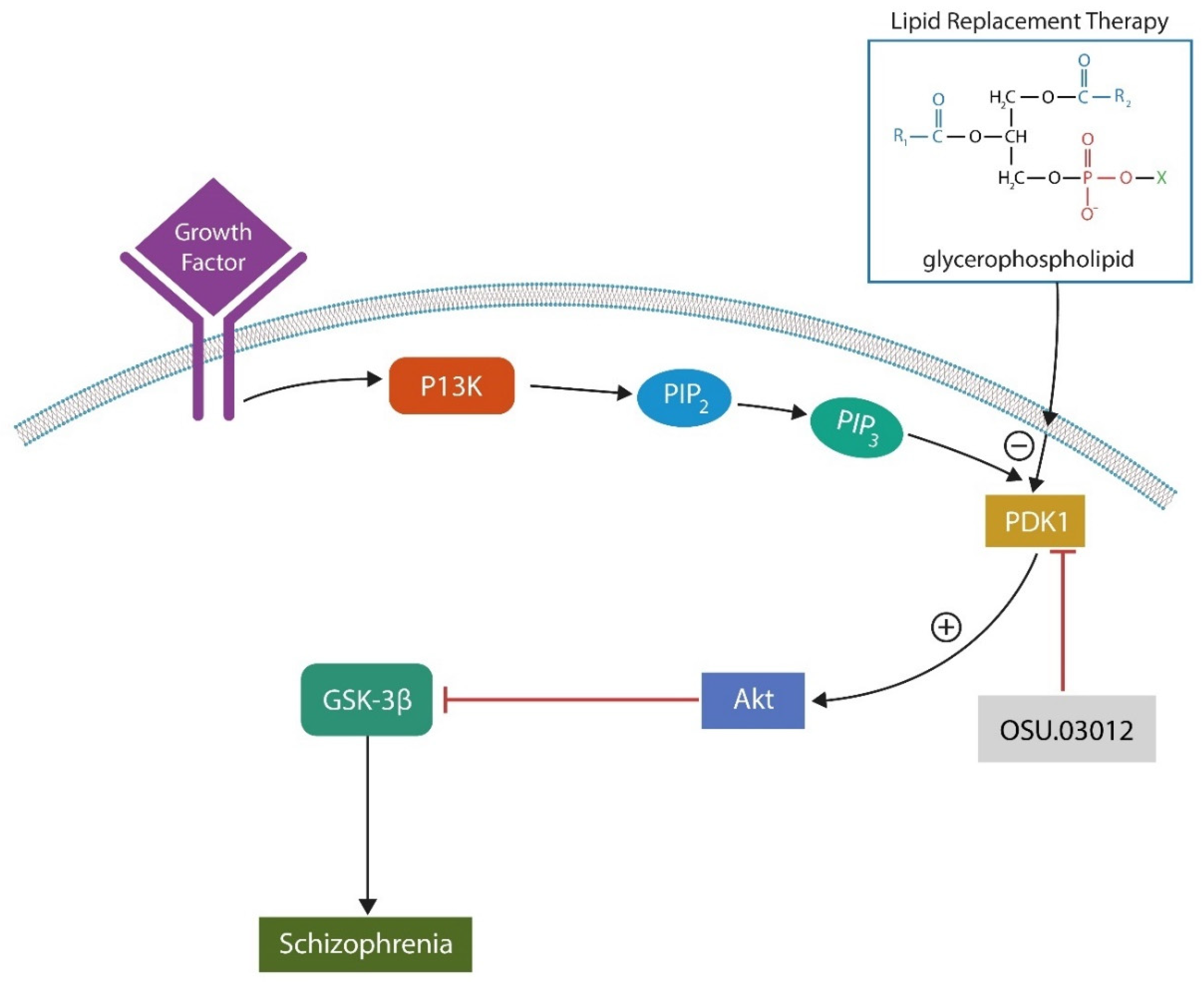
Phosphoinositide-dependent kinase 1 (PDK-1) inhibitors
Recombinant human interleukin-22 (IL-22)
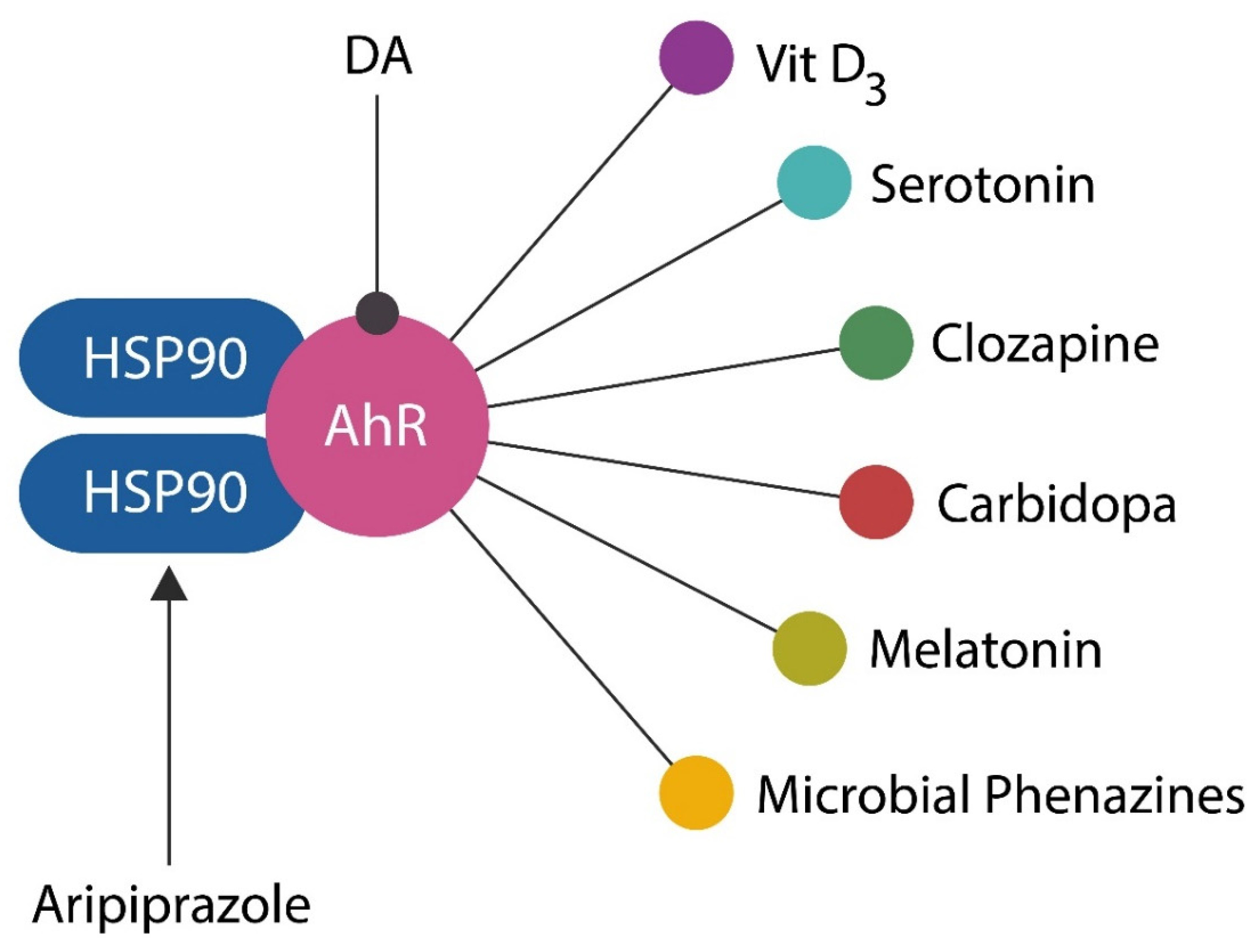
Aryl hydrocarbon receptor (AhR) antagonists
Conclusions
References
- Mendez, M.F. The Neurobiology of Moral Behavior: Review and Neuropsychiatric Implications. CNS Spectrums 2009, 14, 608–620. [Google Scholar] [CrossRef]
- Savopoulos, P.; Lindell, A.K. Born criminal? Differences in structural, functional and behavioural lateralization between criminals and noncriminals. Laterality 2018, 23, 738–760. [Google Scholar] [CrossRef]
- Shapira, J.S.; Saul, R.E.; Guimet, N.M.; Zapata-Restrepo, L.M.; Miller, B.L.; Mendez, M.F.; Moheb, N.; Charuworn, K.; Ashla, B.M.M.; Desarzant, B.R.; et al. The Spectrum of Sociopathy in Dementia. J. Neuropsychiatry 2011, 23, 132–140. [Google Scholar] [CrossRef]
- Lehrer, D.S.; Lorenz, J. Anosognosia in schizophrenia: hidden in plain sight. Innov. Clin. Neurosci. 2014, 11, 10–17. [Google Scholar]
- Räsänen, P.; Tähonen, J.; Isohanni, M.; Rantakallio, P.; Lehtonen, J.; Moring, J. Schizophrenia, Alcohol Abuse, and Violent Behavior: A 26-Year Followup Study of an Unselected Birth Cohort. Schizophr. Bull. 1998, 24, 437–441. [Google Scholar] [CrossRef]
- Polat, H.; Uğur, K.; Aslanoğlu, E.; Yıldız, S.; Yagin, F.H. The effect of functional remission and cognitive insight on criminal behavior in patients with schizophrenia. Arch. Psychiatr. Nurs. 2023, 45, 176–183. [Google Scholar] [CrossRef]
- Lien, Y.-J.; Chang, H.-A.; Kao, Y.-C.; Tzeng, N.-S.; Lu, C.-W.; Loh, C.-H. Insight, self-stigma and psychosocial outcomes in Schizophrenia: a structural equation modelling approach. Epidemiology Psychiatr. Sci. 2016, 27, 176–185. [Google Scholar] [CrossRef]
- Lincoln, T.M.; Hodgins, S. Is Lack of Insight Associated With Physically Aggressive Behavior Among People With Schizophrenia Living in the Community? J. Nerv. Ment. Dis. 2008, 196, 62–66. [Google Scholar] [CrossRef]
- Buckley, P.F.; Hrouda, D.R.; Friedman, L.; Noffsinger, S.G.; Resnick, P.J.; Camlin-Shingler, K. Insight and Its Relationship to Violent Behavior in Patients With Schizophrenia. Am. J. Psychiatry 2004, 161, 1712–1714. [Google Scholar] [CrossRef]
- Zago, S.; Scarpazza, C.; Difonzo, T.; Arighi, A.; Hajhajate, D.; Torrente, Y.; Sartori, G. Behavioral Variant of Frontotemporal Dementia and Homicide in a Historical Case. J Am Acad Psychiatry Law. 2021, 49, 219–227. [Google Scholar] [CrossRef]
- Wander, C. Schizophrenia: opportunities to improve outcomes and reduce economic burden through managed care. The American Journal of Managed Care 2020, 26, S62–S68. [Google Scholar] [CrossRef] [PubMed]
- Dregan, A.; McNeill, A.; Gaughran, F.; Jones, P.B.; Bazley, A.; Cross, S.; Lillywhite, K.; Armstrong, D.; Smith, S.; Osborn, D.P.J.; et al. Potential gains in life expectancy from reducing amenable mortality among people diagnosed with serious mental illness in the United Kingdom. PLOS ONE 2020, 15, e0230674. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, A.; Chesney, E.; Patel, R. Improving life expectancy in people with serious mental illness: Should we place more emphasis on primary prevention? Br. J. Psychiatry 2017, 211, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Stoliker, B.E.; Kerodal, A.G.; Jewell, L.M.; Brown, K.; Kent-Wilkinson, A.; Peacock, S.; O’connell, M.E.; Wormith, J.S. Older people in custody in a forensic psychiatric facility, prevalence of dementia, and community reintegration needs: an exploratory analysis. Health Justice 2022, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Cai, L.; Huang, J. Schizophrenia and risk of dementia: a meta-analysis study. Neuropsychiatr. Dis. Treat. 2018, 14, 2047–2055. [Google Scholar] [CrossRef] [PubMed]
- Kales, H.C.; Valenstein, M.; Kim, H.M.; McCarthy, J.F.; Ganoczy, D.; Cunningham, F.; Blow, F.C. Mortality Risk in Patients With Dementia Treated With Antipsychotics Versus Other Psychiatric Medications. Am. J. Psychiatry 2007, 164, 1568–1576. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.S.; Bronskill, S.E.; Normand, S.-L.T.; Anderson, G.M.; Sykora, K.; Lam, K.; Bell, C.M.; Lee, P.E.; Fischer, H.D.; Herrmann, N.; et al. Antipsychotic Drug Use and Mortality in Older Adults with Dementia. Ann. Intern. Med. 2007, 146, 775–786. [Google Scholar] [CrossRef]
