Submitted:
20 September 2023
Posted:
22 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. The First and Second Parts of Making the Surgical Guide for TADs
2.1. Part 1: Rationale for Using a Surgical Guide in the Implantation of TADs
- The thickness of the mucosal layer in different areas of the mouth can affect the selection of the TAD’s length [30]. When selecting a placement location, choose an attached gingival site rather than a flabby mucosa [31]. However, in some cases, implantation on a flabby mucosa cannot be avoided. Using a surgical guide makes locating the initial pilot hole made during the pre-drilling process easy. The surgical guide will save time and effort searching for the insertion point, as mucosa often covers it. For optimal results, it is recommended to utilize two surgical guides during the procedure: one for the pilot drill and another for the TAD. When placing them in the interdental bone between two teeth, having 0.5 mm of septal bone around the TAD is crucial [32]. In interdental placement, at least 2.4 mm of the interdental bone may be needed to avoid damaging the roots, considering that TADs usually have a diameter of 1.4 mm [33,34].
- Different TADs come in various head designs and sizes, so it is recommended to create a surgical guide to match the chosen TAD’s dimensions. Laboratory technicians and clinicians should communicate to design an appropriate surgical guide. While the body of the TAD may be self-drilling, it is still recommended to use a pilot drill surgical guide to minimize any trauma to the soft tissue [35]. The surgical guide is particularly important for angulated insertion procedures to make it easier to enter the implantation site. The angle at which screws are inserted can vary depending on personal preference. Some people prefer an angle for stability, while others aim to avoid root collisions and position the screw tip apically. However, angled screw insertion is more challenging than straight insertion. A surgical guide can assist with accurate angulation insertion, and directional drilling requires a guide to prevent slipping. Designing the surgical guide insertion process for easy handpiece and bur manoeuvrability1 during implantation is crucial.
- Using a healthy tooth structure is necessary for a surgical guide to be in a stable position. If there is any doubt about the stability of the teeth in the intended placement, the number of teeth to be used as support for the surgical guide should be increased [36].
- The force required to penetrate bone with a TAD varies from 20 N to 35 N, depending on the diameter. Placement typically occurs at a speed of 25 Rpm, while drilling occurs at 800 Rpm with water irrigation [37]. It is better to load immediately rather than waiting for weeks and leaving it unloaded [38,39].
- It is mandatory to maintain sterilization and follow the aseptic procedure during the implantation process.
2.1.1. Collecting Data, Planning, and Designing in Consideration of the Making of the Surgical Guide
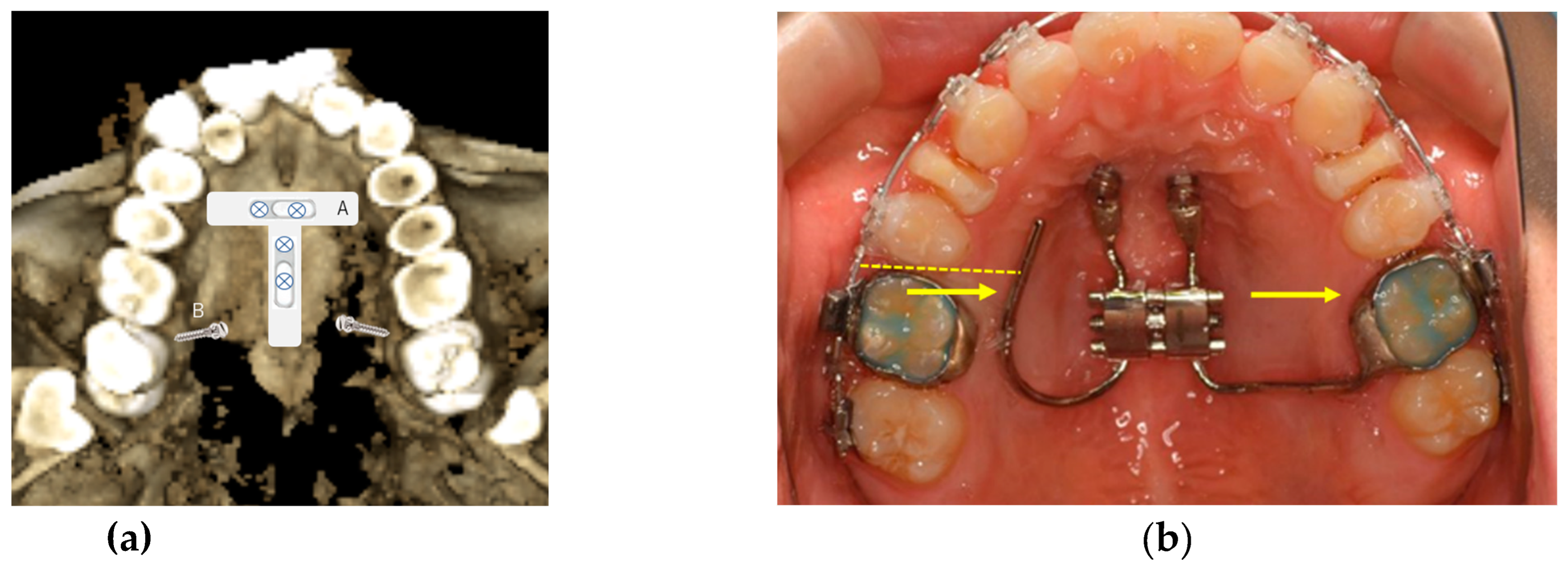
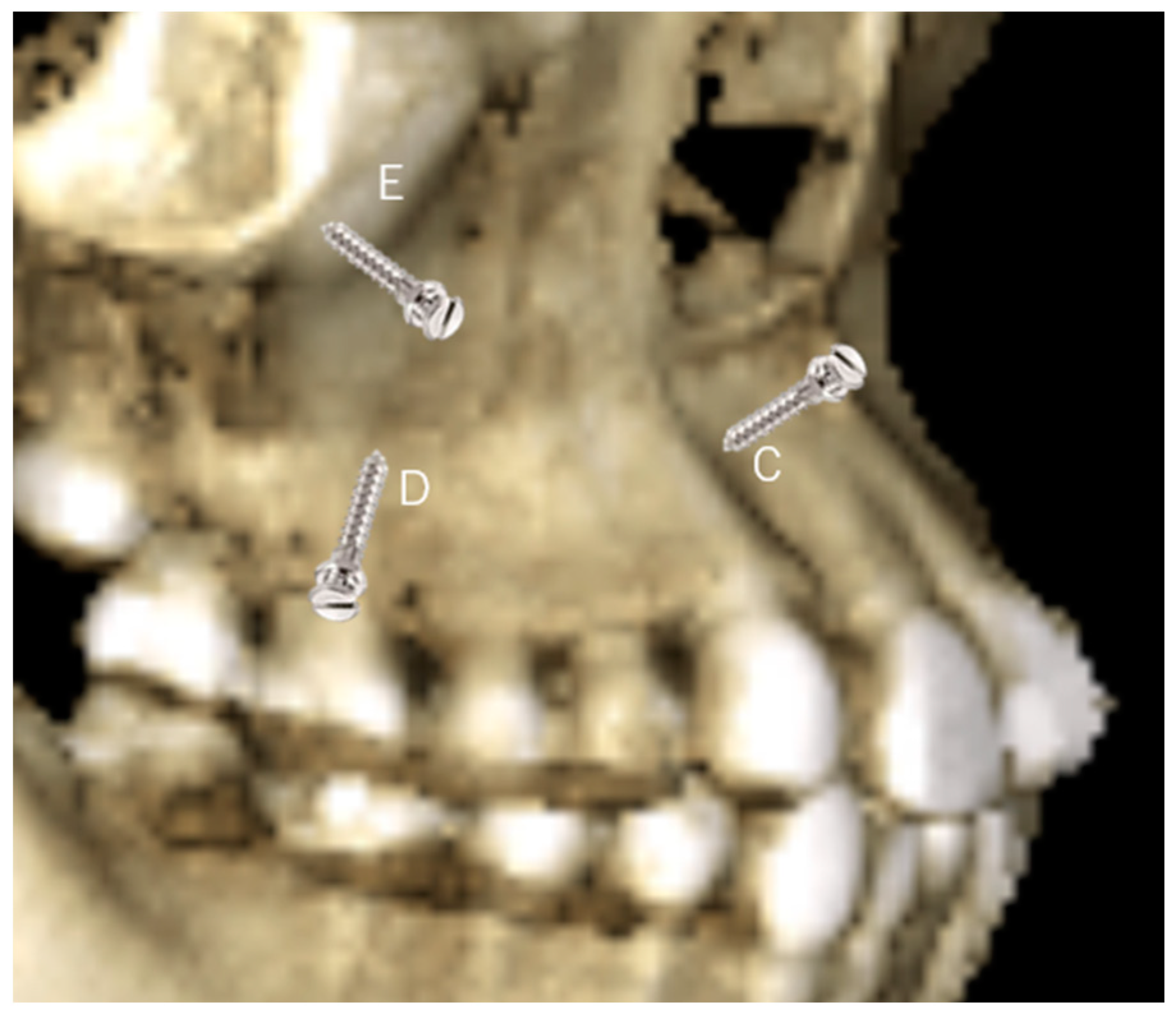
- In the maxilla, CBCT is used to look for the ideal places and the palatal sites in the T-zone, as described by Wilmes [39]. The system’s benefit is two screws being used to connect a plate to make it a sturdy anchorage for 3D movement of the upper teeth. Therefore, the two screws’ placement is critical to insert the plate easily and quickly, such as parallel or close to the parallel to provide easy fixation [40,41,42,43]. The surgical guide will facilitate the parallel insertion of TADs. TADs are placed at the best bone density in the area intended to be the anchorage placement. The other option for the TAD’s site in the palatal bone is between the first molar and the second bicuspid area; the first molar has only a single palatal root (two roots on buccal), and the distance to the second bicuspid’s root is the widest space available between the root’s placement in the posterior region [44]. The placement on the buccal side can also be performed with the surgical guide in the anterior teeth between the central and lateral teeth, interdental for the bicuspids, and the buccal ridge underneath the zygomatic process [45].
