1. Introduction
Firefighter-rescuers are particularly vulnerable to high levels of anxiety and stress as a result of attending incidents where their health and lives may be at risk. Stress is inherent in the work of a firefighter [
1]. Cortisol is an essential mediator between psychological states and health-related outcomes. As the end product of the hypothalamic-pituitary-adrenal (HPA) axis, cortisol helps to regulate the stress response [
2]. Perceiving a stressor induces the release of corticotropin-releasing hormone (CRH) from the paraventricular nucleus (PVN) in the hypothalamus [
3]. CRH then triggers adrenocorticotropin hormone (ACTH) secretion from the pituitary gland into the bloodstream. ACTH binds to receptors in the adrenal cortex that stimulate the secretion of cortisol [
3]. This stress response system optimally regulates stress when a quick onset is required, followed by a swift termination once a threat has passed [
2,
3]. Short-term psychological stress provides the stimulus for the 'fight or flight response' and adaptive hormonal responses to maintain systemic homeostasis, while excessive or chronic stress, through elevated cortisol, can have maladaptive, widespread effects on health [
2]. Cortisol has been shown to have an adverse effect on hippocampal and prefrontal cortex neurons, which in turn leads to altered memory and cognitive functioning [
4]. Cortisol may also intensify age-related neurodegenerative processes in the brain [
4]. Growing evidence indicates that the pathological manifestations of chronic stress include neuronal and synaptic atrophy/malfunction, as well as immunosuppression [
4]. Glucocorticoids can have adverse effects on hippocampal and prefrontal neurons, leading to a reduction in the volume of these structures, and dysfunction in them enhances HPA axis activity [
5]. In addition, both stress and exogenous glucocorticoids induce behavioural changes that are mainly characteristic of depression and anxiety disorders [
6]. In helping a person who is burdened by excessive anxiety the focus should be on balancing the activity of the autonomic nervous system, reducing muscle tension and lowering the level of perceived stress [
7].
Attention is increasingly being paid to techniques associated with a holistic approach, which means that body and mind should be taken into consideration equally [
8]. In Norway, for example, craniosacral therapy has been used as a complementary method for treating people with trauma [
8]. What is specific to the cranial area of osteopathy is the extension of osteopathic principles to the cranial sphere and the synchronisation with micro-movements in the tissue and speculative tissue rhythms [
9].
Osteopathy in the cranial sphere was developed in the early 1930s by the osteopathic physicians W. G. Sutherland and C. Weaver [
9]. The aim of craniosacral therapy is to reduce tension in the cranium, pelvis, diaphragm, thorax and sacrum, which in turn leads to relaxing the connective tissue structures, in which tension is usually the cause of health problems [
8]. Craniosacral therapy is also used to reduce chronic tension-type headaches [
10]. Craniosacral therapy is effective for treating pain in patients experiencing neck and back pain, migraine, fibromyalgia, epicondylitis, and pelvic pain [
10]. The efficiency of cranial treatments has also been demonstrated in the treatment of premature infants [
11]. Another study showed the influence of the CV-4 technique in autonomic-related parameters such as heart rate, blood pressure, blood flow velocity, electroencephalography alpha power and muscle sympathetic nerve activity [
12]. Current evidence demonstrating the effectiveness of craniosacral therapy in reducing stress is promising [
13]. It has also been shown that a single OMT session of approximately 20 minutes with a light touch on the craniosacral body regions led to a faster recovery of the heart rate and sympathovagal balance in healthy participants and prevented the typical rise in cortisol levels after a psychological stressor [
14].
The aim of our study was to evaluate the effectiveness of craniosacral therapy on levels serum cortisol and CRH as objective indicators of HPA axis activity.in healthy men (fire service cadets).
Before proceeding with the study, the following research hypothesis was defined:
The groups analyzed, i.e., CS - Craniosacral group and CO - Control group, are statistically significantly different, and the values of Cortisol (C) and CRH (Corticotropin-Releasing Hormone) levels are statistically significantly different between the research group (CS - Craniosacral) and the control group (CO - Control Group) before and after the study.
2. Materials and Methods
2.1. Participants
Fifty-seven firefighter cadets aged 18– 24 (21.63 ± 1.41), with a mean Body Mass Index of 24.44 ± 3.05 kg/m2, volunteered to participate in the study. These were only men, as circulating cortisol levels have been shown to be influenced by gender (in particular, the phase of the menstrual cycle in women) [
15]. Participants in the study were recruited through meetings held at the fire academy, posters and leaflets, and they also received comprehensive information about the study project. Those interested in participating in the study were interviewed to check the inclusion and exclusion criteria. Inclusion criteria were male gender and being a fire academy cadet. The exclusion criteria were physiotherapeutic or osteopathic therapy applied now or in the past, daily cigarette smoking, alcohol abuse, caffeine use (>300mg/day), medication, drug use, reported medical illness, and the following types of disorders: endocrine, cardiovascular disease and psychiatric.
2.2. Randomization
To assign participants to groups, a block randomization was performed using an Excel file. First, a block was generated to assign sample numbers equally to each group. The block size was randomly generated (2-, 4- or 6-letter combinations of A and B). Following this, each block was assigned to a group. Each participant was provided with a printed number in order that the therapist could not predict which treatment placebo or craniosacral therapy) would be performed until the participant came.
2.3. Cortisol and CRH assessment
All blood samples were taken at the beginning of the study and at the end of the study, i.e. after five weeks by a qualified nurse in the doctor's office at the Fire Cadet School after a 10-12 h overnight rest (sleep). Blood samples (15 mL) were obtained between 7:00 and 9:00 a.m. from the antecubital vein, Vacutainer tubes were used; the cadet had blood drawn in a sitting position.
