2.1. Case Presentation
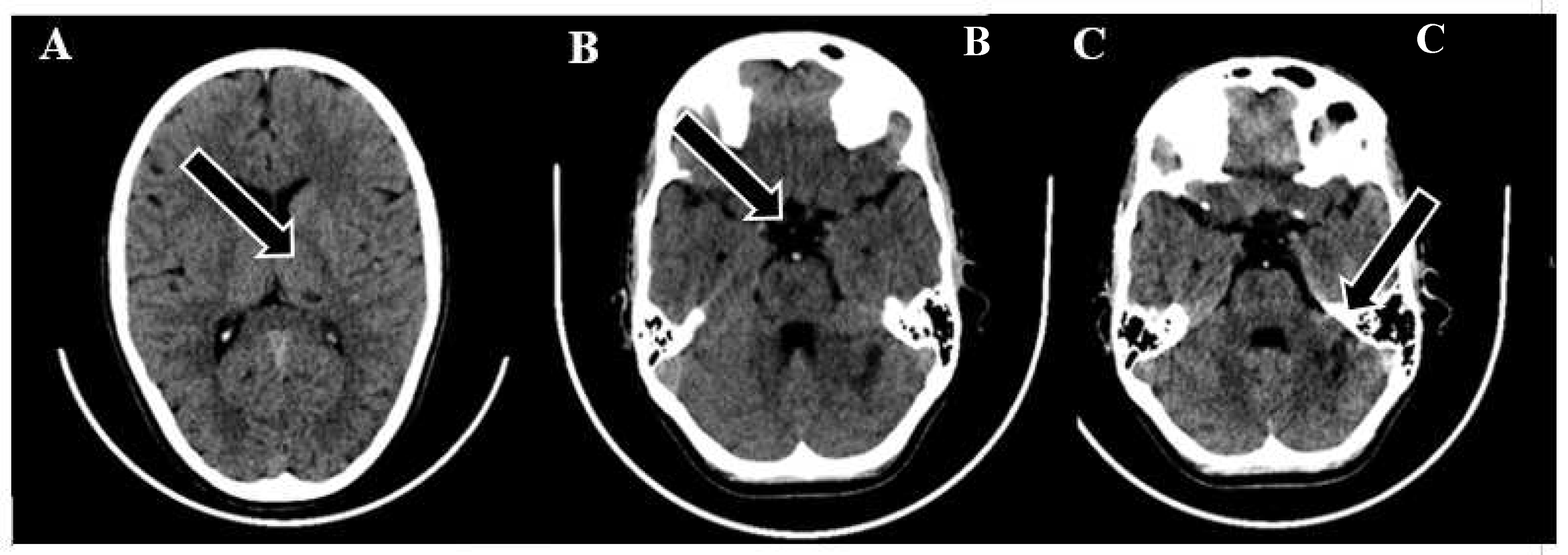
A 9-year-old male was admitted to a regional hospital due to a persistent complaint of diarrhea, exceeding ten episodes in two days, accompanied by a single episode of vomiting, tension headache, and mild vertigo. Initial diagnostic assessments did not reveal any notable abnormalities, leading to a diagnosis of gastroenteritis. Following rehydration therapy, the patient's overall condition improved, and discharge plans were being considered. However, on the subsequent day after admission, at approximately 16:00, the patient suddenly experienced weakness localized to the left side of his body. Recognizing the urgency of the situation, an emergency consultation with a neurologist was promptly arranged. Two hours following the onset of these new symptoms, a computed tomography (CT) scan of the brain was conducted, which did not show any acute changes in the brain. Nevertheless, the CT scan did reveal two hypodense regions in the left cerebellum, which raised suspicion of malignancy, along with a hyperdense appearance of the basilar artery (BA). Additionally, a hypodense region was noted in the left thalamic region, suggesting a potential prior lacunar stroke.
Figure 1.
Emergency CT scan of the brain. (A) hypodense region in the left thalamic region; (B) hyperdense basilar artery (HDBA) sign; (C) 2 hypodense regions in the left cerebellum.
Figure 1.
Emergency CT scan of the brain. (A) hypodense region in the left thalamic region; (B) hyperdense basilar artery (HDBA) sign; (C) 2 hypodense regions in the left cerebellum.