- 2.
- In the mandible, TAD placement on the lingual side of the mandibular arch be challenging; there is an advantage if there are lingual tori that are large enough to provide the TAD’s implantation [46]. Most of the time, the buccal region is the only choice. The anterior part of the buccal dental arch will have limited interdental bone availability, and the quality of bone is often questionable. A critical evaluation of available bone width is necessary before the implantation. Interdental space can be more suitable when appropriately placing the brackets to flare the crowded roots. Changing angulation of the roots by adjusting bracket placement beforehand is a common practice in placing TADs in the anterior region.
- 3.
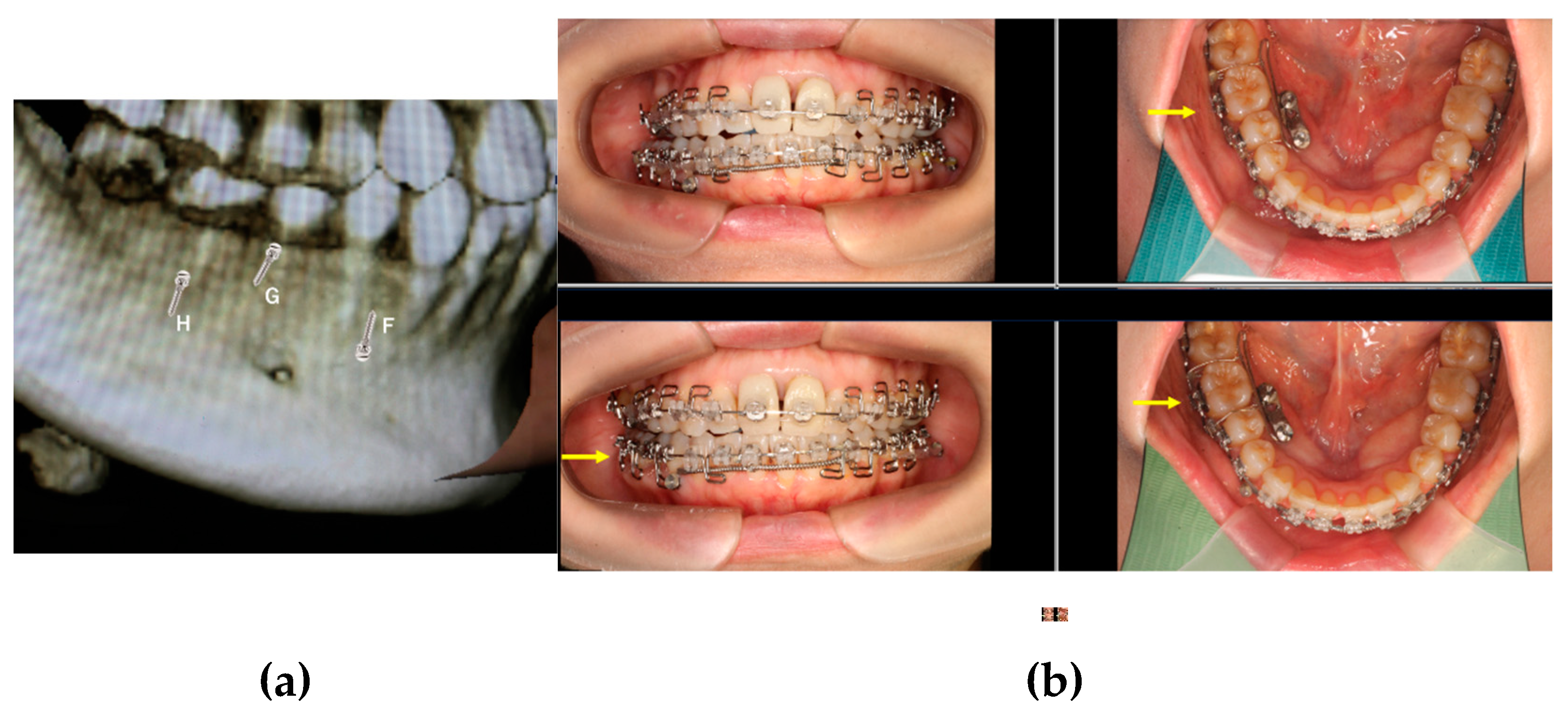
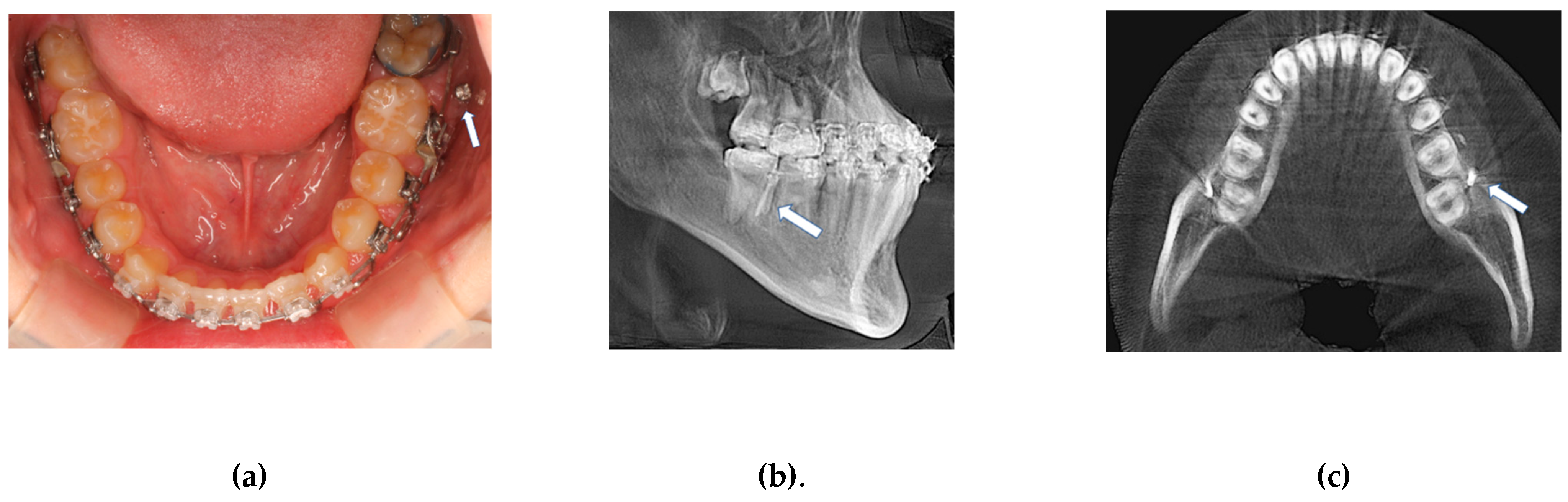
- The implantation in the interdental bone will limit the movement of the tooth, mesial and distal. Therefore, to avoid interferences with roots, the TADs are preferred on the mandible’s ridge or the mandible’s oblique line (Figure 3a, H), especially when en mass retraction of the arch is desirable. The ridge of the mandible between the body and the ramus of the mandible is a favorable site for TAD placement [47]. The tricky part is that the mandible ridge may seem insignificant in women relative to men, and modification may be needed in the surgical guide’s design [48,49]. Since the placement location is a steep bone wall, manual placement will be challenging, so a surgical guide is preferred. The angulated placement of the TADs in this area and the flabby mucosa also necessitates using a surgical guide. Care must be taken during the intraoral scan as the superficial mucous membrane above the ridge must be gently stretched to record this critical area. Lack of recorded data in this area will affect the visibility of the area site, and the surgical guide cannot be planned. Implantation in this area is recommended using contra-angle motorized instruments, as the buccal cheek tissue prevents using a hand screwdriver and will obstruct the surgeon’s vision. The buccal musculature, maxillary teeth, and mouth opening will limit the manoeuvrability of the placement procedure. These limitations should be evaluated during a clinical examination. Considering the hindrance of lower lip movements, placement between the four incisors should be avoided as much as possible. TADs in this area can cause painful lip ulcerations with delayed healing. The location of the canine and the first bicuspid (Figure 3a, F) is an area that can fit for the implantation choice. This location is between anterior and posterior dental arch segments and thus will provide an excellent place to resolve both anterior and posterior malocclusion. Depending on the extraction case or non-extraction case, considerations can be different, and placement in the extraction site of the bicuspid and adjacent area is required to avoid proximity to vital structures in the mentalis foramen. In Figure 3a, G location is possible when there is a need to retract the anterior teeth after an extraction case where placement of the ridge of the mandible is difficult or impossible due to the younger age of the patient. Placement at a young age, e.g., under 12, is risky as bone metabolism is still high in this area.
