Submitted:
06 September 2023
Posted:
07 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
- a)
- patients with first ever attack of acute vertigo.
- b)
- patients who reported recurring vertigo and dizziness (present or not at the time of observation) for at least three episodes, both spontaneous and provoked (for example by movements of the head, change in body positions, physical efforts etc.).
- c)
- patients with chronic imbalance
3. Results
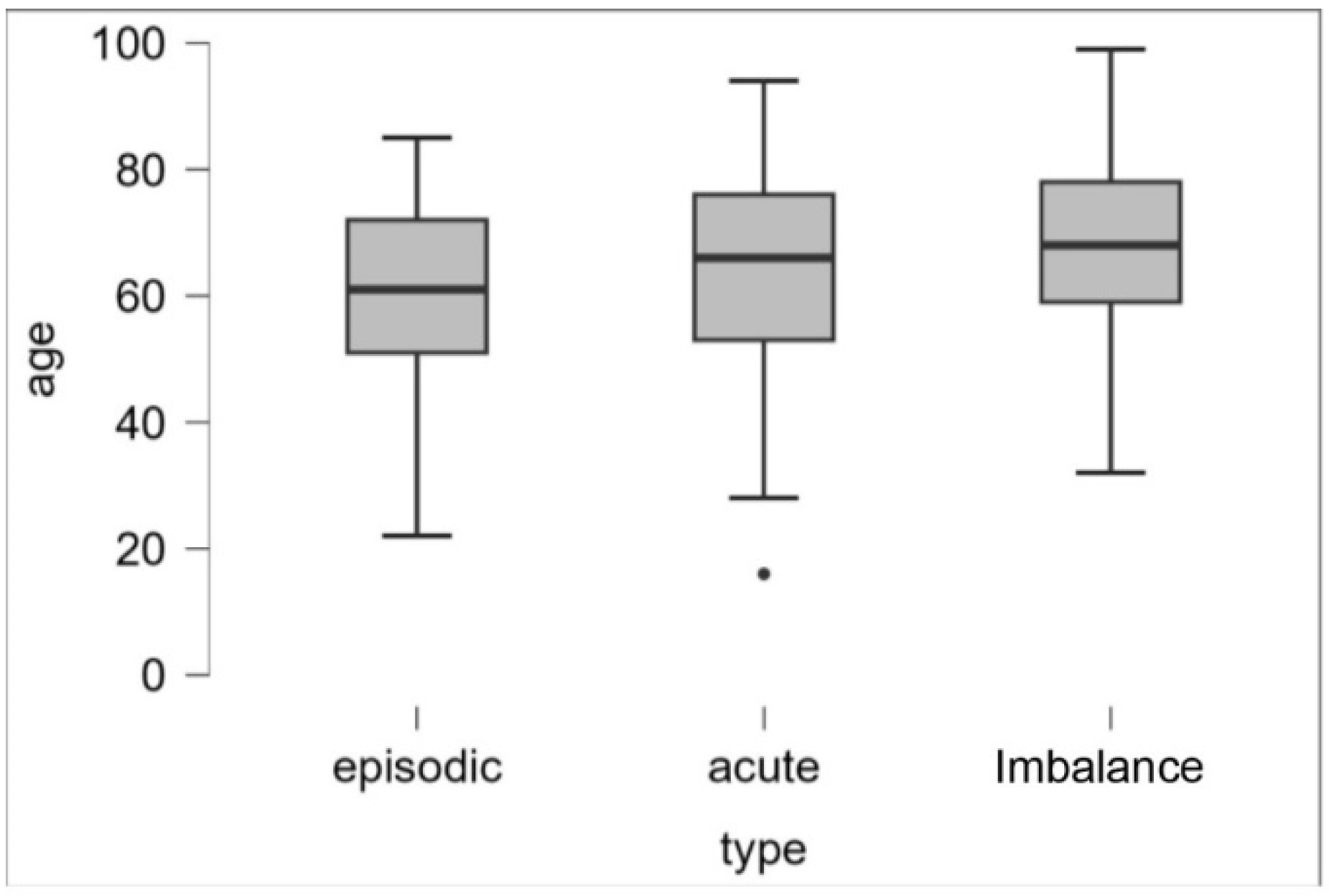
