A 31 years old male reported to Neurorehabilitation department with the complains of weakness in left upper limb with more affection on the distal aspect without any sensory signs. He is a known case of Cerebrovascular accident 1 year back, without any co-morbidities. The patient is under regular medication. He underwent various investigations where the magnetic resonance imaging (MRI) revealed Encephalomalacia with surrounding Gliosis in the right parieto-temporal lobe (
Figure 1). The term "gliosis" refers to a disorder that causes the formation of astrocytes (glial tissue), whereas the term "encephalomalacia" describes the softness of the brain after a stroke or haemorrhages that are brought on by cerebral infarction, cerebral ischemia, infection, craniocerebral trauma, or other injuries [
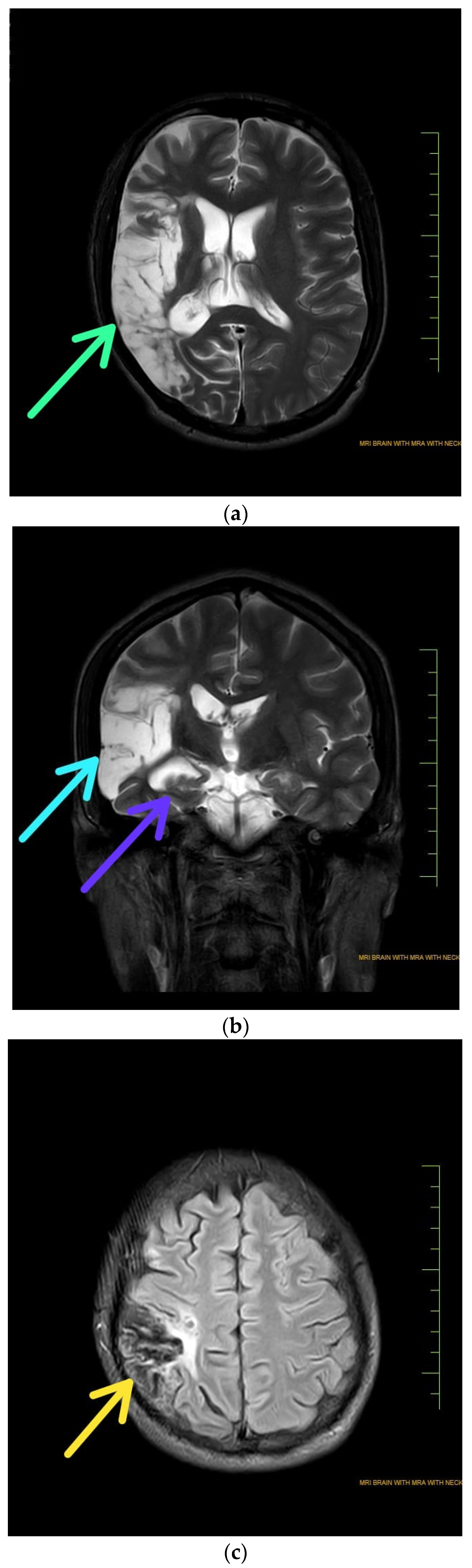
1]. Depending on the underlying reason, softening might only be visible in a small area or might be extensive. The frontal, occipital, parietal, and temporal lobes, as well as other areas of the brain, may all be impacted. The most typical locations for cerebral softening are those where there has been an unusual buildup of blood. A specific area of the brain may occasionally soften as a result of poor blood flow. In this case, the MR Angiography revealed M3 branches of right middle cerebra artery appears narrow (
Figure 2). The blood flow issue could be caused by a stroke in this case, the other causes are severe brain oedema that prevents cerebral blood flow the removal of internal brain tumours that have invaded and damaged surrounding tissues. When stroke affects a portion of the brain, astrocyte-based scar tissue replaces the dying neurons in that area. Imaging studies frequently reveal the gliosis as a "scar" at the site of the brain lesion. In the brain, this scar tissue contracts and develops encephalomalacia which may present with a variety of motor and sensory impairments [
2,
3]. Here, the patient presented with weakness of left upper extremity without any sensory impairments.
Encephalomalacia can be divided into three primary categories based on colour and stage of development, i.e., When blood supply is restored to a portion of the brain that was previously stopped by an embolus, resulting in a haemorrhagic infarct, red softening takes place. Usually, this kind of softening affects the middle cerebral artery or one of its branches. Yellow softening happens when the haemorrhagic infarct liquefies and necrotizes, creating a cavity filled with a yellowish fluid. Degeneration and gliosis symptoms may also be present in the surrounding tissue. The basal ganglia, thalamus, and cerebellum are frequently affected by this kind of softening [
4]. White softening is the process by which the necrotic tissue eventually resorbs and is replaced by a cystic cavity. A porencephalic cyst could be created if the cyst communicates with the ventricles or the subarachnoid region. Atrophy and gliosis may also be present in the nearby tissue. Any area of the brain may experience this kind of softening [
5]. This may be a case of white softening as per presentation.
