Submitted:
21 September 2023
Posted:
21 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study design and questionnaires
2.2. Statistical analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Attia, S.; Mausbach, K.; Klugar, M.; Howaldt, H.P.; Riad, A. Prevalence and Drivers of COVID-19 Vaccine Booster Hesitancy Among German University Students and Employees. Front Public Health. 2022, 10, 846861. [Google Scholar] [CrossRef] [PubMed]
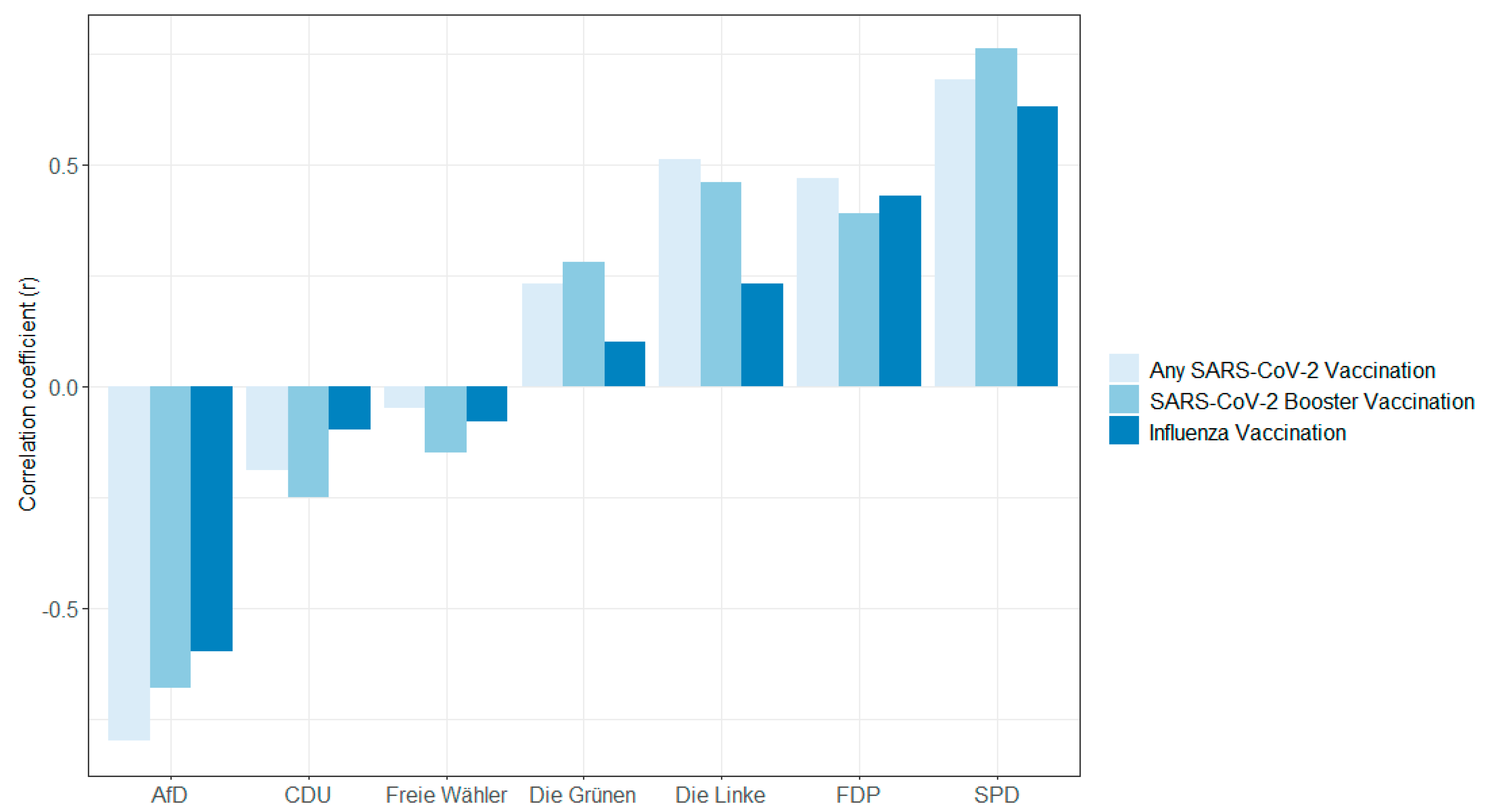
- Jackle, S.; Timmis, J.K. Left-Right-Position, party affiliation and regional differences explain low COVID-19 vaccination rates in Germany. Microb Biotechnol. 2023, 16, 662–677. [Google Scholar] [CrossRef] [PubMed]
- Galagali, P.M.; Kinikar, A.A.; Kumar, V.S. Vaccine Hesitancy: Obstacles and Challenges. Curr Pediatr Rep. 2022, 10, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015-2017. Vaccine. 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; deHart, M.P.; Halsey, N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef]
- Larson, H.J.; Mnookin, S. Trust and Confidence in Vaccines: Tales of Three Vaccines, Lessons for Others. 2016, 529–540.
