Submitted:
31 August 2023
Posted:
06 September 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Things all Babesia infections in dogs have in common
The Babesia rossi and Babesia canis examples
Mortality
Systemic Inflammatory Response Syndrome (SIRS) and multiple Organ Dysfunction Syndrome (MODS)
Organ Pathology
Inflammation
Serum Biochemistry Markers of Disease Severity
Endocrine markers of disease severity
Conclusions
References
- Collett: M.G. Survey of canine babesiosis in South Africa. Journal of the South African Veterinary Association 2000, 71, 180-186.
- Nevils, M.A.; Figueroa, J.V.; Turk, J.R.; Canto, G.J.; Le, V.; Ellersieck, M.R.; Carson, C.A. Cloned lines of Babesia bovis differ in their ability to induce cerebral babesiosis in cattle. Parasitology research 2000, 86, 437-443. [CrossRef]
- Krause, P.J.; Daily, J.; Telford, S.R.; Vannier, E.; Lantos, P.; Spielman, A. Shared features in the pathobiology of babesiosis and malaria. Trends in parasitology 2007, 23, 605-610. [CrossRef]
- Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000, 94 Suppl 1, S1-90.
- Anstey, N.M.; Douglas, N.M.; Poespoprodjo, J.R.; Price, R.N. Plasmodium vivax: clinical spectrum, risk factors and pathogenesis. Advances in parasitology 2012, 80, 151-201.
- S., G.L. Malaria. Clinics in Laboratory Medicine 2010, 30, 93-129.
- Rapsang, A.G.; Shyam, D.C. Scoring systems in the intensive care unit: a compendium. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine 2014, 18, 220.
- Ruys, L.J.; Gunning, M.; Teske, E.; Robben, J.H.; Sigrist, N.E. Evaluation of a veterinary triage list modified from a human five-point triage system in 485 dogs and cats. Journal of Veterinary Emergency and Critical Care 2012, 22, 303-312. [CrossRef]
- Hayes, G.; Mathews, K.; Kruth, S.; Doig, G.; Dewey, C. Illness severity scores in veterinary medicine: what can we learn? Journal of Veterinary Internal Medicine 2010, 24, 457-466.
- Goggs, R.; Dennis, S.; Di Bella, A.; Humm, K.R.; McLauchlan, G.; Mooney, C.; Ridyard, A.; Tappin, S.; Walker, D.; Warman, S. Predicting outcome in dogs with primary immune-mediated hemolytic anemia: results of a multicenter case registry. Journal of Veterinary Internal Medicine 2015, 29, 1603-1610. [CrossRef]
- Leisewitz, A.L.; Goddard, A.; Clift, S.; Thompson, P.N.; de Gier, J.; Van Engelshoven, J.; Schoeman, J.P. A clinical and pathological description of 320 cases of naturally acquired Babesia rossi infection in dogs. Veterinary parasitology 2019, 271, 22-30. [CrossRef]
- Mathe, A.; Voros, K.; Papp, L.; Reiczigel, J. Clinical manifestations of canine babesiosis in Hungary (63 cases). Acta Vet Hung 2006, 54, 367-385. [CrossRef]
- Jackson, A.P.; Otto, T.D.; Darby, A.; Ramaprasad, A.; Xia, D.; Echaide, I.E.; Farber, M.; Gahlot, S.; Gamble, J.; Gupta, D. The evolutionary dynamics of variant antigen genes in Babesia reveal a history of genomic innovation underlying host–parasite interaction. Nucleic acids research 2014, 42, 7113-7131. [CrossRef]
- Matjila, P.T.; Carcy, B.; Leisewitz, A.L.; Schetters, T.; Jongejan, F.; Gorenflot, A.; Penzhorn, B.L. Preliminary evaluation of the BrEMA1 gene as a tool for associating babesia rossi genotypes and clinical manifestation of canine Babesiosis. Journal of clinical microbiology 2009, 47, 3586-3592. [CrossRef]
- Gazzinelli, R.T.; Denkers, E.Y. Protozoan encounters with Toll-like receptor signalling pathways: implications for host parasitism. Nature Reviews Immunology 2006, 6, 895-906. [CrossRef]
- Leoratti, F.M.; Farias, L.; Alves, F.P.; Suarez-Mútis, M.C.; Coura, J.R.; Kalil, J.; Camargo, E.P.; Moraes, S.L.; Ramasawmy, R. Variants in the toll-like receptor signaling pathway and clinical outcomes of malaria. The Journal of infectious diseases 2008, 198, 772-780. [CrossRef]
- Conrad, P.; Thomford, J.; Yamane, I.; Whiting, J.; Bosma, L.; Uno, T.; Holshuh, H.J.; Shelly, S. Hemolytic anemia caused by Babesia gibsoni infection in dogs. Journal of the American Veterinary Medical Association 1991, 199, 601-605.
