Background: The future of the world entirely depends on the health and wellbeing of newborns and their survival. Worldwide, their health is development and health global indicator [
1] . According to global conventions and declarations, every child has the right to grow healthier, to be protected from harms and diseases and harvest the highest possible health care [
2,
3,
4,
5]. Ethiopia have been also adapting and implementing those global child rights, health and survival recommendations i.e., establishment of ministry of women, children and youth affairs [
6,
7,
8]. High income countries have high health have high infant survival and low neonatal mortality. This is also guaranteed by reduction of the burden of morbidities and mortalities and the increment of life expectancies [
9] .
In 2019, worldwide an estimated 1.88 million deaths had occurred due to Neonatal disorders which accounts 37.3% of death of under five children. Similarly, Neonatal disorders are the second leading cause of Years Lived with Disability (YLDs) [
10] . About 47% of under five children death occur among newborns worldwide. One third occurring within 24 hours of birth and three forth within the first week of life. About 2 million babies were born with no sign of life sig and as a result 295,000 maternal deaths per annum [
11] .Vast majority in LMICs [
12] . Sub Saharan African Countries. In Ethiopia, high under five child mortality and infant mortality occurs at neonatal period [
13] . The majority of neonatal deaths occur at early neonatal time covering the intra-delivery, perinatal and early neonatal time followed by late neonatal period [
14]. Ethiopia is also not exceptional and the neonatal and infant mortalities are 28 and 48 mortalities per 1000 live births respectively [
15]. In Ethiopia, according to the health atlas 2021 report neonatal disorders are among the major causes of premature mortality
(MOH. EPHI. Health Atlas, 2021). Use it in the discussion section
To intervene this prior national public health emergency, Ministry of Health has introduced various packages of strategies including introduction of new disciplines in the field of health and expansion of the already existing services with highly recommended quality of care [
16] . Furthermore, evidence-based interventions targeting newborn and their mothers are running in Ethiopia. For example, the introduction and expansion of training and of health care professional’s targeting them were on board. E.g., training of the neonatal and pediatric nurses to halt it [
17] . This is to refill the failure of achieving the fourth MDGs four which dictated reduction of Child mortality by two third at 2015 and to ‘end preventable diseases’ and reduce the ‘preventable deaths of newborns and under five children to 12 and 25 per 1000 live births respectively by 2030 [
18]. In addition, in line with SDGs 2030[
19], MOH-Ethiopia had also promised to reduce the infant and neonatal mortality from 48 and 28 in to 35 and 21 respectively in 2025 [
20]. However, the national and sub national trends of Neonatal Mortality and its health loss in the past three decades is not well documented in Ethiopia. Hence, this study had analyzed the national and sub national distributions of Neonatal Mortality and its health loss by using Global Burden of Diseases study, 2019 data.
Methods
Study Setting and Period
According to the recent estimate of United Nations, Ethiopia is one of the oldest and second populous country in Africa which is the common habitat for 126 million people
(). Ethiopia has nine regions and two administrative cities [
21].The study period had encompassed from 1990 to 2019.
Study Methods:
This study had two data sources: primary and secondary data source. The data sources comprise; medical record reviews, surveys on sociodemographic, health care utilizations, household surveys, risk factors, morbidity and mortalities as well as demographic surveillance, scientific published and unpublished literate and case notifications and health facility observations and interviews [
22].
GBD study 2019, had included the causes of neonatal morbidity and mortality are as neonatal sepsis and other infections, preterm birth, neonatal encephalopathy and hemolytic diseases and other jaundices and analyzed incidence, prevalence, deaths and health losses secondary to neonatal disorders in Ethiopia from 1990 to 2019. The study had Guidance for Accurate and Transparent Estimates Reporting (GATHER) method. This method analyzes population level estimates of burden of diseases and its health loss as well as health conditions indicator, socio-demographic indicators, incidence, prevalence and other determinants of health and diseases. Additionally, this model also determines the cause of neonatal deaths by using ensemble model. It calculates DALYs (Years Lived with Disability, Years Lived with Disability (YLDs) and Years Life Lost (YLL). It calculates the Disability Adjusted Life Years which takes in to account the injuries and disabilities related health loss as a result of neonatal disorders. The GBD study 2019 study is becoming one of the rigorous and trusted data collection tools, data collection procedure, analysis schemes to analyze, estimate, predict and project global and national public health problems and produce reliable evidence for the policy makers [
23] . In this study early neonates, late neonates and neonates refers to neonates aged 0 to 6 days, 7-28 days and 0-28 days respectively. Hence, this study had analyzed the national and sun national burden of neonatal disorders, neonatal deaths and health losses i.e., DALYs, YLD and YLL. In addition,
Statement of Ethics
This study was the result of the Collaborator Network of Global Burden of Diseases (GBD) study in agreement with the GBD Protocol (IHME ID 4239-GBD2019-042022). Informed consent of the Global burden of diseases study was waivered and approved by the University of The Washington, United Stated of America (USA) (
https://www.healthdata.org/gbd/2019).
