Submitted:
24 September 2023
Posted:
28 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Emergency medical services (EMS)
Study design
Statistical analysis
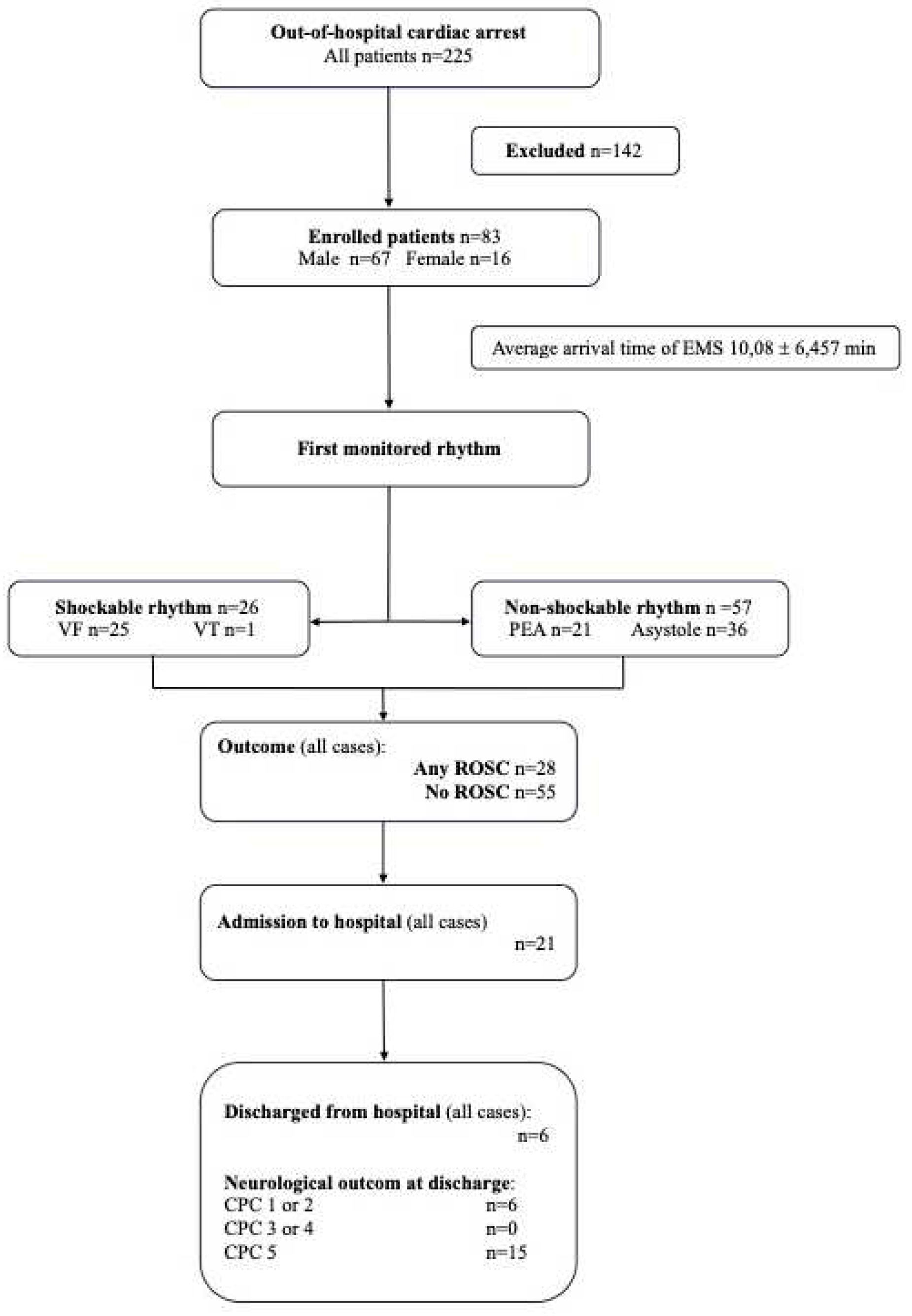
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Lurie, K.G.; Nemergut, E.C.; Yannopoulos, D.; Sweeney, M. The Physiology of Cardiopulmonary Resuscitation. Obstet. Anesthesia Dig. 2016, 122, 767–783. [Google Scholar] [CrossRef] [PubMed]
- Porzer M, Mrazkova E, Homza M, Janout V. Out-of-hospital cardiac arrest. 2017, 161, 348–353.