- Kjemtrup, A.M.; Conrad, P.A. A review of the small canine piroplasms from California: Babesia conradae in the literature. Veterinary parasitology 2006, 138, 112-117. [CrossRef]
- Malherbe, W.D.; Immelman, A.; Haupt, W.H.; Walzl, H.J. The diagnosis and treatment of acid-base deranged dogs infected with Babesia canis. Journal of the South African Veterinary Association 1976, 47, 29-33.
- Malherbe, W.D. A clinico-pathological study of Babesia canis infection in dogs. University of Pretoria, Pretoria, 1968.
- Malherbe, W.D.; Parkin, B.S. Atypical symptomatology in Babesia canis infection. Journal of the South African Veterinary Association 1951, 22, 25-36.
- Uilenberg, G.; Franssen, F.F.; Perie, N.M.; Spanjer, A.A. Three groups of Babesia canis distinguished and a proposal for nomenclature. The Veterinary quarterly 1989, 11, 33-40. [CrossRef]
- Carret, C.; Walas, F.; Carcy, B.; Grande, N.; Precigout, E.; Moubri, K.; Schetters, T.P.; Gorenflot, A. Babesia canis canis, Babesia canis vogeli, Babesia canis rossi: differentiation of the three subspecies by a restriction fragment length polymorphism analysis on amplified small subunit ribosomal RNA genes. J Eukaryot Microbiol 1999, 46, 298-303. [CrossRef]
- Maegraith, B.; Gilles, H.M.; Devakul, K. Pathological processes in Babesia canis infections. Zeitschrift fur Tropenmedizin und Parasitologie 1957, 8, 485-514.
- Baneth, G.; Cardoso, L.; Brilhante-Simões, P.; Schnittger, L. Establishment of Babesia vulpes n. sp.(Apicomplexa: Babesiidae), a piroplasmid species pathogenic for domestic dogs. Parasites & vectors 2019, 12, 1-8. [CrossRef]
- Barash, N.R.; Thomas, B.; Birkenheuer, A.J.; Breitschwerdt, E.B.; Lemler, E.; Qurollo, B.A. Prevalence of Babesia spp. and clinical characteristics of Babesia vulpes infections in North American dogs. Journal of veterinary internal medicine 2019, 33, 2075-2081.
- Camacho, A.T.; Guitian, F.J.; Pallas, E.; Gestal, J.J.; Olmeda, A.S.; Goethert, H.K.; III, S.R.T.; Spielman, A. Azotemia and mortality among Babesia microti-like infected dogs. Journal of veterinary internal medicine 2004, 18, 141-146. [CrossRef]
- Miró, G.; Checa, R.; Paparini, A.; Ortega, N.; González-Fraga, J.L.; Gofton, A.; Bartolomé, A.; Montoya, A.; Gálvez, R.; Mayo, P.P. Theileria annae (syn. Babesia microti-like) infection in dogs in NW Spain detected using direct and indirect diagnostic techniques: clinical report of 75 cases. Parasites & vectors 2015, 8, 1-11. [CrossRef]
- Simões, P.B.; Cardoso, L.; Araújo, M.; Yisaschar-Mekuzas, Y.; Baneth, G. Babesiosis due to the canine Babesia microti-like small piroplasm in dogs-first report from Portugal and possible vertical transmission. Parasites & vectors 2011, 4, 1-6. [CrossRef]
- Zahler, M.; Rinder, H.; Schein, E.; Gothe, R. Detection of a new pathogenic Babesia microti-like species in dogs. Veterinary parasitology 2000, 89, 241-248. [CrossRef]
- Birkenheuer, A.J.; Neel, J.; Ruslander, D.; Levy, M.; Breitschwerdt, E. Detection and molecular characterization of a novel large Babesia species in a dog. Veterinary parasitology 2004, 124, 151-160. [CrossRef]
- Morters, M.K.; Archer, J.; Ma, D.; Matthee, O.; Goddard, A.; Leisewitz, A.L.; Matjila, P.T.; Wood, J.L.N.; Schoeman, J.P. Long-term follow-up of owned, free-roaming dogs in South Africa naturally exposed to Babesia rossi. International journal for parasitology 2020, 50, 103-110. [CrossRef]
- Weingart, C.; Helm, C.S.; Müller, E.; Schäfer, I.; Skrodzki, M.; von Samson-Himmelstjerna, G.; Krücken, J.; Kohn, B. Autochthonous Babesia canis infections in 49 dogs in Germany. Journal of Veterinary Internal Medicine 2023. [CrossRef]
- Rojas, A.; Rojas, D.; Montenegro, V.; Gutiérrez, R.; Yasur-Landau, D.; Baneth, G. Vector-borne pathogens in dogs from Costa Rica: first molecular description of Babesia vogeli and Hepatozoon canis infections with a high prevalence of monocytic ehrlichiosis and the manifestations of co-infection. Veterinary parasitology 2014, 199, 121-128. [CrossRef]
- Di Cataldo, S.; Ulloa-Contreras, C.; Cevidanes, A.; Hernandez, C.; Millan, J. Babesia vogeli in dogs in Chile. Transboundary and emerging diseases 2020, 67, 2296-2299. [CrossRef]
- Beck, R.; Vojta, L.; Mrljak, V.; Marinculić, A.; Beck, A.; Živičnjak, T.; Cacciò, S.M. Diversity of Babesia and Theileria species in symptomatic and asymptomatic dogs in Croatia. International journal for parasitology 2009, 39, 843-848. [CrossRef]
- Liu, P.-C.; Lin, C.-N.; Su, B.-L. Clinical characteristics of naturally Babesia gibsoni infected dogs: A study of 60 dogs. Veterinary Parasitology: Regional Studies and Reports 2022, 28, 100675. [CrossRef]
- Botros, B.A.; Moch, R.W.; Barsoum, I.S. Some observations on experimentally induced infection of dogs with Babesia gibsoni. American journal of veterinary research 1975, 36, 293-296.