2.1.2. The Clinical Application of TADs Using the Surgical Guide, an Example Case
2.2. Part Two: The Procedure of Making the Surgical Guide for TADs
2.2.1. The Surgical Guide Technique for TAD Placement
2.2.2. Sequences of Digital Workflow to Make Surgical Guides
- We used an intraoral scan for the SLT (CEREC of Sirona Co., Erlangen, Germany) and a CBCT X-ray (Planmeca, Finland) machine for the DICOM data to obtain a digital impression. Afterward, we superimposed the STL and DICOM data using a commercialized application.
- The 3Shape Ortho System 2021.1 Appliance Designer software completes the process of designing a surgical guide. By utilizing software, the diameter of the drill bur and screw holder can be determined, ensuring no contact with the roots during the procedure. The 3-Shape software simulates the screw placement within the bone’s anatomic area. This simulation helps determine the tube design required for drilling and screw placement.
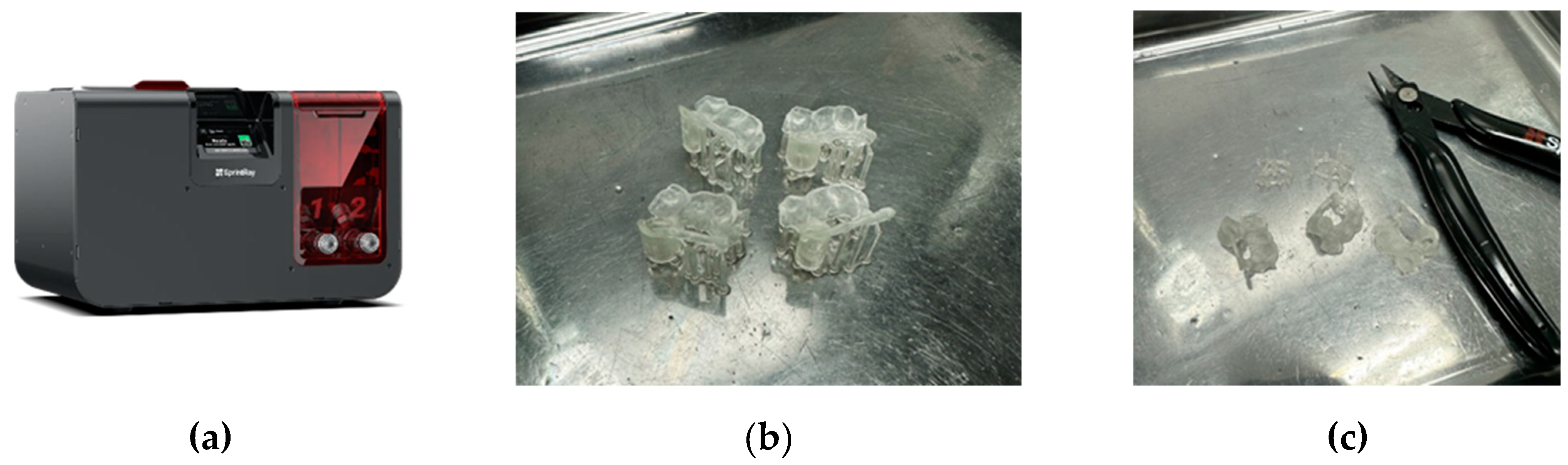
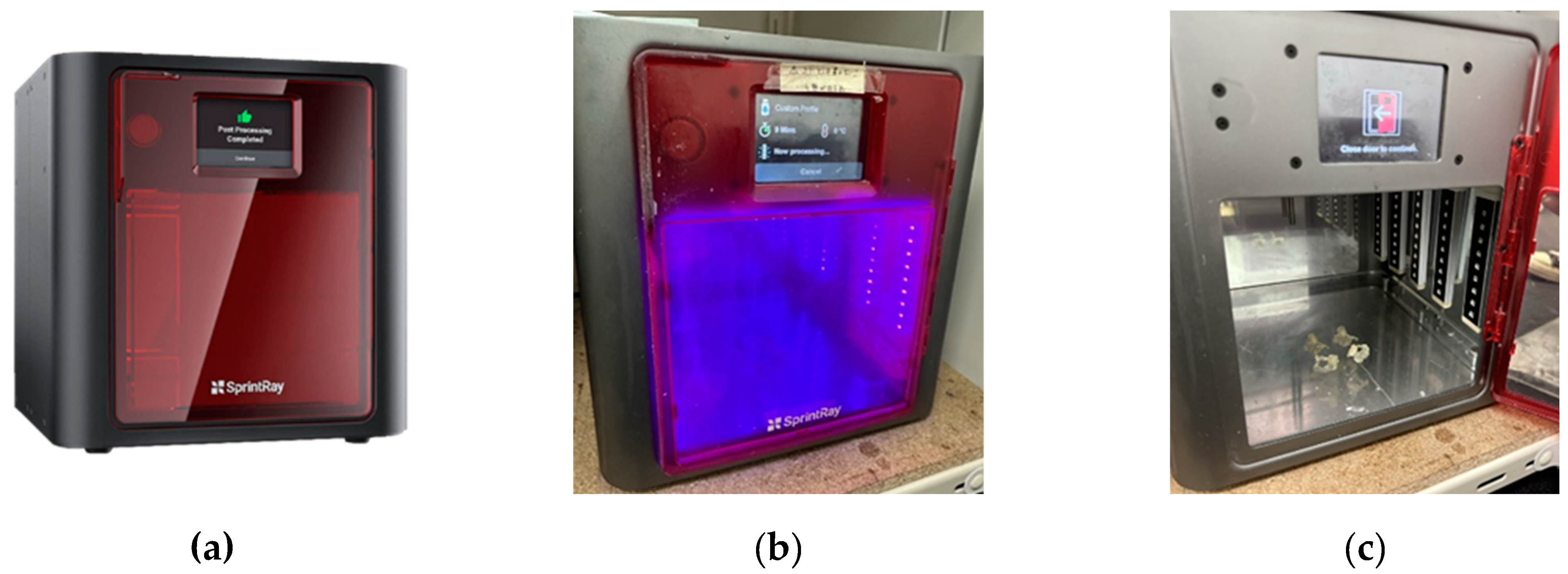
- It is easy to print in a 3D printer (SprintRay Pro95: (SprintRay, Los Angeles, CA, USA) with the material of SprintRay Sugical Guide3 (SprintRay, Los Angeles, LA, USA).
- Next, there is cleaning, washing, drying, and cutting of the supporting pillars, followed by post-curing (ProWash/Dry (SprintRay, Los Angeles, CA, USA).
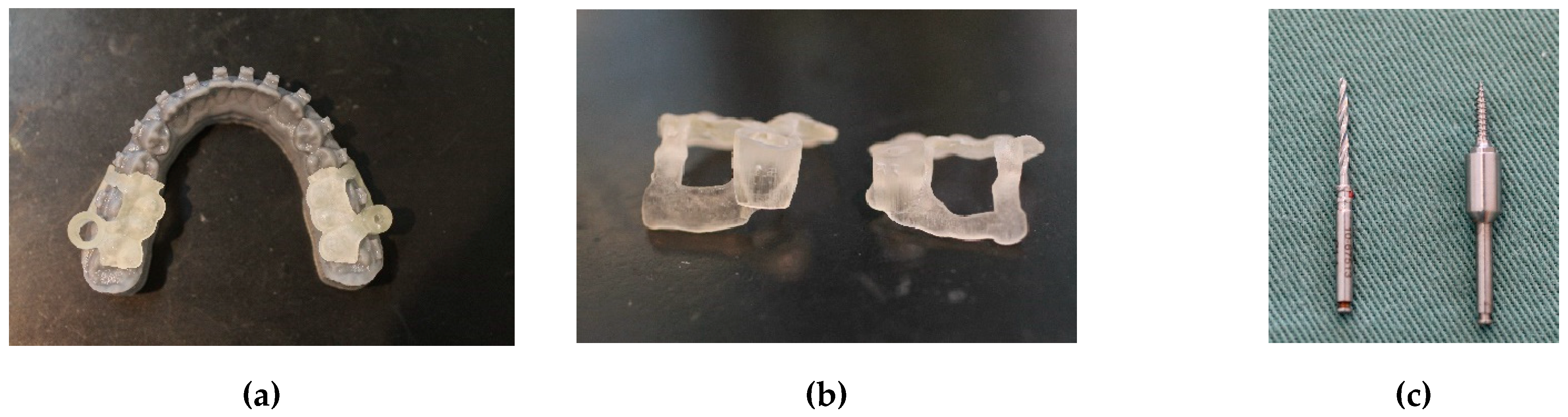
- After checking and testing the surgical guide of both the drilling guide and screw, the holder guide is then placed upon the model of the jaw to check its fitness. When there are brackets, holes can be made to avoid retentions.
2.2.3. Digital TAD Guide Production Process
- 1.