- Randle, J.M.; Heckman, G.; Oremus, M.; Ho, J. Intermittent antipsychotic medication and mortality in institutionalized older adults: A scoping review. Int. J. Geriatr. Psychiatry 2019, 34, 906–920. [Google Scholar] [CrossRef]
- Desai, V.C.; Heaton, P.C.; Kelton, C.M. Impact of the Food and Drug Administration's antipsychotic black box warning on psychotropic drug prescribing in elderly patients with dementia in outpatient and office-based settings. Alzheimer's Dement. 2012, 8, 453–457. [Google Scholar] [CrossRef]
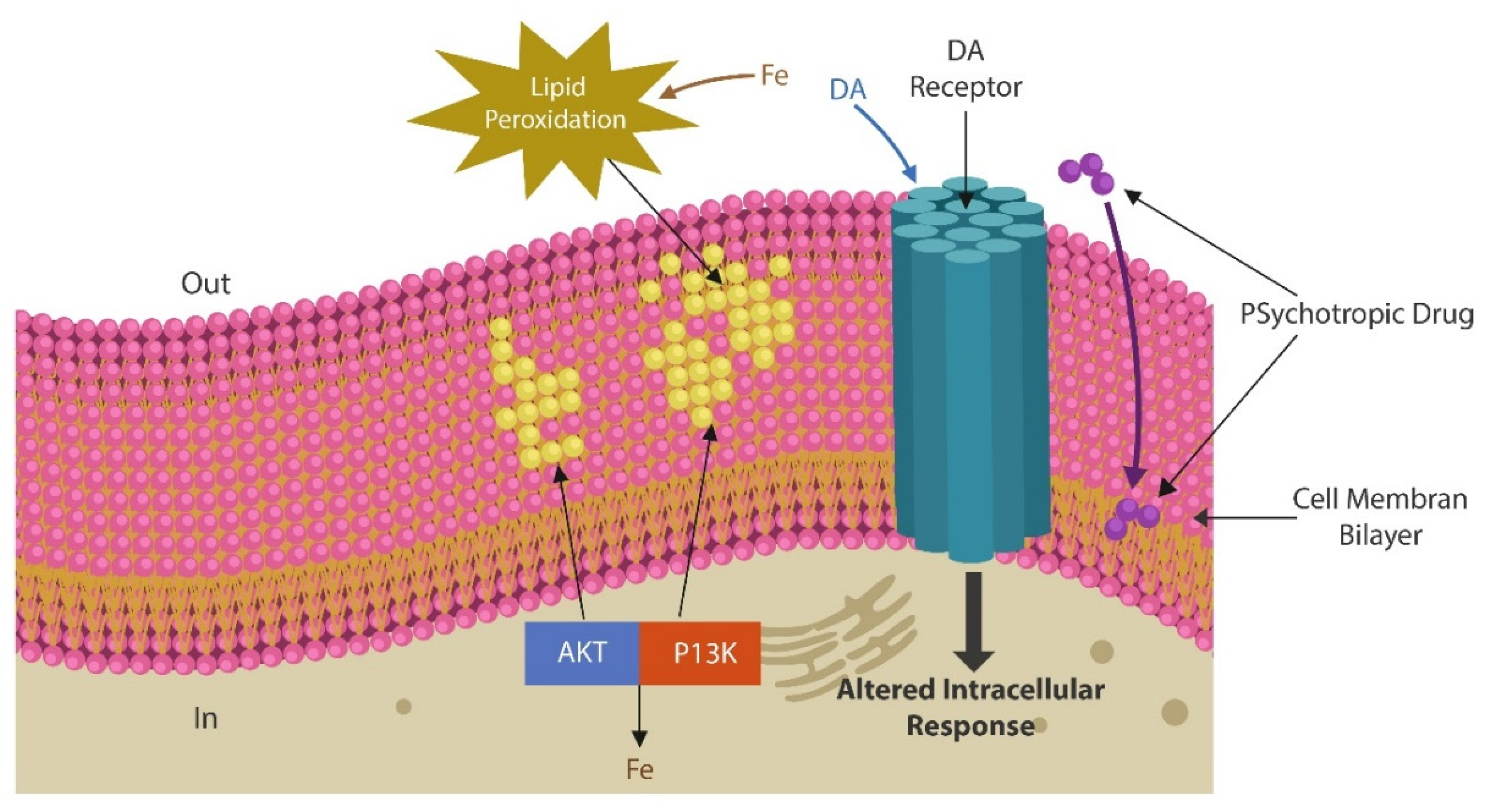
- Tessier, C.; Sweers, K.; Frajerman, A.; Bergaoui, H.; Ferreri, F.; Delva, C.; Lapidus, N.; Lamaziere, A.; Roiser, J.P.; De Hert, M.; et al. Membrane lipidomics in schizophrenia patients: a correlational study with clinical and cognitive manifestations. Transl. Psychiatry 2016, 6, e906. [Google Scholar] [CrossRef]
- Maxwell, C.; Kanes, S.; Abel, T.; Siegel, S. Phosphodiesterase inhibitors: A novel mechanism for receptor-independent antipsychotic medications. Neuroscience 2004, 129, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Surmeier, D.J.; Shen, W.; Day, M.; Gertler, T.; Chan, S.; Tian, X.; Plotkin, J.L. The role of dopamine in modulating the structure and function of striatal circuits. Prog Brain Res. 2010, 183, 148–167. [Google Scholar] [CrossRef]
- Shen, W.; Flajolet, M.; Greengard, P.; Surmeier, D.J. Dichotomous Dopaminergic Control of Striatal Synaptic Plasticity. Science 2008, 321, 848–851. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Kai, L.; Day, M.; Ronesi, J.; Yin, H.H.; Ding, J.; Tkatch, T.; Lovinger, D.M.; Surmeier, D.J. Dopaminergic Control of Corticostriatal Long-Term Synaptic Depression in Medium Spiny Neurons Is Mediated by Cholinergic Interneurons. Neuron 2006, 50, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, A.; Voineskos, D.; Daskalakis, Z.J.; Rajji, T.K.; Blumberger, D.M. A Review of Impaired Neuroplasticity in Schizophrenia Investigated with Non-invasive Brain Stimulation. Front. Psychiatry 2016, 7, 45–45. [Google Scholar] [CrossRef] [PubMed]
- Goel, P.; Chakrabarti, S.; Goel, K.; Bhutani, K.; Chopra, T.; Bali, S. Neuronal cell death mechanisms in Alzheimer’s disease: An insight. Front. Mol. Neurosci. 2022, 15, 937133. [Google Scholar] [CrossRef]
- Berry, A.S.; Shah, V.D.; Baker, S.L.; Vogel, J.W.; O'Neil, J.P.; Janabi, M.; Schwimmer, H.D.; Marks, S.M.; Jagust, W.J. Aging Affects Dopaminergic Neural Mechanisms of Cognitive Flexibility. J. Neurosci. 2016, 36, 12559–12569. [Google Scholar] [CrossRef]
- Braskie, M.N.; Wilcox, C.E.; Landau, S.M.; O'Neil, J.P.; Baker, S.L.; Madison, C.M.; Kluth, J.T.; Jagust, W.J. Relationship of Striatal Dopamine Synthesis Capacity to Age and Cognition. J. Neurosci. 2008, 28, 14320–14328. [Google Scholar] [CrossRef]
- Huber, M.; Beyer, L.; Prix, C.; Schönecker, S.; Palleis, C.; Rauchmann, B.; Morbelli, S.; Chincarini, A.; Bruffaerts, R.; Vandenberghe, R.; et al. Metabolic Correlates of Dopaminergic Loss in Dementia with Lewy Bodies. Mov. Disord. 2019, 35, 595–605. [Google Scholar] [CrossRef]
- Lubec, J.; Kalaba, P.; Hussein, A.M.; Feyissa, D.D.; Kotob, M.H.; Mahmmoud, R.R.; Wieder, O.; Garon, A.; Sagheddu, C.; Ilic, M.; et al. Reinstatement of synaptic plasticity in the aging brain through specific dopamine transporter inhibition. Mol. Psychiatry 2021, 26, 7076–7090. [Google Scholar] [CrossRef]
- Canfrán-Duque, A.; Pastor, Ó.; García-Seisdedos, D.; Molina, Y.L.; Babiy, B.; Lerma, M.; Sánchez-Castellano, C.; Martínez-Botas, J.; Gómez-Coronado, D.; Lasunción, M.A.; et al. The Antipsychotic Risperidone Alters Dihydroceramide and Ceramide Composition and Plasma Membrane Function in Leukocytes In Vitro and In Vivo. Int. J. Mol. Sci. 2021, 22, 3919. [Google Scholar] [CrossRef] [PubMed]
- Vantaggiato, C.; Panzeri, E.; Citterio, A.; Orso, G.; Pozzi, M. Antipsychotics Promote Metabolic Disorders Disrupting Cellular Lipid Metabolism and Trafficking. Trends Endocrinol. Metab. 2019, 30, 189–210. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.; Au, E.; Agarwal, S.M.; Wright, D.C.; Hahn, M.K. Antipsychotic-Induced Alterations in Lipid Turnover. Endocrinology 2023, 164. [Google Scholar] [CrossRef] [PubMed]
- Dietrich-Muszalska, A.; Kolińska-Łukaszuk, J. Comparative effects of aripiprazole and selected antipsychotic drugs on lipid peroxidation in plasma. Psychiatry Clin. Neurosci. 2018, 72, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Kuzu, O.F.; Toprak, M.; Noory, M.A.; Robertson, G.P. Effect of lysosomotropic molecules on cellular homeostasis. Pharmacol. Res. 2017, 117, 177–184. [Google Scholar] [CrossRef]