- Birkenheuer, A.J.; Levy, M.G.; Savary, K.C.; Gager, R.B.; Breitschwerdt, E.B. Babesia gibsoni infections in dogs from North Carolina. Journal of the American Animal Hospital Association 1999, 35, 125-128. [CrossRef]
- Macintire, D.K.; Boudreaux, M.K.; West, G.D.; Bourne, C.; Wright, J.C.; Conrad, P.A. Babesia gibsoni infection among dogs in the southeastern United States. Journal of the American Veterinary Medical Association 2002, 220, 325-329. [CrossRef]
- Dear, J.D.; Owens, S.D.; Lindsay, L.L.; Biondo, A.W.; Chomel, B.B.; Marcondes, M.; Sykes, J.E. Babesia conradae infection in coyote hunting dogs infected with multiple blood-borne pathogens. Journal of veterinary internal medicine 2018, 32, 1609-1617. [CrossRef]
- Groves, M.G.; Dennis, G.L. Babesia gibsoni: field and laboratory studies of canine infections. Experimental parasitology 1972, 31, 153-159. [CrossRef]
- Matijatko, V.; Mrljak, V.; Kis, I.; Kucer, N.; Forsek, J.; Zivicnjak, T.; Romic, Z.; Simec, Z.; Ceron, J.J. Evidence of an acute phase response in dogs naturally infected with Babesia canis. Veterinary parasitology 2007, 144, 242-250. [CrossRef]
- Solano-Gallego, L.; Trotta, M.; Carli, E.; Carcy, B.; Caldin, M.; Furlanello, T. Babesia canis canis and Babesia canis vogeli clinicopathological findings and DNA detection by means of PCR-RFLP in blood from Italian dogs suspected of tick-borne disease. Veterinary parasitology 2008, 157, 211-221. [CrossRef]
- Wang, J.; Zhang, J.; Kelly, P.; Zheng, X.; Li, M.; You, J.; Huang, K.; Qiu, H.; Wang, Y.; Zhang, R. First description of the pathogenicity of Babesia vogeli in experimentally infected dogs. Veterinary parasitology 2018, 253, 1-7. [CrossRef]
- Arsenault, A.C.; Foley, P.M.; Clancey, N.P. Babesia vulpes in a dog from Prince Edward Island, Canada. The Canadian Veterinary Journal 2022, 63, 589.
- Radyuk, E.; Karan, L. A case of Babesia vulpes infection in a dog in Russia. Veterinary Parasitology: Regional Studies and Reports 2020, 22, 100467.