- Tizard, I.R. Safety and sexual promiscuity: Hepatitis B, human papilloma virus, and influenza vaccines. 2023, 281–292.
- Sorell, T.; Butler, J. The Politics of Covid Vaccine Hesitancy and Opposition. Polit Q. 2022, 93, 347–351. [Google Scholar] [CrossRef]
- Bundesministerium für Gesundheit. Current vaccination status. [Available from: https://impfdashboard.de/en/.
- Robert Koch Institute. Monitoring Des COVID-19-Impfgeschehens in Deutschland 2022 [Available from: https://www.rki.de/DE/Content/Infekt/Impfen/ImpfungenAZ/COVID-19/Monatsberichte/2022-07-07.pdf?__blob=publicationFile.
- Rieck T, Steffen A, Schmid-Küpke N, Feig M, Wichmann O, Siedler A. Impfquoten bei Erwachsenen in Deutschland–Aktuelles aus der KV-Impfsurveillance und der Onlinebefragung von Krankenhauspersonal OKaPII. 2020.
- Poethko-Muller C, Schmitz R. [Vaccination coverage in German adults: Results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013, 56, 845–857. [Google Scholar]
- Robert Koch Institut. Epidemiologisches Bulletin 2022 [Available from: https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2022/Ausgaben/49_22.pdf?__blob=publicationFile.
- Gottschick C, Diexer S, Massag J, Klee B, Broda A, Purschke O; et al. Mental health in Germany in the first weeks of the Russo-Ukrainian war. BJPsych Open. 2023, 9, e66. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development. Classifying Educational Programmes: Manual for ISCED-97 Implementation in OECD Countries. 1999.
- Sachsen, W. Waglergebnisse 2019 [Available from: https://www.wahlen.sachsen.de/landtagswahl-2019-informationen-und-downloads.html?_cp=%7B%22accordion-content-6555%22%3A%7B%220%22%3Atrue%7D%2C%22previousOpen%22%3A%7B%22group%22%3A%22accordion-content-6555%22%2C%22idx%22%3A0%7D%7D.
- Wahlergebnisse Sachsen-Anhalt. Statistisches Landesamt Sachsen-Anhalt - Wahl des 8. Landtages von Sachsen-Anhalt am 06. Juni 2021 2021 [Available from: https://wahlergebnisse.sachsen-anhalt.de/wahlen/lt21/erg/kreis/lt.15091.ergtab.php.