Blood was distributed in one tube with gel and a clot activator (10 mL) to obtain serum. Serum was stored at -80° C until analysis. All laboratory measurements are conducted by medical laboratory scientist. Cortisol levels were measured using an Eagle Biosciences Cortisol ELISA (enzyme-linked immunosorbent assay) kit (cat. DCM020-9) from DiaMetra (Perugia, Italy). CRH levels were measured using an ELISA Kit for Corticotropin-Releasing Hormone (cat. SEC935Hu) from Cloud Clone Corp. (Katy, TX, USA). All the samples from each part of the experiment (pre/post) were analysed with the same ELISA kit (one kit enables 90 samples to be analysed), the assay sensitivity was 0.8 nmol/L, and the inter-and intraassay variation coefficients were all below 10%.
2.4. Therapeutic techniques of craniosacral therapy
Before performing craniosacral therapy, all participants in the study group (CS – Craniosacral group) (N = 30) were introduced to the therapy. The therapy sessions took place in a quiet and warm room, and were held once a week for five consecutive weeks from 9.30 a.m. to 1 p.m. by the same therapist. Participants lay in a supine position on a couch, and the therapy was conducted each time by the therapist herself, according to a set methodology. In this study, we used a structural approach to craniosacral therapy. The therapist used craniosacral therapy (sacrum compression and traction, AO - Atlanto-occipital joint, mobilization of the frontal bone, parietal bones, sphenoid bone and temporal bones), and the final step was the CV4 technique - for a full description of the procedure see: [
16,
17].
Participants in the no-intervention group (CO - control group) (N = 27) did not receive any therapy. In this group, the therapist only held the subject's head (while the cadet was in a supinated position) and did not use her hands to apply any techniques). The therapy time for individual subjects in both groups was 20 min. None of the 57 subjects had received osteopathic or physiotherapeutic therapy prior to the study, and the subjects had no prior knowledge or experience of osteopathic craniosacral treatments.
2.5. Statistical analysis
For the purpose of this research, statistical analysis was performed using R ver. 4.2.2 software [
18]. Both the craniosacral therapy experimental group and the control group were analysed. The values of cortisol and CRH levels in the CS and CO groups are presented as descriptive statistics before and after the research. As the data do not follow a normal distribution, the non-parametric Kruskal-Wallis test to see if these groups are statistically significantly different, and the Wilxocon test and Dunn test with Bonferroni adjustment to see which groups are statistically significantly different. The results were also presented as boxplots.
3. Results
After data collection, statistical analysis was performed using the R package [
18]. First, descriptive statistics were determined for the values of cortisol (
Table 1) and CRH -corticotropin-releasing hormone (
Table 2) in the CS and CO groups before and after the study.
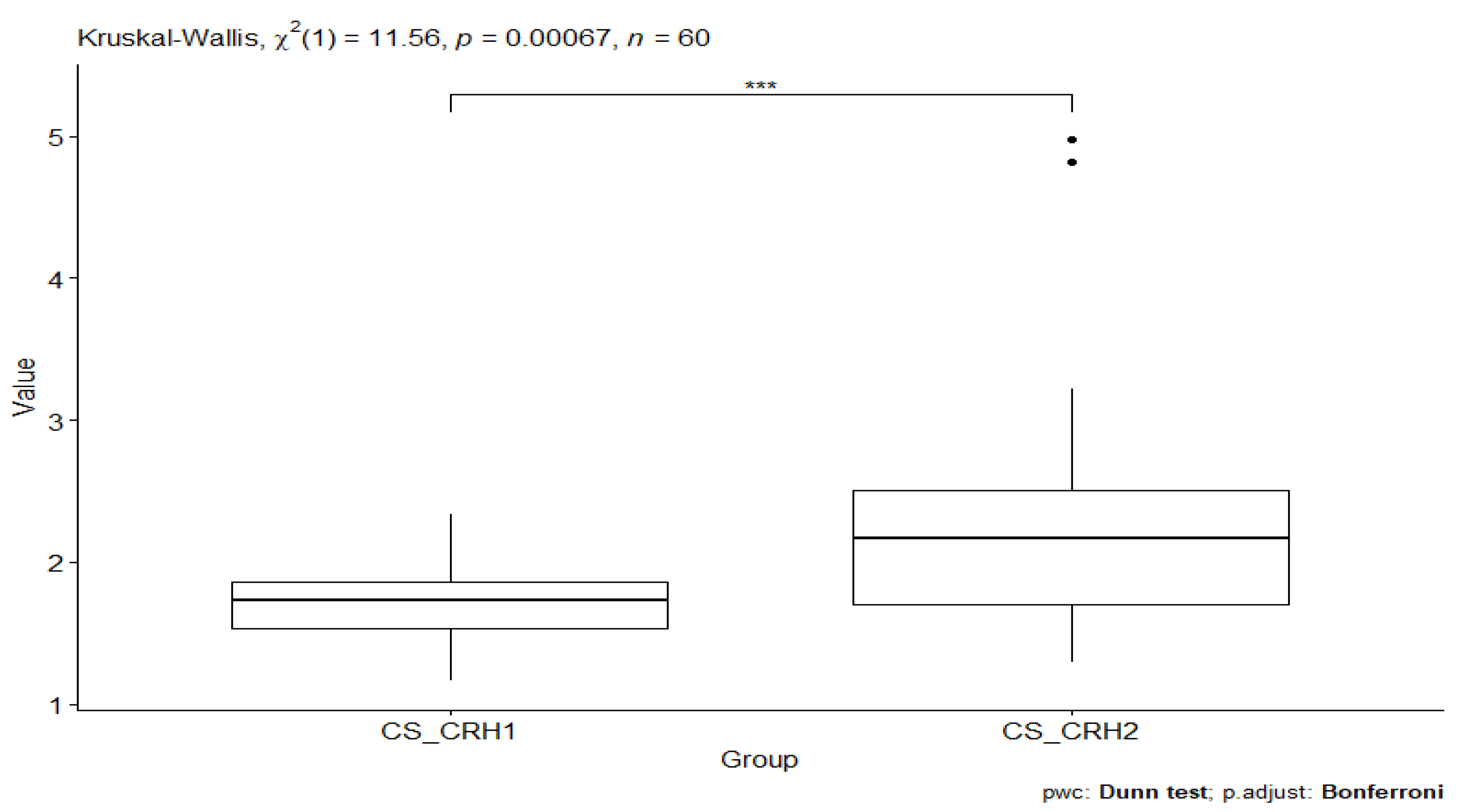
Further statistical analysis was performed using the Kruskal-Wallis test to check whether the groups being analysed were statistically different. The result obtained from the analysis of the CS_CRH1 and CS_CRH2 groups indicates the presence of statistical significance, p-value = 0.00067 (
Figure 1).