- Oakley, M.S.; Gerald, N.; McCutchan, T.F.; Aravind, L.; Kumar, S. Clinical and molecular aspects of malaria fever. Trends in parasitology 2011, 27, 442-449. [CrossRef]
- Máthé, A.; Vörös, K.; Papp, L.; Reiczigel, J. Clinical manifestations of canine babesiosis in Hungary (63 cases). Acta Veterinaria Hungarica 2006, 54, 367-385. [CrossRef]
- Brown, A.L.; Shiel, R.E.; Irwin, P.J. Clinical, haematological, cytokine and acute phase protein changes during experimental Babesia gibsoni infection of beagle puppies. Experimental parasitology 2015, 157, 185-196. [CrossRef]
- Bilwal, A.K.; Mandali, G.C.; Tandel, F.B. Clinicopathological alterations in naturally occurring Babesia gibsoni infection in dogs of Middle-South Gujarat, India. Vet World 2017, 10, 1227-1232. [CrossRef]
- Birkenheuer, A.J.; Correa, M.T.; Levy, M.G.; Breitschwerdt, E.B. Geographic distribution of babesiosis among dogs in the United States and association with dog bites: 150 cases (2000-2003). Journal of the American Veterinary Medical Association 2005, 227, 942-947. [CrossRef]
- Crnogaj, M.; Cerón, J.J.; Šmit, I.; Kiš, I.; Gotić, J.; Brkljačić, M.; Matijatko, V.; Rubio, C.P.; Kučer, N.; Mrljak, V. Relation of antioxidant status at admission and disease severity and outcome in dogs naturally infected with Babesia canis canis. BMC Veterinary Research 2017, 13, 1-9. [CrossRef]
- Zygner, W.; Gójska, O.; Rapacka, G.; Jaros, D.; Wędrychowicz, H. Hematological changes during the course of canine babesiosis caused by large Babesia in domestic dogs in Warsaw (Poland). Veterinary parasitology 2007, 145, 146-151. [CrossRef]
- Zaki, A.A.; Attia, M.M.; Ismael, E.; Mahdy, O.A. Prevalence, genetic, and biochemical evaluation of immune response of police dogs infected with Babesia vogeli. Veterinary World 2021, 14, 903. [CrossRef]
- Gülanber, A.; Gorenflot, A.; Schetters, T.P.; Carcy, B. First molecular diagnosis of Babesia vogeli in domestic dogs from Turkey. Veterinary parasitology 2006, 139, 224-230.
- Lee, M.J.; Yu, D.H.; Yoon, J.S.; Li, Y.H.; Lee, J.H.; Chae, J.S.; Park, J. Epidemiologic and clinical surveys in dogs infected with Babesia gibsoni in South Korea. Vector Borne Zoonotic Dis 2009, 9, 681-686. [CrossRef]
- Meinkoth, J.H.; Kocan, A.A.; Loud, S.D.; Lorenz, M.D. Clinical and hematologic effects of experimental infection of dogs with recently identified Babesia gibsoni-like isolates from Oklahoma. Journal of the American Veterinary Medical Association 2002, 220, 185-189. [CrossRef]