-
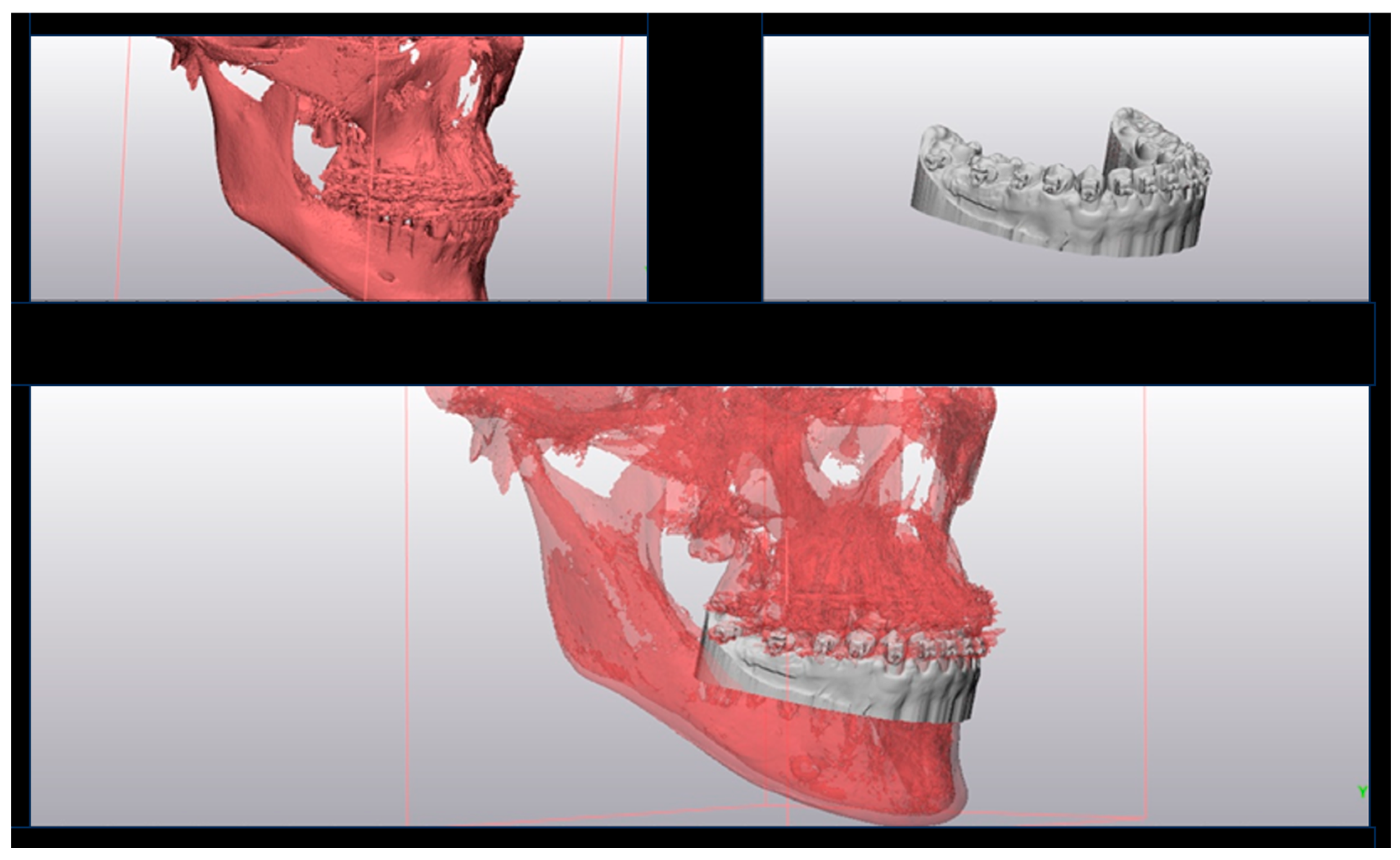
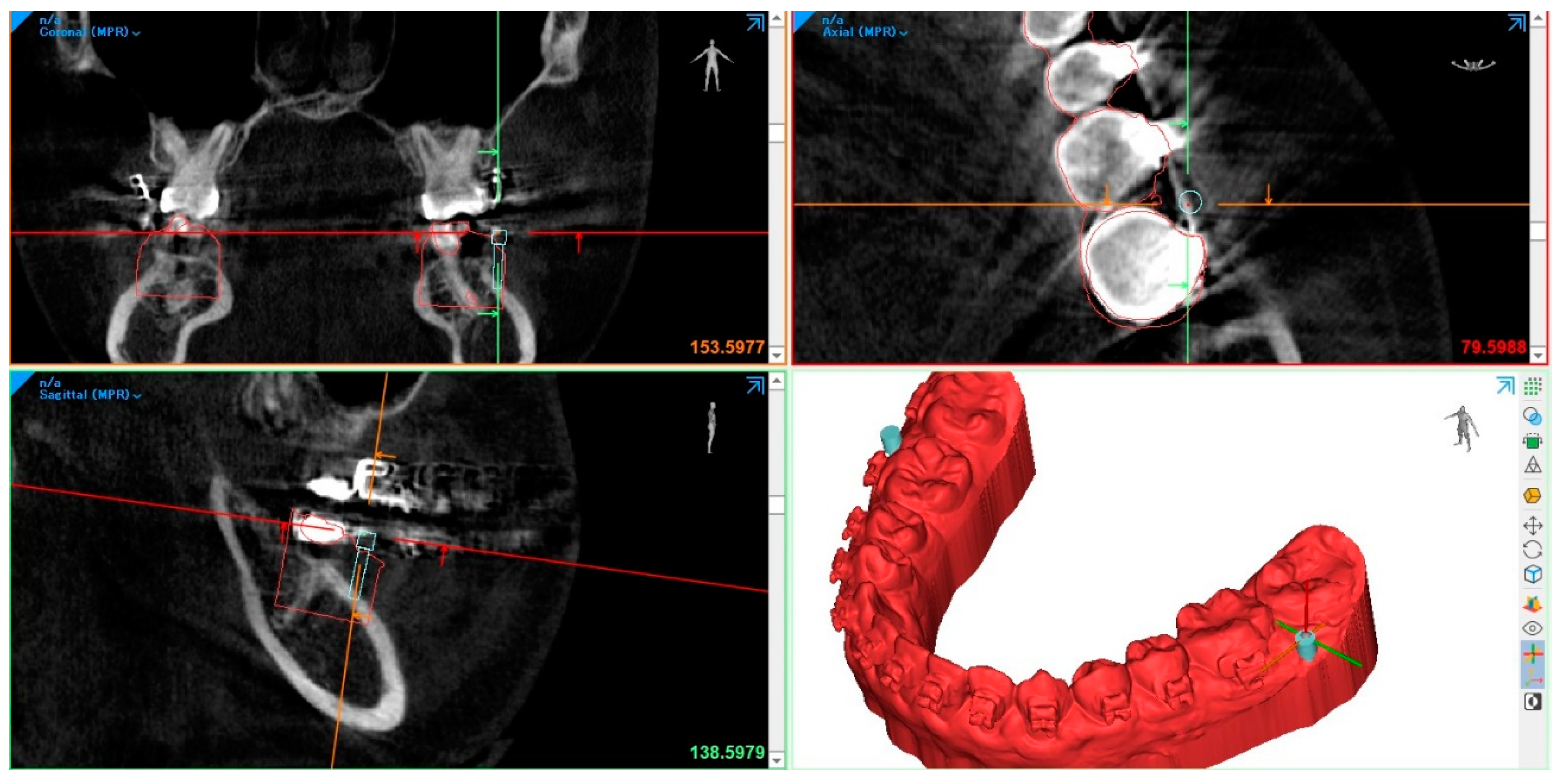
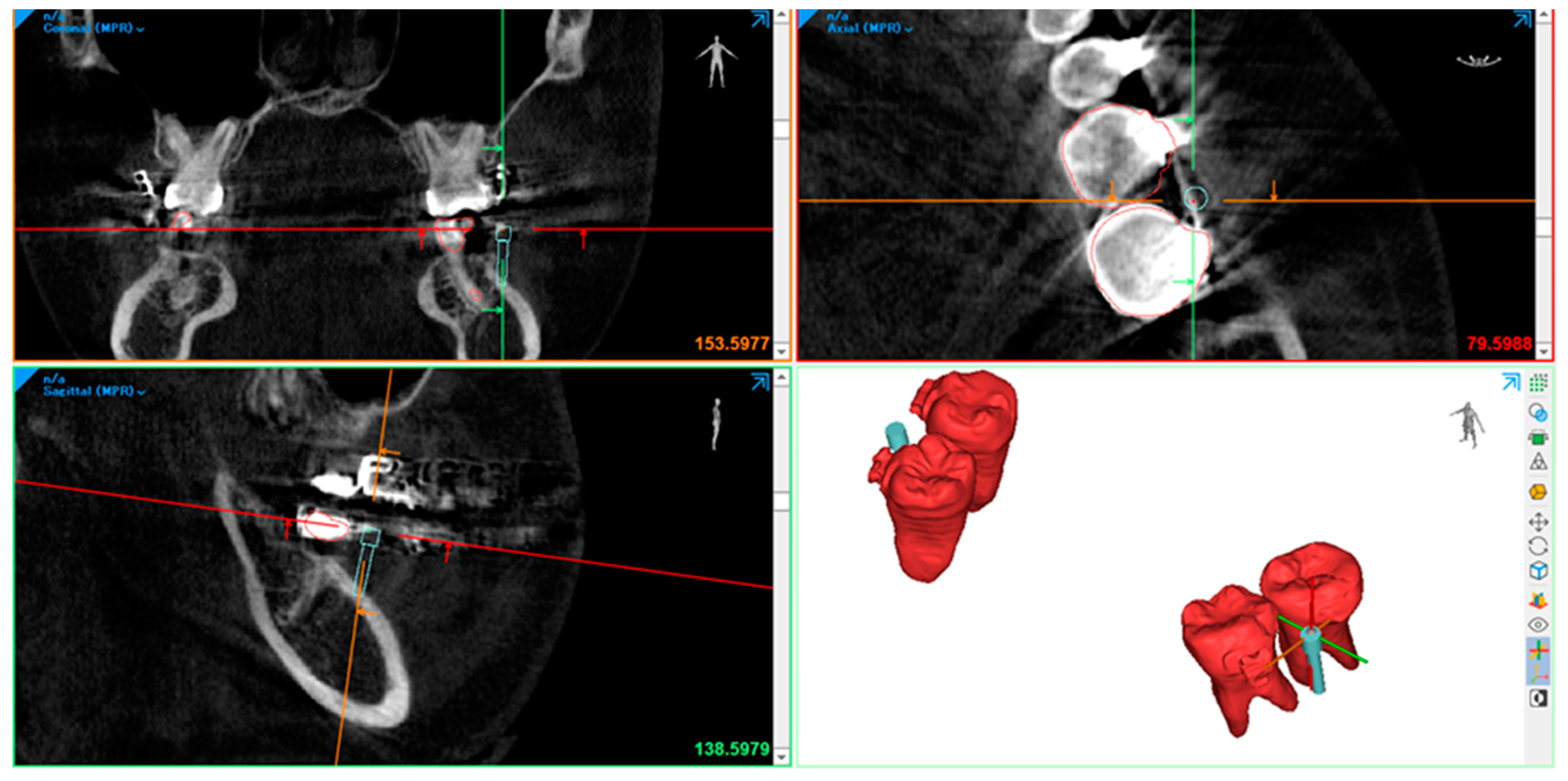
For dentition, STL and CBCT (DICOM) data are superimposed using 3-Matic SLT10.0 (Materialize, Leuven, Belgium). The 3-Matic application has been used to evaluate the three-dimensional root monitoring of root movement during orthodontic treatment [64] without exposing radiation in controlling the position of the roots.
