Submitted:
04 September 2023
Posted:
06 September 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Understanding Pharmacodynamic Biomarkers
Omics Technologies
Proteomics
| Technologies | |
|---|---|
| Technology | Application |
| Mass Spectrometry (MS) | Characterization and post-translational modification analysis[54]. |
| Surface Plasmon Resonance (SPR) | Protein interaction studies[55] |
| Capillary Electrophoresis (CE) | Biosimilar comparability studies.[56] |
| Two-Dimensional Gel Electrophoresis | Separation and identification of proteins [57] |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Specific protein quantification and immunogenicity studies.[58] |
| X-ray Crystallography and Nuclear Magnetic Resonance (NMR) Spectroscopy | Structural analysis and 3D modeling.[59] |
| Protein Microarrays | High-throughput analysis of protein functions and interactions.[60] |
| Circular Dichroism | In vivo and in vitro stability analysis -[61]. |
| Immunoassays | Pharmacokinetic and pharmacodynamic studies.[62] |
| Differential Scanning Calorimetry | Thermal stability analysis.[63] |
| Stable Isotope Labeling by Amino acids in Cell culture | Quantitative proteomics for expression analysis.[64] |
| Yeast Two-Hybrid System | Protein-protein interaction mapping.[65] |
| Liquid Chromatography-Mass Spectrometry | Comprehensive protein characterization [66] |
| Hydrogen-Deuterium Exchange Mass Spectrometry | Conformational dynamics and higher-order structure analysis.[67] |
| Multi-Angle Light Scattering (MALS) | Molar mass and size distribution.[68] |
| Size-Exclusion Chromatography | Protein aggregation and purity assessment.[69] |
| Matrix-Assisted Laser Desorption/Ionization Time-of-Flight MS | Rapid identification and characterization of proteins [70] |
| Isoelectric Focusing (IEF) | Protein separation based on isoelectric point -[71]. |
| Reversed-Phase High-Performance Liquid Chromatography | Analysis of Protein purity and heterogeneity [72] |
| Chemical Cross-Linking Coupled with MS | Studying spatial arrangement and interactions within protein complexes.[73] |
| Fourier Transform Infrared Spectroscopy (FTIR) | Secondary structure analysis and stability monitoring.[74] |
| Flow Cytometry | Cell line development and monitoring of protein expression.[75] |
| Biacore (SPR-based technology) | Label-free interaction analysis.[76] |
| Selected Reaction Monitoring MS | Targeted protein quantification in biosimilar development.[77] |
| Fluorescence Spectroscopy | Folding and conformational analysis.[78] |
| Hydrophobic Interaction Chromatography (HIC) | Analysis of hydrophobicity and aggregation.[79] |
| Ion Exchange Chromatography | Charge heterogeneity analysis.[80] |
| Native MS | Structural characterization and complex formation analysis.[81] |
| Affinity Chromatography | Purification and target binding analysis. |
| N-Terminal Sequencing | Analysis of protein sequence and modifications.[82] |
| Dynamic Light Scattering (DLS) | Size and stability analysis.[83] |
| Peptide Mapping and Fingerprinting | Identification and characterization of proteins.[84] |
| Immunoprecipitation and Pull-Down Assays | Protein interaction studies.[85] |
| Chromatography Coupled with Multi-Angle Light Scattering | Absolute molar mass, size, and conformation.[86] |
| NMR Spectroscopy in Conjunction with Hydrogen Exchange | Conformational dynamics and structural analysis.[87] |
| Examples of Use of Biomarkers | |
| Antibody Drug Conjugates (ADCs) | Brentuximab vedotin, an ADC used for Hodgkin's lymphoma and systemic anaplastic large cell lymphoma, delivers the cytotoxic drug monomethyl auristatin E (MMAE) to CD30-expressing cells, and the measurement of MMAE can serve as a marker of target engagement[88]. |
| Antigen-antibody complex | The formation of antigen-antibody complexes provides direct evidence of target engagement. For example, in the case of adalimumab, an anti-tumor necrosis factor (TNF)-α antibody, the serum levels of the adalimumab-TNFα complex can be measured as evidence of the drug binding to its target[89]. |
| Antigenic Modulation | This refers to the downregulation or loss of antigen expression on the cell surface in response to antibody binding and can be used as a marker of monoclonal antibody (mAb) engagement. Rituximab, a monoclonal antibody against the CD20 antigen on B cells, causes antigenic modulation, decreasing CD20 expression and indicating rituximab engagement[90]. |
| Binding of mAbs to Fc Receptors | The Fc region of mAbs can bind to Fc receptors on immune cells. This binding can modulate the activity of these cells, making Fc receptor occupancy a valuable PD marker. The occupancy of RIIIa on natural killer cells by rituximab can be used as a PD marker[91]. |
| Cell Proliferation Markers | mAbs may also be designed to inhibit cell proliferation. Here, decreased cell proliferation markers, such as Ki-67, can indicate successful target engagement[92]. |
| Circulating Tumor Antigen Levels | In cancer therapy, mAbs are often designed for binding to specific tumor antigens. Reduction in the levels of these circulating antigens following mAb therapy can serve as a marker of target engagement. For instance, CA-125 levels in patients with ovarian cancer have been treated with mAbs targeting the CA-125 antigen[93]. |
| Complement System Alterations | mAbs can modulate the complement system. Eculizumab, a mAb that inhibits complement component C5, reduces hemolytic activity and can be used as a PD marker[94]. |
| Cytokine Release Syndrome | mAbs, particularly those targeting immune cells, increase the release of specific cytokines. For instance, administration of the anti-CD28 mAb TGN1412 releases many cytokines, such as interleukin (IL)-2 and interferon (IFN)-γ, which could be monitored as PD markers[95]. Measuring cytokines, such as IL-2, IL-6, or TNF- α, can estimate target engagement. This is particularly relevant for immunomodulatory mAbs such as ipilimumab, which can increase circulating cytokine levels upon engagement with its target, cytotoxic T lymphocyte-associated (CTLA-4)[96]. |
| Fluorescent Tag | Flow cytometry can be a valuable tool for assessing target engagement when the target of a mAb is expressed on cell surfaces. Labeling the mAb with a fluorescent tag confirms its binding to the target cells in a sample. This has been utilized in therapies, such as those using rituximab, wherein binding to CD20+ B cells can be confirmed using flow cytometry[97]. |
| Gut Microbiota Alterations | Specific mAb therapies can alter gut microbiota, serving as functional response markers. Vedolizumab, a mAb against the α4β7 integrin used in treating inflammatory bowel disease, can restore gut microbial diversity, indicating a functional response to therapy[98]. |
| Immune Response Markers | Some mAbs stimulate immune responses against specific antigens. Hence, increased antibodies against the target antigen in the patient's serum can serve as a target engagement marker. For instance, palivizumab, a mAb that prevents respiratory syncytial virus (RSV) infection in high-risk infants, engages its target through anti-RSV antibodies in the patient's serum[99]. Immune response can be measured as a functional response marker. For instance, ipilimumab, a mAb that targets the immune checkpoint protein CTLA-4, is the most widely used mAb. |
Glycomics
Transcriptomics
Genomics
- Whole Genome Sequencing[155]
- RNA-Seq): Analyzing the quantity and sequences of RNA[156]
- Quantitative PCR: Quantitative measurement of specific DNA or RNA levels [157]
- Microarrays: High-throughput gene expression analysis [158]
- Comparative Genomic Hybridization: Detecting and mapping chromosomal imbalances[159]
Epigenomics
- DNA methylation: In mammals, DNA methylation typically occurs at cytosine residues in the cytosine-phosphate-guanine context and is an essential process for normal development. Changes in DNA methylation patterns are associated with several key processes, including carcinogenesis.
- Histone modification: Histone proteins can be modified post-translationally by methylation, acetylation, and ubiquitination. These modifications can alter the chromatin structure and affect gene expression.
- Studying the extent to which combinations of DNA-, RNA-, and PTM-level variations contribute to the complexity of the human proteome.
Metabolomics
FDA Omics Perspective
FDA Research
PCSK9 Inhibitor Markers.[199]
IL-5 Antagonists Biomarkers.[201]
IFNβ-1a Biomarkers.[203]
Model-based Testing Markers[204]
The Practicality of Omics Technologies
- Relevance to the mechanism of action
- Sensitive to differences between the proposed biosimilar and the reference product
- Analytical validity
- Time of onset correlated with dosing
- The dynamic range over exposure range
- Proteins located remain unidentified, and these may well be testing process dependent.
- Proteins may not be related to clinical efficacy and only represent a clinical pharmacological profile.
- The availability of technology for proteomic testing is limited, and its random use may be even more detrimental.
Biosimilars and Omics Technologies
| Omics Technology | Role | Rationale |
| Proteomics[205] | Determine the protein expression profile, post-translational modifications (like glycosylation), and protein-protein interactions of the biosimilar compared to the reference product. | Minor differences in protein structure or modifications can impact the efficacy. |
| Transcriptomics | Analyze the gene expression profile of cells producing the biosimilar, ensuring that the cellular machinery has the therapeutic protein in a manner consistent with the reference product. | Differences in gene expression may hint at differences in protein product production, folding, or modification. |
| Metabolomics[206] | Examine the metabolic profile of the biosimilar-producing cells. | The metabolic state of a cell can influence the final product's quality and consistency. For instance, changes in nutrient levels can influence glycosylation patterns of proteins. |
| Genomics | Ensures genetic stability of the cell line producing the biosimilar. | Over time, cell lines might undergo genetic drift, which can impact the product's quality, consistency, and efficacy. |
| Microbiomics | Understanding the microbiome can be essential if the biological product has a microbial origin (like some recombinant proteins produced in bacteria). | Microbial contaminants or shifts in the microbial population can influence the final product's quality and safety. |
| Phosphoproteomics | Analyze phosphorylation patterns on proteins, which can be critical for some biologics' function or stability. | Changes in phosphorylation can affect protein activity, stability, or interaction with other proteins. |
Omics Surrogates
Receptor Binding
| mAb (Brand) | Receptor |
| Abciximab (ReoPro)[210] | GPIIb/IIIa |
| Adalimumab (Humira)[211] | TNFα |
| Alemtuzumab (Lemtrada)[212] | CD52 |
| Atezolizumab (Tecentriq)[213] | PD-L1 |
| Basiliximab (Simulect)[214] | CD25 |
| Belimumab (Benlysta)[215] | BLyS |
| Bevacizumab (Avastin)[216] | VEGF |
| Cetuximab (Erbitux)[217] | EGFR |
| Daclizumab (Zinbryta)[218] | CD25 |
| Daratumumab (Darzalex)[219] | CD38 |
| Denosumab (Prolia)[220] | RANKL |
| Dupilumab (Dupixent)[221] | IL-4Rα |
| Eculizumab (Soliris)[222] | C5 |
| Infliximab (Remicade)[223] | TNFα |
| Ipilimumab (Yervoy)[224] | CTLA-4 |
| Nivolumab (Opdivo)[225] | PD-1 |
| Obinutuzumab (Gazyva)[226] | CD20 |
| Ofatumumab (Arzerra)[227] | CD20 |
| Omalizumab (Xolair)[228] | IgE |
| Palivizumab (Synagis)[229] | RSV F protein |
| Pembrolizumab (Keytruda)[230] | PD-1 |
| Rituximab (Rituxan)[231] | CD20 |
| Sarilumab (Kevzara)[232] | IL-6R |
| Secukinumab (Cosentyx)[233] | IL-17A |
| Tocilizumab (Actemra)[234] | IL-6R |
| Trastuzumab (Herceptin)[235] | HER2/neu |
| Vedolizumab (Entyvio)[236] | α4β7 integrin |
Pharmacokinetic Profiling
- Cancer Chemotherapy: Modeling Vd(t) can lead to better predictions of drug concentrations in tumor tissue versus surrounding tissues, potentially optimizing dosing schedules for maximum efficacy and minimal toxicity. [250]
- Infectious Diseases: Understanding Vd(t) can help design dosage regimens that ensure sufficient drug concentrations at the infection site while minimizing systemic exposure. [251]
- Autoimmune Diseases: For monoclonal antibodies used in conditions like rheumatoid arthritis, Vd can change over time due to factors like target-mediated drug disposition. Understanding Vd(t) can inform individualized dosing. [252]
- Geriatric Pharmacology: Age-related physiological changes can impact Vd, and considering Vd as a function of time provides insights into drug disposition in elderly patients. [253]
- Drug Development: During the pre-clinical phase, understanding Vd(t) can guide decisions about advancing a drug candidate to the next stage, potentially saving time and resources. [254]
Finding Biomarkers for Biosimilars
| Type | Count |
| Fab | 1 |
| Toxin | 1 |
| Carrier Protein | 1 |
| Single-Domain Antibody | 1 |
| Fusion Proteins | 1 |
| Bispecific Antibody | 3 |
| Coagulation Factor | 4 |
| Cytokine | 4 |
| Peptide | 4 |
| Growth Factor | 4 |
| Enzyme | 9 |
| Enzyme Inhibitor | 11 |
| Hormone | 11 |
| Monoclonal Antibody Conjugate | 13 |
| Monoclonal Antibody | 96 |
| Total | 164 |
| Mode of Action | Biomarker Potential |
| AMPK and mTORC1 Signaling | Monitoring these central energy sensors and regulators can be vital for drugs targeting cellular energy status or metabolic health.[257] |
| Angiogenesis Indicators | If a protein drug affects blood vessel formation, angiogenic factors like VEGF can be used as biomarkers.[258] |
| Apoptosis Markers | Evaluation of cell death can be instrumental for drugs designed to induce or inhibit apoptosis. Markers such as caspase activation or phosphatidylserine externalization can be employed.[259] |
| Autophagy Markers | LC3-II and p62/SQSTM1, for drugs modulating autophagic activity.[260] |
| Autophagy-lysosomal Pathway Markers | Monitoring markers like p62/SQSTM1 or LAMP1 can give insights into the autophagy-lysosomal activity upon drug treatment.[261] |
| Blood Coagulation Factors | For protein drugs affecting hemostasis, measurement of specific clotting factors or clotting times might be used.[262] |
| Bone Turnover Markers | For protein drugs acting on the skeletal system, bone resorption or formation markers can provide insight into their effect.[263] |
| Calcium Signaling | Monitoring intracellular calcium flux and associated proteins can be important for drugs that modulate calcium homeostasis or signaling pathways.[264] |
| Cell Cycle Regulators | Drugs aiming at modulating the cell cycle might alter levels or activities of cyclins, cyclin-dependent kinases, or associated inhibitors.[265] |
| Cell Metabolism | Assessing the metabolic profile of cells or tissues after drug treatment, for instance, glucose uptake, lactate production, or ATP levels.[266] |
| Cell Surface Markers | These markers can be evaluated for drugs targeting cell surface proteins or for those that induce phenotypic changes in cells.[267] |
| Cellular Apoptosis or Proliferation | Some protein drugs may induce or inhibit apoptosis or cell proliferation, which can be quantified.[268] |
| Cellular Signaling Pathways | Assessment of downstream or upstream signaling pathways that might be affected by the protein drug. MAPK, PI3K/AKT, or JAK/STAT pathways.[269] |
| Changes in specific cell populations | Especially in immunology, a protein drug can lead to the proliferation or reduction of specific cell populations.[270] |
| Circadian Rhythms | For protein drugs affecting cellular or physiological rhythms, markers related to circadian clock genes such as PER, CRY, or CLOCK might be relevant.[271] |
| Complement Activation | For specific therapeutic proteins, activation or inhibition of the complement system can serve as a pharmacodynamic readout.[272] |
| Cytokine Levels | Many protein drugs target specific cytokines or have effects on cytokine levels.[273] |
| DNA Damage and Repair Markers | γH2AX and other proteins associated with DNA damage response can be relevant for drugs targeting genomic stability.[274] |
| Drug Concentration | Although this is more of a pharmacokinetic parameter, the concentration of the drug in the bloodstream can sometimes serve as a surrogate for its pharmacodynamic effects, significantly when the concentration closely correlates with the drug's effect.[275] |
| Endocannabinoid System Markers | Components include CB1 and CB2 receptors or endocannabinoids (anandamide, 2-AG) for drugs affecting this system.[276] |
| Endocrine Biomarkers | For protein drugs affecting the endocrine system, hormones or hormone precursors might be potential pharmacodynamic indicators.[277] |
| Endocytosis and Exocytosis Metrics | Protein drugs targeting cell trafficking mechanisms might alter the rates of endocytosis or exocytosis, which can be tracked using various cellular assays.[278] |
| Endogenous Antioxidant Enzymes | Superoxide dismutase (SOD), catalase, and glutathione peroxidase levels can be tracked for oxidative stress modulation.[279] |
| Endoplasmic Reticulum (ER) Stress Markers | GRP78/BiP, CHOP, XBP1, ATF6 for drugs influencing ER homeostasis or targeting diseases related to protein misfolding.[280] |
| Endosome Trafficking | Protein drugs that interfere with endosomal pathways can be monitored for their effects using markers of early, late, and recycling endosomes.[281] |
| Endothelial Activation Markers | For drugs impacting vascular inflammation or barrier function, such as E-selectin, ICAM-1, and VCAM-1.[282] |
| Enzyme Activity | If the protein drug targets an enzyme, measuring the change in enzyme activity can be an effective biomarker.[283] |
| Epigenetic Markers | Changes in DNA methylation, histone modification, or other epigenetic markers might indicate a response to certain protein drugs.[284] |
| Exosome Release and Composition | Certain protein drugs can influence exosomes and their cargo (RNA, protein, lipids), especially those impacting intercellular communication.[285] |
| Extracellular Matrix (ECM) Components | Matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs) are relevant for tissue remodeling or cancer invasion.[286] |
| Fatty Acid Oxidation (FAO) Rates | Drugs targeting metabolic states might shift cells between carbohydrate and fatty acid metabolism.[287] |
| Flow Cytometry | This is particularly relevant for drugs that target cells of the immune system. Flow cytometry can provide insights into cell numbers, phenotypes, and functions.[288] |
| Functional Assays | Depending on the intended drug action, functional assays can be developed. For instance, if a protein drug aims to inhibit a specific cellular function, assays can be set up to measure that specific function.[289] |
| Gene Expression Profiles | Transcriptomics can reveal the downstream effects of a protein drug on cellular gene expression.[290] |
| Glycolytic versus Oxidative Metabolism | Assessing the switch between glycolytic and oxidative metabolism can be crucial for drugs targeting metabolic diseases or cancer.[291] |
| Glycosylation Patterns | Alterations in the glycosylation patterns of cells or proteins can directly or indirectly affect some protein drugs.[292] |
| Gut Microbiota Composition | Sequencing or metabolomic profiles of gut bacteria can be helpful for drugs impacting the gut environment.[293] |
| Heat Shock Proteins (HSPs) | As molecular chaperones, changes in HSP levels can indicate cellular stress responses or protein homeostasis disruptions.[294] |
| Heat Shock Proteins (HSPs) | These proteins respond to cellular stress and can be targets or indicators for several drugs, especially in protein misfolding diseases.[295] |
| Histone Modifications | Epigenetic changes, like histone acetylation or methylation, can be markers for drugs targeting chromatin remodeling or gene expression.[296] |
| Hormone Levels | Assessment of specific hormone levels, like insulin, glucagon, or thyroid hormones, can indicate drug impact on endocrine systems.[297] |
| Hypoxia Indicators | For protein drugs affecting cellular responses to oxygen deprivation, markers like HIF-1α can be interesting.[298] |