- Dasch, S.; Wachinger, J.; Barnighausen, T.; Chen, S.; McMahon, S.A. Deliberation, context, emotion and trust - understanding the dynamics of adults' COVID-19 vaccination decisions in Germany. BMC Public Health. 2023, 23, 136. [Google Scholar] [CrossRef]
- Lindholt, M.F.; Jorgensen, F.; Bor, A.; Petersen, M.B. Public acceptance of COVID-19 vaccines: Cross-national evidence on levels and individual-level predictors using observational data. BMJ Open. 2021, 11, e048172. [Google Scholar] [CrossRef]
- Murphy J, Vallieres F, Bentall RP, Shevlin M, McBride O, Hartman TK; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Desson, Z.; Kauer, L.; Otten, T.; Peters, J.W.; Paolucci, F. Finding the way forward: COVID-19 vaccination progress in Germany, Austria and Switzerland. Health Policy Technol. 2022, 11, 100584. [Google Scholar] [CrossRef] [PubMed]
- Steinert, J.I.; Sternberg, H.; Prince, H.; Fasolo, B.; Galizzi, M.M.; Buthe, T.; et al. COVID-19 vaccine hesitancy in eight European countries: Prevalence, determinants, and heterogeneity. Sci Adv. 2022, 8, eabm9825. [Google Scholar] [CrossRef] [PubMed]
- Walach, H.; Ofner, M.; Ruof, V.; Herbig, M.; Klement, R.J. Why do people consent to receiving SARS-CoV-2 vaccinations? A representative survey in Germany. BMJ Open. 2022, 12, e060555. [Google Scholar] [CrossRef] [PubMed]
- Lenart, C.; Prager, M.; Sachs, M.; Steininger, C.; Fernandes, C.; Thannesberger, J. Tackling Vaccine Hesitancy and Increasing Vaccine Willingness Among Parents of Unvaccinated Children in Austria. International Journal of Public Health. 2023, 68. [Google Scholar] [CrossRef] [PubMed]
