1. Introduction
Core stabilisation provides the necessary muscular balance and control required about the pelvic-hip complex, trunk (throughout the cervical, thoracic, and lumbar spinal segments) and scapular girdle to effectively preserve the stability and function of the entire human body [
1]. A stable core provides sufficient proximal stability for appropriate distal mobility with the ability to control the movement of the trunk during static or dynamic motor tasks and functions as a connection to force and energy transfer between the central region and the lower and upper limbs [
2,
3,
4]. Thus, a stable and strengthened core is proposed as a key element within the training programmes for fitness and athletic performance enhancement and within musculoskeletal injury prevention and spinal rehabilitation programmes [
5,
6,
7].
The core can be understood as an interdependent kinetic system working synergistically as a united functional structure [
3,
8]. The passive stiffness provided by the osteo-ligamentous structures and the fascial system, alongside the active stiffness supplied by muscular coactivation mechanisms and coordinated by the sensory-motor control system, stabilises the spine and preserves trunk posture during whole-body movements and postural adjustments [
9,
10]. The abdominal and lumbopelvic-hip muscular complex is formed by different deep and superficial layers [
10,
11,
12]. The deep-layer musculature, which includes the internal oblique (IO) and transversus abdominis (TrA) muscles, enhances the segmental control of the lumbar spine by joining the thoracolumbar fascia (TLF) and increasing intra-abdominal pressure during different dynamic or static motor tasks [
13,
14]. The superficial-layer musculature includes the rectus abdominis (RA), external oblique (EO) and erector spinae muscles and contributes to an efficient force and energy transfer between the upper and lower limbs [
13,
14]. The increasing of the muscular stiffness by synergistic cocontraction of all involved core muscles is essential to assure the stabilisation of the lumbar spine and preserve trunk posture [
15,
16,
17].
One of the main goals of any core strengthening and stabilisation programme should be the enhancement of this active muscular stiffness, aiming to improve the mechanical stabilisation of the trunk [
1]. Although research has extensively quantified the effects of different types of core stabilisation exercises, it is still a challenge for fitness professionals, therapists, or athletes to properly know which exercises or which specific variation will best meet their specific requirements [
18]. Abdominal bridging exercises are effective strategies to retrain or strengthen the trunk muscles into the therapy or training processes by decreasing lower back disorders, preventing lower limb injuries, or improving athletic performance [
1,
19,
20,
21,
22,
23]. Into these exercises, the prone bridge or prone plank is a traditional bridging exercise that can cause the cocontraction of the core musculature, producing an abdominal bracing effect by raising the intraabdominal pressure to provide active stiffness that improves lower back stability and function [
24,
25]. Thus, it has been pointed as essential exercise within current athletic, fitness and rehabilitation programs [
1,
8,
22,
23,
26].
It has been stated that the suitable technique to properly perform the prone plank exercise should involve the need to effectively maintain the natural spinal curvatures, throughout the lumbar, thoracic, and cervical regions, within physiological neutral ranges for minimising passive tissue stress [
12,
27,
28]. This is a key question because the way in which the prone plank exercise is performed can provide different loads on the spine and different levels of abdominal activity [
23,
29,
30,
31,
32,
33]. Consequently, clinicians, physical therapists, and strength and conditioning specialists should know in-depth how the core works in this essential core stabilisation exercise for accurately instructing and correcting their patients or athletes to perform the traditional prone plank, maximising its exercise’s safety, functionality, and efficacy. Otherwise, the misunderstanding could make the same exercise less functional, efficient, or even painful [
6,
28].
In this sense, previous studies investigating the prone plank exercise have reported how the activity of the abdominal wall musculature, as well as the rating of perceived exertion (RPE), can be influenced depending on the position of certain joint regions, linking their specific positioning to the magnitude of the abdominal and RPE responses [
32,
34,
35,
36]. Based on these studies, it seems that the specific pelvic position strongly modulates the activity of the abdominal musculature and the RPE during abdominal tasks and bridging exercises [
32,
34,
37,
38,
39]. Likewise, it has been found that the scapular position during the prone plank performance has also an important influence increasing the activation of the core muscles and the RPE values, specifically when a posterior pelvic tilt position is adopted, and the scapulae are in adduction [
34].
In this context, it would be important to monitor and evaluate whether other spinal segments, such as the cranio-cervical region, could also influence and modulate the abdominal response and the perceived neuromuscular fatigue in this bridging exercise. Preliminary studies have revealed how specific variations in head and gaze orientation, mainly by adopting a flexed position, affected trunk muscle activity and lumbar motion during exercises performed in the standing and supine hook-lying positions [
40,
41] or during controlled tasks such as the active leg straight raising test or the forward trunk flexion movement [
42,
43]. Interestingly, while executing the prone plank, it is often observed that in some untrained individuals, in individuals under fatigue, or when a plank variation is too challenging and causes too high core demands, they often shift towards a cranio-cervical flexion posture. However, limited evidence is currently available on the effect that different cranio-cervical postures have in modulating the activity of the core muscles and the perceived exertion during the performance of the traditional prone plank.
Consequently, in this study, we aim to investigate whether the specific position of the head and the cervical spine influences the magnitude of the activity of the core muscles in the performance of the prone plank exercise, measuring muscle activation by surface electromyography (sEMG) and evaluating the perceived neuromuscular fatigue reported by participants. It was hypothesised that performing cranio-cervical flexion would provide greater sEMG responses on overall abdominal musculature. In comparison, cranio-cervical extension would elicit higher sEMG responses on the lumbar extensor musculature. Additionally, it was hypothesised that both flexion and extension postures would elicit more perceived effort on participants than the traditional cranio-cervical neutral posture.
2. Materials and Methods
2.1. Study Design
A cross-sectional study of within-subjects repeated measures was designed to examine the influence of actively maintaining different positions of the cranium and the cervical spinal segment on the sEMG response of six trunk muscles – the right side of the RA, left side of the external oblique (LEO), right side of the external oblique (REO), left side of the internal oblique (LIO), right side of the internal oblique (RIO) and right side of the lumbar portion of the erector spinae (LES) – during the isometric prone plank execution. Thus, the magnitude of the muscle activation and the RPE were examined within each measured variation and compared across the three following testing conditions: the standard performance of the prone plank exercise with a neutral cranio-cervical position (NEUTRAL); a variation from the standard prone plank performed with active cranio-cervical full flexion (FLEXION); and a variation executed with active cranio-cervical full extension (EXTENSION). Additionally, all experimental conditions were recorded from a sagittal plane using a motion capture system to ensure that there were no postural variations in both the cranio-cervical and lumbopelvic-hip complex positions during sEMG data collection.
2.2. Participants
A convenience sample of 20 volunteers (13 men and seven women), recruited from healthy and physically active university students of Sport Sciences Degree, were selected as participants for this study (mean ± SD age: 24.2 ± 3.5 years; height: 1.7 ± 9.5 m; and body mass: 66.4 ± 8.4 kg). All participants had experience in core stabilisation and resistance training (4.4 ± 1.7 years) and were active, performing several physical exercise sessions per week at moderate or vigorous intensity (4.7 ± 1.7 sessions).
Inclusion criteria were as follows: no history of neurological or musculoskeletal disorders; no surgeries in the core region; and no injuries or acute or chronic pain located around the neck, shoulders, elbows, spine, or hips during the past year. Also, prior knowledge and practice on the performance of the traditional prone plank exercise were requested. In addition, it was controlled that all participants had thin skinfolds in the abdominal and supra-iliac areas to obtain the most accurate sEMG signal by minimising the attenuating effects and possible artefacts on the sEMG signal due to excessive subcutaneous adipose tissue lying between the superficial electrodes’ area and the examined abdominal musculature, following criteria from previous research [
44,
45]. Consequently, those with a skinfold thickness bigger than 20 mm were not included as participants (sample mean ± SD values: abdominal skinfold thickness: 12.23 ± 2.45 mm; supra-iliac skinfold thickness: 10.36 ± 1.82 mm). Participants were informed about the aim and the study protocol and signed the written informed consent before participating in the experimental procedures.