| Imaging Biomarkers | Techniques like MRI, PET, and CT can be used to measure the effects of protein drugs at the tissue or organ level.[299] |
| Immune Response Markers | The immune system might mount an antibody response for protein drugs, especially those foreign to the human body. Monitoring anti-drug antibodies (ADAs) can be a biomarker for potential immunogenicity issues.[300] |
| Inflammasome Activation | Monitoring inflammasome components can be helpful in drugs targeting inflammatory conditions or diseases like Alzheimer's.[301] |
| Ion Channel Activity | For protein drugs targeting ion channels, the measurement of ion flux or electrical properties of cells could directly indicate drug action.[302] |
| Iron Metabolism Markers | Ferritin, transferrin, and hepcidin for drugs modulating iron homeostasis.[303] |
| Levels of circulating drug target | If the target of the protein drug circulates in the bloodstream (like a soluble receptor or ligand), measuring its levels can serve as a biomarker.[304] |
| Ligand-Receptor Interactions | Investigating a protein drug's binding dynamics and affinity to its target receptor can provide insights into its effectiveness.[305] |
| Lipidomic Profile | Analyzing the cellular lipid composition can be informative, especially for drugs impacting lipid metabolism or signaling.[306] |
| Lipophagy Markers | Indicators of lipid droplet autophagy crucial for lipid metabolism-related conditions.[307] |
| Lysosomal Enzymes | The levels and activity of the specific lysosomal enzymes can be essential biomarkers for enzyme replacement therapies in lysosomal storage disorders.[308] |
| Markers of Fibrosis | In conditions like liver or lung fibrosis, protein drugs might target fibrogenesis, and thus, markers such as tissue collagen or specific matrix proteins can serve as indicators.[309] |
| Metabolic Enzymes | Monitoring the levels or activities of critical metabolic enzymes, such as those involved in glycolysis or the TCA cycle, can provide insights into the metabolic state of cells upon drug treatment.[310] |
| MicroRNAs (miRNAs) | Changes in the expression of specific miRNAs can serve as biomarkers since they play pivotal roles in gene regulation and might be influenced by protein drugs.[311] |
| Mitochondrial Dynamics | Assessing mitochondrial morphology and dynamics can indicate cellular health and metabolism, especially for drugs targeting these organelles.[312] |
| Mitophagy Indicators | Monitoring mitophagy, a process to degrade damaged mitochondria, can be helpful in drugs targeting cellular health.[313] |
| mRNA Splicing Markers | Such as components of the spliceosome for drugs modulating RNA splicing or targeting splicing-related diseases.[314] |
| mTOR Signaling | The mechanistic target of the rapamycin (mTOR) pathway, central to cell growth and metabolism, might be affected by certain protein drugs. Monitoring components like p70S6 kinase or 4E-BP1 can be informative.[315] |
| Myelination Markers | Proteins like MBP or PLP can be tracked for drugs targeting neurodegenerative diseases or demyelinating conditions.[316] |
| NAD+/NADH Ratio | A marker for cellular redox state and metabolism, especially relevant for aging |
| Neural Activity Markers | c-Fos, Arc, or immediate early genes can be indicators of neural activity and synaptic plasticity.[317] |
| Neurotransmitter Levels | If the drug has a neurological target, neurotransmitter levels in the central nervous system or peripheral tissues can be evaluated.[318] |
| Neurotrophic Factors | In neurodegenerative diseases, protein drugs might aim to modulate the levels of neurotrophic factors like BDNF, NGF, or GDNF.[319] |
| NO (Nitric Oxide) Production | Relevant for cardiovascular or immunomodulatory drugs, NO levels can indicate endothelial function and inflammatory states.[320] |
| Nrf2-Keap1 Pathway | Tracking the Nrf2-Keap1 pathway components can be vital for drugs that modulate oxidative stress.[321] |
| Nucleotide Metabolites | Monitoring the levels of specific nucleotide metabolites can indicate cellular activity or stress in response to certain protein drugs.[322] |
| Oxidative Phosphorylation (OXPHOS) Metrics | For protein drugs targeting mitochondrial function, OXPHOS or mitochondrial health markers can be relevant.[323] |
| Oxidative Stress Markers | Oxidative stress plays a role in numerous diseases, and markers like reactive oxygen species (ROS) or antioxidant levels can be used to assess drug effects.[324] |
| Oxysterols | Such as 24(S)-hydroxycholesterol 27-hydroxycholesterol for drugs targeting cholesterol metabolism or diseases like Niemann-Pick type C.[325] |
| Peroxisome Proliferators-Activated Receptors (PPARs) | As metabolic regulators, PPARs can be markers for drugs impacting lipid metabolism or inflammation.[326] |
| Pharmacogenomic Biomarkers | Some patients might respond differently to protein drugs based on genetic variations. Exploring these can provide insights into efficacy and safety.[327] |
| Phosphorylation status of proteins | The activation or deactivation of specific signaling pathways can be tracked by looking at the phosphorylation status of essential proteins.[328] |
| Proteasome Activity | Assessing proteasomal activity can be insightful for protein drugs that modulate protein degradation.[329] |
| Proteomic Analysis | To assess broader proteome for changes in protein levels or post-translational modifications upon drug treatment.[330] |
| Reactive Oxygen Species (ROS) Levels | As an indicator of oxidative stress, ROS can be monitored for drugs that either induce or counteract cellular stress.[331] |
| Receptor Occupancy | Measuring the degree to which a protein drug binds to its target receptor can be a direct biomarker of its activity.[332] |
| Senescence-associated Secretory Phenotype (SASP) Factors | Monitoring factors associated with cellular senescence might be relevant for drugs targeting aging or oncogenesis.[333] |
| Sirtuin Activity | Monitoring sirtuin proteins can be essential for drugs modulating cellular longevity or metabolic health.[334] |
| Telomerase Activity | Telomerase activity or telomere length might be relevant biomarkers for drugs targeting cancer or aging processes.[335] |
| Tight Junction Proteins | Markers like claudins, occludin, and ZO-1 are relevant for drugs targeting barrier integrity, such as in gut or blood-brain barrier conditions.[336] |
| Tissue Repair and Regeneration Markers | For protein drugs that facilitate tissue healing, markers of tissue repair or stem cell activation might be relevant.[337] |
| Tumor Microenvironment Components | Factors like TGF-beta, PD-L1, and various cytokines/chemokines for drugs targeting cancer immune evasion.[338] |
| Unfolded Protein Response (UPR) in the ER | For protein drugs that might induce ER stress, tracking components of the UPR can be informative.[339] |
| Wnt Signaling Pathway Components | Tracking this pathway can be crucial for drugs that modulate developmental processes, tissue regeneration, or certain cancers.[340] |
| No | Protein Drug | Pharmacodynamic Marker |
| 1. | Abatacept (Orencia) | T cell proliferation & co-stimulation[341] |
| 2. | Adalimumab (Humira) | TNF-alpha levels & inflammatory cytokine reduction[342] |
| 3. | Aducanumab (Aduhelm) | Beta-amyloid plaques in brain[343] |
| 4. | Aflibercept (Eylea) | VEGF levels, Central retinal thickness[344] |
| 5. | Agalsidase Alfa (Replagal) | Lyso-Gb3 levels, Kidney function[345] |
| 6. | Agalsidase Beta (Fabrazyme) | Lyso-Gb3 levels, Kidney function[346] |
| 7. | Albiglutide (Tanzeum) | Blood glucose & GLP-1 levels[347] |
| 8. | Albutrepenonacog Alfa (Idelvion) | Factor IX activity levels[348] |
| 9. | Aldesleukin (Proleukin) | T cell count, IL-2 levels[349] |
| 10. | Alefacept (Amevive) | CD4 and CD8 memory T-cell count[350] |
| 11. | Alemtuzumab (Lemtrada) | CD52-expressing cell count[351] |
| 12. | Alglucerase (Ceredase) | Gaucher cell count, Chitotriosidase levels [352] |
| 13. | Alirocumab (Praluent) | LDL cholesterol levels[353] |
| 14. | Alpha-1-proteinase inhibitor (Prolastin, etc.) | Alpha-1 antitrypsin levels, Neutrophil elastase activity[354] |
| 15. | Alteplase (Activase) | Fibrinolytic activity, clot dissolution[355] |
| 16. | Amivantamab (Rybrevant) | EGFR and MET signaling inhibition[356] |
| 17. | Anakinra (Kineret) | IL-1β levels[357] |
| 18. | Ancestim (Stemgen) | CD34+ cell count in peripheral blood[358] |
| 19. | Andexanet Alfa (Andexxa) | Reversal of factor Xa inhibitors[359] |
| 20. | Anifrolumab (Saphnelo) | Type I interferon gene signature[360] |
| 21. | Anistreplase (Eminase) | Fibrinolytic activity[361] |
| 22. | Ansuvimab (Ebanga) | Reduction in viral load of Ebola virus[362] |
| 23. | Atezolizumab (Tecentriq) | PD-L1 expression on tumor & immune cells [363] |
| 24. | Avelumab (Bavencio) | PD-L1 expression & T cell activation [364] |
| 25. | Benralizumab (Fasenra) | Reduction in eosinophil counts[365] |
| 26. | Bermekimab (Xilonix) | IL-1α levels[366] |
| 27. | Bevacizumab (Avastin) | VEGF level & microvessel density[367] |
| 28. | Bezlotoxumab (Zinplava) | Reduction in C. difficile infection recurrence[368] |
| 29. | Bimekizumab (Bimzelx) | IL-17A and IL-17F levels[369] |
| 30. | Bivalirudin (Angiomax) | Thrombin activity[370] |
| 31. | Blinatumomab (Blincyto) | CD19+ B cell count[371] |
| 32. | Bone Morphogenetic Proteins (BMPs) | Bone density or new bone formation[372] |
| 33. | Botulinum Toxin Type A (Botox) | Neuromuscular transmission inhibition[373] |
| 34. | Botulinum Toxin Type B (Myobloc) | Neuromuscular transmission inhibition[374] |
| 35. | Brodalumab (Siliq) | IL-17 receptor A occupancy [375] |
| 36. | Brolucizumab (Beovu) | VEGF levels, Central retinal thickness[376] |
| 37. | Burosumab (Crysvita) | Serum phosphorus levels[377] |
| 38. | Calaspargase pegol (Asparlas) | Asparagine levels[378] |
| 39. | Canakinumab (Ilaris) | IL-1β levels & CRP[379] |
| 40. | Cetuximab (Erbitux) | EGFR expression & phosphorylation[380] |
| 41. | Chymopapain (Chymodiactin) | Disc volume reduction[381] |
| 42. | Coagulation factor IX (BeneFIX) | Factor IX clotting activity[382] |
| 43. | Coagulation Factor VIIa (NovoSeven) | Clotting activity[383] |
| 44. | Collagenase (Santyl) | Degrades necrotic tissue[384] |
| 45. | Conestat alfa (Ruconest) | Bradykinin levels[385] |
| 46. | Corticotropin (Acthar) | Adrenal gland stimulation[386] |
| 47. | Cosyntropin-ACTH(1-24) (Cortrosyn) | Adrenal gland stimulation[387] |
| 48. | Crizanlizumab (Adakveo) | P-selectin inhibition[388] |
| 49. | Darbepoetin alfa (Aranesp) | Hemoglobin or hematocrit level[389] |
| 50. | Denosumab (Prolia, Xgeva) | RANKL inhibition & bone turnover markers [390] |
| 51. | Denosumab (Prolia) | Bone mineral density & serum C-telopeptide[391] |
| 52. | Dupilumab (Dupixent) | IL-4 and IL-13 signaling pathways [392] |
| 53. | Durvalumab (Imfinzi) | PD-L1 expression in tumor cells[393] |
| 54. | Eculizumab (Soliris) | Complement component C5 activity [394] |
| 55. | Edrecolomab (Panorex) | EpCAM expression[395] |
| 56. | Efalizumab (Raptiva) | CD11a expression[396] |
| 57. | Efgartigimod alfa | IgG reduction[397] |
| 58. | Elapegademase (Revcovi) | ADA enzyme activity[398] |
| 59. | Elosulfase Alfa (Vimizim) | GAG reduction[399] |
| 60. | Elotuzumab (Empliciti) | SLAMF7 expression in myeloma cells[400] |
| 61. | Emapalumab (Gamifant) | IFNγ levels[401] |
| 62. | Emicizumab (Hemlibra) | Factor IXa and factor X bridging[402] |
| 63. | Enfortumab vedotin (Padcev) | Nectin-4 expression[403] |
| 64. | Erenumab (Aimovig) | CGRP receptor binding and inhibition [404] |
| 65. | Erythropoietin (EPO) | Hemoglobin or hematocrit level[405] |
| 66. | Eteplirsen (Exondys 51) | Dystrophin production in muscle tissue[406] |
| 67. | Evolocumab (Repatha) | LDL cholesterol levels [407] |
| 68. | Fibrinolysin (Elase) | Fibrin degradation[408] |
| 69. | Filgrastim (Neupogen) | Neutrophil count[409] |
| 70. | Follitropin (Follistim, Gonal-f) | Follicular development, Estradiol levels[410] |
| 71. | Fremanezumab (Ajovy) | CGRP levels[411] |
| 72. | Galcanezumab (Emgality) | CGRP levels[412] |
| 73. | Galcanezumab (Emgality) | CGRP binding[413] |
| 74. | Galsulfase (Naglazyme) | Urinary glycosaminoglycan levels[414] |
| 75. | Gemtuzumab ozogamicin (Mylotarg) | CD33 antigen expression[415] |
| 76. | Girentuximab | CAIX expression[416] |
| 77. | Glatiramer acetate (Copaxone) | Immune modulation; T-cell response[417] |
| 78. | Glucagon recombinant (GlucaGen) | Blood glucose elevation[418] |
| 79. | Glucarpidase (Voraxaze) | Methotrexate levels reduction[419] |
| 80. | Golimumab (Simponi) | TNFα inhibition[420] |
| 81. | Growth Hormone | IGF-1 (Insulin-like Growth Factor 1) level[421] |
| 82. | Guselkumab (Tremfya) | IL-23 levels & PASI score [422] |
| 83. | Human C1-esterase inhibitor (Berinert, Cinryze) | C1-INH levels and activity[423] |
| 84. | Ibalizumab (Trogarzo) | HIV-1 viral load & CD4+ T-cell count [424] |
| 85. | Imiglucerase (Cerezyme) | Glucocerebroside levels, macrophage activity[425] |
| 86. | Inebilizumab (Uplizna) | B-cell depletion[426] |
| 87. | Infliximab (Remicade) | TNF-alpha levels & CRP[427] |
| 88. | Inotuzumab ozogamicin (Besponsa) | CD22 expression[428] |
| 89. | Insulin Regular (Humulin R, etc) | Glucose levels[429] |
| 90. | Interferons | Expression of interferon-responsive genes[430] |
| 91. | Ipilimumab (Yervoy) | T-cell activation[431] |
| 92. | Isatuximab (Sarclisa) | CD38 expression[432] |
| 93. | Itolizumab (Alzumab) | CD6 expression[433] |
| 94. | Ixekizumab (Taltz) | PASI score, serum IL-17A levels[434] |
| 95. | Lanadelumab (Takhzyro) | Plasma kallikrein activity[435] |
| 96. | Lanadelumab (Takhzyro) | Plasma kallikrein inhibition[436] |
| 97. | Laronidase (Aldurazyme) | Reduction of glycosaminoglycans[437] |
| 98. | Lepirudin (Refludan) | Inhibition of thrombin[438] |
| 99. | Leuprolide (Lupron) | Reduction in testosterone or estradiol[439] |
| 100. | Liraglutide (Victoza) | Blood glucose & GLP-1 levels[440] |
| 101. | Lixisenatide (Adlyxin) | GLP-1 receptor activation |
| 102. | Loncastuximab tesirine (Zynlonta) | CD19 expression[441] |
| 103. | Lucinactant (Surfaxin) | Improved lung compliance[442] |
| 104. | Luspatercept-aamt (Reblozyl) | Erythroid maturation[443] |
| 105. | Lutropin alfa (Luveris) | LH receptor activation[444] |
| 106. | Margetuximab (Margenza) | HER2 expression[445] |
| 107. | Mecasermin (Increlex) | IGF-1 receptor activation[446] |
| 108. | Menotropins (Menopur) | FSH and LH receptor activation[447] |
| 109. | Mepolizumab (Nucala) | IL-5 neutralization[448] |
| 110. | Metreleptin (Myalept) | Leptin receptor activation[449] |
| 111. | Mirvetuximab Soravtansine | Folate receptor alpha targeting[450] |
| 112. | Mogamulizumab (Poteligeo) | CCR4 targeting[451] |
| 113. | Moxetumomab pasudotox (Lumoxiti) | CD22 expression[452] |
| 114. | Muromonab (Orthoclone OKT3) | CD3 expression[453] |
| 115. | Natalizumab (Tysabri) | α4-integrin saturation[454] |
| 116. | Naxitamab (Danyelza) | GD2 expression[455] |
| 117. | Necitumumab (Portrazza) | EGFR targeting[456] |
| 118. | Nesiritide (Natrecor) | Natriuretic peptide receptor A activation[457] |
| 119. | Netakimab (Netakimab) | IL-17A inhibition[458] |
| 120. | Nimotuzumab (Theraloc, h-R3) | EGFR targeting[459] |
| 121. | Nivolumab (Opdivo) | PD-1 receptor occupancy & T cell function [460] |
| 122. | Nofetumomab merpentan (Verluma) | Carcinoembryonic antigen (CEA) targeting[461] |
| 123. | Obiltoxaximab (Anthim) | Protective antigen (PA) binding of Bacillus anthracis [462] |
| 124. | Obinutuzumab (Gazyva) | CD20 targeting[463] |
| 125. | Ocrelizumab (Ocrevus) | CD20 targeting[464] |
| 126. | Ocriplasmin (Jetrea) | Vitreomacular adhesion dissolution[465] |
| 127. | Ofatumumab (Arzerra) | CD20 targeting[466] |
| 128. | Olaratumab (Lartruvo) | PDGFRα phosphorylation levels[467] |
| 129. | Olipudase alfa (Xenpozyme) | Acid sphingomyelinase replacement[468] |
| 130. | Omalizumab (Xolair) | Free serum IgE levels & FcεRI expression on basophils [469] |
| 131. | Oportuzumab monatox (Vicineum) | N-acetylgalactosamine-4-sulfatase targeting[470] |
| 132. | Oprelvekin (Neumega) | Thrombopoietin receptor activation[471] |
| 133. | Oxytocin (Pitocin) | Oxytocin receptor activation[472] |
| 134. | Palifermin (Kepivance) | Keratinocyte growth factor receptor activation[473] |
| 135. | Palivizumab (Synagis) | RSV neutralization in serum[474] |
| 136. | Pancrelipase amylase (Creon) | Pancreatic enzyme replacement[475] |
| 137. | Panitumumab (Vectibix) | EGFR receptor occupancy & phosphorylation [476] |
| 138. | Parathyroid/Preotact (Preos) | Parathyroid hormone (PTH) receptor activation[477] |
| 139. | Pegademase bovine (Adagen) | ADA enzyme replacement[478] |
| 140. | Pegaspargase (Oncaspar) | Asparagine depletion[479] |
| 141. | Pegcetacoplan (Empaveli) | Complement C3 inhibition[480] |
| 142. | Peginterferon alfa-2a (Pegasys) | Interferon alpha receptor activation[481] |
| 143. | Peginterferon alfa-2b (PegIntron) | Interferon alpha receptor activation[482] |
| 144. | Pegloticase (Krystexxa) | Uric acid metabolism[483] |
| 145. | Pegvisomant (Somavert) | Growth hormone receptor antagonist[484] |
| 146. | Pembrolizumab (Keytruda) | PD-1 receptor occupancy & PD-L1 expression[485] |
| 147. | Pertuzumab (Perjeta) | HER2 receptor dimerization inhibition [486] |
| 148. | Pertuzumab (Perjeta) | HER2/neu targeting[487] |
| 149. | Pramlintide (Symlin) | Amylin analogue[488] |
| 150. | Protein S human (PROS) | Protein S supplementation[489] |
| 151. | Ramucirumab (Cyramza) | VEGFR2 targeting[490] |
| 152. | Ranibizumab (Lucentis) | VEGF level & macular thickness[491] |
| 153. | Rasburicase (Elitek) | Uric acid conversion to allantoin[492] |
| 154. | Reteplase (Retavase) | Plasminogen activation[493] |
| 155. | Rilonacept (Arcalyst) | Interleukin-1 blockade[494] |
| 156. | Rituximab (Rituxan) | CD20+ B cell depletion [495] |
| 157. | Romiplostim (Nplate) | Thrombopoietin receptor stimulation[496] |
| 158. | Romosozumab (Evenity) | Sclerostin levels & bone mineral density[497] |
| 159. | Sacrosidase (Sucraid) | Sucrase replacement for sucrose digestion[498] |
| 160. | Sargramostim (Leukine) | GM-CSF receptor activation[499] |
| 161. | Sarilumab (Kevzara) | IL-6 receptor blockade & CRP[500] |
| 162. | Sebelipase alfa (Kanuma) | Lysosomal acid lipase replacement[501] |
| 163. | Secretin (SecreFlo) | Secretin receptor activation[502] |
| 164. | Secukinumab (Cosentyx) | PASI score, serum IL-17A levels[503] |
| 165. | Sermorelin (Geref) | GHRH receptor activation[504] |
| 166. | Siltuximab (Sylvant) | IL-6 targeting[505] |
| 167. | Somatotropin (Genotropin) | GH receptor activation[506] |
| 168. | Streptokinase (Streptase) | Plasminogen activation[507] |
| 169. | Tagraxofusp (Elzonris) | CD123-directed cytotoxin[508] |
| 170. | Taliglucerase alfa (Elelyso) | Glucocerebrosidase enzyme replacement[509] |
| 171. | Teduglutide (Gattex) | GLP-2 receptor activation[510] |
| 172. | Tenecteplase (TNKase) | Plasminogen activation[511] |
| 173. | Teriparatide (Forteo) | Bone formation stimulation[512] |
| 174. | Terlipressin (Varpress) | Vasoconstriction through V1 receptor activation[513] |
| 175. | Tesamorelin (Egrifta) | GH-releasing hormone receptor activation[514] |
| 176. | Thymalfasin (Zadaxin) | Immunomodulation, T-cell stimulation[515] |
| 177. | Thyrotropin Alfa (Thyrogen) | Thyroid-stimulating hormone receptor activation[516] |
| 178. | Tirzepatide (Mounjaro) | Dual GLP-1 and GIP receptor agonism[517] |
| 179. | Tisotumab vedotin (Tivdak) | ADC targeting tissue factor[518] |
| 180. | Tocilizumab (Actemra) | IL-6 receptor blockade[519] |
| 181. | Tositumomab (Bexxar) | CD20 targeting[520] |
| 182. | Trastuzumab (Herceptin) | HER2/neu receptor expression [521] |
| 183. | Urofollitropin (Bravelle) | Follicle-stimulating hormone stimulation[522] |
| 184. | Urokinase (Abbokinase) | Plasminogen activation[523] |
| 185. | Ustekinumab (Stelara) | Inhibition of the p40 subunit of interleukin-12 (IL-12) and interleukin-23 (IL-23).[524] |
| 186. | Vasopressin (Vasostrict) | V1 and V2 receptor activation[525] |
| 187. | Vedolizumab (Entyvio) | α4β7 integrin receptor occupancy[526] |
| 188. | Velaglucerase alfa (Vpriv) | Glucocerebrosidase enzyme replacement[527] |
Conclusions
References
- https://tinyurl.com/niazi11.