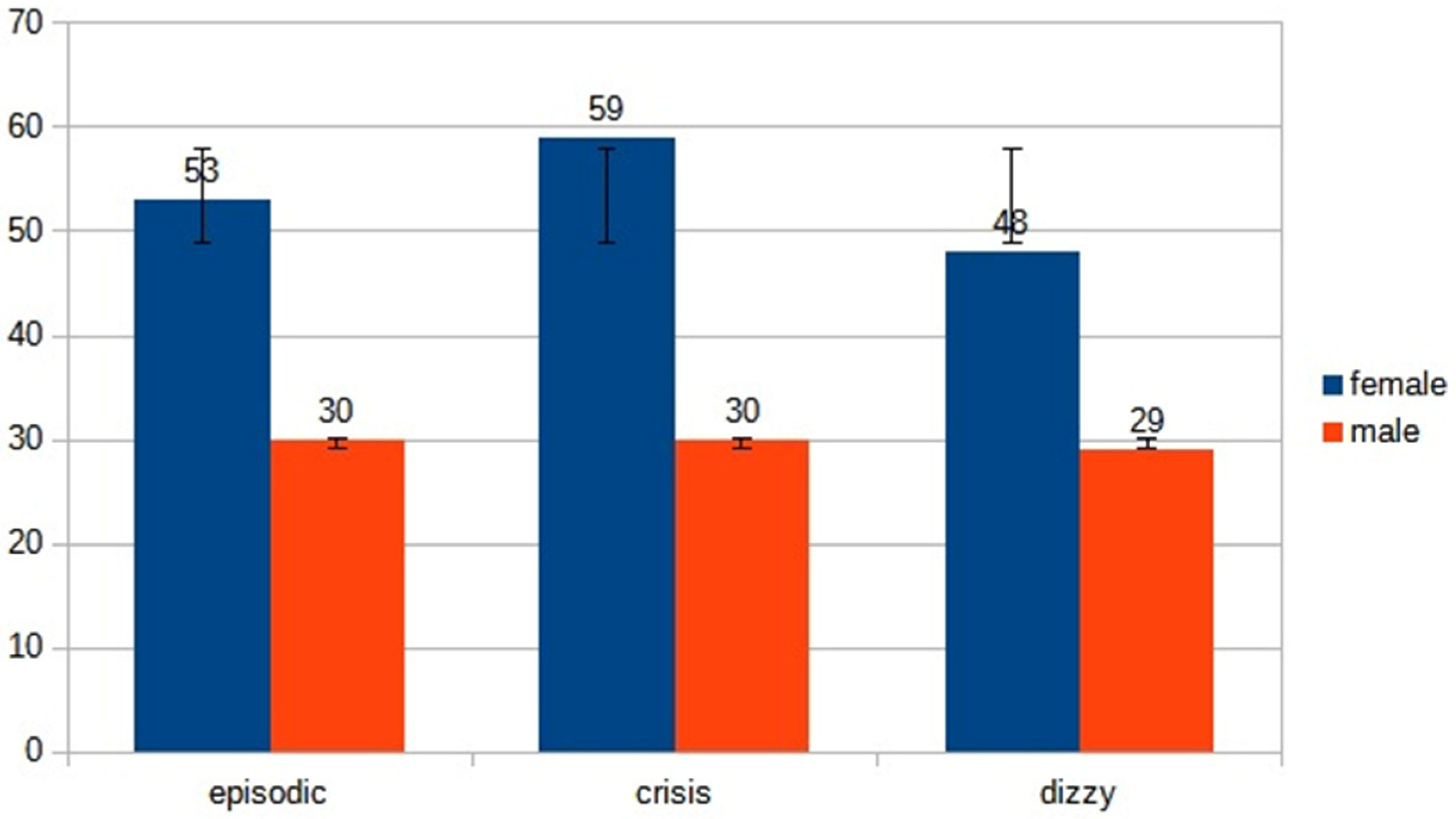
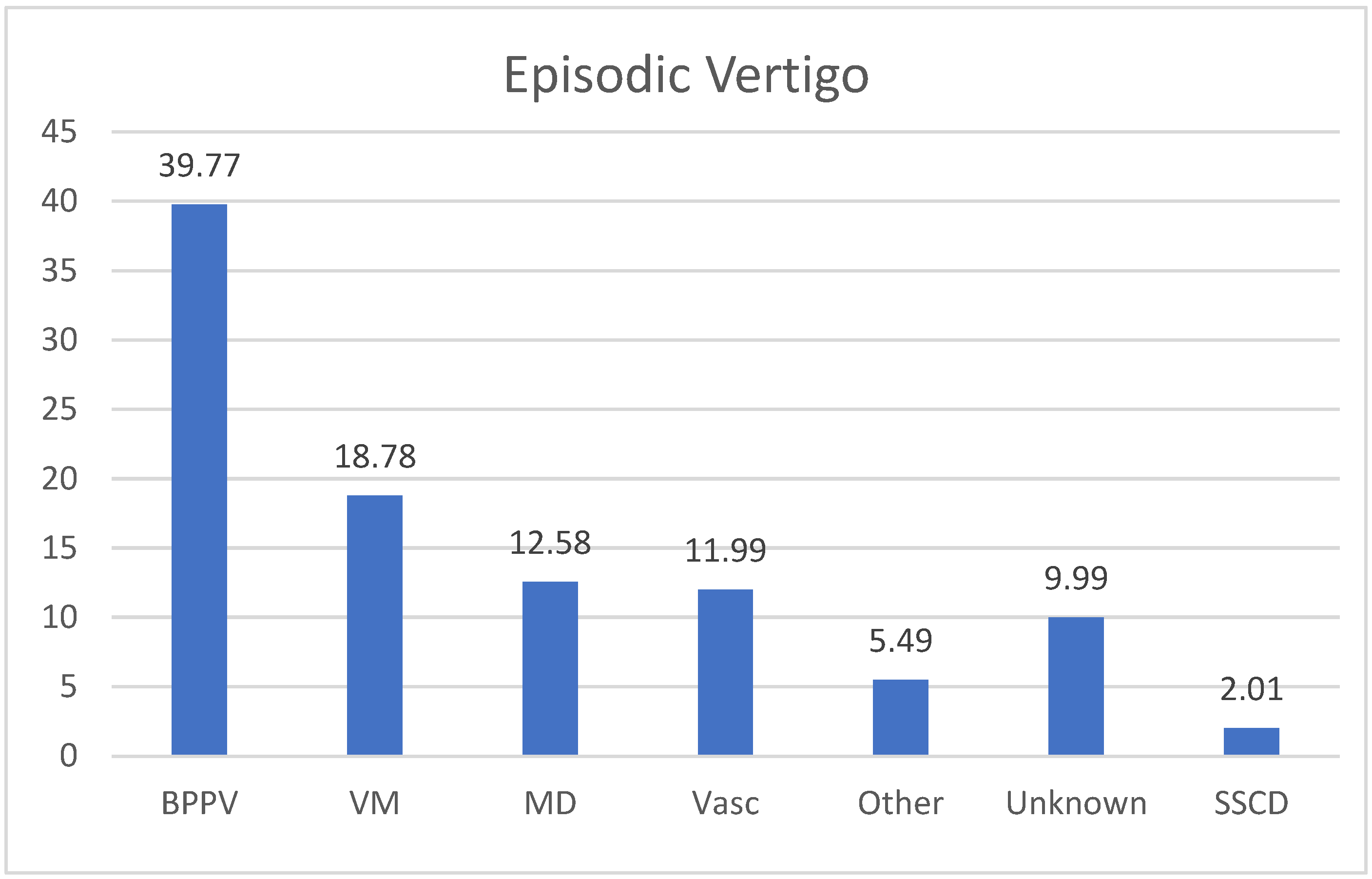
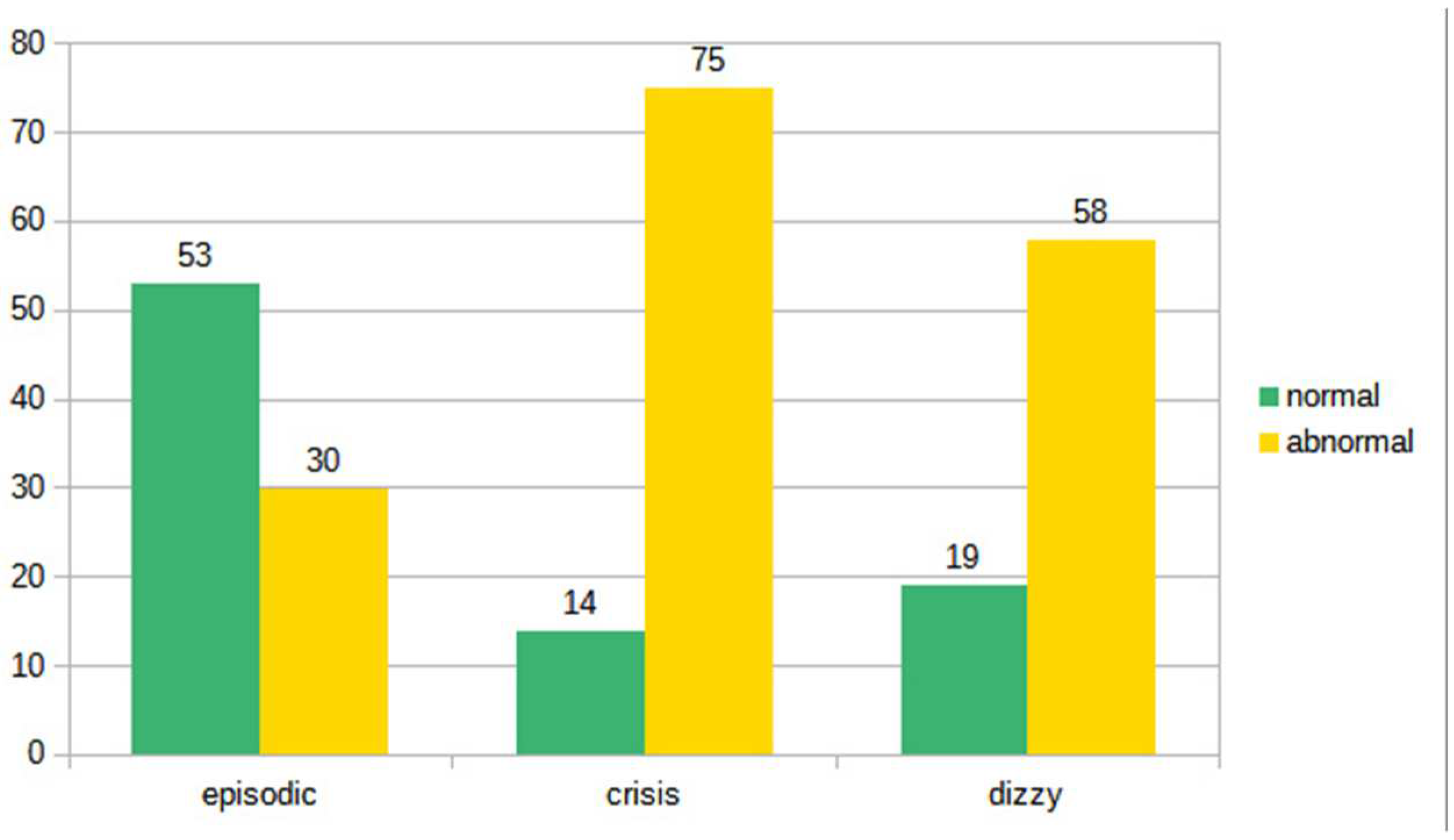
- 83 (53 males, 30 females, mean age ranging from 22 y to 85 y, mean 53,5 y) patients suffering from episodic vertigo and dizziness attacks.