- Patil, K.D.; Halperin, H.R.; Becker, L.B.; J, C.; M, S.; T, Y.; G, N.; K, S.; J, S.; L, B.; et al. Cardiac Arrest. Circ. Res. 2015, 116, 2041–2049. [Google Scholar] [CrossRef]
- Varvarousis, D.; Varvarousi, G.; Iacovidou, N.; D'Aloja, E.; Gulati, A.; Xanthos, T. The pathophysiologies of asphyxial vs dysrhythmic cardiac arrest: implications for resuscitation and post-event management. Am. J. Emerg. Med. 2015, 33, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-S.; Huang, C.-H.; Tsai, S.-H.; Tsai, C.-Y.; Chen, H.-W.; Cheng, H.-J.; Hsu, C.-Y.; Wang, T.-D.; Chang, W.-T.; Chen, W.-J. The difference in myocardial injuries and mitochondrial damages between asphyxial and ventricular fibrillation cardiac arrests. Am. J. Emerg. Med. 2012, 30, 1540–1548. [Google Scholar] [CrossRef]
- Phypers, B.; Pierce, J.T. Lactate physiology in health and disease. Contin. Educ. Anaesth. Crit. Care Pain 2006, 6, 128–132. [Google Scholar] [CrossRef]
- Hunter, C.L.; Silvestri, S.; Dean, M.; Falk, J.L.; Papa, L. End-tidal carbon dioxide is associated with mortality and lactate in patients with suspected sepsis. Am. J. Emerg. Med. 2013, 31, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Caputo ND, Fraser RM, Paliga A, et al. Nasal cannula end-tidal CO2 correlates with serum lactate levels and odds of operative intervention in penetrating trauma patients: a prospective cohort study. J Trauma Acute Care Surg 2012, 73, 1202–1207. [CrossRef] [PubMed]
- McGillicuddy DC, Tang A, Caaldo L, et al. Evaluation of end-tidal carbon dioxide role in predicting elevated SOFA scores and lactic acidosis. Intern Emerg Med 2009, 4, 41–45. [CrossRef] [PubMed]
- Lah, K.; Vujanovic, V.; Krizmaric, M.; Grmec, S. Difference in end-tidal carbon dioxide between asphyxial cardiac arrest and ventricular fibrillation/pulseless ventricular tachycardia cardiac arrest in cardiopulmonary resuscitation—Comparison of 2000 and 2005 CPR guidelines. Resuscitation 2010, 81, S58–S58. [Google Scholar] [CrossRef]
- Grmec. ; Lah, K.; Tušek-Bunc, K. Difference in end-tidal CO2 between asphyxia cardiac arrest and ventricular fibrillation/pulseless ventricular tachycardia cardiac arrest in the prehospital setting. Crit. Care 2003, 7, R139–R144. [Google Scholar] [CrossRef]
- Hunter, C.L.; Silvestri, S.; Ralls, G.; Bright, S.; Papa, L. The sixth vital sign: prehospital end-tidal carbon dioxide predicts in-hospital mortality and metabolic disturbances. Am. J. Emerg. Med. 2014, 32, 160–165. [Google Scholar] [CrossRef]
- Wang, C.-H.; Huang, C.-H.; Chang, W.-T.; Tsai, M.-S.; Yu, P.-H.; Wu, Y.-W.; Hung, K.-Y.; Chen, W.-J. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit. Care 2015, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cocchi, M.N.; Miller, J.; Hunziker, S.; Carney, E.; Salciccioli, J.; Farris, S.; Joyce, N.; Zimetbaum, P.; Howell, M.D.; Donnino, M.W. The association of lactate and vasopressor need for mortality prediction in survivors of cardiac arrest. . 2011, 77. [Google Scholar]
- Starodub, R.; Abella, B.S.; Grossestreuer, A.V.; Shofer, F.S.; Perman, S.M.; Leary, M.; Gaieski, D.F. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation 2013, 84, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Momiyama, Y.; Yamada, W.; Miyata, K.; Miura, K.; Fukuda, T.; Fuse, J.; Kikuno, T. Prognostic values of blood pH and lactate levels in patients resuscitated from out-of-hospital cardiac arrest. Acute Med. Surg. 2016, 4, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Gernardin, G.; Pradier, C.; Tiger, F.; Deloffre, P.; Mattei, M. Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensiv. Care Med. 1996, 22, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Ralston, S.H.; Voorhees, W.D.; Showen, L.; Schmitz, P.; Kougias, C.; Tacker, W.A. Venous and arterial blood gases during and after cardiopulmonary resuscitation in dogs. Am. J. Emerg. Med. 1985, 3, 132–136. [Google Scholar] [CrossRef]
- Carden, D.L.; Martin, G.B.; Nowak, R.M.; Foreback, C.C.; Tomlanovich, M.C. Lactic acidosis during closed-chest CPR in dogs. Ann. Emerg. Med. 1987, 16, 1317–1320. [Google Scholar] [CrossRef]
- Weil, M.H.; Ruiz, C.E.; Michaels, S.B.; Rackow, E.C. Acid-base determinants of survival after cardiopulmonary resuscitation. Crit. Care Med. 1985, 13, 888–892. [Google Scholar] [CrossRef]
- Stewart JSS, Glasg MB,. Stewart WK, Gillies HG. Cardiac arrest and acidosis. The Lancet 1962, 280, 964–967.
