1. Introduction
Pancreatic cancer is a lethal and aggressive cancer that has less than 10% of five-year survival rate [
1]. Because it is difficult to detect early, most patients have pancreatic cancer at an advanced stage, which lowers the success rate of surgical treatment. Therefore, these patients tend to receive chemotherapy [
2,
3]. Currently, gemcitabine is one of the most widely used medications for the treatment of patients with pancreatic cancer [
4]. However, the effects of gemcitabine are limited because drug resistance occurs within weeks of treatment [
5]. Because there are relatively few studies on gemcitabine-resistance in pancreatic cancer, a new strategy is necessary to alleviate drug resistance in pancreatic cancer.
Solute carrier family 38 membrane 5 (SLC38A5), also known as sodium-coupled neutral amino acid transporter 5 (SNAT5), transports amino acids such as asparagine, glutamine, methionine, serine, and glycine across the cell membrane [
6]. Unlike other amino acid transporters, SLC38A5 mainly transports glutamine into the cancer cells [
7,
8]. For example, upregulation of SLC38A5 induces cell proliferation by inducing macropinocytosis in triple-negative breast cancer [
9]. Moreover, a previous study reported that SLC38A5 initiates pancreatic neuroendocrine tumor formation [
10]. However, there have been no studies on the biological mechanisms of SLC38A5 and gemcitabine-resistance in pancreatic cancer. According to The Cancer Genome Atlas (TCGA) database, upregulation of SLC38A5 tends to result in a poor survival rate in pancreatic cancer. Therefore, we hypothesized that there could be a crucial role of SLC38A5 in pancreatic cancer.
Glutamine is an important nutrient in cancer metabolism and is involved in the synthesis of proteins and lipids and de novo glutathione production [
11]. Cancer cells tend to consume more glutamine than normal cells during cell proliferation and epithelial-to-mesenchymal transition (EMT) [
12]. However, the correlation between glutamine and gemcitabine-resistance in pancreatic cancer remains unclear. Therefore, we aimed to study the effect of glutamine transported by SLC38A5 in gemcitabine-resistant cancer cells. As glutamine enters cells, it is converted into glutamate via glutaminolysis in the mitochondria [
13]. Eventually, glutamate is secreted from the mitochondria and contributes to glutathione synthesis [
14]. Glutathione is an antioxidant that regulates reactive oxygen species (ROS) levels in cancer cells [
15]. Additionally, glutamine regulates the mTOR-SREBP1 signaling pathway in cancer cells [
16]. SCD1 is a downstream target gene of SREBP1 signaling and plays a role in converting polyunsaturated fatty acids (PUFAs) that induce lipid ROS into monounsaturated fatty acids (MUFAs) [
17]. Therefore, glutamine deprivation upregulates lipid ROS levels in pancreatic cancer cells. Hence, we hypothesized that glutamine depletion may increase the effect of gemcitabine on gemcitabine-resistant pancreatic cancer cells.
Ferroptosis is a type of programmed cell death associated with lipid ROS accumulation [
18]. Recently, several studies have shown that ferroptosis plays an important role in various cancers, including pancreatic cancer. Previous studies have shown that ferroptosis alleviates sorafenib resistance in hepatocellular carcinoma and cisplatin resistance in head and neck cancers [
19,
20]. However, the relationship between ferroptosis and gemcitabine-resistance in pancreatic cancer remains unclear. Therefore, we examined ROS and lipid ROS-related genes as indicators of ferroptosis [
21].
In this study, we observed that glutamine uptake was increased in gemcitabine-resistant pancreatic cancer. Moreover, the upregulated glutamine levels ultimately contribute to the inhibition of ferroptosis, making pancreatic cancer more resistant to gemcitabine. Conversely, gemcitabine-resistance was weakened when SLC38A5 expression was suppressed. We also demonstrated that the depletion of SLC38A5 induces mitochondrial dysfunction and ROS levels and decreases mTOR-SREBP1 signaling. These pathways ultimately induced ferroptosis by increasing lipid ROS levels. Moreover, SLC38A5 inhibition effectively sensitized pancreatic cancer cells to gemcitabine treatment, suppressing tumor weight and metastasis in vivo. Taken together, our results suggest that SLC38A5 is a novel therapeutic target for ameliorating gemcitabine-resistance in pancreatic cancer.
2. Materials and Methods
2.1. The Cancer Genome Atlas analysis
Expression data for pancreatic cancer were obtained from TCGA, and SLC38A5 levels were analyzed with transcripts per million (TPM) as log2 (TPM + 1) in the Gene Expression Profiling Interactive Analysis (GEPIA) portal. Clinical parameters and survival data were also acquired from TCGA pancreatic cancer database. Overall survival and disease-specific survival were analyzed using Kaplan-Meier plots. Correlation analysis of indicated genes was evaluated in GEPIA portal.
2.2. Cell culture.
Human pancreatic cancer cell lines (PANC-1 and Capan-1) were purchased from American Type Culture Collection (ATCC MD, VA, USA). PANC-1 and Capan-1 were cultured in DMEM and RPMI 1640 supplemented with 10% fetal bovine serum (Biowest, Nuaillé, France), and 1% antibiotic-antimycotic reagent (Gibco, Waltham, MA, USA) at 37°C and 5% CO2. After one passage, gemcitabine was treated to PANC-1 and Capan-1 cells to establish gemcitabine-resistant cell line. After that, the surviving cells were subcultured and continuously treated with increasing gemcitabine concentration (0.1 uM to 10 uM) for 3 months. After the gemcitabine-resistant cells stabilized, they were treated with the same concentration of gemcitabine for 3 months.
2.3. Patient’s tissues mRNA and protein
Pancreatic tissues were obtained from patients diagnosed with pancreatic cancer at Gangnam Severance Hospital. mRNA samples were isolated using the TRIZOL reagent (Sigma-Aldrich, Munich, Germany). Protein samples were extracted using RIPA lysis buffer (Sigma-Aldrich). The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Gangnam Severance Hospital (no.3-2021-0414).
2.4. Small-Interfering RNA transfection
The cells were transfected with small-interfering RNA (siRNA) targeting SLC38A5 (Santa Cruz Biotechnology, Dallas, TX, USA) using Lipofectamine® RNAiMAX transfection reagent (Invitrogen, Waltham, Massachusetts, USA) in Opti-MEM (GIBCO) according to the manufacturer’s protocol.
2.5. WST assay
The cells were seeded in 96-well plates at a density of 5 × 103 (PANC-1) and 7 × 103 (Capan-1) cells per well and incubated for 24 h. They were then treated with the indicated concentrations of gemcitabine for 72 h. Growth medium was replaced with 10% water-soluble tetrazolium (WST)-1 reagent (DoGenBio) and incubated for 1 h at 37°C in the dark. The absorbance of each well was measured at 450 nm wavelength using a VersaMax microplate reader (Molecular Devices, San Jose, CA, USA).
2.6. Wound healing assay
The cells were seeded in 12-well plates at densities of 2 × 105 (PANC-1) and 4 × 105 (Capan-1) per well. The next day, they were transfected with siRNA, and wound scratches were made 24 h after transfection. Microscopic images of the migrated cells were captured at the indicated time intervals.
2.7. Invasion assay
For invasion assay, 8-µm pore size Transwell system was coated with Matrigel for 1 h at room temperature. The cells were seeded in 24-well plates at a density of 1 × 105 (PANC-1) and 2 × 105 (Capan-1). Cells were then transfected with siRNA. After 24h, cells were transferred to the transwell at a density of 0.7 x 105 (PANC-1) and 2.5 × 105 (Capan-1) and incubated for 24 h. The transwell plate was washed with PBS and fixed in 4% paraformaldehyde for 5 min. The transferred cells were stained with crystal violet (JUNSEI, Tokyo, Japan).
2.8. RNA sequencing
Total RNA was isolated using the TRIzol reagent (Invitrogen). RNA quality was assessed using an Agilent 2100 Bioanalyzer with an RNA 6000 Nano Chip (Agilent Technologies, Amstelveen, The Netherlands), and RNA quantification was performed using an ND-2000 Spectrophotometer (Thermo Inc., DE, USA). For control and test RNAs, library construction was performed using QuantSeq 3’ mRNA-Seq Library Prep Kit (Lexogen, Inc., Austria), according to the manufacturer’s instructions. High-throughput sequencing was performed as 75-bp single-end sequencing using NextSeq 500 (Illumina, Inc., USA). QuantSeq 3 mRNA-Seq reads were aligned using the Bowtie2 (Langmead and Salzberg, 2012).
2.9. Glutamine uptake assay
The cells were seeded in a 6-well plate at a density of 2.5 x 105 (PANC-1) and 5 × 105 (Capan-1) per well. The next day, they were transfected with siRNA and harvested using lysis buffer and prepared for the measurement of glutamine using the Glutamine Detection Assay Kit (ab197011) from Abcam (Cambridge, U.K.), according to the manufacturer’s instructions. Relative glutamine uptake was normalized to the number of cells in each experimental group.
2.10. OCR and ECAR measurement
The Oxygen consumption rate (OCR) was measured using a Seahorse XF24 extracellular flux analyzer (Seahorse Bioscience, North Billerica, MA, USA). The cells were seeded onto XF-24 plates at a density of 5 × 105 cells/well for 24 h and treated with siRNA. Thereafter, they were incubated XF assay media for 1 h at 37°C in a non-CO2 incubator and stressed with sequential addition of 1 µM oligomycin, 2 µM carbonyl cyanide p-(trifluoromethoxy) phenylhydrazone, and a 0.5 µM cocktail of rotenone/antimycin A. The OCR was normalized to the total cellular protein concentration.
2.11. Glutathione level assay
The cells were seeded in a 6-well plate at a density of 2.5 x 105 (PANC-1) and 5 × 105 (Capan-1) per well. The next day, they were transfected with siRNA and collected by scraping and prepared for the measurement of glutathione using the Glutathione Assay Kit (No. 703002) from Cayman Chemical (Michigan, USA) according to the manufacturer’s protocol. Glutathione concentrations were calculated using a standard curve and normalized to the total protein levels in each sample.
2.12. ROS and lipid ROS measurement
The cells were seeded in a 6-well plate at a density of 2.5 x 105 (PANC-1) and 5 × 105 (Capan-1) per well. The next day, they were transfected with siRNA and treated with fer-1 (20uM) for 48 h. After treatment, they were incubated with 20 μM 2ʹ7ʹ-dichlorodihydrofluorescein diacetate (DCF-DA; Sigma-Aldrich) and 10uM BODIPY-C11 (D3861, Invitrogen) for 30 min at 37°C in the dark. They were then washed twice with PBS. The ROS and lipid ROS levels were measured by fluorescence using a FACScanto II flow cytometer (BD Biosciences). A minimum of 10,000 events was recorded for each sample.
2.13. RT-PCR and qPCR
The cells were seeded in a 6-well-plate and incubated for 24 h, and then transfected with siRNA. RNA was isolated using the TRIZOL reagent. The isolated total RNA samples were analyzed by RT-PCR using a Maxime RT-PCR premix kit (Intron, Gyeonggi-do, Korea). RT-qPCR was performed using SYBR qPCR reaction mix (Applied Biosystems, Foster City, CA, USA). The primer sequences used in this study are listed in Table 1. Relative mRNA expression level was calculated using the 2−ΔΔCT method, with GAPDH as the reference gene.
