1. Introduction
Acute anterior cruciate ligament (ACL)and medial patellofemoral ligament(MPFL) are two important stable structure of the knee. ACL injury results from the knee suddenly changing landing directions, pivoting, or deceleration while MPFL injury results from including not only the kinematic forces but also the anatomical abnormality such as femur or patella morphological abnormality16, 31. Since ACL or MPFL injury will lead to knee pain and functional instability, ACLrupture as well as patellar dislocation are two of the depressing events in knee injuries. so it is important to explore the injury mechanisms of them. Previous studies have explored the mechanisms of patellar dislocation and ACL rupture, including cadaver studies, numerical simulation studies39 and video analysis18, 19,which could help to provide preventions to reduce injury rates for ACL rupture and patellar dislocation4, 9, 17, 23. Though these methods provide valuable information for understanding of the motions leading to ACL rupture and patellar dislocation injury, but the knee joint moving in a three-dimensional space of 6 degrees of freedomsince, video analysis and simple computer model may not simulate the real motion trajectory of knee joint injury accurately.
Traumatically involved, geographic, and nonlinear areas of decreased signal intensity on T1-weighted scans and increased signal intensity on T2-weighted scans after a force on the bone or a bone-to-bone impact is defined as bone bruise14. Bone bruises is commonly observed on magnetic resonance imaging (MRI), followed by ACL rupture or patellar dislocation. As the distribution of bone bruise is like a footprint left behind injury, which providing mechanisms insight to knee injuries, the location patterns and severity of bone bruise in patients may indicated the primary mechanisms of non-contact ACL rupture and patellar dislocation 31, 35.
As early as 1990s, sensitivity intraosseous signal abnormality was found in femoral and tibial after ACL rupture by JH Mink and the medial patellar and lateral femoral after patellar dislocation by E lance20, 24, suggesting that axial MRI would be a valuable adjunct in the evaluation of the acutely injured knee. Previous studies have also shown that bone bruises of the knee on MRI could provide implications for the mechanism of ACL and patellar dislocation injury20, 35, 37. In addition, the bone bruise patterns of femur and tibia in ACL injury differed with the femur and patella bone bruises in patellar dislocation 25, 41, and there are actually limited reports that have compared the bone bruise patterns between different knee injury.
Therefore, the purpose of this retrospective study was to explore the different bone bruise patterns by retrospectively glancing over MRI of ACL rupture and patellar dislocation, which can help us to better understand not only the performance patterns of bone bruise but also the non-contact sports injury mechanism of ACL rupture and patellar dislocation. We hypothesized that the bruise patterns of ACL rupture and patellar dislocation was completely different, we also hypothesized that there are only lateral femur and medial bone bruises in patellar dislocation while there are both lateral and medial bone bruises of femur and tibia in ACL rupture.
2. Materials and Methods
2.1. Selection Criteria and MR Imaging
This retrospective study was approved by our Institutional Ethics Committee from the institutional review board (IRB00006761-M2023142), MR images of 77 ACL rupture and 77 patellar dislocation patients were performed at our institution between August 2020 and March 2022 met the inclusion and exclusion criteria were included in the study. The inclusion criteria were as follows: (1) ACL rupture or patellar dislocation was confirmed by an experienced radiologist and a sport medicine doctor with the help of MRI (2) MRI performed within 4 weeks of injury (3) injury sustained during non-contact, (4) patients aged 18 to 40 years. The 