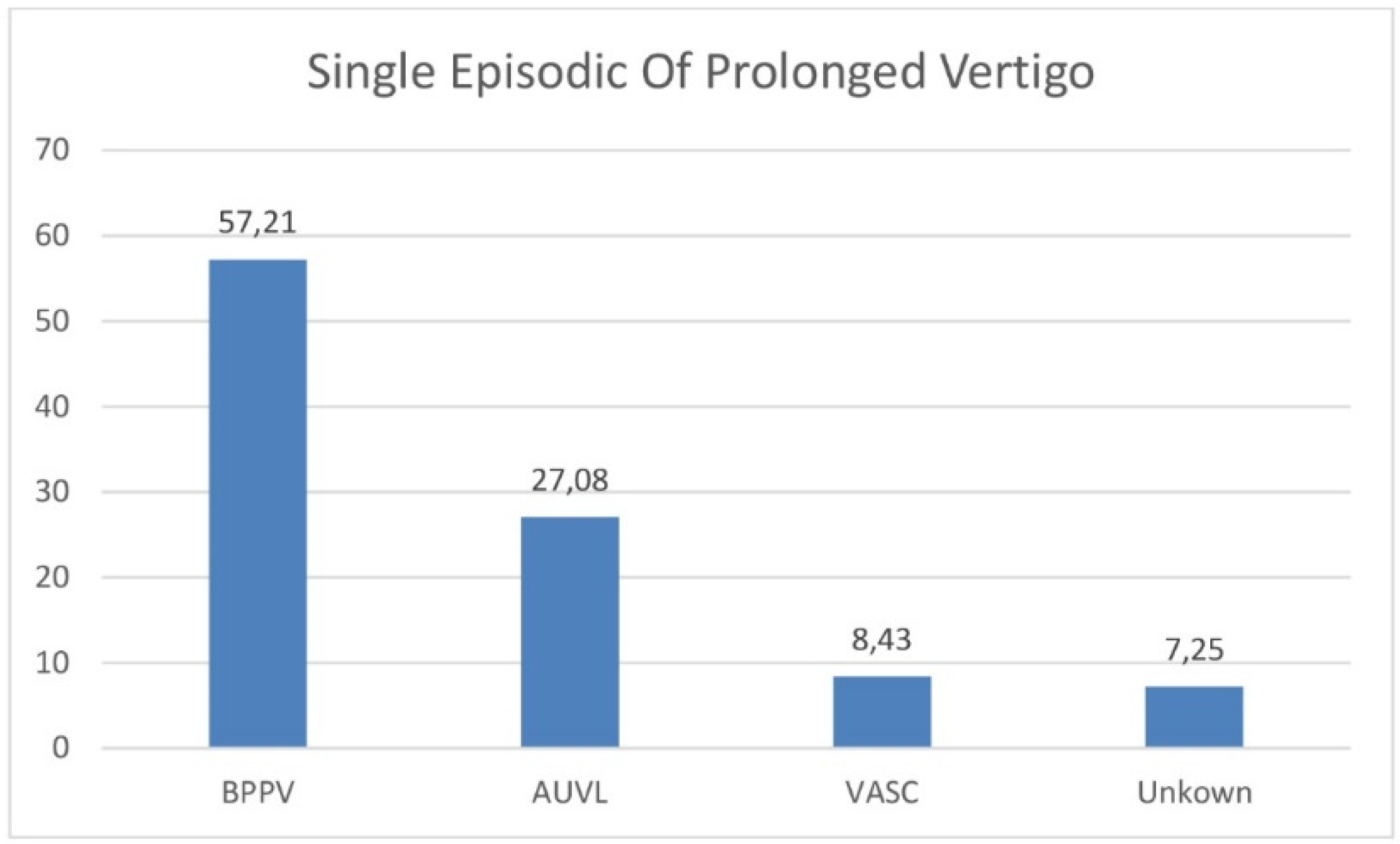
- 89 (59 males, 30 females, mean age ranging from 29 y to 92 y, mean 60,5 y) with a first-ever attack of acute vertigo.