2.3. Procedures
Each participant took part in two different sessions: familiarisation and experimental sessions, both separated between 48 – 72 hours. All data collection procedures were conducted at the same laboratory by the same researchers, considering neutral conditions of temperature and humidity. In the familiarisation session, each participant accepted some required restrictions for the subsequent data collection session: no drinks or food intake, or medication or any neurological stimulant used in the 2 – 4 hours before measurements; no performing any moderate or vigorous physical activity during 24 – 48 hours before data collection; and a sleep duration of 7 – 8 hours the night before to the measurement day. All experimental protocols and study procedures follow the ethical principles described in the Declaration of Helsinki of 2013 and they were approved by the University Ethics Committee (UA-2018-11-16). Additionally, this manuscript observes the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) standards [
46].
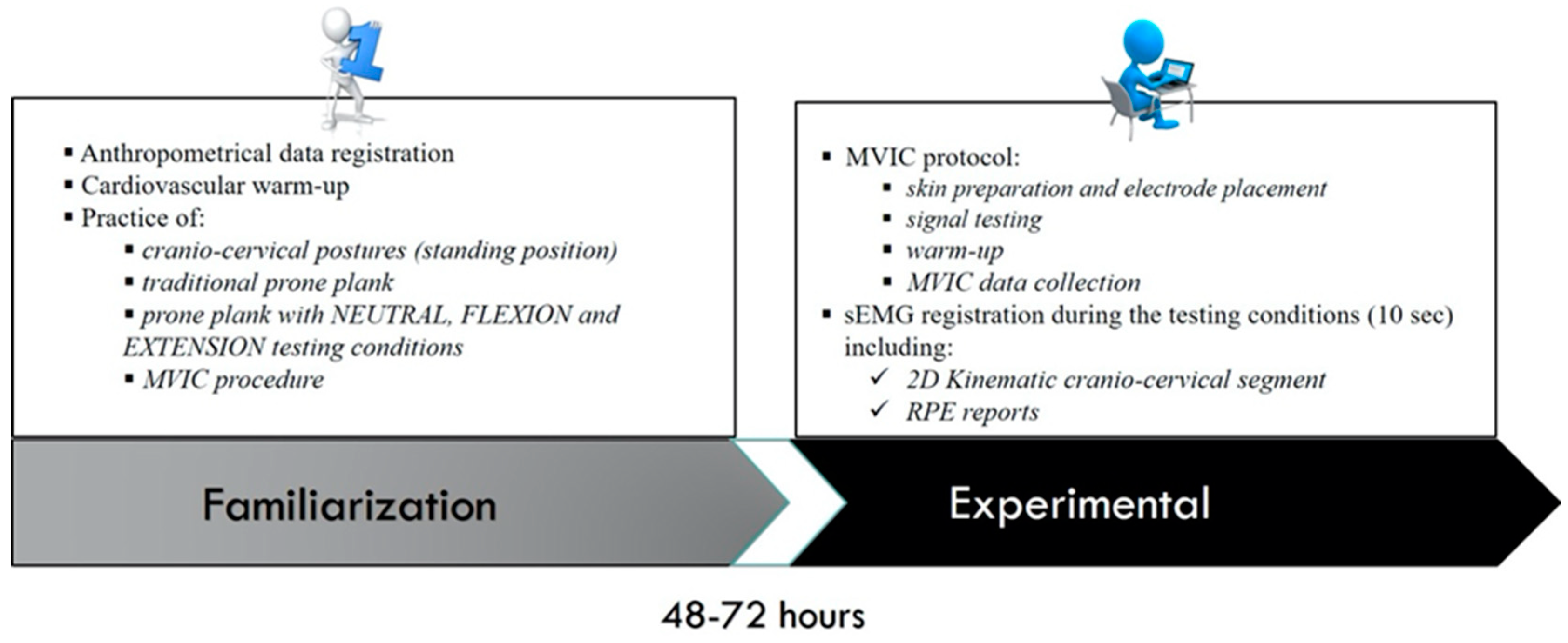
Figure 1 summarises the protocol followed by study participants in the familiarisation and experimental sessions.
2.3.1. Familiarisation Session
Before the data collection session, each participant completed an initial familiarisation session at the same place and at the same time of their experimental session, with the aim to properly know all the study procedures and correctly perform all the experimental conditions. Also, each participant was familiarised with the laboratory facilities and measurement instruments for the sEMG, kinematics, and RPE data collection. The anthropometrical data of the sample were registered starting this session by a skilled III-Level ISAK (International Society for the Advancement of Kinanthropometry) specialist, using instruments and procedures accordingly to the ISAK standards [
47].
After a light warm-up involving joint mobilisation and mild cardiovascular exercise, participants practised under supervision the full flexion-extension range of motion (ROM) of the cranio-cervical spinal segment in a standing position until they understood each proposed cranio-cervical posture. Then, participants practised all the different study conditions until ensuring the correct and controlled performance of each prone plank variation. For this purpose, a detailed description of this exercise was first provided by a certified strength and conditioning specialist. Then, each participant was individually trained and corrected using verbal and manual feedback for accurately performing each plank condition.
Additionally, participants performed a practice trial including maximal voluntary isometric contraction (MVIC) tests and RPE assessments to ensure that they understood these tasks for the experimental session. Finally, they were evaluated on the precise practice of the NEUTRAL, FLEXION and EXTENSION testing conditions, thereby reaching accurate exercise control. Only those who properly executed all the plank variations continued into this study. Ending this session, each participant was informed about the previously described constraints for the data collection session. The duration of the familiarisation session varied between 40–60 min for each participant.
Table 1 summarises the protocols for each testing condition, which were founded on the traditional prone plank protocol, as already have been established in previous research [
31,
32,
34].
2.3.2. Experimental Session
Once participants were familiarised with the study procedures, they took part in the experimental session. sEMG of the analysed core muscles and 2D Body kinematics of the cranio-cervical and lumbopelvic-hip segments were recorded during the performance of the NEUTRAL, FLEXION and EXTENSION testing conditions. The RPE of participants was also collected immediately after every plank condition, using the OMNI Perceived Exertion Scale for Resistance Exercise (OMNI-RES) [
48].
2.3.3. sEMG Instrumentation
The sEMG response of the six core muscles analysed was collected across all experimental plank variations. The sEMG signals were recorded for a 10-s period by telemetry through the Mega WBA® wireless system (Mega Electronics LTD, Kuopio, Finland), using pre-gelled disposable bipolar Ag-AgCl surface electrodes (Arbo Infant Electrodes, Tyco Healthcare, Germany). Electrodes were placed parallel to the muscle fibre orientations with a centre-to-centre spacing of 20 mm [
49]. Previously to the electrode placement, the testing skin area was prepared shaving and cleaning with alcohol wipes the overlying skin region for each examined core muscle. Electrodes were then placed on the right side of the trunk for the RA and LES, assuming their symmetrical activation during isometric abdominal exercises [
50], and on both sides for the IO and EO muscles, looking for possible differences in muscle activation. Electrode positions were chosen according to the procedures of Surface EMG for Non-Invasive Assessment of Muscles (SENIAM) project [
49], and if not obtainable, following related studies [
28,
51,
52]. For the location of the anatomical landmarks, the manual palpation technique was used with a skin marker to correctly point and place every electrode [
53]. Lastly, the quality of the sEMG signal was tested by asking participants to contract the involved musculature by performing basic movements.
2.3.4. sEMG Maximal Voluntary Isometric Contraction Measurements
The sEMG data were normalised as a percentage of MVIC. For the normalisation, before the performance of the testing conditions and after a light warm-up, three MVIC tests against manual resistance were performed for all the analysed muscles. After measurements, the worst set was discarded, and the mean of the two more similar sets were considered for sEMG normalisation, establishing the average root-mean-square (RMS) values of them as MVIC reference values (100% MVIC). The Intraclass Correlation Coefficient (ICC2,1) was used to calculate the intra-session relative reliability of the selected MVICs. The MVIC protocol was performed as established in previous research [
54]. For the RA, participants executed MVICs from a trunk flexion counter-resisted movement (ICC2,1) = 0.999), and MVICs from a lateral bend and twist counter-resisted movements for the EO (ICC2,1= 0.998 for the LEO and 0.999 for the REO) and the IO (ICC2,1 = 0.999 for the LIO and 0.999 for the RIO). For the back-extensor LES muscle, participants performed MVICs in a trunk extension counter-resisted movement from a Biering-Sorensen position (ICC2,1= 0.999). The MVICs were sustained for 5 s, resting for 5 min between the three MVIC sets to reduce the possibility of neuromuscular fatigue. Participants were encouraged with motivating verbal feedback to help them achieve the maximal efforts.