- https://www.iqvia.com/insights/the-iqvia-institute/reports/biosimilars-in-the-united-states-2023-2027.
- https://www.mckinsey.com/industries/life-sciences/our-insights/three-imperatives-for-r-and-d-in-biosimilars.
- https://www.fda.gov/media/114574/download.
- https://www.fda.gov/drugs/drug-safety-and-availability/fda-withdraws-draft-guidance-industry-statistical-approaches-evaluate-analytical-similarity.
- https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analytical-assessment-and-other-quality.
- https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-immunogenicity-considerations-biosimilar-and-interchangeable-insulin-products.
- https://www.fda.gov/drugs/biosimilars/biosimilars-science-and-research.
- https://www.congress.gov/bill/117th-congress/senate-bill/5002.
- Niazi SK. End animal testing for biosimilar approval. Science. 2022 Jul 8;377(6602):162-163. Epub 2022 Jul 7. [CrossRef] [PubMed]
- https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/fda-policy-protection-human-subjects.
- https://www.congress.gov/bill/110th-congress/senate-bill/1695/text.
- Niazi S. Scientific Rationale for Waiving Clinical Efficacy Testing of Biosimilars. Drug Des Devel Ther. 2022 Aug 24;16:2803-2815. [CrossRef] [PubMed] [PubMed Central]
- Moore TJ, Mouslim MC, Blunt JL, Alexander GC, Shermock KM. Assessment of Availability, Clinical Testing, and US Food and Drug Administration Review of Biosimilar Biologic Products. JAMA Intern Med. 2021;181(1):52–60. [CrossRef]
- Clinical Trials Database. https://clinicaltrials.gov/ct2/results?cond=&term=biosimilar&cntry=&state=&city=&dist=&recrs=e (accessed on 25 April 2023).
- FDA. Clinical Pharmacology Data to Support a Demonstration of Biosimilarity to a Reference Product.Guidance for Industry. Published December 2016.
- https://www.fda.gov/media/114574/download?attachment.
- https://www.fda.gov/media/152279/download?attachment.
- https://www.fda.gov/drugs/news-events-human-drugs/fda-workshop-increasing-efficiency-biosimilar-development-programs-09192022.
- https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/division-applied-regulatory-science.
- Chiu, K., et al., (2023). New science, drug regulation, and emergent public health issues: The work of FDA’s division of applied regulatory science. Frontiers in Medicine, 9. [CrossRef]
- US Food and Drug Administration. FDA Guidance: Clinical Pharmacology Data to Support a Demonstration of Biosimilarity to a Reference Product <https://www.fda.gov/media/88622/ download> (2016).
- Chiu K, et al., New science, drug regulation, and emergent public health issues: The work of FDA's division of applied regulatory science. Front Med (Lausanne). 2023 Jan 19;9:1109541. [CrossRef] [PubMed] [PubMed Central]
- Li, L. et al. Quantitative relationship between AUEC of absolute neutrophil count and duration of severe neutropenia for GCSF in breast cancer patients. Clin Pharmacol Ther 104, 742–748 (2018). [CrossRef]
- Li J, Florian J, Campbell E, Schrieber S, Bai J, Weaver J, et al. Advancing biosimilar development using pharmacodynamic biomarkers in clinical pharmacology studies. Clin Pharmacol Ther. (2020) 107:40–2. [CrossRef]
- Sheikhy M, Schrieber S, Sun Q, Gershuny V, Matta M, Bai J, et al. Considerations for use of pharmacodynamic biomarkers to support biosimilar development.(I) a randomized trial with PCSK9 inhibitors. Clin Pharmacol Ther. (2022). [CrossRef]
- Gershuny V, Sun Q, Schrieber S, Matta M, Weaver J, Ji P, et al. Considerations for use of pharmacodynamic biomarkers to support biosimilar development.(II) a randomized trial with IL-5 antagonists. Clin Pharmacol Ther. (2022). [CrossRef]
- Florian JG, Sun Q, Schrieber S, Matta M, Hazel A, Sheikhy M, et al. Considerations for use of pharmacodynamic biomarkers to support biosimilar development – (III) a randomized trial with interferon beta-1a products. Clin Pharmacol Ther. (2022). [CrossRef]
- Hyland P, Chekka L, Samarth D, Rosenzweig B, Decker E, Mohamed E, et al. Evaluating the utility of proteomics for the identification of circulating pharmacodynamic biomarkers of IFNbeta-1a biologics. Clin Pharmacol Ther. (2022). [CrossRef]
- Wang YM, Strauss DG. Advancing Innovations in Biosimilars. Clin Pharmacol Ther. 2023 Jan;113(1):11-15. [CrossRef] [PubMed]
- US Food and Drug Administration. FDA Guidance: Scientific Considerations in Demonstrating Biosimilarity to a Reference Product <https://www.fda.gov/media/82647/download> (2015). (accessed on 25 April 2023).
- US Food and Drug Administration. FDA Guidance: Clinical Pharmacology Data to Support a Demonstration of Biosimilarity to a Reference Product <https://www.fda.gov/media/88622/download> (2016). (accessed on 25 April 2023).
- https://www.fda.gov/drugs/news-events-human-drugs/increasing-efficiency-biosimilar-development-programs-reevaluating-need-comparative-clinical.
- Hughes, T., & Branford, S. (2006). Molecular monitoring of BCR-ABL as a guide to clinical management in chronic myeloid leukaemia. Blood Reviews, 20(1), 29-41. [CrossRef]
- Stone, N. J., et al. (2014). 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology, 63(25_PA), 2889-2934. [CrossRef]
- Slamon, D. J., et al. (2001). Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. New England Journal of Medicine, 344(11), 783-792. [CrossRef]
- Shafer, R. W., Schapiro, J. M. (2008). HIV-1 drug resistance mutations: an updated framework for the second decade of HAART. Antiviral Therapy, 13(2), 145-176.
- Blennow, K., Zetterberg, H., & Fagan, A. M. (2012). Fluid biomarkers in Alzheimer disease. Cold Spring Harbor Perspectives in Medicine, 2(9), a006221.
- Brinkmann, V. (2009). FTY720 (fingolimod) in Multiple Sclerosis: therapeutic effects in the immune and the central nervous system. British Journal of Pharmacology, 158(5), 1173-1182. [CrossRef]
- Paul, C., et al. (2005). Risk of hepatotoxicity from tumor necrosis factor antagonists. Drug Safety, 28(3), 181-197.
- Ansell, J., et al. (2008). Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest, 133(6_suppl), 160S-198S. [CrossRef]
- Vasikaran, S., et al. (2011). Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporosis International, 22(2), 391-420. [CrossRef]
- Tumeh, P. C., et al. (2014). PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature, 515(7528), 568-571. [CrossRef]
- Wallis, R. S., et al. (2013). Biomarkers for tuberculosis disease activity, cure, and relapse. The Lancet Infectious Diseases, 10(2), 68-69. [CrossRef]
- Jenkins, R. G., et al. (2012). Longitudinal change in collagen degradation biomarkers in idiopathic pulmonary fibrosis: an analysis from the prospective, multicentre PROFILE study. The Lancet Respiratory Medicine, 2(6), 434-440. [CrossRef]
- Blennow, K., & Zetterberg, H. (2018). Biomarkers for Alzheimer's disease: current status and prospects for the future. Journal of Internal Medicine, 284(6), 643-663.
- Jones, A. G., & Hattersley, A. T. (2013). The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabetic Medicine, 30(7), 803-817. [CrossRef]
- Baker, D. J., et al. (2016). Naturally occurring p16^Ink4a-positive cells shorten healthy lifespan. Nature, 530(7589), 184-189. [CrossRef]
- Baylin, S. B., & Jones, P. A. (2011). A decade of exploring the cancer epigenome - biological and translational implications. Nature Reviews Cancer, 11(10), 726-734. [CrossRef]
- Mizushima, N., & Komatsu, M. (2011). Autophagy: renovation of cells and tissues. Cell, 147(4), 728-741. [CrossRef]
- Gandara, D. R., et al. (2018). Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nature Medicine, 24(9), 1441-1448. [CrossRef]
- Aebersold, R., & Mann, M. (2003). Mass spectrometry-based proteomics. Nature, 422(6928), 198–207. [CrossRef]
- Cox, J., & Mann, M. (2011). Quantitative, high-resolution proteomics for data-driven systems biology. Annual Review of Biochemistry, 80, 273–299. [CrossRef]
- Zhang, Y., et al. (2013). Chemical Reviews, 113(4), 2343-2394.
- Lofblom, J., et al. (2010). Trends in Biotechnology, 28(6), 298-306.
- Beck, A., et al. (2013). TrAC Trends in Analytical Chemistry, 48, 81-95.
- Gorg, A., et al. (2004). Electrophoresis, 25(9), 1451-1466.
- Crowther, J. R. (2009). The ELISA Guidebook. Methods in Molecular Biology, vol 516.
- Wüthrich, K. (2003). Journal of Biomolecular NMR, 27(1), 13-39.
- Zhu, H., et al. (2001). Science, 293(5537), 2101-2105.
- Kelly, S. M., & Price, N. C. (2000). Current Protein & Peptide Science, 1(4), 349-384.
- Xu, K., et al. (2013). AAPS Journal, 15(4), 897-909.
- Freire, E., et al. (1990). Analytical Biochemistry, 191(2), 31-37.
- Ong, S. E., et al. (2002). Molecular & Cellular Proteomics, 1(5), 376-386.
- Fields, S., & Song, O. (1989). Nature, 340(6230), 245-246.
- Doneanu, C. E., et al. (2012). mAbs, 4(1), 24-44.
- Engen, J. R. (2009). Analytical Chemistry, 81(19), 7870-7875.
- Wyatt, P. J. (1993). Particle Size Analysis, 48-68.
- Philo, J. S. (2009). Journal of Chromatography A, 1216(41), 6923-6930.
- Hillenkamp, F., et al. (1991). Analytical Chemistry, 63(24), 1193A-1203A.
- Righetti, P. G., et al. (1983). Journal of Chromatography A, 266, 471-509.
- Cserháti, T., & Forgács, E. (2004). Journal of Chromatography B, 804(1), 35-52.
- Leitner, A., et al. (2012). Journal of Mass Spectrometry, 47(6), 735-742.
- Barth, A. (2007). Biochimica et Biophysica Acta (BBA).Biomembranes, 1767(9), 1073-1101.
- Gossett, D. R., et al. (2012). Analytical and Bioanalytical Chemistry, 397(8), 3249-3261.
- Karlsson, R., et al. (2006). Analytical Biochemistry, 349(1), 136-147.
- Lange, V., et al. (2008). Molecular & Cellular Proteomics, 7(10), 1885-1897.
- Eftink, M. R. (1991). Methods in Enzymology, 205, 353-388.
- Yigzaw, Y., et al. (2005). Journal of Chromatography A, 1089(1-2), 83-92.
- Jungbauer, A., & Hahn, R. (2004). Journal of Chromatography B, 807(1), 3-22.
- Heck, A. J. R. (2008). Nature Methods, 5(11), 927-933.
- Harris, R. J. (1995). Current Opinion in Biotechnology, 6(4), 377-384.
- Berne, B. J., & Pecora, R. (2000). Dynamic Light Scattering.
- Suckau, D., et al. (1992). Methods in Enzymology, 218, 474-521.
- Dieriks, B., et al. (2009). Journal of Proteome Research, 8(10), 4863-4872.
- Wyatt, P. J. (1993). Particle Size Analysis, 48-68.
- Bai, Y., et al. (1993). Science, 262(5136), 998-1001.
- Francisco, J. A., et al. (2003). cAC10-vcMMAE, an anti-CD30-monomethyl auristatin E conjugate with potent and selective antitumor activity. Blood, 102(4), 1458-1465.
- Bendtzen, K., et al. (2003). Individualized monitoring of drug bioavailability and immunogenicity in rheumatoid arthritis patients treated with the tumor necrosis factor alpha inhibitor infliximab. Arthritis & Rheumatism, 48(12), 3782-3789. [CrossRef]
- Beum, P.V., et al. (2006). Loss of CD20 and bound CD20 antibody from opsonized B cells occurs more rapidly because of trogocytosis mediated by Fc receptor-expressing effector cells than direct internalization by the B cells. J Immunol, 177(11), 8071-8079. [CrossRef]
- Cartron, G., et al. (2002). Therapeutic activity of humanized anti-CD20 monoclonal antibody and polymorphism in IgG Fc receptor FcgammaRIIIa gene. Blood, 99(3), 754-758.
- Gerdes, J., et al. (1984). Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. Journal of Immunology, 133(4), 1710-1715. [CrossRef]
- Bast, R. C., et al. (1983). A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. New England Journal of Medicine, 309(15), 883-887. [CrossRef]
- Hillmen, P., et al. (2004). Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria. New England Journal of Medicine, 350(6), 552-559. [CrossRef]
- Suntharalingam, G., et al. (2006). Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. New England Journal of Medicine, 355(10), 1018-1028. [CrossRef]
- Wolchok, J.D., et al. (2010). Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res, 16(24), 7412-7420.
- Beers, S.A., et al. (2010). Antigenic modulation limits the efficacy of anti-CD20 antibodies: implications for antibody selection. Blood, 115(25), 5191-5201. [CrossRef]
- Ananthakrishnan, A.N., et al. (2017). Gut microbiome function predicts response to anti-integrin biologic therapy in inflammatory bowel diseases. Cell Host & Microbe, 21(5), 603-610. [CrossRef]
- Johnson, S., et al. (1997). Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus. Journal of Infectious Diseases, 176(5), 1215-1224. [CrossRef]
- Varki, A. (2017). Biological roles of glycans. Glycobiology, 27(1), 3-49. [CrossRef]
- Moremen, K. W., Tiemeyer, M., & Nairn, A. V. (2012). Vertebrate protein glycosylation: diversity, synthesis and function. Nature Reviews Molecular Cell Biology, 13(7), 448–462. [CrossRef]
- Varki, A., et al. (2009). Essentials of Glycobiology (2nd edition).
