Background
In the 1970s, CT was invented by British engineer Godfrey N. Hounsfield and American surgeon A. M. Cormack by integrating X-ray technology with computers. This innovative X-ray method depicts not only bones but also surrounding tissues by collecting slice-by-slice images of various body parts. A few years before, Cormack had developed an approach for determining the distribution and attenuation of x-rays within the body as well as a mathematical theory for image reconstruction. In 1979, the two scientists received Nobel Prize in Medicine for their efforts and discovery [
1,
2]. This study aimed at evaluating radiation exposure in coronary angiography CT scans and establishing a diagnostic reference level specific to the population of Northeast Assam. There may be a need for a comprehensive risk-benefit assessment of coronary angiography CT scans in this population. Understanding the balance between diagnostic benefits and potential radiation risks is crucial for informed decision-making.
Coronary arteries are the “arterial blood vessels” that provide the heart muscle with oxygenated blood via coronary circulation. The heart, like all other organs or tissue in the body, needs an ongoing oxygen supply to operate and survive [
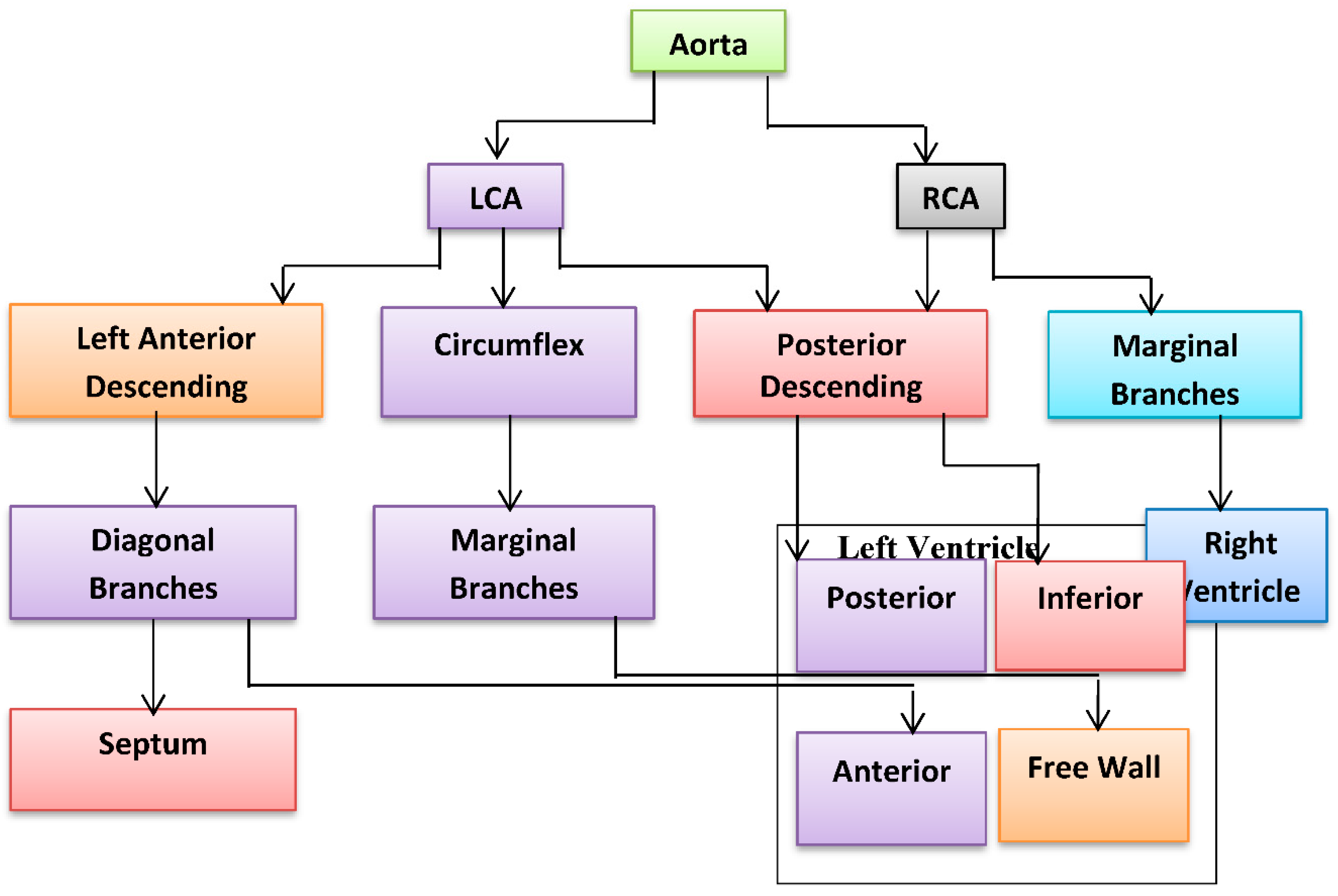
3]. The coronary arteries encircle the whole heart. The Right and left Coronary Artery are two main types of coronary arteries that supply blood to the heart. These arteries can also be classified into different groups based on the regions of the heart that they supply with blood flow. These classifications are referred to as microvascular classifications, which supply blood to the innermost heart tissue, or near to the endocardium, and epicardial classifications, which supply blood across the epicardium, or the outermost heart tissue [
4]. A bridged coronary artery function may lead to less blood carrying nutrients and oxygen to the heart. This may have an impact on the heart’s capacity to circulate blood throughout the body as well as on the blood supply to heart muscle itself. As a consequence, any disease or illness of the “coronary arteries” could have a significant health effect and even cause heart attack, angina, or even mortality [
5]. The LCA and RCA which each have multiple branches, make up the majority of the “coronary arteries”, as illustrated in “Coronary artery” flow
Figure 1.
Using X-ray technology and computer processing, the medical imaging procedure known as CT angiography may provide precise pictures of the body’s blood vessels, including the coronary arteries of the heart. The process utilised in CCTA or CTA is especially intended to assess blood flow and obstructions in the coronary arteries.
Since there is no need for catheterization or the insertion of any equipment into the body, the process is non-invasive. Instead, the patient is lying on a table that passes through an apparatus with the shape of a doughnut and emits X-rays at various angles. A computer processes the X-ray pictures to produce finely detailed, three-dimensional views of the heart and blood arteries.
The necessity for enhancing blood flow or repairing blocked arteries may need a different technique because there is no catheter insertion performed during a CT coronary angiography. The coronary calcium scan is a different method that is comparable to a CT coronary angiography. It employs specialized CT images rather than contrast media to evaluate the amounts of calcium or plaque in the constricted arteries. When estimating the risk of main Contrary Cardiac Procedures, CT Angiogram is superior to a coronary CT calcium scan [
6].