2.3.5. sEMG Data Collection
Three different sets of 10-s isometric contractions for each plank variation were performed from a cranio-cervical posture supervised and corrected by two different researchers. Participants were also ordered to preserve the pelvis, the lumbar and thoracic spinal segments, and the scapulae in a neutral position since changing these joint positions could modify the sEMG activation of the examined muscles [
32,
34,
37]. If participants could not preserve a correct trunk or head posture during the 10 s of data collection, the measurement was discarded and repeated. The order for each plank variation was randomised through a balanced Latin Square method to reduce possible confounding effects on the collected data [
34]. To minimise the probability of residual neuromuscular fatigue, a 5-min rest between conditions was determined.
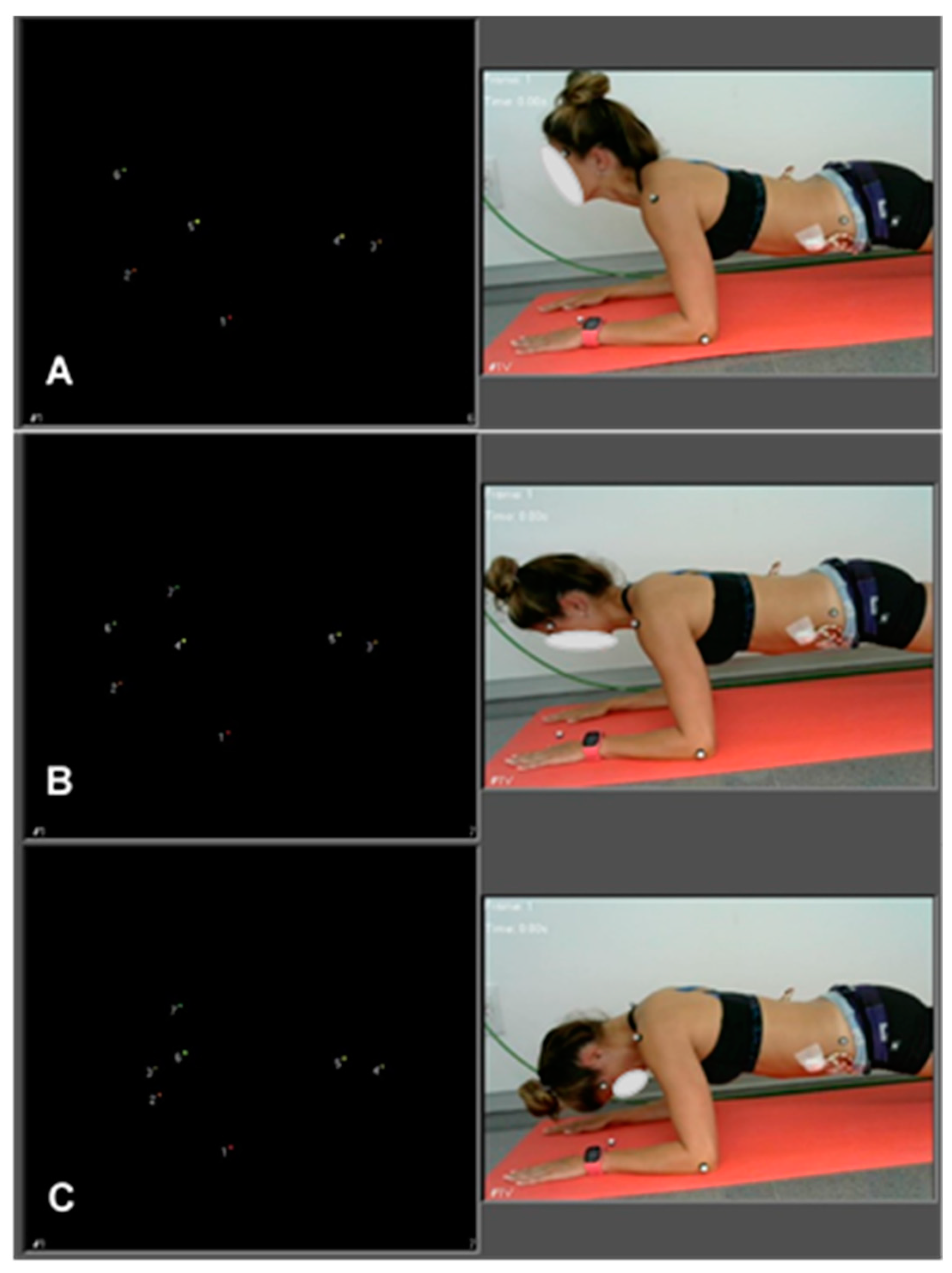
Figure 2 shows images of the performance of the different testing conditions.
2.3.6. sEMG Data Analysis
The sEMG data were recorded using the MegaWin software (MegaWin® 3.0; Mega Electronics LTD), stablishing the sampling frequency at 1000 Hz, and were bandpass filtered (12 - 450 Hz) with a fourth-order Butterworth filter. The analogue signal was transformed to a digital signal through an A/D converter (National Instruments, New South Wales, Australia). Upon visual inspection of all collected data to eliminate any potential measurement artefacts, the raw sEMG signals were registered on a computer for subsequent examination. Later, the average RMS value for all muscles was analysed for a 10-s period with the LabVIEW software package (National Instruments, TX, USA). To calculate the sEMG average RMS values, the length of the time window of the moving RMS method was established at 500 ms. Next, the least reliable set was removed, and the mean of the two most alike sets were used for sEMG data analysis. The intra-session relative reliability of the selected sets was calculated using the ICC(2,1). Apart from the individual sEMG muscle response across conditions, the overall sEMG muscle activity produced in each experimental condition, designated as total intensity (TI), was also considered for later analyses. TI was referred to as the sum of the normalised sEMG values of the six core muscles analysed, as already used in other related studies [
31,
34].
2.3.7. Kinematics Data Collection
Each testing condition was recorded from the sagittal plane through a 2D motion-capture system (Qualisys, Gothenburg, Sweden), controlling that no changes in the cranio-cervical posture occurred during the performance of every plank variation. The 2D motion-capture camera was located 145 cm from the participant and 50 cm from the ground. The lumbopelvic-hip complex was also controlled to remain in a neutral position, as changes in these joint positions can have a significant effect on the SEMG signal amplitude of the muscles studied [
32,
34,
37]. Thus, each specific cranio-cervical position, as well as the shoulder, humerus, hip and pelvis positions were also controlled by placing seven passive retro-reflective markers on the following anatomic locations: cranium (right side of the head, located over the centre of the sphenoid bone (named TEMPLE)); cervical spine (the spinous process of the 7th cervical vertebra (C7)); left and right shoulder, placed on the acromion protuberance); humerus (most caudal point on lateral epicondyle); pelvis (iliac crest (midway between anterior-superior iliac spine and posterior-superior iliac spine, (ASIS-PSIS)) and hip (greater trochanter of the femur (GT)) [
55,
56,
57,
58].
Figure 2 shows the location of the markers. Additionally, one passive retro-reflective marker was also placed on the ground (LAND), in a vertical straight line from the TEMPLE marker, from a neutral cranio-cervical position. The neutral cranio-cervical position was defined as the lying face-down position within the prone plank performance, with a supervised neutral alignment of the cervical spine. This position was established as the starting point and thus as the reference position for angular ROM measurements. Both extremes of the flexion-extension ROM reached by the participants were established as the measuring points of FLEXION and EXTENSION conditions, respectively. Then, the angular ROM between the TEMPLE and C7 as well as the distance from TEMPLE and the LAND, were registered through the software package Qualisys Tracking Manager (Qualisys), monitoring each cranio-cervical posture, controlling each lumbopelvic-hip movement, and detecting the eventual postural changes occurred in every sEMG measurement.
2.3.8. RPE data collection
The 0-10 OMNI-RES scale was utilised to measure the degree of perceived exertion of the different testing conditions [
48]. Each individual RPE was registered at the end of each 10-s trial ensuring that the RPE was referred to the experimental condition performed. Following data collection, the mean of the two most similar sets chosen for sEMG data analysis was applied to the RPE data analysis as well. Therefore, the intra-session relative reliability of these selected sets of RPE was determined using ICC(2,1). A printed copy of the scale was utilised as visual feedback, assisting the participants in their responses.