- Lauber, M. A., et al. (2015). Anal Chem, 87(1), 652-659.
- Mechref, Y., et al. (2009). Electrophoresis, 30(24), 4046-4060.
- Yamaguchi, Y., et al. (2008). Glycobiology, 18(6), 464-477.
- Harvey, D. J. (1999). Mass Spectrom Rev, 18(6), 349-450.
- Cummings, R. D., & Pierce, J. M. (2014). Chem Biol, 21(1), 1-15.
- Yamashita, K., et al. (1987). Anal Biochem, 164(2), 374-381.
- Kailemia, M. J., et al. (2017). Anal Chem, 89(2), 952-959.
- Tate, E. W., et al. (2006). Org Biomol Chem, 4(10), 1953-1961.
- Royle, L., et al. (2008). Nat Protoc, 3(8), 1299-1310.
- Zhou, S., et al. (2014). J Proteome Res, 13(12), 6078-6088.
- Mrksich, M. (2002). Chem Biol, 9(4), 443-454.
- Ciucanu, I., & Kerek, F. (1984). Carbohydrate Research, 131(2), 209-217.
- Domon, B., & Costello, C. E. (1988). Glycoconjugate Journal, 5(4), 397-409.
- Royle, L., et al. (2008). Methods Mol Biol, 484, 159-173.
- Anumula, K. R., & Taylor, P. B. (1992). Anal Biochem, 203(1), 101-108.
- Zeng, Y., et al. (2006). Analytical Chemistry, 78(19), 6832-6838.
- Wyatt, P. J. (1993). Analytica Chimica Acta, 272(1), 1-40.
- Spicer, S. S., et al. (1983). Histochemistry, 77(4), 471-490.
- Apweiler, R., et al. (1999). Biochim Biophys Acta, 1473(1), 4-8.
- Washburn, N., et al. (2013). J Chromatogr A, 1313, 212-219.
- Apweiler, R., et al. (1999). Trends Biotechnol, 17(9), 375-378.
- Laine, R. A. (1994). Glycobiology, 4(5), 759-767.
- Rich, R. L., & Myszka, D. G. (2011). J Mol Recognit, 24(6), 892-914.
- Lütteke, T., & von der Lieth, C. W. (2004). Curr Opin Struct Biol, 14(5), 583-589.
- Provencher, S. W. (1982). Comput Phys Commun, 27(3), 229-242.
- Morelle, W., & Michalski, J. C. (2007). Nature Protocols, 2(7), 1585-1602.
- Fazel R, et al., Structural and In Vitro Functional Comparability Analysis of Altebrel™, a Proposed Etanercept Biosimilar: Focus on Primary Sequence and Glycosylation. Pharmaceuticals (Basel). 2019 Jan 17;12(1):14. [CrossRef]
- Di Marco F, Blümel G, Blöchl C, Wuhrer M, Huber CG. A semi-automated hybrid HPLC-MS approach for in-depth characterization of intact non-covalent heterodimer glycoforms of gonadotropin biopharmaceuticals. Anal Chim Acta. 2023 Sep 15;1274:341574. [CrossRef]
- Čaval T, et al., Discrepancies between High-Resolution Native and Glycopeptide-Centric Mass Spectrometric Approaches: A Case Study into the Glycosylation of Erythropoietin Variants. J Am Soc Mass Spectrom. 2021 Aug 4;32(8):2099-2104.
- Hahm YH, Lee JY, Ahn YH. Investigation of Site-Specific Differences in Glycan Microheterogeneity by N-Glycopeptide Mapping of VEGFR-IgG Fusion Protein. Molecules. 2019 Oct 30;24(21):3924.
- Di Marco F, et al.,. Glycoproteomics of a single protein: revealing tens of thousands of Myozyme® glycoforms by hybrid HPLC-MS approaches. Mol Cell Proteomics. 2023 Jul 19:100622. [CrossRef]
- Moises JE, Regl C, Hinterholzer A, Huber CG, Schubert M. Unambiguous Identification of Glucose-Induced Glycation in mAbs and other Proteins by NMR Spectroscopy. Pharm Res. 2023 Jun;40(6):1341-1353. [CrossRef]
- Pegg CL, Zacchi LF, Recinos DR, Howard CB, Schulz BL. Identification of novel glycosylation events on human serum-derived factor IX. Glycoconj J. 2020 Aug;37(4):471-483. [CrossRef]
- Zaia J. Mass spectrometry and glycomics. OMICS. 2010 Aug;14(4):401-18. [CrossRef]
- Sanchez-De Melo I, et al., N-glycosylation profile analysis of Trastuzumab biosimilar candidates by Normal Phase Liquid Chromatography and MALDI-TOF MS approaches. J Proteomics. 2015 Sep 8;127(Pt B):225-33.
- Rosati S, et al., In-depth qualitative and quantitative analysis of composite glycosylation profiles and other micro-heterogeneity on intact monoclonal antibodies by high-resolution native mass spectrometry using a modified Orbitrap. MAbs. 2013 Nov-Dec;5(6):917-24. [CrossRef]
- Srikanth J, et al.,. Targeted, Site-specific quantitation of N-and O-glycopeptides using 18-O-labeling and product ion based mass spectrometry. Glycoconj J. 2017 Feb;34(1):95-105. [CrossRef]
- Yang Y, Liu F, Franc V, Halim LA, Schellekens H, Heck AJ. Hybrid mass spectrometry approaches in glycoprotein analysis and their usage in scoring biosimilarity. Nat Commun. 2016 Nov 8;7:13397. [CrossRef]
- Wang, Z., Gerstein, M., & Snyder, M. (2009). RNA-Seq: a revolutionary tool for transcriptomics. Nature Reviews Genetics, 10(1), 57–63. [CrossRef]
- Conesa, A., Madrigal, P., Tarazona, S., Gomez-Cabrero, D., Cervera, A., McPherson, A., Szcześniak, M. W., Gaffney, D. J., Elo, L. L., Zhang, X., & Mortazavi, A. (2016). A survey of best practices for RNA-seq data analysis. Genome Biology, 17, 13. [CrossRef]
- Vilaca, P., et al. (2014). Enhanced biosynthesis of lipidated proteins in Escherichia coli by selective introduction of lipids into proteins. ACS Synthetic Biology, 3(10), 761-770.
- Rosano, G. L., & Ceccarelli, E. A. (2014). Recombinant protein expression in Escherichia coli: Advances and challenges. Frontiers in Microbiology, 5, 172. [CrossRef]
- Krogan, N. J., et al. (2006). Global landscape of protein complexes in the yeast Saccharomyces cerevisiae. Nature, 440(7084), 637-643. [CrossRef]
- Gao, X., et al. (2018). Recombinant Protein Quality Evaluation: Proposal for a Minimal Information Standard. Scientific Reports, 8, 15737.
- de Marco, A. (2009). Strategies for successful recombinant expression of disulfide bond-dependent proteins in Escherichia coli. Microbial Cell Factories, 8, 26.
- Li, H., et al. (2016). Design and application of a mevalonate-responsive regulatory protein. Angewandte Chemie International Edition, 55(8), 2824-2828.
- Castrillo, J. I., et al. (2007). Growth control of the eukaryote cell: a systems biology study in yeast. Journal of Biology, 6(2), 4. [CrossRef]
- Geiger, T., et al. (2012). Initial Quantitative Proteomic Map of 28 Mouse Tissues Using the SILAC Mouse. Molecular & Cellular Proteomics, 11(5), M111.014050. [CrossRef]
- Hasin, Y., Seldin, M., & Lusis, A. (2017). Multi-omics approaches to disease. Genome Biology, 18(1), 83. [CrossRef]
- Green, E. D., Watson, J. D., & Collins, F. S. (2015). Human Genome Project: Twenty-five years of big biology. Nature, 526(7571), 29–31. [CrossRef]
- Goodwin, S., McPherson, J. D., & McCombie, W. R. (2016). Coming of age: ten years of next-generation sequencing technologies. Nature Reviews Genetics, 17(6), 333–351. [CrossRef]
- Yang, J.-H., Petty, C.A., Dixon-Mcdougall, T., Lopez, M.V., Tyshkovskiy, A., Maybury-Lewis, S., Tian, X., Ibrahim, N., Chen, Z., Griffin, P.T., Arnold, M., Li, J., Martinez, O.A., Behn, A., Rogers-Hammond, R., Angeli, S., Gladyshev, V.N., Sinclair, D.A., 2023. Chemically induced reprogramming to reverse cellular aging. Aging 15, 5966–5989. [CrossRef]
- Complete sequencing of an organism's DNA Lander, E. S., et al. (2001). Nature, 409(6822), 860-921.
- Wang, Z., et al. (2009). Nature Reviews Genetics, 10(1), 57-63.
- Bustin, S. A., et al. (2009). Clinical Chemistry, 55(4), 611-622.
- Schena, M., et al. (1995). Science, 270(5235), 467-470.
- Kallioniemi, A., et al. (1992). Science, 258(5083), 818-821.
- Amanda M. Lewis, Nicholas R. Abu-Absi, Michael C. Borys, Zheng Jian Li. The use of ‘Omics technology to rationally improve industrial mammalian cell line performance. (2015). Biotechnol Bioeng.. 2016 Jan;113(1):26-38. [CrossRef]
- Gustafsson, C., Govindarajan, S., & Minshull, J. (2004). Codon bias and heterologous protein expression. Trends in Biotechnology, 22(7), 346-353. [CrossRef]
- Edwards, A. M. et al. (2011). Too many roads not taken. Nature, 470(7333), 163-165. [CrossRef]
- Goldenzweig, A., et al. (2016). Automated Structure- and Sequence-Based Design of Proteins for High Bacterial Expression and Stability. Molecular Cell, 63(2), 337-346. [CrossRef]
- Hamburg, M. A., & Collins, F. S. (2010). The path to personalized medicine. New England Journal of Medicine, 363(4), 301-304. [CrossRef]
- Keasling, J. D. (2010). Manufacturing molecules through metabolic engineering. Science, 330(6009), 1355-1358. [CrossRef]
- Hood, L., & Friend, S. H. (2011). Predictive, personalized, preventive, participatory (P4) cancer medicine. Nature Reviews Clinical Oncology, 8(3), 184-187. [CrossRef]
- Gabaldón, T., & Huynen, M. A. (2004). Shaping the mitochondrial proteome. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, 1659(2-3), 212-220.
- Hartl, F. U., Bracher, A., & Hayer-Hartl, M. (2011). Molecular chaperones in protein folding and proteostasis. Nature, 475(7356), 324-332. [CrossRef]
- Hopkins, A. L., & Groom, C. R. (2002). The druggable genome. Nature Reviews Drug Discovery, 1(9), 727-730.
- Lewis AM, Abu-Absi NR, Borys MC, Li ZJ. The use of 'Omics technology to rationally improve industrial mammalian cell line performance. Biotechnol Bioeng. 2016 Jan;113(1):26-38. Epub 2015 Oct 27. [CrossRef] [PubMed]
- Berger, S.L., Kouzarides, T., Shiekhattar, R., & Shilatifard, A. (2009). An operational definition of epigenetics. Genes & Development, 23(7), 781–783. [CrossRef]
- Feinberg, A.P. (2007). Phenotypic plasticity and the epigenetics of human disease. Nature, 447(7143), 433–440. [CrossRef]
- Lister, R., & Ecker, J.R. (2009). Finding the fifth base: genome-wide sequencing of cytosine methylation. Genome Research, 19(6), 959–966. [CrossRef]
- Mikkelsen, T. S., et al. (2007). Genome-wide maps of chromatin state in pluripotent and lineage-committed cells. Nature, 448(7153), 553-560. [CrossRef]
- Walsh, G. (2010). Post-translational modifications of protein biopharmaceuticals. Drug Discovery Today, 15(17-18), 773-780. [CrossRef]
- Laugesen, A., & Helin, K. (2014). Chromatin repressive complexes in stem cells, development, and cancer. Cell Stem Cell, 14(6), 735-751. [CrossRef]
- Rothbart, S. B., & Strahl, B. D. (2014). Interpreting the language of histone and DNA modifications. Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms, 1839(8), 627-643.
- Dillon, S. C., Zhang, X., Trievel, R. C., & Cheng, X. (2005). The SET-domain protein superfamily: Protein lysine methyltransferases. Genome Biology, 6(8), 227. [CrossRef]
- Egger, G., Liang, G., Aparicio, A., & Jones, P. A. (2004). Epigenetics in human disease and prospects for epigenetic therapy. Nature, 429(6990), 457-463. [CrossRef]
- Beck, A., et al. (2013). Analytical characterization of biosimilar antibodies and Fc-fusion proteins. TrAC Trends in Analytical Chemistry, 48, 81-95. [CrossRef]
- Nicholson, J.K., Lindon, J.C., Holmes, E. (1999). 'Metabonomics': understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica, 29, 1181–1189. [CrossRef]
- Wishart, D. S. (2008). Metabolomics: Applications to food science and nutrition research. Trends in Food Science & Technology, 19(9), 482-493. [CrossRef]
- Johnson, C. H., Gonzalez, F. J. (2012). Challenges and opportunities of metabolomics. Journal of Cellular Physiology, 227(8), 2975–2981. https://doi.org/. [CrossRef]
- Sengupta, N., et al. (2018). Metabolomics Analysis of Recombinant Escherichia coli Expression Systems for Recombinant Protein Production. Journal of Proteomics & Bioinformatics, 11(5), 110-120.
- Becker, J., et al. (2011). Metabolic flux analysis of Escherichia coli in glucose-limited continuous culture. II. Dynamic response to famine and feast, activation of the methylglyoxal pathway and oscillatory behaviour. Microbiology, 157(Pt 3), 707-717.
- Barteneva, N. S., et al. (2013). Circulating microparticles: square the circle. BMC Cell Biology, 14, 23. [CrossRef]
- Bollard, M. E., et al. (2005). A study of metabolic compartmentation in the rat heart and cardiac mitochondria using high-resolution magic angle spinning 1H NMR spectroscopy. FEBS Letters, 579(8), 1779-1788. [CrossRef]
- Rogers, R. S., et al. (2013). Development of a quantitative mass spectrometry multi-attribute method for characterization, quality control testing and disposition of biologics. mAbs, 7(5), 881-890. [CrossRef]
- Zhao, Y. Y., & Lin, R. C. (2014). UPLC-MS(E) application in disease biomarker discovery: the discoveries in proteomics to metabolomics. Chemico-Biological Interactions, 215, 7-16.
- Patti, G. J., Yanes, O., & Siuzdak, G. (2012). Innovation: Metabolomics: the apogee of the omics trilogy. Nature Reviews Molecular Cell Biology, 13(4), 263-269.
- Lange, M., et al. (2017). Multi-platform metabolomics analyses of ergosterol-induced dynamic changes in Nicotiana tabacum cells. PloS One, 12(1), e0169741.
- Ku, G.Y., et al. (2010). Single-institution experience with ipilimumab in advanced melanoma patients in the compassionate use setting. Cancer, 116(7), 1767-1775. [CrossRef]
- Burmester, G.R., et al. (2003). Adalimumab (a fully human anti-tumour necrosis factor α monoclonal antibody) in the treatment of active rheumatoid arthritis: the initial results of five trials. Annals of the Rheumatic Diseases, 62(Suppl 2), ii46-ii50.
- Ribas, A., et al. (2016). PD-1 Blockade Expands Intratumoral Memory T Cells. Cancer Immunology Research, 4(3), 194-203. [CrossRef]
- Gottenberg, J.E., et al. (2010). Serum immunoglobulin levels and risk factors for hypogammaglobulinemia during longterm treatment with rituximab in primary Sjögren’s syndrome. Journal of Autoimmunity, 35(3), 241-247.
- Ternant, D., et al. (2008). An enzyme-linked immunosorbent assay for therapeutic drug monitoring of infliximab. Ther Drug Monit, 30(2), 169-174. [CrossRef]
- Hyland PL, et al., Evaluating the Utility of Proteomics for the Identification of Circulating Pharmacodynamic Biomarkers of IFNβ-1a Biologics. Clin Pharmacol Ther. 2023 Jan;113(1):98-107. [CrossRef]
- Innovations in Biosimilars. Clin Pharmacol Ther. 2023 Jan. 1-195. [CrossRef]
- Sheikhy M, Schrieber SJ, Sun Q, et al. Considerations for use of pharmacodynamic biomarkers to support biosimilar development – (I) a randomized trial with PCSK9 inhibitors. Clin Pharmacol Ther. 2023 Jan. 71-79. [CrossRef]
- https://www.fda.gov/drugs/news-events-human-drugs/pharmacodynamic-biomarkers-their-role-biosimilar-product-development#footnote4_55gxd3i.
- Gershuny V, Sun Q, Schrieber SJ, et al. Considerations for use of pharmacodynamic biomarkers to support biosimilar development – (II) a randomized trial with IL-5 antagonists. Clin Pharmacol Ther. 2023 Jan. 80-89. [CrossRef]
- https://www.fda.gov/drugs/news-events-human-drugs/pharmacodynamic-biomarkers-their-role-biosimilar-product-development#footnote5_8tarc9n.
- Hyland, PL, Chekka LMS, Samarth DP, et al. Evaluating the utility of proteomics for the identification of circulating pharmacodynamic biomarkers of IFNβ-1a biologics. Clin Pharmacol Ther. 2023 Jan. 98-107. [CrossRef]
- Li F, Sun Q, Du S, et al. Model-Based Approach to Selecting Pegfilgrastim Dose for Pharmacokinetic and Pharmacodynamic Similarity Studies in Biosimilar Development. Clin Pharmacol Ther. 2023 Jan. 62-70. [CrossRef]
- Schiestl, M., Stangler, T., Torella, C., Čepeljnik, T., Toll, H., & Grau, R. (2011). Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nature Biotechnology, 29(4), 310-312. [CrossRef]
- Sellick, C. A., Croxford, A. S., Maqsood, A. R., Stephens, G., & Goodacre, R. (2015). Metabolite profiling of recombinant CHO cells: designing tailored feeding regimes that enhance recombinant antibody production. Biotechnology and Bioengineering, 112(12), 2575-2585. [CrossRef]
- U.S. Food and Drug Administration (FDA). (2020). Clinical Pharmacology Data to Support a Demonstration of Biosimilarity to a Reference Product: Guidance for Industry. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-pharmacology-data-support-demonstration-biosimilarity-reference-product.
- European Medicines Agency (EMA). (2014). Guideline on similar biological medicinal products. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-similar-biological-medicinal-products-rev1_en.pdf.
- https://drugs.ncats.io/substances?facet=Development%20Status%2FUS%20Approved%20Rx&facet=Substance%20Class%2Fprotein&facet=Substance%20Form%2FPrincipal%20Form&page=1.