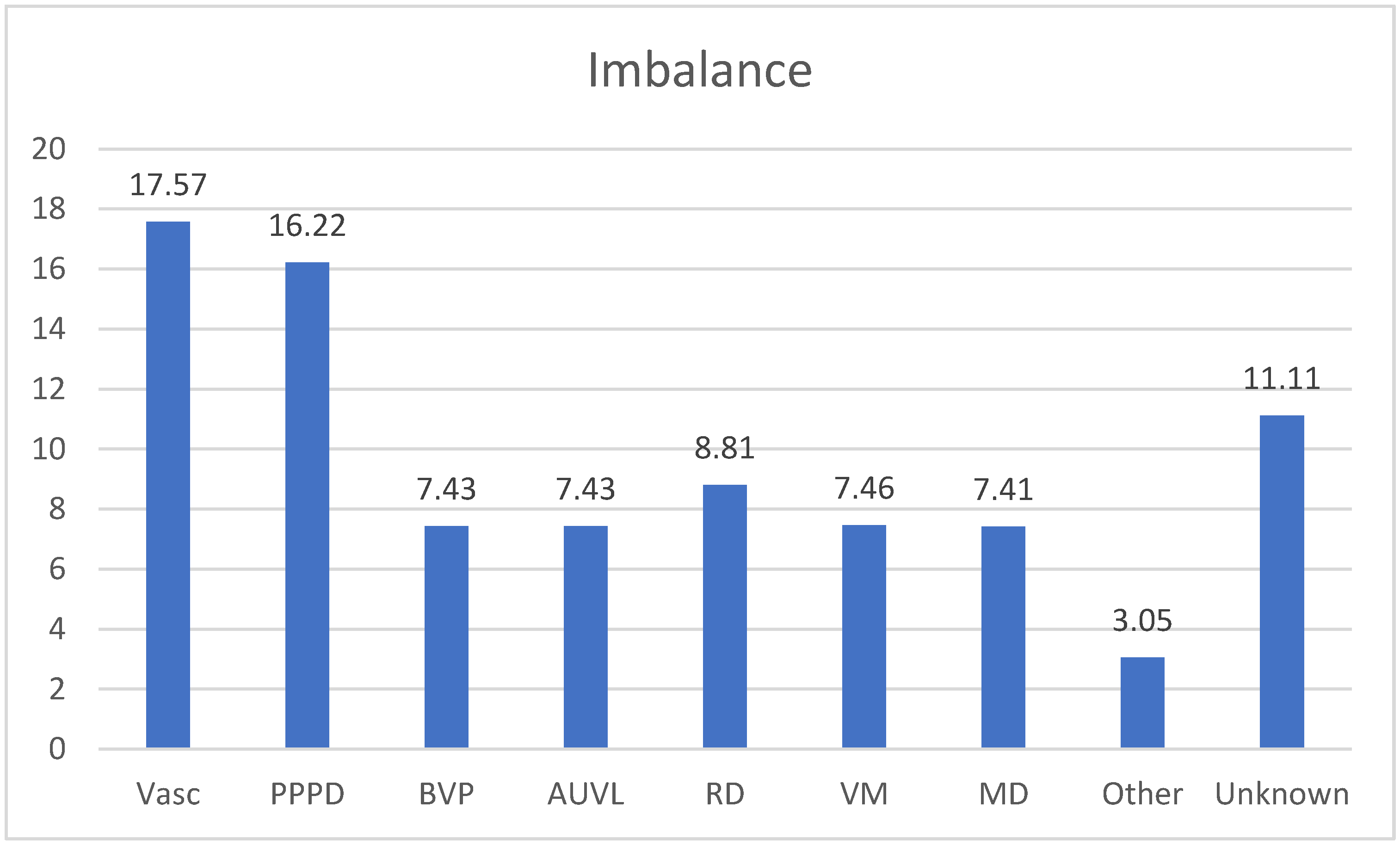
- 77 (48 males, 29 females, mean age ranging from 30 y to 99 y, mean 64,5 y) with imbalance.
4. Discussion
- 1)
- Benign paroxysmal positional vertigo.
- 2)
- Vestibular Migraine.
- 3)
- Menière’s disease.
- 4)
- Vertebrobasilar TIAs.
- 5)
- Orthostatic hypotension.