2.4. Statistical analyses
The SPSS Package, version 24.0 (SPSS Inc. Chicago, IL, USA) was used for the statistical analyses. After testing the normal distribution of the data with the Shapiro-Wilk test (p > 0.05) and verify the homogeneity of the variance with the Levene’s test (p > 0.05), a 2-way (muscle x condition) repeated-measures analysis of variance (ANOVA) was carried out to explore the sEMG differences across muscular responses and experimental conditions. Significant interactions between factors were analysed using DMS post-hoc test. Statistical significance was set at p ≤ 0.05.
The relative reliability of the MVIC tests, the RPE assessments, and the sets of plank variations performed during the experimental session was evaluated using 2-way random effect model ICC(2,1) [
59]. ICC(2,1) values were interpreted according to the following criteria: excellent (0.90-1.00), good (0.70-0.89), fair (0.50-0.69), low (<0.50) [
60]. The confidence interval limits were calculated at 95% for selected sets of plank conditions, TI values and RPE assessments. Effect size (ES) for differences across conditions was estimated using Hedges g [
61], with the following scale to categorise the magnitude of this ES: < 0.2 = trivial; 0.2–0.5 = small; 0.5–0.8 = medium; 0.8–1.3 large; and > 1.3 very large [
61]. All variables are reported as mean ± Standard Deviation (SD).
3. Results
3.1. sEMG Differences Across Muscles
Table 2 shows the mean and SD values of the normalised sEMG muscle response (%MVIC), as well as the ICC(2,1) and 95% confidence interval (CI) values for all analysed core muscles across the different testing conditions. For NEUTRAL, no significant differences on sEMG muscle activity were observed across all abdominal musculature (RA-LEO, p = 0.541; RA-REO, p = 0.264; RA- LIO, p = 0.381; RA-RIO, p = 0.737; LEO-REO, p = 0.656; LEO-LIO, p = 0.828; LEO-RIO, p = 0.768; REO-LIO, p = 0.809; REO-RIO, p = 0.433; LIO-RIO, p = 0.588). However, compared to each abdominal muscle, the sEMG response of the back-muscle LES was significantly lower (LES compared to the RA, REO, LEO, LIO and RIO: p = 0.000).
Similarly, for EXTENSION, no differences on the sEMG muscle activation were detected across all evaluated abdominal muscles (RA-LEO, p = 0.752; RA-REO, p = 0.551; RA- LIO, p = 0.640; RA-RIO, p = 0.646; LEO-REO, p = 0.806; LEO-LIO, p = 0.449; LEO-RIO, p = 0.454; REO-LIO, p = 0.288; REO-RIO, p = 0.292; LIO-RIO, p = 0.994). However, the LES showed significantly lower sEMG activation compared to each abdominal muscle (LES compared to the rest of abdominal musculature: p = 0.000).
However, statistical differences on sEMG muscle activity across all abdominal muscles were found for FLEXION. Particularly, FLEXION elicited a higher sEMG activation of the RA compared to both EO (RA-LEO, p = 0.044; RA-REO, p = 0.002) but not in comparison to both IO (RA-LIO, p = 0.524; RA-RIO, p = 0.645). FLEXION also triggered a higher sEMG response in both IO when compared to the REO (LIO-REO, p = 0.013; RIO-REO, p = 0.008) but not to the LEO (LIO-LEO, p = 0.154; RIO-LEO, p = 0.112). No significant differences were observed when comparing the both sides of external and internal obliques, (REO-LEO, p = 0.352; RIO-LIO, p = 0.860). Finally, the sEMG activation on the LES during FLEXION remained significantly lower in comparison to each one of the analysed abdominal muscles (LES-RA, p = 0.000; LES-LEO, p = 0.000; LES-REO, p = 0.001; LES-LIO, p = 0.000; LES-RIO, p = 0.000).
3.2. sEMG Differences Across Conditions
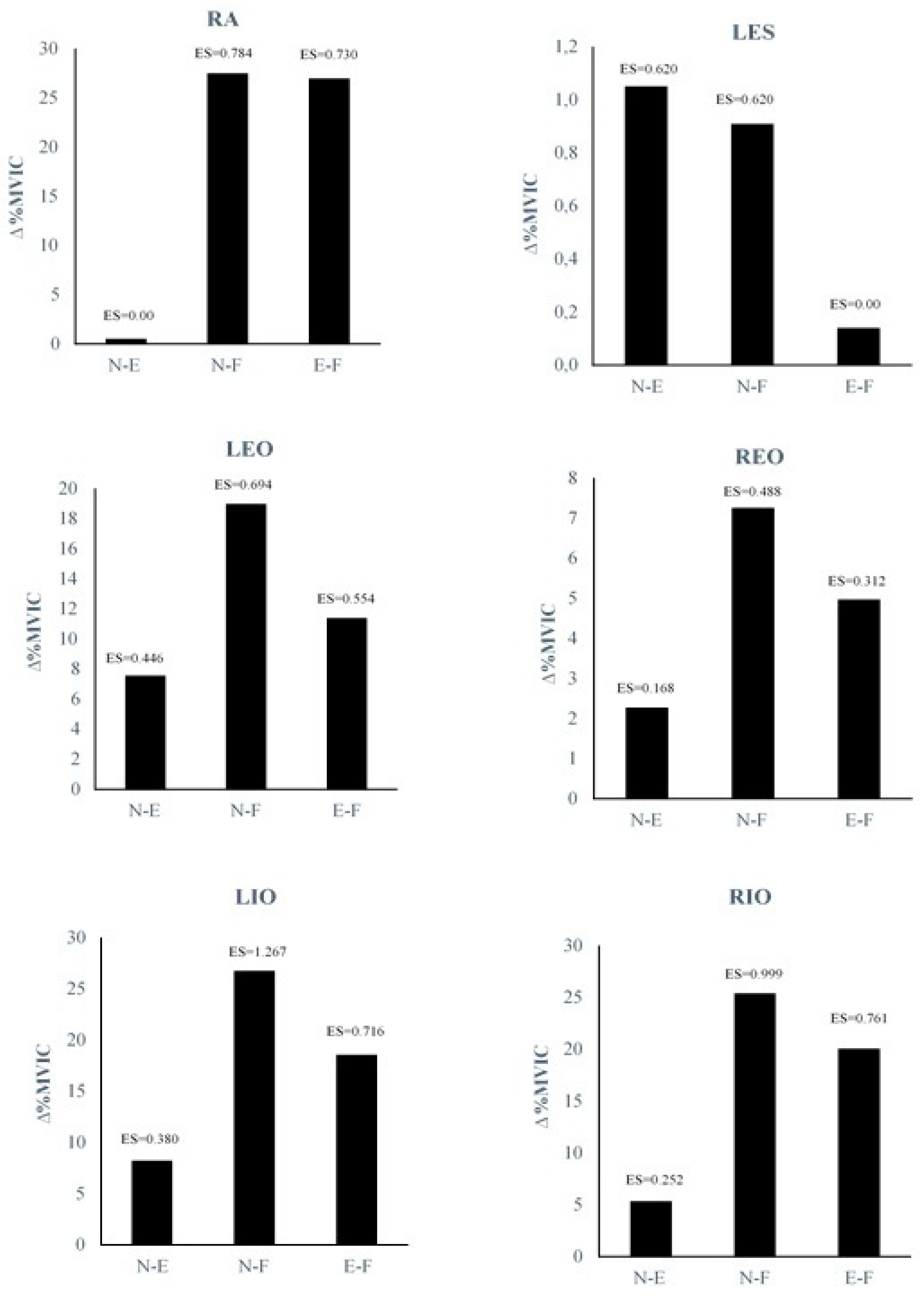
Figure 3 represents the percentage of change in normalised sEMG muscle activity (Δ%MVIC) across the different plank variations for all core muscles examined. The RA showed higher sEMG activation in FLEXION compared to NEUTRAL (p = 0.012) and to EXTENSION (p = 0.013). However, no significant differences were observed for the RA between NEUTRAL and EXTENSION conditions (p = 0.962). The LES showed no significant differences across all experimental conditions (NEUTRAL-FLEXION, p = 0.163; NEUTRAL-EXTENSION, p = 0.110; FLEXION-EXTENSION, p = 0.835). For the LEO, FLEXION elicited a greater sEMG response compared to NEUTRAL (p = 0.047), but not compared to EXTENSION (p = 0.079). Also, no significant differences between NEUTRAL and EXTENSION conditions were found (p = 0.802). For the REO, no statistical differences for FLEXION were observed when compared to NEUTRAL (p = 0.120) or when compared to EXTENSION (p = 0.284). Likewise, no significant differences between NEUTRAL and EXTENSION conditions were detected (p = 0.622). Both the LIO and RIO elicited higher sEMG activation levels in FLEXION in comparison with NEUTRAL (for the LIO: p = 0.001; for the RIO p = 0.002) and EXTENSION (for the LIO: p = 0.015; for the RIO p = 0.011). However, no significant differences were found on the NEUTRO-EXTENSION comparison (for the LIO: p = 0.268; for the RIO p = 0.485).
