Submitted:
02 September 2023
Posted:
20 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
3. Diagnostic steps to perform before running mp-US
4. Mp-US methodological standards
Scrotal/testicular color-Doppler ultrasonography (CDUS)
Contrast-enhanced US (CEUS)
Sonoelastography (SE)
5. Non-neoplastic testicular lesions
5.1. Intratesticular cysts
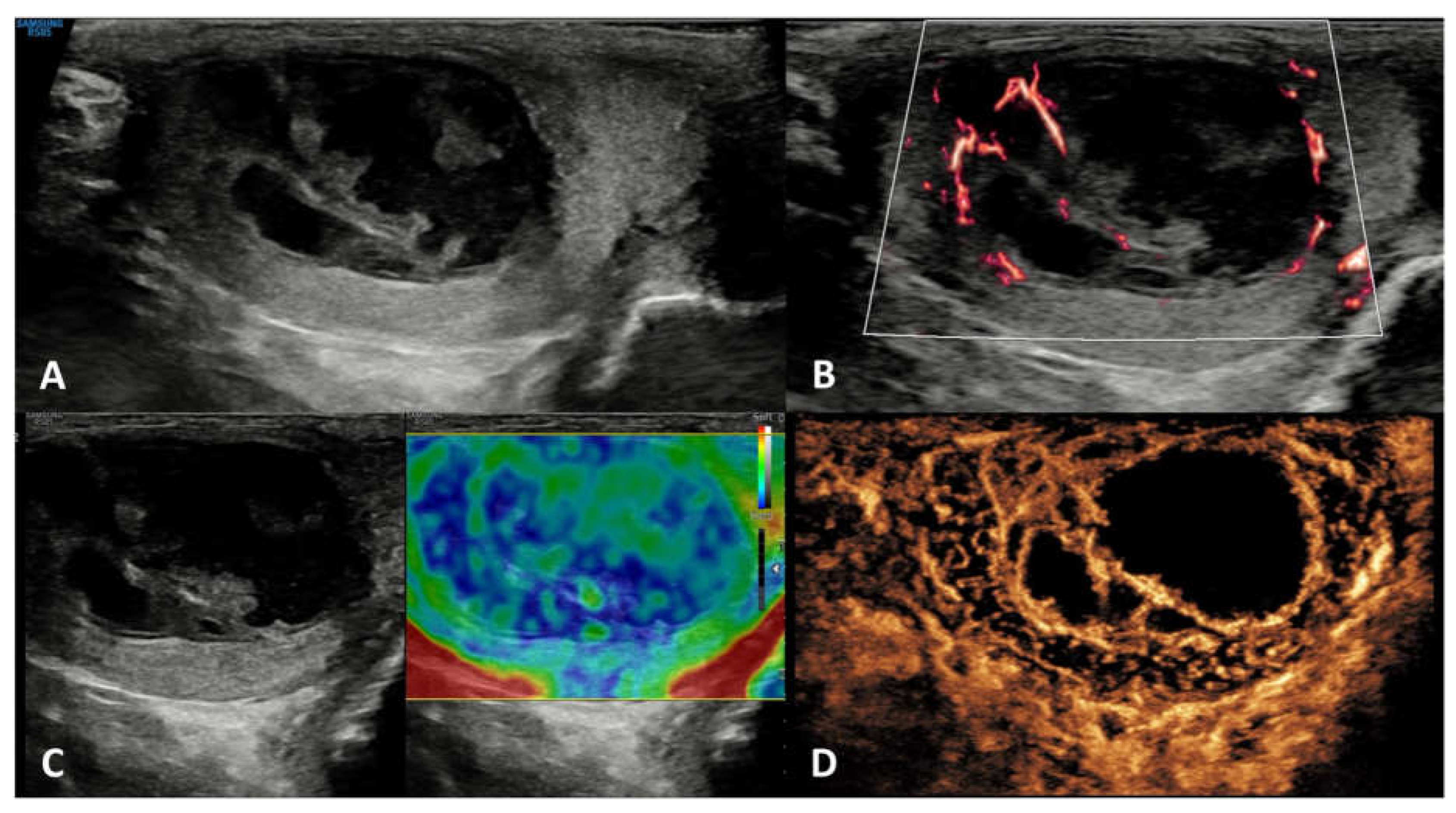
5.2. Epidermoid cysts
5.3. Testicular Adrenal Rest Tumors (TARTs)
5.4. Sarcoidosis
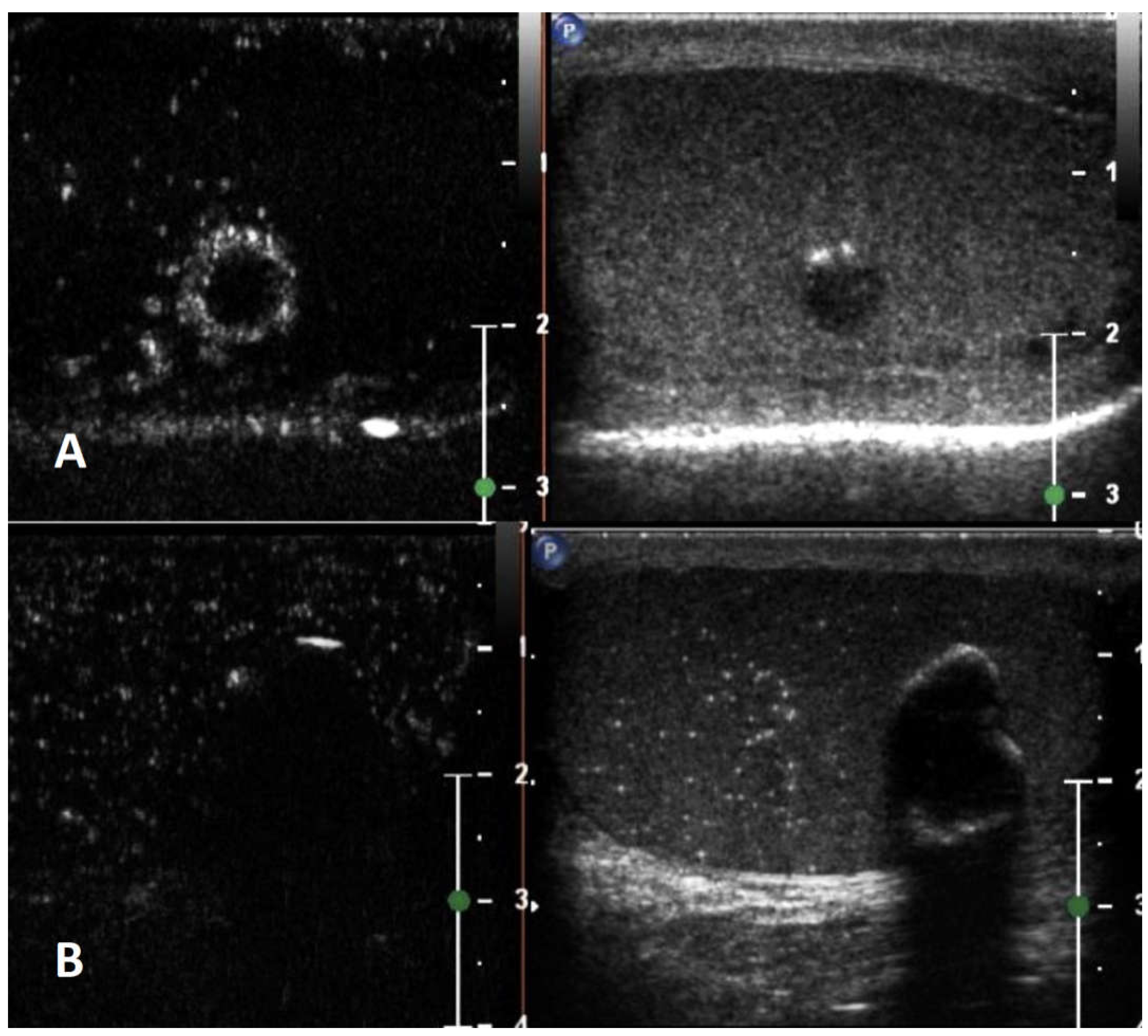
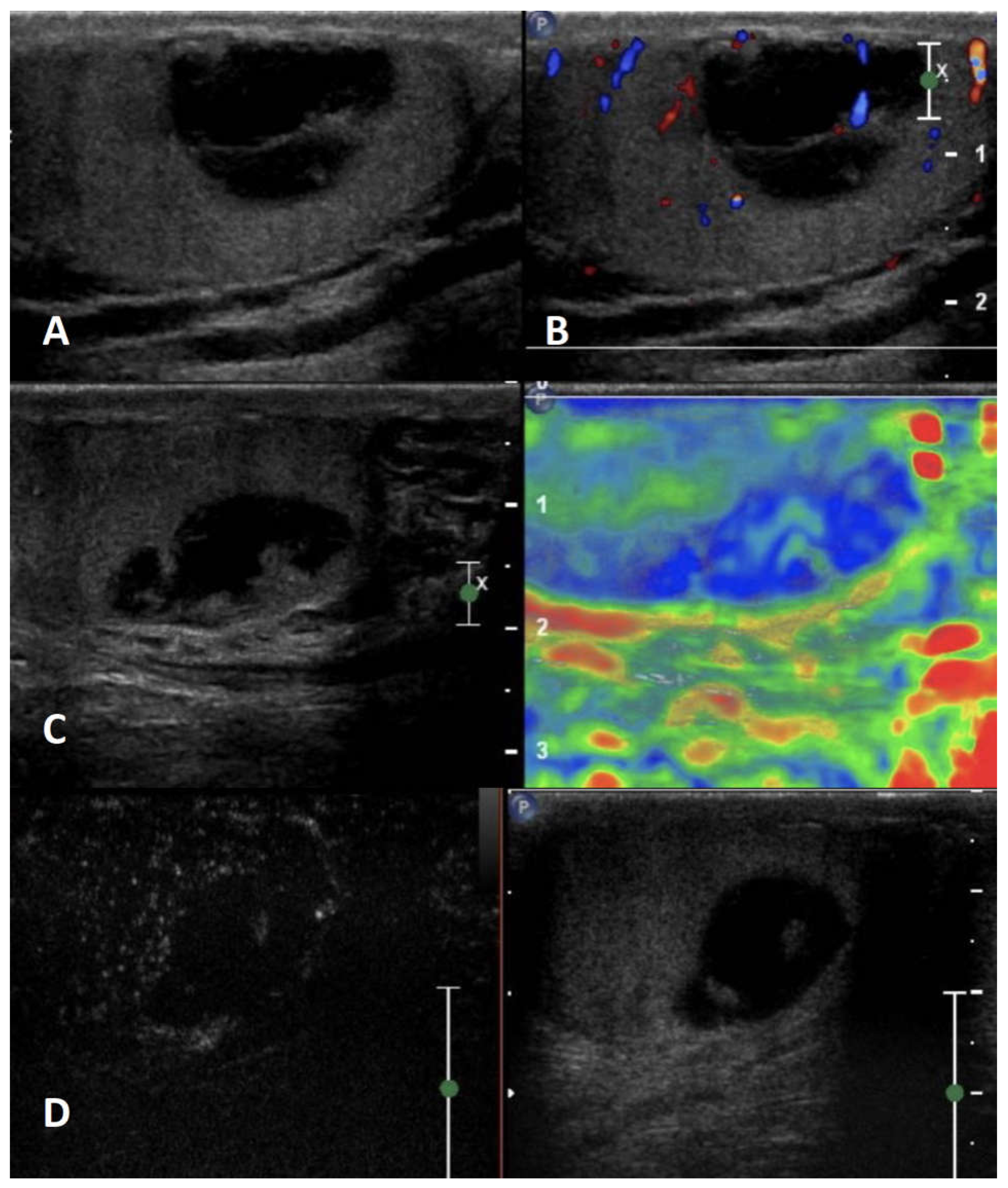