- Róg, T.; Girych, M.; Bunker, A. Mechanistic Understanding from Molecular Dynamics in Pharmaceutical Research 2: Lipid Membrane in Drug Design. Pharmaceuticals 2021, 14, 1062. [Google Scholar] [CrossRef]
- Elbaradei, A.; Wang, Z.; Malmstadt, N. Oxidation of Membrane Lipids Alters the Activity of the Human Serotonin 1A Receptor. Langmuir 2022, 38, 6798–6807. [Google Scholar] [CrossRef]
- Li, M.; Gao, Y.; Wang, D.; Hu, X.; Jiang, J.; Qing, Y.; Yang, X.; Cui, G.; Wang, P.; Zhang, J.; et al. Impaired Membrane Lipid Homeostasis in Schizophrenia. Schizophr. Bull. 2022, 48, 1125–1135. [Google Scholar] [CrossRef]
- Pillai, A.; Parikh, V.; Terry, A.V.; Mahadik, S.P. Long-term antipsychotic treatments and crossover studies in rats: Differential effects of typical and atypical agents on the expression of antioxidant enzymes and membrane lipid peroxidation in rat brain. J. Psychiatr. Res. 2007, 41, 372–386. [Google Scholar] [CrossRef]
- Oruch, R.; Lund, A.; Pryme, I.F.; Holmsen, H. An intercalation mechanism as a mode of action exerted by psychotropic drugs: results of altered phospholipid substrate availabilities in membranes? J. Chem. Biol. 2010, 3, 67–88. [Google Scholar] [CrossRef]
- Schoretsanitis, G.; Nikolakopoulou, A.; Guinart, D.; Correll, C.U.; Kane, J.M. Iron homeostasis alterations and risk for akathisia in patients treated with antipsychotics: A systematic review and meta-analysis of cross-sectional studies. Eur. Neuropsychopharmacol. 2020, 35, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.-A.; Mythily; Remington, G. Tardive Dyskinesia and Iron Status. J. Clin. Psychopharmacol. 2004, 24, 235–236. [Google Scholar] [CrossRef] [PubMed]
- Calarge, C.A.; Ziegler, E.E.; Del Castillo, N.; Aman, M.; McDougle, C.J.; Scahill, L.; McCracken, J.T.; Arnold, L.E. Iron homeostasis during risperidone treatment in children and adolescents. J. Clin. Psychiatry 2015, 76, 1500–1505. [Google Scholar] [CrossRef] [PubMed]
- Dichtl, S.; Demetz, E.; Haschka, D.; Tymoszuk, P.; Petzer, V.; Nairz, M.; Seifert, M.; Hoffmann, A.; Brigo, N.; Würzner, R.; et al. Dopamine Is a Siderophore-Like Iron Chelator That Promotes Salmonella enterica Serovar Typhimurium Virulence in Mice. Mbio 2019, 10, e02624-18. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Gan, M.; Yen, S.-H.C. Dopamine prevents lipid peroxidation-induced accumulation of toxic α-synuclein oligomers by preserving autophagy-lysosomal function. Front. Cell. Neurosci. 2013, 7, 81. [Google Scholar] [CrossRef] [PubMed]
- Tung, M.-C.; Lin, Y.-W.; Lee, W.-J.; Wen, Y.-C.; Liu, Y.-C.; Chen, J.-Q.; Hsiao, M.; Yang, Y.-C.; Chien, M.-H. Targeting DRD2 by the antipsychotic drug, penfluridol, retards growth of renal cell carcinoma via inducing stemness inhibition and autophagy-mediated apoptosis. Cell Death Dis. 2022, 13, 400. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Chen, H.; Chen, K.; Zhong, C.; Song, C.; Huang, Y.; Wang, T.; Chen, L.; Li, C.; Huang, A.; et al. The DRD2 Antagonist Haloperidol Mediates Autophagy-Induced Ferroptosis to Increase Temozolomide Sensitivity by Promoting Endoplasmic Reticulum Stress in Glioblastoma. Clin. Cancer Res. 2023, OF1–OF17. [Google Scholar] [CrossRef] [PubMed]
- Vita, A.; De Peri, L.; Deste, G.; Barlati, S.; Sacchetti, E. The Effect of Antipsychotic Treatment on Cortical Gray Matter Changes in Schizophrenia: Does the Class Matter? A Meta-analysis and Meta-regression of Longitudinal Magnetic Resonance Imaging Studies. Biol. Psychiatry 2015, 78, 403–412. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Y.; Liao, J.; Jiang, S.; Yan, J.; Yue, W.; Zhang, D.; Yan, H. Progressive Grey Matter Volume Changes in Patients with Schizophrenia over 6 Weeks of Antipsychotic Treatment and Their Relationship to Clinical Improvement. Neurosci. Bull. 2018, 34, 816–826. [Google Scholar] [CrossRef]
- Chen, Y.; Womer, F.Y.; Feng, R.; Zhang, X.; Zhang, Y.; Duan, J.; Chang, M.; Yin, Z.; Jiang, X.; Wei, S.; et al. A Real-World Observation of Antipsychotic Effects on Brain Volumes and Intrinsic Brain Activity in Schizophrenia. Front. Neurosci. 2022, 15, 749316. [Google Scholar] [CrossRef]
- Pustilnik, Amanda C., "Violence on the Brain: A Critique of Neuroscience in Criminal Law" (2009). Faculty Scholarship. 1035. Available online: https://digitalcommons.law.umaryland.edu/fac_pubs/1035.