2.14. Western blotting
Cell lysates were separated using sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to polyvinylidene fluoride membranes. After blocking with 5% skim milk for 1 h, the membranes were incubated with primary antibodies (1:1000) at 4 °C overnight, followed by incubation with horseradish peroxidase (HRP)-conjugated secondary antibodies (1:5000) for 1 h. The protein bands were then exposed to an enhanced chemiluminescent HRP substrate (Waltham, MA, USA) and detected using X-ray film. The primary antibodies: GAPDH (# sc-365062), NRF2 (# sc-365949), GPX4 (# sc-166570), SREBP1 (# sc-17755) SCD1 (# sc-515844) were purchased from Santa Cruz Biotechnology (Dallas, TX, USA). mTOR (# 2972S), Phospho-mTOR (# 5536S), PI3K (# 4292S), pAKT (# 9271S), AKT (# 9272S), pSTAT3 (# 9145S), STAT3 (# 9139S) were purchased from Cell Signaling Technology (Danvers, MA, USA). SLC38A5 (# ab72717), RRM1 (# ab226391) were purchased from Abcam. N-cadherin (# 610920) and E-cadherin (# 610181) antibodies were purchased from BD Biosciences (Franklin Lakes, New Jersey, USA). Horseradish peroxidase-conjugated goat anti-mouse (# 7076S) and HRP-conjugated goat anti-rabbit (#7074S) secondary antibodies were purchased from Cell Signaling Technology.
2.15. Animal studies
Six-week-old male nude BALB/c mice were purchased from Orient Bio (Tokyo, Japan). To establish the orthotopic mouse model, 3 × 106 PANC-1 cells were injected into the pancreas of each mouse. After two months, the mice were randomized into two sensitive groups (n = 6) and three resistance groups (n = 6). Then, 4.5 x 106 shRNA lentiviral particles (TL506284V, ORIGENE) were injected into the vein. The following week, gemcitabine (10 mg/kg) and ferrostatin-1 (1 mg/kg) were intraperitoneally injected three times a week for 14 days. On the 14th day, the mice were euthanized. The tumors were harvested, weighed, and fixed in 4% paraformaldehyde. Metastases were photographed. Tumor volume was measured using calipers and calculated using the following formula = 0.5 x length × width2. All animal experimental procedures followed the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were performed in accordance with protocols approved by the Institutional Animal Care and Use Committee of the Seoul Yonsei Pharmaceutical University Experimental Animal Center (approval #2019-0104).
2.16. Statistical analysis
Statistical analyses were performed using one-way or two-way analysis of variance (ANOVA) in GraphPad Prism version 8.0. Data are presented as mean ± standard deviation. Statistical significance was indicated (*P < 0.05; **P < 0.01; ***P < 0.001; #P < 0.05; ##P < 0.01; ###P < 0.001).
3. Results
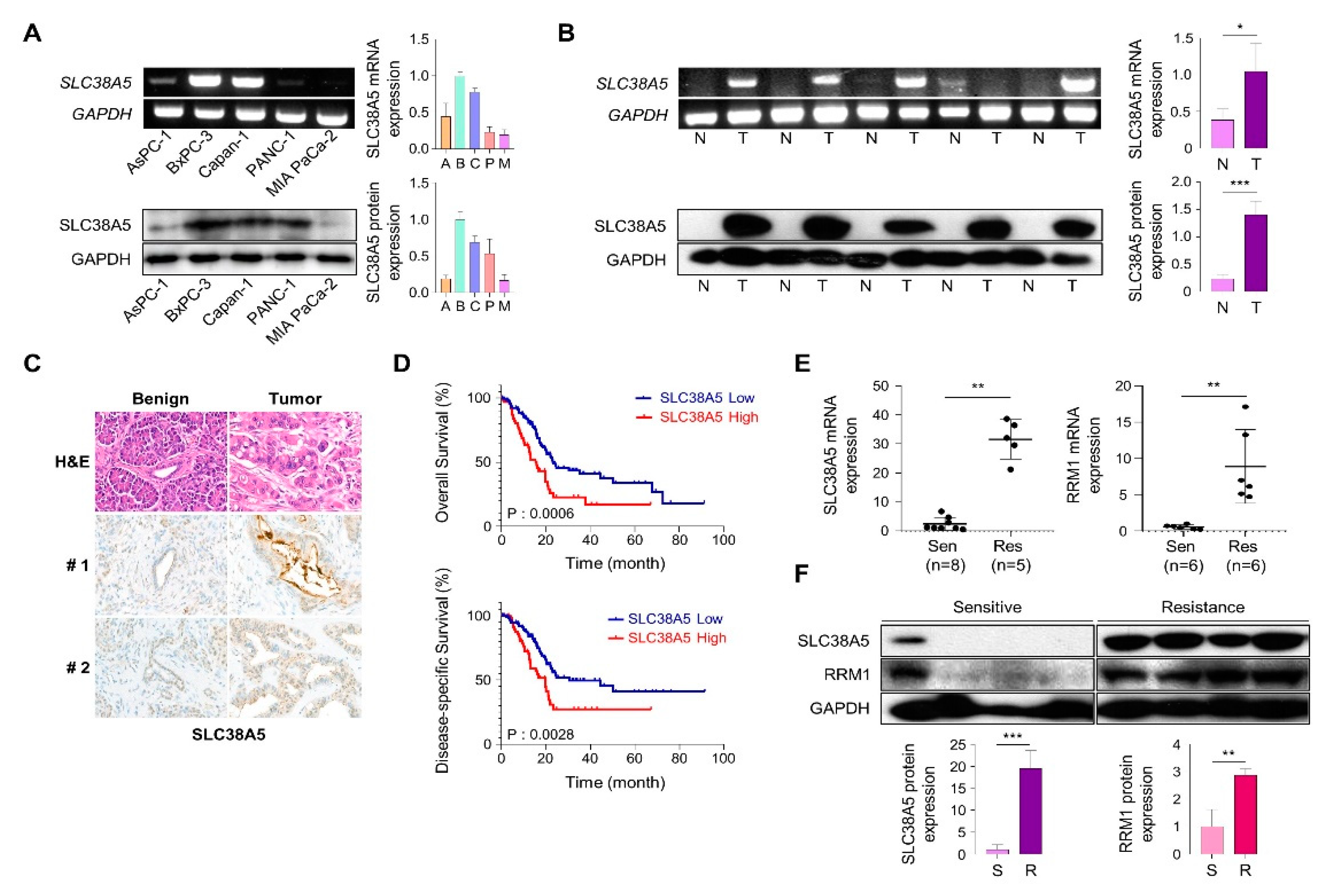
3.1. SLC38A5 correlates with gemcitabine-resistance pancreatic cancer patients
To investigate SLC38A5 expression in pancreatic cancer cells, we analyzed mRNA and protein levels in human pancreatic cancer cell lines. We confirmed that expression of SLC38A5 in five PDAC cell lines (Aspc-3, Bxpc-3, Capan-1, PANC-1, and MIA PaCa-2) using RT-PCR and western blot analysis (Figure 1A). We examined the expression of SLC38A5 in pancreatic cancer using RT-PCR, western blotting, and immunohistochemical staining. Based on these experiments, we found that pancreatic tumor tissues have higher expression levels of SLC38A5 than normal tissues (Figure 1B and C). Moreover, increased levels of SLC38A5 tended to decrease the overall survival (OS) and disease-specific survival (DSS) of patients with pancreatic cancer (Figure 1D). To verify whether SLC38A5 and gemcitabine-resistance are significantly correlated, we confirmed the mRNA expression levels of SLC38A5, RRM1, and gemcitabine-resistance markers in both gemcitabine-sensitive and gemcitabine-resistant patient samples [
22,
23]. Both SLC38A5 and RRM1 mRNA levels were higher in gemcitabine-resistant pancreatic cancer tissues than in gemcitabine-sensitive patient tissues (Figure 1E). Similarly, the protein levels of both SLC38A5 and RRM1 were increased in drug-resistant pancreatic cancer patients compared to those in the drug-sensitive group (Figure 1F). We also constructed a stage plot related to SLC38A5 expression in human data. SLC38A5 expression gradually increased up to stage 3; however, no increase was observed in stage 4 (Figure S1). We hypothesized that SLC38A5 is overexpressed in gemcitabine-resistant conditions and plays an important role in the regulation of gemcitabine-resistant environments.
Figure 1.
SLC38A5 correlates with gemcitabine-resistance pancreatic cancer patients. (A) mRNA and protein expression of SLC38A5 in pancreatic cancer cell lines. (B) mRNA and protein expression of SLC38A5 in normal tissues and pancreatic cancer tissues. (C) H&E staining of the SLC38A5 in tumor tissue. (D) Kaplan-Meier analysis for overall survival, and disease-specific survival between SLC38A5 high group and low group. (E) Dot plot of SLC38A5 and RRM1 gene expression level in purified mRNA from gemcitabine sensitive and resistance pancreatic cancer patient tissue. (F) Protein expression of SLC38A5 and RRM1 between gemcitabine sensitive and resistance pancreatic cancer patient tissue. Bars represent means ± SD. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 1.