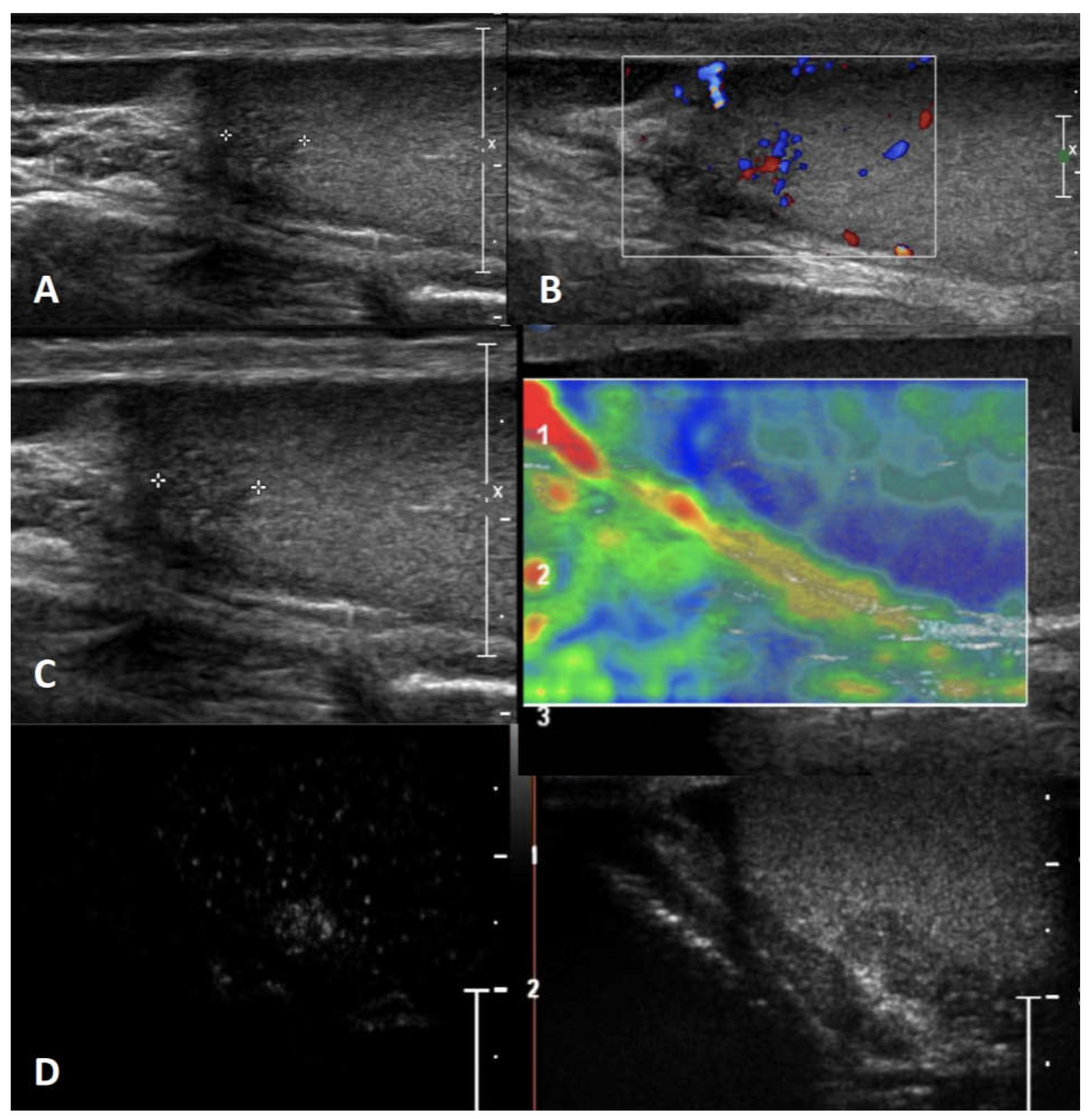
5.5. Segmental testicular infarction
5.6. Abscess
5.7. Hematoma
5.8. Viral orchitis and bacterial orchitis (epididymo-orchitis)
5.9. Idiopathic granulomatous orchitis
5.10. Infectious granulomatous orchitis
6. Neoplastic testicular lesions
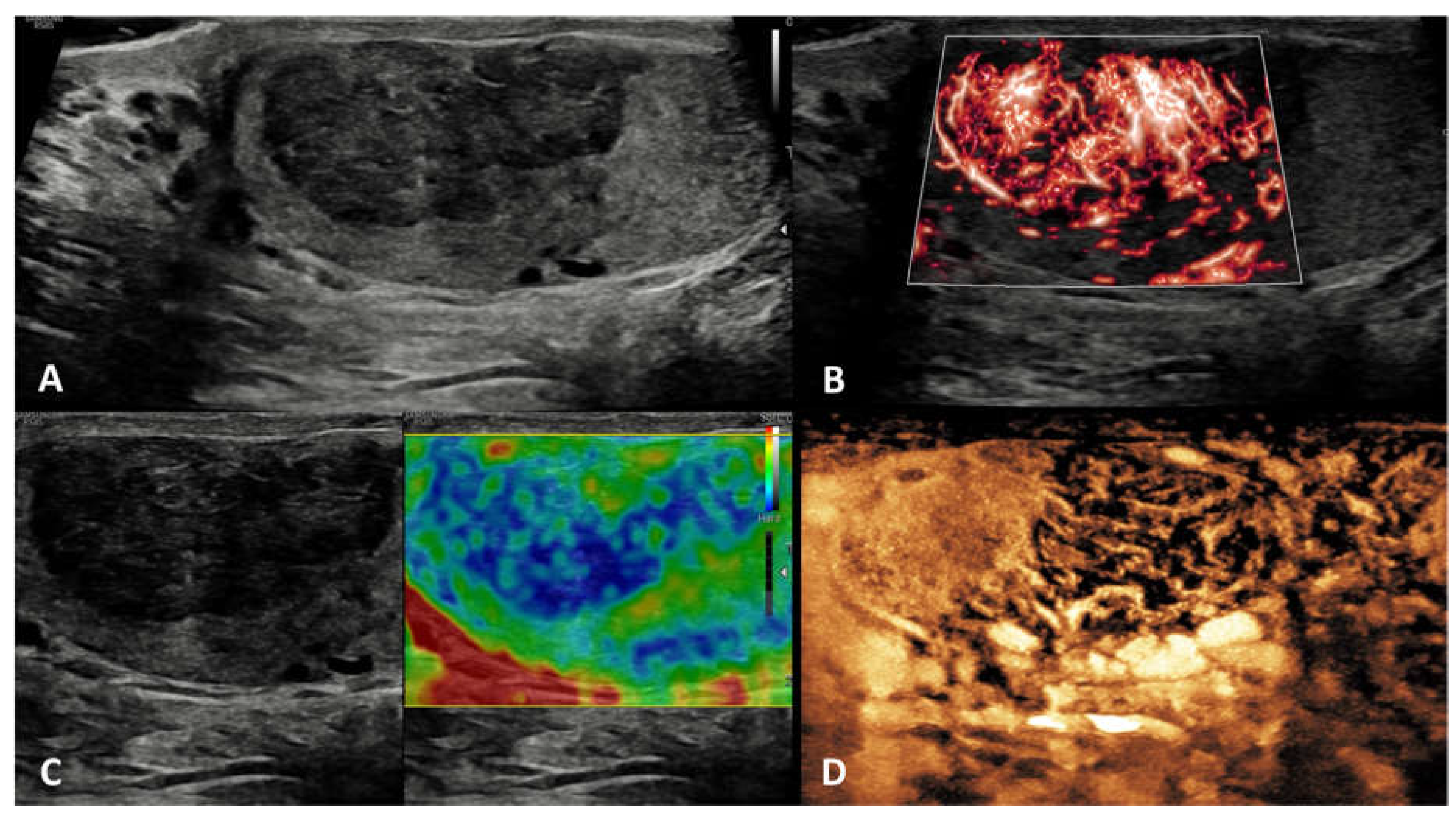
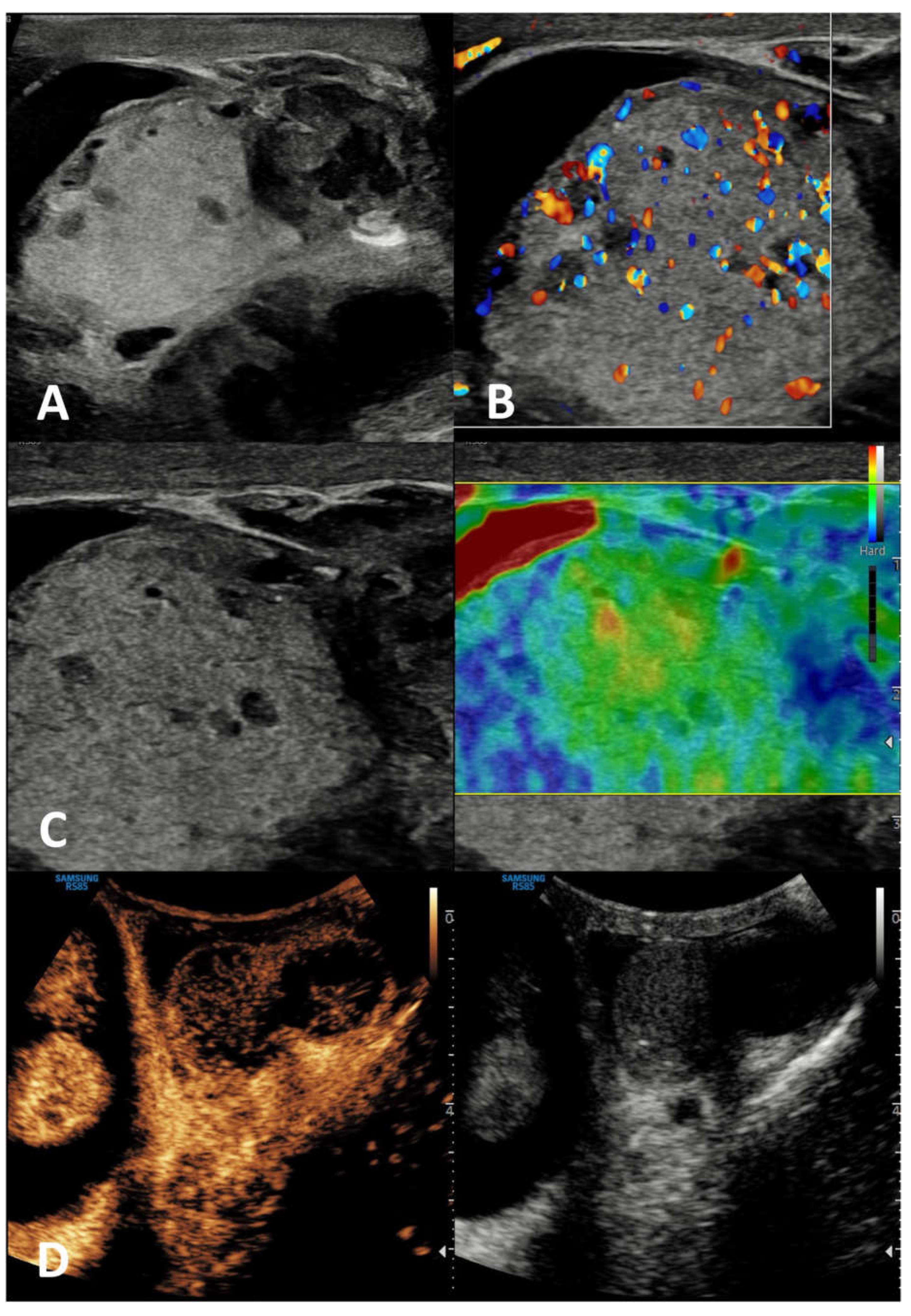
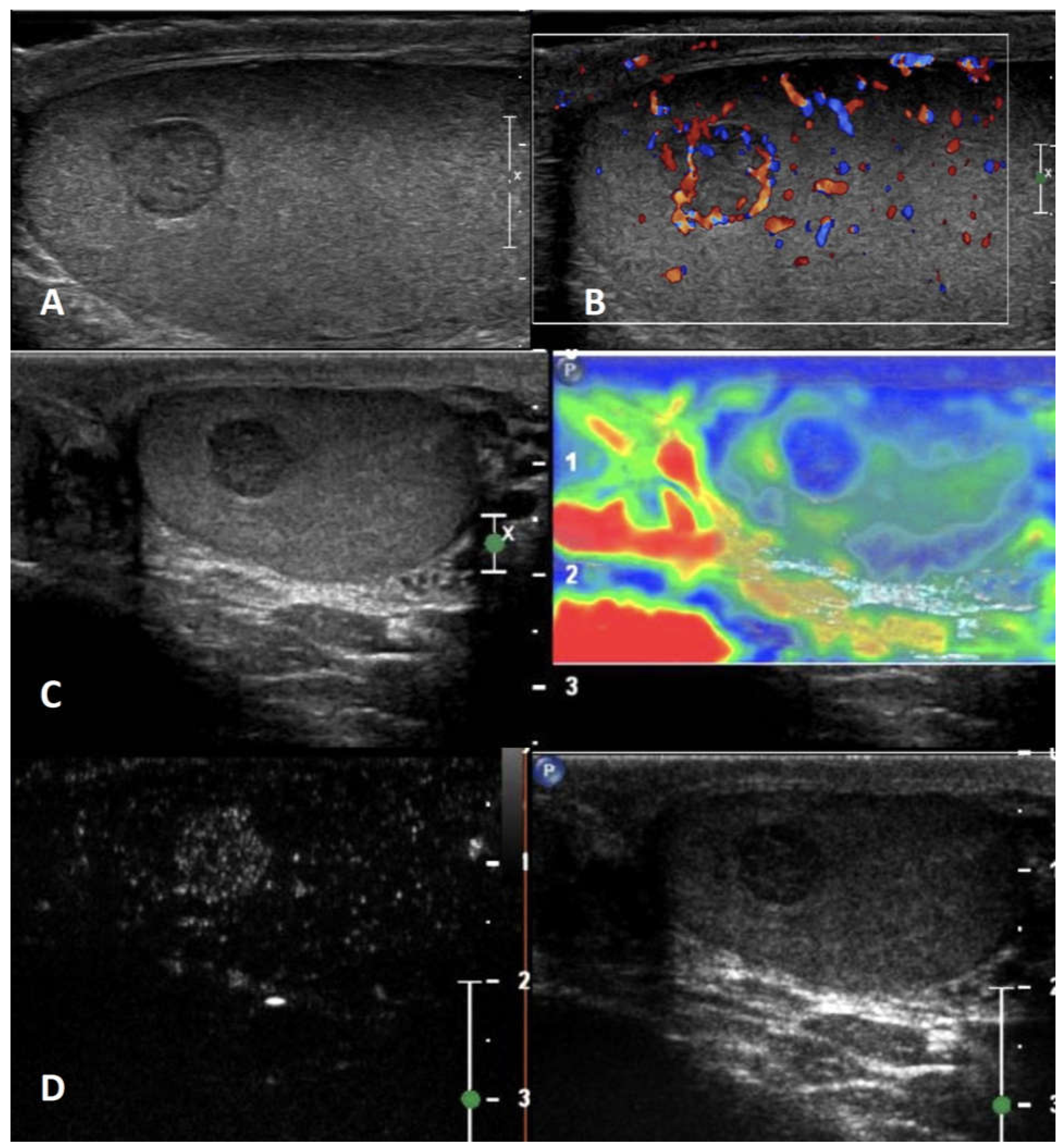
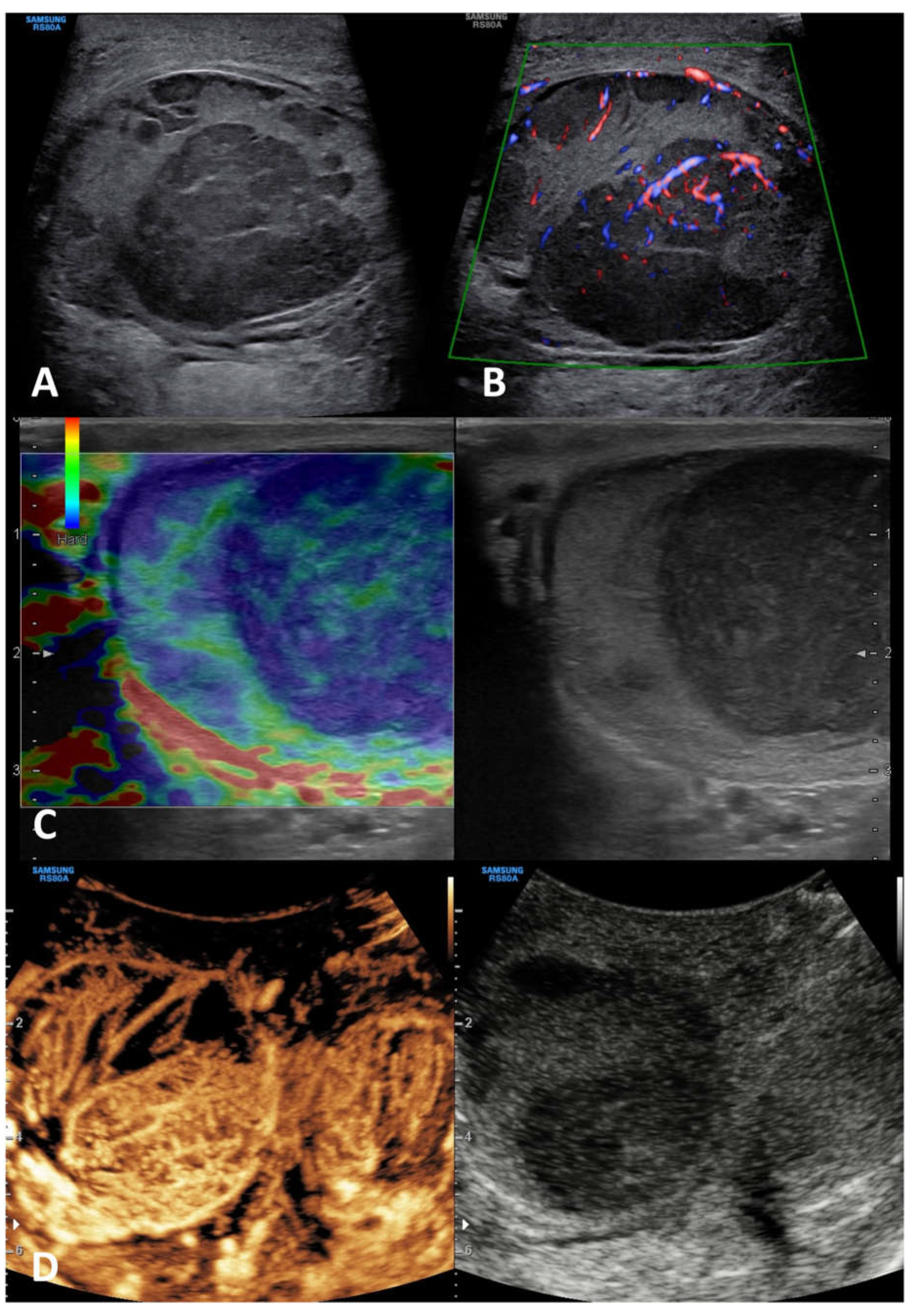
6.1. Seminomatous TGCTs (s-TGCTs)
6.2. Non-seminomatous TGCTs (ns-TGCTs)
6.2.1. Embryonal carcinoma
6.2.2. Teratoma
6.2.3. Choriocarcinoma