4-week threshold was selected to minimize timing errors further and ensure the signal characteristics of bone bruises 38. Only patients aged 18 to 40 years were selected since bone mineral density decreases gradually in patients aged >40 / 50years, which could affect the signal characteristics of a bone bruise,21, 34. The exclusion criteria were (1) contact injury (2) there are other injuries besides patella dislocation or ACL rupture (3) medial or Vertical patellar dislocation (4) unavailable or poor-quality MRI scans. Clinical notes, operative reports, and MRI scans were retrospectively reviewed to provide detailed information about the injury.
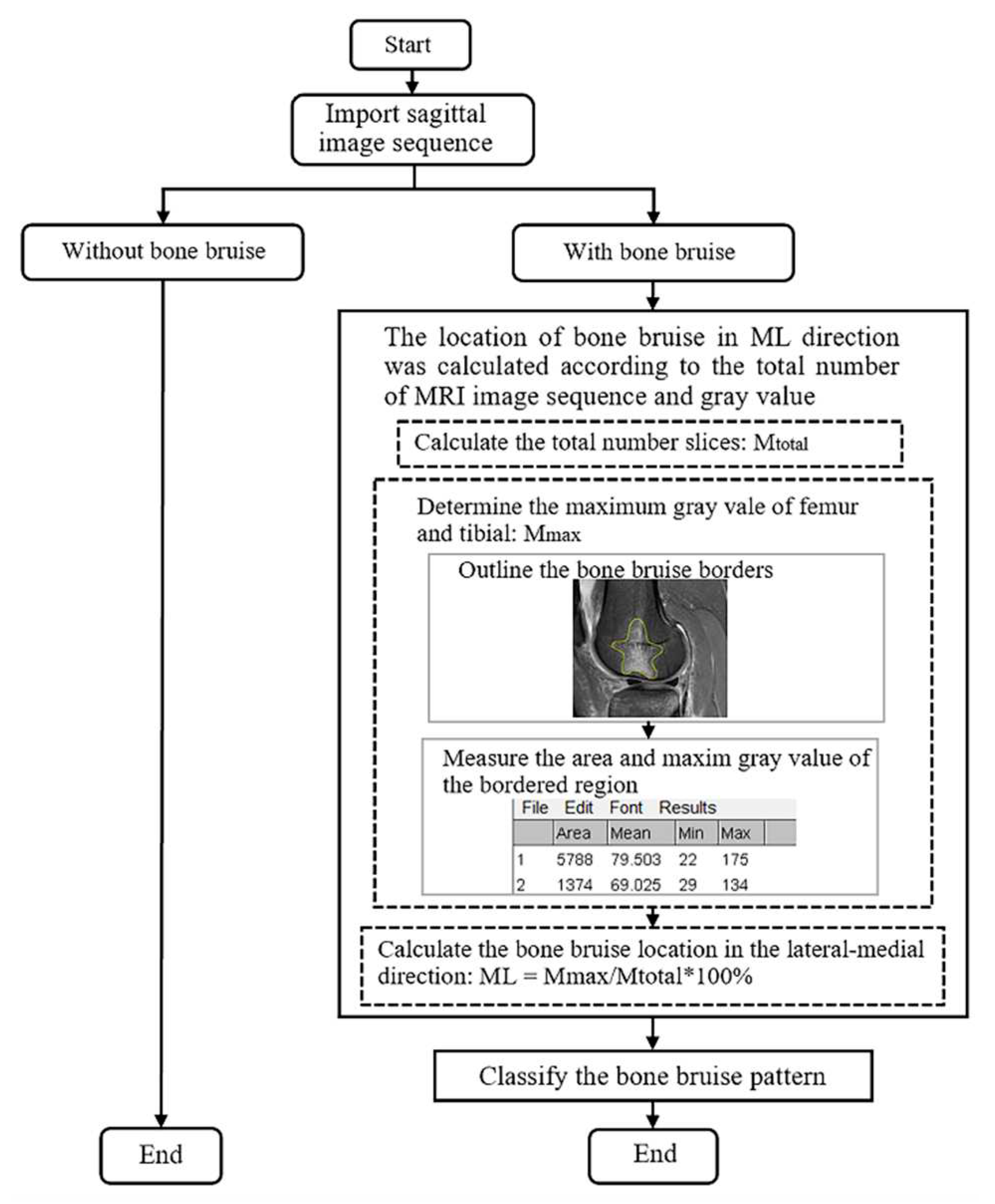
2.2. Determination of Bone Bruise Location
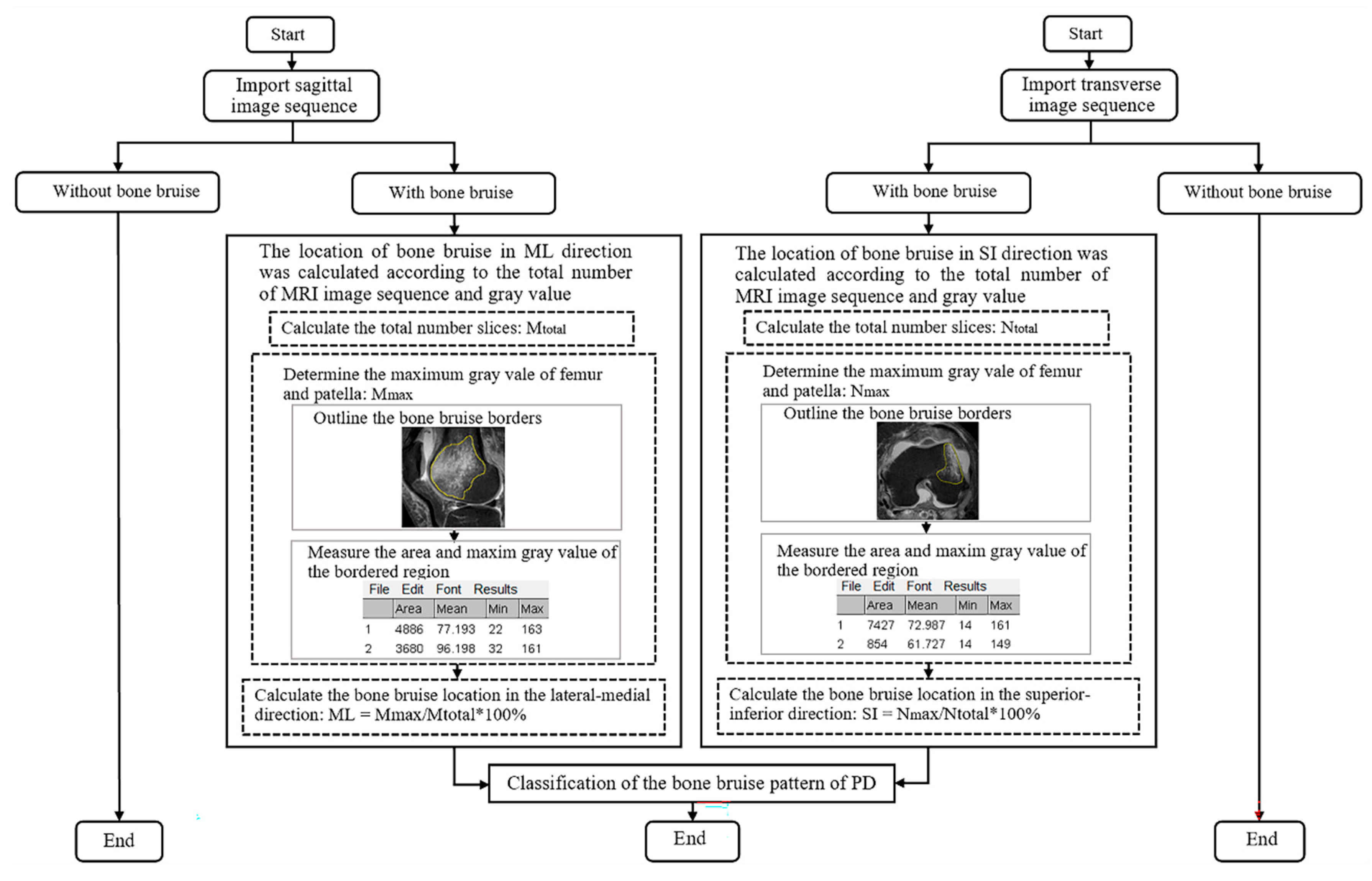
Standard scans were acquired on a 1.5-T scanner (SIGNA; GE Healthcare) with a 3.5-mm slice space and 512 × 512 matrix in the sagittal and transverse planes of the injured knee of ACL rupture or patellar dislocation patients. Imaging sequences of the sagittal and transverse planes were used to determine the bone bruise location in the lateral-medial and superior-inferior directions, respectively. First classified the participants according to the presence or absence of bone bruise, then the bone bruise borders were traced using the freehand region-of-interest function of the ImageJ software (National Institutes of Health), and the gray values were recorded based on imaging pixels. The signal intensity could reflect the impact of bone since the gray value of pixels is determined by the MRI signal intensity of the voxel represented on MRI. The maximum gray value of the pixels and the boundary area was measure by ImageJ. The gray value was used to evaluate the severity of bone bruise within an imaging sequence in this study. The larger the gray value, the greater the signal intensity and the more serious the bone bruise. The largest gray value was considered the site of bone impact. When a bone bruise showing the same maximum gray value in different slices, the level of the bone bruise was further determined according to the area.
The bone bruise location in the lateral-medial and superior-inferior directions was first determined using a sagittal and transverse plane imaging sequence. (
Figure 1 and
Figure 2). The precise locations in the lateral-medial direction were confirmed using the following formula:
Mmax is defined as the number of slices at which the gray value is maximum among all the slices in the order of lateral-medial sides in the sagittal plane, whereas Mtotal is the total number of slices in the sagittal plane based on the presence of bone segments. ML is a measure of the location in the lateral-medial direction, and it ranges from 0% (closer to the lateral side of the femoral trochlea or patellar) to 100% (closer to the medial side of the femoral trochlea or patellar).
The method of precise bone bruise location in the superior-inferior direction was similar to the lateral-medial sides of the bone, which was determined using the following formula:
Nmax is defined as the number of slices at which the gray value is maximum among all the slices in the order of superior-inferior sides in the transverse plane, whereas Ntotal is the total number of slices in the transverse plane based on the presence of bone segments. SI is a measure of the location in the superior-inferior direction, and it ranges from 0% (closer to the superior side of the femoral trochlea or patellar) to 100% (closer to the inferior side of the femoral trochlea or patellar). Selecting the image of the largest anterior and posterior diameter of the femoral condyle as the reference, bone bruise in femur most superior ends was defined as the location where three slices (10.5mm) from horizontal tangent of femoral posterior condyle cartilage margin, and bone bruise in femur most inferior ends was defined as where horizontal tangent parallel to the bottom of femoral condyle in sagittal plane.