SLC38A5 correlates with gemcitabine-resistance pancreatic cancer patients. (A) mRNA and protein expression of SLC38A5 in pancreatic cancer cell lines. (B) mRNA and protein expression of SLC38A5 in normal tissues and pancreatic cancer tissues. (C) H&E staining of the SLC38A5 in tumor tissue. (D) Kaplan-Meier analysis for overall survival, and disease-specific survival between SLC38A5 high group and low group. (E) Dot plot of SLC38A5 and RRM1 gene expression level in purified mRNA from gemcitabine sensitive and resistance pancreatic cancer patient tissue. (F) Protein expression of SLC38A5 and RRM1 between gemcitabine sensitive and resistance pancreatic cancer patient tissue. Bars represent means ± SD. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
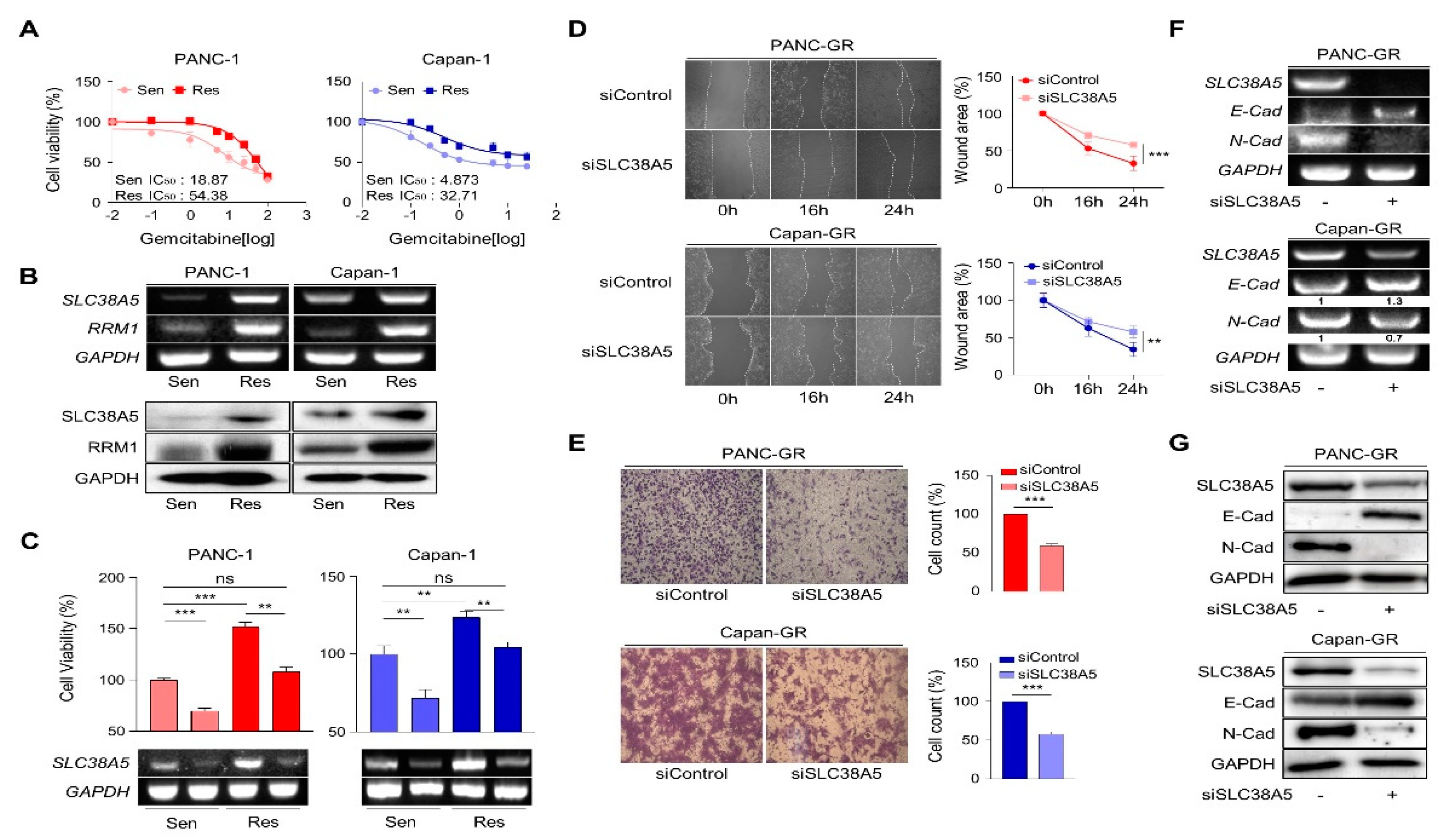
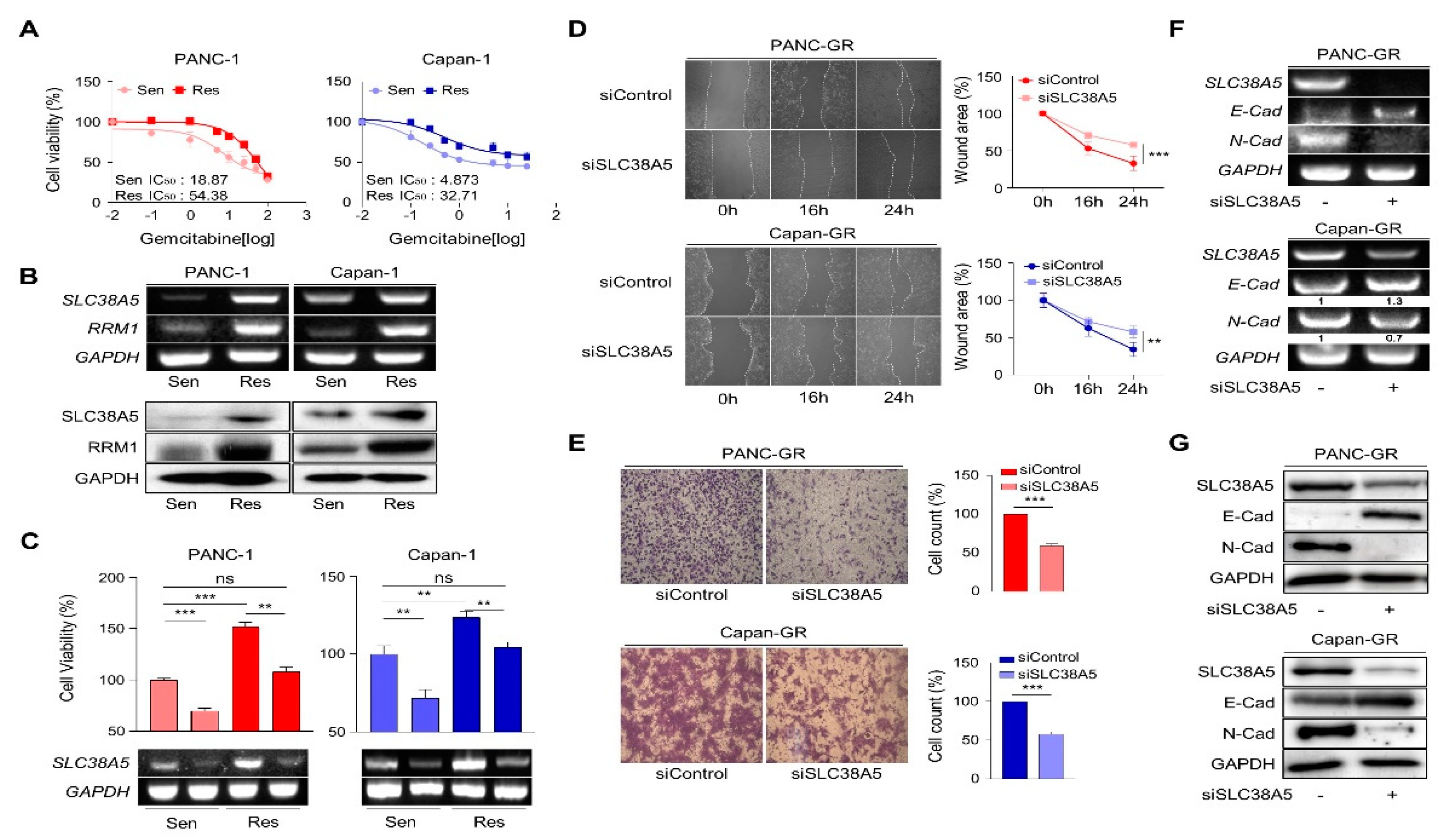
3.2. Deletion of SLC38A5 down-regulates cell viability and migration in gemcitabine-resistance pancreatic cancer cells
To elucidate the role of SLC38A5 in gemcitabine-resistance, we established gemcitabine-resistant pancreatic cancer cell lines using PANC-1 and Capan-1 cells (PANC-GR and Capan-GR, respectively) by confirming the half-maximal inhibitory concentration (IC50) via a cell viability test (Figure 2A and Figure S2A). Consistent with previous results, higher SLC38A5 and RRM1 expression was confirmed at the mRNA and protein levels in the gemcitabine-resistant cell lines than in the gemcitabine-sensitive cell lines (Figure 2B). To investigate whether SLC38A5 modulates the sensitivity of GR cell lines to gemcitabine, a WST assay was performed in the presence of gemcitabine (10 μM). Gemcitabine-resistant cells were more proliferative than gemcitabine-sensitive cells. Conversely, when SLC38A5 was deleted in both sensitive and resistant cells, each cell type showed decreased proliferation according to both cell viability and RT-PCR (Figure 2C). Previous studies have shown that gemcitabine-resistant pancreatic cancer cells show increased levels of both migration and invasion compared to gemcitabine-sensitive cells [
24,
25]. However, it remains unclear whether SLC38A5 plays a significant role in cancer metastasis. Knockdown of SLC38A5 expression hindered both the migration and invasion abilities of cancer cells in the wound healing and transwell invasion assays (Figure 2D and E). To verify whether SLC38A5 controls epithelial-to-mesenchymal transition (EMT), we confirmed EMT-related genes by regulating SLC38A5 mRNA and protein expression in GR cell lines. E-cadherin, an epithelial marker, increased in SLC38A5 knockdown cells. Conversely, the expression of N-cadherin, a mesenchymal marker, decreased (Figure 2F and G). We also analyzed the gene set enrichment analysis (GSEA) results using RNA sequencing data. SLC38A5 deletion was found to reduce wound healing ability, EMT, and angiogenesis in PANC-GR cells (Figure S2D). Therefore, we confirmed that SLC38A5 is involved in the proliferation and EMT of gemcitabine-resistant pancreatic cancer cells.
Figure 2.
Deletion of SLC38A5 down-regulates cell viability and migration in gemcitabine-resistance pancreatic cancer cells. (A) Median inhibitory concentration (IC50) values of gemcitabine for each cell line (PANC-1 and Capan-1). (B) mRNA and protein expression of SLC38A5 and RRM1 in gemcitabine-sensitive PDAC cell lines (PANC-1 and Capan-1) and gemcitabine-resistance PDAC cell lines (PANC-GR and Capan-GR). (C) Cell viability of PANC-1, PANC-GR, Capan-1 and Capan-GR is determined using the WST assay. Each cell lines transfected with siSLC38A5. Transfection is confirmed via RT-PCR. (D) Migration of cells is measured with wound healing assay. The statistical analysis of wound closure percentage is measured by Image J software. (E) Representative photographs of the number of invaded cells that pass through the Matrigel-coated Transwell invasion assay. (F) and (G) The EMT marker expression of siRNA transfected PANC-GR and Capan-GR is analyzed by RT-PCR (F), and western blot (G). Bars represent means ± SD. ns = not significant; **, P < 0.01; ***, P < 0.001.
Figure 2.
Deletion of SLC38A5 down-regulates cell viability and migration in gemcitabine-resistance pancreatic cancer cells. (A) Median inhibitory concentration (IC50) values of gemcitabine for each cell line (PANC-1 and Capan-1). (B) mRNA and protein expression of SLC38A5 and RRM1 in gemcitabine-sensitive PDAC cell lines (PANC-1 and Capan-1) and gemcitabine-resistance PDAC cell lines (PANC-GR and Capan-GR). (C) Cell viability of PANC-1, PANC-GR, Capan-1 and Capan-GR is determined using the WST assay. Each cell lines transfected with siSLC38A5. Transfection is confirmed via RT-PCR. (D) Migration of cells is measured with wound healing assay. The statistical analysis of wound closure percentage is measured by Image J software. (E) Representative photographs of the number of invaded cells that pass through the Matrigel-coated Transwell invasion assay. (F) and (G) The EMT marker expression of siRNA transfected PANC-GR and Capan-GR is analyzed by RT-PCR (F), and western blot (G). Bars represent means ± SD. ns = not significant; **, P < 0.01; ***, P < 0.001.