Although the importance of the low radiation doses utilized in “diagnostic imaging” is uncertain, there is serious concern about the possibility of an increase in cancer incidence in the community. This impending risk must be balanced in contradiction of the risk of failure to identify serious medical issues, such as coronary artery disease, in a particular individual [
7,
8].
DRL are dose levels determined as 75
th percentile of “dose distribution” for X-ray diagnostic investigations, collections of standard phantoms or standard-sized patients for widely different kinds of equipment. In general, when standard procedures are used, it is anticipated that these thresholds will not exceed for regular processes. A DRL is never given to a single patient; rather, it is given to a group of individuals. However, comparing a patient’s dose to the DRL for a particular examination will give some perspective whether the dose is reasonable; if it is too high or too low, one must consider the clinical justification for the use of the dose or the image quality, respectively [
9]. DRLs are officially described in the ICRP reports as “a type of research level that is applied to an easily measurable quantity, typically the radiation dose absorbed in air or objects that are equivalent to tissue on the surface of a simple standard phantom or a model patient” [
10]. This explanation highlights that DRLs are not dose limits and do not assist in distinguishing between suitable and improper medical activity. Dose reference levels (DRLs) are different from dose limits, as they can be exceeded if it is clinically necessary to do so. Unlike dose limits for occupational exposure, which only require justification and optimization, medical exposures are based on clinical judgment. The dose received by a patient during a CT scan can be influenced by factors such as their weight and body size. DRLs must not be defined as effective doses; instead, they should be established as clearly quantifiable and highly reproducible dose metrics for people with standard sizes or phantoms [
11].
Before establishing DRLs, dose measurements are made using a method that has been previously standardized for each kind of radiation examination. Due to the effect of optimization, DRL may not always apply to current procedures with smaller dose distributions. DRLs developed in specific countries or regions are also frequently assessed to ensure compliance with modifications to standard clinical practice and equipment.
The founding of DRL has provided an enhanced diagnostic advantage across the globe. Data from medical CT procedures must be compared to the reference values to establish DRL. As there are no studies to establish the DRL in North East India, it is crucial to establish the standard dose. As recommended by ICRP (“International Commission on Radiological Protection”) 1991, it is vital to optimizing the usage of ionizing radiation in healthcare and the current study aims to compare all the existing data from India and generate baseline information about the existing practice. This study has the potential to pave the way for more advanced investigations in the future or improve the data of studies that are very comparable to those that may be undertaken in the future.
Methods
During coronary CT examinations, the purpose of this study was to determine the local dose–response curve (DRL) as well as the effective dosage received by the patient. The information used in this research came from one hospital in the Kamrup district of the Assam state, which will be referred to as (X), and one diagnostic center, which will be referred to as (Y) (
Table 2). The study determined a cohort sample size of 380 participants using Raosoft, Inc. software. This calculation was based on a margin of error of 5% and a confidence level of 95%, for a population size of roughly 2,000,000 individuals in Guwahati, Assam. The sample size was determined with consideration of the precision and confidence level desired for the study’s results, relative to the estimated population size in the study area (
Table 1).
For the purpose of this research, data were collected from two different CT scanners. There was one public hospital and one private diagnostic centre having Radiology department that each include required equipment’s. In advance of any data collection, the equipment carried out all quality control tests in accordance with the recommendations of AERB. Experiments were carried out by a Radiological Safety officer who had received authorization from the Atomic Energy Regulatory Board (AERB). Any data tallies that were within a range that was deemed appropriate were included in the study.
To ensure CT scan accuracy, a patient-specific data sheet was used. Every CT machine has a dosimetry CT unit. A data sheet was created to evaluate patient doses and radiation-related factors. Gender, age, tube potential (mA), tube current-time product settings (mAs), pitch, slice thickness, and slice count were collected. All scanning parameters, the dose-length product (DLP) in mSv.cm, and the CT Dose Index volume (CTDIvol) were recorded. Each variable affected radiation dose differently. The Atomic Energy Regulatory Board-authorized radiological safety officer had undertaken quality control tests on the hospital’s and Diagnostic Centre’s CT equipment and found that they met this research’s standards. Ethics were based on ICRP and AERB guidelines (
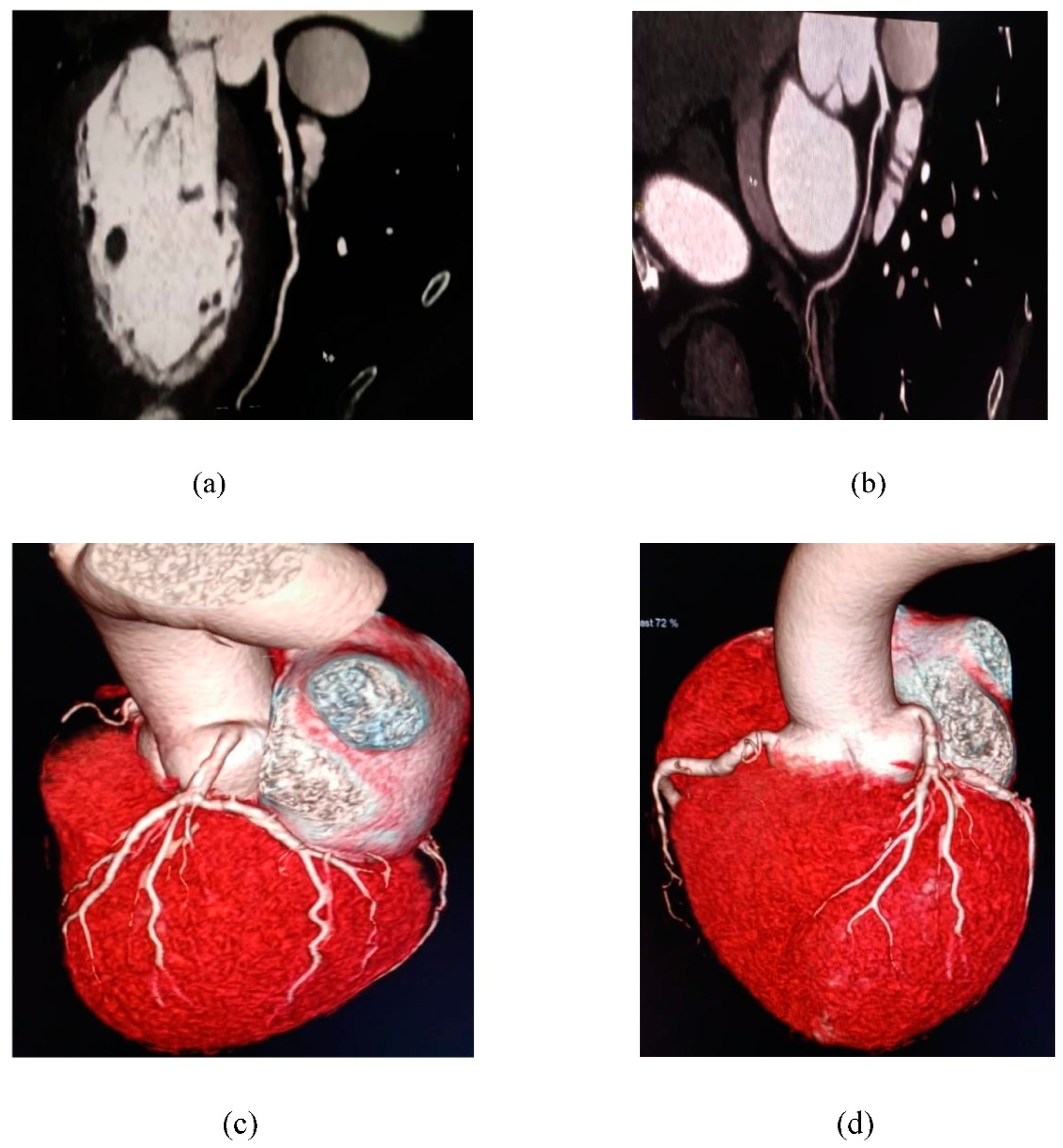
Figure 2,
Figure 3 and
Figure 4).