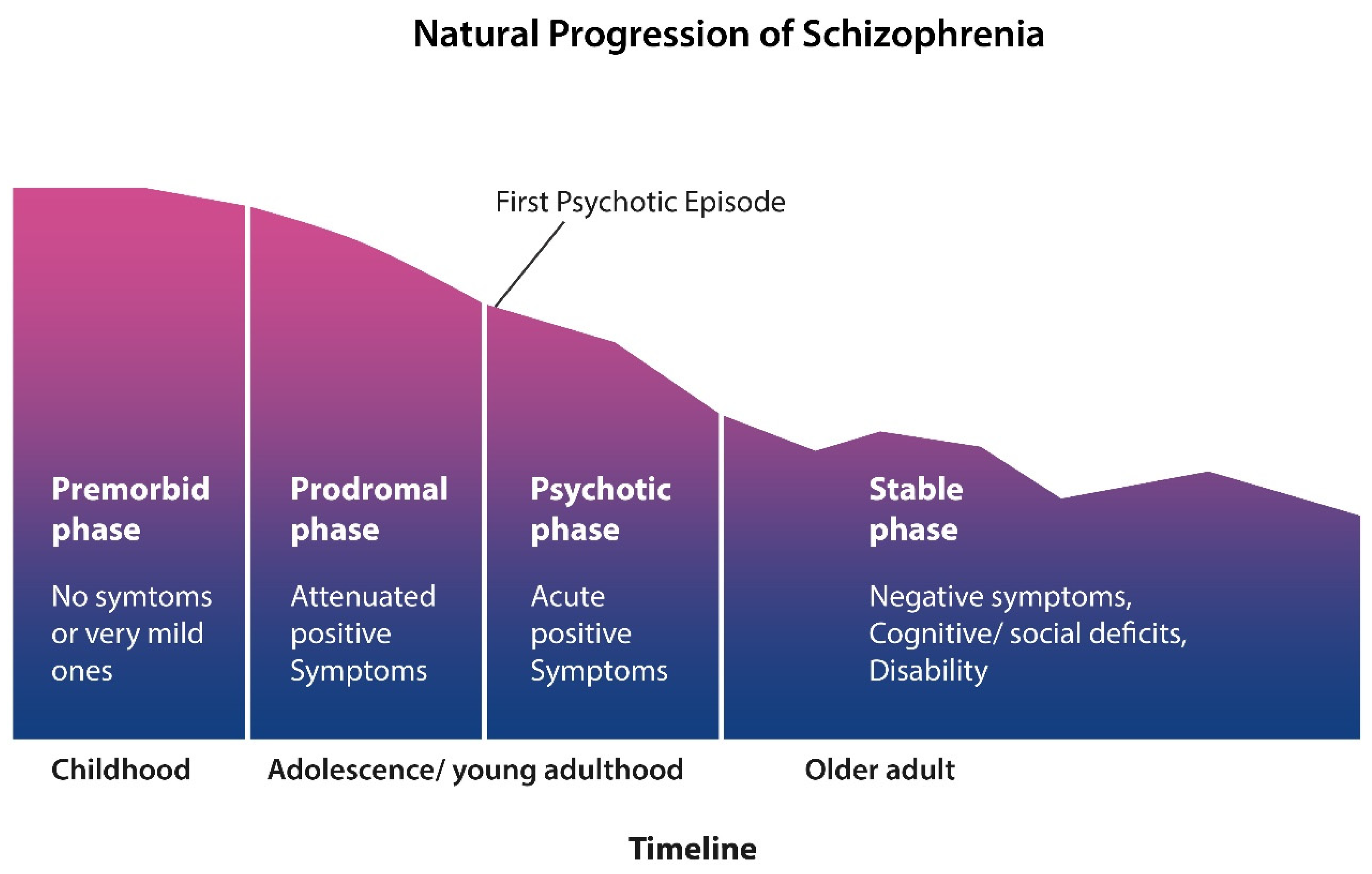
- Insel, T.R. Rethinking schizophrenia. Nature 2010, 468, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Warner, R. Recovery from schizophrenia and the recovery model. Curr. Opin. Psychiatry 2009, 22, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Sfera, A. Six Decades of Dopamine Hypothesis: Is Aryl Hydrocarbon Receptor the New D2? Reports 2023, 6, 36. [Google Scholar] [CrossRef]
- Williams, S.S. The terrorist inside my husband's brain. Neurology 2016, 87, 1308–1311. [Google Scholar] [CrossRef] [PubMed]
- Fields, R.D. THE ROOTS OF HUMAN AGGRESSION: Experiments in humans and animals have started to identify how violent behaviors begin in the brain. Sci Am. 2019, 320, 65–71. [Google Scholar] [PubMed]
- Parton, A.; Malhotra, P.; Husain, M. Hemispatial neglect. J. Neurol. Neurosurg. Psychiatry. 2004, 75, 13–21. [Google Scholar] [PubMed]
- Grattan, E.S.; Skidmore, E.R.; Woodbury, M.L. Examining Anosognosia of Neglect. OTJR: Occup. Particip. Heal. 2017, 38, 113–120. [Google Scholar] [CrossRef]
- Koreki, A.; Funayama, M.; Terasawa, Y.; Onaya, M.; Mimura, M. Aberrant Interoceptive Accuracy in Patients With Schizophrenia Performing a Heartbeat Counting Task. Schizophr. Bull. Open 2020, 2, sgaa067. [Google Scholar] [CrossRef]
- Torregrossa, L.J.; Amedy, A.; Roig, J.; Prada, A.; Park, S. Interoceptive functioning in schizophrenia and schizotypy. Schizophr. Res. 2021, 239, 151–159. [Google Scholar] [CrossRef]
- Yao, B.; Thakkar, K. Interoception abnormalities in schizophrenia: A review of preliminary evidence and an integration with Bayesian accounts of psychosis. Neurosci. Biobehav. Rev. 2021, 132, 757–773. [Google Scholar] [CrossRef]
- Ribolsi, M.; Daskalakis, Z.J.; Siracusano, A.; Koch, G. Abnormal Asymmetry of Brain Connectivity in Schizophrenia. Front. Hum. Neurosci. 2014, 8, 1010. [Google Scholar] [CrossRef] [PubMed]
- Brüne, M.; Schöbel, A.; Karau, R.; Benali, A.; Faustmann, P.M.; Juckel, G.; Petrasch-Parwez, E. Von Economo neuron density in the anterior cingulate cortex is reduced in early onset schizophrenia. Acta Neuropathol. 2010, 119, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Brasso, C.; Stanziano, M.; Bosco, F.M.; Morese, R.; Valentini, M.C.; Vercelli, A.; Rocca, P. Alteration of the Functional Connectivity of the Cortical Areas Characterized by the Presence of Von Economo Neurons in Schizophrenia, a Pilot Study. J. Clin. Med. 2023, 12, 1377. [Google Scholar] [CrossRef] [PubMed]
- López-Ojeda, W.; Hurley, R.A. Von Economo Neuron Involvement in Social Cognitive and Emotional Impairments in Neuropsychiatric Disorders. J. Neuropsychiatry 2022, 34, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Kraepelin, E. (1990) Psychiatry. A Textbook for Students and Physicians, 2 vols, translated by H. Metoui and S. Ayed (Canton, MA: Science History Publications); originally publishedas Psychiatrie. Ein Lehrbuch fur Studirende und Aerzte (6th edn, 1899).