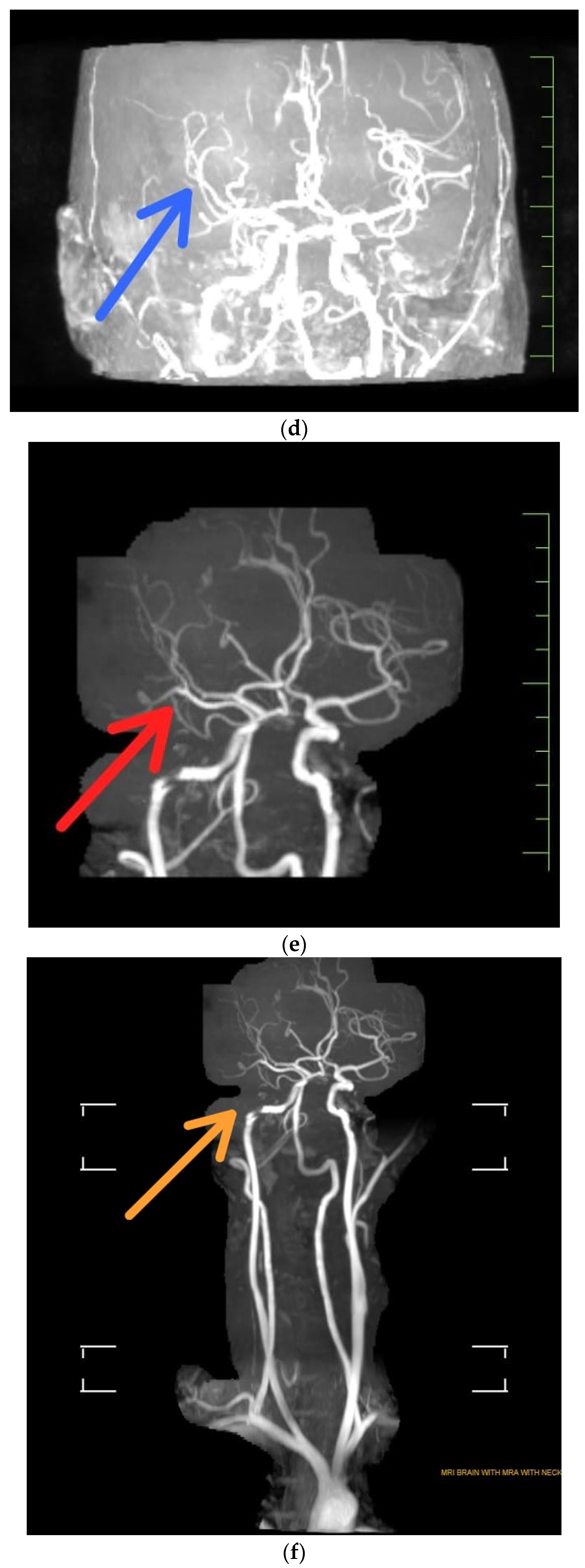
Figure 1.
Radiologic findings unveils Encephalomalacia with surrounding gliosis noted in right parieto-temporal lobe [
1,
6].
Figure 1.
Radiologic findings unveils Encephalomalacia with surrounding gliosis noted in right parieto-temporal lobe [
1,
6].
- (a)
T2 Weighted MRI unveiling Encephalomalacia with surrounding gliosis in right parieto-temporal lobe with green arrow
- (b)
Coronal T2 weighted indicating Stage 3 Wallerian degeneration with purple arrow where Gliosis replaces the degenerating axons and myelin sheaths, and myelin lipid breakdown (more than 14 weeks). Gliosis appears as an area with increased T2/FLAIR signal, somewhat reduced T1 signal. Light blue arrow indicates Encephalomalacia with surrounding gliosis noted in right parieto-temporal lobe.
- (c)
T2 FLAIR (Fluid Attenuated Inversion Recovery) indicated atrophy of right middle cerebral peduncle s/o Wallerian degeneration [
7].
Author Contributions
Conceptualization, data curation, original draft preparation, review and editing- PH. All authors have read and agreed to the published version of the manuscript.
Funding
This article received no external funding.
Informed Consent Statement
Consent was taken from the patient beforehand.
Data Availability Statement
Not applicable.
Acknowledgments
The authors wish to thank all the anonymous reviewerfor their helpful suggestions in improving the quality of the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Karaman E, Isildak H, Yilmaz M, Enver O, Albayram S: Encephalomalacia in the frontal lobe: complication of the endoscopic sinus surgery. J Craniofac Surg. 2011, 22, 2374–2375. [CrossRef]
- Matlung SE, Bilo R a. C, Kubat B, van Rijn RR: Multicystic encephalomalacia as an end-stage finding in abusive head trauma. Forensic Sci Med Pathol. 2011, 7, 355–363. [CrossRef]
- Naidich TP, Chakera TM: Multicystic encephalomalacia: CT appearance and pathological correlation. J Comput Assist Tomogr. 1984, 8, 631–636. [CrossRef]
- MD DCT: Encephalomalacia: Causes, Types, Symptoms, Diagnosis, Treatment, Complications and Prevention - Scope Heal. 2018.
- Lunardo E: Bel Marra Health. Bel Marra Health - Breaking Health News and Health Information. (2017). Available online: https://www.belmarrahealth.com (accessed on 31 August 2023).
- Garg V: Encephalomalacia | Radiology Reference Article | Radiopaedia.org. Radiopaedia. Available online: https://radiopaedia.org/articles/encephalomalacia (accessed on 29 August 2023). [CrossRef]
- St-Amant M: Wallerian degeneration | Radiology Reference Article | Radiopaedia.org. Radiopaedia. Available online: https://radiopaedia.org/articles/wallerian-degeneration?lang=us (accessed on 29 August 2023). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).