- a.
- STL and DICOM data are superimposed using a 3-Matic application, as shown in Figure 6.
- a.
- b.
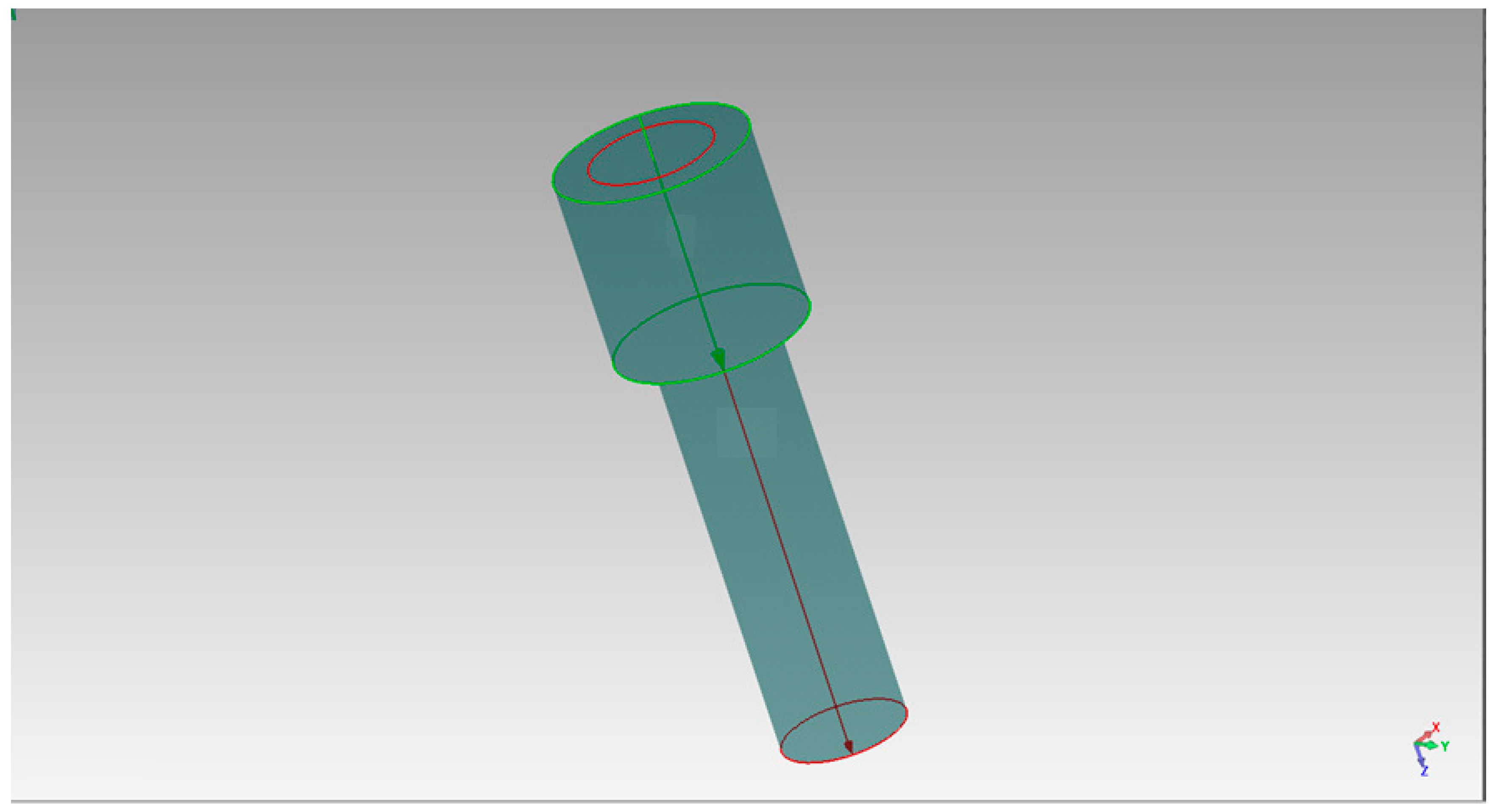
- Making three-dimensional images and analyzing them using the Geomagic Studio 5 software (Raindrop Geomagic, Inc., Morrisville, NC, USA) is necessary. We created cylinder data of the same size (φ1.6 × 8.0 mm) imitating the screw (product of TADs, brand OSAS by DEWIMED) to be placed as shown in Figure 8.
- c.
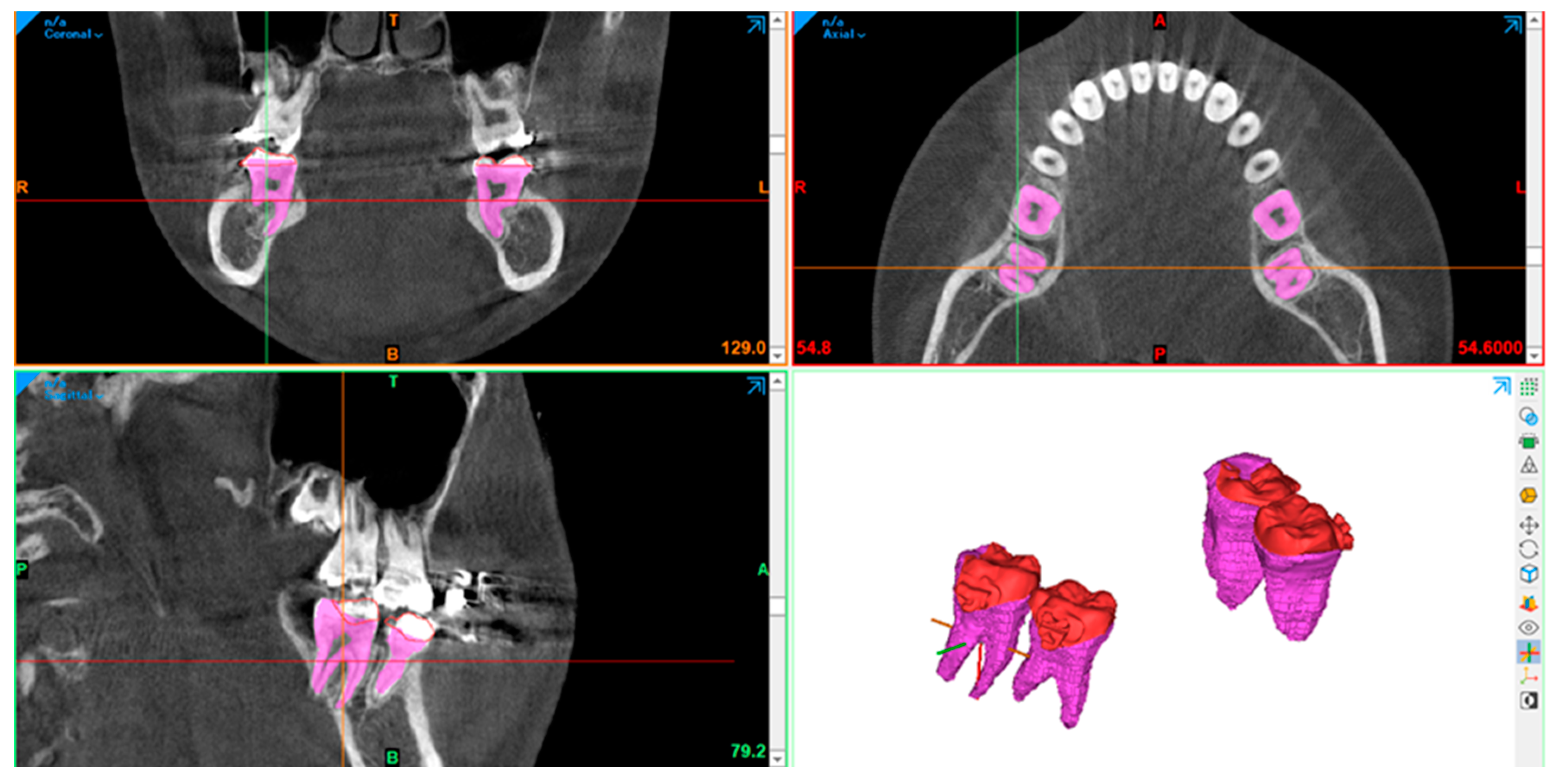
- The CBCT, intraoral scanner, and cylinder data are loaded into Mimics and a placement simulation is performed, shown in Figure 9.