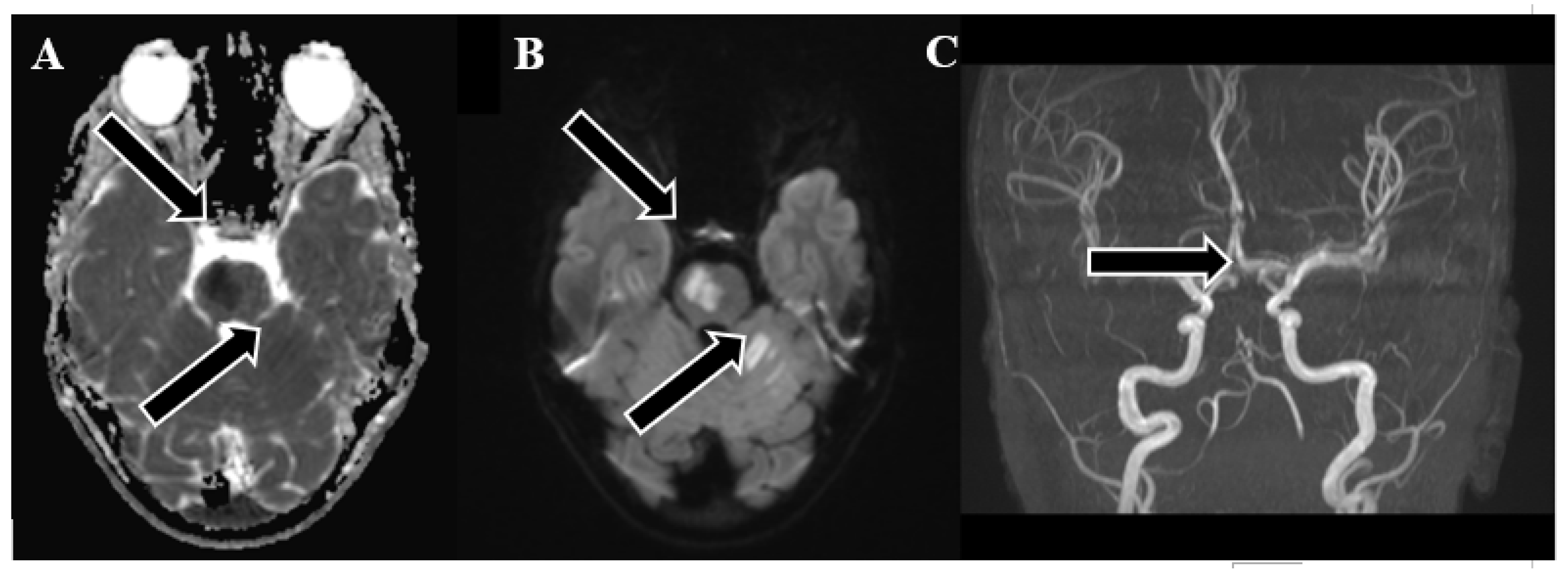
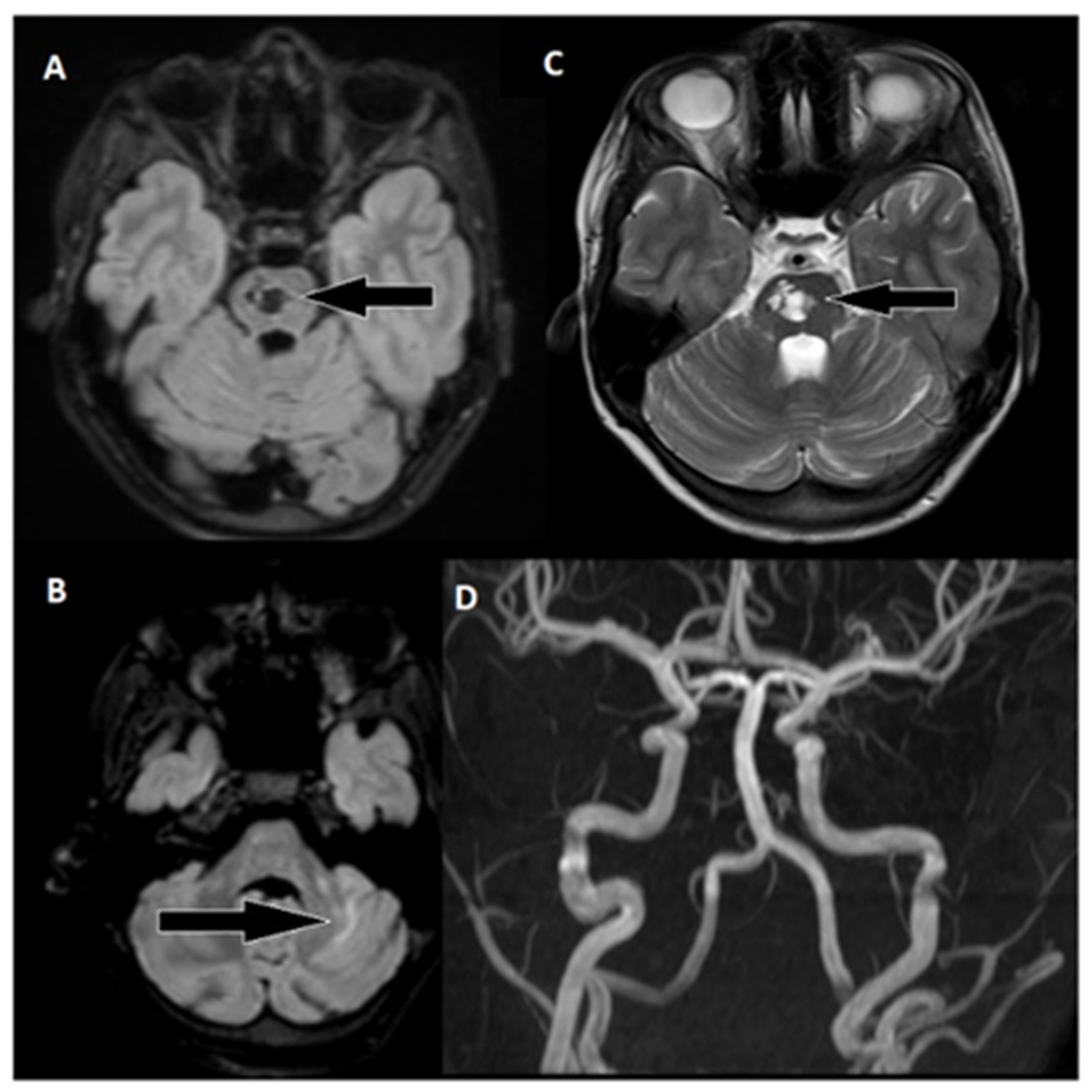
Following 3.5 hours and in consultation with a pediatric specialist, the decision was made to transfer the patient to the Children's Clinical University Hospital for a more comprehensive diagnostic assessment. An emergency magnetic resonance imaging (MRI) was conducted, revealing acute ischemia within the vascularization area supplied by the left posterior inferior cerebellar artery (PICA). Moreover, this MRI also indicated involvement in regions supplied by the left anterior inferior cerebellar artery (AICA) and superior cerebellar artery (SCA). The magnetic resonance angiography (MRA) performed concurrently showed evidence of a thrombus causing occlusion in the distal one-third of the basilar artery (BA). This comprehensive imaging assessment illuminated the extent of the vascular compromise and provided critical information for further evaluation and treatment planning.
Figure 2.
Emergency magnetic resonance imaging (MRI) before intervention. (A) Changes in the ADC map seen in the left PICA, as well as slightly in the AICA and SCA regions; (B) diffusion-weighted images showing acute changes in the left PICA, as well as slightly in the AICA and SCA regions; (C) MRA showing stop of flow in the distal 1/3 of the basilar artery.
Figure 2.
Emergency magnetic resonance imaging (MRI) before intervention. (A) Changes in the ADC map seen in the left PICA, as well as slightly in the AICA and SCA regions; (B) diffusion-weighted images showing acute changes in the left PICA, as well as slightly in the AICA and SCA regions; (C) MRA showing stop of flow in the distal 1/3 of the basilar artery.
Although the MRI revealed significant brain damage, as evidenced by positive findings on FLAIR (fluid-attenuated inversion recovery) and DWI (diffusion-weighted imaging), and despite the elapsed time of approximately 8.5 hours from the onset of symptoms, a collaborative decision involving a team of medical specialists including a pediatrician, radiologist, strokologist, and interventional radiologist was made to proceed with Endovascular Treatment (EVT) as the patient was deemed ineligible for intravenous thrombolysis due to the exceeding of the time window. This decision was reached despite the limited experience with pediatric strokes, underlining the urgency of the situation.