- Voruz, P.; Cionca, A.; de Alcântara, I.J.; Nuber-Champier, A.; Allali, G.; Benzakour, L.; Thomasson, M.; Lalive, P.H.; Lövblad, K.-O.; Braillard, O.; et al. Functional connectivity underlying cognitive and psychiatric symptoms in post-COVID-19 syndrome: is anosognosia a key determinant? Brain Commun. 2022, 4, fcac057. [Google Scholar] [CrossRef]
- Juengst, S.; Skidmore, E.; Pramuka, M.; McCue, M.; Becker, J. Factors contributing to impaired self-awareness of cognitive functioning in an HIV positive and at-risk population. Disabil. Rehabilitation 2011, 34, 19–25. [Google Scholar] [CrossRef]
- Allman, J.M.; Tetreault, N.A.; Hakeem, A.Y.; Park, S. The von economo neurons in apes and humans. Am. J. Hum. Biol. 2010, 23, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Faissner, A. Low-density lipoprotein receptor-related protein-1 (LRP1) in the glial lineage modulates neuronal excitability. Front. Netw. Physiol. 2023, 3, 1190240. [Google Scholar] [CrossRef]
- Pillmann, F.; Rohde, A.; Ullrich, S.; Draba, S.; Sannemüller, U.; Marneros, A. Violence, Criminal Behavior, and the EEG. J. Neuropsychiatry 1999, 11, 454–457. [Google Scholar] [CrossRef]
- Marwaha, S. Prevalence of Principles of Piaget’s Theory Among 4-7-year-old Children and their Correlation with IQ. J. Clin. Diagn. Res. 2017, 11, ZC111–ZC115. [Google Scholar] [CrossRef]
- Gefen, T.; Papastefan, S.T.; Rezvanian, A.; Bigio, E.H.; Weintraub, S.; Rogalski, E.; Mesulam, M.-M.; Geula, C. Von Economo neurons of the anterior cingulate across the lifespan and in Alzheimer's disease. Cortex 2017, 99, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Cauda, F.; Nani, A.; Costa, T.; Palermo, S.; Tatu, K.; Manuello, J.; Duca, S.; Fox, P.T.; Keller, R. The morphometric co-atrophy networking of schizophrenia, autistic and obsessive spectrum disorders. Hum. Brain Mapp. 2018, 39, 1898–1928. [Google Scholar] [CrossRef] [PubMed]
- Papanastasiou, E.; Gaughran, F.; Smith, S. Schizophrenia as segmental progeria. J. R. Soc. Med. 2011, 104, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.Y.; Chang, H.W.; Lin, C.H.; Cho, C.L. Short telomeres in patients with chronic schizophrenia who show a poor response to treatment. J Psychiatry Neurosci. Erratum in: J Psychiatry Neurosci. 2008, 33, 343. 2008, 33, 244–247. [Google Scholar] [PubMed]
- Laursen, T.M. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr. Res. 2011, 131, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Peritogiannis, V.; Ninou, A.; Samakouri, M. Mortality in Schizophrenia-Spectrum Disorders: Recent Advances in Understanding and Management. Healthcare 2022, 10, 2366. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Shen, J.; He, J.; Lu, M. Schizophrenia and cell senescence candidate genes screening, machine learning, diagnostic models, and drug prediction. Front. Psychiatry 2023, 14, 1105987. [Google Scholar] [CrossRef]
- Acosta, J.C.; Banito, A.; Wuestefeld, T.; Georgilis, A.; Janich, P.; Morton, J.P.; Athineos, D.; Kang, T.-W.; Lasitschka, F.; Andrulis, M.; et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nature 2013, 15, 978–990. [Google Scholar] [CrossRef]
- Ishida, I.; Ogura, J.; Aizawa, E.; Ota, M.; Hidese, S.; Yomogida, Y.; Matsuo, J.; Yoshida, S.; Kunugi, H. Gut permeability and its clinical relevance in schizophrenia. Neuropsychopharmacol. Rep. 2022, 42, 70–76. [Google Scholar] [CrossRef]
- Zhao, Y.; Cong, L.; Lukiw, W.J. Lipopolysaccharide (LPS) Accumulates in Neocortical Neurons of Alzheimer’s Disease (AD) Brain and Impairs Transcription in Human Neuronal-Glial Primary Co-cultures. Front. Aging Neurosci. 2017, 9, 407. [Google Scholar] [CrossRef]
- Sung, K.; Zhang, B.; Wang, H.E.; Bai, Y.; Tsai, S.; Su, T.; Chen, T.; Hou, M.; Lu, C.; Wang, Y.; et al. Schizophrenia and risk of new-onset inflammatory bowel disease: a nationwide longitudinal study. Aliment. Pharmacol. Ther. 2022, 55, 1192–1201. [Google Scholar] [CrossRef] [PubMed]
- Yanuck, S.F. Microglial Phagocytosis of Neurons: Diminishing Neuronal Loss in Traumatic, Infectious, Inflammatory, and Autoimmune CNS Disorders. Front. Psychiatry 2019, 10, 712. [Google Scholar] [CrossRef] [PubMed]
- Secher, T.; Samba-Louaka, A.; Oswald, E.; Nougayrède, J.-P. Escherichia coli Producing Colibactin Triggers Premature and Transmissible Senescence in Mammalian Cells. PLOS ONE 2013, 8, e77157. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Gao, F.; Zhou, L.; Fan, Y.; Zhao, B.; Xi, W.; Wang, C.; Zhu, F.; Ma, X.; Wang, W.; et al. Characterizing serum amino acids in schizophrenic patients: Correlations with gut microbes. J. Psychiatr. Res. 2022, 153, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Dietrich-Muszalska, A.; Kolodziejczyk-Czepas, J.; Nowak, P. Comparative Study of the Effects of Atypical Antipsychotic Drugs on Plasma and Urine Biomarkers of Oxidative Stress in Schizophrenic Patients. Neuropsychiatr. Dis. Treat. 2021, 17, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.; Parikh, V.; Terry, A.V.; Mahadik, S.P. Long-term antipsychotic treatments and crossover studies in rats: Differential effects of typical and atypical agents on the expression of antioxidant enzymes and membrane lipid peroxidation in rat brain. J. Psychiatr. Res. 2007, 41, 372–386. [Google Scholar] [CrossRef]
- Li, M.; Gao, Y.; Wang, D.; Hu, X.; Jiang, J.; Qing, Y.; Yang, X.; Cui, G.; Wang, P.; Zhang, J.; et al. Impaired Membrane Lipid Homeostasis in Schizophrenia. Schizophr. Bull. 2022, 48, 1125–1135. [Google Scholar] [CrossRef]
- Lotan, A.; Luza, S.; Opazo, C.M.; Ayton, S.; Lane, D.J.R.; Mancuso, S.; Pereira, A.; Sundram, S.; Weickert, C.S.; Bousman, C.; et al. Perturbed iron biology in the prefrontal cortex of people with schizophrenia. Mol. Psychiatry 2023. [Google Scholar] [CrossRef]
- Killilea, D.W.; Atamna, H.; Liao, C.; Ames, B.N. Iron Accumulation During Cellular Senescence in Human FibroblastsIn Vitro. Antioxidants Redox Signal. 2003, 5, 507–516. [Google Scholar] [CrossRef]
- Santillo, A.F.; Nilsson, C.; Englund, E. von E conomo neurones are selectively targeted in frontotemporal dementia. Neuropathol. Appl. Neurobiol. 2013, 39, 572–579. [Google Scholar] [CrossRef]
- Lin, L.-C.; Nana, A.L.; Hepker, M.; Hwang, J.-H.L.; Gaus, S.E.; Spina, S.; Cosme, C.G.; Gan, L.; Grinberg, L.T.; Geschwind, D.H.; et al. Preferential tau aggregation in von Economo neurons and fork cells in frontotemporal lobar degeneration with specific MAPT variants. Acta Neuropathol. Commun. 2019, 7, 159. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Guo, Z. Recent progress in ferroptosis: inducers and inhibitors. Cell Death Discov. 2022, 8, 501. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Dong, Y.; Chu, Y.; Guo, Y.; Li, L. The mechanisms of ferroptosis and its role in alzheimer’s disease. Front. Mol. Biosci. 2022, 9, 965064. [Google Scholar] [CrossRef] [PubMed]
- Nuñez, M.T.; Chana-Cuevas, P. New Perspectives in Iron Chelation Therapy for the Treatment of Neurodegenerative Diseases. Pharmaceuticals 2018, 11, 109. [Google Scholar] [CrossRef] [PubMed]
- Huxley, P.; Krayer, A.; Poole, R.; Prendergast, L.; Aryal, S.; Warner, R. Schizophrenia outcomes in the 21st century: A systematic review. Brain Behav. 2021, 11, e02172. [Google Scholar] [CrossRef]