- d.
-
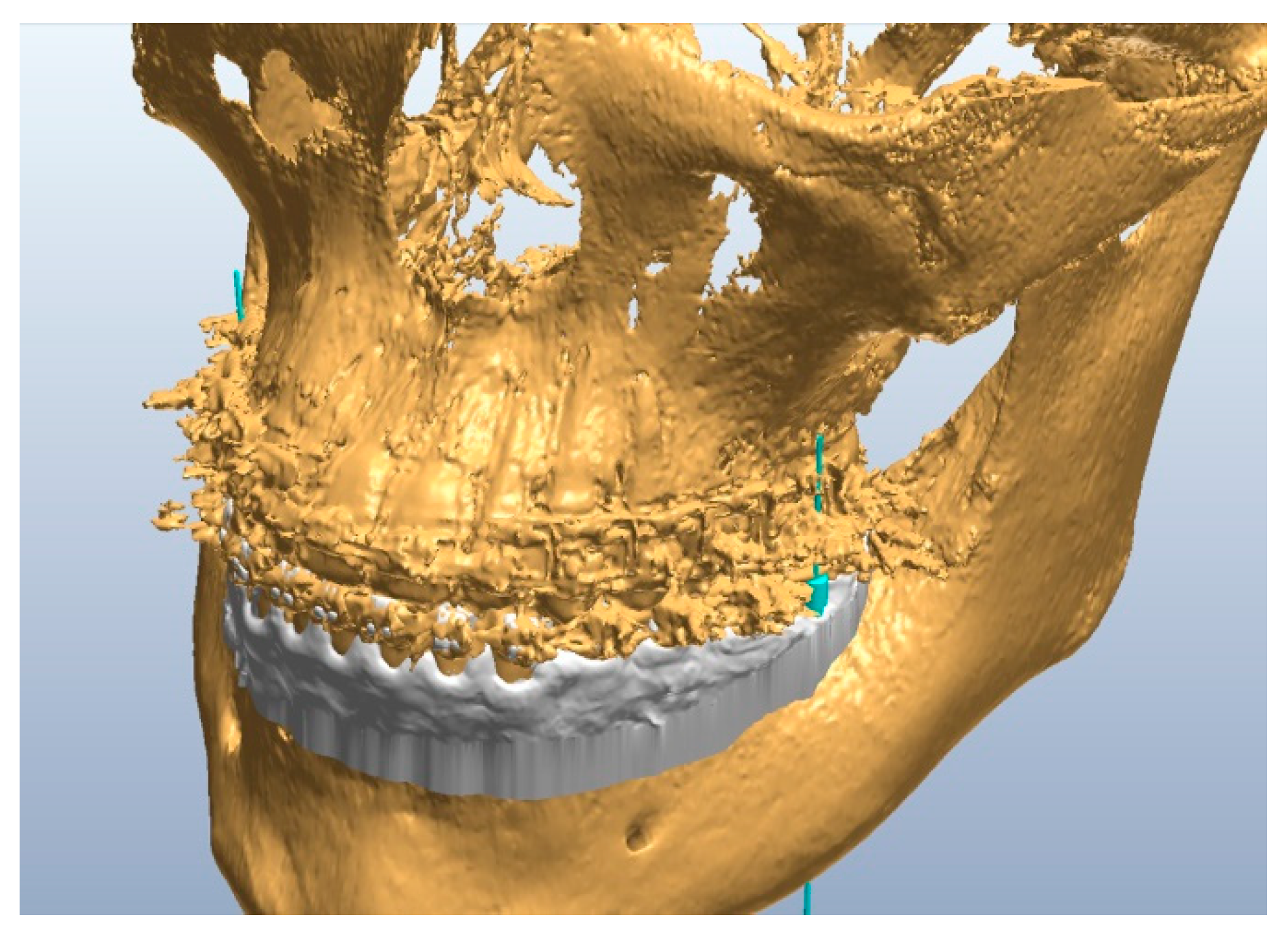
At this stage, the orthodontist performs the simulation to the best bone quality that will guarantee the success of the implantation. The process below shows the simulation performed by the doctors. The soft tissue thickness will also dictate the length of the TADs used (Figure 10).TADs are adjusted to the ideal location using the 3D simulation program, and in the final stage, the hard and soft tissue is removed, so it is easy to see only the TAD and teeth relationship (Figure 10). The lower right-side figure shows the intended situation.The plan is sent back to the laboratory, and the technician then confirms whether the simulation is visible for the 3D surgical guide printing.Figure 11 shows that, to begin with, the printing, the first step is to apply the data from 3-Shape to an easy printing program.
- a.
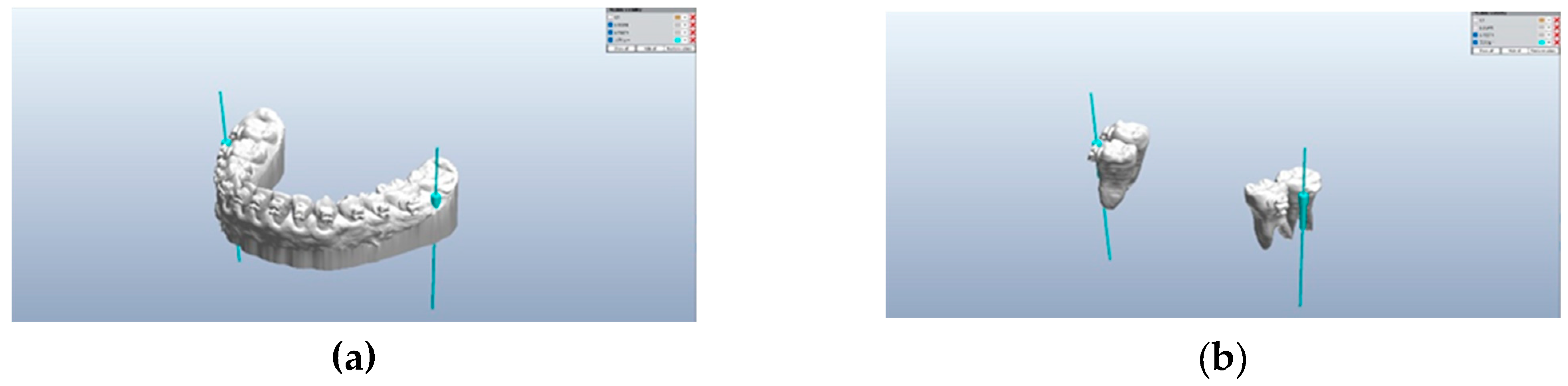
- Appliance designer of 3-Shape, Copenhagen, Denmark, was used to simulate the drill and the surgical guide to make the TAD placement position easy and straightforward, as shown below in Figure 12.
- b.
- After the screw length and position are observed, the outer guide for both the drilling screw and the screw guide constructed. The occlusal surface is used for the guide to position the surgical guide. All brackets should be avoided by making a hole to make repositioning smooth. It is also important to check the mucosa below the drilling guide, which should fit or have light pressure without sacrificing the fitness of the guide to hold the mucosa when doing the initial drilling. Figure 13a shows the drilling surgical guide, while Figure 13b shows the TADs surgical guide virtual images.
- 2.
-
Printing
- a.
-
The designed data is printed using a 3D printing machine for the pre-drill guide and TAD screw guide. The 3D printer is a SprintRay Pro95: (SprintRay, Los Angeles, CA, USA) with the material of SprintRay Sugical Guide3 (SprintRay, Los Angeles, LA, USA).
- b.
- The use of SprintRay Dashboard 2.0 software helps to monitor the printing process flow. Dashboard 2.0 is also used to communicate between designers and doctors and save the design in storage. After printing, it needs to be washed and dried as there is residue in the form of not fully cured resin. The washing and cleaning of the pre-drill guide and TAD screw guide is performed with ProWash/Dry (SprintRay, Los Angeles, CA, USA) to remove excess material and dry it (Figure 15a,b). The base and the surgical guide supports were then removed and trimmed (Figure 15c).
- c.
- d.
- The model is made from the STL to check the fitness of each guide to the model, paying attention to the area of the brackets to avoid any retention. In the bracket areas, window is made that also will benefit checking fitness during the implantation (Figure 17a,b). The surgical guide for both the pre-drilling and the screw placement guides are ready to be used at this point. The external oblique line, where the buccal shelf is, presents the most-used surgical guide: it has thick cortical bone, and, in many cases, the mucosa is an intact, attached mucosa. Even if the area is covered with flabby mucosa, the surgical guide’s bottom side presses the mucosa. It prevents the mucosa from moving during the drilling and insertion of the TAD procedure. The buccal shelf is important as it is not an interdental placement and can simultaneously do the en mass retraction of the whole lower teeth.