Results
Prevalence of neonatal disorders in Ethiopia, 2019
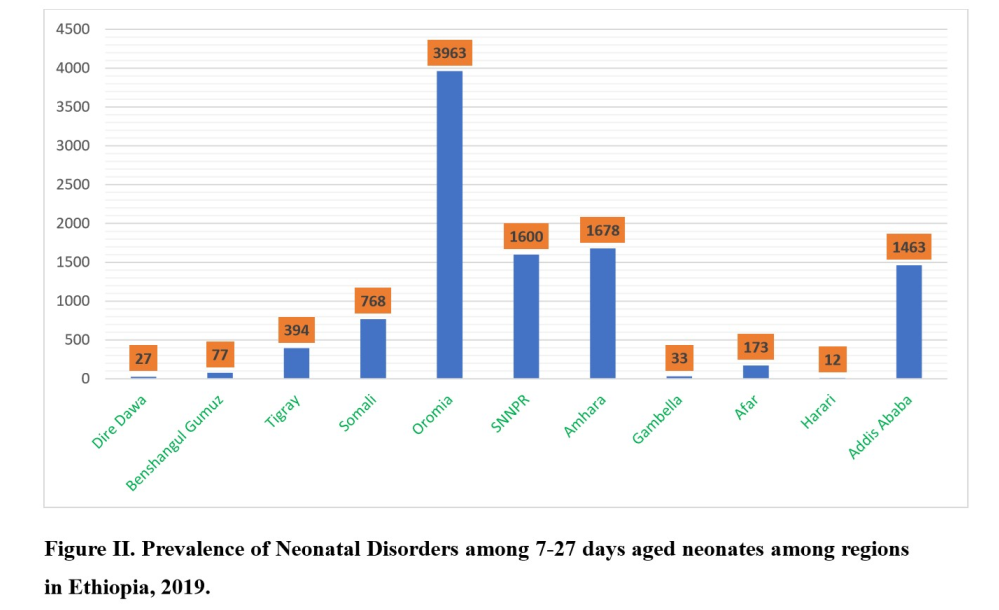
Our result reported; by the year 1990, the prevalence of neonatal disorders in Ethiopia among neonates aged <28 days was 26, 204 (95% UI,23,479-28,405). After fifteen years in 2015, it became 37,325 (95%UI, 33575-39,934. After additional fifteen years in 2019, the prevalence was 38, 132 (95% UI, 34,487-40,842). Before three decades, in 1990, the prevalence of neonatal disorders in Ethiopia among neonates aged 7-27 years was 19, 264 (95% UI, 17,273-20,917). In 2019, it had increased by 47% in to 28,319 (95% UI, 25646-30,361). In 2015, the prevalence among those aged 7-27 days was 27,688 (95%UI, 24,977-29,686). Furthermore, the prevalence of neonatal sepsis and other infections, preterm birth, neonatal encephalopathy disorders and hemolytic diseases and other jaundice were the common causes of neonatal disorders (Table I). Between 1990 and 2019, the national age standardized neonatal sepsis and other infections among neonates aged <28 days had increased from 119, 403 (95% UI, 80,757-171,863) in 1990 to 203,508 (95%UI, 133,210-296,840) in 2019 increasing by about 70 %. Regarding sub-national burden of neonatal disorders, Oromia and Harari region had the highest and the lowest prevalence. Almost two third of neonatal disorders (about 70%) had occurred among neonates aged 0-6 days (Figure I and II).