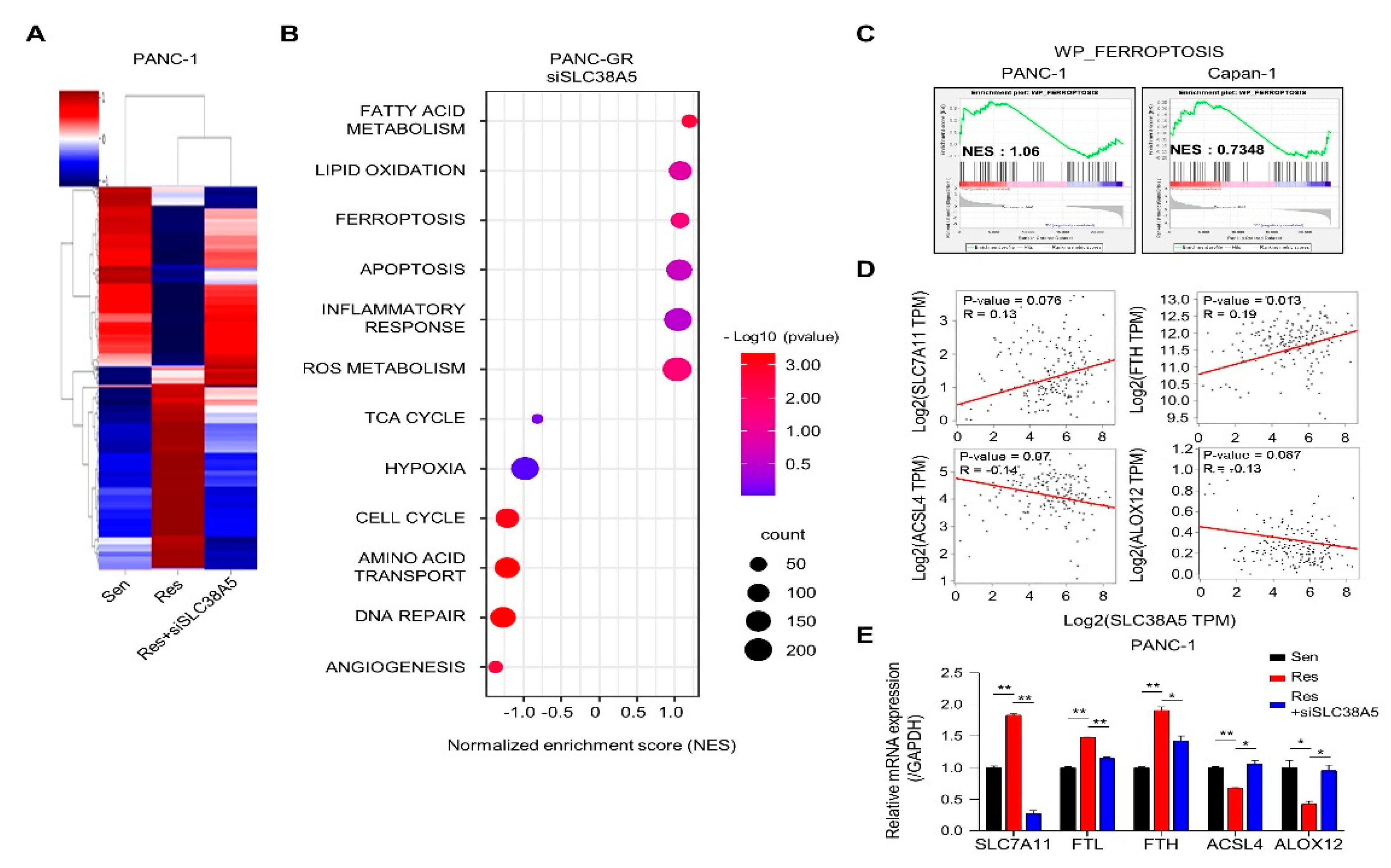
3.3. Overview of enrichment analyses between gemcitabine-resistance cells and SLC38A5 inhibition
Next, we performed RNA sequencing to determine whether SLC38A5 plays a crucial role in any biological mechanism in gemcitabine-resistant cells. Using heat map data, we identified various differential genes compared among PANC-1, PANC-GR, and PANC-GR cells with SLC38A5 knockdown (Figure 3A). Using the DAVID analysis tool, a bubble plot showed that inhibition of SLC38A5 upregulated ferroptosis and lipid oxidation (Figure 3B). Furthermore, the TCA cycle, hypoxia, and cell cycle pathways are downregulated [
26,
27]. Additionally, we analyzed the inhibition of SLC38A5 in promoting ferroptosis through the GSEA graph for both PANC-GR and Capan-GR (Figure 3C). Ferroptosis is a programmed cell death pathway associated with lipid ROS. We performed a correlation analysis of the expression of SLC38A5 and ferroptosis-related genes. We found that SLC7A11 and FTH, ferroptosis-inhibiting genes, were positively correlated with SLC38A5, whereas ACSL4 and ALOX12, ferroptosis-inducing genes, were negatively correlated with SLC38A5 [
28,
29] (Figure 3D). Also, we examined the similar results via q-PCR analysis compared among PANC-1, PANC-GR, and PANC-GR with SLC38A5 knockdown (Figure 3E). Collectively, we found that SLC38A5 inhibition in PANC-GRs induced lipid ROS and ferroptosis. We believe that the results of this study will play an important role in overcoming gemcitabine-resistance.
Figure 3.
Inhibition of SLC38A5 induces ferroptosis in mRNA sequencing. (A) Heat map analysis of distribution of genes from PANC-1, PANC-GR, and PANC-GR with siSLC38A5 cells. (B) DAVID-based gene ontology bubble plot analysis of mRNA sequencing results from PANC-GR and PANC-GR with siSLC38A5 cells. (C) Gene Set Enrichment Analysis (GSEA) for significant enrichment for ferroptosis. (D) Correlation analysis of SLC38A5 and ferroptosis-related genes in pancreatic cancer. (E) mRNA levels of the ferroptosis-related genes were quantified by qPCR in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bars represent means ± SD. *, P < 0.05; **, P < 0.01.
Figure 3.
Inhibition of SLC38A5 induces ferroptosis in mRNA sequencing. (A) Heat map analysis of distribution of genes from PANC-1, PANC-GR, and PANC-GR with siSLC38A5 cells. (B) DAVID-based gene ontology bubble plot analysis of mRNA sequencing results from PANC-GR and PANC-GR with siSLC38A5 cells. (C) Gene Set Enrichment Analysis (GSEA) for significant enrichment for ferroptosis. (D) Correlation analysis of SLC38A5 and ferroptosis-related genes in pancreatic cancer. (E) mRNA levels of the ferroptosis-related genes were quantified by qPCR in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bars represent means ± SD. *, P < 0.05; **, P < 0.01.
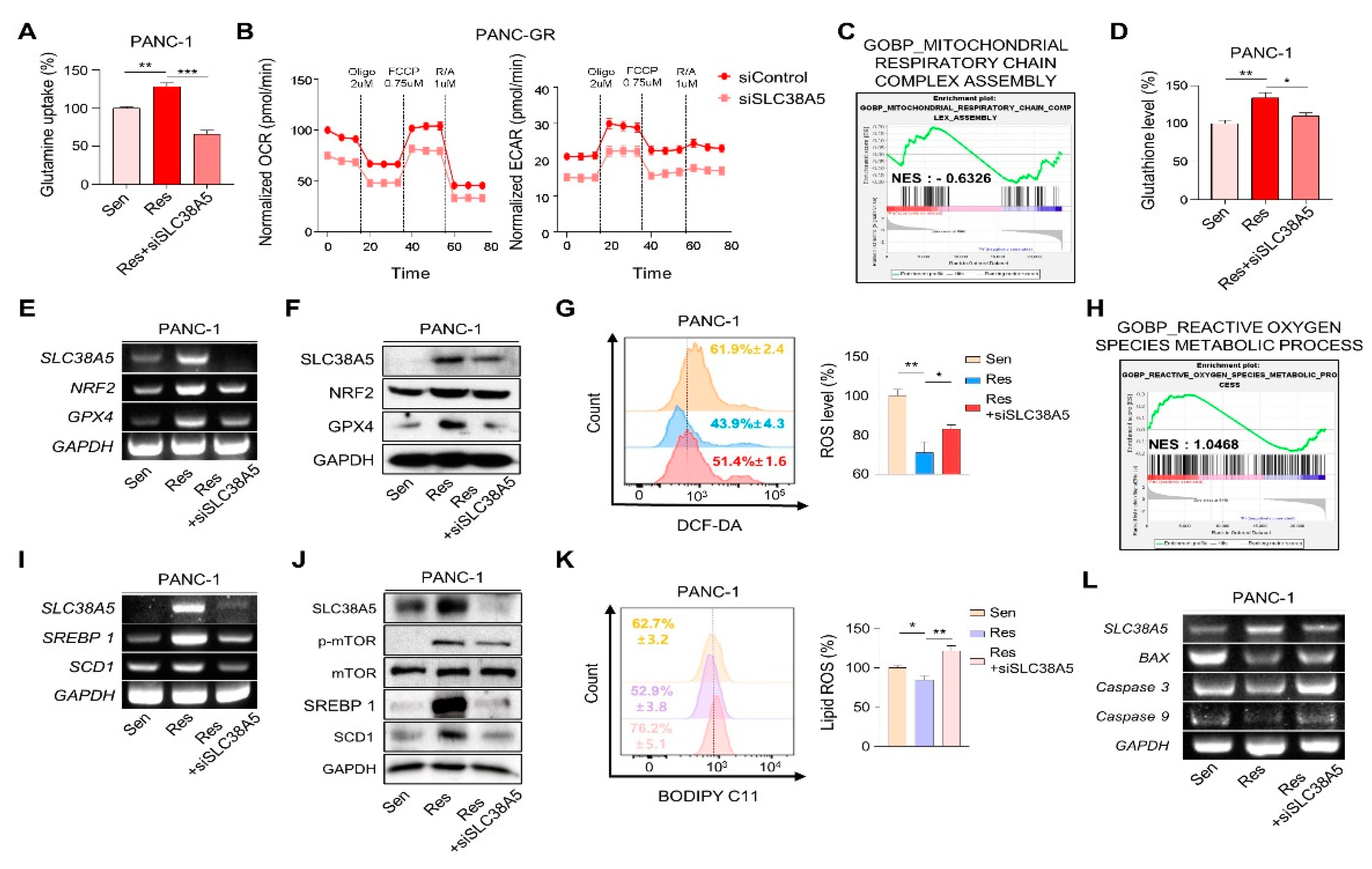
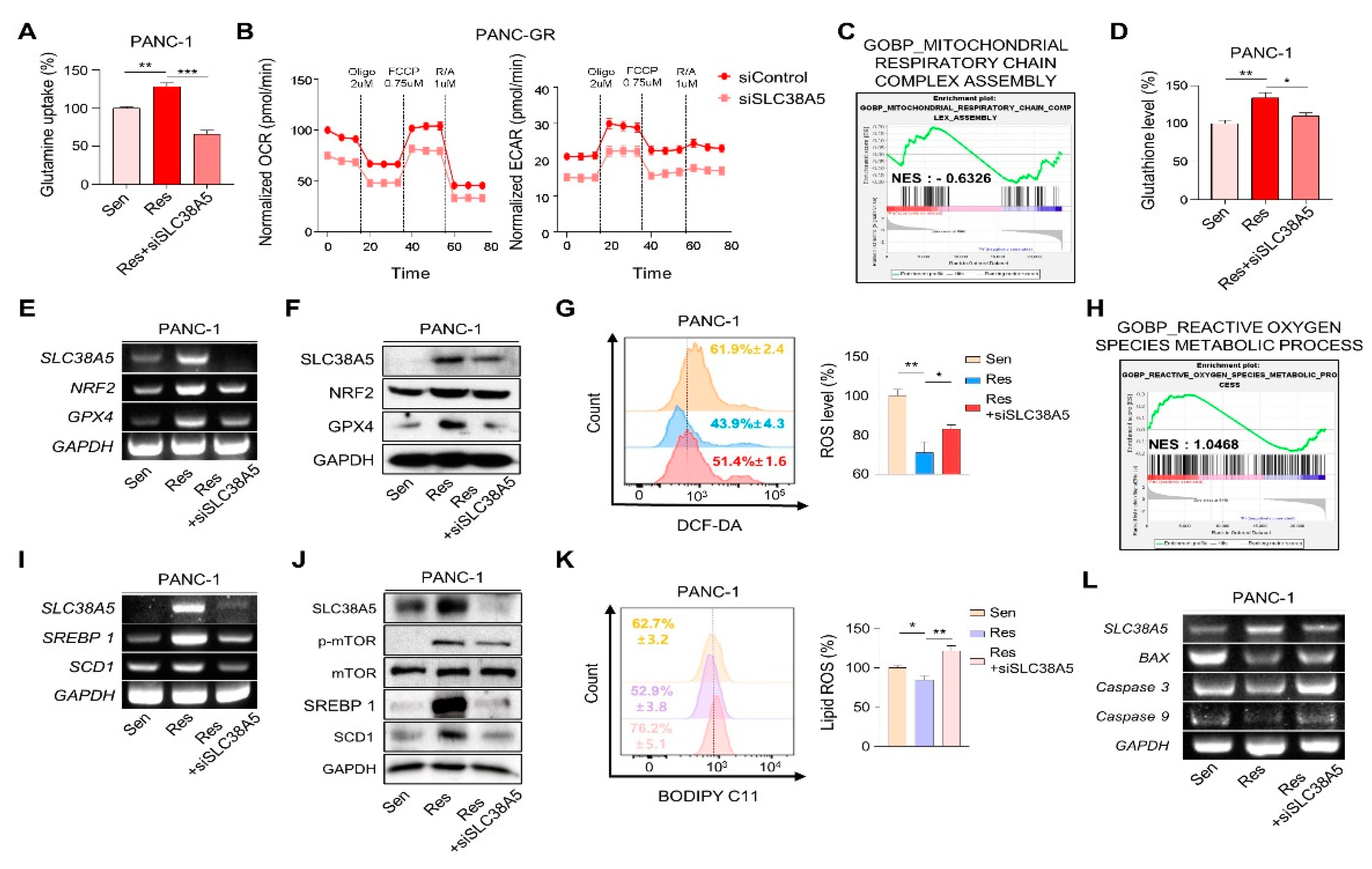
3.4. SLC38A5 modulates lipid ROS through GSH-mediated ROS and mTOR-SREBP1 signaling in gemcitabine-resistance pancreatic cancer cells
Cancer cells, specifically drug-resistant cells, rely more on nutrients than normal cells because of their rapid cell proliferation and migration. Glutamine is the main fuel used by cancer cells. Therefore, we examined whether SLC38A5 regulates glutamine consumption in gemcitabine-resistant cells using a glutamine assay kit. We found that the glutamine consumption rate was much higher in gemcitabine-resistant cells (PANC-GR and Capan-GR) than in gemcitabine-sensitive cells (PANC-1 and Capan-1). Additionally, its rate was downregulated when SLC38A5 was silenced (Figure 4A and Figure S3A). When glutamine enters cells, it is involved in mitochondrial functions, such as the TCA cycle, is converted to glutamate through glutaminolysis, and is then released from the mitochondria [
13]. Therefore, we measured the oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) using a Seahorse XF24 extracellular flux analyzer to confirm mitochondrial activity. Both OCR and ECAR levels were lower in PANC-GR cells with SLC38A5 deletion (Figure 4B). Additionally, GSEA showed that the inhibition of SLC38A5 reduced mitochondrial activity (Figure 4C and Figure S3B). The presence of glutamate in cells contributes to GSH synthesis [
30]. Glutathione is a key factor in the ROS levels related to ferroptosis [
31]. Using a glutathione assay kit, glutathione levels were found to be higher in gemcitabine-resistant cells than in gemcitabine-sensitive cells. Conversely, when SLC38A5 was suppressed, glutathione levels decreased (Figure 4D and Figure S3C). We further confirmed that the GSH-related genes NRF2 and GPX4 were upregulated in PANC-GR and downregulated in PANC-GR transfected with siSLC38A5 by RT-PCR and western blotting (Figure 4E and F). To investigate whether SLC38A5 regulates intercellular ROS levels, we performed fluorescence-activated cell sorting (FACS) analysis using DCF-DA staining by manipulating the expression levels of SLC38A5 in GR cell lines. We observed that ROS levels were much lower in gemcitabine-resistant cell lines than in gemcitabine-sensitive cell lines. As SLC38A5 expression decreased, ROS levels also increased. (Figure 4G and Figure S3E). Based on the previous results from FACS analysis, we also confirmed by GSEA that ROS levels increased when SLC38A5 expression levels were suppressed. (Figure 4H and Figure S3F). Previous studies have reported that glutamine uptake leads to upregulation of the mTOR-SREBP1 signaling pathway, which regulates lipid ROS [