- Starodub, R.; Abella, B.S.; Grossestreuer, A.V.; Shofer, F.S.; Perman, S.M.; Leary, M.; Gaieski, D.F. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation 2013, 84, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Donnino, M.W.; Miller, J.; Goyal, N.; Loomba, M.; Sankey, S.S.; Dolcourt, B.; Sherwin, R.; Otero, R.; Wira, C. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation 2007, 75, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Oddo M, Ribordy V, Feihl F, Rossetti AO, Schaller MD, et al. Early predictors of outcome in comatose survivors of ventricular fibrillation and non-ventricular fibrillation cardiac arrest treated with hypothermia: a prospective study. Crit Care Med. 2008, 36, 2296–2301. [Google Scholar]
- Adrie C, Cariou A, Mourvillier B, Laurent I, Dabbane H, et al. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J. 2006, 27, 2840–2845. [Google Scholar] [CrossRef]
- Kliegel, A.; Losert, H.; Sterz, F.; Holzer, M.; Zeiner, A.; Havel, C.; Laggner, A.N. Serial Lactate Determinations for Prediction of Outcome After Cardiac Arrest. Medicine 2004, 83, 274–279. [Google Scholar] [CrossRef]
- Seeger, F.H.; Toenne, M.; Lehmann, R.; Ehrlich, J.R. Simplistic approach to prognosis after cardiopulmonary resuscitation—value of pH and lactate. J. Crit. Care 2013, 28, 317–e13. [Google Scholar] [CrossRef]
- Kaji, A.H.; Hanif, A.M.; Bosson, N.; Ostermayer, D.; Niemann, J.T. Predictors of Neurologic Outcome in Patients Resuscitated from Out-of-Hospital Cardiac Arrest Using Classification and Regression Tree Analysis. Am. J. Cardiol. 2014, 114, 1024–1028. [Google Scholar] [CrossRef]
- Lee, T.R.; Kang, M.J.; Cha, W.C.; Shin, T.G.; Sim, M.S.; Jo, I.J.; Song, K.J.; Jeong, Y.K.; Cho, J.H. Better lactate clearance associated with good neurologic outcome in survivors who treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Crit. Care 2013, 17, R260–R260. [Google Scholar] [CrossRef]
- Wu, C.-J.; Li, C.-S.; Zhang, Y.; Yang, J.; Yin, Q.; Hang, C.-C. Differences of postresuscitation myocardial dysfunction in ventricular fibrillation versus asphyxiation. Am. J. Emerg. Med. 2013, 31, 1690–1696. [Google Scholar] [CrossRef]
- albay A, Çakir Z, Bayramoğlu A. Prognostic value of blood gas parameters and end-tidal carbon dioxide values in out-of-hospital cardiopulmonary arrest patients. Turkish J Med Sci. 2019, 49, 1298–1302. [Google Scholar] [CrossRef] [PubMed]
- Paiva EF, Paxton JH, O’Neil BJ. The use of end-tidal carbon dioxide (ETCO2) measurment to guide management of cardiac arrest: A systematic review. Resuscitation 2018, 123, 1–7. [Google Scholar]
- Asplin, B.R.; White, R.D. Prognostic Value Of End-Tidal Carbon Dioxide Pressures During Out-Of-Hospital Cardiac Arrest. Ann. Emerg. Med. 1995, 25, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Grmec S, Klemen P. Does the end-tidal carbon dioxide (EtCO2) concentration have prognostic value during out-of-hospital cardiac arrest? Eur J Emerg Med 2001, 8, 263–269. [Google Scholar]
- Corral Torres E, Hernández-Tejedor A, Suárez Bustamante R, de Elías Hernández R, Casado Flórez I, San Juan Linares A. Prognostic value of venous blood analysis at the start of CPR in non-traumatic out-of-hospital cardiac arrest: association with ROSC and the neurological outcome. Crit Care. 2020, 24, 60. [Google Scholar]
- Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation 2008, 79, 350–379. [Google Scholar]
- Allen, S.E. and Holm, J.L.Lactate: physiology and clinical utility. Journal of Veterinary Emergency and Critical Care 2008, 18, 123–132. [Google Scholar]
- Mohindra, RohitPatel, MatthewLin, Steve et al. A new paradigm of resuscitation: Perfusion-guided cardiopulmonary resuscitation.