Between1990 to 2019, the national prevalence of preterm birth had increased by one third from 21, 263 (95UI, 18,858-23,102) in to 31, 340 (28,221-33,517). Among which, the national prevalence of neonatal sepsis and other infections amongst those aged 7-27 days had increased by two third from 1518 (95UI, 1116-2031) in 1990 in to 2683(95%UI, 2096-3455) in 2019. Oromia region has the highest prevalence 1468 (95% UI, 1140-1890) whereas Harari region had the lowest prevalence 6 (95%UI, 5-7) neonatal sepsis and other infections (Figure IIII). The lowest and the highest prevalence of preterm birth was observed in Addis Ababa 50,547 (95% UI, 43,205-58,717) and Harari region 37 (95% UI, 33-41). In 2019, two third of the preterm birth disorders had occurred amongst those aged 7-27 days 23,268 (95UI, 20,929-24,887) and 8,072 (7292-8630) had occurred amongst 0-6 days-aged neonates (Figure IV).
The two other common causes of neonatal disorders in Ethiopia were neonatal encephalopathy disorders and hemolytic disease and other jaundice. Accordingly, between 1990 and 2019, the prevalence of neonatal encephalopathy among neonates in Ethiopia had doubled from 1990 (1386-2774) to 4337 (95% UI, 3278-5665) in 2019. Likewise, prevalence of neonatal encephalopathy in Ethiopia among neonates aged 0-6 and days was 1,135 (95% UI,856-1477) and 7-27 days was 3,202 95% UI (2,409-4,191) respectively. Oromia and Harari region had the highest and the lowest prevalence, which was 1757 (95% UI, 1297-2299) and 8 (95% UI, 6-10) accordingly (Figure V). The same year, the national prevalence of hemolytic disease of the newborn and other jaundice was 1,074 (95% UI, 811-1374). Similarly, the highest and lowest prevalence had occurred in Oromia region 444 (95% UI, 336-569) and Harari region 2 (95% UI, 1-3). Among those aged 0-6 days, it had increased from 191 (95%UI, 144 (245) in to 271 (95% UI, 205-347) in 2019 (Figure VI).
Deaths and health losses secondary to Neonatal Disorders in Ethiopia, 2019
In 2019, the highest number of estimated neonatal deaths caused by neonatal sepsis and other infections had shifted from SNNPR to Oromia region while Harari remains to bear the lowest burden throughout the three decades. As a result, the highest and the lowest number of neonatal deaths secondary to neonatal disorders had occurred in Oromia (2,939) and Harari (2) regions respectively. Regarding regional distributions of Neonatal sepsis and other infections similarly in Ethiopia; before three decades in 1990, the highest and the lowest neonatal sepsis and other infections had occurred in SNNPR (1,504) and Harari (13) respectively. In 2019, the highest and the lowest neonatal sepsis and other infections had occurred in Oromia region (2,909) and Harari (12) region respectively. In the past thirty years, neonatal sepsis and other infections in Addis Ababa was reduced from 120 to 56 (Figure VII).
In 2019, 1, 155, 761 age standardized Disability Adjusted Life Years (DALYs) had occurred among neonates as a result of neonatal sepsis and other infections in Ethiopia among which 645,454 and 510, 307 was observed among 0-6 days and 7-27 days correspondingly. The highest DALYs were observed among early neonates. Oromia and Harari regions have the highest and the lowest DALYs that was 407,802 and 1,735 respectively. Addis Ababa DALYs due to neonatal sepsis and other infections was 8,092. The same year, 73,224 (95% UI 40,833-113,967) DALYs resulting from hemolytic disease of the newborn and other neonatal jaundice had occurred among neonates with the highest DALYs occurring among early neonates, 54,621 (95%UI 30,683-86,682) which was two times higher than late neonates. The highest DALYs secondary to hemolytic disease and other neonatal jaundice were observed in Oromia region, 28,708 (95%UI 14,499-50,719). By the year 2019, 3,097,543 (95%UI 2,318,819-4,037,129) age standardized DALYs due to neonatal encephalopathy had occurred among which the highest had occurred amongst early neonates, 2,859,303 (UI 2,136,085-3,734,040) which was 2,621,064 higher than the late neonates (7-27 days age). Years Lived with Disability (YLD) secondary to neonatal disorders in Ethiopia in 2019 was 2,484 (95% UI, 1,808-3235). In 2019, 903 (95% UI 646-1,191) years lived with disability (YLDs) had occurred due to preterm birth. In addition, the same year years live lost due to neonatal disorders in Ethiopia was 6,649,765 (UI 95% 5,243,873). The two regions with the highest YLL due to neonatal disorders were Oromia [(2,753,038,95% UI, 2,184,142-3,497-926) and Amhara 1,360,847 [(95% UI, 95% UI, 1,062,660-1,762,028)] regions where as Harari [(11,298,95%UI,8,428-14,813) had the lowest YLL health loss (Table II).