2.3. Statistical Analysis
Kolmogorov–Smirnov test was used to evaluate whether the data conformed to a normal distribution. Continuous data was described as mean ± standard deviation (SD), whereas non-normal distribution data are expressed as the mean with interquartile range, M (Q1, Q3). Categorical data was described as number. Unpaired Student t tests were used to detect differences between the ACL rupture and dislocation groups in the continuous variables. Mann-Whitney tests was used to detect differences between the ACL rupture and dislocation groups of non-normal distribution data of the continuous and categorical variables (age, time from injury, sex, injury causes). A p-value of <0.05 was considered statistically significant.
3. Result
3.1. Descriptive statistics
MR images of 77 ACL rupture (63 men [81.8%], 14 women [18.2%], aged 29.06 ± 6.09 years) and 77 patellar dislocation (32 men [41.6%], 45 women [58.4%], aged 24.83 ± 6.02 years) patients met the inclusion criteria and were recorded in the study (
Table 1). The causes of ACL rupture are all sports while nearly half of patellar dislocation were caused by daily activities. The epidemiology of patients of age, BMI, sex, and injury causing events were significantly different between ACL rupture and patellar dislocation group (
Table 1).
3.2. Bone bruises patterns of ACL rupture and patellar dislocation.
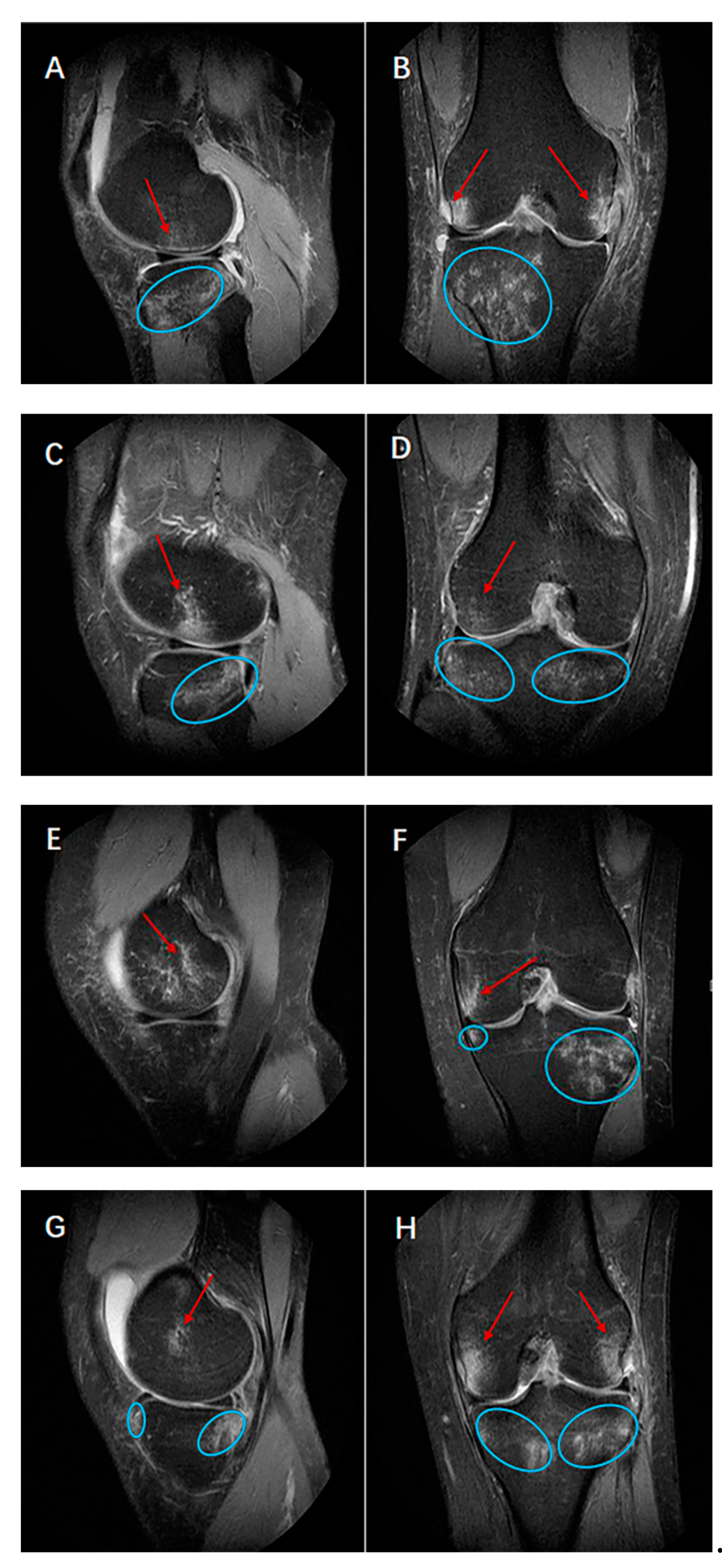
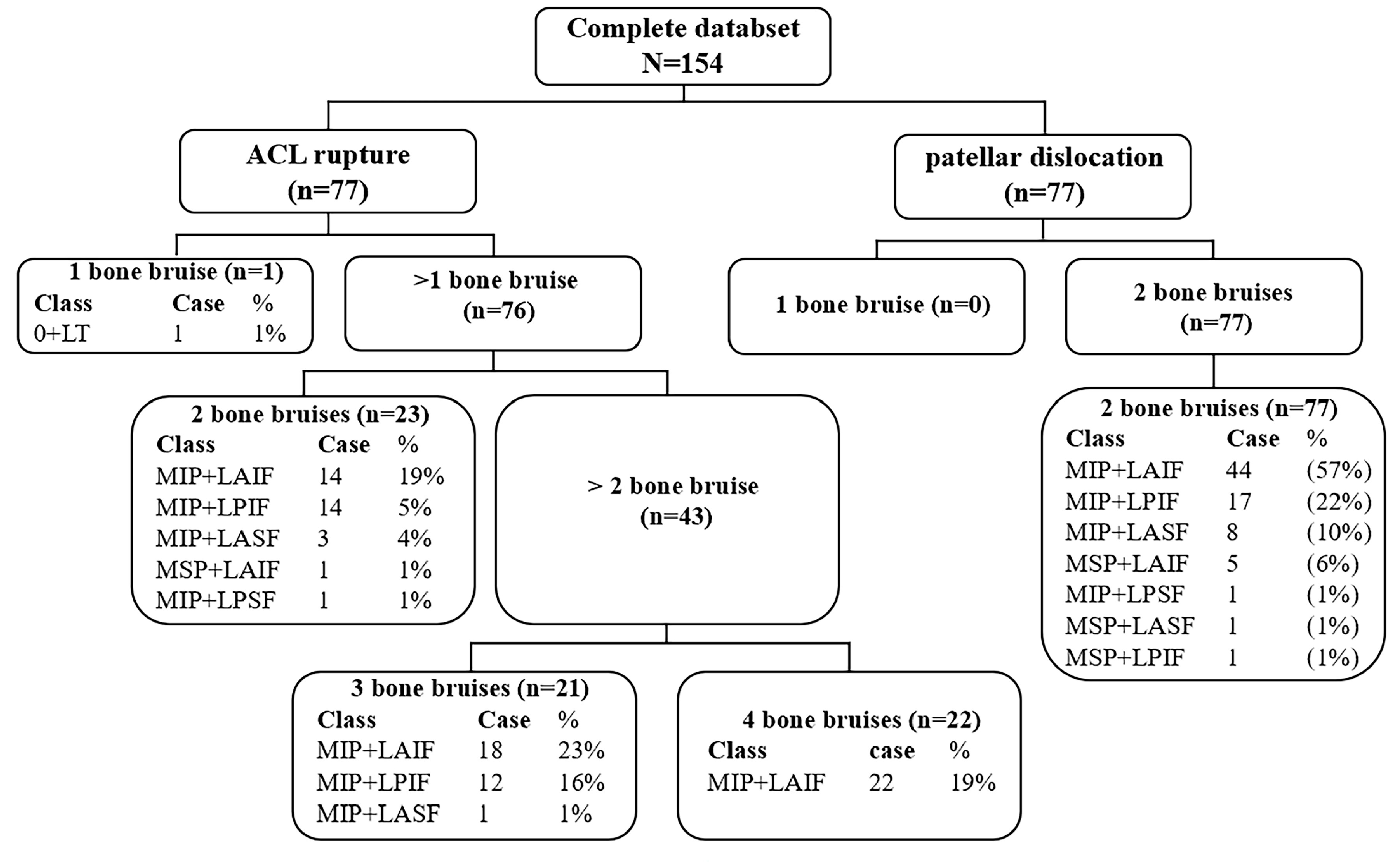
By calculating the position of bone bruises in sagittal and coronal planes, there were 4 kinds of bone bruise (1-,2-,3-,4- bone bruises) patterns among ACL rupture bone bruise patients (