| Clinical factor | score | |
| Age 60 years or older | 1 | |
| BP ≥ 140/90 mm Hg | 1 | |
| Clinical: speech disturbance | 1 | |
| Clinical: unilateral weakness | 2 | |
| Duration < 10 minutes | 0 | |
| Duration 10 – 59 minutes | 1 | |
| Duration 10 – 59 min | 1 | |
| Diabetes | 1 |
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Welgampola, M.S.; Young, A.S.; Pogson, J.M.; Bradshaw, A.P.; Halmagyi, G.M. Dizziness demystified. Pract. Neurol. 2019, 19, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Cutfield, N.J.; Seemungal, B.M.; Millington, H.; Bronstein, A.M. Diagnosis of acute vertigo in the emergency department. J. Emerg. Med. 2011, 28, 9. [Google Scholar] [CrossRef] [PubMed]
- Kiran, A.; James, H.; Nishchay, M.; Fiona, H.; Diego, K. Acute vertigo: getting the diagnosis right. BMJ 2022, 378. [Google Scholar] [CrossRef]
- Nuti, D.; Zee, D.S.; Mandalà, M. Benign paroxysmal positional vertigo: what we do and do not know. Semin Neurol 2020, 40, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Peña Navarro, P.; Pacheco López, S.; Almeida Ayerve, C.N.; Marcos Alonso, S.; Serradilla López, J.M.; Santa Cruz Ruiz, S.; Gómez Sánchez, J.C.; Kaski, D.; Batuecas Caletrío, Á. Early Diagnosis of Central Disorders Mimicking Horizontal Canal Cupulolithiasis. Brain Sci. 2023, 13, 562. [Google Scholar] [CrossRef] [PubMed]
- Lempert, T. Recurrent spontaneous attacks of dizziness. CONTINUUM: Lifelong Learning in Neurol 2012, 18, 1086–1101. [Google Scholar] [CrossRef]
- Staab, J.P.; Eckhardt-Henn, A.; Horii, A.; Jacob, R.; Strupp, M.; Brandt, T.; Bronstein, A. Diagnostic criteria for persistent postural- perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Bárány Society. J. Vestib. Res. 2017, 27, 191–208. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Escamez, J.A.; Carey, J.; Chung, W.-H.; Goebel, J.A.; Magnusson, M.; Mandalà, M.; Newman-Toker, D.E.; Strupp, M.; Suzuki, M.; Trabalzini, F.; et al. Diagnostic criteria for Menière’s disease. J. Vestib. Res. 2015, 25, 1–7. [Google Scholar] [CrossRef]
- Lempert, T.; Olesen, J.; Furman, J.; Waterston, J.; Seemungal, B.; Carey, J.; Bisdorff, A.; Versino, M.; Evers, S.; Newman-Toker, D. Vestibular migraine: Diagnostic criteria. J. Vestib. Res. 2012, 22, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Von Brevern, M.; Bertholon, P.; Brandt, T.; Fife, T.; Imai, T.; Nuti, D.; Newman-Toker, D. Benign paroxysmal positional vertigo: Diagnostic criteria. Consensus document of the Committee for the Classification of Vestibular Disorders of the Barany Society. J. Vestib. Res. 2015, 25, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Bronstein, A.; Lempert, T. Dizziness. A practical approach to diagnosis and management. Cambridge University Press. J. Neurol. Neurosurg. Psychiatry 2007, 78, 779. [Google Scholar]
- Agrawal, Y.; Ward, B.K.; Minor, L.B. Vestibular dysfunction: prevalence, impact and need for targeted treatment. J. Vestib. Res. 2013, 23, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.S.; Simpson, K.N.; Johnson, J.M.; Rizk, H.G. Assessment of the Cost Burden of Episodic Recurrent Vestibular Vertigo in the US. JAMA Otol. Head & Neck Surg. 2022, 148, 1103–1110. [Google Scholar]
- Espinosa Sanchez, J.M.; Lopez-Escamez, J.A. Menière’s disease. In: Furman J, Lempert T, editors. Handbook of Clin. Neurol 2016, 137, 257–277. [Google Scholar]
- Seemungal, B.; Kaski, D.; Lopez-Escamez, J.A. Early diagnosis and management of acute vertigo from vestibular migraine and Ménière’s disease. Neurol. Clin. 2015, 33, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Casani, A.P.; Sellari-Franceschini, S.; Napolitano, A.; Muscatello, L.; Dallan, I. Otoneurologic dysfunctions in migraine patients with or without vertigo. Otol. Neurotol. 2009, 30, 961–967. [Google Scholar] [CrossRef]
- Young, A.S.; Nham, B.; Bradshaw, A.P.; Calic, Z.; Pogson, J.M.; D’Souza, M.; Halmagyi, G.M.; Welgampola, M.S. Clinical, oculographic, and vestibular test characteristics of vestibular migraine. Cephalalgia 2021, 41, 1039–1052. [Google Scholar] [CrossRef]
- Fu, W.; Wang, Y.; He, F.; Wei, D.; Bai, Y.; Han, J.; Wang, X. Vestibular and oculomotor function in patients with vestibular migraine. Am. J. Otolaryngol. 2021, 42. [Google Scholar] [CrossRef]
- Shim, D.B.; Ko, K.M.; Lee, J.H.; Park, H.J.; Song, M.H. Natural history of horizontal canal benign paroxysmal positional vertigo is truly short. J Neurol. 2015, 262, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Gufoni, M.; Ducci, N.; Casani, A.P. Update on the treatment of benign positional paroxysmal vertigo of the horizontal semi-circular canal. J. Otolaryngol. 2022, 72, 101–106. [Google Scholar] [CrossRef]