Subsequently, three hours after the MRI, the patient was transferred to Pauls Stradins Clinical University Hospital, a comprehensive stroke center. Upon admission, the patient displayed a Glasgow Coma Scale (GCS) score of 15 but presented with left-sided hemiparesis, as assessed by the National Institutes of Health Stroke Scale (NIHSS), which recorded a score of 6. The left arm and leg exhibited no effort against gravity. Vital signs at admission were as follows: blood pressure at 106/75 mmHg, heart rate at 80 beats per minute, oxygen saturation (SpO2) at 100%, respiratory rate (RR) at 18 breaths per minute, and a body temperature of +37.6°C. The patient was expeditiously transferred to the EVT suite for immediate intervention.
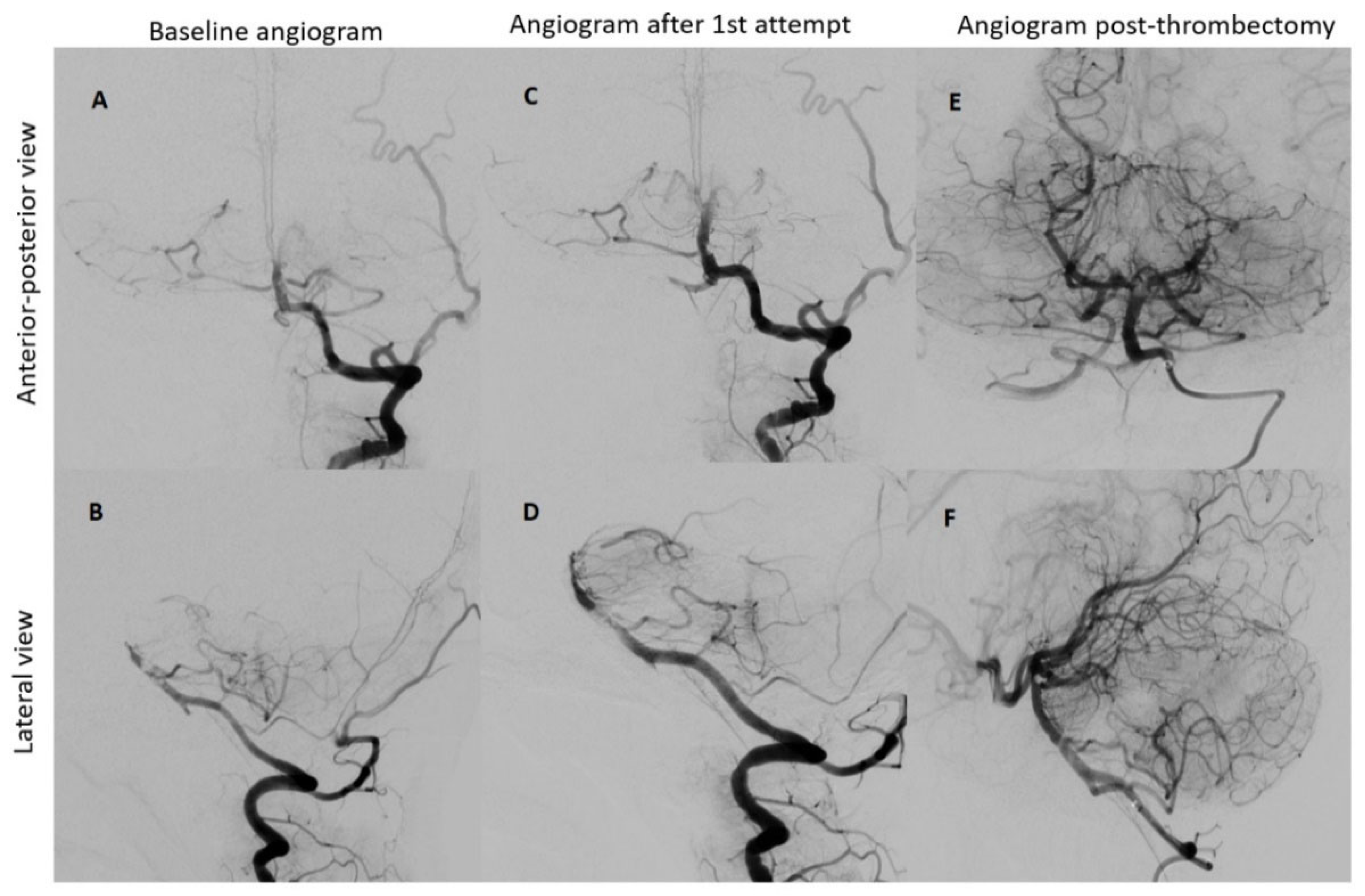
2.2. Interventional Procedure
Under the administration of general anesthesia, a retrograde puncture was performed in the right common femoral artery, utilizing a 5F sheath. Subsequent to this, a left vertebral angiogram was conducted, revealing a significant blockage in the upper third of the basilar artery. This obstruction resulted in an absence of contrast in both posterior cerebral arteries, which was graded as Thrombolysis in cerebral infarction (TICI) scale score of 0, indicating minimal to no blood flow.