3.3. Total Intensity and Rating of Perceived Exertion
Table 3 presents mean, SD, and 95% CI of TI, as well as the mean, SD, 95% CI, and ICC(2,1) of RPE values, for the three prone plank variations analysed. Regarding TI values, expressed in %MVIC, the FLEXION variation significantly elicited higher sEMG response in overall core muscles in comparison to the NEUTRAL and EXTENSION variations. Otherwise, no differences were found between the NEUTRAL and EXTENSION conditions (p = 0.489, ES = 0.253). In terms of RPE, both FLEXION and EXTENSION results were significantly greater, compared to NEUTRAL, and showed no significant differences between FLEXION and EXTENSION conditions (p = 0.653, ES = 0.000).
3.4. Kinematic Analysis
The results of the kinematic analysis showed that the angular ROM between C7 and TEMPLE, as well as the distances from the LAND to TEMPLE, did not change for each condition during the 10-s period of the sEMG measurement. Similarly, no changes in ASIS-PSIS and GT marker positions were observed during the experimental conditions in the lumbopelvic-hip complex. Specifically, the averaged full angular ROM for the cranio-cervical flexion-extension, measured from C7 to TEMPLE, was 102.01 ± 17.99º. Within this angular full ROM, the NEUTRAL condition showed measured values of 0º for each participant, as reference point of initial angular ROM. Then, the measured angular values for FLEXION were 60.88 ± 11.14º, and for EXTENSION were 41.13 ± 10.35º. The resulting values for the distance from the LAND to TEMPLE was for NEUTRAL 28.25 ± 2.27 cm; for FLEXION 19.89 ± 2.95 cm; and for EXTENSION 44.84 ± 3.09 cm.
4. Discussion
This study investigated whether the cranio-cervical position influences the core muscle activity when performing the traditional prone plank exercise. Our hypotheses were partially confirmed by showing that the specific cranio-cervical position modulated the abdominal response, providing the greatest sEMG activation by performing the prone plank in a cranio-cervical flexion posture. This shift on the sEMG was significant both in terms of TI and individually in each of the abdominal muscles, although this effect was slighter for the EO. Nevertheless, contrary to our initial hypothesis, the LES activity remained at similar values along the three experimental conditions evaluated, thereby indicating no influence of cranio-cervical position in the measured lower back musculature. Additionally, supporting our initial hypothesis, participants perceived the highest levels of exertion when the cranio-cervical position varied from the neutral position, regardless of the sEMG responses. These findings evidence the influence that cranio-cervical position have in modulating the intensity of core muscle recruitment and the perceived effort of the participants during the performance of the traditional prone plank, particularly when placing the head and the cervical spine in a flexion posture.
4.1. Comparison of sEMG Activation Across Muscles and Conditions
Results from the kinematic controlled sEMG analysis revealed that the intensity of the muscular responses differed amongst testing conditions. To classify as low-to-high intensity of these responses, the criteria of related research were used [
62,
63]. The NEUTRAL condition was considered the reference plank performance for determining the extent of influence of the other two experimental conditions. Both in terms of TI and for each abdominal muscle assessed, this plank variation produced similar levels of moderate activity. Otherwise, the LES activity remained unchanged, showing a low muscle activity – around 5% MVIC – thereby indicating no influence of cranio-cervical position on the lower back muscle activity. The consistency of these findings with previous research indicates a similar standard performance of this traditional bridging exercise [
20,
32,
63,
64]. Interestingly, EXTENSION caused a similar effect on the core activation as NEUTRAL, showing parallel amplitudes of moderate abdominal activity as well as low activity in the LES. In terms of TI, the compounded sEMG response only varied by 2.92% MVIC (ES = 0.253) by placing the head at the end of the cranio-cervical extension range. This slight increase in the sEMG response produced a non-significant variation across muscles, as shown in
Figure 3.
However, when participants were asked to place an active cranio-cervical full flexion posture, they experienced a significant intensification in the magnitude of the overall abdominal response, although its extent was different depending on the muscle group analysed. The greatest sEMG response to FLEXION was detected for the RA and both IO sides. Both muscles almost achieved levels of very high muscle activity, reaching values of 60% MVIC for the RA and around 56% for both sides of the IO. Based on previous research, this may be due to a greater muscular effort to provide the necessary active stiffness by synergistic cocontraction of the deep and superficial core muscles to supply more efficiently the stabilising and weight-bearing demands for this FLEXION variation [
10,
11,
12,
16,
17,
31]. For the EO muscles, the sEMG response was moderate, differing slightly between both EO sides, and did not change for the LES which continued showing low levels of muscle activity in FLEXION as well.
When comparing across conditions, the sEMG increase from NEUTRAL to FLEXION highlights a large effect for the RA and IO activity and a small effect for the LES and EO muscles, as can be seen in
Figure 3. A similar effect occurred when comparing FLEXION and EXTENSION – but milder compared to NEUTRAL –. The integrated sEMG response of TI significantly raised by 15.59% MVIC by placing the head to the end of the flexion range. This effect was similar but smaller when comparing from the extension to the flexion ranges, with a significant variation of 12.67% MVIC. Therefore, it can be concluded that cranio-cervical flexion effectively influences abdominal activation, increasing neuromuscular recruitment during prone plank.
4.2. Comparison of RPE across conditions
The results of the RPE assessments revealed that the intensity of the perceptual responses differed between the test conditions. Participants perceived a low effort during the NEUTRAL performance of the prone plank. However, the reported exertion was higher only by modifying the cranio-cervical position from NEUTRAL to FLEXION, showing a significant variation of 1.53 points in the OMNI-RES scale, according to the sEMG response. Interestingly, despite the no change in sEMG activity, the perceived level of effort had a significant increase of 1.30 points when switching from NEUTRAL to EXTENSION. However, no differences were found in the RPE between FLEXION and EXTENSION, although there were significant differences in sEMG activity. RPE has previously been used as an indicator of exercise intensity and neuromuscular fatigue of the core muscles for this stabilisation bridge exercise [
35,
36]. Related studies have reported how different pelvic and scapular positions, as well as the performance of specific lumbar stabilisation manoeuvres, can modulate participants' RPE and intensify perceived neuromuscular fatigue when the prone plank differs from traditional performance [
31,
34]. In this sense, our findings would seem to corroborate the fact that perceived neuromuscular fatigue is affected when the prone plank differs from typical performance by showing how participants rated the highest levels of exertion when the cranio-cervical segment was modified from the natural alignment of the cervical spine, increasing their RPE regardless of core muscle activity.
4.3. Biomechanical foundations and hypotheses
The suitable technique to perform the prone plank should involve that the core stabilising system should be able to provide a proper muscle activation while effectively preserve the neutral zone of the spine by maintaining all the natural spinal curvatures within physiologic ranges to minimise the passive tissue stress [
12,
27,
28]. This need of controlling the spine posture requires to know in depth how the core works in this essential stabilisation exercise for instructing and correcting patients or athletes to achieve an appropriate muscle activation and spine posture [
6,
28]. Previous studies of the prone plank have reported how the abdominal activity can be influenced by the position of certain joint regions, linking their specific position to the magnitude of the sEMG and RPE response [
32,
34,
37,
38,
39]. Consequently, it was necessary to test whether the cranio-cervical region could influence the abdominal response during the prone plank, as this aspect remains unclear.