- Robinson, D.G.; Woerner, M.G.; McMeniman, M.; Mendelowitz, A.; Bilder, R.M.; Velthorst, E.; Fett, A.-K.J.; Reichenberg, A.; Perlman, G.; van Os, J.; et al. Symptomatic and Functional Recovery From a First Episode of Schizophrenia or Schizoaffective Disorder. Am. J. Psychiatry 2004, 161, 473–479. [Google Scholar] [CrossRef]
- Harrison, G.; Hopper, K.; Craig, T.; Laska, E.; Siegel, C.; Wanderling, J.; Dube, K.C.; Ganev, K.; Giel, R.; Der Heiden, W.A.; et al. Recovery from psychotic illness: A 15- and 25-year international follow-up study. Br. J. Psychiatry 2001, 178, 506–517. [Google Scholar] [CrossRef]
- Holm, M.; Taipale, H.; Tanskanen, A.; Tiihonen, J.; Mitterdorfer-Rutz, E. Employment among people with schizophrenia or bipolar disorder: A population-based study using nationwide registers. Acta Psychiatr. Scand. 2020, 143, 61–71. [Google Scholar] [CrossRef]
- Lévesque, I.S.; Abdel-Baki, A. Homeless youth with first-episode psychosis: A 2-year outcome study. Schizophr. Res. 2019, 216, 460–469. [Google Scholar] [CrossRef]
- Jääskeläinen, E.; Juola, P.; Hirvonen, N.; McGrath, J.J.; Saha, S.; Isohanni, M.; Veijola, J.; Miettunen, J. A Systematic Review and Meta-Analysis of Recovery in Schizophrenia. Schizophr. Bull. 2012, 39, 1296–1306. [Google Scholar] [CrossRef]
- Kotov, R.; Fochtmann, L.; Li, K.; Tanenberg-Karant, M.; Constantino, E.A.; Rubinstein, J.; Perlman, G.; Velthorst, E.; Fett, A.-K.J.; Carlson, G.; et al. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am. J. Psychiatry 1994, 151, 1409–1416. [Google Scholar] [CrossRef]
- Vita, A.; De Peri, L.; Deste, G.; Sacchetti, E. Progressive loss of cortical gray matter in schizophrenia: a meta-analysis and meta-regression of longitudinal MRI studies. Transl Psychiatry 2012, 2, e190. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.A. Neurobiology and the natural history of schizophrenia. J. Clin. Psychiatry 2006, 67, e14. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Smieskova, R.; Kempton, M.; Ho, B.; Andreasen, N.; Borgwardt, S. Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies. Neurosci. Biobehav. Rev. 2013, 37, 1680–1691. [Google Scholar] [CrossRef] [PubMed]
- Ho, B.C.; Andreasen, N.C.; Ziebell, S.; Pierson, R.; Magnotta, V. Long-term antipsychotic treatment and brain volumes: A longitudinal study of first-episode schizophrenia. Arch. Gen. Psychiatry 2011, 68, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Cahn, W.; Pol HE, H.; Lems, E.B.; van Haren, N.E.; Schnack, H.G.; van der Linden, J.A.; Schothorst, P.F.; van Engeland, H.; Kahn, R.S. Brain volume changes in first-episode schizophrenia: A 1-year follow-up study. Arch. Gen. Psychiatry 2002, 59, 1002–1010. [Google Scholar] [CrossRef]
- Ting, C.; Rajji, T.K.; Ismail, Z.; Tang-Wai, D.F.; Apanasiewicz, N.; Miranda, D.; Mamo, D.; Mulsant, B.H. Differentiating the Cognitive Profile of Schizophrenia from That of Alzheimer Disease and Depression in Late Life. PLOS ONE 2010, 5, e10151. [Google Scholar] [CrossRef]
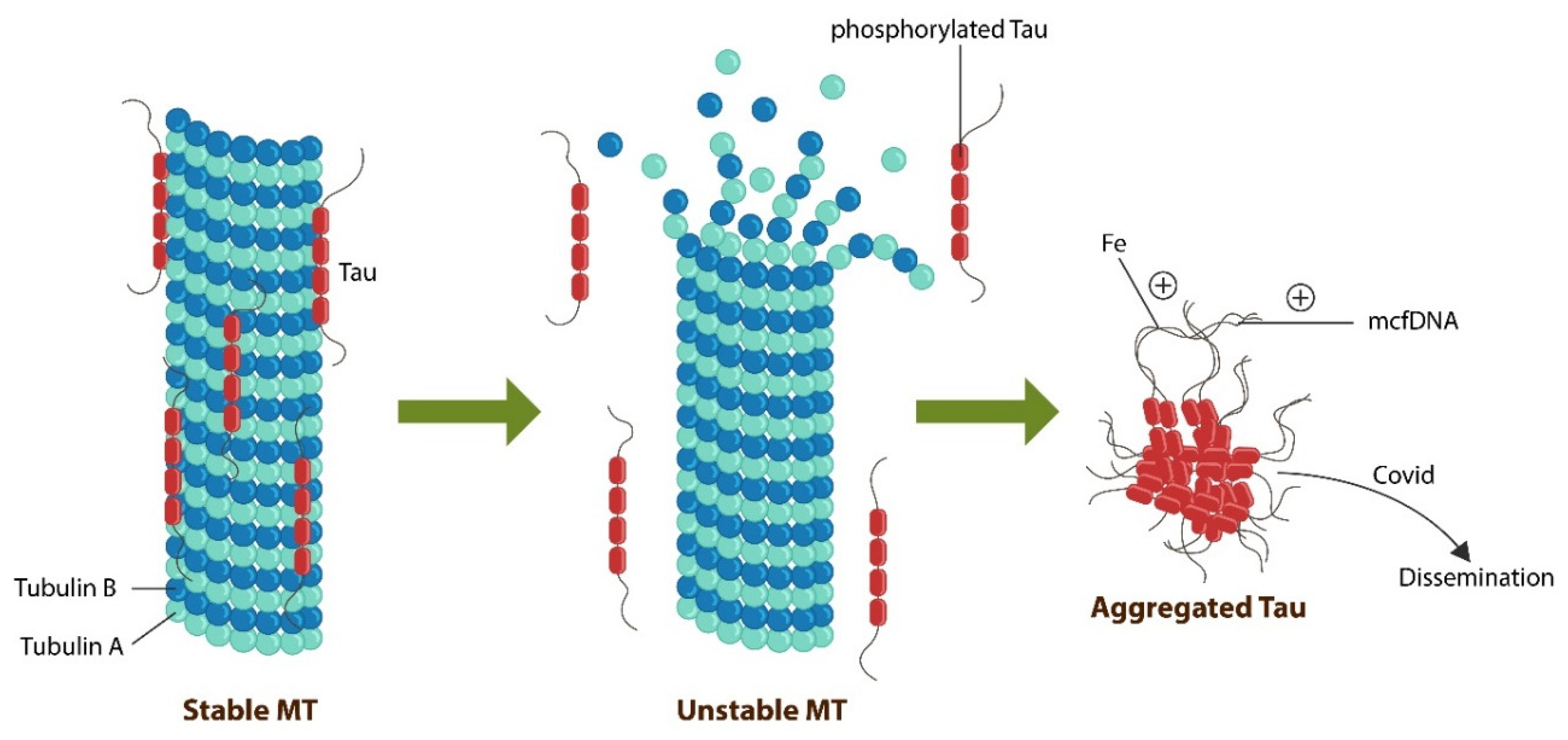
- Dehmelt, L.; Halpain, S. The MAP2/Tau family of microtubule-associated proteins. Genome Biol. 2004, 6, 204. [Google Scholar] [CrossRef]
- Hameroff, S. Consciousness, Cognition and the Neuronal Cytoskeleton – A New Paradigm Needed in Neuroscience. Front. Mol. Neurosci. 2022, 15, 869935. [Google Scholar] [CrossRef]
- Tonello, L.; Cocchi, M.; Gabrielli, F.; Tuszynski, J.A. On the possible quantum role of serotonin in consciousness. J. Integr. Neurosci. 2015, 14, 295–308. [Google Scholar] [CrossRef]
- Craddock, T.J.A.; Priel, A.; Tuszynski, J.A. Keeping time: Could quantum beating in microtubules be the basis for the neural synchrony related to consciousness? J. Integr. Neurosci. 2014, 13, 293–311. [Google Scholar] [CrossRef] [PubMed]
- Planel, E.; Krishnamurthy, P.; Miyasaka, T.; Liu, L.; Herman, M.; Kumar, A.; Bretteville, A.; Figueroa, H.Y.; Yu, W.H.; Whittington, R.A.; et al. Anesthesia-Induced Hyperphosphorylation Detaches 3-Repeat Tau from Microtubules without Affecting Their StabilityIn Vivo. J. Neurosci. 2008, 28, 12798–12807. [Google Scholar] [CrossRef] [PubMed]
- Run, X.; Liang, Z.; Zhang, L.; Iqbal, K.; Grundke-Iqbal, I.; Gong, C.-X. Anesthesia Induces Phosphorylation of Tau. J. Alzheimer's Dis. 2009, 16, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Rowinsky, E.K.; Chaudhry, V.; Cornblath, D.R.; Donehower, R.C. Neurotoxicity of Taxol. J Natl Cancer Inst Monogr. 1993, 107–115. [Google Scholar] [PubMed]
- Luciani, M.; Montalbano, M.; Troncone, L.; Bacchin, C.; Uchida, K.; Daniele, G.; Wolf, B.J.; Butler, H.M.; Kiel, J.; Berto, S.; et al. Big tau aggregation disrupts microtubule tyrosination and causes myocardial diastolic dysfunction: from discovery to therapy. Eur. Hear. J. 2023, 44, 1560–1570. [Google Scholar] [CrossRef]
- Bunzel, B.; Schmidl-Mohl, B.; Wollenek, G.; Grundböck, A. Does changing the heart mean changing personality? A retrospective inquiry on 47 heart transplant patients. Qual. Life Res. 1992, 1, 251–256. [Google Scholar] [CrossRef]
- Pearsall, P.; Schwartz, G.E.; Russek, L.G. Changes in heart transplant recipients that parallel the personalities of their donors. Integr. Med. 2000, 2, 65–72. [Google Scholar] [CrossRef]
- Prinzen, F.W.; Vernooy, K.; Cornelussen, R.N. Cardiac Memory and Cortical Memory. Circulation 2004, 109, e226. [Google Scholar] [CrossRef]
- Liester, M.B. Personality changes following heart transplantation: The role of cellular memory. Med Hypotheses 2019, 135, 109468. [Google Scholar] [CrossRef]
- Bahramnezhad, F.; Asgari, P.; Jackson, A.C. Adjustment to a new heart: Concept analysis using a hybrid model. Iran. J. Nurs. Midwifery Res. 2021, 26, 89–96. [Google Scholar] [CrossRef]
- Letourneau, J.; Holmes, Z.C.; Dallow, E.P.; Durand, H.K.; Jiang, S.; Carrion, V.M.; Gupta, S.K.; Mincey, A.C.; Muehlbauer, M.J.; Bain, J.R.; et al. Ecological memory of prior nutrient exposure in the human gut microbiome. ISME J. 2022, 16, 2479–2490. [Google Scholar] [CrossRef] [PubMed]
- Snijders, T.; Aussieker, T.; Holwerda, A.; Parise, G.; Loon, L.J.C.; Verdijk, L.B. The concept of skeletal muscle memory: Evidence from animal and human studies. Acta Physiol. 2020, 229, e13465. [Google Scholar] [CrossRef] [PubMed]
- Vogel, D.; Dussutour, A. Direct transfer of learned behaviour via cell fusion in non-neural organisms. Proc. R. Soc. B: Boil. Sci. 2016, 283, 20162382. [Google Scholar] [CrossRef] [PubMed]
- Tetz, G.; Pinho, M.; Pritzkow, S.; Mendez, N.; Soto, C.; Tetz, V. Bacterial DNA promotes Tau aggregation. Sci. Rep. 2020, 10, 2369. [Google Scholar] [CrossRef] [PubMed]
- Seneff, S.; Kyriakopoulos, A.M.; Nigh, G.; A McCullough, P.; McCullough, P.A. A Potential Role of the Spike Protein in Neurodegenerative Diseases: A Narrative Review. Cureus 2023, 15, e34872. [Google Scholar] [CrossRef]
- Demirel. F.; Cetin, I.; Turan,.; Yıldız, N.; Sağlam, T.; Duran, A. Total Tau and Phosphorylated Tau Protein Serum Levels in Patients with Schizophrenia Compared with Controls. Psychiatr. Q. 2017, 88, 921–928. [Google Scholar] [CrossRef]
- Grubisha, M.J.; Sun, X.; MacDonald, M.L.; Garver, M.; Sun, Z.; Paris, K.A.; Patel, D.S.; DeGiosio, R.A.; Lewis, D.A.; Yates, N.A.; et al. MAP2 is differentially phosphorylated in schizophrenia, altering its function. Mol. Psychiatry 2021, 26, 5371–5388. [Google Scholar] [CrossRef]