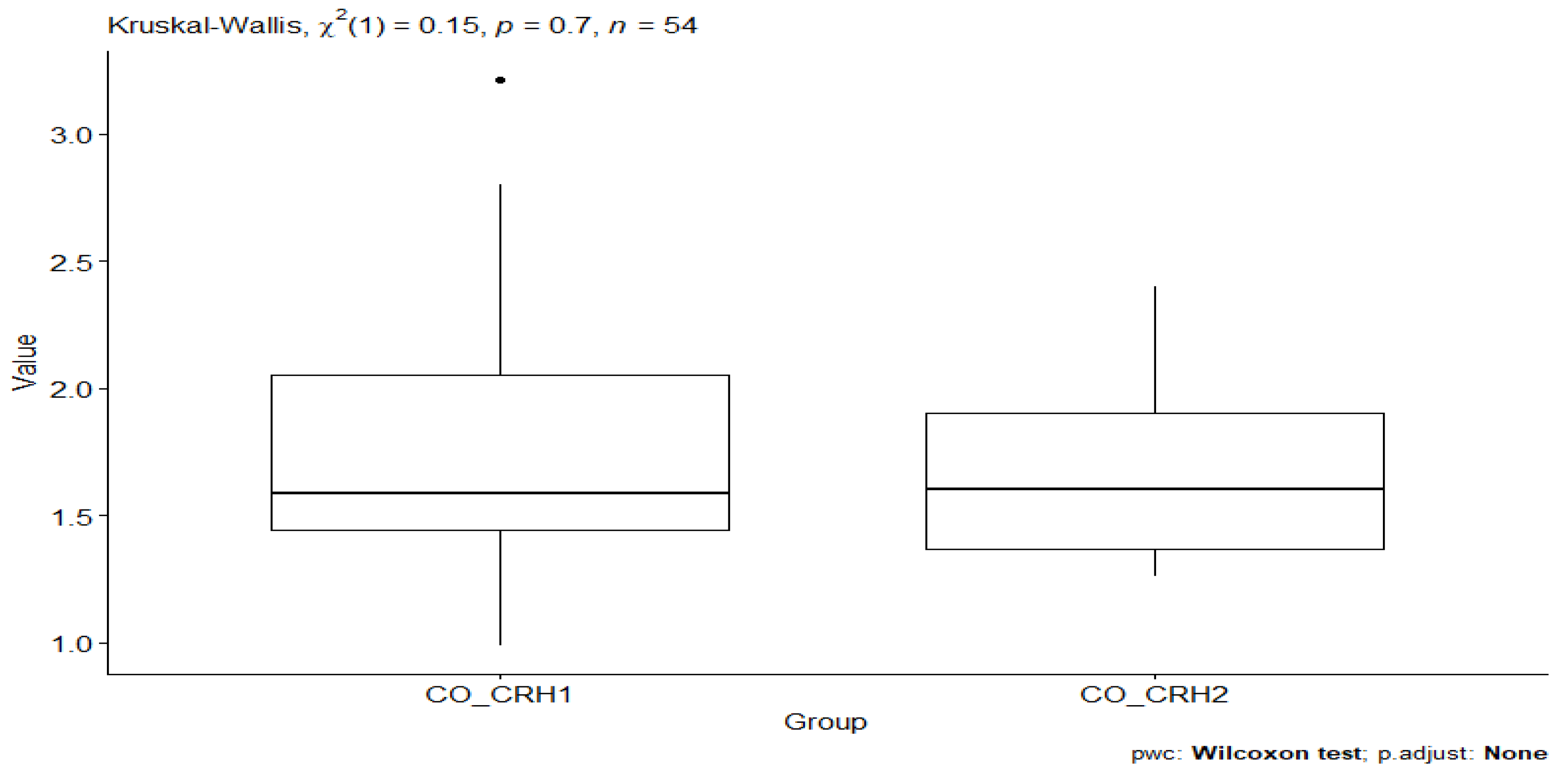
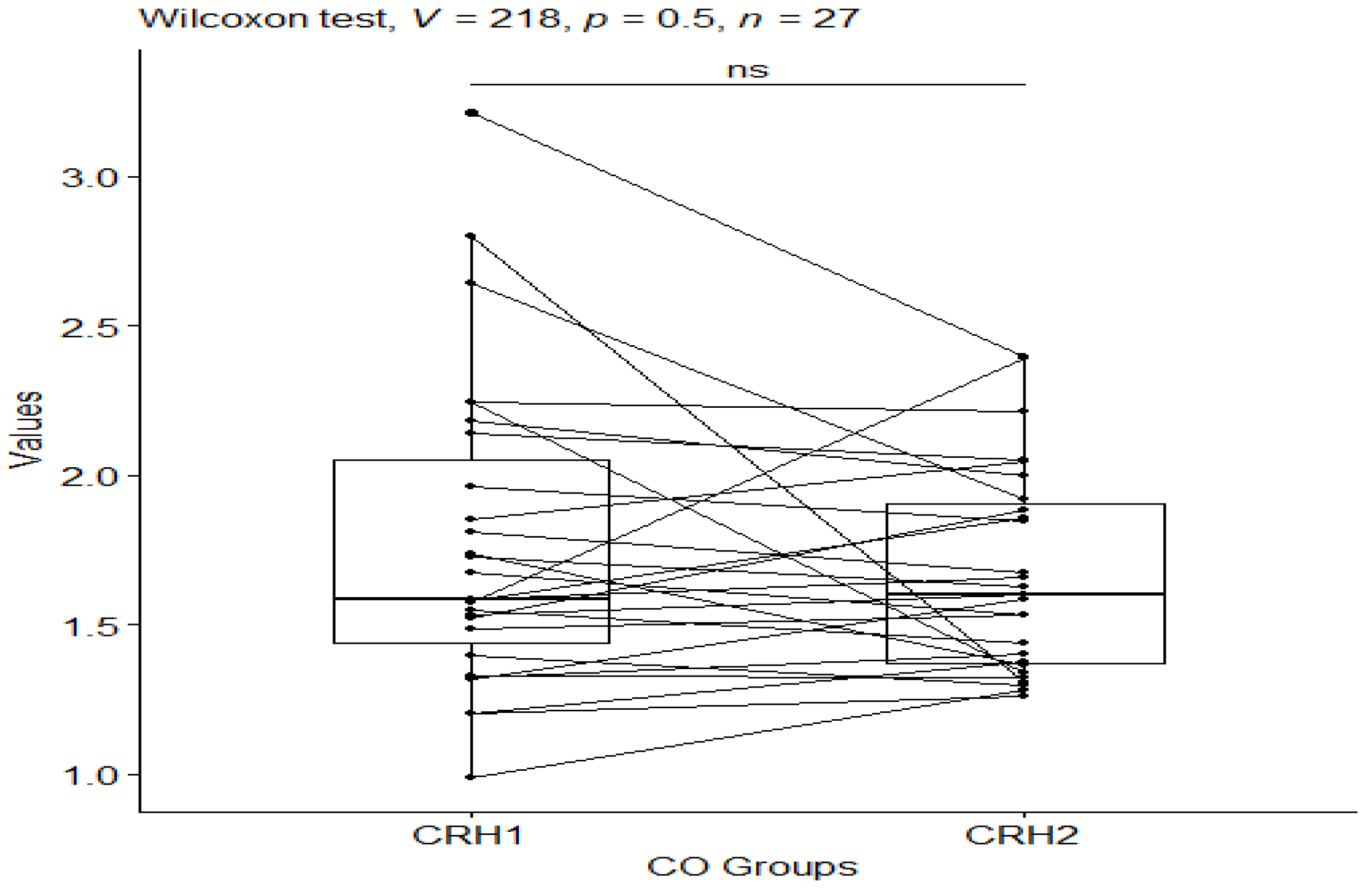
However, comparing CO_CRH1 (CRH value in the control group before testing) and CO_CRH2 (CRH value in the control group after testing) groups, no statistical significance was observed between the groups p-value=0.7. (