- Topol EJ, et al. (1994). Randomised placebo-controlled and balloon-angioplasty-controlled trial to assess safety of coronary stenting with use of platelet glycoprotein-IIb/IIIa blockade. Lancet. 344(8916): 494-502. [CrossRef]
- Weinblatt ME, et al. (2003). Adalimumab, a fully human anti-tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 48(1):35-45. [CrossRef]
- Hill-Cawthorne GA, et al. (2012). Long-term lymphocyte reconstitution after alemtuzumab treatment of multiple sclerosis. J Neurol Neurosurg Psychiatry. 83(3):298-304. [CrossRef]
- Rittmeyer A, et al. (2017). Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 389(10066):255-265. [CrossRef]
- Nashan B, et al. (1997). Randomised trial of basiliximab versus placebo for control of acute cellular rejection in renal allograft recipients. Lancet. 350(9086):1193-8. [CrossRef]
- Navarra SV, et al. (2011). Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet. 377(9767):721-31. [CrossRef]
- Hurwitz H, et al. (2004). Bevacizumab plus Irinotecan, Fluorouracil, and Leucovorin for Metastatic Colorectal Cancer. N Engl J Med. 350:2335-2342. [CrossRef]
- Cunningham D, et al. (2004). Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 351(4):337-45. [CrossRef]
- Kappos L, et al. (2015). Daclizumab HYP versus Interferon Beta-1a in Relapsing Multiple Sclerosis. N Engl J Med. 373(15):1418-28. [CrossRef]
- Lokhorst HM, et al. (2015). Targeting CD38 with Daratumumab Monotherapy in Multiple Myeloma. N Engl J Med. 373:1207-1219. [CrossRef]
- Cummings SR, et al. (2009). Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 361(8):756-65.
- Simpson EL, et al. (2016). Two Phase 3 Trials of Dupilumab versus Placebo in Atopic Dermatitis. N Engl J Med. 375(24):2335-2348. [CrossRef]
- Hillmen P, et al. (2006). Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria. N Engl J Med. 355(12):1233-43. [CrossRef]
- Hanauer SB, et al. (2002). Maintenance infliximab for Crohn's disease: the ACCENT I randomised trial. Lancet. 359(9317):1541-9.
- Hodi FS, et al. (2010). Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 363(8):711-23. [CrossRef]
- Brahmer J, et al. (2015). Nivolumab versus Docetaxel in Advanced Squamous-Cell Non–Small-Cell Lung Cancer. N Engl J Med. 373:123-35. [CrossRef]
- Goede V, et al. (2014). Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 370(12):1101-10. [CrossRef]
- Wierda WG, et al. (2010). Ofatumumab as single-agent CD20 immunotherapy in fludarabine-refractory chronic lymphocytic leukemia. J Clin Oncol. 28(10):1749-55. [CrossRef]
- Busse W, et al. (2001). Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol. 108(2):184-90. [CrossRef]
- The IMpact-RSV Study Group. (1998). Palivizumab, a Humanized Respiratory Syncytial Virus Monoclonal Antibody, Reduces Hospitalization From Respiratory Syncytial Virus Infection in High-risk Infants. Pediatrics. 102(3 Pt 1):531-537. [CrossRef]
- Robert C, et al. (2015). Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med. 372(26):2521-2532. [CrossRef]
- Maloney DG, et al. (1997). IDEC-C2B8 (Rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed low-grade non-Hodgkin's lymphoma. Blood. 90(6):2188-95.
- Fleischmann R, et al. (2017). Sarilumab and Nonbiologic Disease-Modifying Antirheumatic Drugs in Patients With Active Rheumatoid Arthritis and Inadequate Response or Intolerance to Tumor Necrosis Factor Inhibitors. Arthritis Rheumatol. 69(2):277-290. [CrossRef]
- Langley RG, et al. (2014). Secukinumab in Plaque Psoriasis--Results of Two Phase 3 Trials. N Engl J Med. 371(4):326-38. [CrossRef]
- Maini RN, et al. (2006). Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 41(9):1552-63.
- Slamon DJ, et al. (2001). Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 344(11):783-92. [CrossRef]
- Feagan BG, et al. (2013). Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 369(8):699-710. [CrossRef]
- Wagner, J.G. (1968). Fundamentals of Clinical Pharmacokinetics. American Pharmaceutical Association.
- Jin, J.Y., Almon, R.R., DuBois, D.C., & Jusko, W.J. (2017). Comparative Pharmacodynamics of Rosiglitazone, Pioglitazone, and Troglitazone in Cultured Human and Rat Adipocytes. Drug Metabolism and Disposition, 45(2), 160-167.
- Mager, D.E., & Jusko, W.J. (2001). General Pharmacokinetic Model for Drugs Exhibiting Target-Mediated Drug Disposition. Journal of Pharmacokinetics and Pharmacodynamics, 28(6), 507-532. [CrossRef]
- Lee, J.Y., Lee, J.H., & Kim, Y.H. (2010). Clinical Pharmacology in Drug Development: An Overview of Phase 1 Studies. Korean Journal of Physiology & Pharmacology, 14(5), 283-290.
- Bruno, R., Washington, C.B., Lu, J.F., Lieberman, G., Banken, L., & Klein, P. (2005). Population Pharmacokinetics of Trastuzumab in Patients With HER2+ Metastatic Breast Cancer. Cancer Chemotherapy and Pharmacology, 56(4), 361-369. [CrossRef]
- Frampton, J.E., & Peters, D.H. (1999). Epoetin Alfa: A Review of its Pharmacodynamic and Pharmacokinetic Properties and Therapeutic Use in Nonrenal Applications. Drugs, 57(2), 233-260.
- FDA. (2019). Considerations in Demonstrating Interchangeability With a Reference Product: Guidance for Industry. U.S. Food and Drug Administration.
- Turner, D.C., Navid, F., Daw, N.C., Mao, S., Wu, J., Santana, V.M., & Neel, M. (2018). Population Pharmacokinetics of Bevacizumab in Children with Osteosarcoma: Implications for Dosing. Clinical Cancer Research, 24(6), 1480-1487.
- Mould, D.R., Upton, R.N., Wojciechowski, J. (2012). Dashboards for Monitoring Clinical Trials. Clinical Pharmacology & Therapeutics, 91(5), 927-937.
- Davies, B., Morris, T. (2013). Physiological Parameters in Laboratory Animals and Humans. Pharmaceutical Research, 10(7), 1093-1095. [CrossRef]
- Thompson, L., Boudinot, F.D., Nagar, S. (2019). Pharmacokinetics and Pharmacodynamics of Approved and Investigational Janus Kinase Inhibitors. Clinical Pharmacokinetics, 58(9), 1103-1118.
- Mager, D.E., & Krzyzanski, W. (2005). Quasi-equilibrium pharmacokinetic model for drugs exhibiting target-mediated drug disposition. Pharmaceutical Research, 22(10), 1589-1596. [CrossRef]
- Danhof, M., de Lange, E.C., Della Pasqua, O.E., Ploeger, B.A., & Voskuyl, R.A. (2007). Mechanism-based pharmacokinetic-pharmacodynamic (PK-PD) modeling in translational drug research. Trends in Pharmacological Sciences, 28(4), 186-191. [CrossRef]
- El-Kareh, A.W., & Secomb, T.W. (2000). A mathematical model for comparison of bolus injection, continuous infusion, and liposomal delivery of doxorubicin to tumor cells. Neoplasia, 2(4), 325-338. [CrossRef]
- Craig, W.A. (1998). Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clinical Infectious Diseases, 26(1), 1-10. [CrossRef]
- Gibiansky, L., & Gibiansky, E. (2009). Target-mediated drug disposition model and its approximations for antibody-drug conjugates. Journal of Pharmacokinetics and Pharmacodynamics, 36(1), 25-45. [CrossRef]
- Turnheim, K. (2003). When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Experimental Gerontology, 38(8), 843-853. [CrossRef]
- Bonate, P.L. (2011). Pharmacokinetic-Pharmacodynamic Modeling and Simulation. Springer. [CrossRef]
- Leach, M.W. & Ruff, D. (2013). Biomarkers, Pharmacodynamics and Drug Development. Journal of Pharmacology & Experimental Therapeutics. 3:153–158.
- Sung, J.A., et al., (2015). Dual-Affinity Re-Targeting proteins direct T cell-mediated cytolysis of latently HIV-infected cells. J Clin Invest. 125(11):4077-4090. [CrossRef]
- Hardie DG. AMPK: positive and negative regulation, and its role in whole-body energy homeostasis. Curr Opin Cell Biol. 2015;33:1-7. [CrossRef]
- Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473(7347):298-307.
- Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35(4):495-516.
- Klionsky DJ, Abdelmohsen K, Abe A, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy. 2016;12(1):1-222.
- Mizushima N, Levine B. Autophagy in mammalian development and differentiation. Nat Cell Biol. 2010;12(9):823-830. [CrossRef]
- Davie EW, Kulman JD. An overview of the structure and function of thrombin. Semin Thromb Hemost. 2006;32(Suppl 1):3-15. [CrossRef]
- Seibel MJ. Biochemical markers of bone turnover part I: biochemistry and variability. Clin Biochem Rev. 2005;26(4):97-122.
- Berridge MJ, Bootman MD, Roderick HL. Calcium signalling: dynamics, homeostasis and remodelling. Nat Rev Mol Cell Biol. 2003;4(7):517-529. [CrossRef]
- Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9(3):153-166. [CrossRef]
- Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324(5930):1029-1033. [CrossRef]
- Maecker HT, Ghanekar SA, Suni MA, et al. Factors affecting the efficiency of CD8+ T cell cross-priming with exogenous antigens. J Immunol. 2001;166(12):7268-7275. [CrossRef]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646-674. [CrossRef]
- Manning BD, Toker A. AKT/PKB Signaling: Navigating the Network. Cell. 2017;169(3):381-405.
- Maecker HT, McCoy JP, Nussenblatt R. Standardizing immunophenotyping for the Human Immunology Project. Nat Rev Immunol. 2012;12(3):191-200. [CrossRef]
- Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18(3):164-179. [CrossRef]
- Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11(9):785-797. [CrossRef]
- Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281(1):8-27. [CrossRef]
- Ciccia A, Elledge SJ. The DNA damage response: making it safe to play with knives. Mol Cell. 2010;40(2):179-204. [CrossRef]
- Gabrielsson J, Weiner D. Pharmacokinetic and Pharmacodynamic Data Analysis: Concepts and Applications. 5th Edition. Swedish Pharmaceutical Press. 2016.
- Lu HC, Mackie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79(7):516-525. [CrossRef]
- Newell-Price J, Bertagna X, Grossman AB, Nieman LK. Cushing's syndrome. Lancet. 2006;367(9522):1605-1617.
- Doherty GJ, McMahon HT. Mechanisms of endocytosis. Annu Rev Biochem. 2009;78:857-902.
- Poljsak B, Šuput D, Milisav I. Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxid Med Cell Longev. 2013;2013:956792. [CrossRef]
- Hetz C, Zhang K, Kaufman RJ. Mechanisms, regulation, and functions of the unfolded protein response. Nat Rev Mol Cell Biol. 2020;21(8):421-438. [CrossRef]
- Huotari J, Helenius A. Endosome maturation. EMBO J. 2011;30(17):3481-3500.
- Pober JS, Sessa WC. Evolving functions of endothelial cells in inflammation. Nat Rev Immunol. 2007;7(10):803-815.
- Copeland RA, Pompliano DL, Meek TD. Drug-target residence time and its implications for lead optimization. Nat Rev Drug Discov. 2006;5(9):730-739. [CrossRef]
- Feinberg AP. Phenotypic plasticity and the epigenetics of human disease. Nature. 2007;447(7143):433-440. [CrossRef]
- Mathieu M, Martin-Jaular L, Lavieu G, Théry C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat Cell Biol. 2019;21(1):9-17.
- Lu P, Takai K, Weaver VM, Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol. 2011;3(12):a005058.
- Jeong JH, Chang JS, Jo YH. Fatty acid-induced lipotoxicity in pancreatic beta-cells during development of type 2 diabetes. Front Endocrinol (Lausanne). 2018;9:384.
- Perfetto SP, Chattopadhyay PK, Roederer M. Seventeen-colour flow cytometry: unravelling the immune system. Nat Rev Immunol. 2004;4(8):648-655. [CrossRef]
- Macarron R, Banks MN, Bojanic D, et al. Impact of high-throughput screening in biomedical research. Nat Rev Drug Discov. 2011;10(3):188-195. [CrossRef]
- Quackenbush J. Microarray analysis and tumor classification. N Engl J Med. 2006;354(23):2463-2472. [CrossRef]
- Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324(5930):1029-1033. [CrossRef]
- Varki A. Biological roles of glycans. Glycobiology. 2017;27(1):3-49.
- Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375(24):2369-2379.
- Kampinga HH, Hageman J, Vos MJ, et al. Guidelines for the nomenclature of the human heat shock proteins. Cell Stress Chaperones. 2009;14(1):105-111. [CrossRef]
- Hartl FU, Bracher A, Hayer-Hartl M. Molecular chaperones in protein folding and proteostasis. Nature. 2011;475(7356):324-332. [CrossRef]
- Bannister AJ, Kouzarides T. Regulation of chromatin by histone modifications. Cell Res. 2011;21(3):381-395.
- Rosen ED, Spiegelman BM. Adipocytes as regulators of energy balance and glucose homeostasis. Nature. 2006;444(7121):847-853. [CrossRef]
- Semenza GL. Hypoxia-inducible factors in physiology and medicine. Cell. 2012;148(3):399-408. [CrossRef]
- Gambhir SS. Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer. 2002;2(9):683-693. [CrossRef]
- van Schouwenburg PA, Rispens T, Wolbink GJ. Immunogenicity of anti-TNF biologic therapies for rheumatoid arthritis. Nat Rev Rheumatol. 2013;9(3):164-172. [CrossRef]
- Heneka MT, Kummer MP, Latz E. Innate immune activation in neurodegenerative disease. Nat Rev Immunol. 2014;14(7):463-477. [CrossRef]
- Jan LY, Jan YN. Structural elements involved in specific K+ channel functions. Nature. 1990;346(6286):672-675. [CrossRef]
- Muckenthaler MU, Rivella S, Hentze MW, Galy B. A red carpet for iron metabolism. Cell. 2017;168(3):344-361.
- Mager DE, Jusko WJ. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn. 2001;28(6):507-532. [CrossRef]
- Schreiber G, Keating AE. Protein binding specificity versus promiscuity. Curr Opin Struct Biol. 2011;21(1):50-61.
- Wenk MR. The emerging field of lipidomics. Nat Rev Drug Discov. 2005;4(7):594-610. [CrossRef]
- Singh R, Kaushik S, Wang Y, et al. Autophagy regulates lipid metabolism. Nature. 2009;458(7242):1131-1135.
- Platt FM, d'Azzo A, Davidson BL, Neufeld EF, Tifft CJ. Lysosomal storage diseases. Nat Rev Dis Primers. 2018;4:27.
- Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115(2):209-218.
- DeBerardinis RJ, Thompson CB. Cellular metabolism and disease: what do metabolic outliers teach us? Cell. 2012;148(6):1132-1144.
- Rupaimoole R, Slack FJ. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov. 2017;16(3):203-222. [CrossRef]
- Youle RJ, van der Bliek AM. Mitochondrial fission, fusion, and stress. Science. 2012;337(6098):1062-1065.
- Pickles S, Vigié P, Youle RJ. Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr Biol. 2018;28(4):R170-R185.
- Scotti MM, Swanson MS. RNA mis-splicing in disease. Nat Rev Genet. 2016;17(1):19-32. [CrossRef]
- Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149(2):274-293. [CrossRef]
- Franklin RJ, Ffrench-Constant C. Regenerating CNS myelin – from mechanisms to experimental medicines. Nat Rev Neurosci. 2017;18(12):753-769. [CrossRef]
- Minatohara K, Akiyoshi M, Okuno H. Role of immediate-early genes in synaptic plasticity and neuronal ensembles underlying the memory trace. Front Mol Neurosci. 2015;8:78. [CrossRef]
- Hinz M, Stein A, Uncini T. Monoamine oxidase inhibition and mood. Neurotox Res. 2011;21(1):81-89.
- Skaper SD. Neurotrophic factors: an overview. Methods Mol Biol. 2018;1727:1-17. [CrossRef]
- Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33(7):829-837. [CrossRef]
- Suzuki T, Yamamoto M. Molecular basis of the Keap1–Nrf2 system. Free Radic Biol Med. 2015;88(Pt B):93-100.
- Lane AN, Fan TW. Regulation of mammalian nucleotide metabolism and biosynthesis. Nucleic Acids Res. 2015;43(4): 2466-2485. [CrossRef]
- Wallace DC. Mitochondria and cancer. Nat Rev Cancer. 2012;12(10):685-698.
- Sies H. Oxidative stress: a concept in redox biology and medicine. Redox Biol. 2015;4:180-183. [CrossRef]
- Griffiths WJ, Wang Y. Oxysterol research: a brief review. Biochem Soc Trans. 2019;47(2):517-526. [CrossRef]
- Ahmadian M, Suh JM, Hah N, et al. PPARγ signaling and metabolism: the good, the bad and the future. Nat Med. 2013;19(5):557-566.
- Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature. 2015;526(7573):343-350.
- Cohen P. The role of protein phosphorylation in human health and disease. Eur J Biochem. 2001;268(19):5001-5010. [CrossRef]
- Bedford L, Paine S, Sheppard PW, Mayer RJ, Roelofs J. Assembly, structure, and function of the 26S proteasome. Trends Cell Biol. 2010;20(7):391-401. [CrossRef]
- Aebersold R, Mann M. Mass spectrometry-based proteomics. Nature. 2003;422(6928):198-207.
- Ray PD, Huang BW, Tsuji Y. Reactive oxygen species (ROS) homeostasis and redox regulation in cellular signaling. Cell Signal. 2012;24(5):981-990. [CrossRef]
- Lobo ED, Hansen RJ, Balthasar JP. Antibody pharmacokinetics and pharmacodynamics. J Pharm Sci. 2004;93(11):2645-2668. [CrossRef]
- Coppé JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol. 2010;5:99-118. [CrossRef]
- Houtkooper RH, Pirinen E, Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol. 2012;13(4):225-238. [CrossRef]
- Shay JW, Wright WE. Role of telomeres and telomerase in cancer. Semin Cancer Biol. 2011;21(6):349-353. [CrossRef]
- Turner JR. Molecular basis of epithelial barrier regulation: from basic mechanisms to clinical application. Am J Pathol. 2006;169(6):1901-1909.
- Watt FM, Driskell RR. The therapeutic potential of stem cells. Philos Trans R Soc Lond B Biol Sci. 2010;365(1537):155-163.
- Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423-1437. [CrossRef]
- Walter P, Ron D. The unfolded protein response: from stress pathway to homeostatic regulation. Science. 2011;334(6059):1081-1086.