- Di Cicco, M.F.; Downey, M.E.; Beeler, E.; Marr, H.; Cyrog, P.; Kidd, L.; Diniz, P.P.V.; Cohn, L.A.; Birkenheuer, A.J. Re-emergence of Babesia conradae and effective treatment of infected dogs with atovaquone and azithromycin. Veterinary parasitology 2012, 187, 23-27. [CrossRef]
- Bodi, J.; Nsibu, C.; Hirayama, K. Immunogenetic mechanisms of black water fever: article review. Gene Technol 2021, 10, 1-8.
- Smith, R.L.; Goddard, A.; Boddapati, A.; Brooks, S.; Schoeman, J.P.; Lack, J.; Leisewitz, A.; Ackerman, H. Experimental Babesia rossi infection induces hemolytic, metabolic, and viral response pathways in the canine host. BMC genomics 2021, 22, 1-16.
- Defauw, P.; Schoeman, J.P.; Leisewitz, A.L.; Goddard, A.; Duchateau, L.; Aresu, L.; Meyer, E.; Daminet, S. Evaluation of acute kidney injury in dogs with complicated or uncomplicated Babesia rossi infection. Ticks Tick Borne Dis 2020, 11, 101406. [CrossRef]
- Jacobson, L.S. The South African form of severe and complicated canine babesiosis: clinical advances 1994-2004. Veterinary parasitology 2006, 138, 126-139. [CrossRef]
- Wang, J.; Applefeld, W.N.; Sun, J.; Solomon, S.B.; Feng, J.; Couse, Z.G.; Risoleo, T.F.; Danner, R.L.; Tejero, J.; Lertora, J. Mechanistic Insights into Cell-free Hemoglobin-induced Injury During Septic Shock. American Journal of Physiology-Heart and Circulatory Physiology 2021. [CrossRef]
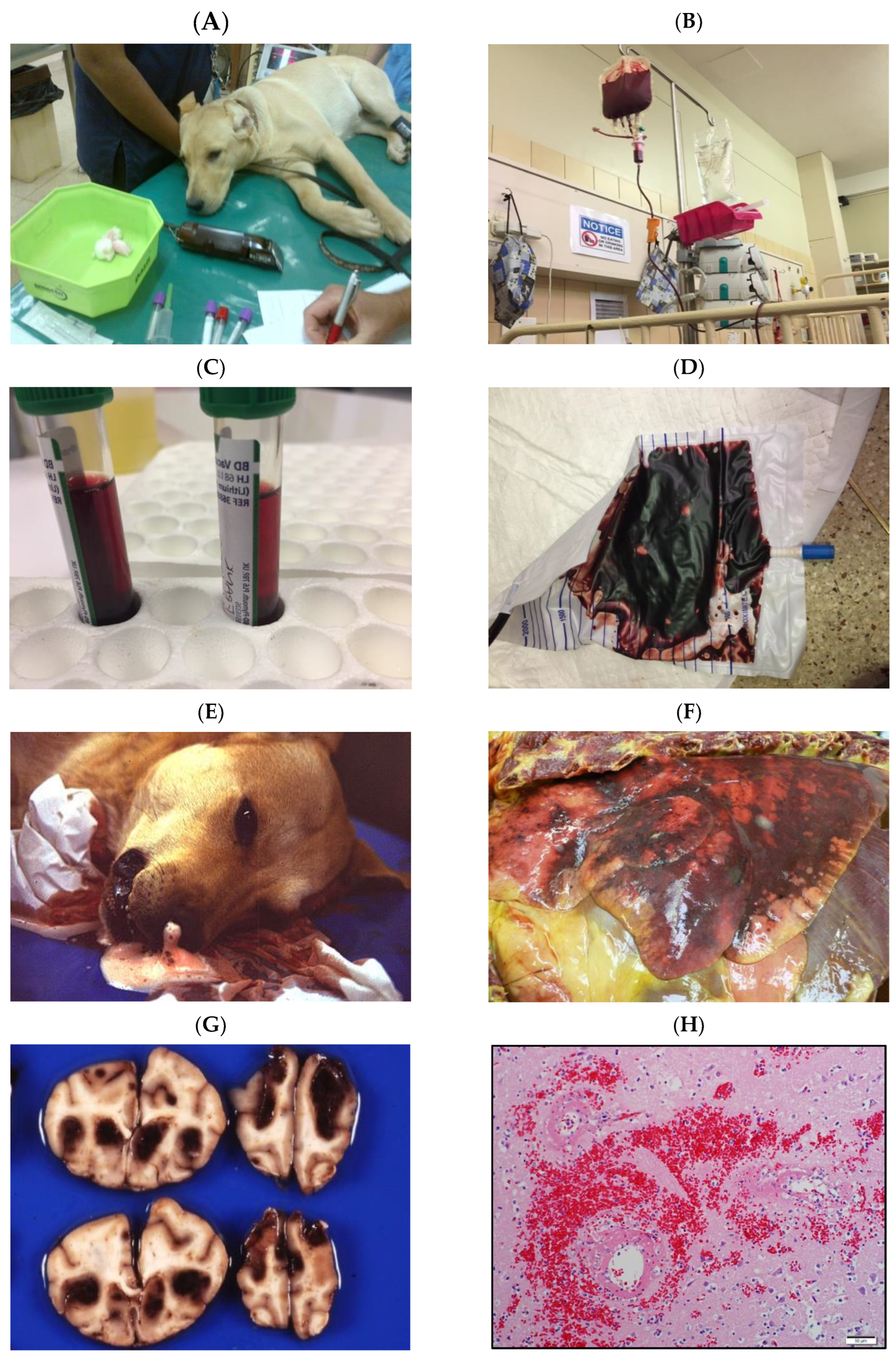
- Henning, A.; Clift, S.J.; Leisewitz, A.L. The pathology of the spleen in lethal canine babesiosis caused by Babesia rossi. Parasite immunology 2020, 42, e12706. [CrossRef]
- Wozniak, E.J.; Barr, B.C.; Thomford, J.W.; Yamane, I.; McDonough, S.P.; Moore, P.F.; Naydan, D.; Robinson, T.W.; Conrad, P.A. Clinical, anatomic, and immunopathologic characterization of Babesia gibsoni infection in the domestic dog (Canis familiaris). The Journal of parasitology 1997, 83, 692-699. [CrossRef]
- Matijatko, V.; Kiš, I.; Torti, M.; Brkljačić, M.; Barić Rafaj, R.; Žvorc, Z.; Mrljak, V. Systemic inflammatory response syndrome and multiple organ dysfunction syndrome in canine babesiosis. Veterinarski Arhiv 2010, 80, 611-626.
- Adaszek, Ł.; Winiarczyk, S.; Skrzypczak, M. The clinical course of babesiosis in 76 dogs infected with protozoan parasites Babesia canis canis. Polish Journal of Veterinary Sciences 2009, 12, 81-87.