Figure 2).
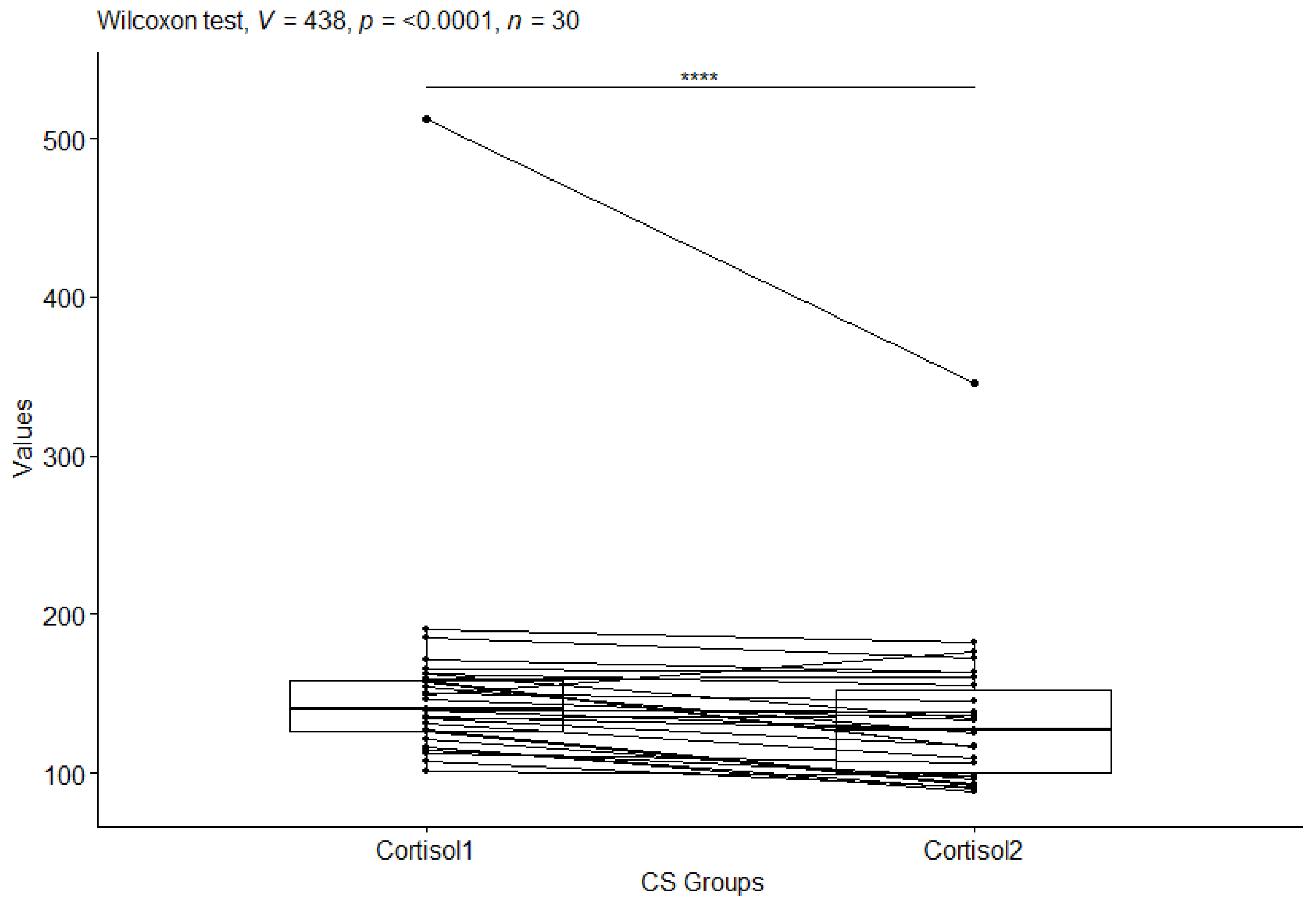
The next step in the statistical analysis was to determine which groups were statistically significantly different, for the CS group before and after the study and for the CO group before and after the study. For this purpose, the