To restore normal blood flow to the affected areas, an aspiration catheter known as "Sofia" was carefully positioned in the distal V2 segment. Throughout the procedure, multiple left vertebral arteriograms were performed, consistently illustrating blockages in the middle segment of the basilar artery. After six meticulous attempts, a final angiogram conclusively confirmed the complete removal of the obstructions in both the basilar artery and the posterior cerebral arteries, achieving a TICI scale score of 3, indicating full and successful revascularization.
Following the procedure, manual compression was applied to the puncture site, and the thrombectomy process, which lasted for a duration of 60 minutes, concluded without any complications or adverse events.
Figure 3.
Neurointerventional procedure. (A, B) Initial angiogram from anterior-posterior and lateral views reveals an upper third basilar artery occlusion and no enhancement in both posterior cerebral arteries (TICI scale: 0). (C, D) After the first attempt, angiogram views show improved basilar artery enhancement, but filling defects and absent enhancement persist in both posterior cerebral arteries. (E, F) Post-thrombectomy angiograms demonstrate enhanced perfusion in the basilar artery and both posterior cerebral arteries (TICI scale: 3).
Figure 3.
Neurointerventional procedure. (A, B) Initial angiogram from anterior-posterior and lateral views reveals an upper third basilar artery occlusion and no enhancement in both posterior cerebral arteries (TICI scale: 0). (C, D) After the first attempt, angiogram views show improved basilar artery enhancement, but filling defects and absent enhancement persist in both posterior cerebral arteries. (E, F) Post-thrombectomy angiograms demonstrate enhanced perfusion in the basilar artery and both posterior cerebral arteries (TICI scale: 3).