Discussion
Our study had revealed; the prevalence of neonatal disorders in 2019, (38, 132) had increased 11,928 higher than 1990. Two third) of prevalence of neonatal disorders had occurred among early neonates in Ethiopia. The four commonest neonatal disorders in Ethiopia were neonatal sepsis, preterm birth, Neonatal encephalopathy and Hemolytic disease and other jaundice disorders. This agrees with the study that had assessed the progress of ending neonatal deaths by SDGs in 2019/20 in Ethiopia. It further witnessed the non-lowering of neonatal deaths and high share of under-five child mortality [
24]. Secondly, it is similar with high neonatal mortality is observed in Kenya which was 35.4 deaths per 1000 live births [
25] . On the other hand, it is different from the study done in Nigeria that reported low share of neonatal mortality from under five child deaths [
26] .
Between 1990-2019, the prevalence of neonatal sepsis had increase nearly by three-fold (70%), which was 203,508. The same year, the prevalence of preterm birth had increased by one-fold in to 31,340. Nearly 44% of cause of neonatal death was reported in Nigeria 25. Addis Ababa has the second highest prevalence of early neonatal sepsis and other infections (2,395). However, Neonatal deaths secondary to early neonatal sepsis and other infections was one of the lowest. This could be due to better infrastructure availability and quality of care in the city when compared with other regions.
Similarly, this study revealed preterm birth had one third additional increment, which was 31,340. This is consistent with the study done through review of Kenya and South Africa neonatal survival status, that reported preterm birth as the main cause of most of the neonatal deaths in the two countries
24. Again, systematic review and metanalysis had reported the prevalence of preterm in Ethiopia was 10.48% [
27]. Three forth (3,202) of the neonatal encephalopathy had occurred among late neonates. Additionally, the prevalence of hemolytic disease of the newborn and other jaundice among neonates was 1,074 in 2019. This was also shared by Ethiopian study, which reported the overall pooed prevalence of perinatal asphyxia as 24.06% among 49,417 neonates [
28]. The highest and the lowest burden of all neonatal disorders except preterm birth had occurred in Oromia and Harari region respectively. The high share of Oromia region can be attributed to the largest number of populations in the country. Regarding the prevalence of preterm birth, Addis Ababa and Harari bear the highest and the lowest proportion. More than half of the prevalence (52%) of preterm birth had occurred in Addis Ababa alone in 2019. Th reasons for this result could be fear of labor pain, raised institutional deliver care, increased literacy status, urban residence, premature rupture of membrane and previous history of medical and obstetric history of the birth giving women and expansion of private and public maternal and newborn caring hospitals [
29,
30]. The lowest neonatal disorders occur in Harari region secondary to small number of people in the region. In similar way, sub nationally, in Amhara region and in Gojjam Zone of Ethiopia, 11.41% and 13.2% of preterm prevalence was reported respectively [
29,
31].
Never the less, this finding wis dissimilar from the EDHS further analysis findings that has assessed the individual and community level determinants of infant mortality rate in Ethiopia. According to the study, the highest infant mortality rate had occurred in Afar and Amhara regions while Oromia region bear the third highest death [
32]. This difference could be explained to the sampling procedure, timing of the survey, the sample size as well as use of only one source that means household survey for EDHS. In addition, even if the largest share of infant mortality occurs in Neonatal period, but not mentioned in the study [
33]. This is in line with the highest cause of global neonatal death, neonatal disorders and monitoring of the country against SDG3.2 target. In addition, Neonatal disorders results in neonatal death. This high number of deaths is also evidenced by the study done to assess neonatal, infant and under five child mortalities in ninety-nine Low and MICs and including Sub Saharan African Countries[
34,
35].