Wilxocon test was used. For cortisol (cortisol) values in the craniosacral group, a statistical significance of p-value=<0.0001 was observed (
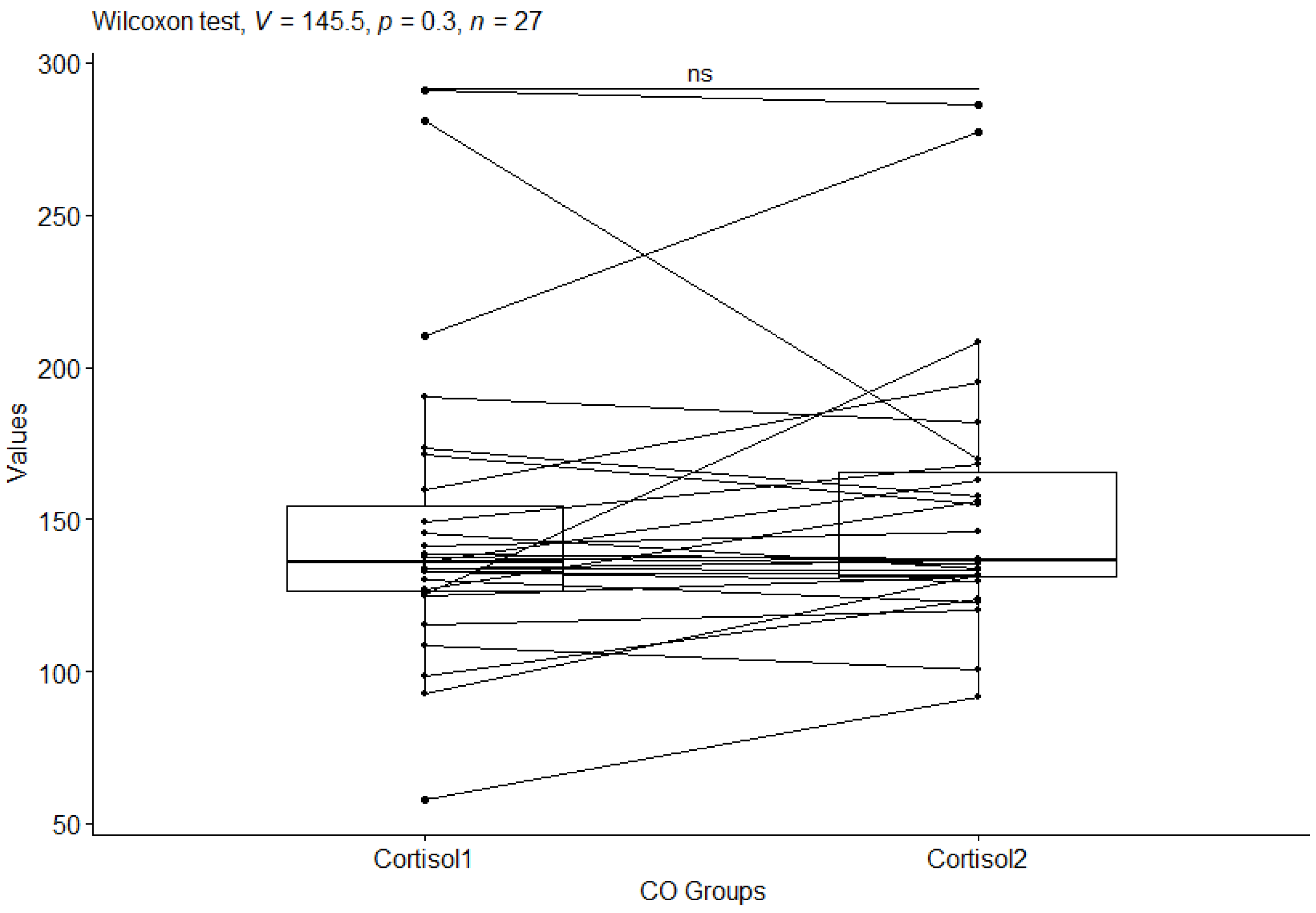
Figure 3), while no statistical significance of p-value=0.3 was observed in the control group (
Figure 4).