Table 2). The most common two patterns of ACL rupture were 3 (40%) bone bruises (lateral side of femur and both lateral and medial side of tibia, LF+BT [23%]; both lateral and medial side of femur and lateral side of tibia, BF+LT [16%], medial side of femur and both lateral and medial side of tibia, MF+BT [1%]), followed by 4 (29%) bone bruises (both lateral and medial side of femur and tibia, BF+BT) (
Figure 3, A-H) and 2 (30%) bone bruises (lateral side of femur and tibia, LF+LT [19%]; medial side of femur and lateral side of tibia, MF+LT [5%];lateral side of femur and medial side of tibia, LF+MT [4%]; medial side of femur and tibia, MF+MT [1%]; lateral and medial side of tibia, 0+BT [1%]). Only 1 bone bruise including lateral side of tibia (0+LT, 1%).
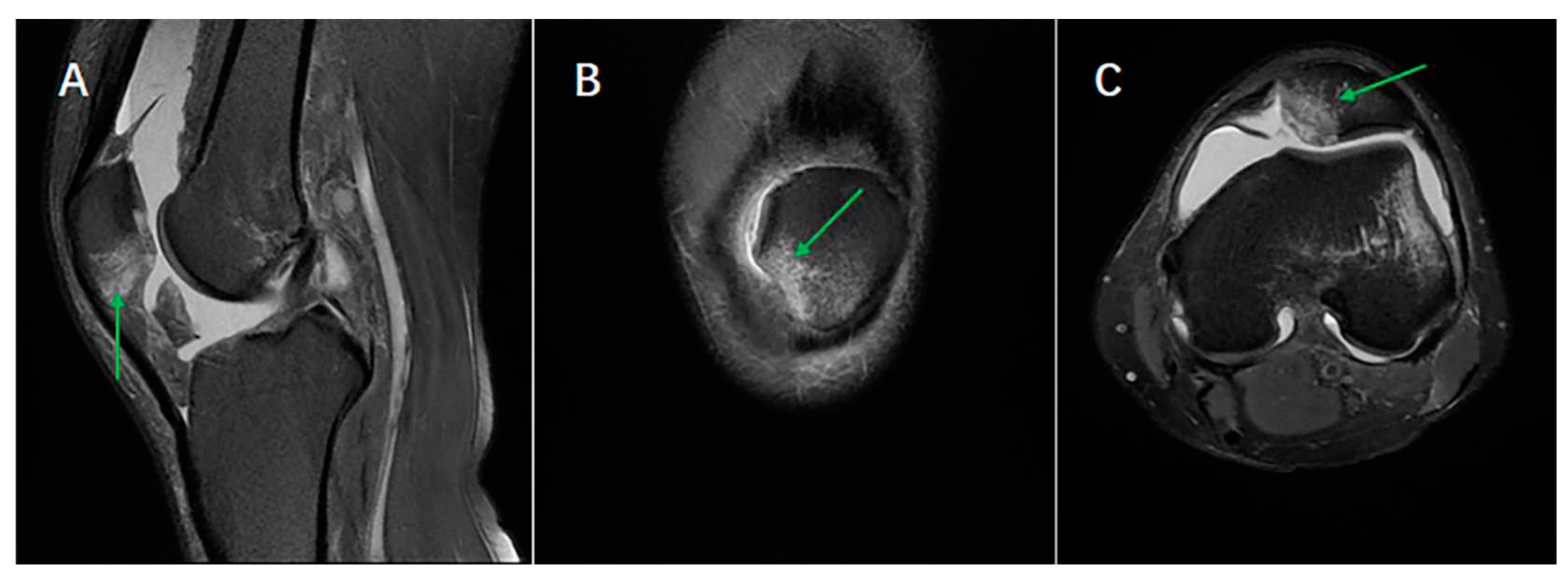
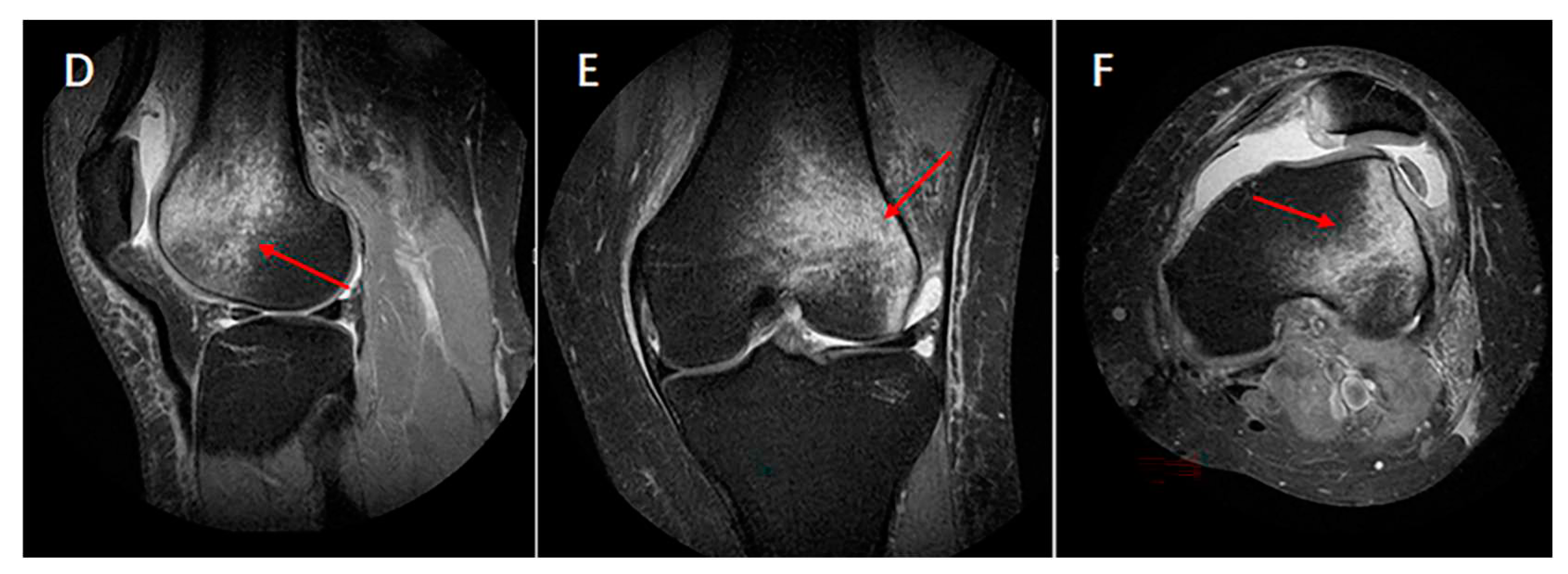
By calculating the position of bone bruises in sagittal and transvers planes, there was only 1 pattern bone bruise (latera femur and medial patella bone bruise) of patellar dislocation (
Figure 4), bone bruise was in the inferior medial patella and lateral anterior inferior femur (
Table 3), and seven categories of bone bruises characteristics were obtained as follows, MIP+LAIF (medial inferior side of patellar and lateral anterior inferior side of femur, 57%); MIP+LPIF (medial inferior side of patellar and lateral posterior inferior side of femur, 22%); MIP+LASF (medial inferior side of patellar and lateral anterior superior of femur, 10%); MSP+LAIF (medial superior side of patellar and lateral anterior inferior side of femur, 6%); MIP+LPSF (medial inferior side of patellar and lateral posterior superior side of femur,1%); MSP+LASF (medial superior side of patellar and lateral anterior superior of femur,1%); MSP+LPIF (medial superior side of patellar and lateral posterior inferior side of femur,1%).