Neonatal disorder resulted in to Disability Adjusted life years (DALYs), Years Lived with Disability (YLD) and Years Life Lost (YLL). In Ethiopia, about 1, 155, 761 age standardized adjusted life years (DALYs) had occurred due to neonatal sepsis in Ethiopia. The highest DALYs was observed among early neonates (510, 307). Oromia (407,802) and Harari (1,735) regions have the highest and the lowest DALYs. DALYs due to neonatal sepsis in Addis Ababa was 8,092. The same year, 73,224 DALYs had resulted from hemolytic disease of the newborn and other neonatal jaundice. Early neonates had the highest DALYs (54,621) which was two times higher than late neonates DALYs. The highest DALYs secondary to hemolytic disease and other neonatal jaundice were observed in Oromia region, 28,708. Similarly, in 2019, age standardized DALYs (3,097) due to neonatal encephalopathy had occurred among which the highest were observed among early neonates, 2,859,303. It is 262,1064 higher DALYs than the late neonates. In 2019, in Ethiopia, Neonatal disorders had been resulted in YLDs (2,484), among which 903 YLDs had occurred secondary to preterm birth. The lowest and the highest YLDs due to neonatal disorders had been observed in Harari region 1,043 and Harari region (4) respectively. Additionally, 6,649,765, YLL had occurred due to neonatal disorders. Oromia; 2,753,038) and Amhara; 1,360,847 regions had the highest YLL as a result of neonatal disorders and Harari region;11,298 had the lowest.
An estimated 74,837 number of neonatal deaths had occurred in Ethiopia in 2019. This is in agreement with the further analysis of mini-EDHS survey that reported 35 neonatal deaths per 1000 live births[
36]. Both were done in 2019. This increment after three years of EDHS 16 survey could be explained by occurrence of COVID 19 pandemics [
37] and the small sample size of mini-EDHS. The number of neonatal deaths secondary to neonatal sepsis and other neonatal infections among neonates was 11, 637, in 2019; with almost equal prevalence among early and late neonates. In 2019, after three decades, the lowest and the highest number of neonatal deaths caused by neonatal sepsis had occurred in Oromia (2,939) and Harari (2) regions respectively. This is analogous with the cohort study done in Ethiopia which reported 56% of neonatal deaths primarily due to neonatal sepsis [
38] . The highest prevalence of neonatal sepsis and other infections from SNNPR in 1990 to Oromia region in 2019 and Harari remains to bear the lowest burden. The number of deaths secondary to neonatal preterm birth among 0-6 days had been reduced from 19,733 in 1990 to 13,888 in 2019 indicating 30% reduction. In the same period, among those aged 7-27 days it was reduced by close to forty percent (38.3%). This was also depicted by the study done in Ethiopia, that described prematurity as the second common cause of neonatal death
35. The other cause of neonatal death was neonatal encephalopathy due to birth asphyxia and trauma. The number of neonatal deaths secondary to neonatal sepsis and other neonatal infections among all aged neonates was 11, 637 that constitutes 5,804 among early neonates and 5,832 among late neonates. A similar study had reported asphyxia as the third common cause of neonatal death in Ethiopia
35. Hemolytic disease of the newborn and other jaundice had also been measured as causes for neonatal death. Hence, 826 and 611 deaths were attributed to it among 0-6 days and 7-27 days aged neonates. In 1990, the highest and the lowest number of neonatal deaths as a result of neonatal sepsis and other infections had occurred in SNNPR (1,508) and Harari (13) regions respectively.
Implications: In 2019, the findings of this study revealed that, neonatal deaths as a result of neonatal sepsis and other infections, preterm birth, neonatal encephalopathy and hemolytic disease and other jaundice were continued to be the main neonatal health burden and resulted in to huge health losses in Ethiopia. Seven in ten of neonatal disorders had occurred among early neonates, narrowing the occurrence of neonatal death around the time of birth. Oromia region secondary to its largest population bear most of neonatal disorders. Addis Ababa had the second highest early neonatal sepsis and other infections. Unusually, Addis Ababa city had the highest burden of preterm birth due to increased literacy rate, escalated institutional delivery seeking care, expansion of public and private maternal health care services and high proportion of elected cesarean section.