The Wilcoxon test was also applied to check which groups differed statistically significantly for the CS group before and after testing, and for the CO group before and after testing for CRH (corticotropin-releasing hormone) values. For the CRH values in the CS group, a statistical significance of p-value=<0.0001 was observed (
Figure 5), while no statistical significance of p-value=0.5 was observed in the control group (
Figure 6).
The next step in the statistical analysis was to see which of more than two groups were statistically different for cortisol and CRH (corticotropin-releasing hormone) values. For this purpose, the Dunn test with Bonferroni adjustment was used.
Statistical significance was obtained for cortisol values between the craniosacral and control groups. Statistical significance was obtained for cortisol level between the CCO2 and CCS2 groups p=0.0377 (
Table 3). In contrast, there is no statistical significance for cortisol level between groups: CCO1 and CCO2, CCO1 and CCS1, CCO1 and CCS2, CCO2 and CCS1, and CCS1 and CCS2.
For CRH, statistical significance was obtained between (
Table 4): CO_CRH1 and CS_CRH2 p=0.00634; CO_CRH2 and CS_CRH2 p=0.000887; CS_CRH1 and CS_CRH2 p=0.0101. In contrast, there is no statistical significance between (
Table 4) groups: CO_CRH1 and CO_CRH2, CO_CRH1 and CS_CRH1, CO_CRH2 and CS_CRH1.
4. Discussion
The current study was designed to evaluate whether craniosacral therapy might be helpful in reducing stress in male firefighter cadets. Our study demonstrated that craniosacral therapy significantly affected the serum cortisol level and CRH participants with therapy. Although manual therapies-manual techniques are offered chiefly for chronic tension musculoskeletal system, some studies have recommended the use of this therapeutic modality for increasing patients’ general well-being [
19]. A prospective study by Edwards et al. showed that osteopathic therapy can indeed be an effective intervention in reducing perceived stress as well as improving mental health outcomes [
20]. Fornari et al. also showed that osteopathic manipulative therapy can improve the effects of conventional therapy for stress [
13]. This treatment modality can also induce a relaxation response. For example, Girsberger et al. demonstrated the effect of craniosacral techniques on reducing autonomic nervous system tension [
21].
Systemic cortisol is among the most widely used biomarkers of acute and chronic stress [
22]. Cortisol contributes to maintaining glucose homeostasis and the cardiovascular system. It is released in a non-specific manner during stressful events. The amygdala, which plays a role in processing the severity of stress, sends a response to the hypothalamus if the threat deems it necessary [
23]. The hypothalamus then activates the sympathetic nervous system responsible for the fight or flight response.
The main function of CRH is to stimulate pituitary synthesis [
24]. To being produced in the hypothalamus, CRH is also synthesised in peripheral tissues – in particular, the immune system - such as acting in opposition to cortisol, namely stimulating the immunological response [
25]. CRH is the origin and main driver of the HPA axis; this guarantees that the body has the appropriate stress responses and maintains a heightened state of alertness [
7].
The chronic stress associated with it induces pro-inflammatory changes that are directly linked to the hypothalamic-pituitary axis (HPA), thereby increasing the risk of excessive systemic inflammation [
26]. Stress also has an impact on the sympathomedullo-adrenal (SMA) axis. This pathway involves the release of cytokines such as C-reactive protein (CRP), an acute-phase protein released from the liver that increases its response following interleukin-6 (IL-6) secretion. IL-6 is an important pro-inflammatory cytokine. CRP is a sensitive marker in systemic inflammation, and chronically elevated values are an independent risk factor for cardiovascular disease in both children and adults [
27].
The firefighting profession is fraught with the incidence of diseases like hypertension and heart attack [
28]. Cardiac death is the most common cause of duty-related death among firefighters [
29]. Our own research has shown a positive effect of craniosacral therapy on heart rhythm parameters, indicating a reduction in the excitability of the autonomic system [
30]. Firefighters are usually exposed to traumatic events while performing their professional duties, putting them at risk of developing post-traumatic stress disorder and depression [
28,
31].
The incidence of cardiovascular disease and its disability-related effects carries a high financial cost [
32]. Prevention appears to be the cheapest form of treatment. Therefore, it seems reasonable to look for non-invasive methods to influence the reduction of stress hormones. Our research shows that craniosacral therapy can be such a method.
A very good prevention of cardiovascular disease is physical activity, which firefighters, by virtue of their profession, should have a high level of [
33]. Firefighters are also exposed to heat stress, which is associated with cerebral oxygenation and vascular hemodynamics, and, in turn, can affect cognitive decline [
34]. In the firefighting profession, the development of physical fatigue, which can limit the performance of professional activities, also plays an important role [
35]. Stress-induced fatigue can affect neuronal activation patterns, altering them and slowing down simple mental operations [
36].
It is very important to prepare an algorithm for general monitoring and coaching systems for firefighters to improve their resilience to stress and reduce risks in their professional activities [
37]. The firefighting profession is fraught with the following: high level of stress [
38], physical risk, chemical risk, mechanical hazard, and psychosocial risk [
39].
Limitations
The relatively small size, convenience and homogeneity of the sample limit the generalizations that can be made from this study. The intervention was delivered by one practitioner, which might enhance the observed effect of craniosacral therapy. Moreover, we did not consider female participants, so the results can refer only to men. When considering female participants, such variables as menstrual cycle phase, using contraception and pregnancy/lactation period should be taken into account.