- Srivastav, A.; Lu, P.J.; Amaya, A.; Dever, J.A.; Stanley, M.; Franks, J.L.; et al. Prevalence of influenza-specific vaccination hesitancy among adults in the United States, 2018. Vaccine. 2023, 41, 2572–2581. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch Institute. Wochenberichte zu COVID-19 (bis 8.6.2023) 2023 [Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Wochenbericht/Wochenberichte_Tab.html?nn=13490888&cms_gtp=16396118_list%253D2.
- Altarawneh, H.N.; Chemaitelly, H.; Hasan, M.R.; Ayoub, H.H.; Qassim, S.; AlMukdad, S.; et al. Protection against the Omicron Variant from Previous SARS-CoV-2 Infection. N Engl J Med. 2022, 386, 1288–1290. [Google Scholar] [CrossRef] [PubMed]
- Pather, S.; Madhi, S.A.; Cowling, B.J.; Moss, P.; Kamil, J.P.; Ciesek, S.; et al. SARS-CoV-2 Omicron variants: Burden of disease, impact on vaccine effectiveness and need for variant-adapted vaccines. Front Immunol. 2023, 14, 1130539. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Madewell, Z.J.; Liu, M.; Longini, I.M.; Yang, Y. Effectiveness of SARS-CoV-2 vaccines against Omicron infection and severe events: A systematic review and meta-analysis of test-negative design studies. Front Public Health. 2023, 11, 1195908. [Google Scholar] [CrossRef] [PubMed]
- Tamandjou Tchuem, C.R.; Auvigne, V.; Vaux, S.; Montagnat, C.; Paireau, J.; Monnier Besnard, S.; et al. Vaccine effectiveness and duration of protection of COVID-19 mRNA vaccines against Delta and Omicron BA.1 symptomatic and severe COVID-19 outcomes in adults aged 50 years and over in France. Vaccine. 2023, 41, 2280–2288. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Value | RespondersN (n=37,078) | Responders% (95% CI) | Non-respondersN (n=33,476) | Non-responders % (95% CI) |