4. Discussion
The purpose of this study was to summarize and compare the different bone bruises patterns between ACL rupture and patellar dislocation. Previous studies have already reported that there were femur and tibial bone bruise of ACL rupture and patellar and femur bone bruise of patellar dislocation
11, 14, 15, 17, 35. However, the bone bruise patterns didn’t be systematically counted and made a comparison between ACL rupture and patellar dislocation. In total 4 types of bone bruise patterns after ACL rupture and 1 type after patellar dislocation were counted and classified by our study, which would help understand their different epidemiology characteristics and injury mechanisms (
Table 2 and
Table 3).
Methods were used to explore the mechanism of knee joint injury. Pretty good consistent bone bruise patterns were revealed between MRI and video analysis in professional football players with an acute ACL knee injury6. Bone bruise is a phenomenon caused by bone-bone hitting or bone suffering heaven strain one-sidedness observed on MR images as decreased signal intensity on T1-weighted scans and increased signal intensity on T2-weighted14. Studies have reported the femur and patellar bone bruise locations of patellar dislocation patients, and the femur and tibia bone bruises of ACL injury patients2, 5, 17, 27; however, they separately reported the frequency and location of the coronal section and, did not combine the sagittal and cross-sectional locations in patients. Furthermore, the femur and patella as well as tibial are all three-dimensional structures39, the location of bone bruises in various sections provides valuable clues to the associated injuries, which would help in understanding the mechanism of ACL rupture and patellar dislocation 32, 37. Therefore, we hypothesized that the bruise patterns of ACL rupture and patellar dislocation was completely different, we also hypothesized that there are only lateral femur and medial bone bruises in patellar dislocation while there are both lateral and medial bone bruises of femur and tibia in ACL rupture.
AB, lateral side of femur and both lateral and medial side of tibia (LF+BT); CD, both lateral and medial side of femur and lateral side of tibia (BF+LT); EF, medial side of femur and both lateral and medial side of tibia (MF+BT); GH, both lateral and medial side of femur and tibia (BF+BT).
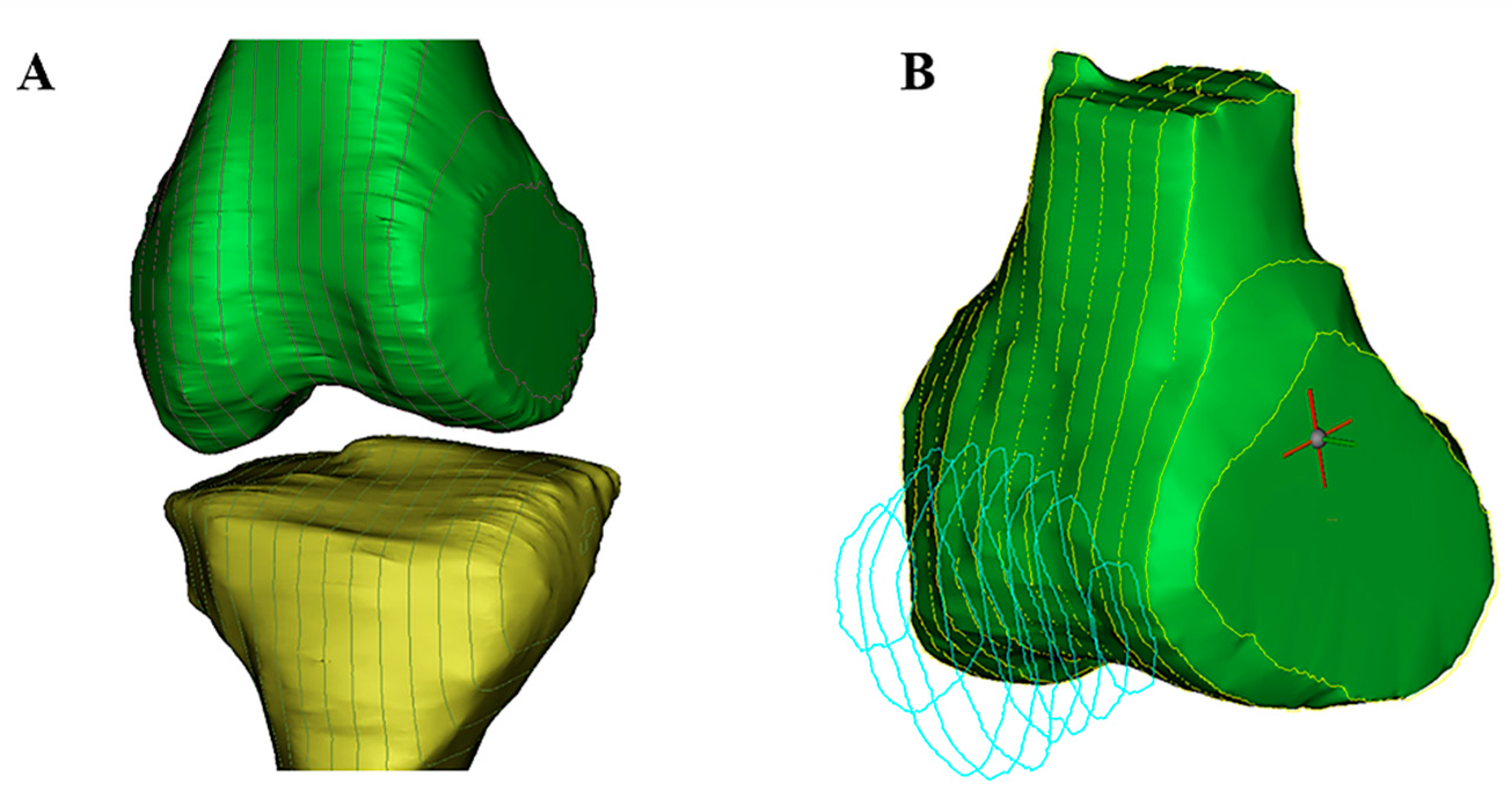
To test our hypotheses, we reviewed the MR images ACL rupture and patellar dislocation patients with bone bruises. Imaging sequences of the sagittal and transverse planes were used to quantitatively calculated relative lateral-medial and superior-inferior direct positions of bone bruises in distal femur, proximal tibia and patella. As showed in our study, there were 4 (1-,2-,3-,4-) kinds of bone bruise patterns of ACL rupture, and the commonly seen bone bruise patterns were 3- (LF+BT, BF+LT, MF+BT) , followed by 4 (BF+BT) and 2- (LF+LT, MF+LT, LF+MT, MF+MT, 0+BT;
Table 2) bone bruises in femur and tibial respectively while there was only 1 pattern of patellar dislocation which in lateral femur and medial patella (
Figure 1 and
Figure 2,
Table 3). ACL rupture and patellar dislocation have the completely different bone bruise patterns which may represents the different injury mechanisms of the knee. The ACL rupture patients who displayed 1- bone bruises of femur and tibia respectively, suggesting that the knee displayed anterior and translated tibia to the femur at the time of injury. The ACL rupture patients who displayed 3- or 4- bone bruises in 1- or 2- femur and 2- tibia suggesting that the knee joint was unstable when ACL was injured, not only anterior and translated tibia to the femur but also shaking obviously in the lateral-medial direction was performed of the knee at the time of injury. Similarly, the difference of the superior-inferior direct positions of femoral and patellar bone bruises in patellar dislocation also indicated that different bone bruise patterns reflect different knee flexion angles at the time of injury (
Figure 4 and
Figure 5).
Although many studies have been conducted on the bone bruise locations, they only pointed out the bone bruises, there is no description of the specific location, nor has there been a systematic report on the pattern classification of bone bruises after ACL rupture and patellar dislocation
2, 5, 35. Our study not only recorded the bone bruise but also calculate the specific location of bone bruises of ACL rupture and patellar dislocation (
Figure 6). For non-contact sports knee injury, bone bruise is not only an intensity signal, but also a footprint of damaging process, which could be as implications of injury mechanism, or the product of the mechanism since different mechanisms of injury have different bone bruise patterns