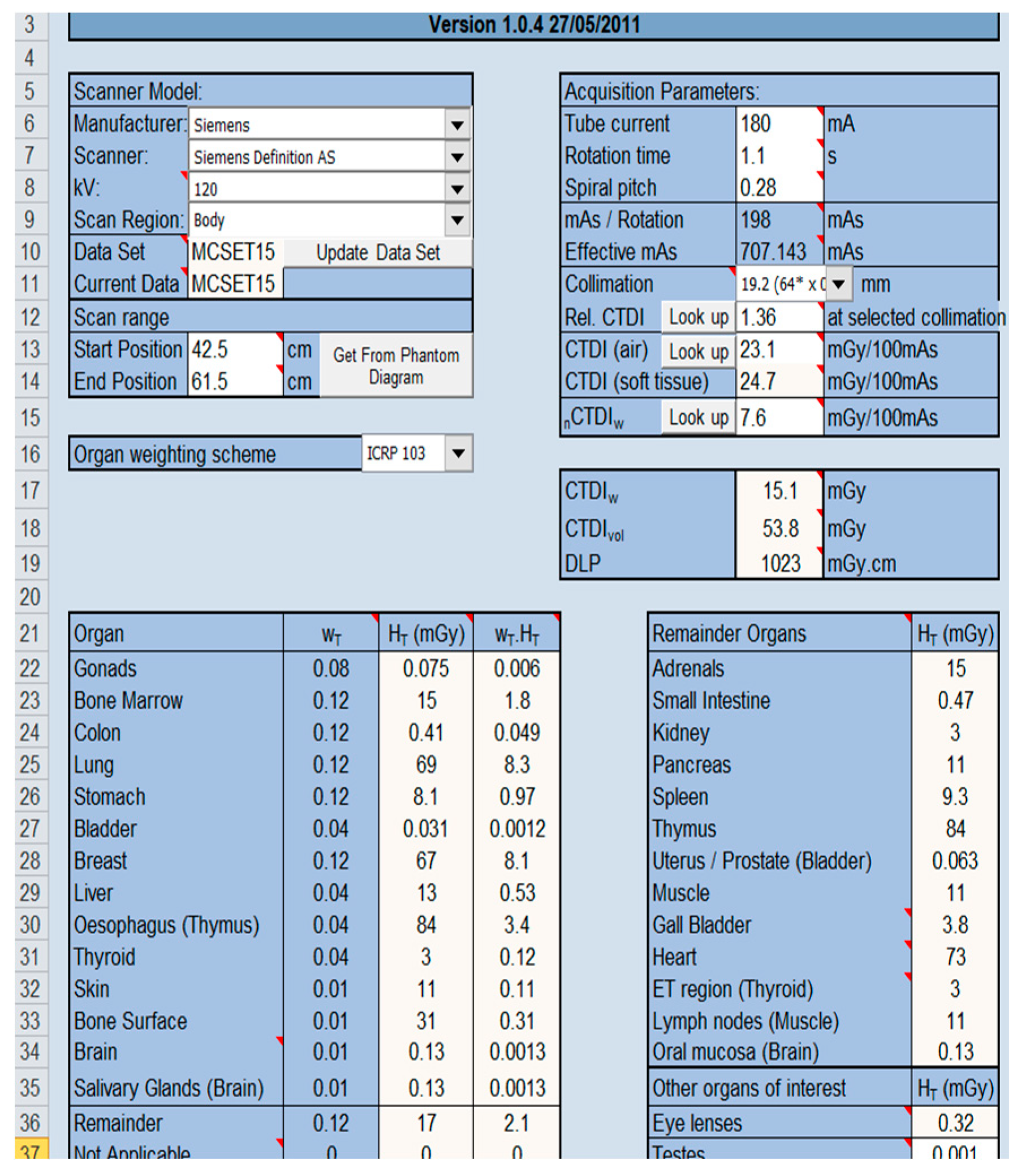
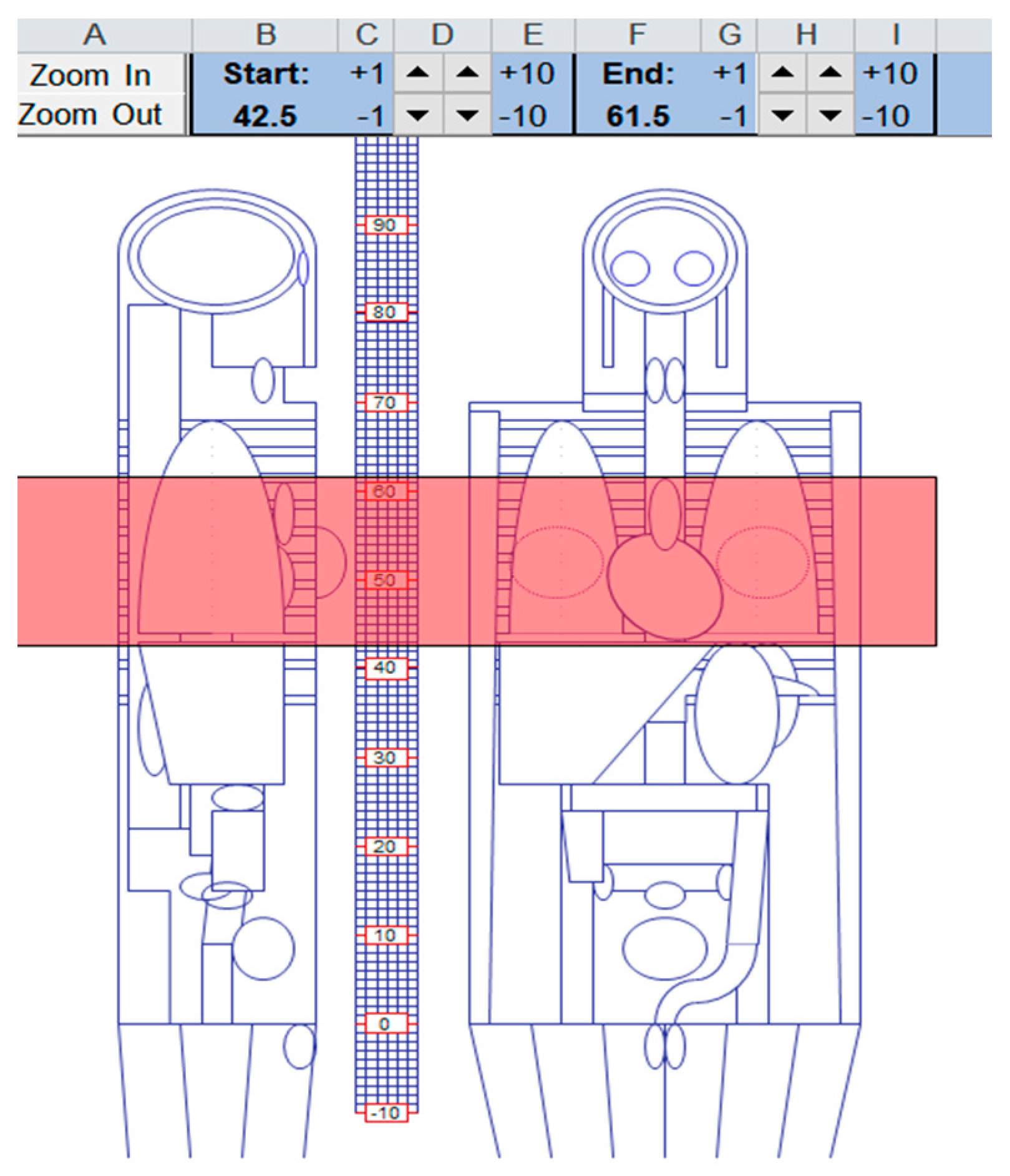
The ImPACT CT patient dosage calculator version 1.0.4, which is a CT dosimetry programme that is available for purchase was utilised. In order to compare and validate the dose values that were generated by the CT scanners to evaluate the accuracy of the dose levels were generated by the machines. The Impact Scan dose evaluator is a system that uses the SR250 Monte Carlo dataset provided by the National Radiological Protection Board in order to simulate exposure circumstances in mathematical phantoms of many well-known brands of CT scanners. These simulations are performed using the Impact Scan (
Figure 2 and
Figure 3).
To measure a patient’s radiation exposure during a CT scan, various parameters are used, such as the CT dose index (CTDI) and the dose length product (DLP). The CTDI measures radiation dose at a point in air, while the CTDIvol considers patient size and tissue thickness. The DLP is the total radiation dose over the entire scan length. To calculate the effective dosage, organ weighting factors and dose coefficients from international radiation protection organizations are used. This information is used by software to provide accurate measurements of radiation dose during a CT scan. These measurements are important to prevent excessive radiation exposure, which can lead to cancer or other health problems related to radiation.