|---|---|---|---|---|---|
| Sex | Male | 14,216 | 38.3 (37.8-38.8) | 14,984 | 44.8 (44.2-45.3) |
| Female | 22,583 | 60.9 (60.4-61.4) | 17,308 | 51.7 (51.2-52.2) | |
| Diverse | 29 | 0.1 (0.1-0.1) | 77 | 0.2 (0.2-0.3) | |
| NA | 250 | 0.7 (0.6-0.8) | 1,107 | 3.3 (3.1-3.5) | |
| Age group | 18-29 | 2,633 | 7.1 (6.8-7.4) | 5,166 | 15.4 (15.0-15.8) |
| 30-39 | 5,079 | 13.7 (13.4-14.1) | 6,193 | 18.5 (18.1-18.9) | |
| 40-49 | 6,065 | 16.4 (15.9-16.7) | 5,499 | 16.4 (16.0-16.8) | |
| 50-59 | 9,241 | 24.9 (24.5-25.4) | 6,264 | 18.7 (18.3-19.1) | |
| 60-69 | 8,831 | 23.8 (23.3-24.3) | 5,327 | 15.9 (15.5-16.3) | |
| 70-79 | 4,023 | 10.9 (10.5-11.2) | 2,990 | 8.9 (8.6-9.2) | |
| 80+ | 890 | 2.4 (2.2-2.6) | 854 | 2.6 (2.4-2.7) | |
| NA | 316 | 0.9 (0.8-0.9) | 1,183 | 3.5 (3.3-3.7) | |
| Educationa | Low | 840 | 2.3 (2.1-2.4) | 2,177 | 6.5 (6.2-6.8) |
| Medium | 10,714 | 28.9 (28.4-29.4) | 10,223 | 30.5 (30.0-31.0) | |
| High | 23,319 | 62.9 (62.4-63.4) | 18,396 | 54.9 (54.4-55.5) | |
| NA | 2,205 | 5.9 (5.7-6.2) | 2,680 | 8.0 (7.7-8.3) | |
| Net household equivalent incomeb | Below 1250€ | 3,607 | 9.8 (9.4-10.0) | 4,958 | 14.8 (14.4-15.2) |
| 1250- <1750€ | 7,966 | 21.5 (21.1-21.9) | 7,229 | 21.6 (21.2-22.0) | |
| 1750- <2250€ | 5,061 | 13.6 (13.3-14.0) | 4,405 | 13.2 (12.8-13.5) | |
| 2250- <3000€ | 9,170 | 24.7 (24.3-25.2) | 7,115 | 21.2 (20.8-21.7) | |
| 3000- <4000€ | 7,568 | 20.4 (20.0-20.1) | 5,089 | 15.2 (14.8-15.6) | |
| 4000- <5000€ | 293 | 0.8 (0.7-0.9) | 200 | 0.6 (0.5-0.7) | |
| 5000€+ | 223 | 0.6 (0.5-0.7) | 154 | 0.5 (0.4-0.5) | |
| NA | 3,190 | 8.6 (8.3-8.9) | 4,326 | 12.9 (12.6-13.3) | |