6.2.4. Yolk sac tumor
6.2.5. Mixed germ cell tumor
6.3. Stromal cell tumors
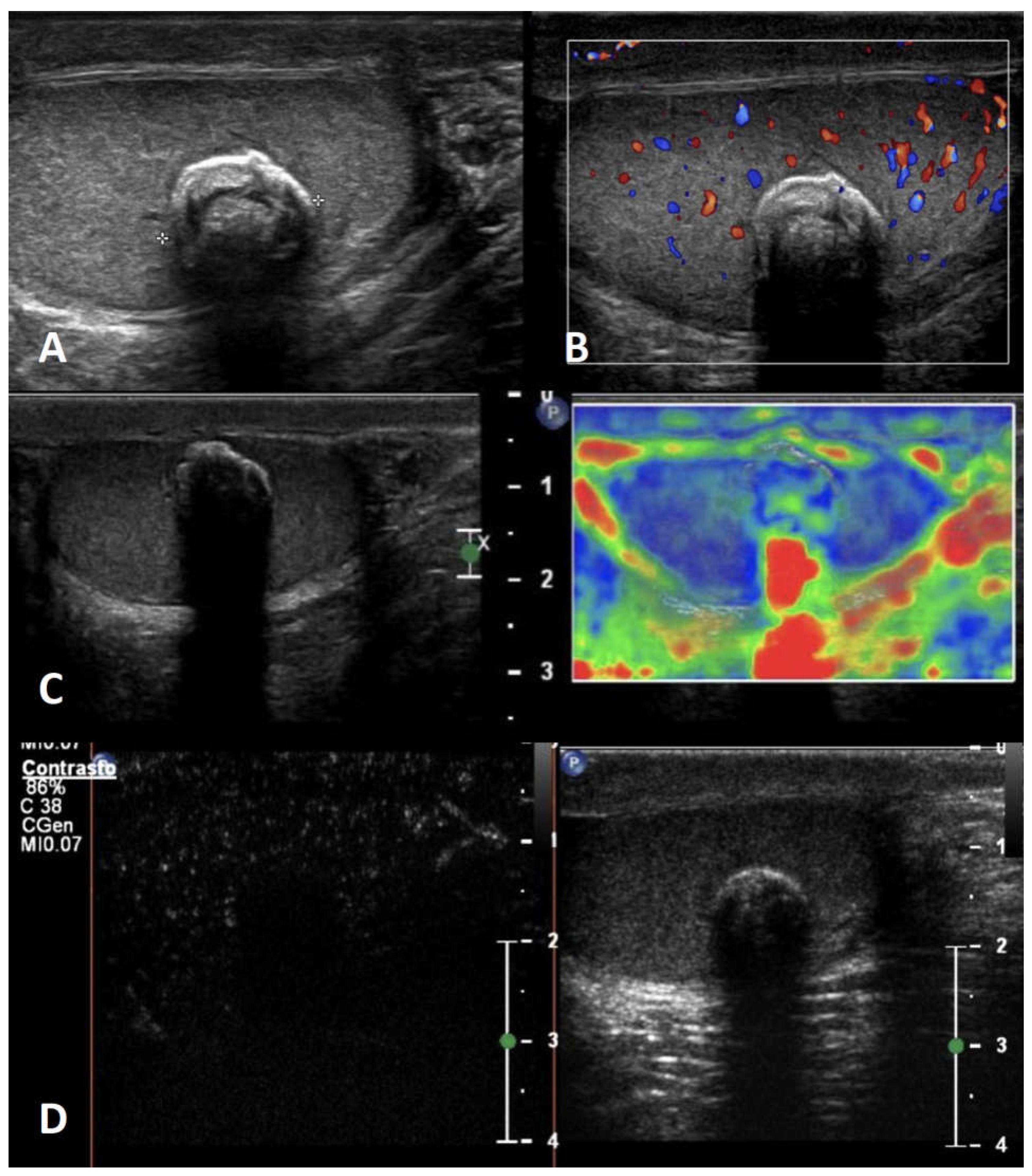
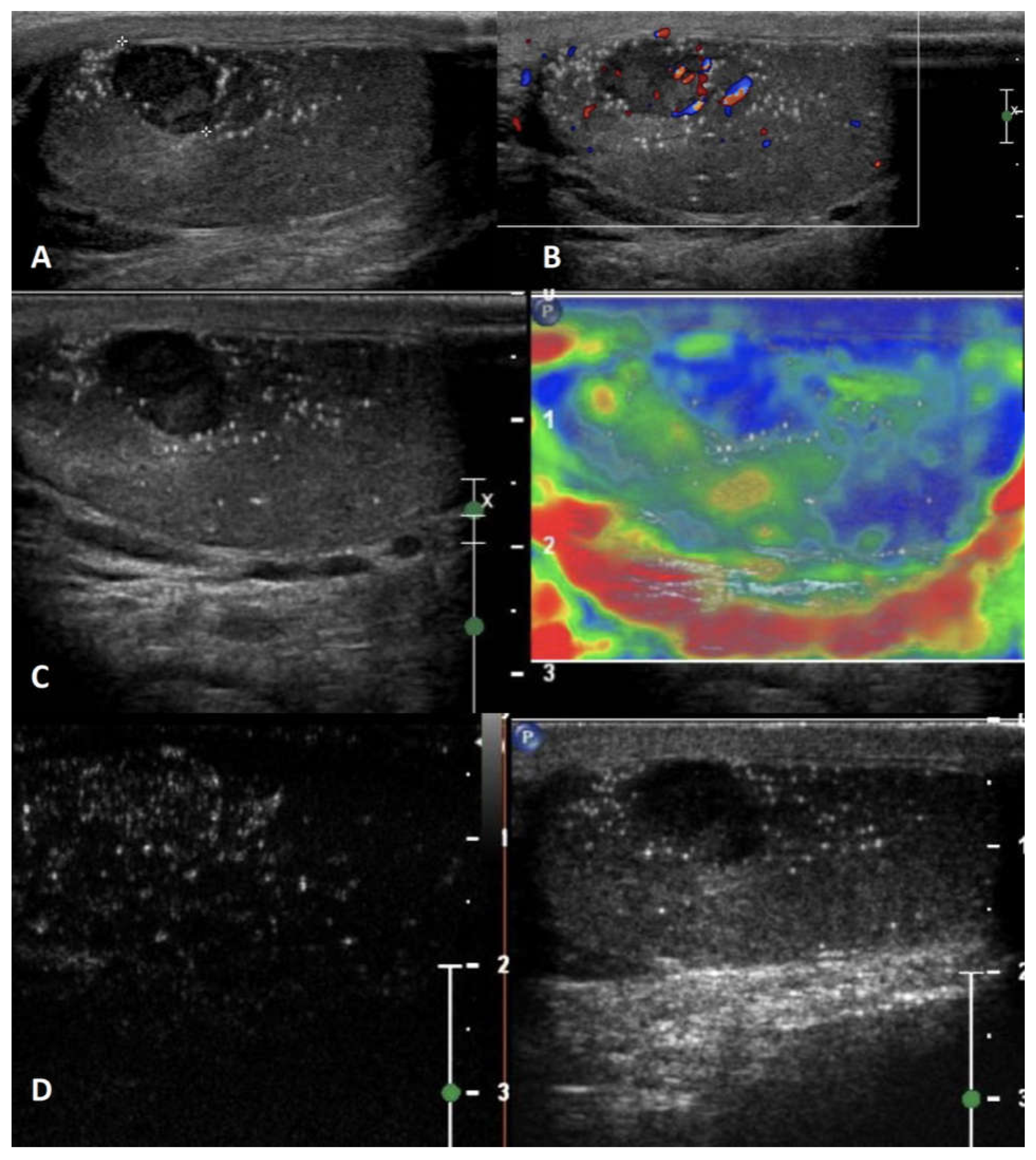
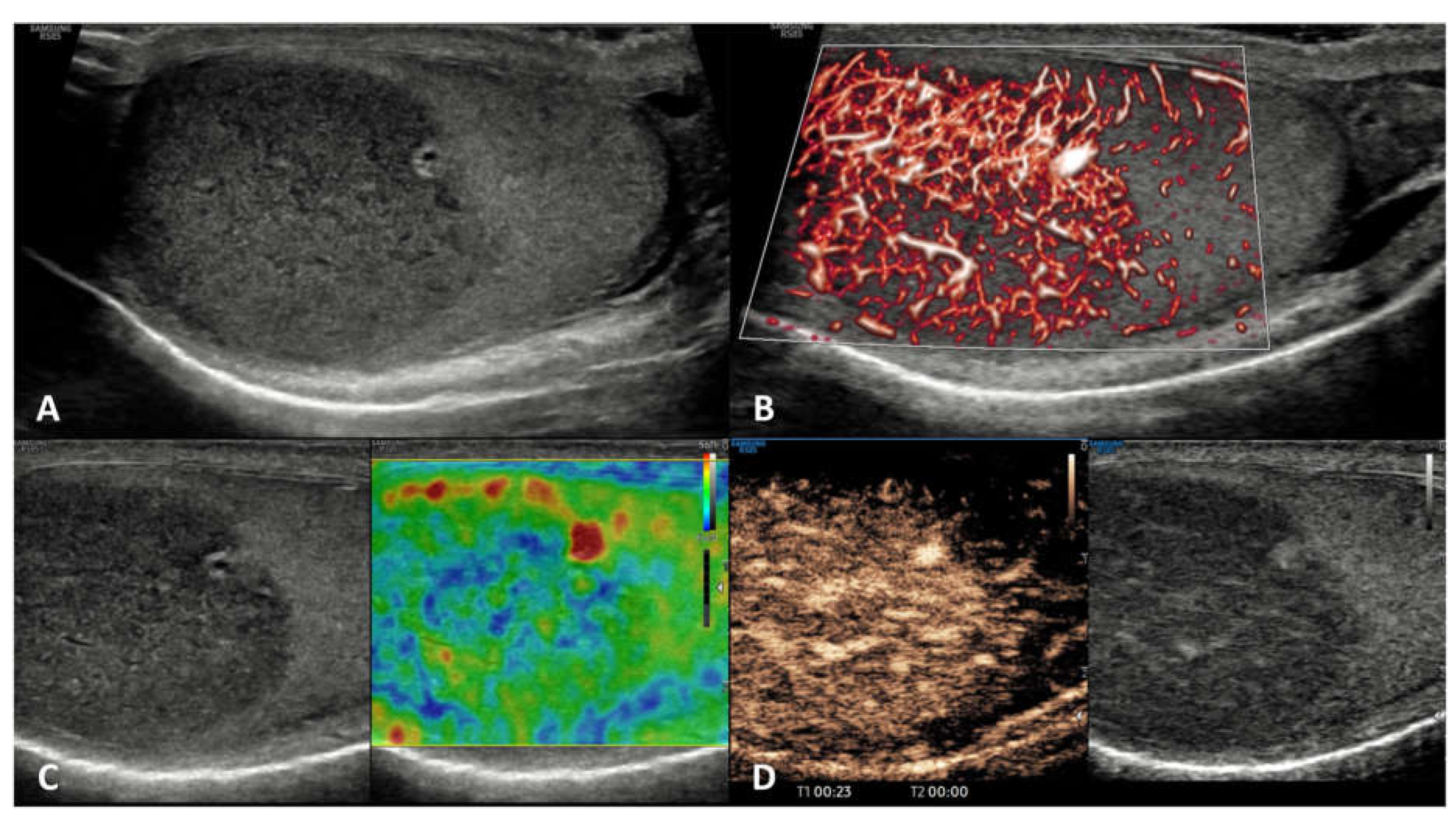
6.3.1. Leydig cell tumor (LCT)
6.3.2. Sertoli cell tumor (SCT)
6.4. Non-primary malignant tumors
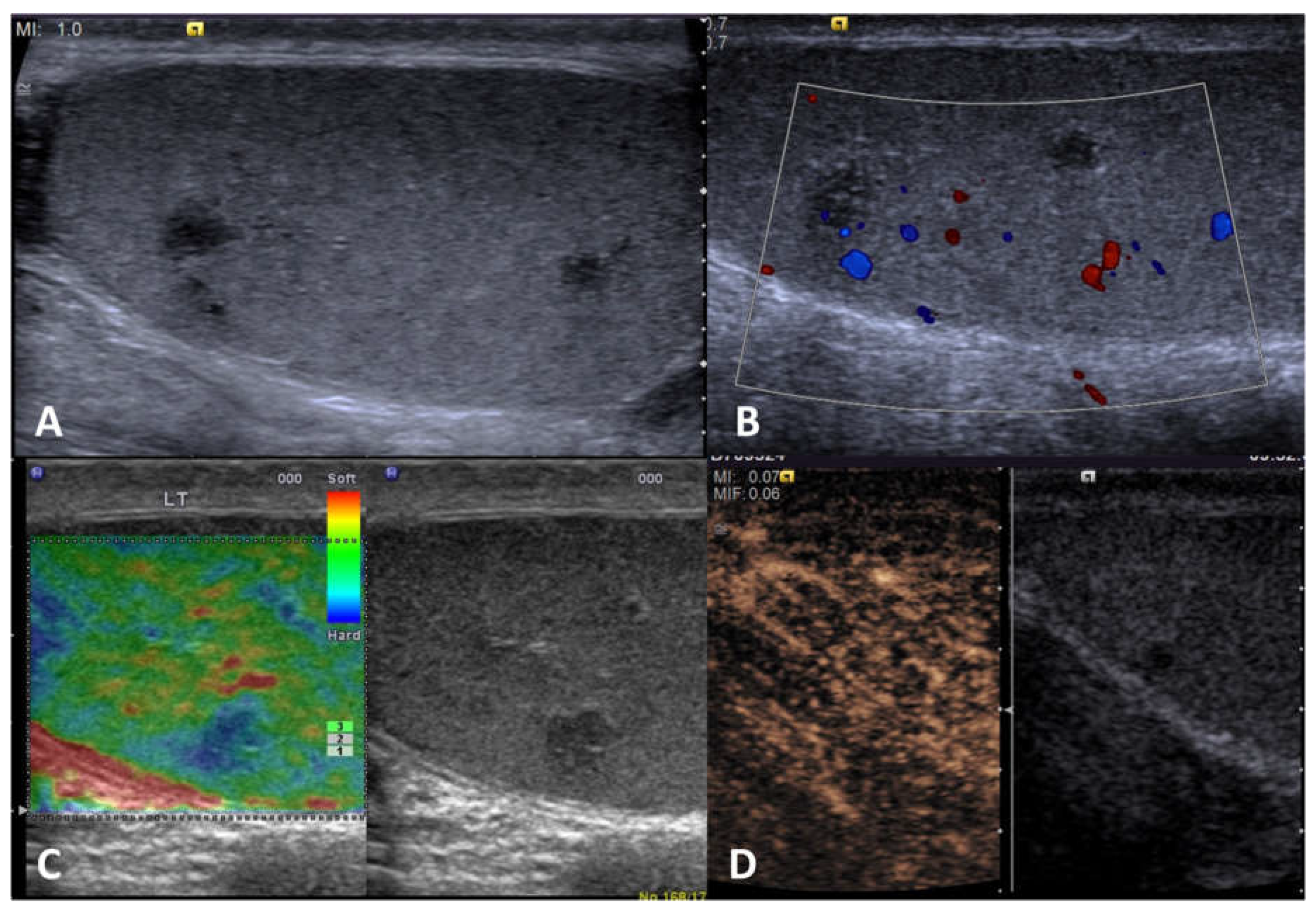
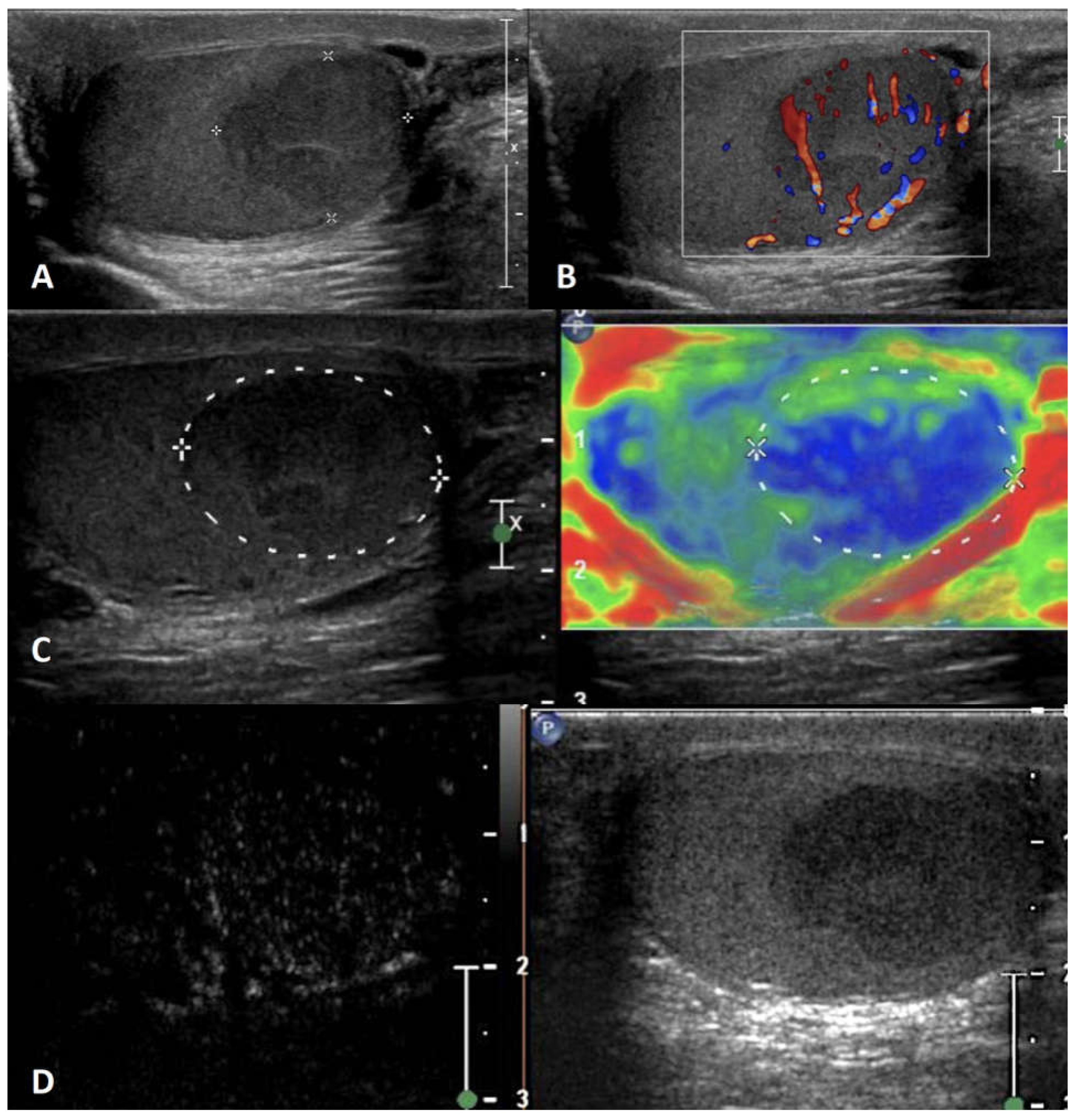
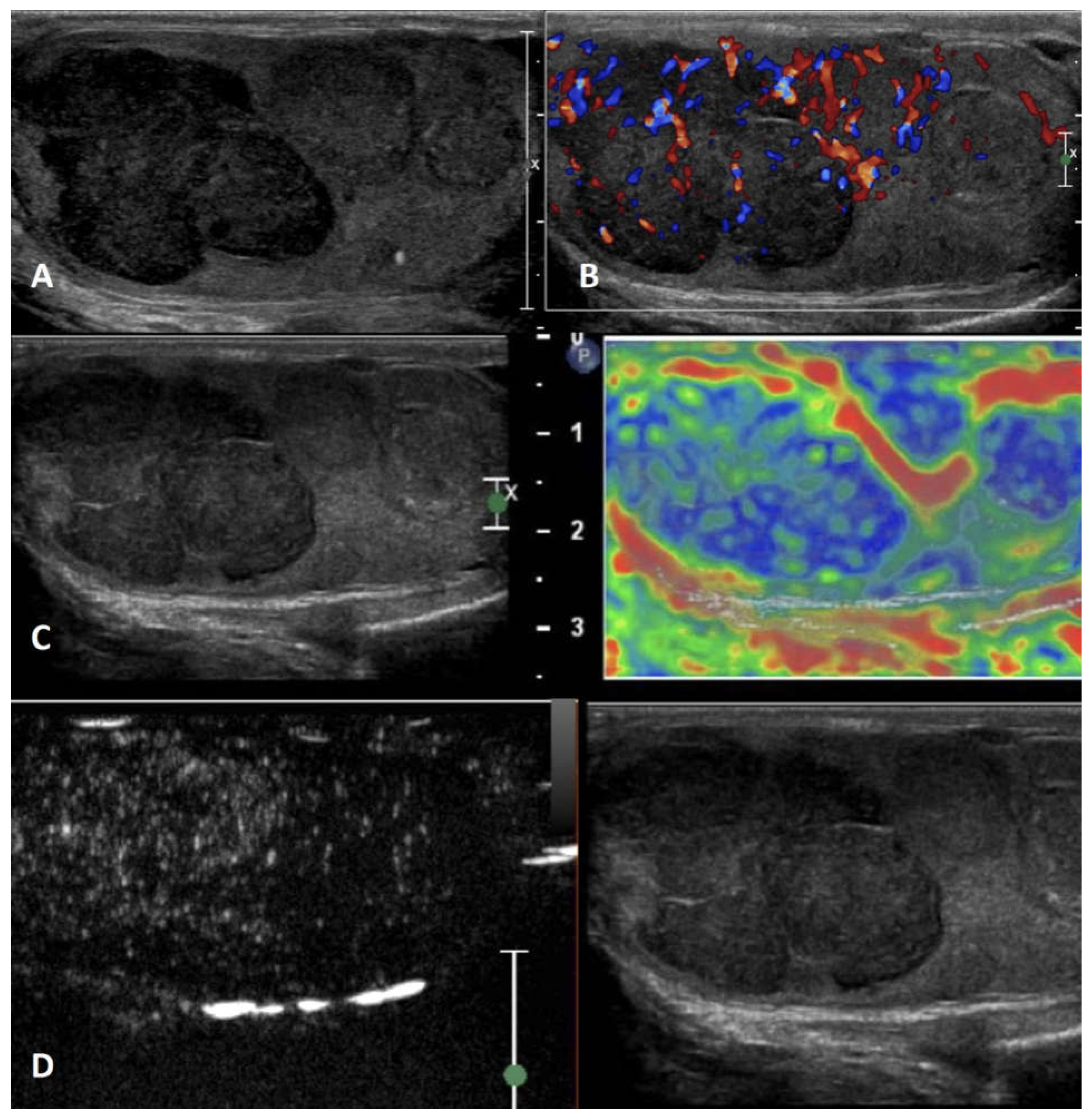
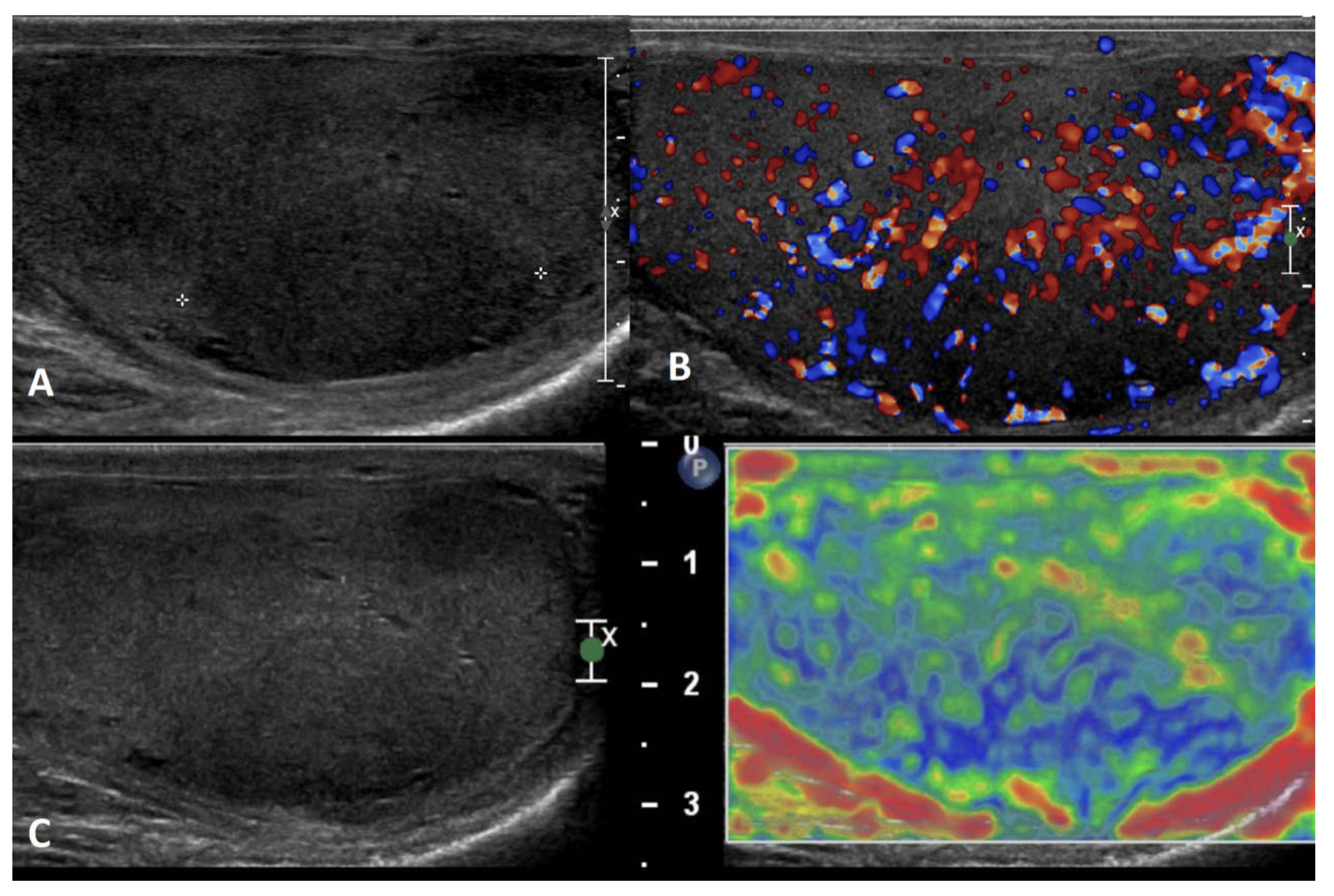
6.4.1. Lymphoma
6.4.2. Primary testicular leukemia
6.4.3. Plasmacytoma
6.4.4. Metastases
6.5. Burned out tumor
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lotti, F.; Maggi, M. Ultrasound of the Male Genital Tract in Relation to Male Reproductive Health. Hum. Reprod. Update 2015, 21, 56–83. [Google Scholar] [CrossRef]
- Lotti, F.; Bertolotto, M.; Maggi, M. Historical Trends for the Standards in Scrotal Ultrasonography: What Was, What Is and What Will Be Normal. Andrology 2021, 9, 1331–1355. [Google Scholar] [CrossRef]
- Isidori, A.M.; Lenzi, A. Ultrasound of the Testis for the Andrologist: Morphological and Functional Atlas; Springer, 2018; ISBN 9783319518268.