16]. SREBP1 (sterol regulatory element-binding protein 1) is one of the proteins regulating lipid metabolism and acts as a transcription factor for lipid synthesis-related genes such as FASN, ACLY, and SCD1 [
32]. Recent studies have demonstrated that SCD1 accumulates monounsaturated fatty acids (MUFAs), which suppress and inhibit ferroptosis [
17,
33]. Both the mRNA and protein levels of SREBP1 and SCD1 were increased in gemcitabine-resistant cells and were downregulated when SLC38A5 was silenced (Figure 4I, J and Figure S3G). Prior to this experiment, we confirmed that mTOR phosphorylation was reduced in a glutamine-deficient environment by culturing cells in glutamine-free media. Western blotting showed that phospho-mTOR levels decreased in glutamine-free media (Figure S3I). To determine whether SLC38A5 significantly regulates ferroptosis by controlling lipid ROS levels, we measured lipid ROS levels in gemcitabine-resistant cell lines by manipulating SLC38A5 expression via FACS analysis with staining BODIPY-C11. As a result, lipid ROS levels were decreased in gemcitabine-resistant cells but were stored when SLC38A5 expression levels were inhibited (Figure 4K and Figure S3H). Gemcitabine induces apoptosis; however, this apoptotic effect is weakened under gemcitabine-resistant conditions [
34,
35]. To investigate whether SLC38A5 regulates apoptosis, we measured the mRNA expression levels of apoptosis-related genes in PANC-GR cells. PANC-GR showed more anti-apoptotic effects than PANC-GS based on the downregulated levels of BAX, caspase 3, and caspase 9 than PANC-GS. Conversely, the mRNA levels of the apoptosis-inducing genes were upregulated when SLC38A5 was silenced (Figure 4L). Thus, glutamine uptake through SLC38A5 ultimately suppresses lipid ROS production through the GSH-mediated ROS and mTOR-SREBP1 signaling pathway in gemcitabine-resistant cells, leading to apoptosis.
Figure 4.
SLC38A5 modulates lipid ROS through GHS-mediated ROS and mTOR-SREBP1 signaling in gemcitabine-resistance pancreatic cancer cells. (A) Comparison of glutamine uptake of PANC-1, PANC-GR and PANC-GR with siSLC38A5. (B) Oxygen consumption rate (OCR) is determined and calculated under oligomycin, carbonyl cyanide p-(trifluoromethoxy) phenylhydrazone (FCCP), and Rot/antimycin A treatments. Data represents the meant SD (n=3). (C) GSEA for significant enrichment for mitochondrial activity. (D) Comparison of glutathione level of PANC-1, PANC-GR and PANC-GR with siSLC38A5. (E) and (F) Expression of glutathione-related genes in PANC-1, PANC-GR and PANC-GR with siSLC38A5 is analyzed by RT-PCR (E) and western blot (F). (G) Relative ROS production in PANC-1, PANC-GR and PANC-GR with siSLC38A5 were measured using flow cytometry after dichlorofluorescein (DCF)-staining. Bar graph was analyzed by Image J software. (H) GSEA for significant enrichment for ROS level. (I) and (J) Expression of mTOR-SREBP1 signaling genes was analyzed by RT-PCR (I), and western blot (J). (K) Flow cytometry analysis of lipid ROS in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bar graph is analyzed by Image J software. (L) mRNA levels of apoptosis-related genes in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bar represent means ± SD. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 4.
SLC38A5 modulates lipid ROS through GHS-mediated ROS and mTOR-SREBP1 signaling in gemcitabine-resistance pancreatic cancer cells. (A) Comparison of glutamine uptake of PANC-1, PANC-GR and PANC-GR with siSLC38A5. (B) Oxygen consumption rate (OCR) is determined and calculated under oligomycin, carbonyl cyanide p-(trifluoromethoxy) phenylhydrazone (FCCP), and Rot/antimycin A treatments. Data represents the meant SD (n=3). (C) GSEA for significant enrichment for mitochondrial activity. (D) Comparison of glutathione level of PANC-1, PANC-GR and PANC-GR with siSLC38A5. (E) and (F) Expression of glutathione-related genes in PANC-1, PANC-GR and PANC-GR with siSLC38A5 is analyzed by RT-PCR (E) and western blot (F). (G) Relative ROS production in PANC-1, PANC-GR and PANC-GR with siSLC38A5 were measured using flow cytometry after dichlorofluorescein (DCF)-staining. Bar graph was analyzed by Image J software. (H) GSEA for significant enrichment for ROS level. (I) and (J) Expression of mTOR-SREBP1 signaling genes was analyzed by RT-PCR (I), and western blot (J). (K) Flow cytometry analysis of lipid ROS in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bar graph is analyzed by Image J software. (L) mRNA levels of apoptosis-related genes in PANC-1, PANC-GR and PANC-GR with siSLC38A5. Bar represent means ± SD. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