| Born in Germany | Yes | 35,678 | 96.2 (96.0-96.4) | 30,866 | 92.2 (91.9-92.4) |
| No | 1,165 | 3.1 (2.9-3.3) | 1,507 | 4.5 (4.3-4.7) | |
| NA | 235 | 0.6 (0.6-0.7) | 1,103 | 3.3 (3.1-3.5) | |
| Living in a city > 100,000 | Yes | 13,210 | 35.6 (35.1-36.1) | 13,084 | 39.0 (38.6-39.6) |
| No | 23,322 | 62.9 (62.4-63.4) | 19,731 | 58.9 (58.4-59.5) | |
| NA | 546 | 1.5 (1.4-1.6) | 661 | 1.9 (1.8-2.1) | |
| Federal state | Saxony-Anhalt | 9,225 | 24.9 (24.4-25.3) | 10,201 | 30.5 (29.9-30.9) |
| Saxony | 7,633 | 20.6 (20.2-21.0) | 7,143 | 21.3 (20.9-21.8) | |
| Baden-Württemberg (only city of Stuttgart) | 459 | 1.2 (1.1-1.4) | 518 | 1.6 (1.4-1.7) | |
| Bavaria | 3,329 | 9.0 (8.7-9.3) | 3,675 | 10.9 (10.6-11.3) | |
| Berlin | 479 | 1.3 (1.2-1.4) | 456 | 1.4 (1.2-1.5) | |
| Brandenburg | 3,272 | 8.8 (8.5-9.1) | 2,425 | 7.2 (6.9-7.5) | |
| Hamburg | 509 | 1.4 (1.3-1.5) | 501 | 1.5 (1.4-1.6) | |
| Rhineland-Palatinate | 4,352 | 11.7 (11.4-12.1) | 3,676 | 10.9 (10.6-11.3) | |
| Mecklenburg-Western Pomerania | 2,071 | 5.6 (5.4-5.8) | 1,456 | 4.3 (4.1-4.6) | |
| Lower Saxony | 1,816 | 4.9 (4.7-5.1) | 999 | 2.9 (2.8-3.2) | |
| Saarland | 1,134 | 3.1 (2.9-3.2) | 560 | 1.7 (1.5-1.8) | |
| Schleswig-Holstein | 2,162 | 5.8 (5.6-6.1) | 1,136 | 3.4 (3.2-3.6) | |
| Other | 91 | 0.2 (0.2-0.3) | 69 | 0.2 (0.2-0.3) | |
| NA | 546 | 1.5 (1.4-1.6) | 661 | 1.9 (1.8-2.1) |
| Characteristics | Value | Any SARS-CoV-2 vaccination% (95% CI) | SARS-CoV-2 booster vaccination% (95% CI) | Influenza vaccination % (95% CI) |
|---|---|---|---|---|
| Sex | Male | 93.5 (93.0-93.9) | 31.8 (31.1-32.6) | 47.8 (46.9-48.6) |