- Huang, D.Y.; Sidhu, P.S. Focal Testicular Lesions: Colour Doppler Ultrasound, Contrast-Enhanced Ultrasound and Tissue Elastography as Adjuvants to the Diagnosis. Br. J. Radiol. 2012, 85 Spec No 1, S41–S53. [Google Scholar] [CrossRef]
- Sidhu, P.S. Multiparametric Ultrasound (MPUS) Imaging: Terminology Describing the Many Aspects of Ultrasonography. Ultraschall Med. 2015, 36, 315–317. [Google Scholar] [CrossRef]
- Shah, A.; Lung, P.F.; Clarke, J.L.; Sellars, M.E.; Sidhu, P.S. Re: New Ultrasound Techniques for Imaging of the Indeterminate Testicular Lesion May Avoid Surgery Completely. Clin. Radiol. 2010, 65, 496–497. [Google Scholar] [CrossRef]
- Tenuta, M.; Sesti, F.; Bonaventura, I.; Mazzotta, P.; Pofi, R.; Gianfrilli, D.; Pozza, C. Use of Contrast Enhanced Ultrasound in Testicular Diseases: A Comprehensive Review. Andrology 2021, 9, 1369–1382. [Google Scholar] [CrossRef]
- Pozza, C.; Gianfrilli, D.; Fattorini, G.; Giannetta, E.; Barbagallo, F.; Nicolai, E.; Cristini, C.; Di Pierro, G.B.; Franco, G.; Lenzi, A.; et al. Diagnostic Value of Qualitative and Strain Ratio Elastography in the Differential Diagnosis of Non-Palpable Testicular Lesions. Andrology 2016, 4, 1193–1203. [Google Scholar] [CrossRef]
- Cantisani, V.; Di Leo, N.; Bertolotto, M.; Fresilli, D.; Granata, A.; Polti, G.; Polito, E.; Pacini, P.; Guiban, O.; Del Gaudio, G.; et al. Role of Multiparametric Ultrasound in Testicular Focal Lesions and Diffuse Pathology Evaluation, with Particular Regard to Elastography: Review of Literature. Andrology 2021, 9, 1356–1368. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.-P.; Frey, U.; Lock, G. Contemporary Diagnostic Work-up of Testicular Germ Cell Tumours. Nat. Rev. Urol. 2013, 10, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Marko, J.; Wolfman, D.J.; Aubin, A.L.; Sesterhenn, I.A. Testicular Seminoma and Its Mimics: From the Radiologic Pathology Archives. Radiographics 2017, 37, 1085–1098. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Xiong, G.-Y.; Fan, Y.; Huang, C.; Kang, Y.-M.; Ji, G.-J.; Chen, J.-C.; Xin, Z.-C.; Zhou, L.-Q. The Role of Tumor Size, Ultrasonographic Findings, and Serum Tumor Markers in Predicting the Likelihood of Malignant Testicular Histology. Asian J. Androl. 2019, 21, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Patrikidou, A.; Cazzaniga, W.; Berney, D.; Boormans, J.; de Angst, I.; Di Nardo, D.; Fankhauser, C.; Fischer, S.; Gravina, C.; Gremmels, H.; et al. European Association of Urology Guidelines on Testicular Cancer: 2023 Update. Eur. Urol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Carmignani, L.; Gadda, F.; Gazzano, G.; Nerva, F.; Mancini, M.; Ferruti, M.; Bulfamante, G.; Bosari, S.; Coggi, G.; Rocco, F.; et al. High Incidence of Benign Testicular Neoplasms Diagnosed by Ultrasound. J. Urol. 2003, 170, 1783–1786. [Google Scholar] [CrossRef] [PubMed]
- Rocher, L.; Ramchandani, P.; Belfield, J.; Bertolotto, M.; Derchi, L.E.; Correas, J.M.; Oyen, R.; Tsili, A.C.; Turgut, A.T.; Dogra, V.; et al. Incidentally Detected Non-Palpable Testicular Tumours in Adults at Scrotal Ultrasound: Impact of Radiological Findings on Management Radiologic Review and Recommendations of the ESUR Scrotal Imaging Subcommittee. Eur. Radiol. 2016, 26, 2268–2278. [Google Scholar] [CrossRef]
- Schröder, C.; Lock, G.; Schmidt, C.; Löning, T.; Dieckmann, K.-P. Real-Time Elastography and Contrast-Enhanced Ultrasonography in the Evaluation of Testicular Masses: A Comparative Prospective Study. Ultrasound Med. Biol. 2016, 42, 1807–1815. [Google Scholar] [CrossRef]
- Kachramanoglou, C.; Rafailidis, V.; Philippidou, M.; Bertolotto, M.; Huang, D.Y.; Deganello, A.; Sellars, M.E.; Sidhu, P.S. Multiparametric Sonography of Hematologic Malignancies of the Testis: Grayscale, Color Doppler, and Contrast-Enhanced Ultrasound and Strain Elastographic Appearances With Histologic Correlation. J. Ultrasound Med. 2017, 36, 409–420. [Google Scholar] [CrossRef]
- Lock, G.; Schröder, C.; Schmidt, C.; Anheuser, P.; Loening, T.; Dieckmann, K.P. Contrast-Enhanced Ultrasound and Real-Time Elastography for the Diagnosis of Benign Leydig Cell Tumors of the Testis - a Single Center Report on 13 Cases. Ultraschall Med. 2014, 35, 534–539. [Google Scholar] [CrossRef]
- Liu, H.; Dong, L.; Xiang, L.-H.; Xu, G.; Wan, J.; Fang, Y.; Ding, S.-S.; Jin, Y.; Sun, L.-P.; Xu, H.-X. Multiparametric Ultrasound for the Assessment of Testicular Lesions with Negative Tumoral Markers. Asian J. Androl. 2023, 25, 50–57. [Google Scholar] [CrossRef]
- Auer, T.; De Zordo, T.; Dejaco, C.; Gruber, L.; Pichler, R.; Jaschke, W.; Dogra, V.S.; Aigner, F. Value of Multiparametric US in the Assessment of Intratesticular Lesions. Radiology 2017, 285, 640–649. [Google Scholar] [CrossRef]
- Bernardo, S.; Konstantatou, E.; Huang, D.Y.; Deganello, A.; Philippidou, M.; Brown, C.; Sellars, M.E.; Sidhu, P.S. Multiparametric Sonographic Imaging of a Capillary Hemangioma of the Testis: Appearances on Gray-Scale, Color Doppler, Contrast-Enhanced Ultrasound and Strain Elastography. J. Ultrasound 2016, 19, 35–39. [Google Scholar] [CrossRef]
- Bertolotto, M.; Muça, M.; Currò, F.; Bucci, S.; Rocher, L.; Cova, M.A. Multiparametric US for Scrotal Diseases. Abdom Radiol (NY) 2018, 43, 899–917. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Y.; Pesapane, F.; Rafailidis, V.; Deganello, A.; Sellars, M.E.; Sidhu, P.S. The Role of Multiparametric Ultrasound in the Diagnosis of Paediatric Scrotal Pathology. Br. J. Radiol. 2020, 93, 20200063. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.-F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) Ultrasound Study on Healthy, Fertile Men: An Overview on Male Genital Tract Ultrasound Reference Ranges. Andrology 2022, 10 Suppl 2, 118–132. [Google Scholar] [CrossRef]
- Martino, P.; Galosi, A.B.; Bitelli, M.; Consonni, P.; Fiorini, F.; Granata, A.; Gunelli, R.; Liguori, G.; Palazzo, S.; Pavan, N.; et al. Practical Recommendations for Performing Ultrasound Scanning in the Urological and Andrological Fields. Arch. Ital. Urol. Androl. 2014, 86, 56–78. [Google Scholar] [CrossRef] [PubMed]
- Guideline developed in collaboration with the American College of Radiology; Society for Pediatric Radiology; Society of Radiologists in Ultrasound AIUM Practice Guideline for the Performance of Scrotal Ultrasound Examinations. J. Ultrasound Med. 2015, 34, 1–5. [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.-F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) Ultrasound Study on Healthy, Fertile Men: Prostate-Vesicular Transrectal Ultrasound Reference Ranges and Associations with Clinical, Seminal and Biochemical Characteristics. Andrology 2022, 10, 1150–1171. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) Ultrasound Study on Healthy, Fertile Men: Scrotal Ultrasound Reference Ranges and Associations with Clinical, Seminal, and Biochemical Characteristics. Andrology 2021, 9, 559–576. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.-F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) Ultrasound Study on Healthy, Fertile Men: Clinical, Seminal and Biochemical Characteristics. Andrology 2020, 8, 1005–1020. [Google Scholar] [CrossRef]
- Sidhu, P.S.; Cantisani, V.; Dietrich, C.F.; Gilja, O.H.; Saftoiu, A.; Bartels, E.; Bertolotto, M.; Calliada, F.; Clevert, D.-A.; Cosgrove, D.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018, 39, e2–e44. [Google Scholar] [CrossRef]
- Săftoiu, A.; Gilja, O.H.; Sidhu, P.S.; Dietrich, C.F.; Cantisani, V.; Amy, D.; Bachmann-Nielsen, M.; Bob, F.; Bojunga, J.; Brock, M.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Elastography in Non-Hepatic Applications: Update 2018. Ultraschall Med. 2019, 40, 425–453. [Google Scholar] [CrossRef]
- Bamber, J.; Cosgrove, D.; Dietrich, C.F.; Fromageau, J.; Bojunga, J.; Calliada, F.; Cantisani, V.; Correas, J.-M.; D’Onofrio, M.; Drakonaki, E.E.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013, 34, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Correas, J.M.; Drakonakis, E.; Isidori, A.M.; Hélénon, O.; Pozza, C.; Cantisani, V.; Di Leo, N.; Maghella, F.; Rubini, A.; Drudi, F.M.; et al. Update on Ultrasound Elastography: Miscellanea. Prostate, Testicle, Musculo-Skeletal. Eur. J. Radiol. 2013, 82, 1904–1912. [Google Scholar] [CrossRef] [PubMed]
- Hoag, N.A.; Afshar, K.; Youssef, D.; Masterson, J.S.T.; Murphy, J.; Macneily, A.E. Cystic Intratesticular Lesions in Pediatric Patients. J. Pediatr. Surg. 2013, 48, 1773–1777. [Google Scholar] [CrossRef] [PubMed]
- Gooding, G.A.; Leonhardt, W.; Stein, R. Testicular Cysts: US Findings. Radiology 1987, 163, 537–538. [Google Scholar] [CrossRef] [PubMed]
- Hamm, B.; Fobbe, F.; Loy, V. Testicular Cysts: Differentiation with US and Clinical Findings. Radiology 1988, 168, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Dogra, V.S.; Gottlieb, R.H.; Rubens, D.J.; Liao, L. Benign Intratesticular Cystic Lesions: US Features. Radiographics 2001, 21 Spec No, S273–S281. [Google Scholar] [CrossRef]
- Shah, K.H.; Maxted, W.C.; Chun, B. Epidermoid Cysts of the Testis: A Report of Three Cases and an Analysis of 141 Cases from the World Literature. Cancer 1981, 47, 577–582. [Google Scholar] [CrossRef]
- Dogra, V.S.; Gottlieb, R.H.; Oka, M.; Rubens, D.J. Sonography of the Scrotum. Radiology 2003, 227, 18–36. [Google Scholar] [CrossRef]
- Anheuser, P.; Kranz, J.; Stolle, E.; Höflmayer, D.; Büscheck, F.; Mühlstädt, S.; Lock, G.; Dieckmann, K.P. Testicular Epidermoid Cysts: A Reevaluation. BMC Urol. 2019, 19, 52. [Google Scholar] [CrossRef]
- Patel, K.; Sellars, M.E.; Clarke, J.L.; Sidhu, P.S. Features of Testicular Epidermoid Cysts on Contrast-Enhanced Sonography and Real-Time Tissue Elastography. J. Ultrasound Med. 2012, 31, 115–122. [Google Scholar] [CrossRef]
- Manning, M.A.; Woodward, P.J. Testicular Epidermoid Cysts: Sonographic Features with Clinicopathologic Correlation. J. Ultrasound Med. 2010, 29, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Isidori, A.M.; Pozza, C.; Gianfrilli, D.; Giannetta, E.; Lemma, A.; Pofi, R.; Barbagallo, F.; Manganaro, L.; Martino, G.; Lombardo, F.; et al. Differential Diagnosis of Nonpalpable Testicular Lesions: Qualitative and Quantitative Contrast-Enhanced US of Benign and Malignant Testicular Tumors. Radiology 2014, 273, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Engels, M.; Span, P.N.; van Herwaarden, A.E.; Sweep, F.C.G.J.; Stikkelbroeck, N.M.M.L.; Claahsen-van der Grinten, H.L. Testicular Adrenal Rest Tumors: Current Insights on Prevalence, Characteristics, Origin, and Treatment. Endocr. Rev. 2019, 40, 973–987. [Google Scholar] [CrossRef]