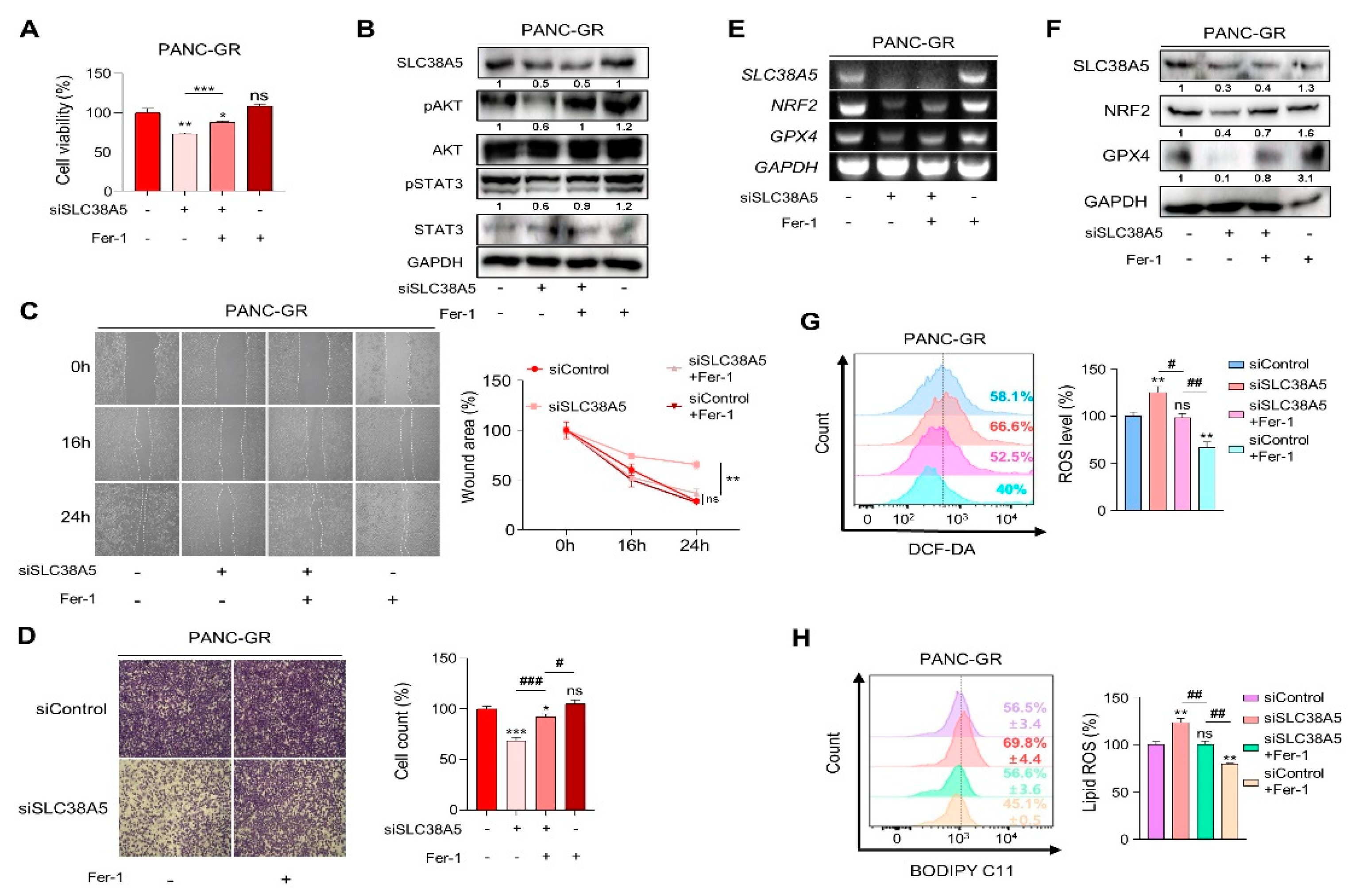
3.5. Inhibition of SLC38A5 induces ferroptosis in gemcitabine-resistance pancreatic cancer cells.
To validate whether SLC38A5 directly regulates ferroptosis, we used ferrostatin-1 as a ferroptosis inhibitor. Inhibition of SLC38A5 sensitized PANC-GR cells to gemcitabine (Figure 2C); however, their viability was rescued when ferrostatin-1 was applied to PANC-GR cells (Figure 5A). With respect to the cell proliferation, we also confirmed that cell proliferation-related genes were upregulated when ferroptosis was inhibited (Figure 5B). Using wound healing and invasion assays, we also confirmed that ferrostatin-1 attenuated the EMT effect of siSLC38A5 in PANC-GR cells (Figure 5C and D). We also utilized NRF2 and GPX4 as antioxidant markers to verify whether ferrostatin-1 could regulate when GR cells expression a low level of SLC38A5 at both mRNA and protein levels. We confirmed that ferrostatin-1 increased the antioxidant levels (Figure 5E and F). Moreover, ferrostatin-1 inhibits ferroptosis by inhibiting lipid ROS [
36,
37]. Consistent with previous studies, our results showed that ferrostatin-1 inhibited both ROS and lipid ROS production (Figure 5G and H). Therefore, the anti-proliferative, EMT, ROS, and ferroptotic effects mediated by SLC38A5 inhibition could be prevented when ferroptosis is suppressed.
Figure 5.
Inhibition of SLc38A5 induces ferroptosis in gemcitabine-resistance pancreatic cancer cells. (A) WST assay is performed to determine cell viability using indicated PANC-GR groups. (B) Cell proliferation marker is confirmed via western blot. (C) and (D) Migration of cell is measured through wound healing assay (C) and Matrigel-coated transwell invasion assay (D). (E)and (F) Expression of glutathione-related genes is measured by RT-PCR (E) and western blot (F). (G) Relative ROS production in indicated PANC-GR groups was measured via FACS analysis. (H) FACS analysis of lipid ROS in indicated PANC-GR groups. Bar graph is analyzed by Image J software. Ferrostatin-1 (Fer-1) is treated with 20 uM. Bar represent means ± SD. ns = not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 5.
Inhibition of SLc38A5 induces ferroptosis in gemcitabine-resistance pancreatic cancer cells. (A) WST assay is performed to determine cell viability using indicated PANC-GR groups. (B) Cell proliferation marker is confirmed via western blot. (C) and (D) Migration of cell is measured through wound healing assay (C) and Matrigel-coated transwell invasion assay (D). (E)and (F) Expression of glutathione-related genes is measured by RT-PCR (E) and western blot (F). (G) Relative ROS production in indicated PANC-GR groups was measured via FACS analysis. (H) FACS analysis of lipid ROS in indicated PANC-GR groups. Bar graph is analyzed by Image J software. Ferrostatin-1 (Fer-1) is treated with 20 uM. Bar represent means ± SD. ns = not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001.
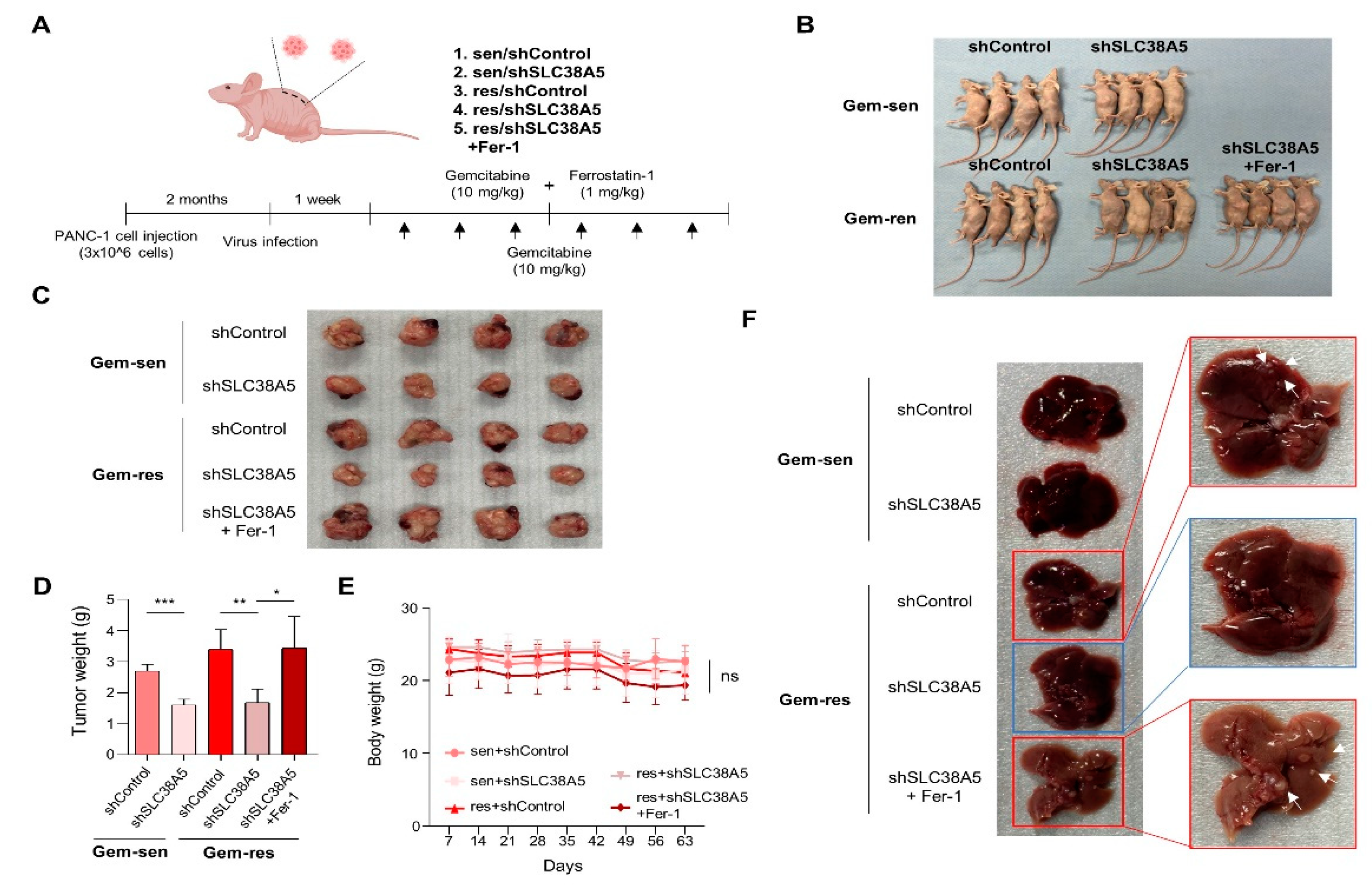
3.6. Suppression of SLC38A5 inhibits tumor growth and metastasis in orthotopic model
To evaluate whether SLC38A5 plays an important role in the metastasis of gemcitabine-resistant pancreatic tumors in vivo, we generated a BALB/c nude mouse model bearing orthotopic tumors. After 2 months, gemcitabine and ferrostatin-1 were intraperitoneally injected at the indicated concentrations three times a week for 2 weeks (Figure 6A). After drug injection, each group exhibited significantly different tumor sizes. The gemcitabine-resistant group had a much larger tumor size than the gemcitabine-sensitive group. Moreover, inhibition of SLC38A5 hindered tumor growth in both the gemcitabine-sensitive and gemcitabine-resistant groups. Furthermore, treatment with ferrostatin-1 increased tumor size (Figure 6B and C). Related to the tumor size, the gemcitabine-resistant group weighed more than the gemcitabine-sensitive. Blockade of SLC38A5 lowered tumor weight, but inhibition of ferroptosis increased tumor weight (Figure 6D). Furthermore, the gemcitabine-resistant group showed liver metastases, whereas the gemcitabine-resistant with SLC38A5 knock-down group showed no liver metastases. Conversely, the inhibition of ferroptosis induced liver metastasis by preventing SLC38A5 inhibition (Figure 6F). However, no significant differences were observed in the body weight (Figure 6E). Collectively, SLC38A5 inhibition sensitizes drug-resistant pancreatic cancer cells to gemcitabine by inducing ferroptosis and suppressing tumor growth and metastasis. Therefore, targeting SLC38A5 may play a major role in improving the 5-year survival rate of patients with pancreatic cancer and overcoming chemoresistance in pancreatic cancer for clinical purposes. Collectively, these results demonstrated that SLC38A5 regulates ferroptosis in gemcitabine-resistant pancreatic cancer in vitro and in vivo (Figure 7).
Figure 6.