| Female | 92.5 (92.1-92.8) | 21.6 (21.1-22.2) | 41.8 (41.2-42.5) | |
| Diverse | 93.1 (75.8-98.8) | 20.7 (8.7-40.3) | 27.6 (13.4-47.5) | |
| NA | 90.4 (85.9-93.6) | 26.8 (21.5-32.8) | 41.6 (35.5-47.9) | |
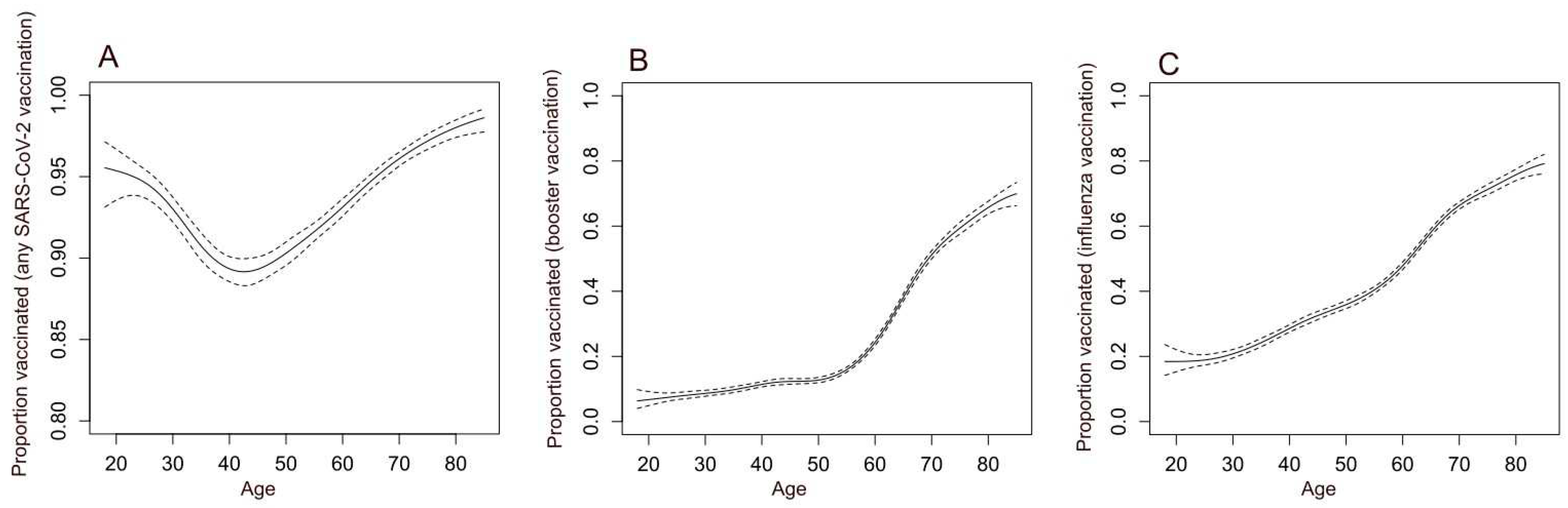
| Age group | 18-29 | 94.7 (93.7-95.5) | 8.1 (7.1-9.2) | 19.6 (18.1-21.2) |
| 30-39 | 90.5 (89.7-91.2) | 10.1 (9.3-11.0) | 24.9 (23.7-26.1) | |
| 40-49 | 89.6 (88.8-90.3) | 12.1 (11.4-13.0) | 32.9 (31.8-34.2) | |
| 50-59 | 91.8 (91.2-92.3) | 16.5 (15.8-17.3) | 40.9 (39.9-41.9) | |
| 60-69 | 94.7 (94.2-95.2) | 39.7 (38.7-40.7) | 58.4 (57.3-59.4) | |
| 70-79 | 96.8 (96.2-97.3) | 57.3 (55.7-58.8) | 69.7 (68.2-71.1) | |
| 80+ | 98.5 (97.4-99.2) | 68.7 (65.5-71.7) | 77.6 (74.7-80.3) | |
| NA | 87.9 (83.7-91.2) | 21.2 (16.9-26.2) | 42.7 (37.3-48.4) | |
| Education | Low | 96.1 (94.5-97.2) | 9.4 (7.6-11.6) | 21.9 (19.1-24.9) |
| Medium | 90.7 (90.1-91.2) | 21.8 (21.0-22.6) | 38.4 (37.5-39.4) | |
| High | 93.9 (93.7-94.3) | 27.8 (27.2-28.3) | 47.8 (47.2-48.5) | |
| NA | 89.7 (88.3-90.9) | 26.7 (24.8-28.6) | ||
| Net equivalent income | Below 1250€ | 88.9 (87.7-89.9) | 17.4 (16.2-18.7) | 33.1 (31.6-34.7) |
| 1250- <1750€ | 91.5 (90.8-92.1) | 26.3 (25.3-27.3) | 45.0 (43.9-46.1) | |
| 1750- <2250€ | 91.7 (90.9-92.4) | 16.6 (15.6-17.7) | 36.6 (35.2-37.9) | |
| 2250- <3000€ | 94.2 (93.7-94.7) | 26.5 (25.6-27.5) | 46.4 (45.4-47.4) | |
| 3000- <4000€ | 95.9 (95.5-96.4) | 33.6 (32.5-34.7) | 51.0 (49.9-52.2) | |
| 4000- <5000€ | 95.9 (92.8-97.8) | 30.0 (24.9-35.7) | 50.5 (44.6-56.4) | |
| 5000€+ | 95.9 (92.2-98.0) | 33.2 (27.1-39.8) | 50.7 (43.9-57.4) | |
| NA | 90.7 (89.6-91.6) | 24.4 (22.9-25.9) | 41.9 (40.2-43.7) | |