2.3. Outcome and Follow-Up
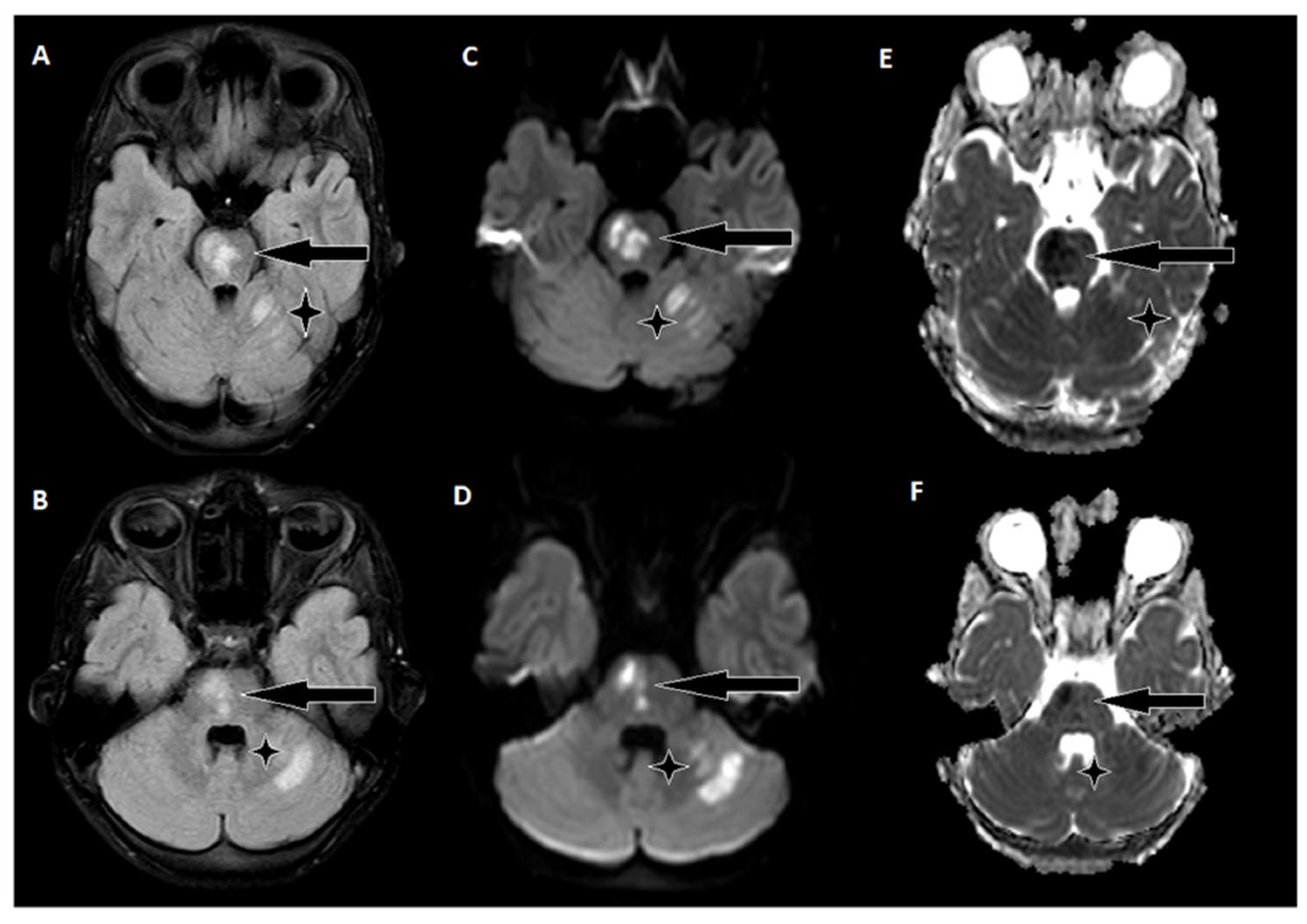
The day following EVT, an MRI of the brain was conducted, revealing hyperintense regions on the right side of the pons and the upper left cerebellum. Importantly, there were no indications of hemorrhagic imbibition, which was reassuring. In terms of treatment, the patient commenced a secondary stroke prevention regimen, consisting of Acetylsalicylic Acid at a daily dose of 75 mg. Additionally, low-weight molecular heparin was initiated, administered twice daily to further mitigate the risk of complications. Just one day after the EVT procedure, the patient embarked on early rehabilitation, overseen by a team of physiotherapists and occupational therapists. Remarkably, the post-procedure period progressed without any significant complications, and the patient was transferred back to the Children's Clinical University Hospital for continued evaluation and rehabilitation. At the time of transfer, the patient's neurological status was characterized by plegia in the left arm and severe paresis in the left leg, with the latter exhibiting no voluntary effort against gravity. The patient's GCS score was recorded as 14, and the NIHSS indicated a score of 8.
Figure 4.
A follow-up brain MRI conducted two days after thrombectomy. (A, B) In the FLAIR sequence, hyperintense areas on the right side of the pons and upper left cerebellum. (C, D) Corresponding hyperintensities on diffusion-weighted images. (E, F) Hypointensities on the ADC map, indicate acute ischemic stroke changes.
Figure 4.
A follow-up brain MRI conducted two days after thrombectomy. (A, B) In the FLAIR sequence, hyperintense areas on the right side of the pons and upper left cerebellum. (C, D) Corresponding hyperintensities on diffusion-weighted images. (E, F) Hypointensities on the ADC map, indicate acute ischemic stroke changes.