Knockdown of SLC38A5 suppress tumor growth and metastasis in vivo. (A) Schematic of mouse experimental grouping and processing of the orthotopic model. (B) Representative tumor bearing mouse image. (C) Images of the tumors harvested from mice. (D) Representative tumor weights. (E) Mice body weights were measured every 7 days. (F) Liver metastasis images. Bars represent means ± SD. ns = not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 6.
Knockdown of SLC38A5 suppress tumor growth and metastasis in vivo. (A) Schematic of mouse experimental grouping and processing of the orthotopic model. (B) Representative tumor bearing mouse image. (C) Images of the tumors harvested from mice. (D) Representative tumor weights. (E) Mice body weights were measured every 7 days. (F) Liver metastasis images. Bars represent means ± SD. ns = not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001.
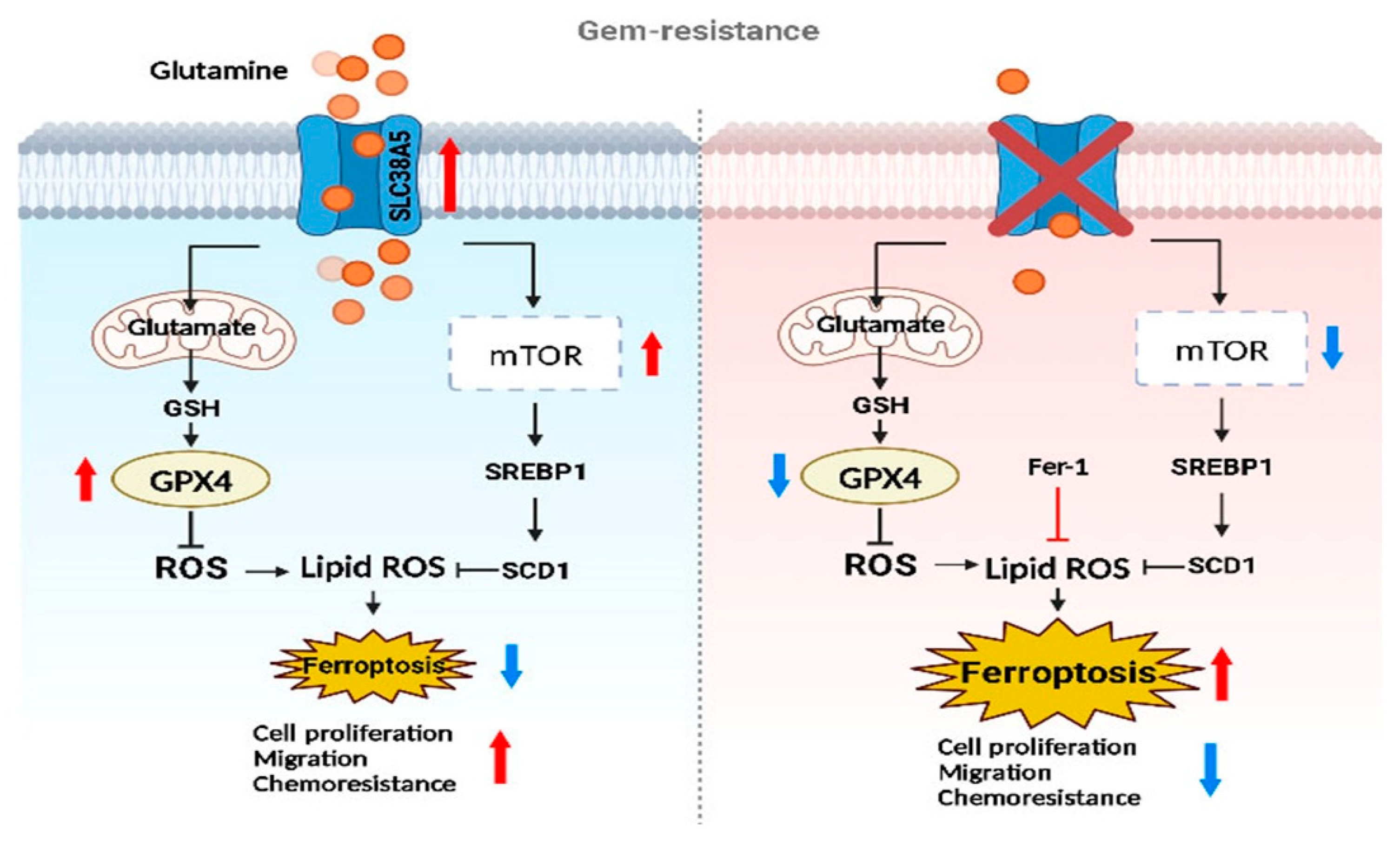
Figure 7.
The graphical abstract illustrates the regulatory mechanism of SLC38A5 in gemcitabine-resistance pancreatic cancer.
Figure 7.
The graphical abstract illustrates the regulatory mechanism of SLC38A5 in gemcitabine-resistance pancreatic cancer.
4. Discussion
Pancreatic cancer is one of the most fatal diseases with one of the highest mortality rates among all major cancers [
38]. Despite the development of many treatments and diagnostic methods, the poor prognosis of pancreatic cancer has not improved compared with that of other cancers. Although gemcitabine is known as a standard drug for the treatment of PDAC, it has a major limitation in that drug resistance can easily develop. Therefore, the present study aimed to overcome gemcitabine-resistance in pancreatic cancer.
SLC38A5 is a well-known amino acid transporter that transport glutamine [
8]. Recent studies have shown that glutamine plays a critical role in the growth, survival, and drug resistance of pancreatic cancer [
39]. Glutamine is a key nutrient that promotes drug resistance in breast cancer [
40]. However, the mechanism through which glutamine affects drug resistance in pancreatic cancer has not yet been elucidated. In this study, we investigated the mechanism by which glutamine regulates gemcitabine-resistance. A previous study has shown that glutamine is transported into the mitochondria and converted into glutamate via glutaminolysis. It is also involved in GSH synthesis [
11]. We confirmed that glutamine uptake and glutathione levels were increased in gemcitabine-resistant PDAC cells and decreased when SLC38A5 was silenced (Figure 4A and D), suggesting that glutamine transported by SLC38A5 contributes to glutathione synthesis in PDAC cells. Synthesized glutathione regulates intracellular ROS levels by modulating the related genes NRF2 and GPX4. Many studies indicate that reduced ROS levels may also induce gemcitabine-resistance and are characteristic of gemcitabine-resistance [
41,
42]. We also confirmed reduced ROS levels in gemcitabine-resistant PDAC cells (PANC-GR and Capan-GR) using FACS analysis. Conversely, the ROS levels increased when SLC38A5 was inhibited (Figure 4G and Figure S3E).
Several studies have demonstrated that glutamine increases mTOR activity through phosphorylation in cancer cells [
16]. We investigated that phosphoryl-mTOR was downregulated in the glutamine-free medium of gemcitabine-resistant PDAC cells (Figure S3I). We found that phosphoryl-mTOR was upregulated in gemcitabine-resistant PDAC cells compared to that in sensitive cells and was downregulated when SLC38A5 was inhibited (Figure 4J). SREBP1 is known to be involved in fatty acid synthesis and is a downstream target of mTOR [
43]. SREBP1 and SCD1 are inhibitory markers of ferroptosis because they convert polyunsaturated fatty acids (PUFAs), which trigger lipid oxidation, to MUFAs [
33]. We showed that the mTOR-SREBP1-SCD1 pathway was upregulated in gemcitabine-resistant PDAC cells but decreased when SLC38A5 was silenced (Figure 4I and J). Lipid ROS production is known to be mediated by several pathways [
44]. We elucidated the lipid ROS levels through two pathways: the GSH-mediated ROS level and the mTOR pathway. We validated that lipid ROS are downregulated in gemcitabine-resistant PDAC cells compared to gemcitabine-sensitive cells. Furthermore, lipid ROS levels increased when SLC38A5 was silenced (Figure 4K and Figure S3H).
Ferroptosis is a type of cell death triggered by the accumulation of lipid ROS [
18]. Our results indicate that SLC38A5 deletion results in the accumulation of lipid ROS in gemcitabine-resistant PDAC cells. In the present study, we used ferrostatin-1, which inhibits ferroptosis by preventing lipid ROS production. As hypothesized, ferrostatin-1 treatment had the opposite effect on SLC38A5 inhibition in gemcitabine-resistant PDAC cells (Figure 5). Based on our previous results, we showed that suppression of ferroptosis in gemcitabine-resistant PDAC cells was triggered by SLC38A5 inhibition.
In Conclusion, upregulation of SLC38A5 in gemcitabine-resistant PDAC cells increased the viability and invasive ability of gemcitabine-resistant PDAC cells compared to sensitive cells by upregulating glutamine uptake. SLC38A5 significantly reduces ferroptosis through inhibition of lipid ROS accumulation in gemcitabine-resistant PDAC cells. However, SLC38A5 silencing in gemcitabine-resistant PDAC cells reduced cell proliferation and EMT and induced ferroptosis. These mechanistic changes eventually increase the sensitivity of cells resistant to gemcitabine. In summary, we believe that targeting SLC38A5 will significantly contribute to the treatment of patients with gemcitabine-resistant pancreatic cancer and improve their 5-year survival rate.
Supplementary Materials
The following supporting information can be downloaded at: Preprints.org.
Author Contributions
Conceptualization, HJK. and JSP; methodology, MJK, HSK, HWK, DEL, JHC, and HJK; validation, MJK; investigation, MJK; resources, HSK and HJK; data curation, MJK, HSK, DEL and HJK; writing—original draft preparation, MJK, HWK; writing—review and editing, MJK, HWK, and HJK; visualization, X.X.; supervision, HSK; project administration, HJK and JSP; funding acquisition, JSP. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean Government, Ministry of Science and ICT (MSIT) (NRF 2022R1A2C1004141 and NRF 2022R1A2C1091712) and a faculty research grant from Yonsei University College of Medicine (6-2021-0126).