- Clevers H, Nusse R. Wnt/β-catenin signaling and disease. Cell. 2012;149(6):1192-1205.
- Ferrara, N., & Adamis, A. P. (2016). Ten years of anti-vascular endothelial growth factor therapy. Nature Reviews Drug Discovery, 15(6), 385. [CrossRef]
- Keystone, E., Heijde, D., Mason Jr, D., Landewé, R., Vollenhoven, R. V., Combe, B., ... & Kavanaugh, A. (2008). Certolizumab pegol plus methotrexate is significantly more effective than placebo plus methotrexate in active rheumatoid arthritis: findings of a fifty-two–week, phase III, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis & Rheumatism, 58(11), 3319-3329.
- Sevigny J. et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature 537.7618 (2016): 50-56.
- Heier JS. et al. Intravitreal Aflibercept (VEGF Trap-Eye) in Wet Age-related Macular Degeneration. Ophthalmology 119.12 (2012): 2537-2548. [CrossRef]
- Schiffmann R. et al. Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA 285.21 (2001): 2743-2749.
- Eng CM. et al. Safety and efficacy of recombinant human alpha-galactosidase A replacement therapy in Fabry's disease. N Engl J Med 345.1 (2001): 9-16.
- GlaxoSmithKline. (2014). Tanzeum (albiglutide) [Package Insert]. U.S. Food and Drug Administration website.
- Santagostino E. et al. Long-acting recombinant coagulation factor IX albumin fusion protein (rIX-FP) in hemophilia B: results of a phase 3 trial. J Thromb Haemost 14.3 (2016): 484-497.
- Atkins MB. et al. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J Sci Am 5.1 (1999): 16-27.
- Krueger GG. et al. A human interleukin-12/23 monoclonal antibody for the treatment of psoriasis. N Engl J Med 356.6 (2007): 580-592.
- Cohen JA. et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet 380.9856 (2012): 1819-1828.
- Brady RO. et al. Replacement therapy for inherited enzyme deficiency. Macrophage-targeted glucocerebrosidase for Gaucher's disease. N Engl J Med 324.21 (1991): 1464-1470.
- Robinson, J. G., Farnier, M., Krempf, M., Bergeron, J., Luc, G., Averna, M., ... & Koren, M. J. (2015). Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. New England Journal of Medicine, 372(16), 1489-1499. [CrossRef]
- Stockley RA. et al. Biochemical efficacy and safety of monthly augmentation therapy for alpha1-antitrypsin deficiency. Chest 121.1 (2002): 57-65.
- Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333.24 (1995): 1581-1587.
- Moores SL, et al. A novel bispecific antibody targeting EGFR and cMet is effective against EGFR inhibitor-resistant lung tumors. Cancer Res 76.13 (2016): 3942-3953. [CrossRef]
- Fleischmann, R. M., Tesser, J., Schiff, M. H., Schechtman, J., Burmester, G. R., Bennett, R., ... & Zheng, S. (2006). Safety of extended treatment with anakinra in patients with rheumatoid arthritis. Annals of Rheumatic Diseases, 65(8), 1006-1012. [CrossRef]
- Bensinger W, et al. A randomized study of peripheral blood progenitor cell mobilization with chemotherapy plus the hematopoietic growth factors recombinant human stem cell factor (ancestim) and recombinant human granulocyte colony-stimulating factor. Blood 95.9 (2000): 2730-2737.
- Connolly SJ, et al. Andexanet alfa for acute major bleeding associated with factor Xa inhibitors. N Engl J Med 375.12 (2016): 1131-1141. [CrossRef]
- Furie R, et al. Anifrolumab, an Anti-Interferon-α Receptor Monoclonal Antibody, in Moderate-to-Severe Systemic Lupus Erythematosus. Arthritis Rheumatol 69.2 (2017): 376-386. [CrossRef]
- Neuhaus KL, et al. Intravenous recombinant tissue-type plasminogen activator (rt-PA) and intracoronary streptokinase in acute myocardial infarction: the European Cooperative Study Group for rt-PA. Am J Cardiol 60.14 (1987): B3-B9.
- Mulangu S, et al. A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med 381.24 (2019): 2293-2303.
- Herbst, R. S., Soria, J. C., Kowanetz, M., Fine, G. D., Hamid, O., Gordon, M. S., ... & Chen, D. S. (2014). Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature, 515(7528), 563-567.
- Kaufman, H. L., Russell, J., Hamid, O., Bhatia, S., Terheyden, P., D'Angelo, S. P., ... & Bannavong, D. (2016). Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. The Lancet Oncology, 17(10), 1374-1385. [CrossRef]
- Bleecker ER, et al. Benralizumab to prevent COPD exacerbations. N Engl J Med 381.11 (2019): 1023-1034.
- Krueger JG, et al. Anti–IL-1α monoclonal antibody MABp1 in patients with hidradenitis suppurativa. JCI Insight 4.2 (2019).
- Ferrara, N., et al. (2005). Vascular endothelial growth factor is essential for corpus luteum angiogenesis. Nat Med, 4(3), 336-340. [CrossRef]
- 367.Wilcox, M. H., et al. (2017). Bezlotoxumab for prevention of recurrent. [CrossRef]
- 368.Wilcox MH, et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med 376.4 (2017): 305-317. [CrossRef]
- Glatt S, et al. Bimekizumab dual inhibition of IL-17A and IL-17F provides evidence of IL-17F contribution to chronic inflammation in disease-relevant cells. Ann Rheum Dis 76.2 (2017): 213-222.
- Lincoff AM, et al. Bivalirudin and provisional glycoprotein IIb/IIIa blockade compared with heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary intervention. JAMA 289.7 (2003): 853-863. [CrossRef]
- Topp, M. S., Gökbuget, N., Stein, A. S., Zugmaier, G., O'Brien, S., Bargou, R. C., ... & Raff, T. (2015). Safety and activity of blinatumomab for adult patients with relapsed or refractory B-precursor acute lymphoblastic leukaemia: a multicentre, single-arm, phase 2 study. The Lancet Oncology, 16(1), 57-66. [CrossRef]
- Katagiri, T., & Watabe, T. (2016). Bone morphogenetic proteins. Cold Spring Harbor Perspectives in Biology, 8(6), a021899. [CrossRef]
- Carruthers A, Carruthers J. Botulinum toxin type A. J Am Acad Dermatol 53.3 (2005): 284-290.
- Comella CL, et al. Botulinum toxin type B in cervical dystonia: a double-blind, placebo-controlled, safety and efficacy study. Neurology 59.5 (2002): 701-707.
- Tap, W. D., Jones, R. L., Van Tine, B. A., Chmielowski, B., Elias, A. D., Adkins, D., ... & Agulnik, M. (2016). Olaratumab and doxorubicin versus doxorubicin alone for treatment of soft-tissue sarcoma: an open-label phase 1b and randomised phase 2 trial. The Lancet, 388(10043), 488-497. [CrossRef]
- Dugel PU, et al. HAWK and HARRIER: Phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology 127.1 (2020): 72-84. [CrossRef]
- Carpenter TO, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med 378.21 (2018): 1987-1998.
- Hijiya N, et al. A phase 2 study of calaspargase pegol extended dosing every 3 weeks versus pegaspargase every 2 weeks in patients with newly diagnosed high-risk acute lymphoblastic leukemia. Blood 130.Suppl 1 (2017): 985-985.
- Ruperto, N., Brunner, H. I., Quartier, P., Constantin, T., Wulffraat, N., Horneff, G., ... & Brik, R. (2012). Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. New England Journal of Medicine, 367(25), 2396-2406. [CrossRef]
- Cunningham, D., Humblet, Y., Siena, S., Khayat, D., Bleiberg, H., Santoro, A., ... & Bets, D. (2004). Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. New England Journal of Medicine, 351(4), 337-345. [CrossRef]
- Fraser RD. Chymopapain for chemonucleolysis. Orthop Clin North Am 33.2 (2002): 375-382.
- White GC 2nd, et al. Use of recombinant factor IX in subjects with haemophilia B undergoing surgery. Haemophilia 8.2 (2002): 91-97.
- Hedner U. Recombinant activated factor VII: 30 years of research and innovation. Blood Rev 29.2 (2015): 81-89. [CrossRef]
- Falabella AF, Carson P. The use of enzymatic agents in the treatment of chronic ulcers. Clin Dermatol 14.1 (1996): 59-65.
- Zuraw BL, et al. Nanofiltered C1 inhibitor concentrate for treatment of hereditary angioedema. N Engl J Med 363.6 (2010): 513-522. [CrossRef]
- Kerrigan JR, Veldhuis JD. Dose response of arginine vasopressin to ACTH in man. J Clin Endocrinol Metab 70.1 (1990): 216-220.
- Abdu TA, et al. ACTH stimulation tests for the diagnosis of adrenal insufficiency: Systematic review and meta-analysis. Endocrine 41.2 (2012): 188-199.
- Ataga KI, et al. Crizanlizumab for the Prevention of Pain Crises in Sickle Cell Disease. N Engl J Med 376.5 (2017): 429-439. [CrossRef]
- Macdougall, I. C., & Cooper, A. C. (2002). The inflammatory response and epoetin sensitivity. Nephrology Dialysis Transplantation, 17(suppl_1), 48-52. [CrossRef]
- Cummings, S. R., San Martin, J., McClung, M. R., Siris, E. S., Eastell, R., Reid, I. R., ... & Reid, D. M. (2009). Denosumab for prevention of fractures in postmenopausal women with osteoporosis. New England Journal of Medicine, 361(8), 756-765. [CrossRef]
- Cummings, S. R., San Martin, J., McClung, M. R., Siris, E. S., Eastell, R., Reid, I. R., ... & Christiansen, C. (2009). Denosumab for prevention of fractures in postmenopausal women with osteoporosis. New England Journal of Medicine, 361(8), 756-765. [CrossRef]
- Simpson, E. L., Bieber, T., Guttman-Yassky, E., Beck, L. A., Blauvelt, A., Cork, M. J., ... & Worm, M. (2016). Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. New England Journal of Medicine, 375(24), 2335-2348.
- Antonia, S. J., Villegas, A., Daniel, D., Vicente, D., Murakami, S., Hui, R., ... & Arrieta, O. (2018). Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. New England Journal of Medicine, 379(24), 2342-2350. [CrossRef]
- Hillmen, P., Young, N. S., Schubert, J., Brodsky, R. A., Socie, G., Muus, P., ... & Hill, A. (2006). The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria. New England Journal of Medicine, 355(12), 1233-1243. [CrossRef]
- Riethmüller G, et al. Randomised trial of monoclonal antibody for adjuvant therapy of resected Dukes' C colorectal carcinoma. The Lancet 343.8907 (1994): 1177-1183.
- Lebwohl M, et al. Efalizumab for the treatment of moderate to severe plaque psoriasis: a randomized controlled trial. JAMA 290.23 (2003): 3073-3080.
- Howard JF, et al. Randomized phase 2 study of FcRn antagonist efgartigimod in generalized myasthenia gravis. Neurology 92.23 (2019): e2661-e2673. [CrossRef]
- Chien YH, et al. PEGylated recombinant adenosine deaminase (mPEG-rADA) therapy in infants and children with severe combined immunodeficiency. J Allergy Clin Immunol 123.3 (2009): 736-741.
- Hendriksz CJ, et al. Efficacy and safety of enzyme replacement therapy with BMN 110 (elosulfase alfa) for Morquio A syndrome (mucopolysaccharidosis IVA): a phase 3 randomised placebo-controlled study. J Inherit Metab Dis 37.6 (2014): 979-990. [CrossRef]
- Lonial, S., Dimopoulos, M., Palumbo, A., White, D., Grosicki, S., Spicka, I., ... & Richardson, P. G. (2015). Elotuzumab therapy for relapsed or refractory multiple myeloma. New England Journal of Medicine, 373(7), 621-631. [CrossRef]
- Locatelli F, et al. Emapalumab in primary hemophagocytic lymphohistiocytosis. N Engl J Med 382.19 (2020): 1811-1822.
- Oldenburg J, et al. Emicizumab prophylaxis in hemophilia A with inhibitors. N Engl J Med 377.9 (2017): 809-818. [CrossRef]
- Rosenberg JE, et al. Pivotal trial of enfortumab vedotin in urothelial carcinoma after platinum and anti-programmed death 1/programmed death ligand 1 therapy. J Clin Oncol 37.29 (2019): 2592.
- Goadsby, P. J., Reuter, U., Hallström, Y., Broessner, G., Bonner, J. H., Zhang, F., ... & Picard, H. (2017). A controlled trial of erenumab for episodic migraine. New England Journal of Medicine, 377(22), 2123-2132.
- Jelkmann, W. (2011). Regulation of erythropoietin production. Journal of Physiology, 589(6), 1251-1258. [CrossRef]
- Mendell, J. R., Goemans, N., Lowes, L. P., Alfano, L. N., Berry, K., Shao, J., ... & Malik, V. (2016). Longitudinal effect of eteplirsen versus historical control on ambulation in Duchenne muscular dystrophy. Annals of Neurology, 79(2), 257-271. [CrossRef]
- Sabatine, M. S., Giugliano, R. P., Keech, A. C., Honarpour, N., Wiviott, S. D., Murphy, S. A., ... & Pedersen, T. R. (2017). Evolocumab and clinical outcomes in patients with cardiovascular disease. New England Journal of Medicine, 376(18), 1713-1722. [CrossRef]
- Kessler CM, et al. An evaluation of Elase (fibrinolysin) ointment in the treatment of minor burns: results of a randomized clinical trial. J Burn Care Rehabil 7.4 (1986): 309-312.
- Crawford, J., & Becker, P. S. (2013). Role of the hematologist in the management of G-CSF–associated leukemia. Blood, 121(4), 509-511.
- van Wely M, et al. Recombinant versus urinary gonadotrophin for ovarian stimulation in assisted reproductive technology cycles. Cochrane Database Syst Rev 2.2 (2011): CD005354.
- Silberstein, S. D., Dodick, D. W., Bigal, M. E., Yeung, P. P., Goadsby, P. J., Blankenbiller, T., ... & Cohen, J. M. (2017). Fremanezumab for the preventive treatment of chronic migraine. New England Journal of Medicine, 377(22), 2113-2122. [CrossRef]
- Stauffer, V. L., Dodick, D. W., Zhang, Q., Carter, J. N., Ailani, J., & Conley, R. R. (2018). Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurology, 75(9), 1080-1088.
- Stauffer VL, et al. A phase 3 placebo-controlled study of galcanezumab in patients with chronic migraine: Results from the 3-month double-blind treatment phase of the REGAIN study. J Neurol Neurosurg Psychiatry 89.6 (2018): 603-611.
- Harmatz P, et al. Enzyme replacement therapy in mucopolysaccharidosis VI (Maroteaux-Lamy syndrome). J Pediatr 144.5 (2004): 574-580.
- Larson RA, et al. Final report of the efficacy and safety of gemtuzumab ozogamicin (Mylotarg) in patients with CD33-positive acute myeloid leukemia in first recurrence. Cancer 104.7 (2005): 1442-1452. [CrossRef]
- Oosterwijk E, et al. Expression of the Mr 34,000 transmembrane carbonic anhydrase isoenzyme IX in human renal cell carcinoma. Cancer Res 54.24 (1994): 6167-6171.
- Johnson KP, et al. Copolymer 1 reduces relapse rate and improves disability in relapsing-remitting multiple sclerosis: results of a phase III multicenter, double-blind, placebo-controlled trial. Neurology 45.7 (1995): 1268-1276. [CrossRef]
- Heller SR, Cryer PE. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Diabetes 40.2 (1991): 223-226.
- Widemann BC, et al. Glucarpidase, leucovorin, and thymidine for high-dose methotrexate–induced renal dysfunction: clinical and pharmacologic factors affecting outcome. J Clin Oncol 28.25 (2010): 3979-3986.
- Kavanaugh A, et al. Golimumab, a new human tumor necrosis factor α antibody, administered every four weeks as a subcutaneous injection in psoriatic arthritis. Arthritis Rheum 60.4 (2009): 976-986. [CrossRef]
- Juul, A. (2001). Serum levels of insulin-like growth factor I and its binding proteins in health and disease. Growth Hormone & IGF Research, 11(4), 113-170. [CrossRef]
- Blauvelt, A., Papp, K. A., Griffiths, C. E., Randazzo, B., Wasfi, Y., Shen, Y. K., ... & Reich, K. (2017). Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: results from the phase III, double-blinded, placebo-and active comparator–controlled VOYAGE 1 trial. Journal of the American Academy of Dermatology, 76(3), 405-417. [CrossRef]
- Zuraw BL, et al. Safety and efficacy of nanofiltered C1 inhibitor concentrate in hereditary angioedema. J Allergy Clin Immunol 126.2 (2010): 410-416.
- Cohen, J. A., Coles, A. J., Arnold, D. L., Confavreux, C., Fox, E. J., Hartung, H. P., ... & Compston, D. A. (2012). Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. The Lancet, 380(9856), 1819-1828. [CrossRef]
- Barton NW, et al. Replacement therapy for inherited enzyme deficiency—macrophage-targeted glucocerebrosidase for Gaucher's disease. N Engl J Med 324.21 (1991): 1464-1470.
- Cree BAC, et al. Inebilizumab for the treatment of neuromyelitis optica spectrum disorder (N-MOmentum): a double-blind, randomised placebo-controlled phase 2/3 trial. Lancet 394.10206 (2019): 1352-1363. [CrossRef]
- Tracey, D., Klareskog, L., Sasso, E. H., Salfeld, J. G., & Tak, P. P. (2008). Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacology & Therapeutics, 117(2), 244-279. [CrossRef]
- Kantarjian H, et al. Inotuzumab ozogamicin versus standard therapy for acute lymphoblastic leukemia. N Engl J Med 375.8 (2016): 740-753. [CrossRef]
- Turner RC, et al. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352.9131 (1998): 854-865. [CrossRef]
- Gibson, S. J., & Imbert-Fernandez, Y. (2014). Type I interferons and the innate immune response--more than just antiviral cytokines. Molecular Medicine Reports, 9(1), 1-6.
- Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363.8 (2010): 711-723. [CrossRef]
- Attal M, et al. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): a randomised, multicentre, open-label, phase 3 study. Lancet 394.10214 (2019): 2096-2107. [CrossRef]
- Moots R, et al. Itolizumab—a humanized anti-CD6 monoclonal antibody with a better side effects profile for the treatment of psoriasis. Clin Immunol 144.1 (2012): 63-67.
- Griffiths, C. E., Reich, K., Lebwohl, M., van de Kerkhof, P., Paul, C., Menter, A., ... & Braun, D. K. (2015). Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. The Lancet, 386(9993), 541-551. [CrossRef]
- Banerji, A., Riedl, M. A., Bernstein, J. A., Cicardi, M., Longhurst, H. J., Zuraw, B. L., ... & Lumry, W. R. (2018). Effect of lanadelumab compared with placebo on prevention of hereditary angioedema attacks: a randomized clinical trial. JAMA, 320(20), 2108-2121.