In this study, DRLs were calculated from effective dose using the formula for the third quartile of the 75th percentile (Q3). Third Quartile (Q3) = {3(n+1)/4}th where “n” is the total number. Origin2021 and Microsoft Excel 2010 were used for the statistical analysis. The acquired data was put into an imPACT 1.0.4 version excel spreadsheet using the Monte Carlo SR250 dataset. Descriptive and inferential data analysis techniques were used for the analysis of the results. Descriptive analysis was used to express quantitative variables to summarise and illustrate the variability of the study’s data in terms of mean, range, and standard deviation.
Results
In two hospitals, 380 CT scans were measured for radiation exposures for this study. Hospital X utilized a Siemens Definition AS (128-slice) scanner, whereas Hospital Y used a Philips Ingenuity (128-slice) scanner. These two hospitals are referred to as Hospital X and Hospital Y. The study evaluated DRLs for the two hospitals and gave the dosage measurements in terms of DLP and ED (
Table 3). The spiral mode is used for typical cardiac CT exams with retrospective ECG gating. Effective dosages up to 21 mSv have been recorded without the use of ECG-based tube current regulation [
12]. In
Table 4, the results are broken out in great depth.
Table 3 presents the patient population of the study, along with the classification of Hospitals and Diagnostic Centers for CT Coronary Angiography Examination.
Table 4 shows patient demographic data and body mass index for both male and female populations. The various parameters viz. Mean, SD, Median, Maximum, and Minimum values for the studied populations were depicted here. In this table, it was observed that the BMI ranges from the minimum weight of 19.68 kg/m
2 to the maximum weight of 24 kg/m
2, where the Mean±SD was 22.42±1.05 and the median value of 22.42.