25. Numerical optimization was used to maximize overlap of the bone bruises on the femur and tibia and to predict the position of injury by Kim Sophia Y, at al who choose the most commonly 3- and 4-bone bruise of ACL rupture as Infrastructure to create 3-dimensional surface models, and found landing on an extended knee is a high risk for ACL injury
15, 17 while others found that knee valgus is the critical component of the injury mechanism
12, 19, 26. However, maybe the initial injury mechanism of 3- and 4-bone bruise of ACL rupture was different. Our study found that the bone bruise patterns of ACL rupture and patellar dislocation injury was completely different. This is related to the different anatomical structures since ACL rupture causing femur and tibial instantaneous impact each other, while patellar dislocation caused by injury of medial patellofemoral ligament partly due to the abnormal anatomy of patella and femur
8, 33.
Although the bone bruises patterns are completely different, they represent their own sports injury mechanism. It was found that the video analysis is consistent with the pattern of bone bruise, which showed that it was feasible and scientific to analyze the injury mechanism according to the bone bruise, and it was also mentioned that although the same kind of injury, different bone bruise patterns may represent different sports injury mechanism patterns6, 7, 29. A more scientific and targeted model combined specific bone bruise pattern should be established to explore the mechanism of non-contact sport injury1.
In addition, characteristics of the patient cohorts, including age, sex, and injury causing events were significantly different between ACL rupture and patellar dislocation group (
Table 1). Age of the patellar dislocation patients was significant younger than that of ACL rupture, and there were more men (81.8%) in ACL rupture group while there were more women (58.4%) in patellar dislocation group. Although the rate of ACL rupture of women were three times higher in mens
40, the results of this study that ACL injury was greater in men than women was due to higher total number of men participating in high level sports, increasing the number of people of tibial forward movement as well as landing torsion, which are the risk factors for ACL injury
3. In our study, the causes of ACL rupture were all sports (100%) while the causes of patellar dislocation were only (54.5%), and the remaining 45.5% patellar dislocation was result from daily activities. As for patellar dislocation patients, since almost all of them have anatomical abnormalities
10, 13, which will more easily result in the patella slips to the outside of the knee joint than those who haven’t anatomical abnormalities, not only the sports activities, but also usual knee flexion and torsion, which is more common occur among women, especially in children
22, 28, 30.
4.1. Limitation
There are several limitations of our study. First, the sample size is too small to reflects the difference between ACL rupture and patellar dislocation with patient information and bone bruise patterns. Second, we didn’t compare the anatomical indexes between the ACL rupture and patellar dislocation.
5. Conclusions
The pattern of bone bruise after ACL rupture and patellar dislocation is completely different. There were 4 kinds (1-,2-,3-,4- bone bruises) bone bruises in femur and tibial of ACL patients while there was only 1 kind bone bruise pattern of patellar dislocation in the inferior medial patella and lateral anterior inferior femur. The epidemiology of ACL rupture and patellar dislocation was also quite different.
References
- Agostinone P., S. Di Paolo, G. A. Lucidi, G. Dal Fabbro, A. Grassi, S. Zaffagnini. Severe bicompartmental bone bruise is associated with rotatory instability in anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc.30:1725-1732,2022. [CrossRef]
- Berger N., G. Andreisek, A. T. Karer, S. Bouaicha, A. Naraghi, A. Manoliu, B. Seifert, E. J. Ulbrich. Association between traumatic bone marrow abnormalities of the knee, the trauma mechanism and associated soft-tissue knee injuries. Eur Radiol.27:393-403,2017. [CrossRef]
- Boden B. P., F. T. Sheehan, J. S. Torg, T. E. Hewett. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg.18:520-527,2010. [CrossRef]
- Bolbos R. I., C. B. Ma, T. M. Link, S. Majumdar, X. Li. In vivo T1rho quantitative assessment of knee cartilage after anterior cruciate ligament injury using 3 Tesla magnetic resonance imaging. Investigative radiology.43:782-788,2008.