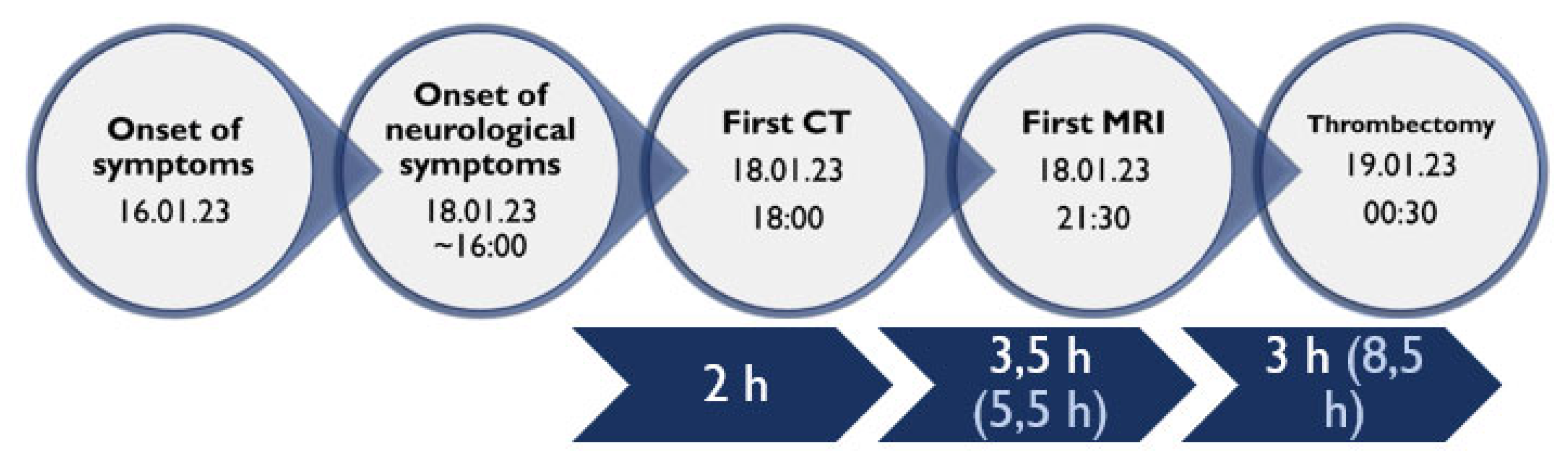
Figure 5.
Timeline of clinical and procedural data.
Figure 5.
Timeline of clinical and procedural data.
The patient's family history did not reveal any pertinent chronic illnesses, heart diseases, or strokes. Furthermore, extensive investigations aimed at uncovering the etiology of the stroke yielded no significant factors. These investigations encompassed thorough assessments, including examinations for thrombophilia gene mutations and vascular malformation panels, as well as evaluations of immunodeficiency, immunology, and infectious diseases. Holter monitoring, employed to detect heart rhythm irregularities, did not reveal any abnormalities. Additionally, transesophageal echocardiography ruled out the presence of interatrial shunts and the potential for a paradoxical embolism originating from the heart. In an effort to explore potential genetic factors, the patient was consulted by a geneticist, and a comprehensive exome analysis was conducted. Regrettably, this analysis did not identify any significant genetic mutations associated with the stroke. Despite the rigorous and meticulous investigative efforts, the precise origin of the stroke remains unknown.
Throughout the patient's hospitalization, a continuous rehabilitation regimen was implemented. After approximately three weeks, the patient was discharged and transferred to a specialized rehabilitation facility. At the time of discharge, there was notable improvement in the patient's overall neurological status. The patient demonstrated limited arm movement against gravity and slight left-sided leg drift. Neurologically, the patient achieved a GCS score of 15, a NIHSS score of 3, and a mRS score of 3.
During the six-month follow-up, the patient exhibited a complete neurological recovery, as evidenced by an NIHSS score of 0 and an mRS score of 0. An MRI scan conducted at this time revealed scarring with hypointense areas on the right pons in the FLAIR sequence. Importantly, magnetic resonance angiography (MRA) confirmed unobstructed flow in the basilar artery. This positive outcome marked a significant milestone in the patient's journey toward recovery and underlined the remarkable resilience of the young patient in overcoming the challenges posed by this enigmatic stroke.
Figure 5.
Follow-up MRI of the brain approximately 6 months after thrombectomy. (A) Markedly hypointense areas on the right side of the pons in the FLAIR sequence, indicating scarring. Corresponding hyperintense changes are observed on: (C) T2 weighted images, with a distinct hyperintense area on the right side of the pons (arrow). (B) Changes in the upper part of the left cerebellar hemisphere are visible in the FLAIR sequence. (D) An MRA examination shows unobstructed flow in the basilar artery and both cerebral posterior arteries.
Figure 5.
Follow-up MRI of the brain approximately 6 months after thrombectomy. (A) Markedly hypointense areas on the right side of the pons in the FLAIR sequence, indicating scarring. Corresponding hyperintense changes are observed on: (C) T2 weighted images, with a distinct hyperintense area on the right side of the pons (arrow). (B) Changes in the upper part of the left cerebellar hemisphere are visible in the FLAIR sequence. (D) An MRA examination shows unobstructed flow in the basilar artery and both cerebral posterior arteries.