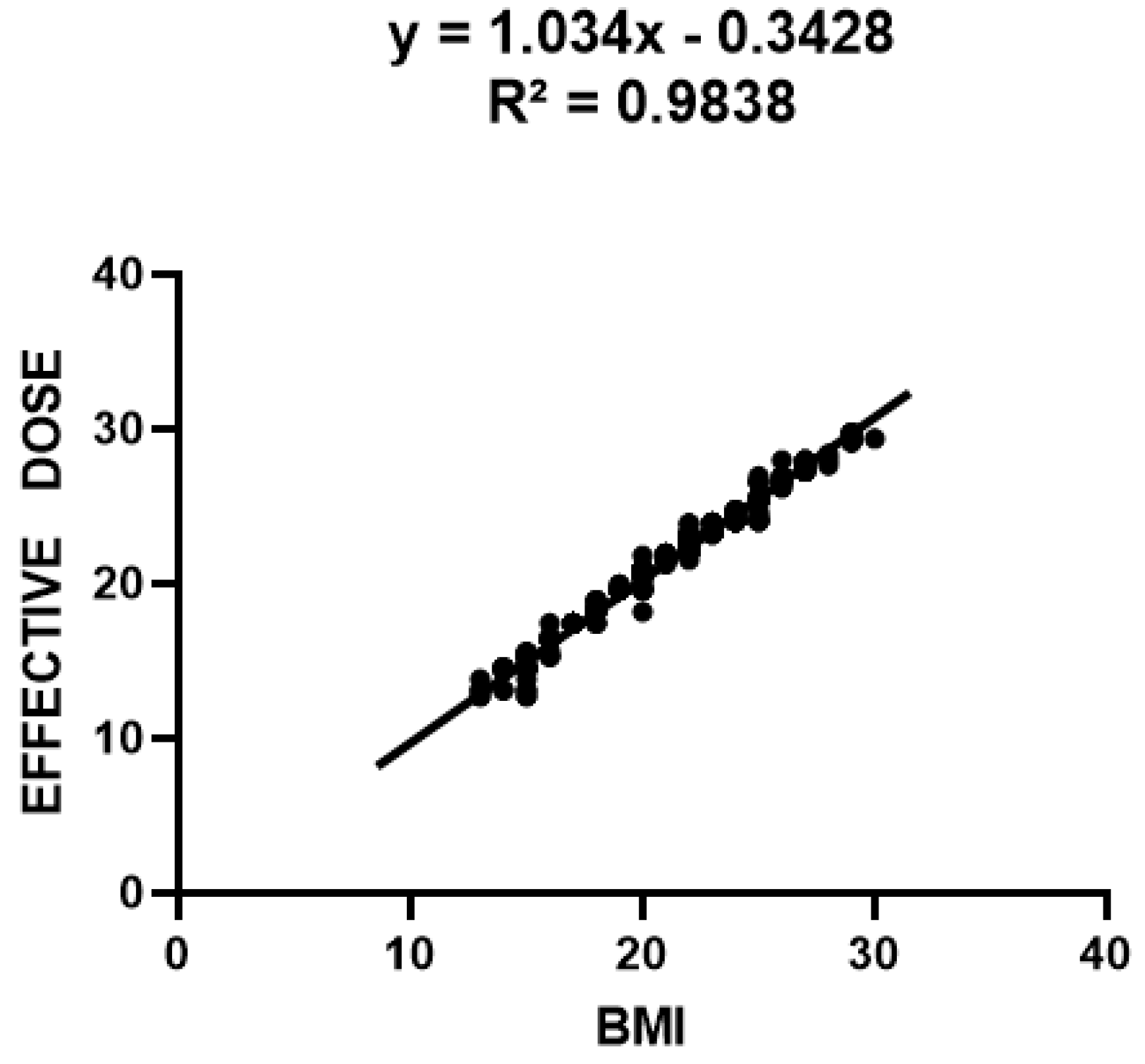
The statistical analysis of the correlation between BMI and Effective Dose for CT Coronary Angiography in a sample of 380 patients is illustrated in
Table 5. This data signifies a robust positive correlation between BMI and the radiation received during CT Coronary Angiography. The Pearson R-value of 0.9918 suggests a highly significant linear correlation between BMI and Effective Dose, with increasing Effective Dose, BMI increases. With an R-square value of 0.9838, the variance can account for around 98% of the variance in Effective Dose in BMI. This suggests that BMI is a very good predictor of Effective Dose for CT Coronary Angiography and that other factors may have little impact on the Effective Dose beyond the influence of BMI. Overall, this information suggests that clinicians should consider the patient’s BMI when determining the appropriate radiation dose for a CT Coronary Angiography, as higher BMIs are likely to require higher doses of radiation to achieve the same image quality.
The link between BMI and effective dosage is depicted in the graph above, which shows a distinct and substantial association between the two factors. Greater BMI levels were shown to correlate to greater effective dosages, indicating a linear link between the two. The fluctuation in BMI may be used to account for 9.84% of the variation in the effective dosage, according to the R square value of 0.09838. A linear connection between BMI (X) and effective dosage (Y) is shown by the equation Y=1.034X-0.3428. The slope of the line is 1.034, while the Y-intercept is -0.3428. The linearity between the effective dosage and BMI in both male and female patients suggests that the effective dose is influenced by the patient’s BMI. Greater BMI values are correlated with greater effective doses, indicating a positive link between BMI and effective dosage.
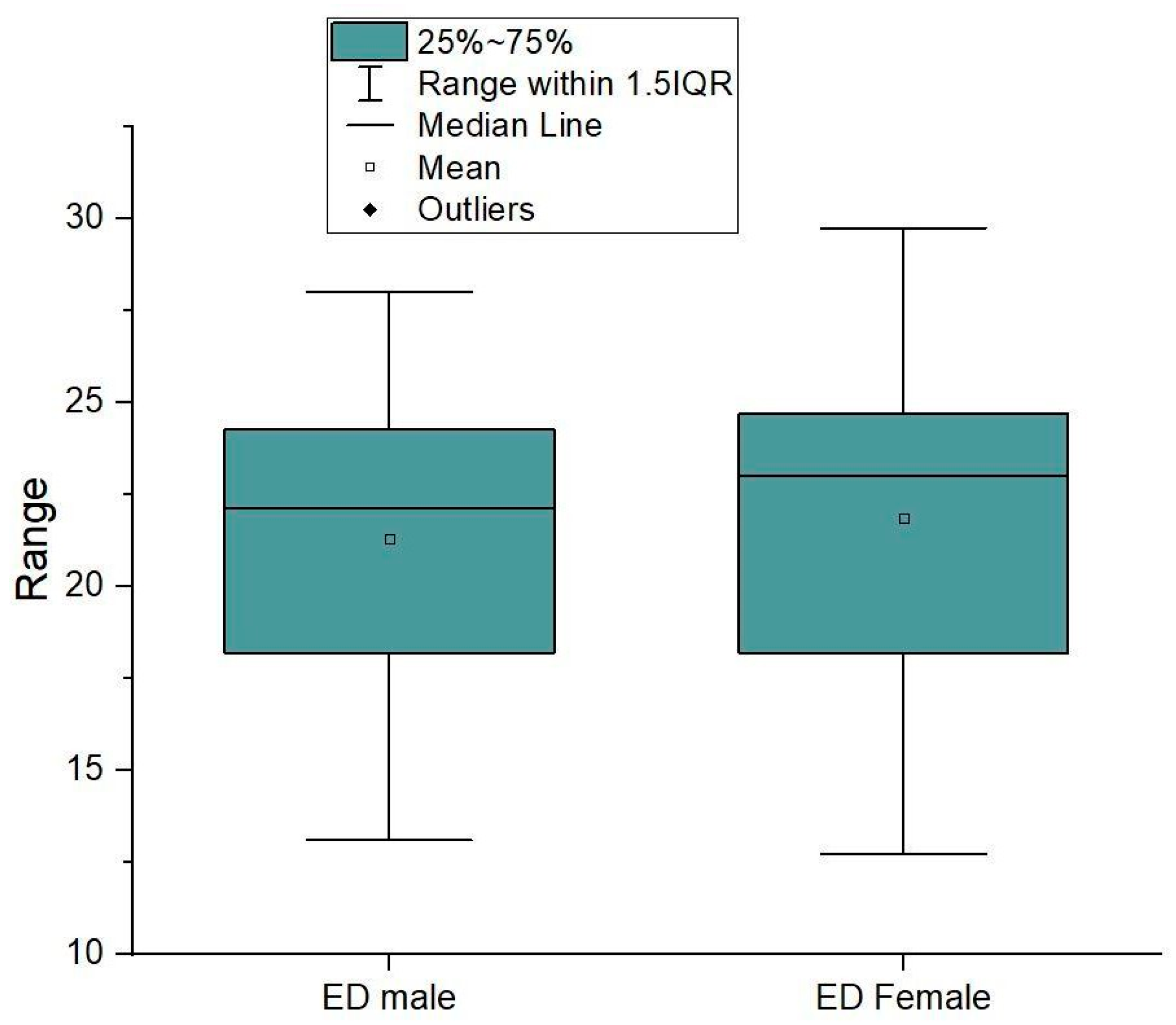
The above