This appears to be the first study investigating this question. Hence, there is limited scientific evidence linking these variables. The relationship between cranio-cervical posture and abdominal activation has previously been investigated only in a few studies from the hook-lying supine position [
40,
41,
42,
65]. Their results are consistent with our study, showing that the cranio-cervical flexion significantly increased RA and IO activity when compared to neutral and extension positions. Thus, it could be suggested that this relationship seems to be synergistic, both in supine and prone abdominal tasks, increasing the stiffness of the core when the cranio-cervical region tends towards the flexion position. This hypothesis could explain why, when a prone plank variation is too challenging for some untrained individuals or some fatigued athletes, they may shift towards cranio-cervical flexion, perhaps instinctively seeking a cranio-cervical position that could involve more abdominal stiffness. Although this is a reasonable assumption, it needs to be confirmed by further research.
However, the possible biomechanical linking mechanisms explaining why this phenomenon occurs remain unclear. It can be assumed that the enhancement of the sEMG response is due, among other factors, to an increase in neural muscle recruitment [
66]. When the contraction is isometric, as occurring in the prone plank exercise, this increase in abdominal recruitment reflects a greater production of force and muscular stiffness to stabilise the trunk [
15,
16]. This suggests that the active cranio-cervical flexion may have had a greater stiffening effect on the abdominal muscles, which would ultimately enhance trunk stabilisation during the exercise performance. This phenomenon could be related to the translation of the neck and head into a flexed posture, which would modify the moment arm around the proximal axis of rotation in the cervico-thoracic spine, inducing greater muscular stiffness in the cervical region [
67]. If this were the case, it would seem that this stiffening effect could facilitate greater abdominal stiffness, linked via the fascial system from the cervical region towards the lumbar region via the postural posterior chain [
68,
69]. Nevertheless, testing these hypotheses will require future research.
Whatever the case, considering the ergonomic and security aspects of the exercise, it is important to note that both the FLEXION and EXTENSION conditions involve end-range postures that may expose the cervico-thoracic spine to greater compressive loads [
67]. From a biomechanical perspective, considering the multi-segmental muscular attachments of the neck and head muscles and the presumably greater muscle activity of the head and neck flexor and extensor muscles actively maintaining these end-range postures, it would be reasonable to assume that higher levels of compressive loading may occur within the cranio-cervical area during these variations of the prone plank [
70,
71]. Consequently, the unnatural curved configuration of the cervical region adopted in these postures could damage the spine more than the natural neutral position, increasing the compressive loads and thus creating a focal point of stress that can lead to postural pain [
68,
72]. Not surprisingly, these two postures were coupled with greater perceived effort in participants than the neutral posture. But curiously, it was not clear whether these RPE values were related to the sEMG response. It could be speculated that this increased RPE when varying the cranio-cervical posture was not only elicited by muscle activation but probably also because these end-range postures with non-physiological curvatures involved discomfort, especially arising from the hyperextension of the cervical spine during the EXTENSION condition. In fact, there were reports of discomfort during extension by some participants, although they did not have neck pain. In conclusion, due to this increased mechanical stress on the cervical facet joints, particularly when performing the extended position, and considering that this position does not significantly challenge the abdominal musculature compared to the neutral position, it would be discouraged to use the full range of extension during the prone plank exercise.
Finally, the present results show that the only muscle whose sEMG activity did not vary significantly was the LES, showing minimal demands for maintaining the static prone plank posture regardless of cranio-cervical position. This finding follows previous research showing how lumbar activity remains lower during this bridging exercise when performed in a neutral cranio-cervical position [
20,
32,
63,
64]. The lack of effect of EXTENSION on LES activity could be explained biomechanically, as this posture is achieved via the thoracic and cervical spinal extensors and would therefore not require activation of the lumbar extensors [
73]. Future studies evaluating sEMG activation on the thoracic or cervical components of the back-erector musculature when performing different cranio-cervical positions in the prone plank should be addressed.
4.4. Practical Applications and Implications for Future Practice
The way in which the prone plank exercise is executed is essential since it can involve different loads on the spine and different levels of core activation [
29,
30,
31,
32,
34]. Consequently, it is important to investigate all the variables influencing the proper performance of this exercise because, otherwise, this misunderstanding could make the same exercise painful [
6,
28]. In this sense, the present findings provide a new understanding of the behaviour of the trunk musculature in this essential core exercise. Therefore, when using the prone plank as part of core stabilisation training, clinicians, physiotherapists, and fitness professionals should consider, this demonstrated increase in sEMG during FLEXION and no change in sEMG during EXTENSION, when compared to NEUTRAL.
Although the different cranio-cervical positions in the prone plank and the corresponding spinal loads for each of these positions need to be evaluated in future studies, the influence of these postures on core muscle activity has been described in this study. Knowledge of these results could help to graduate the intensity of muscle recruitment during the prone plank based on the influence that the changes produced in the cranio-cervical region have on the sEMG activity of the core musculature. In addition, these findings may be useful in providing practical guidance on the initial challenge, corrective technique, progression, and choice of exercise variation.
Our findings also indicate that future studies evaluating the core sEMG activity during bridging exercises should monitor not only the pelvic and shoulder girdle areas, following previous research [
32,
34], but also the cranio-cervical region. Moreover, when performing field tests using the prone plank protocol to assess the postural control of the lumbar spine, the posture of the cranio-cervical region should be controlled to guarantee the validity of the evaluations. Additionally, future research should assess the extent to which the cranio-cervical region and other pelvic, scapular and/or limb positions interact and influence each other during the prone plank or other bridging exercises such as side and back bridges, to gain a deeper understanding of trunk muscle behaviour during core stabilisation training.
The present findings have some methodological limitations. First, the relatively small sample size of 20 participants could have affected the results, principally to explain why some statistical effects on abdominal muscles were not more clearly observed, especially related to the bilateral differences in EO muscle activity. Therefore, more research with a further sample size should be proposed to clarify the activity on the EO muscles. Second, this investigation included only healthy participants, experienced in core stabilisation training, without back or neck pain or disorders. Although analogous findings could be expected in clinical populations, it could be possible that the existence of injuries or back or neck pain could result in different sEMG responses [
74]. Consequently, these findings cannot directly extrapolate to symptomatic populations. Further cross-sectional studies with symptomatic participants should be addressed to prove our results in these clinical samples.
5. Conclusions
The results showed that FLEXION resulted in the most challenging plank variation for the core by providing the greatest sEMG responses, whereas EXTENSION did not enhance the abdominal sEMG response from the NEUTRAL performance. In addition, results evidenced the no influence of the cranio-cervical region on the lumbar sEMG response. Performance of both FLEXION and EXTENSION caused more perceived exertion in participants than NEUTRAL performance, regardless of abdominal sEMG activity. These findings evidence the influence of the cranio-cervical region in effectively modulating the muscle activation of the abdominal wall and RPE of the participants depending on its specific posture during the plank performance. These findings may provide physical therapists and fitness professionals with new guidelines that should be considered when using this exercise as part of core stabilisation training in rehabilitation and sports programmes.
Author Contributions
Conceptualization, JM.C.T. and M.G.J.; methodology, M.G.J., J.K, S.H.S.; formal analysis, JM.C.T. and M.G.J..; investigation, M.G.J.; S.H.S; J.K.; data curation, M.G.J and J.K..; writing—original draft preparation, M.G.J.; S.H.S.; writing—review and editing, M.G.J., S.H.S and JM.C.T.; project administration, JM.C.T..; funding acquisition, M.G.J and JM.C.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Consellería de Educación, Investigación, Cultura y Deporte de la Generalitat Valenciana, and European Social Fund (European Union), Grant Project Number ACIF/2016/048.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the I the University of Alicante Ethics Committee (UA-2018-11-16).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to thank the participants for their time and effort.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hoogenboom, B.J.; Kiesel, K. 74 - Core Stabilization Training A2 - Giangarra, Charles E.; Fourth Edi.; Elsevier Inc., 2018; ISBN 978-0-323-39370-6.