- Banerji A, et al. Inhibiting plasma kallikrein for hereditary angioedema prophylaxis. N Engl J Med 376.8 (2017): 717-728. [CrossRef]
- Kakkis ED, et al. Enzyme-replacement therapy in mucopolysaccharidosis I. N Engl J Med 344.3 (2001): 182-188.
- Greinacher A, et al. Lepirudin (recombinant hirudin) for parenteral anticoagulation in patients with heparin-induced thrombocytopenia. Circulation 100.6 (1999): 587-593. [CrossRef]
- Boccon-Gibod L, et al. Leuprolide depot 3.75 mg and 11.25 mg are effective and safe in a variety of patient populations with prostate cancer. Urology 60.1 (2002): 67-72.
- Marso, S. P., Daniels, G. H., Brown-Frandsen, K., Kristensen, P., Mann, J. F., Nauck, M. A., ... & Buse, J. B. (2016). Liraglutide and cardiovascular outcomes in type 2 diabetes. New England Journal of Medicine, 375(4), 311-322. [CrossRef]
- Hamadani M, et al. Preliminary Results of a Phase 1 Study of Loncastuximab Tesirine in Relapsed/Refractory B-cell Non-Hodgkin Lymphoma. Blood 134 (2019): 5327.
- Moya F, et al. A multicenter, randomized, masked, comparison trial of lucinactant, colfosceril palmitate, and beractant for the prevention of respiratory distress syndrome among very preterm infants. Pediatrics 115.4 (2005): 1018-1029. [CrossRef]
- Piga A, et al. Luspatercept improves hemoglobin levels and blood transfusion requirements in a study of patients with β-thalassemia. Blood 133.12 (2019): 1279-1289. [CrossRef]
- Platteau P, et al. Recombinant luteinizing hormone (r-LH) and recombinant follicle stimulating hormone (r-FSH) for ovarian stimulation in IVF/ICSI cycles: a comparative study. Hum Reprod 19.9 (2004): 2022-2030.
- Rugo HS, et al. Sophia study: a phase 3 (P3) study of margetuximab (M) + chemotherapy (C) versus trastuzumab (T) + C in patients (pts) with HER2+ metastatic (met) breast cancer (MBC) after prior anti-HER2 therapies (Tx). J Clin Oncol 37.15_suppl (2019): 1000. [CrossRef]
- Chernausek SD, et al. Long-term treatment with recombinant insulin-like growth factor (IGF)-I in children with severe IGF-I deficiency due to growth hormone insensitivity. J Clin Endocrinol Metab 93.3 (2008): 902-910. [CrossRef]
- Howles CM, et al. Recombinant follicle-stimulating hormone: development of the first biotechnology product for the treatment of infertility. Hum Reprod Update 1.3 (1995): 232-255.
- Ortega HG, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med 371.13 (2014): 1198-1207. [CrossRef]
- Chan JL, et al. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest 111.9 (2003): 1409-1421. [CrossRef]
- Moore KN, et al. Mirvetuximab soravtansine (IMGN853), a folate receptor alpha–targeting antibody-drug conjugate, in platinum-resistant epithelial ovarian cancer: A phase I expansion study. J Clin Oncol 36.7 (2018): 688-693.
- Ishida T, et al. CCL17 and CCL22 chemokines within tumor microenvironment are related to accumulation of Foxp3+ regulatory T cells in gastric cancer. Int J Cancer 122.10 (2008): 2286-2293.
- Kreitman RJ, et al. Moxetumomab pasudotox in relapsed/refractory hairy cell leukemia. Leukemia 32.8 (2018): 1768-1777. [CrossRef]
- Ortho Multicenter Transplant Study Group. A randomized clinical trial of OKT3 monoclonal antibody for acute rejection of cadaveric renal transplants. N Engl J Med 313.6 (1985): 337-342. [CrossRef]
- Polman, C. H., O'Connor, P. W., Havrdova, E., Hutchinson, M., Kappos, L., Miller, D. H., ... & Rudick, R. A. (2006). A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. New England Journal of Medicine, 354(9), 899-910. [CrossRef]
- Kushner BH, et al. Humanized 3F8 anti-GD2 monoclonal antibody dosing with granulocyte-macrophage colony-stimulating factor in patients with resistant neuroblastoma: a phase 1 clinical trial. JAMA Oncol 4.12 (2018): 1729-1735.
- Thatcher N, et al. Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): an open-label, randomised, controlled phase 3 trial. Lancet Oncol 16.7 (2015): 763-774. [CrossRef]
- Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA 287.12 (2002): 1531-1540.
- Mazurov V, et al. Efficacy and safety of netakimab, a new IL-17 inhibitor, in patients with active ankylosing spondylitis. Rheumatol Int 40.2 (2020): 297-306.
- Reddy BK, et al. Nimotuzumab provides survival benefit to patients with inoperable advanced squamous cell carcinoma of the head and neck: a randomized, open-label, phase IIb, 5-year study in Indian patients. Oral Oncol 50.5 (2014): 498-505. [CrossRef]
- Topalian, S. L., Hodi, F. S., Brahmer, J. R., Gettinger, S. N., Smith, D. C., McDermott, D. F., ... & Taube, J. M. (2012). Safety, activity, and immune correlates of anti–PD-1 antibody in cancer. New England Journal of Medicine, 366(26), 2443-2454.
- Koprowski H, et al. Specific antigen in serum of patients with colon carcinoma. Science 212.4490 (1981): 53-55. [CrossRef]
- Migone, T. S., Subramanian, G. M., Zhong, J., Healey, L. M., Corey, A., Devalaraja, M., ... & Tchistiakova, L. (2009). Raxibacumab for the treatment of inhalational anthrax. New England Journal of Medicine, 361(2), 135-144. [CrossRef]
- Goede V, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions." N Engl J Med 370.12 (2014): 1101-1110. [CrossRef]
- Hauser SL, et al. "Ocrelizumab versus interferon beta-1a in relapsing multiple sclerosis." N Engl J Med 376.3 (2017): 221-234. [CrossRef]
- Stalmans P, et al. "Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes." N Engl J Med 367.7 (2012): 606-615. [CrossRef]
- Wierda WG, et al. "Ofatumumab as single-agent CD20 immunotherapy in fludarabine-refractory chronic lymphocytic leukemia." J Clin Oncol 28.10 (2010): 1749-1755. [CrossRef]
- Papp, K. A., Reich, K., Paul, C., Blauvelt, A., Baran, W., Bolduc, C., ... & Crowley, J. (2016). A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology, 175(2), 273-286.
- Wasserstein MP, et al. "Olipudase alfa for treatment of acid sphingomyelinase deficiency (ASMD): safety and efficacy in adults treated for 30 months." J Inherit Metab Dis 41.5 (2018): 829-838. [CrossRef]
- Holgate, S. T., Chuchalin, A. G., Hébert, J., Lötvall, J., Persson, G. B., Chung, K. F., ... & Bousquet, J. (2004). Efficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clinical and Experimental Allergy, 34(4), 632-638. [CrossRef]
- Dinney CP, et al. "Intravesical valrubicin in patients with bladder carcinoma in situ and contraindication to or failure after bacillus Calmette-Guérin." Urol Oncol 24.4 (2006): 298-302. [CrossRef]
- Basser RL, et al. "Oprelvekin for chemotherapy-induced thrombocytopenia." N Engl J Med 344.17 (2001): 1263-1269.
- Gimpl G, Fahrenholz F. "The oxytocin receptor system: structure, function, and regulation." Physiol Rev 81.2 (2001): 629-683.
- Spielberger R, et al. "Palifermin for oral mucositis after intensive therapy for hematologic cancers." N Engl J Med 351.25 (2004): 2590-2598. [CrossRef]
- Johnson, S., Oliver, C., Prince, G. A., Hemming, V. G., Pfarr, D. S., Wang, S. C., ... & Groothuis, J. R. (1997). Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus. Journal of Infectious Diseases, 176(5), 1215-1224. [CrossRef]
- Whitcomb DC, Lehman GA, Vasileva G, et al. "Pancrelipase delayed-release capsules (CREON) for exocrine pancreatic insufficiency due to chronic pancreatitis or pancreatic surgery: A double-blind randomized trial." Am J Gastroenterol 105.10 (2010): 2276-2286. [CrossRef]
- Douillard, J. Y., Oliner, K. S., Siena, S., Tabernero, J., Burkes, R., Barugel, M., ... & Rivera, F. (2013). Panitumumab–FOLFOX4 treatment and RAS mutations in colorectal cancer. New England Journal of Medicine, 369(11), 1023-1034.
- Neer RM, et al. "Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis." N Engl J Med 344.19 (2001): 1434-1441. [CrossRef]
- Hirschhorn R, et al. "Restoration of immune function in adenosine deaminase deficiency by enzyme replacement or gene therapy." Mol Genet Metab 68.2 (1999): 220-231.
- Avramis VI, Sencer S, Periclou AP, et al. "A randomized comparison of native Escherichia coli asparaginase and polyethylene glycol conjugated asparaginase for treatment of children with newly diagnosed standard-risk acute lymphoblastic leukemia: a Children's Cancer Group study." Blood 99.6 (2002): 1986-1994.
- Dmytrijuk A, et al. "FDA Approval Summary: Eculizumab for the Treatment of Patients with Paroxysmal Nocturnal Hemoglobinuria." The Oncologist 13.9 (2008): 993-1000. Note: This is a citation for a similar mechanism as the drug eculizumab, which also targets complement inhibition.
- Manns MP, et al. "Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial." Lancet 358.9286 (2001): 958-965. [CrossRef]
- Fried MW, et al. "Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection." N Engl J Med 347.13 (2002): 975-982. [CrossRef]
- Sundy JS, et al. "Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment: two randomized controlled trials." JAMA 306.7 (2011): 711-720.
- Trainer PJ, et al. "Treatment of acromegaly with the growth hormone–receptor antagonist pegvisomant." N Engl J Med 342.16 (2000): 1171-. [CrossRef]
- Le, D. T., Uram, J. N., Wang, H., Bartlett, B. R., Kemberling, H., Eyring, A. D., ... & Azad, N. S. (2015). PD-1 blockade in tumors with mismatch-repair deficiency. New England Journal of Medicine, 372(26), 2509-2520. [CrossRef]
- Baselga, J., Cortés, J., Kim, S. B., Im, S. A., Hegg, R., Im, Y. H., ... & Clark, E. (2012). Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. New England Journal of Medicine, 366(2), 109-119. [CrossRef]
- Baselga J, et al. "Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer." N Engl J Med 366.2 (2012): 109-119. [CrossRef]
- Ratner RE, et al. "Adjunctive therapy with pramlintide lowers HbA1c without concomitant weight gain and increased risk of severe hypoglycemia in patients with type 1 diabetes approaching glycemic targets." Endocr Pract 11.5 (2005): 323-329. [CrossRef]
- Marlar RA, et al. "Protein S abnormalities: a diagnostic nightmare." Am J Hematol 29.2 (1988): 108-114. [CrossRef]
- Fuchs CS, et al. "Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial." Lancet 383.9911 (2014): 31-39.
- Rosenfeld, P. J., Brown, D. M., Heier, J. S., Boyer, D. S., Kaiser, P. K., Chung, C. Y., & Kim, R. Y. (2006). Ranibizumab for neovascular age-related macular degeneration. New England Journal of Medicine, 355(14), 1419-1431.
- Pui CH, et al. "Recombinant urate oxidase for the prophylaxis or treatment of hyperuricemia in patients with leukemia or lymphoma." J Clin Oncol 19.3 (2001): 697-704. [CrossRef]
- Cannon CP, et al. "Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban." N Engl J Med 344.25 (2001): 1879-1887. [CrossRef]
- Hoffman HM, et al. "Rilonacept for gout flare prevention in patients receiving uric acid-lowering therapy: results of RESURGE, a phase III, international safety study." J Rheumatol 40.8 (2013): 1452-1461.
- Maloney, D. G., Grillo-López, A. J., White, C. A., Bodkin, D., Schilder, R. J., Neidhart, J. A., ... & Levy, R. (1997). IDEC-C2B8 (Rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed low-grade non-Hodgkin’s lymphoma. Blood, 90(6), 2188-2195.
- Bussel JB, et al. "Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura." N Engl J Med 357.22 (2007): 2237-2247. [CrossRef]
- Cosman, F., Crittenden, D. B., Adachi, J. D., Binkley, N., Czerwinski, E., Ferrari, S., ... & Törring, O. (2016). Romosozumab treatment in postmenopausal women with osteoporosis. New England Journal of Medicine, 375(16), 1532-1543. [CrossRef]
- Treem WR, et al. "Sacrosidase therapy for congenital sucrase-isomaltase deficiency." J Pediatr Gastroenterol Nutr 26.5 (1998): 506-512.
- Nemunaitis J, et al. "Recombinant granulocyte-macrophage colony-stimulating factor after autologous bone marrow transplantation for lymphoid cancer." N Engl J Med 324.25 (1991): 1773-1778. [CrossRef]
- Genovese, M. C., Fleischmann, R., Kivitz, A. J., Rell-Bakalarska, M., Martincova, R., Fiore, S., ... & van Adelsberg, J. (2015). Sarilumab plus methotrexate in patients with active rheumatoid arthritis and inadequate response to methotrexate: results of a phase III study. Arthritis & Rheumatology, 67(6), 1424-1437. [CrossRef]
- Burton BK, et al. "A phase 3 trial of sebelipase alfa in lysosomal acid lipase deficiency." N Engl J Med 373.11 (2015): 1010-1020. [CrossRef]
- Willems G, et al. "Effects of secretin on gastric emptying and small bowel transit in man." Dig Dis Sci 28.8 (1983): 705-709.
- Langley, R. G., Elewski, B. E., Lebwohl, M., Reich, K., Griffiths, C. E., Papp, K., ... & Ho, V. (2014). Secukinumab in plaque psoriasis—results of two phase 3 trials. New England Journal of Medicine, 371(4), 326-338. [CrossRef]
- Bowers CY, et al. "Clinical review 1: Sermorelin: a better approach to management of adult-onset growth hormone insufficiency?." J Clin Endocrinol Metab 87.12 (2002): 5468-5473.
- Kurzrock R, et al. "A phase I study of siltuximab, an anti-interleukin-6 monoclonal antibody, in patients with B-cell non-Hodgkin lymphoma, multiple myeloma, or Castleman disease." Clin Cancer Res 19.13 (2013): 3659-3670.
- Rudman D, et al. "Effects of human growth hormone in men over 60 years old." N Engl J Med 323.1 (1990): 1-6. [CrossRef]
- Yusuf S, et al. "Intravenous and intracoronary fibrinolytic therapy in acute myocardial infarction: overview of results on mortality, reinfarction and side-effects from 33 randomized controlled trials." Eur Heart J 6.7 (1985): 556-585.
- Pemmaraju N, et al. "Tagraxofusp in blastic plasmacytoid dendritic-cell neoplasm." N Engl J Med 380.17 (2019): 1628-1637. [CrossRef]
- Pastores GM, et al. "A phase 3, multicenter, open-label, switchover trial to assess the safety and efficacy of taliglucerase alfa, a plant cell-expressed recombinant human glucocerebrosidase, in adult and pediatric patients with Gaucher disease previously treated with imiglucerase." Blood 120.15 (2012): 2901-2909. [CrossRef]
- Jeppesen PB, et al. "Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure." Gastroenterology 143.6 (2012): 1473-1481.e3. [CrossRef]
- Van De Werf F, et al. "Assessment of the safety and efficacy of a new thrombolytic (Alteplase) in acute myocardial infarction." N Engl.
- Neer RM, et al. "Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis." N Engl J Med 344.19 (2001): 1434-1441. [CrossRef]
- Moreau R, et al. "Terlipressin in patients with cirrhosis and type 1 hepatorenal syndrome: a retrospective multicenter study." Gastroenterology 134.4 (2008): 923-930. [CrossRef]
- Falutz J, et al. "Efficacy of tesamorelin, a growth hormone-releasing factor analogue, in HIV-infected patients with abdominal fat accumulation: a randomized, placebo-controlled trial." J Acquir Immune Defic Syndr 52.3 (2009): 328. [CrossRef]
- Zhou YX, et al. "Randomized, placebo-controlled, double-blind phase III trial of thymalfasin in combination with transcatheter arterial chemoembolization in patients with unresectable primary liver cancer." J Natl Cancer Inst 107.1 (2015): 363.
- Haugen BR, et al. "American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer." Thyroid 26.1 (2016): 1-133.
- Coskun T, et al. "LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: From discovery to clinical proof of concept." Mol Metab 18 (2018): 3-14. [CrossRef]
- Bendell JC, et al. "Clinical activity and safety of tisotumab vedotin, a tissue factor–targeting antibody–drug conjugate, in patients with platinum-resistant ovarian cancer in the phase II innovaTV 204/GOG-3023/ENGOT-ov44 study." J Clin Oncol 39.15 (2021): 3351-3359.
- Nishimoto N, et al. "Mechanisms and pathologic significances in increase in serum interleukin-6 (IL-6) and soluble IL-6 receptor after administration of an anti–IL-6 receptor antibody, tocilizumab, in patients with rheumatoid arthritis and Castleman disease." Blood 112.10 (2008): 3959-3964.
- Kaminski MS, et al. "Radioimmunotherapy of B-cell lymphoma with [131I] tositumomab." N Engl J Med 346.24 (2002): 1865-1876.
- Hudis, C. A. (2007). Trastuzumab—mechanism of action and use in clinical practice. New England Journal of Medicine, 357(1), 39-51. [CrossRef]
- Bergh C, et al. "Monofollicular ovulation induction in previously anovulatory women: a comparative study between purified urinary FSH and purified urinary FSH/FSH depot." Hum Reprod 12.10 (1997): 2132-2137.
- Goldhaber SZ, et al. "A randomized controlled trial of recombinant human tissue plasminogen activator versus urokinase in the treatment of acute pulmonary embolism." Lancet 328.8500 (1986): 293-298.
- Krueger, J.G., Ferris, L.K., Menter, A., Wagner, F., White, A., Visvanathan, S., ... & Rolleri, R.L. (2017). Anti–IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: Safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. The Journal of Allergy and Clinical Immunology, 140(1), 172-182.
- Russell JA, et al. "Vasopressin versus norepinephrine infusion in patients with septic shock." N Engl J Med 358.9 (2008): 877-887. [CrossRef]
- Feagan, B. G., Rutgeerts, P., Sands, B. E., Hanauer, S., Colombel, J. F., Sandborn, W. J., ... & Maroney, A. C. (2013). Vedolizumab as induction and maintenance therapy for ulcerative colitis. New England Journal of Medicine, 369(8), 699-710. [CrossRef]
- Pastores GM, et al. "A multicenter, open-label extension trial of velaglucerase alfa in Gaucher disease type 1: 48-month experience." Am J Hematol 88.6 (2013): 537-543.