Table 6 reflects that in statistical analyzing data of the entire cases correlation in Effective Dose. The Mean±SD values of Effective Dose were 21.29±3.80 for males, 21.85±4.66 for females, and 21.57±4.27 for both sexes respectively. This indicates that, on average, male patients received a slightly lower radiation dose than female patients during contrast CT coronary angiography, which was also reported in other CT studies [
13]. However, the difference in the mean values between males and females is insignificant. The Maximum to Minimum (Max-Min) Effective Dose ranges for those patients were discovered to be 27.99-13.1 for males, 29.74-12.73 for females, and 29.74-12.73 for both sexes, respectively. This suggests that the range of Effective Dose for a contrast CT coronary angiography is wider than that of non-contrast CT coronary angiography, with the highest dose being approximately two times larger than the lowest dose. It is important to note that Effective Dose is a measure of the amount of radiation that a person receives during a medical imaging test. The dose received depends on various aspects, such as the patient’s size, the type of imaging test, and the imaging parameters used during the test. Therefore, it is crucial to optimize the imaging parameters to reduce radiation exposure in patients, especially those more vulnerable to the potential risks associated with radiation exposure.
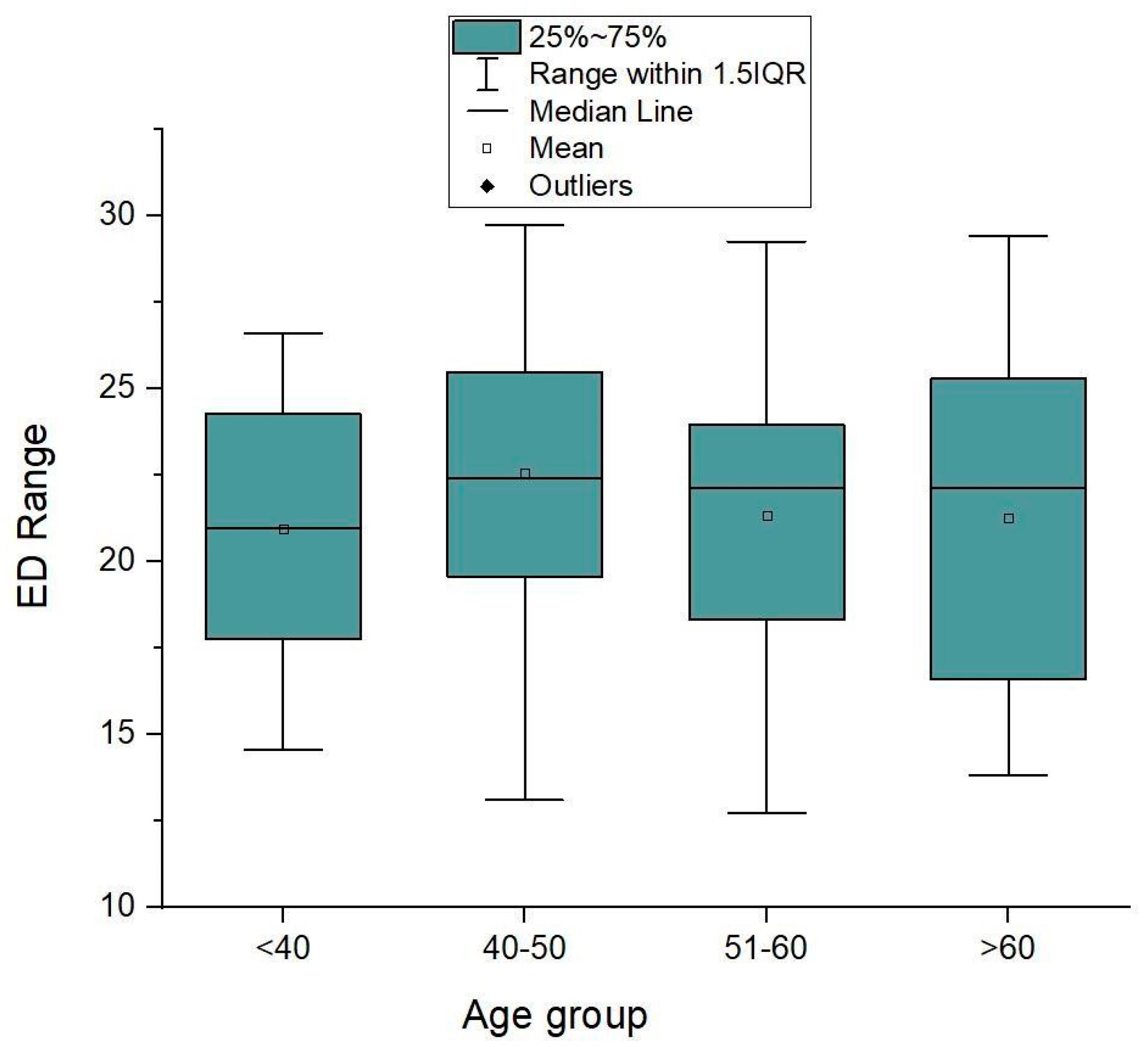
The effective dose range of male and female patients who had contrast CT coronary angiography is shown in the following graph. The average age was somewhere between 29 and 60 years old. In our investigation, a definite age majority was seen. It is generally understood that age may have a substantial impact on how much radiation is exposed during medical imaging exams [
14,
15]. Older patients may require higher radiation doses to obtain images of sufficient quality due to factors such as increased body size, higher body mass index, and the presence of medical comorbidities.
The correlation in DRL for CT Coronary Angiography cases across all cases is shown in
Table 7 above. The DRL values were 24.26 mSv.cm
2 for males, 24.69 mSv.cm
2 for females, and 24.45 mSv.cm
2 for studied populations, respectively.