- Cao H., Q. An, B. Gou, S. Ma, E. L. Goh, L. Xiong, Y. G. Li, F. Ao. A new classification of injury patterns of the medial patellofemoral ligament after acute lateral patella dislocation detected using magnetic resonance imaging studies. Injury.50:534-540,2019. [CrossRef]
- D'Hooghe P., A. Grassi, F. D. Villa, K. Alkhelaifi, E. Papakostas, R. Rekik, T. Marin, F. Tosarelli, S. Zaffagnini. The injury mechanism correlation between MRI and video-analysis in professional football players with an acute ACL knee injury reveals consistent bone bruise patterns. Knee Surg Sports Traumatol Arthrosc.31:121-132,2023. [CrossRef]
- Deangelis J. P., K. P. Spindler. Traumatic Bone Bruises in the Athlete's Knee. Sports Health.2:398-402,2010. [CrossRef]
- Diederichs G., T. Köhlitz, E. Kornaropoulos, M. O. Heller, B. Vollnberg, S. Scheffler. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med.41:51-57,2013. [CrossRef]
- Farahmand F., M. Naghi Tahmasbi, A. Amis. The contribution of the medial retinaculum and quadriceps muscles to patellar lateral stability--an in-vitro study. Knee.11:89-94,2004. [CrossRef]
- Fones L., A. E. Jimenez, C. Cheng, N. Chevalier, M. B. Brimacombe, A. Cohen, J. L. Pace. Trochlear Dysplasia as Shown by Increased Sulcus Angle Is Associated With Osteochondral Damage in Patients With Patellar Instability. Arthroscopy.37:3469-3476,2021. [CrossRef]
- Green D. W., S. Hidalgo Perea, A. M. Kelly, H. G. Potter. Bone Marrow Edema Injury Patterns in the Pediatric Knee: An MRI Study. HSS journal : the musculoskeletal journal of Hospital for Special Surgery.19:107-112,2023.
- Hewett T. E., G. D. Myer, K. R. Ford, R. S. Heidt, Jr., A. J. Colosimo, S. G. McLean, A. J. van den Bogert, M. V. Paterno, P. Succop. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med.33:492-501,2005.
- Imhoff F. B., V. Funke, L. N. Muench, A. Sauter, M. Englmaier, K. Woertler, A. B. Imhoff, M. J. Feucht. The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc.28:897-904,2020.
- Kaplan P. A., R. H. Gehl, R. G. Dussault, M. W. Anderson, D. R. Diduch. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology.211:747-753,1999. [CrossRef]
- Kim-Wang S. Y., C. E. Spritzer, K. Owusu-Akyaw, J. A. Coppock, A. P. Goode, Z. A. Englander, J. R. Wittstein, L. E. DeFrate. The Predicted Position of the Knee Near the Time of ACL Rupture Is Similar Between 2 Commonly Observed Patterns of Bone Bruising on MRI. Am J Sports Med.51:58-65,2023.
- Kim H. K., S. Parikh. Patellofemoral Instability in Children: Imaging Findings and Therapeutic Approaches. Korean journal of radiology.23:674-687,2022.
- Kim S. Y., C. E. Spritzer, G. M. Utturkar, A. P. Toth, W. E. Garrett, L. E. DeFrate. Knee Kinematics During Noncontact Anterior Cruciate Ligament Injury as Determined From Bone Bruise Location. Am J Sports Med.43:2515-2521,2015. [CrossRef]
- Koga H., A. Nakamae, Y. Shima, R. Bahr, T. Krosshaug. Hip and Ankle Kinematics in Noncontact Anterior Cruciate Ligament Injury Situations: Video Analysis Using Model-Based Image Matching. Am J Sports Med.46:333-340,2018. [CrossRef]
- Koga H., A. Nakamae, Y. Shima, J. Iwasa, G. Myklebust, L. Engebretsen, R. Bahr, T. Krosshaug. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med.38:2218-2225,2010.
- Lance E., A. L. Deutsch, J. H. Mink. Prior lateral patellar dislocation: MR imaging findings. Radiology.189:905-907,1993. [CrossRef]
- Lin X., H. Guo, Y. Lian, J. Kou, G. Wang, Y. Chen, J. Wang, X. Han, M. Jiang, Q. Yang. Osteoporosis and Related Health Status Among the Elderly Urban Residents in Elderly-Care Inns in Beijing, a Multicenter DXA Survey. Frontiers in endocrinology.13:875678,2022. [CrossRef]
- Lyons J. G., T. L. Hudson, A. B. Krishnamurthy. Epidemiology of patellar dislocations in the United States from 2001 to 2020: results of a national emergency department database. Phys Sportsmed.1-10,2022. [CrossRef]
- Marchetti D. C., G. Moatshe, B. M. Phelps, K. D. Dahl, M. B. Ferrari, J. Chahla, T. L. Turnbull, R. F. LaPrade. The Proximal Tibiofibular Joint: A Biomechanical Analysis of the Anterior and Posterior Ligamentous Complexes. Am J Sports Med.45:1888-1892,2017. [CrossRef]
- Mink J. H., A. L. Deutsch. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology.170:823-829,1989.
- Moran J., M. S. Lee, K. N. Kunze, J. S. Green, L. D. Katz, A. Wang, W. M. McLaughlin, S. M. Gillinov, A. E. Jimenez, T. E. Hewett, R. F. LaPrade, M. J. Medvecky. Examining the Distribution of Bone Bruise Patterns in Contact and Noncontact Acute Anterior Cruciate Ligament Injuries. Am J Sports Med.51:1155-1161,2023. [CrossRef]
- Owusu-Akyaw K. A., S. Y. Kim, C. E. Spritzer, A. T. Collins, Z. A. Englander, G. M. Utturkar, W. E. Garrett, L. E. DeFrate. Determination of the Position of the Knee at the Time of an Anterior Cruciate Ligament Rupture for Male Versus Female Patients by an Analysis of Bone Bruises. Am J Sports Med.46:1559-1565,2018.
- Paakkala A., P. Sillanpää, H. Huhtala, T. Paakkala, H. Mäenpää. Bone bruise in acute traumatic patellar dislocation: volumetric magnetic resonance imaging analysis with follow-up mean of 12 months. Skeletal Radiol.39:675-682,2010. [CrossRef]
- Parikh S. N., M. G. Lykissas, I. Gkiatas. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med.11:253-260,2018. [CrossRef]
- Patel S. A., J. Hageman, C. E. Quatman, S. C. Wordeman, T. E. Hewett. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports medicine (Auckland, N.Z.).44:281-293,2014. [CrossRef]
- Pruneski J., L. O'Mara, G. S. Perrone, A. M. Kiapour. Changes in Anatomic Risk Factors for Patellar Instability During Skeletal Growth and Maturation. Am J Sports Med.50:2424-2432,2022. [CrossRef]
- Qiu L., B. Sheng, J. Li, Z. Xiao, M. Yuan, H. Yang, F. Lv, F. Lv. Mechanisms of non-contact anterior cruciate ligament injury as determined by bone contusion location and severity. Quantitative imaging in medicine and surgery.11:3263-3273,2021. [CrossRef]
- Quatman C. E., A. Kiapour, G. D. Myer, K. R. Ford, C. K. Demetropoulos, V. K. Goel, T. E. Hewett. Cartilage pressure distributions provide a footprint to define female anterior cruciate ligament injury mechanisms. Am J Sports Med.39:1706-1713,2011. [CrossRef]
- Richmond C. G., K. G. Shea, J. F. Burlile, A. M. Heyer, H. B. Ellis, P. L. Wilson, E. A. Arendt, M. A. Tompkins. Patellar-Trochlear Morphology in Pediatric Patients From 2 to 11 Years of Age: A Descriptive Analysis Based on Computed Tomography Scanning. J Pediatr Orthop.40:e96-e102,2020. [CrossRef]
- Sanchez-Trigo H., J. Rittweger, B. Sañudo. Effects of non-supervised exercise interventions on bone mineral density in adult women: a systematic review and meta-analysis. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA.33:1415-1427,2022.