3. Discussions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Summary
References
- Mah, J.; Bergstrand, F. Temporary anchorage devices: A status report. J. Clin. Orthod. JCO 2005, 39, 132. [Google Scholar] [PubMed]
- Raghis, T.R.; Alsulaiman, T.M.A.; Mahmoud, G.; Youssef, M. Efficiency of maxillary total arch distalization using temporary anchorage devices (TADs) for treatment of Class II-malocclusions: A systematic review and meta-analysis. Int. Orthod. 2022, 20, 100666. [Google Scholar] [CrossRef] [PubMed]
- Bearn, D.R.; Alharbi, F. British Orthodontic Society national audit of temporary anchorage devices (TADs): Report of the first thousand TADs placed. J. Orthod. 2015, 42, 214–219. [Google Scholar] [CrossRef]
- Rooban, T.; Krishnaswamy, N.R.; Mani, K.; Kalladka, G. Root damage and repair in patients with temporary skeletal anchorage devices. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 547–555. [Google Scholar] [CrossRef]
- Güler, Ö.Ç.; Malkoç, S. Effects of orthodontic force on root surface damage caused by contact with temporary anchorage devices and on the repair process. Korean J. Orthod. 2019, 49, 106–115. [Google Scholar] [CrossRef]
- Schätzle, M.; Männchen, R.; Zwahlen, M.; Lang, N.P. Survival and failure rates of orthodontic temporary anchorage devices: A systematic review. Clin. Oral Implant. Res. 2009, 20, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-J.; Chang, H.-H.; Lin, H.-Y.; Lai, E.H.-H.; Hung, H.-C.; Yao, C.-C.J. Stability of miniplates and miniscrews used for orthodontic anchorage: Experience with 492 temporary anchorage devices. Clin. Oral Implant. Res. 2008, 19, 1188–1196. [Google Scholar] [CrossRef]
- Nienkemper, M.; Ludwig, B. Risk of root damage after using lateral cephalogram and intraoral scan for guided insertion of palatal miniscrews. Head Face Med. 2022, 18, 30. [Google Scholar] [CrossRef]
- Deglow, E.R.; Miriam, O.; Esteban, M.; Zubizarreta-Macho, Á.; Hernández Montero, S.; Tzironi, G.; Abella Sans, F.; Albaladejo Martínez, A. Novel digital technique to analyze the accuracy and intraoperative complications of orthodontic self-tapping and self-drilling microscrews placement techniques: An in vitro study. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 201–207. [Google Scholar] [CrossRef]
- Abu Arqub, S.; Gandhi, V.; Mehta, S.; Palo, L.; Upadhyay, M.; Yadav, S. Survival estimates and risk factors for failure of palatal and buccal mini-implants. Angle Orthod. 2021, 91, 756–763. [Google Scholar] [CrossRef]
- Golshah, A.; Gorji, K.; Nikkerdar, N. Effect of miniscrew insertion angle in the maxillary buccal plate on its clinical survival: A randomized clinical trial. Prog. Orthod. 2021, 2021, 22. [Google Scholar] [CrossRef] [PubMed]
- Golshah, A.; Salahshour, M.; Nikkerdar, N. Interradicular distance and alveolar bone thickness for miniscrew insertion: A CBCT study of Persian adults with different sagittal skeletal patterns. BMC Oral Health 2021, 21, 534. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Ossa, D.M.; Escobar-Correa, N.; Ramírez-Bustamante, M.A.; Agudelo-Suárez, A.A. An Umbrella Review of the Effective-ness of Temporary Anchorage Devices and the Factors That Contribute to Their Success or Failure. J. Evid. Based Dent. Pract. 2020, 20, 101402. [Google Scholar] [CrossRef] [PubMed]
- Apostolakis, D.; Kourakis, G. CAD/CAM implant surgical guides: Maximum errors in implant positioning attributable to the properties of the metal sleeve/osteotomy drill combination. Int. J. Implant. Dent. 2018, 4, 34. [Google Scholar] [CrossRef]
- Ramasamy, M.; Raja, R.; Narendrakumar, R. Implant surgical guides: From the past to the present. J. Pharm. Bioallied Sci. 2013, 5 (Suppl 1), S98. [Google Scholar] [CrossRef]
- Brief, J.; Edinger, D.; Hassfeld, S.; Eggers, G. Accuracy of image-guided implantology. Clin. Oral Implant. Res. 2005, 16, 495–501. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Singh, R.P.; Suman, R. 3D printing applications for healthcare research and development. Glob. Health J. 2022, 6, 217–226. [Google Scholar] [CrossRef]
- Jedliński, M.; Janiszewska-Olszowska, J.; Mazur, M.; Ottolenghi, L.; Grocholewicz, K.; Galluccio, G. Guided Insertion of Temporary Anchorage Device in Form of Orthodontic Titanium Miniscrews with Customized 3D Templates—A Systematic Review with Meta-Analysis of Clinical Studies. Coatings 2021, 11, 1488. [Google Scholar] [CrossRef]
- Cho, W.H. Influence of the Operator’s Experience and Drilling Sites on the Root Contact during Drilling for Micro-Implants Insertion. Master Thesis, Kyungpook University, Daegu, Republic of Korea, 2005. [Google Scholar]
- Kirnbauer, B.; Rugani, P.; Santigli, E.; Tepesch, P.; Ali, K.; Jakse, N. Fully guided placement of orthodontic miniscrews—A technical report. Australas. Orthod. J. 2019, 35, 71–74. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Laleman, I.; Jacobs, R.; Quirynen, M. Computer-supported implant planning and guided surgery: A narrative review. Clin. Oral Implant. Res. 2015, 26, 69–76. [Google Scholar] [CrossRef]
- Lai, T.-T.; Chen, M.-H. Factors affecting the clinical success of orthodontic anchorage: Experience with 266 temporary anchorage devices. J. Dent. Sci. 2014, 9, 49–55. [Google Scholar] [CrossRef]
- Hämmerle, C.H.F.; Cordaro, L.; van Assche, N.; Benic, G.I.; Bornstein, M.; Gamper, F.; Gotfredsen, K.; Harris, D.; Hürzeler, M.; Jacobs, R.; et al. Digital technologies to support planning, treatment, and fabrication processes and outcome assessments in implant dentistry. Summary and consensus statements. The 4th EAO consensus conference 2015. Clin. Oral Implant. Res. 2015, 26, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.-M.; Yamamoto, T.T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S68–S73. [Google Scholar] [CrossRef] [PubMed]
- Arısan, V.; Karabuda, C.Z.; Mumcu, E.; Özdemir, T. Implant Positioning Errors in Freehand and Computer-Aided Placement Methods: A Single-Blind Clinical Comparative Study. Int. J. Oral Maxillofac. Implant. 2013, 28, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Willmann, J.H.; Wilmes, B.; Drescher, D. Digitale Mini-Implantat getragene Suprakonstruktionen—Design und Work-flows. J. Compr. Dentof. Orthod. Orthop. 2019, 3, 16–20. [Google Scholar]
- Willmann BWilmes, D. Drescher, Clinical use of digital Workflow Exemplified by Mini Implant. Inf. Orthod. Kieferorthop. 2020, 52, 121–127. [Google Scholar]
- Graf, S.; Vasudavan, S.; Wilmes, B. CAD/CAM Metallic Printing of a Skeletally Anchored Upper Molar Distalizer. J. Clin. Orthod. 2020, 54, 140–149. [Google Scholar]
- Reynders, R.; Ronchi, L.; Bipat, S. Mini-implants in orthodontics: A systematic review of the literature. Am. J. Orthod. Dentofac. 2009, 135, 564. [Google Scholar] [CrossRef]
- Bhatia, G.; Kumar, A.; Khatri, M.; Bansal, M.; Saxena, S. Assessment of the width of attached gingiva using different methods in various age groups: A clinical study. J. Indian. Soc. Periodontol. 2015, 19, 199–202. [Google Scholar] [CrossRef]
- Kim, H.J.; Yun, H.S.; Park, H.D.; Kim, D.H.; Park, Y.C. Soft-tissue and cortical-bone thickness at orthodontic implant sites. Am J Orthod Dentofacial Orthop. 2006, 130, 177–182. [Google Scholar] [CrossRef]
- Vicioni-Marques, F.; Pimentel, D.J.B.; Matsumoto, M.A.N.; Stuani, M.B.S.; Romano, F.L. Orthodontic mini-implants: Clinical and pe-ri-implant evaluation. J. World Fed. Orthod. 2022, 11, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Ashton, K.Y.; Jiang, S.S.; Melo, M.A.; Bosio, J.A. International investigation on temporary anchorage device use: A survey of orthodontists. J. World Fed. Orthod. 2023, 12, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.-S.; Kang, M.-K.; Kim, T.-W.; Kim, K.-H.; Kim, H.-J.; Hua, M.-K.K.K.-S.; Chung, C.J.; Jung, K.-Y.; Choi, Y.J.; Aydoğdu, E.; et al. Relationships between Dental Roots and Surrounding Tissues for Orthodontic Miniscrew Installation. Angle Orthod. 2009, 79, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Tanaka, E. Risks and complications of miniscrew anchorage in clinical orthodontics. Jpn. Dent. Sci. Rev. 2014, 50, 79–85. [Google Scholar] [CrossRef]
- El Kholy, K.; Lazarin, R.; Janner, S.F.M.; Faerber, K.; Buser, R.; Buser, D. Influence of surgical guide support and implant site location on accuracy of static Computer-Assisted Implant Surgery. Clin. Oral Implant. Res. 2019, 30, 1067–1075. [Google Scholar] [CrossRef]