Institutional Review Board Statement
All animal experiments were approved by the animal ethics committee of Yonsei University College of Medicine (approval #2019-0104). The patient study was approved by the Institutional Review Board at Gangnam Severance Hospital, Yonsei University of Korea (3-2014-0153) and complied with the Declaration of Helsinki. Informed consent was obtained from all participants.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The datasets used and analyzed in this paper are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kaur, S.; Baine, M.J.; Jain, M.; Sasson, A.R.; Batra, S.K. Early diagnosis of pancreatic cancer: Challenges and new developments. Biomark Med 2012, 6, 597–612. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.C.; Goggins, M.G.; Fishman, E.K. Diagnosis and detection of pancreatic cancer. Cancer J 2017, 23, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Ansari, D.; Tingstedt, B.; Andersson, B.; Holmquist, F.; Sturesson, C.; Williamsson, C.; Sasor, A.; Borg, D.; Bauden, M.; Andersson, R. Pancreatic cancer: Yesterday, today and tomorrow. Future Oncol 2016, 12, 1929–1946. [Google Scholar] [CrossRef] [PubMed]
- Samanta, K.; Setua, S.; Kumari, S.; Jaggi, M.; Yallapu, M.M.; Chauhan, S.C. Gemcitabine combination nano therapies for pancreatic cancer. Pharmaceutics 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Amrutkar, M.; Gladhaug, I.P. Pancreatic cancer chemoresistance to gemcitabine. Cancers (Basel) 2017, 9. [Google Scholar] [CrossRef]
- Bhutia, Y.D.; Ganapathy, V. Glutamine transporters in mammalian cells and their functions in physiology and cancer. Biochim Biophys Acta 2016, 1863, 2531–2539. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yemanyi, F.; Blomfield, A.K.; Bora, K.; Huang, S.; Liu, C.H.; Britton, W.R.; Cho, S.S.; Tomita, Y.; Fu, Z.; et al. Amino acid transporter slc38a5 regulates developmental and pathological retinal angiogenesis. Elife 2022, 11. [Google Scholar] [CrossRef]
- Sniegowski, T.; Korac, K.; Bhutia, Y.D.; Ganapathy, V. Slc6a14 and slc38a5 drive the glutaminolysis and serine-glycine-one-carbon pathways in cancer. Pharmaceuticals (Basel) 2021, 14. [Google Scholar] [CrossRef]
- Ramachandran, S.; S, R.S.; Sharma, M.; Thangaraju, M.; V, V.S.; Sneigowski, T.; Y, D.B.; Pruitt, K.; Ganapathy, V. Expression and function of slc38a5, an amino acid-coupled na+/h+ exchanger, in triple-negative breast cancer and its relevance to macropinocytosis. Biochem J 2021, 478, 3957–3976. [Google Scholar] [CrossRef]
- Smith, D.K.; Kates, L.; Durinck, S.; Patel, N.; Stawiski, E.W.; Kljavin, N.; Foreman, O.; Sipos, B.; Solloway, M.J.; Allan, B.B.; et al. Elevated serum amino acids induce a subpopulation of alpha cells to initiate pancreatic neuroendocrine tumor formation. Cell Rep Med 2020, 1, 100058. [Google Scholar] [CrossRef]
- Yoo, H.C.; Yu, Y.C.; Sung, Y.; Han, J.M. Glutamine reliance in cell metabolism. Exp Mol Med 2020, 52, 1496–1516. [Google Scholar] [CrossRef] [PubMed]
- Hensley, C.T.; Wasti, A.T.; DeBerardinis, R.J. Glutamine and cancer: Cell biology, physiology, and clinical opportunities. J Clin Invest 2013, 123, 3678–3684. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.C.; Park, S.J.; Nam, M.; Kang, J.; Kim, K.; Yeo, J.H.; Kim, J.K.; Heo, Y.; Lee, H.S.; Lee, M.Y.; et al. A variant of slc1a5 is a mitochondrial glutamine transporter for metabolic reprogramming in cancer cells. Cell Metab 2020, 31, 267–283.e212. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.C. Glutathione synthesis. Biochim Biophys Acta 2013, 1830, 3143–3153. [Google Scholar] [CrossRef]
- Kennedy, L.; Sandhu, J.K.; Harper, M.E.; Cuperlovic-Culf, M. Role of glutathione in cancer: From mechanisms to therapies. Biomolecules 2020, 10. [Google Scholar] [CrossRef]
- Magaway, C.; Kim, E.; Jacinto, E. Targeting mtor and metabolism in cancer: Lessons and innovations. Cells 2019, 8. [Google Scholar] [CrossRef]
- Tesfay, L.; Paul, B.T.; Konstorum, A.; Deng, Z.; Cox, A.O.; Lee, J.; Furdui, C.M.; Hegde, P.; Torti, F.M.; Torti, S.V. Stearoyl-coa desaturase 1 protects ovarian cancer cells from ferroptotic cell death. Cancer Res 2019, 79, 5355–5366. [Google Scholar] [CrossRef]
- Li, J.; Cao, F.; Yin, H.L.; Huang, Z.J.; Lin, Z.T.; Mao, N.; Sun, B.; Wang, G. Ferroptosis: Past, present and future. Cell Death Dis 2020, 11, 88. [Google Scholar] [CrossRef]
- Xu, F.L.; Wu, X.H.; Chen, C.; Wang, K.; Huang, L.Y.; Xia, J.; Liu, Y.; Shan, X.F.; Tang, N. Slc27a5 promotes sorafenib-induced ferroptosis in hepatocellular carcinoma by downregulating glutathione reductase. Cell Death Dis 2023, 14, 22. [Google Scholar] [CrossRef]
- Roh, J.L.; Kim, E.H.; Jang, H.; Shin, D. Nrf2 inhibition reverses the resistance of cisplatin-resistant head and neck cancer cells to artesunate-induced ferroptosis. Redox Biol 2017, 11, 254–262. [Google Scholar] [CrossRef]
- Conrad, M.; Kagan, V.E.; Bayir, H.; Pagnussat, G.C.; Head, B.; Traber, M.G.; Stockwell, B.R. Regulation of lipid peroxidation and ferroptosis in diverse species. Genes Dev 2018, 32, 602–619. [Google Scholar] [CrossRef] [PubMed]
- Nakano, Y.; Tanno, S.; Koizumi, K.; Nishikawa, T.; Nakamura, K.; Minoguchi, M.; Izawa, T.; Mizukami, Y.; Okumura, T.; Kohgo, Y. Gemcitabine chemoresistance and molecular markers associated with gemcitabine transport and metabolism in human pancreatic cancer cells. Br J Cancer 2007, 96, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.D.; Ma, L.; Flagella, M.; Geeganage, S.; Gelbert, L.M.; Slapak, C.A. An increase in the expression of ribonucleotide reductase large subunit 1 is associated with gemcitabine resistance in non-small cell lung cancer cell lines. Cancer Res 2004, 64, 3761–3766. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Zhang, Z.; Li, K.; Gong, L.; Yang, Q.; Huang, X.; Hong, C.; Ding, M.; Yang, H. Linc-dync2h1-4 promotes emt and csc phenotypes by acting as a sponge of mir-145 in pancreatic cancer cells. Cell Death Dis 2017, 8, e2924. [Google Scholar] [CrossRef]
- Funamizu, N.; Honjo, M.; Tamura, K.; Sakamoto, K.; Ogawa, K.; Takada, Y. Micrornas associated with gemcitabine resistance via emt, tme, and drug metabolism in pancreatic cancer. Cancers (Basel) 2023, 15. [Google Scholar] [CrossRef]
- Sun, Y.; Liu, Y.; Ma, X.; Hu, H. The influence of cell cycle regulation on chemotherapy. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef]
- Infantino, V.; Santarsiero, A.; Convertini, P.; Todisco, S.; Iacobazzi, V. Cancer cell metabolism in hypoxia: Role of hif-1 as key regulator and therapeutic target. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef]
- Wu, S.; Zhu, C.; Tang, D.; Dou, Q.P.; Shen, J.; Chen, X. The role of ferroptosis in lung cancer. Biomark Res 2021, 9, 82. [Google Scholar] [CrossRef]
- Xie, Y.; Hou, W.; Song, X.; Yu, Y.; Huang, J.; Sun, X.; Kang, R.; Tang, D. Ferroptosis: Process and function. Cell Death Differ 2016, 23, 369–379. [Google Scholar] [CrossRef]
- Sappington, D.R.; Siegel, E.R.; Hiatt, G.; Desai, A.; Penney, R.B.; Jamshidi-Parsian, A.; Griffin, R.J.; Boysen, G. Glutamine drives glutathione synthesis and contributes to radiation sensitivity of a549 and h460 lung cancer cell lines. Biochim Biophys Acta 2016, 1860, 836–843. [Google Scholar] [CrossRef]
- Sun, Y.; Zheng, Y.; Wang, C.; Liu, Y. Glutathione depletion induces ferroptosis, autophagy, and premature cell senescence in retinal pigment epithelial cells. Cell Death Dis 2018, 9, 753. [Google Scholar] [CrossRef] [PubMed]
- Shimano, H.; Sato, R. Srebp-regulated lipid metabolism: Convergent physiology - divergent pathophysiology. Nat Rev Endocrinol 2017, 13, 710–730. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.; Zhu, J.; Wu, J.; Thompson, C.B.; Jiang, X. Oncogenic activation of pi3k-akt-mtor signaling suppresses ferroptosis via srebp-mediated lipogenesis. Proc Natl Acad Sci U S A 2020, 117, 31189–31197. [Google Scholar] [CrossRef] [PubMed]
- Wattanawongdon, W.; Hahnvajanawong, C.; Namwat, N.; Kanchanawat, S.; Boonmars, T.; Jearanaikoon, P.; Leelayuwat, C.; Techasen, A.; Seubwai, W. Establishment and characterization of gemcitabine-resistant human cholangiocarcinoma cell lines with multidrug resistance and enhanced invasiveness. Int J Oncol 2015, 47, 398–410. [Google Scholar] [CrossRef]
- Jia, Y.; Xie, J. Promising molecular mechanisms responsible for gemcitabine resistance in cancer. Genes Dis 2015, 2, 299–306. [Google Scholar] [CrossRef]
- Zilka, O.; Shah, R.; Li, B.; Friedmann Angeli, J.P.; Griesser, M.; Conrad, M.; Pratt, D.A. On the mechanism of cytoprotection by ferrostatin-1 and liproxstatin-1 and the role of lipid peroxidation in ferroptotic cell death. ACS Cent Sci 2017, 3, 232–243. [Google Scholar] [CrossRef]
- Martín-Saiz, L.; Guerrero-Mauvecin, J.; Martín-Sanchez, D.; Fresnedo, O.; Gómez, M.J.; Carrasco, S.; Cannata-Ortiz, P.; Ortiz, A.; Fernandez, J.A.; Sanz, A.B. Ferrostatin-1 modulates dysregulated kidney lipids in acute kidney injury. J Pathol 2022, 257, 285–299. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Gaduputi, V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J Oncol 2019, 10, 10–27. [Google Scholar] [CrossRef]
- Grasso, C.; Jansen, G.; Giovannetti, E. Drug resistance in pancreatic cancer: Impact of altered energy metabolism. Crit Rev Oncol Hematol 2017, 114, 139–152. [Google Scholar] [CrossRef]
- Cha, Y.J.; Kim, E.S.; Koo, J.S. Amino acid transporters and glutamine metabolism in breast cancer. Int J Mol Sci 2018, 19. [Google Scholar] [CrossRef]
- Yang, Q.; Li, K.; Huang, X.; Zhao, C.; Mei, Y.; Li, X.; Jiao, L.; Yang, H. Lncrna slc7a11-as1 promotes chemoresistance by blocking scf(β-trcp)-mediated degradation of nrf2 in pancreatic cancer. Mol Ther Nucleic Acids 2020, 19, 974–985. [Google Scholar] [CrossRef] [PubMed]
- Xue, D.; Zhou, X.; Qiu, J. Emerging role of nrf2 in ros-mediated tumor chemoresistance. Biomedicine & Pharmacotherapy 2020, 131, 110676. [Google Scholar] [CrossRef]
- Porstmann, T.; Santos, C.R.; Griffiths, B.; Cully, M.; Wu, M.; Leevers, S.; Griffiths, J.R.; Chung, Y.L.; Schulze, A. Srebp activity is regulated by mtorc1 and contributes to akt-dependent cell growth. Cell Metab 2008, 8, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Kang, R.; Tang, D. Ferroptosis by lipid peroxidation: The tip of the iceberg? Front Cell Dev Biol 2021, 9, 646890. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).