- Jedrzejewski, G.; Ben-Skowronek, I.; Wozniak, M.M.; Brodzisz, A.; Budzynska, E.; Wieczorek, A.P. Testicular Adrenal Rest Tumors in Boys with Congenital Adrenal Hyperplasia: 3D US and Elastography--Do We Get More Information for Diagnosis and Monitoring? J. Pediatr. Urol. 2013, 9, 1032–1037. [Google Scholar] [CrossRef]
- Corcioni, B.; Renzulli, M.; Marasco, G.; Baronio, F.; Gambineri, A.; Ricciardi, D.; Ortolano, R.; Farina, D.; Gaudiano, C.; Cassio, A.; et al. Prevalence and Ultrasound Patterns of Testicular Adrenal Rest Tumors in Adults with Congenital Adrenal Hyperplasia. Transl. Androl. Urol. 2021, 10, 562–573. [Google Scholar] [CrossRef] [PubMed]
- Mansoor, N.M.; Huang, D.Y.; Sidhu, P.S. Multiparametric Ultrasound Imaging Characteristics of Multiple Testicular Adrenal Rest Tumours in Congenital Adrenal Hyperplasia. Ultrasound 2022, 30, 80–84. [Google Scholar] [CrossRef]
- Tresoldi, A.S.; Betella, N.; Hasenmajer, V.; Pozza, C.; Vena, W.; Fiamengo, B.; Negri, L.; Cappa, M.; Lania, A.G.A.; Lenzi, A.; et al. Bilateral Testicular Masses and Adrenal Insufficiency: Is Congenital Adrenal Hyperplasia the Only Possible Diagnosis? First Two Cases of TARTS Described in Addison-Only X-Linked Adrenoleukodystrophy and a Brief Review of Literature. J. Endocrinol. Invest. 2021, 44, 391–402. [Google Scholar] [CrossRef]
- Ricker, W.; Clark, M. Sarcoidosis; a Clinicopathologic Review of 300 Cases, Including 22 Autopsies. Am. J. Clin. Pathol. 1949, 19, 725–749. [Google Scholar] [CrossRef]
- Bhatt, S.; Jafri, S.Z.H.; Wasserman, N.; Dogra, V.S. Imaging of Non-Neoplastic Intratesticular Masses. Diagn. Interv. Radiol. 2011, 17, 52–63. [Google Scholar] [CrossRef]
- Stewart, V.R.; Sidhu, P.S. The Testis: The Unusual, the Rare and the Bizarre. Clin. Radiol. 2007, 62, 289–302. [Google Scholar] [CrossRef]
- Rafailidis, V.; Robbie, H.; Konstantatou, E.; Huang, D.Y.; Deganello, A.; Sellars, M.E.; Cantisani, V.; Isidori, A.M.; Sidhu, P.S. Sonographic Imaging of Extra-Testicular Focal Lesions: Comparison of Grey-Scale, Colour Doppler and Contrast-Enhanced Ultrasound. Ultrasound 2016, 24, 23–33. [Google Scholar] [CrossRef]
- Lung, P.F.C.; Fang, C.; Jaffer, O.S.; Deganello, A.; Shah, A.; Hedayati, V.; Obaro, A.; Yusuf, G.T.; Huang, D.Y.; Sellars, M.E.; et al. Vascularity of Intra-Testicular Lesions: Inter-Observer Variation in the Assessment of Non-Neoplastic Versus Neoplastic Abnormalities After Vascular Enhancement With Contrast-Enhanced Ultrasound. Ultrasound Med. Biol. 2020, 46, 2956–2964. [Google Scholar] [CrossRef]
- De Cinque, A.; Corcioni, B.; Rossi, M.S.; Franceschelli, A.; Colombo, F.; Golfieri, R.; Renzulli, M.; Gaudiano, C. Case Report: Testicular Sarcoidosis: The Diagnostic Role of Contrast-Enhanced Ultrasound and Review of the Literature. Front. Med. 2020, 7, 610384. [Google Scholar] [CrossRef] [PubMed]
- Gianfrilli, D.; Isidori, A.M.; Lenzi, A. Segmental Testicular Ischaemia: Presentation, Management and Follow-Up. Int. J. Androl. 2009, 32, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V.; Huang, D.Y.; Sidhu, P.S. Metachronous Bilateral Segmental Testicular Infarction: Multi-Parametric Ultrasound Imaging with Grey-Scale Ultrasound, Doppler Ultrasound, Contrast-Enhanced Ultrasound (CEUS) and Real-Time Tissue Elastography (RTE). J. Ultrasound 2014, 17, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Bilagi, P.; Sriprasad, S.; Clarke, J.L.; Sellars, M.E.; Muir, G.H.; Sidhu, P.S. Clinical and Ultrasound Features of Segmental Testicular Infarction: Six-Year Experience from a Single Centre. Eur. Radiol. 2007, 17, 2810–2818. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pérez, G.C.; Tardáguila, F.M.; Velasco, M.; Rivas, C.; Dos Santos, J.; Cambronero, J.; Trinidad, C.; San Miguel, P. Radiologic Findings of Segmental Testicular Infarction. AJR Am. J. Roentgenol. 2005, 184, 1587–1593. [Google Scholar] [CrossRef] [PubMed]
- Sweet, D.E.; Feldman, M.K.; Remer, E.M. Imaging of the Acute Scrotum: Keys to a Rapid Diagnosis of Acute Scrotal Disorders. Abdom Radiol (NY) 2020, 45, 2063–2081. [Google Scholar] [CrossRef] [PubMed]
- Bertolotto, M.; Derchi, L.E.; Sidhu, P.S.; Serafini, G.; Valentino, M.; Grenier, N.; Cova, M.A. Acute Segmental Testicular Infarction at Contrast-Enhanced Ultrasound: Early Features and Changes during Follow-Up. AJR Am. J. Roentgenol. 2011, 196, 834–841. [Google Scholar] [CrossRef]
- Yusuf, G.T.; Sidhu, P.S. A Review of Ultrasound Imaging in Scrotal Emergencies. J. Ultrasound 2013, 16, 171–178. [Google Scholar] [CrossRef]
- Pavlica, P.; Barozzi, L. Imaging of the Acute Scrotum. Eur. Radiol. 2001, 11, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Valentino, M.; Bertolotto, M.; Derchi, L.; Bertaccini, A.; Pavlica, P.; Martorana, G.; Barozzi, L. Role of Contrast Enhanced Ultrasound in Acute Scrotal Diseases. Eur. Radiol. 2011, 21, 1831–1840. [Google Scholar] [CrossRef] [PubMed]
- Lung, P.F.C.; Jaffer, O.S.; Sellars, M.E.; Sriprasad, S.; Kooiman, G.G.; Sidhu, P.S. Contrast-Enhanced Ultrasound in the Evaluation of Focal Testicular Complications Secondary to Epididymitis. AJR Am. J. Roentgenol. 2012, 199, W345–W354. [Google Scholar] [CrossRef] [PubMed]
- Purushothaman, H.; Sellars, M.E.K.; Clarke, J.L.; Sidhu, P.S. Intratesticular Haematoma: Differentiation from Tumour on Clinical History and Ultrasound Appearances in Two Cases. Br. J. Radiol. 2007, 80, e184–e187. [Google Scholar] [CrossRef]
- Ramanathan, S.; Bertolotto, M.; Freeman, S.; Belfield, J.; Derchi, L.E.; Huang, D.Y.; Lotti, F.; Markiet, K.; Nikolic, O.; Ramchandani, P.; et al. Imaging in Scrotal Trauma: A European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) Position Statement. Eur. Radiol. 2021, 31, 4918–4928. [Google Scholar] [CrossRef]
- Yusuf, G.; Konstantatou, E.; Sellars, M.E.; Huang, D.Y.; Sidhu, P.S. Multiparametric Sonography of Testicular Hematomas: Features on Grayscale, Color Doppler, and Contrast-Enhanced Sonography and Strain Elastography. J. Ultrasound Med. 2015, 34, 1319–1328. [Google Scholar] [CrossRef]
- Öztürk, Ç.; Paşaoğlu, E.; Bölme Şavlı, T. A Lesion Mimicking Malignancy: Granulomatous Orchitis. Üroonkoloji bül. 2021, 20, 126–128. [Google Scholar] [CrossRef]
- Civelli, V.F.; Heidari, A.; Valdez, M.C.; Narang, V.K.; Johnson, R.H. A Case of Testicular Granulomatous Inflammation Mistaken for Malignancy: Tuberculosis Identified Post Orchiectomy. J Investig Med High Impact Case Rep 2020, 8, 2324709620938947. [Google Scholar] [CrossRef]
- Peyrí Rey, E.; Riverola Manzanilla, A.; Cañas Tello, M.A. [Bilateral idiopathic granulomatous orchitis]. Actas Urol. Esp. 2008, 32, 461–463. [Google Scholar] [CrossRef]
- Wegner, H.E.; Loy, V.; Dieckmann, K.P. Granulomatous Orchitis--an Analysis of Clinical Presentation, Pathological Anatomic Features and Possible Etiologic Factors. Eur. Urol. 1994, 26, 56–60. [Google Scholar] [CrossRef]
- Salmeron, I.; Ramirez-Escobar, M.A.; Puertas, F.; Marcos, R.; Garcia-Marcos, F.; Sanchez, R. Granulomatous Epididymo-Orchitis: Sonographic Features and Clinical Outcome in Brucellosis, Tuberculosis and Idiopathic Granulomatous Epididymo-Orchitis. J. Urol. 1998, 159, 1954–1957. [Google Scholar] [CrossRef] [PubMed]
- Lung, P.F.C.; Sidhu, P.S. Role of Ultrasound in the Diagnosis of Testicular Lesions. Imaging Med. 2011, 3, 587–595. [Google Scholar] [CrossRef]
- Nepal, P.; Ojili, V.; Songmen, S.; Kaur, N.; Olsavsky, T.; Nagar, A. “The Great Masquerader”: Sonographic Pictorial Review of Testicular Tuberculosis and Its Mimics. J. Clin. Imaging Sci. 2019, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Viswaroop, B.S.; Kekre, N.; Gopalakrishnan, G. Isolated Tuberculous Epididymitis: A Review of Forty Cases. J. Postgrad. Med. 2005, 51, 109–111. [Google Scholar]
- Park, J.S.; Kim, J.; Elghiaty, A.; Ham, W.S. Recent Global Trends in Testicular Cancer Incidence and Mortality. Medicine 2018, 97, e12390. [Google Scholar] [CrossRef]
- Gurney, J.K.; Florio, A.A.; Znaor, A.; Ferlay, J.; Laversanne, M.; Sarfati, D.; Bray, F.; McGlynn, K.A. International Trends in the Incidence of Testicular Cancer: Lessons from 35 Years and 41 Countries. Eur. Urol. 2019, 76, 615–623. [Google Scholar] [CrossRef]
- Znaor, A.; Skakkebaek, N.E.; Rajpert-De Meyts, E.; Kuliš, T.; Laversanne, M.; Gurney, J.; Sarfati, D.; McGlynn, K.A.; Bray, F. Global Patterns in Testicular Cancer Incidence and Mortality in 2020. Int. J. Cancer 2022, 151, 692–698. [Google Scholar] [CrossRef]
- Moch, H.; Amin, M.B.; Berney, D.M.; Compérat, E.M.; Gill, A.J.; Hartmann, A.; Menon, S.; Raspollini, M.R.; Rubin, M.A.; Srigley, J.R.; et al. The 2022 World Health Organization Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur. Urol. 2022, 82, 458–468. [Google Scholar] [CrossRef]
- Honecker, F.; Aparicio, J.; Berney, D.; Beyer, J.; Bokemeyer, C.; Cathomas, R.; Clarke, N.; Cohn-Cedermark, G.; Daugaard, G.; Dieckmann, K.-P.; et al. ESMO Consensus Conference on Testicular Germ Cell Cancer: Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2018, 29, 1658–1686. [Google Scholar] [CrossRef]
- Gilligan, T.D.; Seidenfeld, J.; Basch, E.M.; Einhorn, L.H.; Fancher, T.; Smith, D.C.; Stephenson, A.J.; Vaughn, D.J.; Cosby, R.; Hayes, D.F.; et al. American Society of Clinical Oncology Clinical Practice Guideline on Uses of Serum Tumor Markers in Adult Males with Germ Cell Tumors. J. Clin. Oncol. 2010, 28, 3388–3404. [Google Scholar] [CrossRef]
- Barlow, L.J.; Badalato, G.M.; McKiernan, J.M. Serum Tumor Markers in the Evaluation of Male Germ Cell Tumors. Nat. Rev. Urol. 2010, 7, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Kanakis, G.A.; Nordkap, L.; Bang, A.K.; Calogero, A.E.; Bártfai, G.; Corona, G.; Forti, G.; Toppari, J.; Goulis, D.G.; Jørgensen, N. EAA Clinical Practice Guidelines-Gynecomastia Evaluation and Management. Andrology 2019, 7, 778–793. [Google Scholar] [CrossRef] [PubMed]
- Hassan, H.C.; Cullen, I.M.; Casey, R.G.; Rogers, E. Gynaecomastia: An Endocrine Manifestation of Testicular Cancer. Andrologia 2008, 40, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Rajpert-De Meyts, E.; McGlynn, K.A.; Okamoto, K.; Jewett, M.A.S.; Bokemeyer, C. Testicular Germ Cell Tumours. Lancet 2016, 387, 1762–1774. [Google Scholar] [CrossRef] [PubMed]
- Hanson, H.A.; Anderson, R.E.; Aston, K.I.; Carrell, D.T.; Smith, K.R.; Hotaling, J.M. Subfertility Increases Risk of Testicular Cancer: Evidence from Population-Based Semen Samples. Fertil. Steril. 2016, 105, 322–328. [Google Scholar] [CrossRef]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Buck Louis, G.M.; Toppari, J.; Andersson, A.-M.; Eisenberg, M.L.; Jensen, T.K.; Jørgensen, N.; Swan, S.H.; Sapra, K.J.; et al. Male Reproductive Disorders and Fertility Trends: Influences of Environment and Genetic Susceptibility. Physiol. Rev. 2016, 96, 55–97. [Google Scholar] [CrossRef]
- Meyts, E.R.-D. Developmental Model for the Pathogenesis of Testicular Carcinoma in Situ: Genetic and Environmental Aspects; 2006.