Conclusions: Despite SDGs promises and national neonatal care interventions, finding revealed that high number of neonatal disorders and neonatal death is still occurring in the country. As a result, the country is suffering from high number of neonatal disorders and deaths as well as health losses characterized by DALYs, YLD and YLL. The highest neonatal disorders and health loses had occurred in Oromia region where as Addis Ababa city had the highest preterm birth in 2019. The three regions mostly affected by the prevalence of neonatal disorders and neonatal deaths as well as DALYs, YLL and YLD were Oromia, Amhara and SNNPR respectively. Unless, peace is ensured the problem will continue to surface and will trigger the country from achieving national and global promises. Though Addis Ababa has the second highest early neonatal sepsis, death as a result of neonatal sepsis and other infection was very low.
Recommendations: In addition to efforts at the ground, the Ministry of Health of Ethiopia should device accelerated, locally accepted, innovative approach to the care and treatment of early neonates. Revised accelerated neonatal intervention should focus Oromia, Amhara and SNNPRs regions and Addis Ababa city administration. Moreover, the availability of infrastructure and quality of care needs to be strengthened more of around the time of birth. In addition, advocacy of institutional delivery should be further enhanced and widen. Handling conflict and ensuring peace will improve the survival of neonates and better the future of children.
Authors’ Contributions
BA, TM, MD, ST and AM had incepted, designed, analyzed and interpreted the data, read and approved the final manuscript for publication and contributed equally in the designed, analysis, interpretation and approved the final version of the manuscript for publication.
Acknowledgement
We the authors acknowledge national data management center for health, Ethiopian public health institute (EPHI) and institute of health metrics and evaluation (IHME), The University of Washington for the necessary support given to us.
Conflict of Interest
We, the authors declare that we have no conflict of interests.
Consent for Publication
Not Applicable
Abbreviations and Acronyms:
| MDGs: |
Millennium Development Goals |
| EPHI: |
Ethiopian Public Health Institute |
| SDGs: |
Sustainable development goal |
| UN: |
United Nations |
| WHO: |
World Health Organization |
References
- WHO.2002.
- United Nations General Assembly Convention of the Rights of the Child adopted and opened for signature, ratification and accession by the General Assembly resolution 44/25 of . Entered in to force 02 September 1990, in accordance with article 49.
- Paul, J. Nelson, Ellen Dorsey. At the nexus of human rights readers and development. New methods and strategies of Global NGOs. World Development 2003, 31, 2013–2026. [Google Scholar]
- Claudo Schufan. Health and Human right readers. Centre for equity in to health and Allied Thees (Cehat), Mumbai, India, September 2003.
- Office of the United Nations Commission for Human rights frequently asked Questions on Human Right Based approach to Development Cooperation, United Nations, New York and Geneva, 2006.
- FDRE. National Population Policy, Addis Ababa, Ethiopia, 1993.
- FDRE. National Gender Policy, Addis Ababa, Ethiopia, 1993.
- FDRE. FDRE. National Health Policy, Addis Ababa, Ethiopia, 1993.
- MDG 15 Evaluation.
- http://www.thelancet.com/.
- WHO fact sheet, 2022 accessed on July 13, 2023.
- WHO fact sheet, 2023, Accessed July 13, 2023.
- MOH. 2022.
- Misganaw, Yemane, MOH.
- MOH. FDRE. Ethiopian Demographic Health Survey, 2016. Central Statistical Agency Addis Ababa, Ethiopia. The DHS Program ICF Rockville, Maryland, USA July 2017.
- Child hood MOH initiatives.
- Jhpiego, Tegbar, Misganaw, 2014.
- UN. SDGs, Transforming our world, 2015.
- UN. Sustainable Development Goals. Transforming Our World. New York, 2015.
- MOH. Health Sector transformational plan, 2020/2021-2024/2025. (2013-2017 EFY). February 2021.
- FDRE. Constitution, 1995.
- IHME. Global Burden of Diseases. https://www.healthdata.org/data-tools-practices/data-collection, accessed on June 2023.