Discussions
The demographic profile of patients undergoing CT Coronary Angiography (CTCA) can provide important information that can aid in the diagnosis, treatment, and prevention of cardiovascular diseases [
16]. Some important aspects of a patient’s demographic profile relevant to CTCA include age, gender, race/ethnicity, medical history, and lifestyle factors such as smoking, diet, and exercise habit [
17]. The mean and median values being close to each other suggest that the distribution of BMI values is roughly symmetric. The relatively small standard deviation of 1.05 kg/m
2 indicates that the BMI values are tightly clustered around the mean. Overall, this information suggests that the population or sample from which the BMI values were obtained has a relatively narrow range of BMI values and is likely to be relatively homogeneous with respect to BMI.
Numerous studies have focused on the relationship between BMI and Effective Dose for CTCA [
18] conducted a study that discovered a positive correlation between BMI and Effective Dose for CTCA, with an average increase of 18% in Effective Dose for every increment of 5 kg/m
2 in BMI [
18]. According to another study, the Effective Dose for CTCA rose by 13% with each 5 kg/m
2 increase in BMI [
19]. They recommended that for patients undergoing CTCA, radiologists should be aware of the association between BMI and radiation exposure and take steps to minimize the radiation dose whenever possible, such as by using lower tube voltage and current settings, optimizing scan parameters, and using dose-reduction techniques.
Similar studies have demonstrated that a higher BMI is linked to an increased radiation dosage because adipose tissue absorbs less radiation due to its lower density than other tissues [
20,
21]. Another study found that higher BMI was associated with increased radiation exposure during medical imaging, particularly for CT scans. The authors noted that this could have important implications for cancer risk, given the known association between radiation exposure and cancer [
22]. The R square value of 0.09838 suggests that only 9.8% of the variability in effective dose can be explained by BMI. While this relationship is statistically significant, it is relatively weak, and other factors such as age, sex, and the specific imaging procedure being performed may also play a role in determining an effective dose. In conclusion, the relationship between BMI and effective dose observed in the
Figure 5 is consistent with findings in the existing literature. However, the relatively weak relationship and the importance of other factors in determining effective dose suggest that caution should be exercised in interpreting this relationship in isolation.
Effective dose is a measure of the amount of radiation energy that is absorbed by the body during a medical imaging test, and it takes into account the type of radiation and the sensitivity of the different organs in the body to radiation. The graph above shows the range of effective doses for male and female patients who underwent a contrast CT coronary angiography study. The mean effective dose ranges for males and females were approximately 13 to 28 mSv and 12 to 29 mSv, respectively. This indicates that there is a wide variability in the amount of radiation exposure that patients receive during this type of imaging test. It is essential to minimize the radiation exposure to patients during imaging tests, especially for those who may require multiple tests or who are more sensitive to radiation. This is where radiation dose reduction techniques become important. These techniques involve optimizing the imaging parameters, such as the tube current, tube voltage, and scan duration, to reduce the radiation exposure while still obtaining high-quality images for accurate diagnosis. It is crucial to note that the effective dose range shown in the graph is influenced by several factors, including patient size, the type of scanner used, the scan protocol, and the operator’s skill level. Therefore, it is essential to follow standard imaging protocols and to have well-trained operators to minimize the variability in radiation exposure between patients. In summary, the graph above (
Figure 6) highlights the importance of optimizing the imaging parameters and using radiation dose reduction techniques to minimize radiation exposure to patients during contrast CT coronary angiography while still obtaining high-quality images for accurate diagnosis. diagnosis [
23,
24]. It is important to regard age as a potential factor when optimizing imaging protocols and reducing radiation dose in patients. It is vital to note that radiation exposure from medical imaging tests, including contrast CT coronary angiography, can pose potential risks to patients, especially those who are more vulnerable, such as children and pregnant women [
22,
25]. Therefore, it is crucial to use the ALARA (As Low As Reasonably Achievable) principle to reduce radiation exposure in patients while preserving diagnostic image quality [
26,
27]. The use of the phantom to quantify CT dosage was the study’s principal flaw. Since it takes into account both controllable (imaging technique, tube voltage, tube current) and uncontrollable (patient orientation, collimation, and distance) factors, the use of the patient may have been preferable. Even though using phantom produces almost identical exposures, it only addresses elements under our control [
28].
DRLs are recommended levels of radiation exposure for typical patients undergoing a specific type of imaging procedure [
29]. They are meant to be a benchmark to optimize imaging protocols and reduce unnecessary radiation exposure while maintaining image quality [
30]. It should be emphasized that these values do not represent absolute limits, and certain patients may require higher doses for diagnostic purposes based on factors such as their age, body size, and the specific medical condition being examined. Nevertheless, medical practitioners should carefully evaluate the potential risks and benefits of the imaging procedure and aim to use the lowest possible dose that will still provide the necessary diagnostic information.
Conclusions
The establishment of a diagnostic reference level (DRL) tailored to the Northeast Assam population is a significant milestone. This DRL serves as a benchmark, enabling healthcare providers to monitor and optimize radiation doses during coronary angiography CT scans, ensuring that patients receive the necessary diagnostic information while minimizing unnecessary exposure.
Additionally, this study underscores the importance of region-specific DRLs, as population characteristics and healthcare practices can vary across different geographic areas. By tailoring radiation dose guidelines to the local population, healthcare providers can further enhance patient safety and contribute to the overall improvement of healthcare quality.
In order to reduce the hazards of radiation exposure and ensure adequate diagnostic data, this research aims to optimise the radiation dose given to patients during Computed Tomography Coronary Angiography (CTCA). For maximising CTCA dosage, the DRL offers a starting point. Optimizing radiation exposure for patients will be made possible by calculating the radiation dose provided during CTCA in relation to the DRL.
CT scanning techniques may be improved as a result of the large reported diversity in effective dosage and organ doses in the current investigation.
It is advised that the current study contribute to the establishment of scanning parameters with regard to the patient’s size and the body region of interest being scanned.
Extensive research involving larger sample size is recommended for employing radio-protective ingredients to protect radiosensitive organs.
There is a need to increase practitioners’ (radiographers, radiologists, medical physicists, and hospital administrators’) understanding of the importance, adherence, and implementation of diagnostic reference levels in optimizing computed tomography practice.
The study findings suggested that the Atomic Energy Regulatory Board may initiate setting up a national dose reference level nationwide for the CTCA examination where this study may contribute as a benchmark for future reference.
The hospitals and the diagnostic centres which practicing this procedure may helpful by utilizing this Radiological data.