- Welzl, C.; Leisewitz, A.L.; Jacobson, L.S.; Vaughan-Scott, T.; Myburgh, E. Systemic inflammatory response syndrome and multiple-organ damage/dysfunction in complicated canine babesiosis. Journal of the South African Veterinary Association 2001, 72, 158-162. [CrossRef]
- Kandasamy, R.; Venkatasubramanian, L.; Loganathasamy, K.; Latha, B.R.; Mani, B. Prognostic markers and their discriminant score in predicting the outcome of Babesia gibsoni infection. Veterinary Record 2021, 188, e29. [CrossRef]
- Bone, R.C.; Sibbald, W.J.; Sprung, C.L. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest 1992, 101, 1481-1483. [CrossRef]
- Okano, S.; Yoshida, M.; Fukushima, U.; Higuchi, S.; Takase, K.; Hagio, M. Usefulness of systemic inflammatory response syndrome criteria as an index for prognosis judgement. The Veterinary record 2002, 150, 245. [CrossRef]
- Vincent, J.-L. Dear SIRS, I’m sorry to say that I don’t like you. Critical care medicine 1997, 25, 372-374.
- Balk, R.A. Systemic inflammatory response syndrome (SIRS): where did it come from and is it still relevant today? Virulence 2014, 5, 20-26. [CrossRef]
- Beletić, A.; Janjić, F.; Radaković, M.; Spariosu, K.; Andrić, J.F.; Chandrashekar, R.; Tyrrell, P.; Radonjić, V.; Balint, B.; Ajtić, J. Systemic inflammatory response syndrome in dogs naturally infected with Babesia canis: Association with the parasite load and host factors. Veterinary parasitology 2021, 291, 109366.
- Schetters, T.P.M.; Kleuskens, J.A.G.M.; Van De Crommert, J.; De Leeuw, P.W.J.; Finizio, A.L.; Gorenflot, A. Systemic inflammatory responses in dogs experimentally infected with Babesia canis; a haematological study. Veterinary parasitology 2009, 162, 7-15. [CrossRef]
- Gourd, N.M.; Nikitas, N. Multiple organ dysfunction syndrome. Journal of intensive care medicine 2020, 35, 1564-1575.
- Osterbur, K.; Mann, F.; Kuroki, K.; DeClue, A. Multiple organ dysfunction syndrome in humans and animals. Journal of veterinary internal medicine 2014, 28, 1141-1151. [CrossRef]
- Lewis, M. Histopathology of cerebral babesiosis in dogs with naturally acquired Babesia rossi infection. University of Pretoria, Pretoria, South Africa, 2022.
- Pardini, D.A. The pathology and pathogenesis of canine cerebral babesiosis. University of Pretoria, Pretoria, South Africa, 2000.
- Ullal, T.; Birkenheuer, A.; Vaden, S. Azotemia and Proteinuria in Dogs Infected with Babesia gibsoni. Journal of the American Animal Hospital Association 2018, 54, 156-160. [CrossRef]
- de Scally, M.P.; Leisewitz, A.L.; Lobetti, R.G.; Thompson, P.N. The elevated serum urea:creatinine ratio in canine babesiosis in South Africa is not of renal origin. Journal of the South African Veterinary Association 2006, 77, 175-178. [CrossRef]
- Martin, C.; Clift, S.; Leisewitz, A. Lung pathology of natural Babesia rossi infection in dogs. Journal of the South African Veterinary Association 2023, 94, 59-69. [CrossRef]
- DeStefano, I.; Wayne, A.; Cudney, S.; Rozanski, E. Successful treatment of suspect Babesia-induced ARDS in a dog using lung-protective positive-pressure ventilation and neuromuscular blockade. Authorea Preprints 2022.
- Leisewitz, A.L.; Jacobson, L.S.; de Morais, H.S.; Reyers, F. The mixed acid-base disturbances of severe canine babesiosis. Journal of veterinary internal medicine/American College of Veterinary Internal Medicine 2001, 15, 445-452.