- Vera-García, F.J.; Barbado, D.; Moreno-Pérez, V.; Hernández-Sánchez, S.; Juan-Recio, C.; Elvira, J.L.L. Core stability. Concepto y aportaciones al entrenamiento y la prevención de lesiones. Rev. Andaluza Med. del Deport. 2015, 8, 79–85. [Google Scholar] [CrossRef]
- Wirth, K.; Hartmann, H.; Mickel, C.; Szilvas, E.; Keiner, M.; Sander, A. Core Stability in Athletes: A Critical Analysis of Current Guidelines. Sport. Med. 2017, 47, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Willardson, J.M. Core stability training: applications to sports conditioning programs. J. strength Cond. Res. 2007, 21, 979–85. [Google Scholar] [CrossRef] [PubMed]
- Huxel Bliven, K.C.; Anderson, B.E. Core Stability Training for Injury Prevention. Sport. Heal. A Multidiscip. Approach 2013, 5, 514–522. [Google Scholar] [CrossRef]
- McGill, S. Core Training: Evidence Translating to Better Performance and Injury Prevention. Strength Cond. J. 2010, 32, 33–46. [Google Scholar] [CrossRef]
- Behm, D.G.; Drinkwater, E.J.; Willardson, J.M.; Cowley, P.M. The use of instability to train the core musculature. Appl. Physiol. Nutr. Metab. 2010, 35, 91–108. [Google Scholar] [CrossRef]
- La Scala Teixeira, C. V.; Evangelista, A.L.; Silva, M.S.; Bocalini, D.S.; Da Silva-Grigoletto, M.E.; Behm, D.G. Ten Important Facts about Core Training. ACSM’s Heal. Fit. J. 2019, 23, 16–21. [Google Scholar] [CrossRef]
- Akuthota, V.; Nadler, S.F. Core strengthening. Arch. Phys. Med. Rehabil. 2004, 85, S86–92. [Google Scholar] [CrossRef]
- Borghuis, J.; Hof, A.L.; Lemmink, K.A.P.M. The Importance of Sensory-Motor Control in Providing Core Stability. Sport. Med. 2008, 38, 893–916. [Google Scholar] [CrossRef]
- Bergmark, A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop. Scand. Suppl. 1989, 230, 1–54. [Google Scholar] [CrossRef]
- Panjabi, M.M. The Stabilizing System of the Spine. Part I. Function, Dysfunction, Adaptation, and Enhancement. J. Spinal Disord. 1992, 5, 383–389. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M. Low Back Stability: From Formal Description to Issues for Performance and Rehabilitation. Exerc. Sport Sci. Rev. 2001, 29, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core Stability Exercise Principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef]
- Kavcic, N.; Grenier, S.; McGill, S.M. Determining the stabilizing role of individual torso muscles during rehabilitation exercises. Spine (Phila. Pa. 1976). 2004, 29, 1254–65. [Google Scholar] [CrossRef]
- van Dieën, J.H.; Cholewicki, J.; Radebold, A. Trunk Muscle Recruitment Patterns in Patients With Low Back Pain Enhance the Stability of the Lumbar Spine. Spine (Phila. Pa. 1976). 2003, 28, 834–841. [Google Scholar] [CrossRef]
- McGill, S.M.; Grenier, S.; Kavcic, N.; Cholewicki, J. Coordination of muscle activity to assure stability of the lumbar spine. J. Electromyogr. Kinesiol. 2003, 13, 353–359. [Google Scholar] [CrossRef]
- Byrne, J.M.; Bishop, N.S.; Caines, A.M.; Crane, K.A.; Feaver, A.M.; Pearcey, G.E.P. Effect of Using a Suspension Training System on Muscle Activation During the Performance of a Front Plank Exercise. J. Strength Cond. Res. 2014, 28, 3049–3055. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Lewis, C.; Pecson, A.; Imamura, R.; Andrews, J.R. Muscle Activation Among Supine, Prone, and Side Position Exercises With and Without a Swiss Ball. Sports Health 2016, 8, 372–379. [Google Scholar] [CrossRef]
- Imai, A.; Kaneoka, K.; Okubo, Y.; Shiina, I.; Tatsumura, M.; Izumi, S.; Shiraki, H. Trunk Muscle Activity During Lumbar Stabilization Exercises on Both a Stable and Unstable Surface. J. Orthop. Sport. Phys. Ther. 2010, 40, 369–375. [Google Scholar] [CrossRef]
- Maeo, S.; Takahashi, T.; Takai, Y.; Kanehisa, H. Trunk muscle activities during abdominal bracing: comparison among muscles and exercises. J. Sports Sci. Med. 2013, 12, 467–74. [Google Scholar]
- Vera-García, F.J.; Barbado, D.; Moreno-Pérez, V.; Hernández-Sánchez, S.; Juan-Recio, C.; Elvira, J.L.L. Core stability: Evaluación y criterios para su entrenamiento. Rev. Andaluza Med. del Deport. 2015, 8, 130–137. [Google Scholar] [CrossRef]
- Oliva-Lozano, J.M.; Muyor, J.M. Core muscle activity during physical fitness exercises: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 1–42. [Google Scholar] [CrossRef]
- Hibbs, A.E.; Thompson, K.G.; French, D.; Wrigley, A.; Spears, I. Optimizing performance by improving core stability and core strength. Sports Med. 2008, 38, 995–1008. [Google Scholar] [CrossRef]
- Myrtos, C.D. Low Back Disorders. Evidence-Based Prevention and Rehabilitation. J. Can. Chiropr. Assoc. 2012, 56, 76. [Google Scholar]
- Arundale, A.J.H.; Bizzini, M.; Giordano, A.; Hewett, T.E.; Logerstedt, D.S.; Mandelbaum, B.; Scalzitti, D.A.; Silvers-Granelli, H.; Snyder-Mackler, L. Exercise-Based Knee and Anterior Cruciate Ligament Injury Prevention. J. Orthop. Sport. Phys. Ther. 2018, 48, A1–A42. [Google Scholar] [CrossRef] [PubMed]
- Faciszewski, T. Biomechanics of Spine Stabilization. Spine J. 2001, 1, 304–305. [Google Scholar] [CrossRef]
- McGill, S.M.; Karpowicz, A. Exercises for Spine Stabilization: Motion/Motor Patterns, Stability Progressions, and Clinical Technique. Arch. Phys. Med. Rehabil. 2009, 90, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Grenier, S.G.; McGill, S.M. Quantification of Lumbar Stability by Using 2 Different Abdominal Activation Strategies. Arch. Phys. Med. Rehabil. 2007, 88, 54–62. [Google Scholar] [CrossRef]
- Scannell, J.P.; McGill, S.M. Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living. Phys. Ther. 2003, 83, 907–17. [Google Scholar] [CrossRef]
- García-Jaén, M.; Cortell-Tormo, J.M.; Hernández-Sánchez, S.; Tortosa-Martínez, J. Influence of abdominal hollowing maneuver on the core musculature activation during the prone plank exercise. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Contreras, B.; Tiryaki-Sonmez, G.; Willardson, J.M.; Fontana, F. An electromyographic comparison of a modified version of the plank with a long lever and posterior tilt versus the traditional plank exercise. Sport. Biomech. 2014, 13, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Calatayud, J.; Casaña, J.; Martín, F.; Jakobsen, M.D.; Colado, J.C.; Andersen, L.L. Progression of Core Stability Exercises Based on the Extent of Muscle Activity. Am. J. Phys. Med. Rehabil. 2017, 96, 694–699. [Google Scholar] [CrossRef] [PubMed]
- Cortell-Tormo, J.M.; García-Jaén, M.; Chulvi-Medrano, I.; Hernández-Sánchez, S.; Lucas-Cuevas, Á.G.; Tortosa-Martínez, J. Influence of scapular position on the core musculature activation in the prone plank exercise. J. Strength Cond. Res. 2017, 31, 2255–2262. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Montecinos, C.; Bustamante, A.; Candia-González, M.; González-Bravo, C.; Gallardo-Molina, P.; Andersen, L.L.; Calatayud, J. Perceived physical exertion is a good indicator of neuromuscular fatigue for the core muscles. J. Electromyogr. Kinesiol. 2019, 49, 102360. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Steffl, M.; Glenney, S.S.; Green, M.; Cashwell, L.; Prajerova, K.; Bunn, J. The prone bridge test: Performance, validity, and reliability among older and younger adults. J. Bodyw. Mov. Ther. 2018, 22, 385–389. [Google Scholar] [CrossRef]