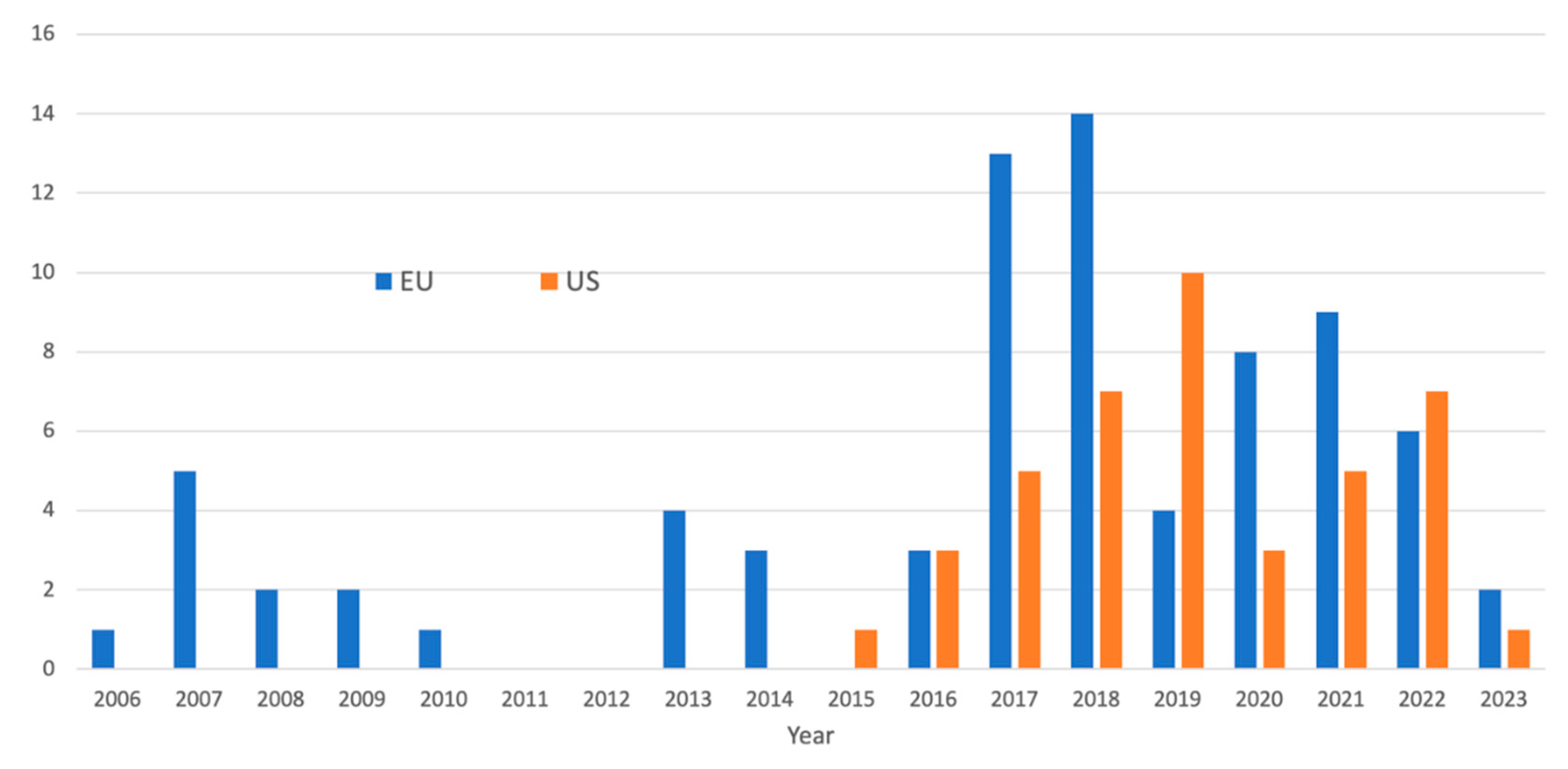

| Function | Usage | Example |
|---|---|---|
| Demonstrate Drug Activity | Early evidence of a drug's effect before overt clinical outcomes manifest. | In treating chronic myeloid leukemia (CML), the BCR-ABL tyrosine kinase inhibitor imatinib is used. The decline in BCR-ABL transcript levels in patients' blood is a functional PD marker of the drug's activity on its target.[34] |
| Guide Dosing | Dose-response relationship, ensuring optimal drug dosing. | For cholesterol-lowering drugs like statins, the low-density lipoprotein cholesterol (LDL-C) levels in the blood serve as a PD marker to guide dosing and assess efficacy.[35] |
| Select Patients | To identify patients likely to benefit from a specific treatment. | In some breast cancers, overexpression of the HER2 protein is observed. HER2 status serves as a functional PD marker to select patients who might benefit from trastuzumab, which targets HER2.[36] |
| Monitor Resistance | Track the development of resistance to treatments. | In HIV treatment, the emergence of specific viral mutations can serve as PD markers indicating resistance to certain antiretroviral drugs.[37] |
| Determine Drug Mechanism of Action | Confirmation of action through its intended mechanism. | In Alzheimer’s disease, the buildup of beta-amyloid plaques is considered a hallmark. Drugs designed to reduce beta-amyloid levels in the brain might use CSF (cerebrospinal fluid) levels of beta-amyloid as a PD marker to show the drug's effect.[38] |
| Validate Target Engagement | Demonstrate that a drug is successfully engaging with and modulating its target. | For multiple sclerosis drugs like fingolimod, a PD marker such as the number of circulating lymphocytes can indicate the drug's effect on immune cell egress from lymph nodes.[39] |
| Evaluate Drug-induced Toxicity | Monitor potential adverse effects of a drug. | In chemotherapy, monitoring the levels of liver enzymes like AST and ALT in the blood can serve as PD markers for drug-induced liver damage.[40] |
| Optimize Therapeutic Window | Establish the range between the minimum effective dose and the onset of adverse effects. | For anticoagulant drugs like warfarin, the INR (International Normalized Ratio) serves as a PD marker to ensure the drug's effect is within a therapeutic range that minimizes the risk of bleeding and clot formation.[41] |
| Predict Long-term Drug Effects | Early changes in PD markers can predict longer-term therapeutic or adverse effects. | In osteoporosis treatments, reducing bone resorption markers like CTX (C-terminal telopeptide) can predict longer-term benefits in bone mineral density and fracture risk.[42] |
| Assess Immune Response | For immunotherapies, to gauge the body's immune response to the treatment. | In cancer immunotherapy, the presence and proliferation of tumor-infiltrating lymphocytes (TILs) in the tumor microenvironment can serve as a PD marker to indicate the activation and targeting of the immune system against tumor cells.[43] |
| Indicate Drug Combination Efficacy | In combination therapies, to show the synergistic or additive effects of the combined drugs. | In treatments for tuberculosis, monitoring bacterial load in sputum samples can serve as a PD marker for the combined efficacy of multiple antimicrobial agents.[44] |
| Track Reversal of Disease Progression | Indicate whether a drug is not just halting but reversing disease progression. | In fibrotic diseases like idiopathic pulmonary fibrosis, measuring levels of collagen-derived peptides in blood or bronchoalveolar lavage fluid can act as PD markers, indicating the repair or degradation of fibrotic tissue.[45] |
| Evaluate Neural Activity and Plasticity | PD markers can track neural activity or connection changes in neurologic disorders and treatments. | For treatments aimed at Alzheimer's or other neurodegenerative conditions, the levels of synaptic proteins or neuronal activity markers in CSF can indicate neural activity and synaptic plasticity.[46] |
| Monitoring Metabolic Responses | To help track changes in metabolic pathways. | In diabetes management, measuring C-peptide levels alongside insulin can give insights into endogenous insulin production and pancreatic function.[47] |
| Monitoring Cellular Senescence and Aging | In treatments aiming to affect aging processes or cellular health, to track cellular senescence. | Measuring levels of senescence-associated beta-galactosidase or p16^INK4a expression can act as PD markers for cellular aging or the efficacy of anti-aging treatments.[48] |
| Evaluating Epigenetic Changes | Track changes in DNA methylation, histone modification, or other epigenetic markers. | In oncology, when treating with drugs targeting DNA methyltransferases, the global or gene-specific changes in DNA methylation levels can serve as PD markers.[49] |
| Assessing Drug-induced Autophagy | For therapies inducing autophagy as a mechanism, to monitor the process. | Monitoring LC3B lipidation, a critical step in autophagosome formation, can serve as a PD marker for autophagy activation.[50] |
| Monitoring Immune Checkpoint Inhibition | Cancer immunotherapy targets immune checkpoints to gauge the effectiveness of checkpoint inhibition. | In patients receiving PD-1 or PD-L1 inhibitors, monitoring circulating tumor DNA (ctDNA) levels can serve as a PD marker to indicate response to therapy.[51] |
| Test Method | Application |
| Mass Spectrometry (MS) | Structural analysis of glycan [102] |
| High-Performance Liquid Chromatography (HPLC) | Separation of glycan structures - [103] |
| Capillary Electrophoresis (CE) | High-resolution separation of glycans - [104] |
| NMR Spectroscopy | Detailed structural analysis of glycan[105] |
| Matrix-assisted laser desorption/ionization (MALDI-MS) | Mass determination of glycan[106] |
| Glycan Microarrays | High-throughput analysis of protein-glycan interactions[107] |
| Lectin Affinity Chromatography | Separation of glycans using specific binding proteins[108] |
| FTIR | Analysis of glycan structure[109] |
| Enzyme-linked Lectin Assay | Quantitative glycan analysis[110] |
| Exoglycosidase Sequencing | Structural characterization of glycans[111] |
| Stable Isotope Labeling | Quantitative glycomics[112] |
| SPR | Real-time glycan-protein interaction analysis[113] |
| Gas Chromatography-Mass Spectrometry | Analysis of volatile derivatives of glycans[114] |
| Tandem Mass Spectrometry | Sequential fragmentation for glycan structure elucidation[115] |
| Hydrophilic Interaction Liquid Chromatography | Separation of polar glycans[116] |
| Fluorescence Detection | Sensitivity enhancement in glycan analysis[117] |
| ELISA | Detection of specific glycan-protein interactions[118] |
| MALS | Characterizing size and composition[119] |
| Immunohistochemistry | Localization of specific glycans in tissues[120] |
| IEF | Separation of glycoproteins by isoelectric point[121] |
| Reverse Phase Liquid Chromatography | Separation of glycopeptides and glycoproteins[122] |
| Glycoproteomic Analysis | Integrative approach for comprehensive glycoprotein study[123] |
| Electron Microscopy | Visualizing glycan structures and localization[124] |
| Optical Glycan Biosensors | Real-time monitoring of glycan-protein interactions[125] |
| X-ray Crystallography | 3D structure determination of glycoproteins[126] |
| DLS | Size distribution analysis of glycoproteins[127] |
| Glycan Sequencing using Edman Degradation | Sequential identification[128] |
| Bottom-up MS | Mass spectrometric analysis for primary sequence analysis, evaluation of N/O-glycosylation sites, and quantification of methionine oxidation.[129] |
| Bioanalytical and bioinformatics | Data integration at different structural levels to identify various glycoforms of recombinant Human Chorionic Gonadotropin (r-hCG), urinary hCG (u-hCG), and recombinant Follicle Stimulating Hormone (r-hFSH) revealed that these biopharmaceuticals differ considerably in their glycosylation patterns.[130] |
| Resolution Discrepancies | Between high-resolution native and glycopeptide-centric mass spectrometric approaches for the glycosylation of erythropoietin variants.[131] |
| Glycan microheterogeneity | To identify multiple glycosylation sites in the vascular endothelial growth factor IgG (VEGFR-IgG) fusion protein to understand the functional significance of each glycosylation pattern.[132] |
| Glycoforms | Several glycoforms using hybrid high-performance liquid chromatography-MS approaches.[133], such as 24 glycoengineered erythropoietin variants with varying glycan branching and sialylation levels, which are crucial parameters for biotherapeutic efficacy. |
| NMR | Identification of glucose-induced glycation in mAbs and other proteins using NMR spectroscopy. [134] |
| Novel glycoforms | Identification of novel glycosylations in human serum-derived factor IX. [135] |
| Mass spectral profiling | The N-linked, O-linked, ganglioside, and glycosaminoglycan compound classes and the tandem mass spectrometry of glycans have led to spectral glycoproteomics.[136] |
| N-glycosylation profile | Analysis of trastuzumab biosimilar candidates using normal-phase liquid chromatography and matrix-assisted laser desorption/ionization-time of flight-MS.[137] |
| Microheterogeneity | Composite glycosylation profiles and other microheterogeneities in intact mAbs via high-resolution native MS using a modified Orbitrap.[138] |
| Targeted site-specific quantitation | N-and O-glycopeptides using 18O-labeling and product ion-based MS.[139] |
| Hybrid MS | Approaches in glycoprotein analysis and their usage in scoring biosimilarity.[140] |
| Gene Expression Profiling | Simultaneous measurement of the expression levels of several genes to create a global picture of cellular functions. |
| Non-coding RNA Analysis | Identifying non-coding RNAs. |
| Alternative Splicing | Events wherein exons of a gene are joined in multiple ways during protein synthesis, thus producing numerous proteins from a single gene. |
| Disease Diagnosis and Treatment | Disease diagnosis, prognosis, and determining the treatment response. |
| Optimization of Host Cells for Protein Expression | Optimize host cells to improve recombinant protein expression.[143] |
| Identifying Suitable Expression Systems | Selection of optimal expression system.[144] |
| Understanding protein function and interactions | How proteins function and interact within cellular networks.[145] |
| Monitoring Quality Control in Biopharmaceutical Production | Manufacturing QC.[146] |
| Improving Protein Solubility and Folding | Enhance the solubility and folding of recombinant.[147] |
| Tailoring Protein Post-Translational Modifications (PTMs) | To produce proteins with the desired PTMs.[148] |
| Enhanced Yield in Industrial Protein Production | To enhance the yield of recombinant proteins for industrial applications.[149] |
| Studying Protein Stability and Degradation | Design recombinant proteins with enhanced stability.[150] |
| Personalized Medicine and Therapeutics | Patient-specific proteins based on individual gene expression profiles.[151] |
| Improving Expression Systems | Researchers can optimize expression systems for recombinant protein production by studying host cell genomes.[161] |
| Designing Recombinant Proteins | Genomics can be used to identify and design recombinant proteins with the desired functions.[162] |
| Enhancing Protein Stability | Understanding the genomic context can aid in designing recombinant proteins with enhanced stability and activity.[163] |
| Personalized Medicine | Personalized genomics allows the development of recombinant proteins tailored to the genetic profiles of individual patients.[164] |
| Metabolic Engineering | Genomic insights can guide the redesign of metabolic pathways to produce recombinant proteins in microbial systems efficiently.[165] |
| Biomarker Discovery | Genomics aids in the identification of biomarkers that can be targeted with recombinant proteins for diagnostic or therapeutic purposes.[166] |
| Understanding Protein Function | Comparative genomics can elucidate the functions of proteins by identifying conserved sequences and structures.[167] |
| Enhanced Protein Folding | Genomic data can be used to understand and improve the folding of recombinant proteins.[168] |
| Development of Novel Therapeutics | Genomics is used to identify potential targets of therapeutic recombinant proteins.[169] |
| Cell Line Optimization | Cell line optimization results from (i) research applied to parental, non-recombinant cell lines; (ii) systems-level datasets generated with recombinant cell lines; (iii) datasets linking phenotypic traits to relevant biomarkers; (iv) data depositories and bioinformatics tools; and (v) in silico model development.[170] |
| Optimization of Expression Systems | Understanding and manipulating epigenetic markers can enhance recombinant proteins' expression in host cells.[174] |
| Production of Recombinant Proteins with Specific Modifications | Epigenomic control enables the production of recombinant proteins with functionally essential PTMs.[175] |
| Development of recombinant proteins for epigenetically targeted therapies | Epigenomics guides the discovery and development of recombinant proteins that target specific epigenetic modifications involved in various diseases.[176] |
| Studying the Epigenetic Control of Protein Function | Recombinant proteins can be used to study how epigenetic modifications regulate endogenous proteins, providing insights into their functions and control.[177] |
| Recombinant Epigenetic Modifiers for Research | Producing recombinant proteins involved in epigenetic modifications, such as methyltransferases, may be helpful for research and drug development.[178] |
| Modeling Diseases | Using epigenomic information for modifying host cells to produce recombinant proteins allows the creation of more accurate disease models, particularly for conditions in which epigenetic alterations play a crucial role.[179] |
| Quality Control and Stability of Biopharmaceuticals | Epigenomic control may improve the quality and stability of recombinant proteins for biopharmaceutical applications.[180] |
| The Optimization of Expression Systems for Protein Production | MS and NMR.[184] |
| Improving Industrial Protein Production Yields | Liquid Chromatography-Mass Spectrometry.[185] |
| Understanding Host-Pathogen Interactions for Recombinant Vaccine Development | Gas Chromatography-Mass Spectrometry.[186] |
| Investigating Protein-Metabolite Interactions | NMR Spectroscopy.[187] |
| Quality Control and Stability of Recombinant Proteins in Biopharmaceuticals | Capillary Electrophoresis-Mass Spectrometry.[188] |
| Assessing the impact of protein therapeutics on metabolic pathways | Using ultra-performance liquid chromatography-mass spectrometry.[189] |
| Designing More Effective Protein-Based Therapies Through Metabolite Profiling | Fourier Transform Mass Spectrometry.[190] |
| Environmental Stress Response in Recombinant Protein Production | Liquid Chromatography-Quadrupole Time-of-Flight Mass Spectrometry.[191] |
| Immune response against tumor cells in patients with melanoma | increases in absolute lymphocyte counts are observed in response to therapy and can serve as a marker of functional immune response[192]. |
| Lab Values Alteration | Changes in specific laboratory values can serve as functional response markers for certain conditions. For example, in patients with rheumatoid arthritis treated with the anti-TNFα mAb, adalimumab, reductions in serum C-reactive protein levels and erythrocyte sedimentation rate, which are markers of inflammation, indicate a positive response to therapy[193]. |
| Modulation of T-cell Response | Some mAbs, particularly immune checkpoint inhibitors such as pembrolizumab, function by modulating the T-cell response, which can be measured using T-cell activation markers, such as CD137, or by enumerating antigen-specific T-cells.[194] |
| Alteration in Serum Immunoglobulin Levels | Some mAbs can cause changes in the serum levels of immunoglobulins, which can serve as PD markers. Rituximab, an anti-CD20 mAb, decreases serum immunoglobulin levels, which can be monitored clinically.[195] |
| PK and PD Correlation | The correlation between PK properties, such as serum drug concentration and PD markers, is a significant component of mAb engagement. This elucidates the dose-response relationship for adjusting the dosing regimens. For instance, with infliximab, an anti-TNFα mAb used in treating autoimmune diseases, measuring the serum drug concentration and correlating this with the clinical response and anti-TNFα activity can indicate effective drug-target engagement[196]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