- Mohr, A.J.; Lobetti, R.G.; van der Lugt, J.J. Acute pancreatitis: a newly recognised potential complication of canine babesiosis. Journal of the South African Veterinary Association 2000, 71, 232-239. [CrossRef]
- Masuda, M.; Otsuka-Yamasaki, Y.; Shiranaga, N.; Iguchi, A.; Uchida, N.; Sato, R.; Yamasaki, M. Retrospective study on intercurrent pancreatitis with Babesia gibsoni infection in dogs. Journal of Veterinary Medical Science 2019, 81, 1558-1563. [CrossRef]
- Goddard, A.; Wiinberg, B.; Schoeman, J.P.; Kristensen, A.T.; Kjelgaard-Hansen, M. Mortality in virulent canine babesiosis is associated with a consumptive coagulopathy. Vet J 2012. [CrossRef]
- Goddard, A.; Wiinberg, B.; Schoeman, J.P.; Kristensen, A.T.; Kjelgaard-Hansen, M. Mortality in virulent canine babesiosis is associated with a consumptive coagulopathy. Vet J 2013, 196, 213-217. [CrossRef]
- Liebenberg, C.; Goddard, A.; Wiinberg, B.; Kjelgaard-Hansen, M.; van der Merwe, L.L.; Thompson, P.N.; Matjila, P.T.; Schoeman, J.P. Hemostatic abnormalities in uncomplicated babesiosis (Babesia rossi) in dogs. Journal of veterinary internal medicine/American College of Veterinary Internal Medicine 2013, 27, 150-156. [CrossRef]
- Dubova, O.; Feshchenko, D.; Bakhur, T.; Zghozinska, O.; Antipov, A.; Rublenko, S.; Goncharenko, V.; Shahanenko, R.; Shahanenko, V. Disseminated intravascular coagulation syndrome as a complication in acute spontaneous canine babesiosis. 2020. [CrossRef]
- de Gopegui, R.R.; Peñalba, B.; Goicoa, A.; Espada, Y.; Fidalgo, L.E.; Espino, L. Clinico-pathological findings and coagulation disorders in 45 cases of canine babesiosis in Spain. The veterinary journal 2007, 174, 129-132. [CrossRef]
- Weltan, S.M.; Leisewitz, A.L.; Goddard, A. A case-controlled retrospective study of the causes and implications of moderate to severe leukocytosis in dogs in South Africa. Veterinary clinical pathology/American Society for Veterinary Clinical Pathology 2008, 37, 164-172. [CrossRef]
- Lobetti, R. Leukaemoid response in two dogs with Babesia canis infection. Journal of the South African Veterinary Association 1995, 66, 182-184.
- Atkinson, B.K.; Thompson, P.; Van Zyl, E.; Goddard, A.; Rautenbach, Y.; Schoeman, J.P.; Mukorera, V.; Leisewitz, A. Kinetics of the inflammatory response during experimental Babesia rossi infection of beagle dogs. Veterinary parasitology 2022, 109717. [CrossRef]
- Rautenbach, Y.A.G.P.N.T.R.J.M.; Leisewitz, A.L. A flow cytometric assessment of the lymphocyte immunophenotypes in dogs naturally infected with Babesia rossi. Veterinary parasitology 2017, 241, 26-34. [CrossRef]
- Yadav, H.; Cartin-Ceba, R. Balance between Hyperinflammation and Immunosuppression in Sepsis. Semin Respir Crit Care Med 2016, 37, 42-50. [CrossRef]
- Inoue, M.; Shinohara, M.L. Hyperinflammation, T cells, and endotoxemia. Oncotarget 2015, 6, 23040-23041. [CrossRef]
- Christensen, M.B.; Langhorn, R.; Goddard, A.; Andreasen, E.B.; Moldal, E.; Tvarijonaviciute, A.; Kirpensteijn, J.; Jakobsen, S.; Persson, F.; Kjelgaard-Hansen, M. Comparison of serum amyloid A and C-reactive protein as diagnostic markers of systemic inflammation in dogs. The Canadian Veterinary Journal 2014, 55, 161.
- Koster, L.S.; Van Schoor, M.; Goddard, A.; Thompson, P.N.; Matjila, P.T.; Kjelgaard-Hansen, M. C-reactive protein in canine babesiosis caused by Babesia rossi and its association with outcome. Journal of the South African Veterinary Association 2009, 80, 87-91. [CrossRef]
- Leisewitz, A.; Goddard, A.; De Gier, J.; Van Engelshoven, J.; Clift, S.; Thompson, P.; Schoeman, J.P. Disease severity and blood cytokine concentrations in dogs with natural Babesia rossi infection. Parasite immunology 2019, 41, e12630. [CrossRef]
- Goddard, A.; Leisewitz, A.L.; Kjelgaard-Hansen, M.; Kristensen, A.T.; Schoeman, J.P. Excessive Pro-Inflammatory Serum Cytokine Concentrations in Virulent Canine Babesiosis. PloS one 2016, 11, e0150113. [CrossRef]
- Galan, A.; Mayer, I.; Rafaj, R.B.; Bendelja, K.; Susic, V.; Ceron, J.J.; Mrljak, V. MCP-1, KC-like and IL-8 as critical mediators of pathogenesis caused by Babesia canis. PloS one 2018, 13, e0190474. [CrossRef]
- Bumby, M.M. Cytological and histopathological bone marrow findings in dogs with natural Babesia rossi infection. University of Pretoria, Pretoria, 2021.
- Rees, P.; Schoeman, J.P. Plasma insulin concentrations in hypoglycaemic dogs with Babesia canis rossi infection. Veterinary parasitology 2008, 152, 60-66. [CrossRef]
- Keller, N.; Jacobson, L.S.; Nel, M.; de Clerq, M.; Thompson, P.N.; Schoeman, J.P. Prevalence and risk factors of hypoglycemia in virulent canine babesiosis. Journal of veterinary internal medicine/American College of Veterinary Internal Medicine 2004, 18, 265-270.