- Workman, J.C.; Docherty, D.; Parfrey, K.C.; Behm, D.G. Influence of pelvis position on the activation of abdominal and hip flexor muscles. J. Strength Cond. Res. 2008, 22, 1563–1569. [Google Scholar] [CrossRef]
- Drysdale, C.L.; Earl, J.E.; Hertel, J. Surface Electromyographic Activity of the Abdominal Muscles during Pelvic-Tilt and Abdominal-Hollowing Exercises. J. Athl. Train. 2004, 39, 32–36. [Google Scholar]
- Vezina, M.J.; Hubley-Kozey, C.L. Muscle activation in therapeutic exercises to improve trunk stability. Arch. Phys. Med. Rehabil. 2000, 81, 1370–1379. [Google Scholar] [CrossRef]
- García-Jaén, M.; Sanchis-Soler, G.; Casanova-Juliá, M.; Sebastia-Amat, S.; Cortell-Tormo, J.M. Can the craniocervical position modulate trunk muscle activation during a deadlift? A preliminary electromyographical analysis comparing conventional and sumo variations. J. Phys. Educ. Sport 2022, 22, 2904–2912. [Google Scholar] [CrossRef]
- Su, J.G.; Won, S.J.; Gak, H. Effect of craniocervical posture on abdominal muscle activities. J. Phys. Ther. Sci. 2016, 28, 654–657. [Google Scholar] [CrossRef]
- Takasaki, H.; Okubo, Y. Deep Neck Flexors Impact Rectus Abdominis Muscle Activity During Active Straight Leg Raising. Int. J. Sports Phys. Ther. 2020, 15, 1044–1051. [Google Scholar] [CrossRef] [PubMed]
- Beaudette, S.M.; Briar, K.J.; Mavor, M.P.; Graham, R.B. The effect of head and gaze orientation on spine kinematics during forward flexion. Hum. Mov. Sci. 2020, 70, 102590. [Google Scholar] [CrossRef] [PubMed]
- Chanthapetch, P.; Kanlayanaphotporn, R.; Gaogasigam, C.; Chiradejnant, A. Abdominal muscle activity during abdominal hollowing in four starting positions. Man. Ther. 2009, 14, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Neumann, P.; Gill, V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2002, 13, 125–32. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. ; STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (London, England) 2007, 370, 1453–7. [Google Scholar] [CrossRef]
- Marfell-Jones, M. J. , Stewart, A. D., de Ridder, J.H. International standards for anthropometric assessment.; International Society for the Advancement of, Kinanthropometry., Ed.; Open Polytechnic of New Zealand’s institutional digital repository for research: Wellington, New Zealand, 2012; ISBN 9780620362078. [Google Scholar]
- Robertson, R.J.; Timmer, J.; Dube, J.; Frazee, K.; Goss, F.L.; Dixon, C.; Rutowski, J.; Andreacci, J.; Lenz, B. Concurrent Validation of the OMNI Perceived Exertion Scale for Resistance Exercise. Med. Sci. Sport. Exerc. 2005, 35, 333–341. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Rutkowska-Kucharska, A.; …, A.S.-A. of bioengineering; 2009, undefined Symmetry of muscle activity during abdominal exercises. Acad. Rutkowska-Kucharska, A Szpala, E PieciukActa Bioeng. Biomech. 2009•academia.edu.
- Ng, J.K.; Kippers, V.; Richardson, C.A. Muscle fibre orientation of abdominal muscles and suggested surface EMG electrode positions. Electromyogr. Clin. Neurophysiol. 1998, 38, 51–8. [Google Scholar]
- Criswell, E. Cram’s introduction to surface electromyography; 2nd Editio.; Jones & Bartlett Publishers.: Sudbury, Massachusetts, 2010; ISBN 3. [Google Scholar]
- Perotto, A.O.; Delagi, E.F. Anatomical Guide for the Electromyographer: The Limbs and Trunk; 4 Ed.; Thomas Charles C Publisher: Illinois, USA, 2011. [Google Scholar]
- Vera-Garcia, F.J.; Moreside, J.M.; McGill, S.M. MVC techniques to normalize trunk muscle EMG in healthy women. J. Electromyogr. Kinesiol. 2010, 20, 10–16. [Google Scholar] [CrossRef]
- Antonaci, F.; Ghirmai, S.; Bono, G.; Nappi, G. Current methods for cervical spine movement evaluation: A review. Clin. Exp. Rheumatol. 2000, 18. [Google Scholar]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Van Der Helm, F.C.T.; Veeger, H.E.J.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion - Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Clark, N.C.; Abt, J.P.; Sell, T.C.; Heebner, N.R.; Smalley, B.W.; Wirt, M.D.; Lephart, S.M. The Effect of Target Position on the Accuracy of Cervical-Spine-Rotation Active Joint-Position Sense. J. Sport Rehabil. 2015, 25, 58–63. [Google Scholar] [CrossRef]
- Research, J.P.W.-T.J. of S.& C.; 2005, undefined Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. journals.lww.comJP WeirThe J. Strength Cond. Res. 2005•journals.lww.com 2005, 19, 231–240. [Google Scholar]
- Fleiss, J.L. The design and analysis of clinical experiments. New York: John Willey and Sons. Acta Physiol Scand.
- Durlak, J.A. How to Select, Calculate, and Interpret Effect Sizes. J. Pediatr. Psychol. 2009, 34, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, R.F.; Lewis, C.; Bell, D.; Bramblet, G.; Daffron, J.; Lambert, S.; Pecson, A.; Imamura, R.; Paulos, L.; Andrews, J.R. Core Muscle Activation During Swiss Ball and Traditional Abdominal Exercises. J. Orthop. Sport. Phys. Ther. 2010, 40, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Ekstrom, R.A.; Donatelli, R.A.; Carp, K.C. Electromyographic Analysis of Core Trunk, Hip, and Thigh Muscles During 9 Rehabilitation Exercises. J. Orthop. Sport. Phys. Ther. 2007, 37, 754–762. [Google Scholar] [CrossRef]
- Okubo, Y.; Kaneoka, K.; Imai, A.; Shiina, I.; Tatsumura, M.; Izumi, S.; Miyakawa, S. Electromyographic Analysis of Transversus Abdominis and Lumbar Multifidus Using Wire Electrodes During Lumbar Stabilization Exercises. J. Orthop. Sport. Phys. Ther. 2010, 40, 743–750. [Google Scholar] [CrossRef]
- Shirado, O.; Ito, T.; Kaneda, K.; Strax, T.E. Electromyographic analysis of four techniques for isometric trunk muscle exercises. Arch. Phys. Med. Rehabil. 1995, 76, 225–229. [Google Scholar] [CrossRef]
- Massó, N.; Rey, F.; Romero, D.; Gual, G.; Costa, L.; Germán, A. Aplicaciones de la electromiografía de superficie en el deporte. Apunts 2010, 45, 127–136. [Google Scholar]
- Caneiro, J.P.; O’Sullivan, P.; Burnett, A.; Barach, A.; O’Neil, D.; Tveit, O.; Olafsdottir, K. The influence of different sitting postures on head/neck posture and muscle activity. Man. Ther. 2010, 15, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl. Ergon. 2016, 53, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Wilke, J.; Krause, F.; Vogt, L.; Banzer, W. What Is Evidence-Based About Myofascial Chains: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Liebsch, C.; Wilke, H.-J. Chapter 3 - Basic Biomechanics of the Thoracic Spine and Rib Cage. In; Galbusera, F., Wilke, H.-J.B.T.-B. of the S., Eds.; Academic Press, 2018; pp. 35–50 ISBN 978-0-12-812851-0.
- Bogduk, N.; Mercer, S. Biomechanics of the cervical spine. I: Normal kinematics. Clin. Biomech. 2000, 15, 633–648. [Google Scholar] [CrossRef] [PubMed]
- Castanharo, R.; Duarte, M.; McGill, S. Corrective sitting strategies: An examination of muscle activity and spine loading. J. Electromyogr. Kinesiol. 2014, 24, 114–119. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine (Phila. Pa. 1976). 2006, 31, E707–12. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Bluemle, L.N.; Dolbeer, J.A.; Baker, S.E.; Molloy, J.M.; Whittaker, J.; Childs, J.D. Changes in Lateral Abdominal Muscle Thickness During the Abdominal Drawing-in Maneuver in Those With Lumbopelvic Pain. J. Orthop. Sport. Phys. Ther. 2009, 39, 791–798. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).