5. Conclusions
The results obtained indicate that craniosacral therapy has an impact on lowering the values of the stress hormones cortisol and CRH. This method may be an effective and non-invasive way to reduce stress in firefighting cadets.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used: Conceptualization, M.W; B.B.; I.S.; and E.Ż.; methodology, M.W; B.B.; I.S.; and E.Ż.; software, M.W and I.S.; validation, M.W and I.S.; formal analysis, M.W.; I.S.; and E.Ż.; investigation, M.W; B.B.; I.S.; E.Ż.; resources, M.W; B.B.; I.S.; and E.Ż.; data curation, M.W; B.B.; I.S.; and E.Ż.; writing—original draft preparation, M.W; B.B.; I.S.; and E.Ż.; writing—review and editing, M.W; B.B.; I.S.; and E.Ż.; visualization, M.W; B.B.; I.S.; and E.Ż.; supervision, M.W; B.B.; I.S.; and E.Ż.; project administration, M.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Bioethics Committee of Nicolaus Copernicus University in Toruń based at Collegium Medicum in Bydgoszcz (permit no. KB/99/2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is available from the corresponding author.
Acknowledgments
We would like to thank those who took part in this study, and Dr. Inga Dziembowska.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lebeaut, A.;Tran, J.K.; Vujanovic, A.A. Posttraumatic stress, alcohol use severity, and alcohol use motives among firefighters: The role of anxiety sensitivity. Addictive Behaviors. 2020;106:106353. [CrossRef]
- Herman, J.P.; McKlveen, J.M.; Ghosal, S.; Kopp, B.; Wulsin, A.; Makinson, R.; Scheimann, J.; Myers, B. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Comprehensive Physiology. 2016,6(2):603–621. [CrossRef]
- Herman, J.P.; Tasker, J.G: Paraventricular Hypothalamic Mechanisms of Chronic Stress Adaptation. Frontiers in Endocrinology (Lausanne). 2016;7:137. [CrossRef]
- Ouanes, S.; Popp, J. High Cortisol and the Risk of Dementia and Alzheimer’s Disease: A Review of the Literature. Frontiers Aging Neuroscience. 2019;11:43. [CrossRef]
- Wellman, C.L.; Moench, K.M. Preclinical studies of stress, extinction, and prefrontal cortex: intriguing leads and pressing questions. Psychopharmacology (Berl). 2019;236(1):59–72. [CrossRef]
- Mayer, S.E.; Lopez-Duran, N.L.; Sen, S.; Abelson, J.L. Chronic stress, hair cortisol and depression: A prospective and longitudinal study of medical internship. Psychoneuroendocrinology. 2018;92:57–65. [CrossRef]
- Denkova, E.; Zanesco, A.P.; Rogers, S.L.; Jha, A.P. Is resilience trainable? An initial study comparing mindfulness and relaxation training in firefighters. Psychiatry Research. 2020;285:112794. [CrossRef]
- Stub, T.; Kiil, M.A.; Lie, B.; Kristoffersen, A.E.; Weiss, T.; Hervik, J.B.; Musial, F. Combining psychotherapy with craniosacral therapy for severe traumatised patients: A qualitative study from an outpatient clinic in Norway. Complementary Therapies in Medicine. 2020;49:102320. [CrossRef]
- Liem, T. Kraniosakrale Osteopathie. Thieme. 2018;7:pp.35,39. (In German]).
- Haller, H.; Lauche, R.; Sundberg, T.; Dobos, G.; Cramer, H. Craniosacral therapy for chronic pain: a systematic review and meta-analysis of randomised controlled trials. BMC Musculoskeletal Disordes. 2019;21(1):1. [CrossRef]
- Cerritelli, F.; Pizzolorusso, G.; Renzetti, C.; Cozzolino, V.; D'Orazio, M.; Lupacchini, M.; Marinelli, B.; Accorsi, A.; Lucci, Ch.; Lancellotti, J.; Ballabio, S.; Castelli, C.; Molteni, D.; Besana, R.; Tubaldi, L.; Perri, F.P.; Fusilli, P.; D'Incecco, C.; Barlafante, G. A PO-0616 A Multicenter, Randomised, Controlled Trial Of Osteopathic Manipulative Treatment On Preterm Infants. PLoS One. 2015;10(5):1–12. [CrossRef]
- Miana, L.; do Vale Bastos, V.H.; Machado, S.; Arias-Carrión, O.; Nardi, E.G.; Almeida, L.; Ribeiro, P.; Machado, D.; King, H.; Silva, J.G. Changes in alpha band activity associated with application of the compression of fourth ventricular (CV-4) osteopathic procedure: a qEEG pilot study. Journal of Bodywork and Movement Therapies. 2013;17(3):291–296. [CrossRef]
- Fornari, M.; Carnevali, L.; Sgoifo, A. Single Osteopathic Manipulative Therapy Session Dampens Acute Autonomic and Neuroendocrine Responses to Mental Stress in Healthy Male Participants. J Am Osteopath Assoc. 2017;117(9):559-567. [CrossRef]
- Hamidovic, A.; Karapetyan, K.; Serdarević, F.; Choi, S.H.; Eisenlohr-Moul, T.A.; Pinna, G. Higher Circulating Cortisol in the Follicular vs. Luteal Phase of the Menstrual Cycle: A Meta-Analysis. Frontiers in Endocrinology. 2020;1:311. [CrossRef]
- Stephens, M.A.C.; Mahon, P.B.; McCaul, M.E.; Wand, G.S. Hypothalamic-pituitary-adrenal axis response to acute psychosocial stress: Effects of biological sex and circulating sex hormones. Psychoneuroendocrinology. 2016;66:47–55. [CrossRef]
- Liem, T. Cranial Osteopathy. Eastland Press: Oxford, England. 2009; pp. 320–345.