- Sanders T. G., M. A. Medynski, J. F. Feller, K. W. Lawhorn. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics.20 Spec No:S135-151,2000.
- Shi H., L. Ding, Y. Jiang, H. Zhang, S. Ren, X. Hu, Z. Liu, H. Huang, Y. Ao. Bone Bruise Distribution Patterns After Acute Anterior Cruciate Ligament Ruptures: Implications for the Injury Mechanism. Orthop J Sports Med.8:2325967120911162,2020. [CrossRef]
- Shi H., L. Ding, S. Ren, Y. Jiang, H. Zhang, X. Hu, H. Huang, Y. Ao. Prediction of Knee Kinematics at the Time of Noncontact Anterior Cruciate Ligament Injuries Based on the Bone Bruises. Annals of biomedical engineering.49:162-170,2021. [CrossRef]
- Shi H., L. Ding, S. Ren, Y. Jiang, H. Zhang, X. Hu, H. Huang, Y. Ao. Response to the Letter to the Editor on "Prediction of Knee Kinematics at Time of Noncontact Anterior Cruciate Ligament Injuries Based on Bone Bruises". Annals of biomedical engineering.49:4-6,2021. [CrossRef]
- Spang R. C., A. Jahandar, K. N. Meyers, J. T. Nguyen, S. A. Maher, S. M. Strickland. Dysplastic Patellofemoral Joints Lead to a Shift in Contact Forces: A 3D-Printed Cadaveric Model. Am J Sports Med.49:3344-3349,2021.
- Sutton K. M., J. M. Bullock. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg.21:41-50,2013.
- Tompkins M. A., S. R. Rohr, J. Agel, E. A. Arendt. Anatomic patellar instability risk factors in primary lateral patellar dislocations do not predict injury patterns: an MRI-based study. Knee Surg Sports Traumatol Arthrosc.26:677-684,2018.
Figure 1.
Method of calculating the bone bruise location to classify the bone bruise pattern of ACL in sagittal plane.
Figure 1.
Method of calculating the bone bruise location to classify the bone bruise pattern of ACL in sagittal plane.
Figure 2.
Method of calculating the bone bruise location to classify the bone bruise pattern of patellar dislocation in sagittal and transvers plane.
Figure 2.
Method of calculating the bone bruise location to classify the bone bruise pattern of patellar dislocation in sagittal and transvers plane.
Figure 3.
The most common 3 bone bruises and 4 bone bruises patterns of ACL rupture. ACEG, sagittal plane; BDFH, coronal plane. Red arrow, femoral bone bruise. Blue ellipse, tibia bone bruise.
Figure 3.
The most common 3 bone bruises and 4 bone bruises patterns of ACL rupture. ACEG, sagittal plane; BDFH, coronal plane. Red arrow, femoral bone bruise. Blue ellipse, tibia bone bruise.
Figure 4.
Distribution of patellar bone bruise in three planes of patellar dislocation patients. A(D), sagittal plane; B€, coronal plane; C(F), transverse plane. Red arrow, femoral bone bruise. Green arrow, patella bone bruise.
Figure 4.
Distribution of patellar bone bruise in three planes of patellar dislocation patients. A(D), sagittal plane; B€, coronal plane; C(F), transverse plane. Red arrow, femoral bone bruise. Green arrow, patella bone bruise.
Figure 5.
Segmentation of bone in sagittal plane. A, segmentation of femur and tibial of ACL rupture patients by MRI. B, segmentation of femur and patella of patellar dislocation patients by MRI. Green, femur; yellow, tibial; blue, patella.
Figure 5.
Segmentation of bone in sagittal plane. A, segmentation of femur and tibial of ACL rupture patients by MRI. B, segmentation of femur and patella of patellar dislocation patients by MRI. Green, femur; yellow, tibial; blue, patella.
Figure 6.
Classification tree of one bruise patterns of ACL rupture and patellar dislocation. LF+BT, BF+LT, MF+BT, BF+BT, LF+LT, MF+LT, LF+MT, MF+MT, 0+BT, 0+LT, MIP+LAIF, MIP+LPIF, MIP+LASF, MSP+LAIF, MIP+LPSF, MSP+LASF, MSP+LPIF, the annotation seen above.
Figure 6.
Classification tree of one bruise patterns of ACL rupture and patellar dislocation. LF+BT, BF+LT, MF+BT, BF+BT, LF+LT, MF+LT, LF+MT, MF+MT, 0+BT, 0+LT, MIP+LAIF, MIP+LPIF, MIP+LASF, MSP+LAIF, MIP+LPSF, MSP+LASF, MSP+LPIF, the annotation seen above.
Table 1.
Patients Information.
Table 1.
Patients Information.
| |
ACL rupture |
Patellar Dislocation |
P value |
| Age |
29.06 ± 6.09 |
24.83 ± 6.02 |
< .001 |
| BMI |
23.98 ± 3.29 |
23.50 ± 3.67 |
.404 |
| Time from injury (d) |
19.22 ± 6.40 |
14.45 ± 8.66 |
< .001 |
| Sex, man/woman, n |
63/14 |
32/45 |
.001 |
| Injury side, left/right, n |
43/34 |
49/28 |
.326 |
| Causing sports / daily activities, n |
77/0 |
42/35 |
< .001 |
Table 2.
Bone bruise patterns of ACL rupture a.
Table 2.
Bone bruise patterns of ACL rupture a.
| |
Bone Bruise Pattern |
N (%) |
| 3 bone bruises |
|
|
| |
LF+BT |
18 (23%) |
| |
BF+LT |
12 (16%) |
| |
MF+BT |
1 (1%) |
| 4 bone bruises |
|
|
| |
BF+BT |
22 (29%) |
| 2 bone bruises |
|
|
| |
LF+LT |
14 (19%) |
| |
MF+LT |
4 (5%) |
| |
LF+MT |
3 (4%) |
| |
MF+MT |
1 (1%) |
| |
0+BT |
1 (1%) |
| 1 bone bruise |
|
|
| |
0+LT |
1 (1%) |
| Total |
|
77(100%) |
Table 3.
Bone bruise patterns of patellar dislocation b.
Table 3.
Bone bruise patterns of patellar dislocation b.
| Bone Bruise Pattern |
N (%) |
| MIP+LAIF |
44 (57%) |
| MIP+LPIF |
17 (22%) |
| MIP+LASF |
8 (10%) |
| MSP+LAIF |
5 (6%) |
| MIP+LPSF |
1 (1%) |
| MSP+LASF |
1 (1%) |
| MSP+LPIF |
1 (1%) |
| Total |
77 (100%) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).