- Zygner, W.; Rapacka, G.; Gojska-Zygner, O.; Dlugosz, E.; Wedrychowicz, H. Biochemical abnormalities observed in serum of dogs infected with large Babesia in Warsaw (Poland). Pol J Vet Sci 2007, 10, 245-253.
- Nel, M.; Lobetti, R.G.; Keller, N.; Thompson, P.N. Prognostic value of blood lactate, blood glucose, and hematocrit in canine babesiosis. Journal of veterinary internal medicine/American College of Veterinary Internal Medicine 2004, 18, 471-476.
- Torti, M.; Kuleš, J.; Matijatko, V.; Brkljačić, M.; Kiš, I.; Gotić, J.; Mrljak, V.; Šmit, I. Acid-base status in canine babesiosis caused by Babesia canis. Veterinarski arhiv 2020, 90, 603-610. [CrossRef]
- Schoeman, J.P.; Herrtage, M.E. Adrenal response to the low dose ACTH stimulation test and the cortisol-to-adrenocorticotrophic hormone ratio in canine babesiosis. Veterinary parasitology 2008, 154, 205-213. [CrossRef]
- Schoeman, J.P.; Herrtage, M.E. Serum thyrotropin, thyroxine and free thyroxine concentrations as predictors of mortality in critically ill puppies with parvovirus infection: a model for human paediatric critical illness? Microbes and infection/Institut Pasteur 2008, 10, 203-207. [CrossRef]
- Schoeman, J.P.; Rees, P.; Herrtage, M.E. Endocrine predictors of mortality in canine babesiosis caused by Babesia canis rossi. Veterinary parasitology 2007, 148, 75-82. [CrossRef]
- Matijatko, V.; Torti, M.; Kiš, I.; Šmit, I.; Štoković, I.; Vranješ-Đurić, S.; Milanović, S.; Mrljak, V.; Brkljačić, M. Serum cor tisol and insulin concentrations in dogs naturally infected Serum cor tisol and insulin concentrations in dogs naturally infected with Babesia canis. Veterinarski arhiv 2014, 84, 551-562.
| Measure of severity | B. rossi | B. canis | B. gibsoni | B. conradea | B. vulpes | B. vogeli |
|---|---|---|---|---|---|---|
| Mortality | 5-35% (multiple studies, hundreds of cases) | 1.5-20% (multiple studies, hundreds of cases) | Low (multiple studies, hundreds of cases) | 25-40% (two small studies) | 22% (one study of 58 cases) | Very low |
| Complicated disease seen | Yes, around 20% of 320 cases | Yes, around 10% of 226 cases. | Occasionally | Occasionally | Unlikely | Very rarely |
| SIRS | Well reported but poorly correlated with outcome | Well reported but poorly correlated with outcome | Not reported but seems possible | Not reported but seems possible | Unlikely | Very rare |
| Single organ failure or MODS | Catastrophic single organ failure of the brain, lungs or kidney are uncommon but carry a very high mortality. MODS well described with much poorer outcomes |
Catastrophic single organ failure of the brain, lungs or kidney are less common than with B. rossi and carry a high mortality. | Evidence of organ dysfunction but catastrophic single organ failure or MODS appears rare. | Not reported but seems possible | Evidence of proteinuric renal failure being the most common cause of death | Very rare. |
| Disease course | Rapidly evolving disease common with most deaths occurring within 24 hours of hospital admission | Disease evolved less acutely than B. rossi | Chronic and waxing and waning disease well described | Appears to be sub-acute | Probably chronic | Infection rarely causes disease |
| Asymptomatic or Self resolving infection | Very rare | Rare | Common | Unknown | Very likely | Asymptomatic infection very common |
| Anemia | Severe anemia is common with blood transfusions frequently required as part of management | Severe anemia is less common and blood transfusions are not usual as part of the management | Severe anemia possible but rare. Blood transfusions rarely required as part of the treatment | Severe anemia possible | Usually mild to moderate | Severe anemia very rare. Blood transfusions not described as part of treatment |
| Extravascular hemolysis | Clinically overt and common | Clinically overt and common | Occurs rarely | Is described | Not described | Occurs rarely |
| Inflammation | Very obviously a profoundly inflammatory disease | Infection results in inflammation but less severe than B. rossi | Evidence of inflammation but less severe and of a more chronic nature | Likely to be moderately inflammatory | Not desxcribed | Host damaging inflammation very rare |
| Hallmarks of poor outcome | Collapse Single organ failure (brain, lung, kidney) Collapse Low body temperature Increased band cell count Elevations in urea (independent of creatinine), creatinine, bilirubin, lactate. Hypoglycemia Increased cortisol, depressed thyroid hormone |
The presence of MODS | Low hemoglobin and elevations in urea, creatine, ALT, ALP and lactate. | Not known | Proteinuria and azotemia | Not known |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