- Liem, T. Praxis de Kraniosakralen Osteopathie. Thieme: Stuttgart, Deutschland. 2019; pp. 21–25. (In German).
-
R Development Core Team. A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna. Austria. 2020. Available at: http://www.r-project.org (Accessed: 09 August 2023).
- King, H.H. Manual Craniosacral Therapy May Reduce Symptoms of Migraine Headache. The Journal of the American Osteopathic Association. 2017;117(1):59. [CrossRef]
- Edwards, D.J.; Toutt, C. An evaluation of osteopathic treatment on psychological outcomes with patients suffering from chronic pain: A prospective observational cohort study collected through a health and well-being academy. Health Psychology Open. 2018;5(1): 2055102918774684. [CrossRef]
- Girsberger, W.; Bänziger, U.; Lingg, G.; Lothaller, H.; Endler, P.C. Heart rate variability and the influence of craniosacral therapy on autonomous nervous system regulation in persons with subjective discomforts: a pilot study. Journal of Integrative Medicine. 2014;12(3):156–161. [CrossRef]
- Lee, D.Y.; Kim, E.; Choi, M.H. Technical and clinical aspects of cortisol as a biochemical marker of chronic stress. BMB Reports. 2015;48(4):209–216. [CrossRef]
- Hakamata, Y.; Komi, S.; Moriguchi, Y.; Izawa, S.; Motomura, Y.; Sato, E.; Mizukami, S.; Kim, Y.; Hanakawa, T.; Inoue, Y.; Tagaya, H. Amygdala-centred functional connectivity affects daily cortisol concentrations: a putative link with anxiety. Sci Rep. 2017;7(1):8313. [CrossRef]
- Kim, J.S.; Han, S.Y.; Iremonger, K.J. Stress experience and hormone feedback tune distinct components of hypothalamic CRH neuron activity. Nature Communications. 2019;10(1):5696. [CrossRef]
- Quintanar, J.L.; Guzmán-Soto, I. Hypothalamic neurohormones and immune responses. Frontiers in Integrative Neuroscience. 2013;7:56. [CrossRef]
- Mehta, D.; Binder, E.B. Gene environment vulnerability factors for PTSD: The HPA-axis. Neuropharmacology. 2012;62:654–662. [CrossRef]
- Coehoorn, C.J.; Neary, J.P.; Krigolson, O.E.; Service, T.W.; Stuart-Hill, L.A. Firefighter salivary cortisol responses following rapid heat stress. J Therm Biol. 2022;108:103305. [CrossRef]
- Van Hasselt, V.B.; Bourke, M.L.; Schuhmann, B.B. Firefighter Stress and Mental Health: Introduction to the Special Issue. Behav Modif. 2022;46(2):259-266. [CrossRef]
- Mathias, K.C.; Bode, E.D.; Stewart, D.F.; Smith, D.L. Changes in Firefighter Weight and Cardiovascular Disease Risk Factors over Five Years. Med Sci Sports Exerc. 2020;52(11):2476-2482. [CrossRef]
- Wójcik, M.; Siatkowski, I. The effect of cranial techniques on the heart rate variability response to psychological stress test in firefighter cadets. Scientific Reports. 2023;13:7780. [CrossRef]
- Obuobi-Donkor, G.; Oluwasina, F.; Nkire, N.; Agyapong, V.I.O. A Scoping Review on the Prevalence and Determinants of Post-Traumatic Stress Disorder among Military Personnel and Firefighters: Implications for Public Policy and Practice. Int J Environ Res Public Health. 2022;19(3):1565. [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Economic Burden of Cardiovascular Disease in Type 2 Diabetes: A Systematic Review. Value Health. 2018;21(7):881-890. [CrossRef]
- Ras, J.; Smith, D.L.; Soteriades, E.S.; Kengne, A.P.; Leach, L. A Pilot Study on the Relationship between Cardiovascular Health, Musculoskeletal Health, Physical Fitness and Occupational Performance in Firefighters. Eur J Investig Health Psychol Educ. 2022;12(11):1703-1718. [CrossRef]
- Coehoorn, C.J.; Neary, P.J.; Krigolson, O.E.; Stuart-Hill, L.A. Firefighter pre-frontal cortex oxygenation and hemodynamics during rapid heat stress. Brain Res. 2023;1798:148156. [CrossRef]
- Bustos, D.; Cardoso, F.; Rios, M.; Vaz, M.; Guedes, J.; Costa, J.T.; Baptista, J.S.; Fernandes, R.J. Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters. Sensors (Basel). 2022;23(1):194. [CrossRef]
- Tornero-Aguilera, J.F.; Jimenez-Morcillo, J.; Rubio-Zarapuz, A.; Clemente-Suárez, V.J. Central and Peripheral Fatigue in Physical Exercise Explained: A Narrative Review. Int J Environ Res Public Health. 2022;19(7):3909. [CrossRef]
- Buecher, J.; Soujon, M.; Sierro, N.; Weiss, J.; Michel, B. Firefighter Stress Monitoring: Model Quality and Explainability. Annu Int Conf IEEE Eng Med Biol Soc. 2022;2022:4653-4657. [CrossRef]
- Sawhney, G.; Jennings, K.S.; Britt, T.W.; Sliter, M.T. Occupational stress and mental health symptoms: Examining the moderating effect of work recovery strategies in firefighters. J Occup Health Psychol. 2018;23(3):443-456. [CrossRef]
- Cuenca-Lozano, M.F.; Ramírez-García, C.O. Occupational Hazards in Firefighting: Systematic Literature Review. Saf Health Work. 2023;14(1):1-9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).