- IHME. Global Burden of Diseases. Data practices | Institute for Health Metrics and Evaluation (healthdata.org), accessed on June 27, 2023.
- Yonas Getaye Tefera1 and Asnakew Achaw AyeleNewborns and Under-5 Mortality in Ethiopia: The Necessity to Revitalize Partnership in Post-COVID-19 Era to Meet the SDG Targets. Journal of Primary Care & Community Health Volume 12: 1–5 © The Author(s) 2021 Article reuse guidelines: sagepub.com/journals-permissions. [CrossRef]
- Brian Barasa Masaba 1 Rose M Mmusi-Phetoe 2. Neonatal Survival in Sub-Sahara: A Review of Kenya and South Africa. Journal of Multidisciplinary Healthcare 2020, 13, 709–716. [CrossRef] [PubMed]
- Adeyinka Odejimi, John Quinley, George Ikechi Eluwa. Causes of deaths in neonates and children aged 1–59 months in Nigeria: verbal autopsy fndings of 2019 Verbal and Social Autopsy study. BMC Public Health 2022, 22, 1130. [CrossRef] [PubMed]
- Kindie Fentahun Muchie, Ayenew Molla Lakew, Destaw Fetene Teshome. Epidemiology of preterm birth in Ethiopia: systematic review and meta-analysis. BMC Pregnancy and Childbirth 2020, 20, 574. [CrossRef] [PubMed]
- The state of birth asphyxia in Ethiopia: An umbrella review of systematic review and meta-analysis reports, 2020 Wubet Alebachew Bayih, Binyam Minuye Birhane, Demeke Mesfin Belay. Heliyon 2021, 7, e08128. [CrossRef] [PubMed]
- Adhanom Gebreegziabher Baraki, Temesgen Yihunie Akalu, Haileab Fekadu Wolde. Factors affecting infant mortality in the general population: evidence from the 2016 Ethiopian demographic and health survey (EDHS). BMC Pregnancy and Childbirth 2020, 20, 299. [CrossRef] [PubMed]
- Dagnew Getnet AdugnaID. Adugna DG. Prevalence and associated risk factors of preterm birth among neonates in referral hospitals of Amhara Region. PLoS ONE 2022, 17, e0276793. [CrossRef] [PubMed]
- Tafere Birlie Ayele and Yikeber Abebaw Moyehodie. Ayele et al. Prevalence of preterm birth and associated factors among mothers who gave birth in public hospitals of east Gojjam zone. BMC Pregnancy and Childbirth 2023, 23, 204. [CrossRef]
- Setegn Muche Fenta, Girum MeseretAyenew, Haile Mekonnen Fenta, Hailegebrael Birhan Biresaw, Kenaw Derebe Fentaw. Community and individual level determinants of infant mortality in rural Ethiopia using data from 2016 Ethiopian demographic and health survey, (2022) 12:16879. 2016; w2. [CrossRef]
- Brian Barasa Masaba, Rose M Mmusi-Phetoe. Neonatal Survival in Sub-Sahara: A Review of Kenya and South Africa. Journal of Multidisciplinary Healthcare 2020, 13, 709–716. [CrossRef] [PubMed]
- Mapping 123 million neonatal, infant and child deaths between 2000 and 2017. [CrossRef]
- Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study 2019 GBD 2019 Under-5 Mortality Collaborators. www.thelancet.com Vol 398 September 4, 2021. [CrossRef]
- Abay Sahile, Dereje Bekele, Habtamu Ayele. Determining factors of neonatal mortality in Ethiopia: An investigation from the 2019 Ethiopia Mini Demographic and Health Survey. PLoS ONE 2022, 17, e0267999. [CrossRef] [PubMed]
- Abiy Seifu Estifanos, Kescha Kazmi, Shaun K. Morris2Could COVID-19 Reverse the Modest Gains Made in Newborn Health in Ethiopia? Maternal and Child Health Journal 2021, 25, 849–854. [CrossRef] [PubMed]
- Berhe Weldearegawi, Yohannes Adama Melaku, Semaw Ferede Abera. Weldearegawi et al. Infant mortality and causes of infant deaths in rural Ethiopia: a population-based cohort of 3684 births. BMC Public Health 2015, 15, 770. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).