- Krause, M.; Theiss, C.; Brüne, M. Ultrastructural Alterations of Von Economo Neurons in the Anterior Cingulate Cortex in Schizophrenia. Anat. Rec. 2017, 300, 2017–2024. [Google Scholar] [CrossRef]
- Agnati, L.F.; Zunarelli, E.; Genedani, S.; Fuxe, K. On the Existence of a Global Molecular Network Enmeshing the Whole Central Nervous System: Physiological and Pathological Implications. Curr. Protein Pept. Sci. 2006, 7, 3–15. [Google Scholar] [CrossRef]
- Boeve, B.F. Behavioral Variant Frontotemporal Dementia. Contin. Lifelong Learn. Neurol. 2022, 28, 702–725. [Google Scholar] [CrossRef]
- Seeley, W.W. Behavioral Variant Frontotemporal Dementia. Contin. Lifelong Learn. Neurol. 2019, 25, 76–100. [Google Scholar] [CrossRef] [PubMed]
- Dols, A.; van Liempt, S.; Gossink, F.; Krudop, W.A.; Sikkes, S.; Pijnenburg, Y.A.L.; Stek, M.L. Identifying Specific Clinical Symptoms of Behavioral Variant Frontotemporal Dementia Versus Differential Psychiatric Disorders in Patients Presenting with a Late-Onset Frontal Lobe Syndrome. J. Clin. Psychiatry 2016, 77, 1391–1395. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, G.; Danti, S.; Nuti, A.; Di Fiorino, M.; Cammisuli, D.M. Is that schizophrenia or frontotemporal dementia? Supporting clinicians in making the right diagnosis. Acta Neurol. Belg. 2020, 120, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Bott, N.T.; Radke, A.; Stephens, M.L.; Kramer, J.H. Frontotemporal dementia: diagnosis, deficits and management. Neurodegener. Dis. Manag. 2014, 4, 439–454. [Google Scholar] [CrossRef] [PubMed]
- Ducharme, S.; Dols, A.; Laforce, R.; Devenney, E.; Kumfor, F.; Stock, J.v.D.; Dallaire-Théroux, C.; Seelaar, H.; Gossink, F.; Vijverberg, E.; et al. Recommendations to distinguish behavioural variant frontotemporal dementia from psychiatric disorders. Brain 2020, 143, 1632–1650. [Google Scholar] [CrossRef] [PubMed]
- Woolley, J.D.; Khan, B.K.; Murthy, N.K.; Miller, B.L.; Rankin, K.P. The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. J Clin Psychiatry 2011, 72, 126–133. [Google Scholar] [CrossRef]
- Liljegren, M.; Naasan, G.; Temlett, J.; Perry, D.C.; Rankin, K.P.; Merrilees, J.; Grinberg, L.T.; Seeley, W.W.; Englund, E.; Miller, B.L. Criminal Behavior in Frontotemporal Dementia and Alzheimer Disease. JAMA Neurol. 2015, 72, 295–300. [Google Scholar] [CrossRef]
- Sfera, A.; Osorio, C.; Gradini, R.; Price, A. Neurodegeneration Behind Bars: from Molecules to Jurisprudence. Front. Psychiatry 2014, 5, 115. [Google Scholar] [CrossRef]
- Meeks, T.W.; Jeste, D.V. Beyond the Black Box: What is The Role for Antipsychotics in Dementia? Curr. Psychiatr. 2008, 7, 50–65. [Google Scholar]
- Desai, V.C.; Heaton, P.C.; Kelton, C.M. Impact of the Food and Drug Administration's antipsychotic black box warning on psychotropic drug prescribing in elderly patients with dementia in outpatient and office-based settings. Alzheimer's Dement. 2012, 8, 453–457. [Google Scholar] [CrossRef]
- Deming, P.; Cook, C.J.; Meyerand, M.E.; Kiehl, K.A.; Kosson, D.S.; Koenigs, M. Impaired salience network switching in psychopathy. Behav. Brain Res. 2023, 452, 114570. [Google Scholar] [CrossRef] [PubMed]
- Kohn, N.; Szopinska-Tokov, J.; Arenas, A.L.; Beckmann, C.; Arias-Vasquez, A.; Aarts, E. Multivariate associative patterns between the gut microbiota and large-scale brain network connectivity. Gut Microbes 2021, 13, 2006586. [Google Scholar] [CrossRef] [PubMed]
- Mulder, D.; Aarts, E.; Vasquez, A.A.; Bloemendaal, M. A systematic review exploring the association between the human gut microbiota and brain connectivity in health and disease. Mol. Psychiatry 2023. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, A.P.; Sanchez-Padilla, D.E.; Drew, J.C.; Oli, M.W.; Roesch, L.F.W.; Triplett, E.W. Saliva microbiome, dietary, and genetic markers are associated with suicidal ideation in university students. Sci. Rep. 2022, 12, 14306. [Google Scholar] [CrossRef] [PubMed]
- Koren, T.; Yifa, R.; Amer, M.; Krot, M.; Boshnak, N.; Ben-Shaanan, T.L.; Azulay-Debby, H.; Zalayat, I.; Avishai, E.; Hajjo, H.; et al. Insular cortex neurons encode and retrieve specific immune responses. Cell 2021, 184, 5902–5915. [Google Scholar] [CrossRef]
- Rolls, A. Immunoception: the insular cortex perspective. Cell. Mol. Immunol. 2023. [Google Scholar] [CrossRef]
- Bodea, L.; Eckert, A.; Ittner, L.M.; Piguet, O.; Götz, J. Tau physiology and pathomechanisms in frontotemporal lobar degeneration. J. Neurochem. 2016, 138, 71–94. [Google Scholar] [CrossRef]
- Rademakers, R.; Cruts, M.; van Broeckhoven, C. The role of tau (MAPT) in frontotemporal dementia and related tauopathies. Hum. Mutat. 2004, 24, 277–295. [Google Scholar] [CrossRef]
- Marchisella, F.; Coffey, E.T.; Hollos, P. Microtubule and microtubule associated protein anomalies in psychiatric disease. Cytoskeleton 2016, 73, 596–611. [Google Scholar] [CrossRef]
- Arnold, S.E.; Lee, V.M.; Gur, R.E.; Trojanowski, J.Q. Abnormal expression of two microtubule-associated proteins (MAP2 and MAP5) in specific subfields of the hippocampal formation in schizophrenia. Proc. Natl. Acad. Sci. USA 1991, 88, 10850–10854. [Google Scholar] [CrossRef]
- Jones, L.B.; Johnson, N.; Byne, W. Alterations in MAP2 immunocytochemistry in areas 9 and 32 of schizophrenic prefrontal cortex. Psychiatry Res. Neuroimaging 2002, 114, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Andreou, D.; Jørgensen, K.N.; Nerland, S.; Smelror, R.E.; Wedervang-Resell, K.; Johannessen, C.H.; Myhre, A.M.; Andreassen, O.A.; Blennow, K.; Zetterberg, H.; et al. Lower plasma total tau in adolescent psychosis: Involvement of the orbitofrontal cortex. J. Psychiatr. Res. 2021, 144, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Shukla, R.; Santoro, J.; Bender, F.C.; Laterza, O.F. Quantitative determination of human interleukin 22 (IL-22) in serum using Singulex-Erenna® Technology. J. Immunol. Methods 2013, 390, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Eichenberger, E.M.; Degner, N.; Scott, E.R.; Ruffin, F.; Franzone, J.; Sharma-Kuinkel, B.; Shah, P.; Hong, D.; Dalai, S.C.; Blair, L.; et al. Microbial Cell-Free DNA Identifies the Causative Pathogen in Infective Endocarditis and Remains Detectable Longer Than Conventional Blood Culture in Patients with Prior Antibiotic Therapy. Clin. Infect. Dis. 2022, 76, e1492–e1500. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-W.; Stewart, R.; Park, W.-Y.; Jhon, M.; Lee, J.-Y.; Kim, S.-Y.; Kim, J.-M.; Amminger, P.; Chung, Y.-C.; Yoon, J.-S. Latent Iron Deficiency as a Marker of Negative Symptoms in Patients with First-Episode Schizophrenia Spectrum Disorder. Nutrients 2018, 10, 1707. [Google Scholar] [CrossRef] [PubMed]
- Wan, W.; Cao, L.; Kalionis, B.; Murthi, P.; Xia, S.; Guan, Y. Iron Deposition Leads to Hyperphosphorylation of Tau and Disruption of Insulin Signaling. Front. Neurol. 2019, 10, 607. [Google Scholar] [CrossRef]
- Rao, S.S.; Adlard, P.A. Untangling Tau and Iron: Exploring the Interaction Between Iron and Tau in Neurodegeneration. Front. Mol. Neurosci. 2018, 11, 276. [Google Scholar] [CrossRef]
- Sheelakumari, R.; Kesavadas, C.; Varghese, T.; Sreedharan, R.; Thomas, B.; Verghese, J.; Mathuranath, P. Assessment of Iron Deposition in the Brain in Frontotemporal Dementia and Its Correlation with Behavioral Traits. Am. J. Neuroradiol. 2017, 38, 1953–1958. [Google Scholar] [CrossRef]