- Piltoft, J.S.; Larsen, S.B.; Dalton, S.O.; Johansen, C.; Baker, J.L.; Cederkvist, L.; Andersen, I. Early Life Risk Factors for Testicular Cancer: A Case-Cohort Study Based on the Copenhagen School Health Records Register. Acta Oncol. 2017, 56, 220–224. [Google Scholar] [CrossRef]
- Pettersson, A.; Richiardi, L.; Nordenskjold, A.; Kaijser, M.; Akre, O. Age at Surgery for Undescended Testis and Risk of Testicular Cancer. N. Engl. J. Med. 2007, 356, 1835–1841. [Google Scholar] [CrossRef]
- Williamson, S.R.; Delahunt, B.; Magi-Galluzzi, C.; Algaba, F.; Egevad, L.; Ulbright, T.M.; Tickoo, S.K.; Srigley, J.R.; Epstein, J.I.; Berney, D.M.; et al. The World Health Organization 2016 Classification of Testicular Germ Cell Tumours: A Review and Update from the International Society of Urological Pathology Testis Consultation Panel. Histopathology 2017, 70, 335–346. [Google Scholar] [CrossRef]
- Kawamoto, A.; Hatano, T.; Saito, K.; Inoue, R.; Nagao, T.; Sanada, S. Sonographic Classification of Testicular Tumors by Tissue Harmonic Imaging: Experience of 58 Cases. J. Med. Ultrason. 2018, 45, 103–111. [Google Scholar] [CrossRef]
- McDonald, M.W.; Reed, A.B.; Tran, P.T.; Evans, L.A. Testicular Tumor Ultrasound Characteristics and Association with Histopathology. Urol. Int. 2012, 89, 196–202. [Google Scholar] [CrossRef]
- Woodward, P.J.; Sohaey, R.; O’Donoghue, M.J.; Green, D.E. From the Archives of the AFIP: Tumors and Tumorlike Lesions of the Testis: Radiologic-Pathologic Correlation. Radiographics 2002, 22, 189–216. [Google Scholar] [CrossRef]
- Necas, M.; Muthupalaniappaan, M.; Barnard, C. Ultrasound Morphological Patterns of Testicular Tumours, Correlation with Histopathology. J Med Radiat Sci 2021, 68, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Barbonetti, A.; Martorella, A.; Minaldi, E.; D’Andrea, S.; Bardhi, D.; Castellini, C.; Francavilla, F.; Francavilla, S. Testicular Cancer in Infertile Men With and Without Testicular Microlithiasis: A Systematic Review and Meta-Analysis of Case-Control Studies. Front. Endocrinol. 2019, 10, 164. [Google Scholar] [CrossRef] [PubMed]
- Richenberg, J.; Belfield, J.; Ramchandani, P.; Rocher, L.; Freeman, S.; Tsili, A.C.; Cuthbert, F.; Studniarek, M.; Bertolotto, M.; Turgut, A.T.; et al. Testicular Microlithiasis Imaging and Follow-up: Guidelines of the ESUR Scrotal Imaging Subcommittee. Eur. Radiol. 2015, 25, 323–330. [Google Scholar] [CrossRef]
- Goddi, A.; Sacchi, A.; Magistretti, G.; Almolla, J.; Salvadore, M. Real-Time Tissue Elastography for Testicular Lesion Assessment. Eur. Radiol. 2012, 22, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Aigner, F.; De Zordo, T.; Pallwein-Prettner, L.; Junker, D.; Schäfer, G.; Pichler, R.; Leonhartsberger, N.; Pinggera, G.; Dogra, V.S.; Frauscher, F. Real-Time Sonoelastography for the Evaluation of Testicular Lesions. Radiology 2012, 263, 584–589. [Google Scholar] [CrossRef]
- Ishida, M.; Hasegawa, M.; Kanao, K.; Oyama, M.; Nakajima, Y. Non-Palpable Testicular Embryonal Carcinoma Diagnosed by Ultrasound: A Case Report. Jpn. J. Clin. Oncol. 2009, 39, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Scandura, G.; Verrill, C.; Protheroe, A.; Joseph, J.; Ansell, W.; Sahdev, A.; Shamash, J.; Berney, D.M. Incidentally Detected Testicular Lesions <10 Mm in Diameter: Can Orchidectomy Be Avoided? BJU Int. 2018, 121, 575–582. [Google Scholar] [CrossRef]
- Stepanas, A.V.; Samaan, N.A.; Schultz, P.N.; Holoye, P.Y. Endocrine Studies in Testicular Tumor Patients with and without Gynecomastia: A Report of 45 Cases. Cancer 1978, 41, 369–376. [Google Scholar] [CrossRef]
- Gerber, D.; Wright, H.C.; Sussman, R.D.; Stamatakis, L. Embryonal Carcinoma Presenting as a Calcified Solitary Testicular Mass on Ultrasound. BMJ Case Rep. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Katabathina, V.S.; Vargas-Zapata, D.; Monge, R.A.; Nazarullah, A.; Ganeshan, D.; Tammisetti, V.; Prasad, S.R. Testicular Germ Cell Tumors: Classification, Pathologic Features, Imaging Findings, and Management. Radiographics 2021, 41, 1698–1716. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Huang, D.Y.; Sidhu, P.S. Elastography of Focal Testicular Lesions: Current Concepts and Utility. Ultrasonography 2019, 38, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Xue, N.; Zhang, S.; Wang, G. The Value of Contrast-Enhanced Ultrasonography in the Diagnosis of Primary Testicular Non-Neoplastic and Neoplastic Lesions in Adults. BMC Urol. 2022, 22, 210. [Google Scholar] [CrossRef]
- Anderson, K.H.; Romao, R.L.P. Testicular Tumors in Children and Adolescents: Long-Term Endocrine and Fertility Issues. Transl. Androl. Urol. 2020, 9, 2393–2399. [Google Scholar] [CrossRef]
- Liu, P.; Phillips, M.J.; Edwards, V.D.; Ein, S.; Daneman, A. Sonographic Findings of Testicular Teratoma with Pathologic Correlation. Pediatr. Radiol. 1992, 22, 99–101. [Google Scholar] [CrossRef]
- Epifanio, M.; Baldissera, M.; Esteban, F.G.; Baldisserotto, M. Mature Testicular Teratoma in Children: Multifaceted Tumors on Ultrasound. Urology 2014, 83, 195–197. [Google Scholar] [CrossRef]
- Pagliaro, L.C. Role of High-Dose Chemotherapy With Autologous Stem-Cell Rescue in Men With Previously Treated Germ Cell Tumors. J. Clin. Oncol. 2017, 35, 1036–1040. [Google Scholar] [CrossRef]
- Lagabrielle, S.; Durand, X.; Droupy, S.; Izard, V.; Marcelli, F.; Huyghe, E.; Ferriere, J.-M.; Ferretti, L. Testicular Tumours Discovered during Infertility Workup Are Predominantly Benign and Could Initially Be Managed by Sparing Surgery. J. Surg. Oncol. 2018, 118, 630–635. [Google Scholar] [CrossRef]
- Maxwell, F.; Savignac, A.; Bekdache, O.; Calvez, S.; Lebacle, C.; Arama, E.; Garrouche, N.; Rocher, L. Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion. Cancers 2022, 14. [Google Scholar] [CrossRef]
- Leonhartsberger, N.; Ramoner, R.; Aigner, F.; Stoehr, B.; Pichler, R.; Zangerl, F.; Fritzer, A.; Steiner, H. Increased Incidence of Leydig Cell Tumours of the Testis in the Era of Improved Imaging Techniques. BJU Int. 2011, 108, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Pozza, C.; Pofi, R.; Tenuta, M.; Tarsitano, M.G.; Sbardella, E.; Fattorini, G.; Cantisani, V.; Lenzi, A.; Isidori, A.M.; Gianfrilli, D.; et al. Clinical Presentation, Management and Follow-up of 83 Patients with Leydig Cell Tumors of the Testis: A Prospective Case-Cohort Study. Hum. Reprod. 2019, 34, 1389–1403. [Google Scholar] [CrossRef] [PubMed]
- Holm, M.; Rajpert-De Meyts, E.; Andersson, A.-M.; Skakkebaek, N.E. Leydig Cell Micronodules Are a Common Finding in Testicular Biopsies from Men with Impaired Spermatogenesis and Are Associated with Decreased testosterone/LH Ratio. J. Pathol. 2003, 199, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Rajpert-De Meyts, E.; Aksglaede, L.; Bandak, M.; Toppari, J.; Jørgensen, N. Testicular Cancer: Pathogenesis, Diagnosis and Management with Focus on Endocrine Aspects. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., Kalra, S., Kaltsas, G., Kapoor, N., Koch, C., Kopp, P., Korbonits, M., Kovacs, C.S., Kuohung, W., Laferrère, B., Levy, M., McGee, E.A., McLachlan, R., New, M., Purnell, J., Sahay, R., Shah, A.S., Singer, F., Sperling, M.A., Stratakis, C.A., Trence, D.L., Wilson, D.P., Eds.; MDText.com, Inc.: South Dartmouth (MA), 2023. [Google Scholar]
- Cheville, J.C.; Sebo, T.J.; Lager, D.J.; Bostwick, D.G.; Farrow, G.M. Leydig Cell Tumor of the Testis: A Clinicopathologic, DNA Content, and MIB-1 Comparison of Nonmetastasizing and Metastasizing Tumors. Am. J. Surg. Pathol. 1998, 22, 1361–1367. [Google Scholar] [CrossRef]
- Washecka, R.; Dresner, M.I.; Honda, S.A.A. Testicular Tumors in Carney’s Complex. J. Urol. 2002, 167, 1299–1302. [Google Scholar] [CrossRef]
- Grogg, J.; Schneider, K.; Bode, P.K.; Kranzbühler, B.; Eberli, D.; Sulser, T.; Lorch, A.; Beyer, J.; Hermanns, T.; Fankhauser, C.D. Sertoli Cell Tumors of the Testes: Systematic Literature Review and Meta-Analysis of Outcomes in 435 Patients. Oncologist 2020, 25, 585–590. [Google Scholar] [CrossRef]
- Connolly, S.S.; D’Arcy, F.T.; Gough, N.; McCarthy, P.; Bredin, H.C.; Corcoran, M.O. Carefully Selected Intratesticular Lesions Can Be Safely Managed with Serial Ultrasonography. BJU Int. 2006, 98, 1005–1007. [Google Scholar] [CrossRef]
- Paffenholz, P.; Held, L.; Loosen, S.H.; Pfister, D.; Heidenreich, A. Testis Sparing Surgery for Benign Testicular Masses: Diagnostics and Therapeutic Approaches. J. Urol. 2018, 200, 353–360. [Google Scholar] [CrossRef]
- Maizlin, Z.V.; Belenky, A.; Kunichezky, M.; Sandbank, J.; Strauss, S. Leydig Cell Tumors of the Testis: Gray Scale and Color Doppler Sonographic Appearance. J. Ultrasound Med. 2004, 23, 959–964. [Google Scholar] [CrossRef]
- Grand, T.; Hermann, A.-L.; Gérard, M.; Arama, E.; Ouerd, L.; Garrouche, N.; Rocher, L. Precocious Puberty Related to Leydig Cell Testicular Tumor: The Diagnostic Imaging Keys. Eur. J. Med. Res. 2022, 27, 67. [Google Scholar] [CrossRef]
- Akman, H.; Ege, G.; Yildiz, S.; Cakiroglu, G. Incidental Bilateral Leydig Cell Tumor of the Testes. Urol. Int. 2003, 71, 316–318. [Google Scholar] [CrossRef] [PubMed]
- Drudi, F.M.; Valentino, M.; Bertolotto, M.; Malpassini, F.; Maghella, F.; Cantisani, V.; Liberatore, M.; De Felice, C.; D’Ambrosio, F. CEUS Time Intensity Curves in the Differentiation Between Leydig Cell Carcinoma and Seminoma: A Multicenter Study. Ultraschall Med. 2016, 37, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Samson, M.; Peale, F.V., Jr; Frantz, G.; Rioux-Leclercq, N.; Rajpert-De Meyts, E.; Ferrara, N. Human Endocrine Gland-Derived Vascular Endothelial Growth Factor: Expression Early in Development and in Leydig Cell Tumors Suggests Roles in Normal and Pathological Testis Angiogenesis. J. Clin. Endocrinol. Metab. 2004, 89, 4078–4088. [Google Scholar] [CrossRef] [PubMed]
- Lock, G.; Schmidt, C.; Helmich, F.; Stolle, E.; Dieckmann, K.-P. Early Experience with Contrast-Enhanced Ultrasound in the Diagnosis of Testicular Masses: A Feasibility Study. Urology 2011, 77, 1049–1053. [Google Scholar] [CrossRef]
- Luzurier, A.; Maxwell, F.; Correas, J.M.; Benoit, G.; Izard, V.; Ferlicot, S.; Teglas, J.P.; Bellin, M.F.; Rocher, L. Qualitative and Quantitative Contrast-Enhanced Ultrasonography for the Characterisation of Non-Palpable Testicular Tumours. Clin. Radiol. 2018, 73, 322–e1. [Google Scholar] [CrossRef]
- Lerchbaumer, M.H.; Auer, T.A.; Marticorena, G.S.; Stephan, C.; Hamm, B.; Jung, E.-M.; Fischer, T. Diagnostic Performance of Contrast-Enhanced Ultrasound (CEUS) in Testicular Pathologies: Single-Center Results. Clin. Hemorheol. Microcirc. 2019, 73, 347–357. [Google Scholar] [CrossRef]
- Pinto, S.P.S.; Huang, D.Y.; Dinesh, A.A.; Sidhu, P.S.; Ahmed, K. A Systematic Review on the Use of Qualitative and Quantitative Contrast-Enhanced Ultrasound in Diagnosing Testicular Abnormalities. Urology 2021, 154, 16–23. [Google Scholar] [CrossRef]
- Young, R.H.; Koelliker, D.D.; Scully, R.E. Sertoli Cell Tumors of the Testis, Not Otherwise Specified: A Clinicopathologic Analysis of 60 Cases. Am. J. Surg. Pathol. 1998, 22, 709–721. [Google Scholar] [CrossRef]
- Harms, D.; Kock, L.R. Testicular Juvenile Granulosa Cell and Sertoli Cell Tumours: A Clinicopathological Study of 29 Cases from the Kiel Paediatric Tumour Registry. Virchows Arch. 1997, 430, 301–309. [Google Scholar] [CrossRef]
- Vitolo, U.; Ferreri, A.J.M.; Zucca, E. Primary Testicular Lymphoma. Crit. Rev. Oncol. Hematol. 2008, 65, 183–189. [Google Scholar] [CrossRef]
- Nguyen, H.T.K.; Terao, M.A.; Green, D.M.; Pui, C.-H.; Inaba, H. Testicular Involvement of Acute Lymphoblastic Leukemia in Children and Adolescents: Diagnosis, Biology, and Management. Cancer 2021, 127, 3067–3081. [Google Scholar] [CrossRef] [PubMed]
- Gutjahr, P.; Humpl, T. Testicular Lymphoblastic Leukemia/lymphoma. World J. Urol. 1995, 13, 230–232. [Google Scholar] [CrossRef] [PubMed]
- de Jesus, L.E.; Dekermacher, S.; Resende, G.C.; Justiniano, R.R. Testicular Involvement in Pediatric Acute Lymphocytic Leukemia: What to Do about It? Int. Braz J Urol 2022, 48, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Koh, S.Y.; Lee, S.; Lee, S.B.; Cho, Y.J.; Choi, Y.H.; Cheon, J.-E.; Kim, W.S. Shear-Wave Elastography for the Assessment of Testicular Involvement of Hematologic Malignancies in Children and Young Adults: A Feasibility Study. Ultrasonography 2022, 41, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Mazzu, D.; Jeffrey, R.B., Jr; Ralls, P.W. Lymphoma and Leukemia Involving the Testicles: Findings on Gray-Scale and Color Doppler Sonography. AJR Am. J. Roentgenol. 1995, 164, 645–647. [Google Scholar] [CrossRef]