| Born in Germany | Yes | 92.8 (92.6-93.1) | 25.3 (24.9-25.8) | 44.1 (43.6-44.6) |
| No | 94.2 (92.6-95.4) | 32.9 (30.2-35.7) | 43.2 (40.3-46.1) | |
| NA | 86.4 (81.2-90.4) | 23.4 (18.3-29.4) | 43.4 (37.0-50.0) | |
| Living in a city > 100,000 | Yes | 95.4 (95.0-95.8) | 27.5 (67.7-28.3) | 46.4 (45.5-47.2) |
| No | 91.4 (91.0-91.8) | 24.5 (23.9-25.1) | 42.8 (42.2-43.5) | |
| NA | 91.8 (89.0-93.9) | 22.9 (19.5-26.7) | 43.8 (39.6-48.1) | |
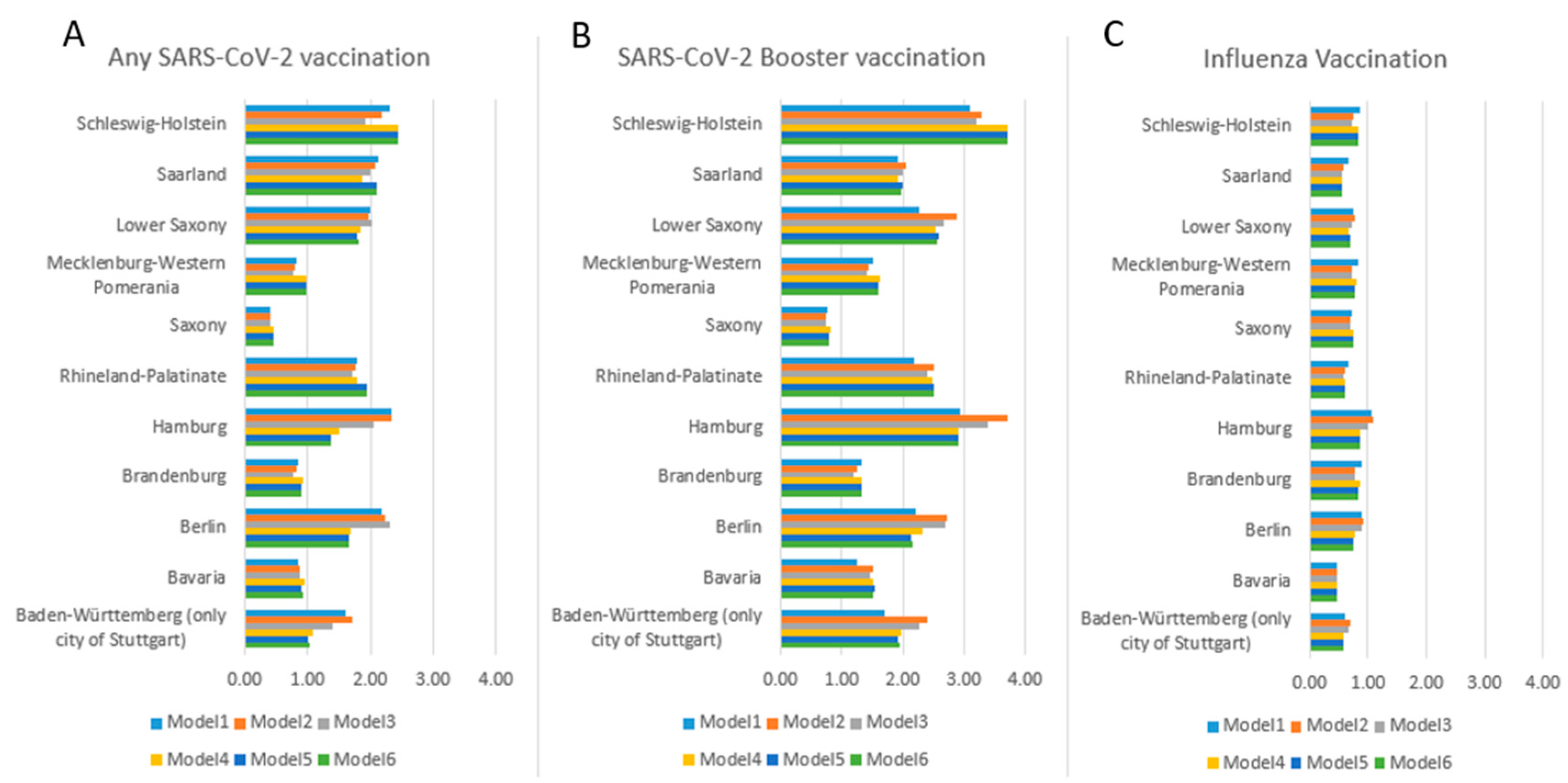
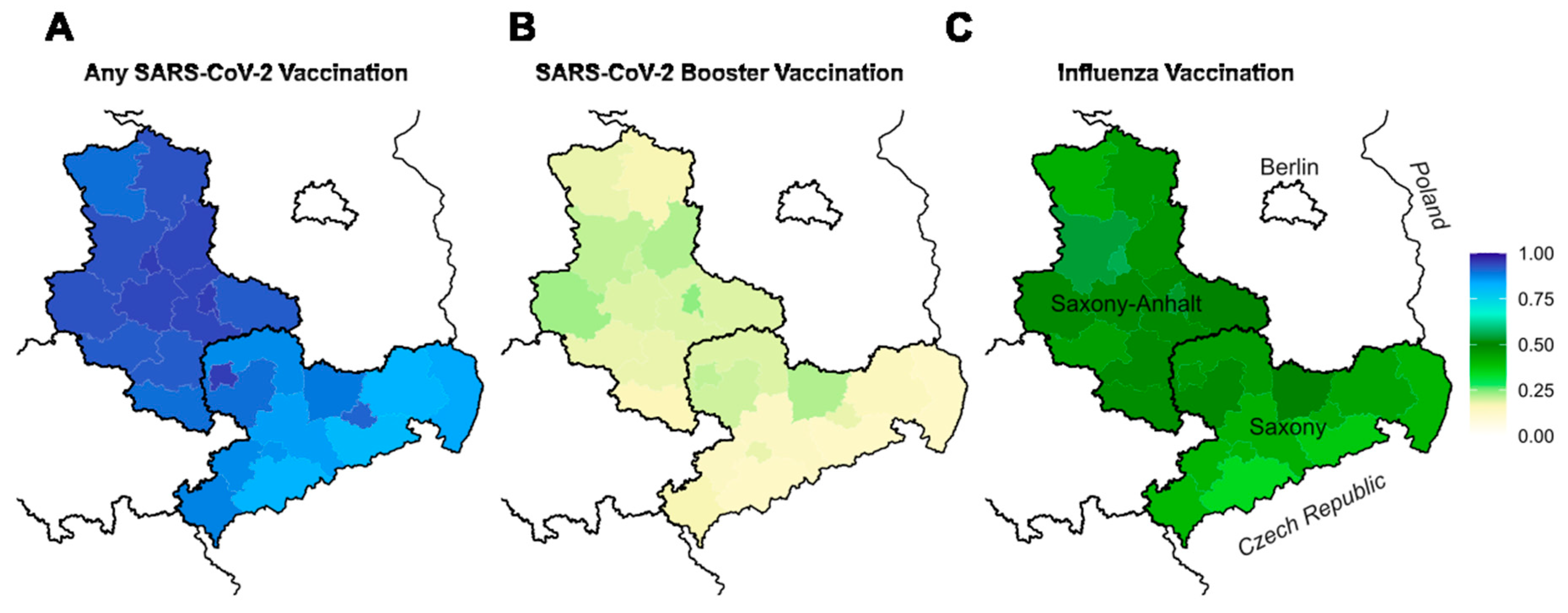
| Federal state | Saxony-Anhalt | 93.8 (93.2-94.3) | 20.1 (19.3-20.9) | 50.3 (49.3-51.4) |
| Saxony | 86.2 (85.3-86.9) | 16.3 (15.5-17.2) | 41.9 (40.8-43.0) | |
| Baden-Württemberg (only Stuttgart) | 96.1 (93.8-97.6) | 30.0 (25.9-34.5) | 38.8 (34.3-43.4) | |
| Bavaria | 92.8 (91.9-93.7) | 24.1 (22.7-25.6) | 32.5 (30.9-34.1) | |
| Berlin | 97.1 (95.0-98.3) | 35.7 (31.4-40.2) | 47.8 (43.2-52.4) | |
| Brandenburg | 92.8 (91.9-93.7) | 24.9 (23.5-26.5) | 47.4 (45.6-49.1) | |
| Hamburg | 97.2 (95.3-98.4) | 42.4 (38.1-46.9) | 52.1 (47.6-56.4) | |
| Rhineland-Palatinate | 96.4 (95.8-96.9) | 35.4 (33.9-36.9) | 40.2 (38.8-41.7) | |
| Mecklenburg-Western Pomerania | 92.6 (91.4-93.7) | 27.6 (25.7-29.6) | 45.3 (43.2-47.5) | |
| Lower Saxony | 96.9 (95.9-97.5) | 36.3 (34.1-38.6) | 43.3 (41.0-45.7) | |
| Saarland | 97.0 (95.8-97.9) | 32.4 (29.7-35.3) | 39.9 (37.1-42.9) | |
| Schleswig-Holstein | 97.2 (96.4-97.9) | 43.8 (41.7-45.9) | 46.7 (44.6-48.8) | |
| Other | 97.8 (91.5-99.6) | 25.3 (17.0-35.7) | 26.4 (17.9-36.8) | |
| NA | 91.8 (89.0-93.9) | 22.9 (19.5-26.7) | 43.8 (39.6-48.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