- Giri, M.; Sabapathy, K.; Govindasamy, B.; Rajamurugan, H. Evaluation of insertion torque and surface integrity of zirconia-coated titanium mini screw implants. J. World Fed. Orthod. 2020, 9, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Migliorati, M.; Drago, S.; Gallo, F.; Amorfini, L.; Dalessandri, D.; Calzolari, C.; Benedicenti, S.; Silvestrini-Biavati, A. Immediate versus delayed loading: Comparison of primary stability loss after miniscrew placement in orthodontic patients—A single-centre blinded randomized clinical trial. Eur. J. Orthod. 2016, 38, 652–659. [Google Scholar] [CrossRef]
- Ritchie, C.; McGregor, S.; Bearn, D.R. Temporary anchorage devices and the forces and effects on the dentition and surrounding structures during orthodontic treatment: A scoping review. Eur. J. Orthod. 2023, 45, 324–337. [Google Scholar] [CrossRef]
- Jaramillo-Bedoya, D.; Villegas-Giraldo, G.; Agudelo-Suárez, A.A.; Ramírez-Ossa, D.M. A Scoping Review about the Charac-teristics and Success-Failure Rates of Temporary Anchorage Devices in Orthodontics. Dent. J. 2022, 10, 78. [Google Scholar] [CrossRef]
- Chang, H.; Tseng, Y. Miniscrew implant applications in contemporary orthodontics. Kaohsiung J. Med. Sci. 2014, 30, 111–115. [Google Scholar] [CrossRef]
- Chugh, T.; Jain, A.K.; Jaiswal, R.K.; Mehrotra, P.; Mehrotra, R. Bone density and its importance in orthodontics. J. Oral Biol. Craniofacial Res. 2013, 3, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.-P.; Tsai, M.-T.; Yu, J.-H.; Huang, H.-L.; Hsu, J.-T. Bone quality affects stability of orthodontic miniscrews. Sci. Rep. 2022, 12, 2849. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Ludwig, B.; Vasudavan, S.; Nienkemper, M.; Drescher, D. The T-Zone: Median vs. Paramedian Insertion of Palatal Mini-Implants. J. Clin. Orthod. JCO 2016, 50, 543–551. [Google Scholar] [PubMed]
- Bjorn, L.; Bettina, G.; Jay, B.; Benedict, W.; Gero, S.M.K.; Jorg, A.L. Anatomical Guidelines for Miniscrew Insertion: Palatal Sites. J. Clin. Orthod. JCO 2011, 45, 433–441. [Google Scholar]
- Kim, T.-W.; Wu, T. Open-Bite Correction Using a Mid-Palatal TAD with an Intrusion TPA: Anteroposterior Position of TAD. Appl. Sci. 2023, 13, 5464. [Google Scholar] [CrossRef]
- Kim, J.-H.; Park, Y.-C. Evaluation of mandibular cortical bone thickness for placement of temporary anchorage devices (TADs). Korean J. Orthod. 2012, 42, 110–117. [Google Scholar] [CrossRef]
- Mendes, L.C.; Delrieu, J.; Gillet, C.; Telmon, N.; Maret, D.; Savall, F. Sexual dimorphism of the mandibular conformational changes in aging human adults: A multislice computed tomographic study by geometric morphometrics. PLOS ONE 2021, 16, e0253564. [Google Scholar] [CrossRef] [PubMed]
- Tunis, T.S.; Hershkovitz, I.; May, H.; Vardimon, A.D.; Sarig, R.; Shpack, N. Variation in Chin and Mandibular Symphysis Size and Shape in Males and Females: A CT-Based Study. Int. J. Environ. Res. Public. Health 2020, 17, 4249. [Google Scholar] [CrossRef]
- Petrey, J.S.; Saunders, M.M.; Kluemper, G.T.; Cunningham, L.L.; Beeman, C.S. Temporary anchorage device insertion variables: Effects on retention. Angle Orthod. 2010, 80, 634–641. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, J.-W.; Cho, W.-H.; Kyung, H.-M. Potential of self-drilling orthodontic microimplants under immediate loading. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 496–502. [Google Scholar] [CrossRef]
- Alkan, Ö.; Kaya, Y. The thickness of posterior buccal attached gingiva at common miniscrew insertion sites in subjects with different facial types. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.F.A.; Lin, Y. Thickness of buccal attached gingiva at miniscrew insertion sites. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 160–161. [Google Scholar] [CrossRef] [PubMed]
- Nayak, U.K.; Hegde, A.M.; Shetty, P.; Jacob, M. Temporary Anchorage Device: An Epitome of Anchorage in Orthodontic Treatment. Int. J. Clin. Pediatr. Dent. 2011, 4, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.M.; Hajeer, M.Y.; Sultan, K.; Almahdi, W.H.; Alhaffar, J.B. Evaluation of the Patient-Reported Outcome Measures (PROMs) With Temporary Skeletal Anchorage Devices in Fixed Orthodontic Treatment: A Systematic Review. Cureus 2023, 15, e36165. [Google Scholar] [CrossRef] [PubMed]
- Aly SA, Alyan D, Fayed MS, Alhammadi MS, Mostafa YA. Success rates and factors associated with failure of temporary anchorage devices: A prospective clinical trial. J Investig Clin Dent. 2018, 9, e12331. [CrossRef] [PubMed]
- Davidowitz G, Kotick PG. The use of CAD/CAM in dentistry. Dent Clin North Am. 2011, 55, 559–70. [CrossRef]
- Impellizzeri, A.; Horodynski, M.; De Stefano, A.; Palaia, G.; Polimeni, A.; Romeo, U.; Guercio-Monaco, E.; Galluccio, G. CBCT and Intra-Oral Scanner: The Advantages of 3D Technologies in Orthodontic Treatment. Int. J. Environ. Res. Public. Health 2020, 17, 9428. [Google Scholar] [CrossRef]
- Aristides, B.M. Advances in digital technology and orthodontics: A reference to the invisalign method. Med. Sci. Monit. 2005, 11, 139–142. [Google Scholar]
- Liu, H.; Liu, D.-X.; Wang, G.; Wang, C.-L.; Zhao, Z. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 728.e1–728.e10. [Google Scholar] [CrossRef]
- Bae, M.-J.; Kim, J.-Y.; Park, J.-T.; Cha, J.-Y.; Kim, H.-J.; Yu, H.-S.; Hwang, C.-J. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 893–901. [Google Scholar] [CrossRef]
- Giudice, A.L.; Rustico, L.; Longo, M.; Oteri, G.; Papadopoulos, M.A.; Nucera, R. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J. Orthod. 2021, 51, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Prescher, A.; Hölzle, F.; Modabber, A.; Wolf, M.; Peters, F. Accuracy of orthodontic mini-implants placed at the anterior palate by tooth-borne or gingiva-borne guide support: A cadaveric study. Clin. Oral Investig. 2019, 23, 4425–4431. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.J.; Weissheimer, A.; Pham, J.; Go, L.; de Menezes, L.M.; Redmond, W.R.; Loos, J.F.; Sameshima, G.T.; Tong, H. Three-dimensional monitoring of root movement during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Altieri, F.; Di Giorgio, R.; Barbato, E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: Description of a technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef]
- Cassetta, M.; Giansanti, M. Accelerating orthodontic tooth movement: A new, minimally-invasive corticotomy technique using a 3D-printed surgical template. 2016, 21, e483. [Google Scholar] [CrossRef]
- Thomas M, Akula U, Ealla KK, Gajjada N. Piezosurgery: A Boon for Modern Periodontics. J Int Soc Prev Community Dent. 2017, 7, 1–7. [CrossRef]
- Jarab, F.; Omar, E.; Bhayat, A.; Mansuri, S.; Ahmed, S. Duration of hospital stay following orthognathic surgery at the jordan university hospital. J Maxillofac Oral Surg. 2012, 11, 314–8. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; et al. Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter. J Mech Behav Biomed Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef]
- Radwan, E.S.; Montasser, M.A.; Maher, A. Influence of geometric design characteristics on primary stability of orthodontic miniscrews. J Orofac Orthop. 2018, 79, 191–203. [Google Scholar] [CrossRef]
- Montasser, M.A.; Scribante, A. Root Injury During Interradicular Insertion is the most Common Complication Asso-ciated with Orthodontic Miniscrews. J Evid Based Dent Pract. 2022, 22, 101688. [Google Scholar] [CrossRef]
- Gelpi, F.; Modena, N.; Poscolere, A.; Bernardello, F.; Torroni, L.; De Santis, D. Accuracy of Computer-Guided Implantology with Pilot Drill Surgical Guide: Retrospective 3D Radiologic Investigation in Partially Edentulous Patients. Medicina 2023, 59, 738. [Google Scholar] [CrossRef] [PubMed]



| Advantages | Disadvantages | |
|---|---|---|
| Fee | More cost (laboratory): “300-600$.” | |
| Accuracy | Reliable and constant | |
| Time | Short appointment time in placement and direct appliance setting |
Scanning and construction time |
| Prospect | Yes, a complex case is possible, paralleling 2 TADs and predetermined angulation feasible |
|
| X-ray radiation |
High doses of CBCT |
| 1. | Superimposed SLT and DICOM data |
| 2. | Designing a surgical guide in 3Shape Ortho System 2021.1 |
| 3. | 3D printing. |
| 4. | Cleaning, washing, and cutting |
| 5. | Checking and testing the surgical guides to the models |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