- Halmagyi, G.M.; Curthoys, I.S.; Brandt, T.; Dieterich, M. Ocular tilt reaction: clinical sign of vestibular lesion. Acta Otolaryngol. Suppl. 1991, 481, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Gufoni, M.; Vianini, M.; Casani, A.P. Analysis of the Skew Deviation to Evaluate the Period of Onset of a Canalolithiasis After Macular Damage. Front. Neurol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Rocha, M.F.; Sacks, B.; Al-Lamki, A.; Koohi, N.; Kaski, D. Acute vestibular migraine: a ghost diagnosis in patients with acute vertigo. J. Neurol. 2023, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Gufoni, M.; Casani, A.P. The Pupillary (Hippus) Nystagmus: A Possible Clinical Hallmark to Support the Diagnosis of Vestibular Migraine. J. Clin. Med. 2023, 12, 1957. [Google Scholar] [CrossRef] [PubMed]
- Cortez, M.M.; Rae, N.; Millsap, L.; McKean, N.; Brennan, K.C. Pupil cycle time distinguishes migraineurs from subjects without headache. Front. Neurol. 2019, 10, 478. [Google Scholar] [CrossRef] [PubMed]
- Bronstein, A.M. Visual vertigo syndrome: Clinical and posturography findings. J. Neurol. Neurosurg. Psychiatry 1995, 59, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Casani, A.P.; Lazzerini, F.; Marconi, O.; Vernassa, N. The role of the functional head impulse test with and without optokinetic stimuli in vestibular migraine and acute unilateral vestibulopathy: Discovering a dynamic visual depenence. J. Clin. Med. 2021, 10, 3787. [Google Scholar] [CrossRef]
- Von Brevern, M.; Lempert, T. Vestibular migraine: treatment and prognosis. Seminars in Neurology. 2020, 40, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Lempert, T.; Olesen, J.; Furman, J.; Waterston, J.; Seemungal, B.; Carey, J.; Bisdorff, A.; Versino, M.; Evers, S.; Kheradmand, A.; Toker, D.M. Vestibular migraine: Diagnostic criteria. An update. J. Vestib. Res. 2022, 32, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Basura, G.J.; Adams, M.E.; Monfared, A.; Schwartz, S.R.; Antonelli, P.J.; Burkard, R.; Bush, M.L.; Bykowski, J.; Colandrea, M.; Derebery, J.; Kelly, E.A.; Kerber, K.A.; Koopman, C.F.; Kuch, A.A.; Marcolini, E.; McKinnon, B.J; Ruckenstein, M.J.; Valenzuela, C.V.; Vosooney, A.; Walsh, S.A.; Nnacheta, L.C.; Dhepyasuwan, N.; Buchanan, E.M. Clinical Practice Guideline: Ménière’s Disease. Otolaryngol. -Head Neck Surg. 2020, 162, S1–S55. [Google Scholar] [CrossRef]
- Pyykkö, I.; Nakashima, T.; Yoshida, T.; Zou, J.; Naganawa, S. Ménière’s disease: a reappraisal supported by a variable latency of symptoms and the MRI visualization of endolymphatic hydrops. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Perez-Carpena, P.; Lopez-Escamez, J.A. Current understanding and clinical management of meniere’s disease: A systematic review. In Proceedings of the Seminars in Neurol. 2020, 40, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Cerchiai, N.; Navari, E.; Dallan, J.; Sellari -Franceschini, S.; Casani, A.P. Assessment of Vestibulo -oculomotor Reflex in Ménière’s Disease: Defining an Instrumental Profile. Otol.Neurotol. 2016, 37, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Hannigan, I.P.; Welgampola, M.S.; Watson, S.R.D. Dissociation of Caloric and Head Impulse Tests: A Marker of Meniere’s Disease. J. Neurol. 2021, 268, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Hotson, J.R.; Baloh, R.W. Acute vestibular syndrome. N Engl J Med. 1998, 339, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Yao, K.; Zu, H.B. Isolated transient vertigo due to TIA: challenge for diagnosis and therapy. J. Neurol. 2023, 270, 769–779. [Google Scholar] [CrossRef] [PubMed]
- Kattah, J.C.; Talkad, A.V.; Wang, D.Z.; Hsieh, Y.H.; Newman-Toker, D.E. HINTS to diagnose stroke in the acute vestibular syndrome: Three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 2009, 40, 3504–3510. [Google Scholar] [CrossRef]
- Lee, H.; Sohn, S.I.; Cho, Y.W.; Lee, S.R.; Ahn, B.H.; Park, B.R.; Baloh, R.W. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurol. 2006, 67, 1178–1183. [Google Scholar] [CrossRef]