Ethical Approval
AdtU/Ethics/PhD Scholar/2021/009 w.e.f 24/09/2021
Consent for Publication
On behalf of all the authors I Corresponding author have given you the consent for publication.
Availability of data and material
Data will be available on request through email.
Author Contributions
AJDS- Manuscript Preparation, Statistical Data analysis, writing of manuscript JS- Concept, Data analysis, writing, Statistical analysis MPS- Concept, Study design, writing, data analysis MKS- Preparation of Manuscript, Study design, writing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
Authors Acknowledge Assam down town University for allowing to conduct this study.
Conflicts of Interest
The authors do not have any competing Interest.
References
- Kalender, W.A. Dose in x-ray computed tomography. Physics in Medicine & Biology 2014, 59, R129. [Google Scholar] [CrossRef]
- Hsieh, J. Computed tomography: principles, design, artifacts, and recent advances, 2003.
- Fernandes, E.D.; Kadivar, H.; Hallman, G.L.; Reul, G.J.; Ott, D.A.; Cooley, D.A. Congenital malformations of the coronary arteries: the Texas Heart Institute experience. The Annals of Thoracic Surgery 1992, 54, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.W.; Pepine, C.J. Microvascular coronary dysfunction and ischemic heart disease: where are we in 2014? Trends in Cardiovascular Medicine 2015, 25, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.S.; Hoffmann, U.; Patel, M.R.; Mark, D.B.; Al-Khalidi, H.R.; Cavanaugh, B.; Cole, J.; Dolor, R.J.; Fordyce, C.B.; Huang, M. Outcomes of anatomical versus functional testing for coronary artery disease. New England Journal of Medicine 2015, 372, 1291–1300. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Lu, B.; Gao, Y.; Jiang, S.; Wang, Y.; Li, W.; Budoff, M.J. Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC: Cardiovascular Imaging 2012, 5, 990–999. [Google Scholar] [CrossRef]
- Hart, D.; Wall, B.F. Radiation exposure of the UK population from medical and dental X-ray examinations. NRPB Chilton, UK, 2002. [CrossRef]
- Gerber, T.C.; Carr, J.J.; Arai, A.E.; Dixon, R.L.; Ferrari, V.A.; Gomes, A.S.; Heller, G.V.; McCollough, C.H.; McNitt-Gray, M.F.; Mettler, F.A. Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radi. Circulation 2009, 119, 1056–1065. [Google Scholar] [CrossRef]
- Abdullah, A. Establishing dose reference level for computed tomography (CT) examinations in Malaysia. Universiti Sains Malaysia, 2009.
- Protection, R. ICRP publication 103. Ann ICRP 2007, 37, 2. [Google Scholar]
- Vassileva, J.; Rehani, M. Diagnostic reference levels. AJR Am J Roentgenol 2015, 204, W1–W3. [Google Scholar] [CrossRef]
- Sarma, A.D.; Singha, M.K.; Sharma, J. Estimation of Patients Effective Dose with respect to BMI using Monte Carlo Simulation method for CT Coronary Angiography Patients. NeuroQuantology 2022, 20, 599. [Google Scholar]
- Hunold, P.; et al. Radiation exposure during cardiac CT: effective doses at multi–detector row CT and electron-beam CT. Radiology 2003, 226, 145–152. [Google Scholar] [CrossRef]
- Alzen, G.; Benz-Bohm, G. Radiation protection in pediatric radiology. Deutsches Ärzteblatt International 2011, 108, 407. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. Jama 2012, 307, 2400–2409. [Google Scholar] [CrossRef]
- Aupongkaroon, P.; Makarawate, P.; Chaosuwannakit, N. Comparison of radiation dose and its correlates between coronary computed tomography angiography and invasive coronary angiography in Northeastern Thailand. The Egyptian Heart Journal 2022, 74, 6. [Google Scholar] [CrossRef]
- Kones, R. Recent advances in the management of chronic stable angina I: approach to the patient, diagnosis, pathophysiology, risk stratification, and gender disparities. Vascular health and risk management 2010, 6, 635. [Google Scholar] [CrossRef] [PubMed]
- Einstein, A.J.; Henzlova, M.J.; Rajagopalan, S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. Jama 2007, 298, 317–323. [Google Scholar] [CrossRef]
- Hausleiter, J.; et al. Estimated radiation dose associated with cardiac CT angiography. Jama 2009, 301, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Das, P.; Subkovas, E.; Buch, A.N.; Rees, M.; Bellamy, C. Radiation dose during coronary angiogram: relation to body mass index. Heart, Lung and Circulation 2015, 24, 21–25. [Google Scholar] [CrossRef]
- Wang, R.; et al. Image quality and radiation dose of low dose coronary CT angiography in obese patients: sinogram affirmed iterative reconstruction versus filtered back projection. European journal of radiology 2012, 81, 3141–3145. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.C. Radiation risk from medical imaging. in Mayo Clinic Proceedings 2010, 85, 1142–1146. [Google Scholar] [CrossRef]
- McCollough, C.H.; Primak, A.N.; Braun, N.; Kofler, J.; Yu, L.; Christner, J. Strategies for reducing radiation dose in CT. Radiologic Clinics 2009, 47, 27–40. [Google Scholar] [CrossRef]
- Gottumukkala, R.V.; Kalra, M.K.; Tabari, A.; Otrakji, A.; Gee, M.S. Advanced CT techniques for decreasing radiation dose, reducing sedation requirements, and optimizing image quality in children. Radiographics 2019, 39, 709–726. [Google Scholar] [CrossRef] [PubMed]
- Power, S.P.; Moloney, F.; Twomey, M.; James, K.; O’Connor, O.J.; Maher, M.M. Computed tomography and patient risk: facts, perceptions and uncertainties. World journal of radiology 2016, 8, 902. [Google Scholar] [CrossRef] [PubMed]
- Hausleiter, J.; Meyer, T. Tips to minimize radiation exposure. Journal of Cardiovascular Computed Tomography 2008, 2, 325–327. [Google Scholar] [CrossRef]
- Shah, N.B.; Platt, S.L. ALARA: is there a cause for alarm? Reducing radiation risks from computed tomography scanning in children. Current opinion in 2008.
- Sarma, A.D.; Singha, M.K.; Sharma, J.; Kashyap, D.M.P. Estimation of Effective Dose in Monte Carlo Simulation Method for CT Coronary Angiography Patients. Int. J. Life Sci. Pharma Res 2023, 13, L194–L201. [Google Scholar]
- Thomas, P. National diagnostic reference levels: What they are, why we need them and what’s next. Journal of Medical Imaging and Radiation Oncology 2022, 66, 208–214. [Google Scholar] [CrossRef]
- Wall, B. Diagnostic reference levels—the way forward. The British Journal of Radiology 2001, 74, 785–788. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).