- Arrigan, M.; Smyth, L.; Harmon, M.; Flynn, C.; Sheehy, N. Imaging Findings in Recurrent Extramedullary Leukaemias. Cancer Imaging 2013, 13, 26–35. [Google Scholar] [CrossRef]
- Hermann, A.-L.; L’Herminé-Coulomb, A.; Irtan, S.; Audry, G.; Cardoen, L.; Brisse, H.J.; Vande Perre, S.; Pointe, H.D.L. Imaging of Pediatric Testicular and Para-Testicular Tumors: A Pictural Review. Cancers 2022, 14. [Google Scholar] [CrossRef]
- Khan, M.; Rajarubendra, N.; Azer, S.; Skene, A.; Harrison, S.J.; Campbell, B.; Lawrentschuk, N. Plasmacytoma of the Testis in a Patient with Relapsed and Refractory Multiple Myeloma: Case Report and Review of the Literature. Urol. Ann. 2015, 7, 530–533. [Google Scholar] [CrossRef]
- Shimokihara, K.; Kawahara, T.; Chiba, S.; Takamoto, D.; Yao, M.; Uemura, H. Extramedullary Plasmacytoma of the Testis: A Case Report. Urol Case Rep 2018, 16, 101–103. [Google Scholar] [CrossRef]
- Schiavo, C.; Mann, S.A.; Mer, J.; Suvannasankha, A. Testicular Plasmacytoma Misdiagnosed as Orchitis. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef]
- McCann, C.; Doherty, A.; Flynn, C.; Mulholland, C. Prostate Cancer Metastasis to the Testis: An Unexpected Presentation of a Solitary Recurrence. BMJ Case Rep. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Birker, I.L.; van der Zee, J.A.; Keizer, K.M. Uncommon Testicular Metastasis of a Primary Neuroendocrine Tumour of the Lung. Can. Urol. Assoc. J. 2013, 7, E614–E617. [Google Scholar] [CrossRef] [PubMed]
- Hatoum, H.A.; Abi Saad, G.S.; Otrock, Z.K.; Barada, K.A.; Shamseddine, A.I. Metastasis of Colorectal Carcinoma to the Testes: Clinical Presentation and Possible Pathways. Int. J. Clin. Oncol. 2011, 16, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Qazi, H.A.R.; Manikandan, R.; Foster, C.S.; Fordham, M.V. Testicular Metastasis from Gastric Carcinoma. Urology 2006, 68, 890–e7. [Google Scholar] [CrossRef]
- Dusaud, M.; Adjadj, L.; Debelmas, A.; Souraud, J.B.; Durand, X. Malignant Melanoma Revealed by Testicular Metastasi. Int. J. Surg. Case Rep. 2015, 12, 102–105. [Google Scholar] [CrossRef]
- Hou, G.; Jiang, Y.; Cheng, X. Testicular Metastasis of Pancreatic Carcinoma on FDG-PET/CT. Clin. Nucl. Med. 2020, 45, 85–86. [Google Scholar] [CrossRef]
- Rouvinov, K.; Neulander, E.Z.; Kan, E.; Asali, M.; Ariad, S.; Mermershtain, W. Testicular Metastasis from Renal Cell Carcinoma: A Case Report and Review of the Literature. Case Rep. Oncol. 2017, 10, 388–391. [Google Scholar] [CrossRef]
- Turo, R.; Smolski, M.; Hatimy, U.; Bromage, S.J.; Brown, S.C.W.; Brough, R.; Collins, G.N. A Rare Case of Testicular Metastasis of Bladder Transitional Cell Carcinoma. Can. Urol. Assoc. J. 2014, 8, E181–E183. [Google Scholar] [CrossRef]
- Appetecchia, M.; Barnabei, A.; Pompeo, V.; Sentinelli, S.; Baldelli, R.; Corsello, S.M.; Torino, F. Testicular and Inguinal Lymph Node Metastases of Medullary Thyroid Cancer: A Case Report and Review of the Literature. BMC Endocr. Disord. 2014, 14, 84. [Google Scholar] [CrossRef]
- Simon, T.; Hero, B.; Berthold, F. Testicular and Paratesticular Involvement by Metastatic Neuroblastoma. Cancer 2000, 88, 2636–2641. [Google Scholar] [CrossRef]
- Sidhu, P.S.; Sriprasad, S.; Bushby, L.H.; Sellars, M.E.; Muir, G.H. Impalpable Testis Cancer. BJU Int. 2004, 93, 888. [Google Scholar] [CrossRef] [PubMed]
- Iannantuono, G.M.; Strigari, L.; Roselli, M.; Torino, F. A Scoping Review on the “Burned out” or “Burnt out” Testicular Cancer: When a Rare Phenomenon Deserves More Attention. Crit. Rev. Oncol. Hematol. 2021, 165, 103452. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, P.S.; Muir, G.H. Extragonadal Tumor and Testicular Microlithiasis: “Burned-out” Tumors Are Represented by Macrocalcification. J. Ultrasound Med. 2011, 30, 1604–1605. [Google Scholar] [CrossRef]
- Pedersen, M.R.; Bartlett, E.C.; Brown, C.; Rafaelsen, S.R.; Sellars, M.E.; Sidhu, P.S. Is Testicular Macrocalcification a Risk for Malignancy?: Tumor Development on Ultrasonographic Follow-up of Preexisting Intratesticular Macrocalcification. J. Ultrasound Med. 2018, 37, 2949–2953. [Google Scholar] [CrossRef] [PubMed]
- Rocher, L.; Glas, L.; Bellin, M.F.; Ferlicot, S.; Izard, V.; Benoit, G.; Albiges, L.; Fizazi, K.; Correas, J.-M. Burned-Out Testis Tumors in Asymptomatic Infertile Men: Multiparametric Sonography and MRI Findings. J. Ultrasound Med. 2017, 36, 821–831. [Google Scholar] [CrossRef]
- Comiter, C.V.; Renshaw, A.A.; Benson, C.B.; Loughlin, K.R. Burned-out Primary Testicular Cancer: Sonographic and Pathological Characteristics. J. Urol. 1996, 156, 85–88. [Google Scholar] [CrossRef]
- Tasu, J.-P.; Faye, N.; Eschwege, P.; Rocher, L.; Bléry, M. Imaging of Burned-out Testis Tumor: Five New Cases and Review of the Literature. J. Ultrasound Med. 2003, 22, 515–521. [Google Scholar] [CrossRef]
- Fabre, E.; Jira, H.; Izard, V.; Ferlicot, S.; Hammoudi, Y.; Theodore, C.; Di Palma, M.; Benoit, G.; Droupy, S. “Burned-out” Primary Testicular Cancer. BJU Int. 2004, 94, 74–78. [Google Scholar] [CrossRef]


| Non-neoplastic intratesticular lesions | |||||
|---|---|---|---|---|---|
| Clinical presentation | GSUS | CDUS | CEUS | SE | |
| Simple cyst | asymptomatic/ incidental finding, usually not palpable |
rounded anechoic lesions with thin, clear, hyperechoic wall and posterior acoustic enhancement | avascular | unenhanced | soft lesion with high elastic strain |
| Epidermoid cyst | asymptomatic/ can be palpable |
well circumscribed rounded lesion with “onion ring” aspect (concentric hypo- and hyper-echoic rings) OR densely calcified mass with acoustic shadow OR cyst with hypoechoic rim and central calcification OR mixed atypical pattern | avascular | unenhanced/ perilesional rim enhancement |
hard lesion with low/absent elastic strain |
| Adrenal rest | patients with CAH; usually not palpable |
hypoechoic lesions with irregular margins, hyperechogenic foci, typically localized in the mediastinum testis, usually bilateral | markedly vascularized |
hyperenhanced | hard lesions with low/absent elastic strain |
| Sarcoidosis | in the context of a mulsystem disease; granulomas in other organs; asymptomatic OR painless/painful mass | hypoechoic lesions with irregular margins, often bilateral | possible signs of internal vascularization |
hypoenhanced | hard lesions with low/absent elastic strain |
| Segmental infarction | idiopathic or consequent to surgery, inflammatory events, blood disorders or autoimmune diseases; usually acute painful swollen scrotum (but also asymptomatic cases) | hypoechoic wedge-shaped or roundish area | Avascular or peripheral rim of low CD |
unenhanced/ perilesional rim enhancement |
soft lesions with high elastic strain |
| Abscess | acute scrotal pain and swelling/ fever/ high WBC | complex heterogeneous low reflecting lesion with irregular walls (in rare cases focal hyperechoic spots due to gas bubble) | avascular/ vascular rim |
unenhanced/ perilesional rim enhancement |
heterogeneous pattern of firmness |
| Hematoma | history of scrotal trauma | well circumscribed hyperechoic lesions which subsequently liquefy over time, becoming complex lesions with septa, cystic components, and fluid levels. Size decrease over time. | avascular | unenhanced/ perilesional rim enhancement |
soft lesion with intermediate/high elastic strain |
| Idiopathic (diffuse) granulomatous orchitis | in the context of a multisystem disease; asymptomatic OR painless/painful mass | diffusely hypoechoic testis or hypoechoic areas with ill-defined margins | markedly vascularized |
hyperenhanced | heterogeneous pattern of firmness |
| Infectious granulomatous (focal) orchitis | acute scrotal pain, testicular enlargement, and fever; possible epididymal enlargement, scrotal wall thickening and hydrocele | single or multiple variable echogenicity areas with blurred margins; appearance depends by the pathologic stages of infection, which include caseous necrosis, granulomas, and healing by fibrosis and calcification | Internal or peripheral depending on the stage |
unenhanced/ perilesional rim enhancement or hyperehnanced |
heterogeneous pattern of firmness depending on the stage |
| Neoplastic intratesticular lesions | ||||||
|---|---|---|---|---|---|---|
| Clinical presentation | Serum tumor markers | GSUS | CDUS | CEUS | SE | |
| Leydig cell tumor | Generally asymptomatic; it can produce androgens | Negative | Hypoechoic, homogeneous well demarcated lesion (possible hyperechoic halo) |
Hypervascularized | Homogeneously hyperenhanced (rapid wash-in, delayed wash-out) |
Hard lesions with low/absent elastic strain |
| Sertoli cell tumor | Asymptomatic; they can be a part of multiple neoplasia syndromes, such as Carney Complex and Peutz-Jegers | Negative | Hypo- or hyper-echoic lesion, with possible calcifications | Hypervascularized | Homogeneously hyperenhanced |
Hard lesions with low/absent elastic strain |
| Seminoma | testicular swelling, pain, lumbar pain OR asymptomatic palpable firm testicular mass; possible gynecomastia |
Negative (possible increase of -hCG,) |
Hypoechoic homogeneous round or oval lesion, occasionally multinodular or with polycyclic lobulated margins (unfrequently inhomogeneous) |
Hypervascularized, with arborization and branches | Homogeneously hyperenhanced (rapid wash-in and wash-out) |
Hard lesions with low/absent elastic strain |
| Embryonal cell carcinoma | testicular swelling, pain, lumbar pain; palpable firm testicular mass; Possible gynecomastia |
Can be positive -FP, -hCG, LDH (not always) |
Hypoechoic heterogeneous lesions with rregular polylobate margins; can present internal cystic areas or calcific margins. |
Hypervascularized /avascular | Enhanced/unenhanced/ perilesional rim enhancement |
Hard lesions with low/absent elastic strain |
| Teratoma | testicular swelling, pain, lumbar pain; palpable firm testicular mass Possible gynecomastia |
Can be positive -FP, -hCG, LDH (not always) |
Heterogeneous lesions, well-circumscribed, with cystic areas and internal septa | Hypervascularized in the solid part | Inhomogeneously hyperenhanced |
Hard lesions with low/absent elastic strain (depending on liquid amount) |
| Choriocarcinoma | testicular swelling, pain, lumbar pain; palpable firm testicular mass Possible gynecomastia |
Can be positive -hCG, (not always) |
Heterogeneous lesions with hypo-anechoic areas (hemorrhage, necrosis) and calcifications | Hypervascularized | Hyperenhanced | Hard lesions with low/absent elastic strain |
| Yolk sac tumors | testicular swelling, pain, lumbar pain; palpable firm testicular mass |
Can be positive -FP (not always) |
Heterogeneous lesions with anechoic areas | Hypervascularized | Hyperenhanced | Hard lesions with low/absent elastic strain |
| Mixed | testicular swelling, pain, lumbar pain; palpable firm testicular mass; possible gynecomastia |
Can be positive -FP, -hCG, LDH (not always) |
Different aspect in regard to main histological component | Hypervascularized | Homogeneously/ inhomogeneously hyperenhanced |
Hard lesions with low/absent elastic strain |
| Burned-out tumor | lumbar pain, vomit; possible gynecomastia |
Can be positive -FP, -hCG, LDH (not always) |
No testicular nodule; highly echogenic foci or gross calcifications/ hypoechoic irregular areas | Hypovascularized | Unenhanced | / |
| Lymphoma | testicular swelling, pain, and specific lymphoma symptoms; affects men older than 50 years, palpable firm testicular mass |
Negative | Hypoechoic lesions with diffuse infiltration or multifocal hypoechoic lesions of various size | Hypervascularized with linear non-branching pattern | Hyperenhanced | Hard lesions with low/absent elastic strain |
| Leukaemia | More frequent in children and young patients; it can be asymptomatic | Negative | Infiltrating pattern with irregular hypoechoic longitudinal striae/ focal pattern with irregular hypoechoic nodules | Hypervascularized | Inhomogeneously hyperenhanced |
Hard lesions with low/absent elastic strain |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