- Casani, A.P.; Dallan, I.; Cerchiai, N.; Lenzi, R.; Cosottini, M.; Sellari Franceschini, S. Cerebellar infarctions mimicking acute peripheral vertigo: how to avoid misdiagnosis? Otolaryngol. Head Neck Surg. 2013, 148, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Gerlier, C.; Hoarau, M.; Fels, A.; Vitaux, H.; Mousset, C.; Farhat, W.; Firmin, M.; Pouyet, V.; Paoli, A.; Chatellier, G.; et al. Differentiating central from peripheral causes of acute vertigo in an emergency setting with the HINTS, STANDING, and ABCD2 tests: A diagnostic cohort study. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2021, 28, 1368–1378. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, A.C.; Merwick, Á.; Dennis, M.; Ferrari, J.; Ferro, J.M.; Kelly, P.; Lal, A.; Ois, A.; Olivot, J.M.; Purroy, F. European Stroke Organization (ESO) guidelines on management of transient ischaemic attack. J. Eur. Stroke. 2021, 6, 163–186. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, H.; Cerchiai, N.; Mancuso, M.; Casani, A.P.; Bronstein, A.M. Are white matter abnormalities associated with “unexplained dizziness”? J. Neurol. Sci. 2015, 358, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Cerchiai, N.; Mancuso, M.; Navari, E.; Giannini, N.; Casani, A.P. Aging with Cerebral Small Vessel Disease and Dizziness: The Importance of Undiagnosed Peripheral Vestibular Disorders. Front Neurol. 2017, 8, 241. [Google Scholar] [CrossRef] [PubMed]
- Ibitoye, R.T.; Castro, P.; Cooke, J. , Allum, J.; Arshad, Q.; Murdin, L.; Wardlaw, J.; Kaski, D.; Sharp, D.J.; Bronstein, A.M. A link between frontal white matter integrity and dizziness in cerebral small vessel disease. NeuroImage Clin. 2022, 35. [Google Scholar]
- Kim, J.; Lee, H. Vertigo Due to Posterior Circulation Stroke. Semin. Neurol. 2013, 33, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.A.; Oh, E.H.; Choi, S.Y.; Choi, J.H.; Park, J.Y.; Lee, H.; Choi, K.D. Transient Vestibular Symptoms Preceding Posterior Circulation Stroke: A Prospective Multicenter Study. Stroke 2021, 52, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.A.; Bisdorff, A.; Bronstein, A.M.; Lempert, T.; Rossi-Izquierdo, M.; Staab, J.P.; Strupp, M.; Kim, JS. Hemodynamic orthostatic dizziness/vertigo: Diagnostic criteria. J. Vestib. Res. 2019, 29, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Radtke, A.; Lempert, T.; Von Brevern, M.; Feldamnn, M.; Lezius, F.; Neuhauser, H. Prevalence and complications of orthostatic dizziness in the general population. Clin. Auton. Res. 2011, 21, 161–168. [Google Scholar] [CrossRef]
- Sarna, B.; Abouzari, M.; Merna, C.; Jamshidi, S.; Saber, T.; Djalilian, H.R. Perilymphatic Fistula: A Review of Classification, Etiology, Diagnosis, and Treatment. Front. Neurol. 2020, 11, 1046. [Google Scholar] [CrossRef] [PubMed]
- Rizer, F.M.; House, J.W. Perilymph fistulas: the house ear clinic experience. Otolaryngol Head Neck Surg. 1991, 104, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Sarna, B.; Abouzari, M.; Merna, C.; Jamshidi, S.; Saber, S.; Djalilian, H.R. Perilymphatic fistula: A review of classification, etiology, diagnosis, and treatment. Front. Neurol. 2020, 11, 1046. [Google Scholar] [CrossRef] [PubMed]
- Minor, L.B.; Solomon, D.; Zinreich, J.S.; Zee, D.S. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal, A. Otolaryngol.-Head & Neck Surg. 1998, 124, 249–258. [Google Scholar]
- Ward, B.K.; Carey, J.P.; Minor, L.B. Superiorcanaldehiscencesyndrome: lessons from the first 20 years. Front. Neurol. 2017, 8, 177. [Google Scholar] [CrossRef]
- Ward, B.K.; Van De Berg, R.; Van Rompaey, V.; Bisdorff, A.; Hullar, T.E.; Welgampola, M.S.; Carey, J.P. Superior semicircular canal dehiscence syndrome: diagnostic criteria consensus document of the committee for the classification of vestibular disorders of the Bárány Society. J. Vestib. Res. 2021, 31, 131–141. [Google Scholar] [CrossRef]
- Dlugaiczyk, J.; Lempert, T.; Lopez-Escamez, J.A.; Teggi, R.; Von Brevern, M.; Bisdorff, A. Recurrent Vestibular Symptoms Not Otherwise Specified: Clinical Characteristics Compared with Vestibular Migraine and Menière’s Disease. Front. Neurol. 2021, 12. [Google Scholar] [CrossRef]
- Van Leeuwen, R.B.; Colijn, C.; Van Esch, B.F.; Schermer, T.R. Benign Recurrent Vertigo: The Course of Vertigo Attacks Compared to Patients with Menière’s Disease and Vestibular Migraine. Front. Neurol. 2022, 13. [Google Scholar] [CrossRef]
- Teggi, R.; Colombo, B.; Cangiano, I.; Gatti, O.; Bussi, M.; Filippi, M. Similarities and Differences between Vestibular Migraine and Recurrent Vestibular Symptoms—Not Otherwise Specified (RVS-NOS). Audiol. Res. 2023, 13, 466–472. [Google Scholar] [CrossRef]
- Ruthberg, J.S.; Rasendran, C.; Kocharyan, A.; Mowry, S.E.; Otteson, T.D. The economic burden of vertigo and dizziness in the United States. J. Vestib. Res. 2021, 31, 81–90. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