- Tisdall, M.D.; Ohm, D.T.; Lobrovich, R.; Das, S.R.; Mizsei, G.; Prabhakaran, K.; Ittyerah, R.; Lim, S.; McMillan, C.T.; Wolk, D.A.; et al. Ex vivo MRI and histopathology detect novel iron-rich cortical inflammation in frontotemporal lobar degeneration with tau versus TDP-43 pathology. NeuroImage: Clin. 2022, 33, 102913. [Google Scholar] [CrossRef]
- Kosyakovsky, J.; Fine, J.M.; Frey, W.H.; Hanson, L.R. Mechanisms of Intranasal Deferoxamine in Neurodegenerative and Neurovascular Disease. Pharmaceuticals 2021, 14, 95. [Google Scholar] [CrossRef]
- Aaronson, A.L.; Bordelon, S.D.; Brakel, S.J.; Morrison, H. A Review of the Role of Chronic Traumatic Encephalopathy in Criminal Court. J. Am. Acad. Psychiatry Law 2020, 49, 60–65. [Google Scholar] [PubMed]
- Byard, R.; Tiemensma, M.; Buckland, M.E.; Vink, R. Chronic traumatic encephalopathy (CTE)—features and forensic considerations. Forensic Sci. Med. Pathol. 2023. [Google Scholar] [CrossRef] [PubMed]
- McKee, A.C.; Stein, T.D.; Kiernan, P.T.; Alvarez, V.E. The Neuropathology of Chronic Traumatic Encephalopathy. Brain Pathol. 2015, 25, 350–364. [Google Scholar] [CrossRef] [PubMed]
- Katsumoto, A.; Takeuchi, H.; Tanaka, F. Tau Pathology in Chronic Traumatic Encephalopathy and Alzheimer's Disease: Similarities and Differences. Front. Neurol. 2019, 10, 980. [Google Scholar] [CrossRef]
- Daglas, M.; Adlard, P.A. The Involvement of Iron in Traumatic Brain Injury and Neurodegenerative Disease. Front. Neurosci. 2018, 12, 981. [Google Scholar] [CrossRef] [PubMed]
- Han, X. Neurolipidomics: challenges and developments. Front. Biosci. 2007, 12, 2601–2615. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Seo, Y.; Jo, Y.S.; Lee, S.; Cho, E.; Cazenave-Gassiot, A.; Shin, Y.-S.; Moon, M.H.; An, H.J.; Wenk, M.R.; et al. Brain lipidomics: From functional landscape to clinical significance. Sci. Adv. 2022, 8, eadc9317. [Google Scholar] [CrossRef]
- Nicolson, G.L.; Ash, M.E. Lipid Replacement Therapy: A natural medicine approach to replacing damaged lipids in cellular membranes and organelles and restoring function. Biochim. et Biophys. Acta (BBA) - Biomembr. 2014, 1838, 1657–1679. [Google Scholar] [CrossRef] [PubMed]
- Hamsanathan, S.; Gurkar, A.U. Lipids as Regulators of Cellular Senescence. Front. Physiol. 2022, 13, 796850. [Google Scholar] [CrossRef] [PubMed]
- Horn, A.; Jaiswal, J.K. Structural and signaling role of lipids in plasma membrane repair. Curr. Top. Membr. 2019, 84, 67–98. [Google Scholar] [CrossRef]
- Cadenas, C.; Vosbeck, S.; Hein, E.-M.; Hellwig, B.; Langer, A.; Hayen, H.; Franckenstein, D.; Büttner, B.; Hammad, S.; Marchan, R.; et al. Glycerophospholipid profile in oncogene-induced senescence. Biochim. et Biophys. Acta (BBA) - Mol. Cell Biol. Lipids 2012, 1821, 1256–1268. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, H.-S.; Choi, D.-H.; Choi, J.; Cho, S.Y.; Kim, S.-H.; Baek, H.-S.; Yoon, K.D.; Son, S.W.; Son, E.D.; et al. Kaempferol tetrasaccharides restore skin atrophy via PDK1 inhibition in human skin cells and tissues: Bench and clinical studies. BioMedicine 2022, 156, 113864. [Google Scholar] [CrossRef] [PubMed]
- Emamian, E.S. AKT/GSK3 signaling pathway and schizophrenia. Front. Mol. Neurosci. 2012, 5, 33. [Google Scholar] [CrossRef] [PubMed]
- Lucas, N.; Cho, W. Phosphatidylserine Binding Is Essential for Plasma Membrane Recruitment and Signaling Function of 3-Phosphoinositide-dependent Kinase-1. J. Biol. Chem. 2011, 286, 41265–41272. [Google Scholar] [CrossRef] [PubMed]
- Noll, R. Kraepelin's `lost biological psychiatry'? Autointoxication, organotherapy and surgery for dementia praecox. Hist. Psychiatry 2007, 18, 301–320. [Google Scholar] [CrossRef] [PubMed]
- Horrobin, D.F. The membrane phospholipid hypothesis as a biochemical basis for the neurodevelopmental concept of schizophrenia. Schizophr. Res. 1998, 30, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.J.; Nazli, A.; Rojas, O.L.; Chege, D.; Alidina, Z.; Huibner, S.; Mujib, S.; Benko, E.; Kovacs, C.; Shin, L.Y.Y.; et al. A role for mucosal IL-22 production and Th22 cells in HIV-associated mucosal immunopathogenesis. Mucosal Immunol. 2012, 5, 670–680. [Google Scholar] [CrossRef]
- Tsounis, E.P.; Triantos, C.; Konstantakis, C.; Marangos, M.; Assimakopoulos, S.F. Intestinal barrier dysfunction as a key driver of severe COVID-19. World J. Virol. 2023, 12, 68–90. [Google Scholar] [CrossRef]
- Fang, S.; Ju, D.; Lin, Y.; Chen, W. The role of interleukin-22 in lung health and its therapeutic potential for COVID-19. Front. Immunol. 2022, 13, 951107. [Google Scholar] [CrossRef]
- Coronas, V.; Arnault, P.; Jégou, J.-F.; Cousin, L.; Rabeony, H.; Clarhaut, S.; Harnois, T.; Lecron, J.-C.; Morel, F. IL-22 Promotes Neural Stem Cell Self-Renewal in the Adult Brain. STEM CELLS 2023, 41, 252–259. [Google Scholar] [CrossRef]
- Rothhammer, V.; Quintana, F.J. The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nat. Rev. Immunol. 2019, 19, 184–197. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Jin, U.-H.; Karki, K.; Jayaraman, A.; Allred, C.; Michelhaugh, S.K.; Mittal, S.; Chapkin, R.S.; Safe, S. Dopamine is an aryl hydrocarbon receptor agonist. Biochem. J. 2020, 477, 3899–3910. [Google Scholar] [CrossRef] [PubMed]
- Fehsel, K.; Schwanke, K.; Kappel, B.; Fahimi, E.; Meisenzahl-Lechner, E.; Esser, C.; Hemmrich, K.; Haarmann-Stemmann, T.; Kojda, G.; Lange-Asschenfeldt, C. Activation of the aryl hydrocarbon receptor by clozapine induces preadipocyte differentiation and contributes to endothelial dysfunction. J. Psychopharmacol. 2022, 36, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Ishima, T.; Iyo, M.; Hashimoto, K. Neurite outgrowth mediated by the heat shock protein Hsp90α: a novel target for the antipsychotic drug aripiprazole. Transl. Psychiatry 2012, 2, e170. [Google Scholar] [CrossRef] [PubMed]
- Sun, L. Recent advances in the development of AHR antagonists in immuno-oncology. RSC Med. Chem. 2021, 12, 902–914. [Google Scholar] [CrossRef] [PubMed]
- De Juan, A.; Segura, E. Modulation of Immune Responses by Nutritional Ligands of Aryl Hydrocarbon Receptor. Front. Immunol. 2021, 12, 645168. [Google Scholar] [CrossRef]
- Salminen, A. Aryl hydrocarbon receptor (AhR) reveals evidence of antagonistic pleiotropy in the regulation of the aging process. Cell. Mol. Life Sci. 2022, 79, 489. [Google Scholar] [CrossRef]
- Ojo, E.S.; Tischkau, S.A. The Role of AhR in the Hallmarks of Brain Aging: Friend and Foe. Cells 2021, 10, 2729. [Google Scholar] [CrossRef]
- Eckers, A.; Jakob, S.; Heiss, C.; Haarmann-Stemmann, T.; Goy, C.; Brinkmann, V.; Cortese-Krott, M.M.; Sansone, R.; Esser, C.; Ale-Agha, N.; et al. The aryl hydrocarbon receptor promotes aging phenotypes across species. Sci. Rep. 2016, 6, 19618–19618. [Google Scholar] [CrossRef]
| INTERVAL | SUSTAINED RECOVERY | EMPLOYED |
|---|---|---|
| 1901- 1920 | 20% | 4.7% |
| 1921- 1940 | 12% | 11.9% |
| 1941- 1955 | 23% | 4.1% |
| 1956- 1975 | 20% | 5.1% |
| 1976- 1995 | 20% | 6.9% |
| Marker Type | Marker Assay | References |
|---|---|---|
| Integrity of gut barrier | IL-22 Singulex-Erenna®® | 155 |
| Translocated microbes | mcfDNA Karius Test®® | 156 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