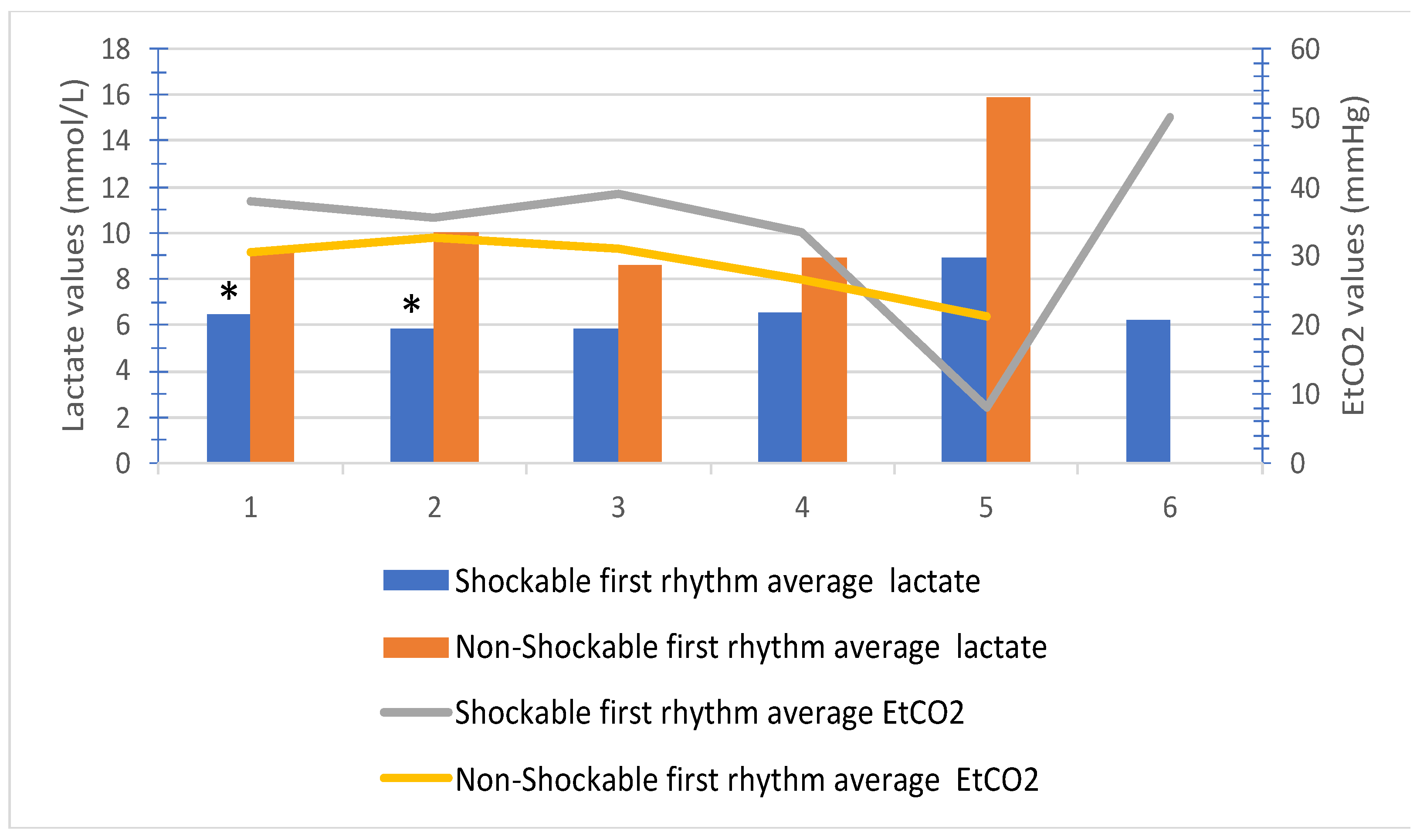
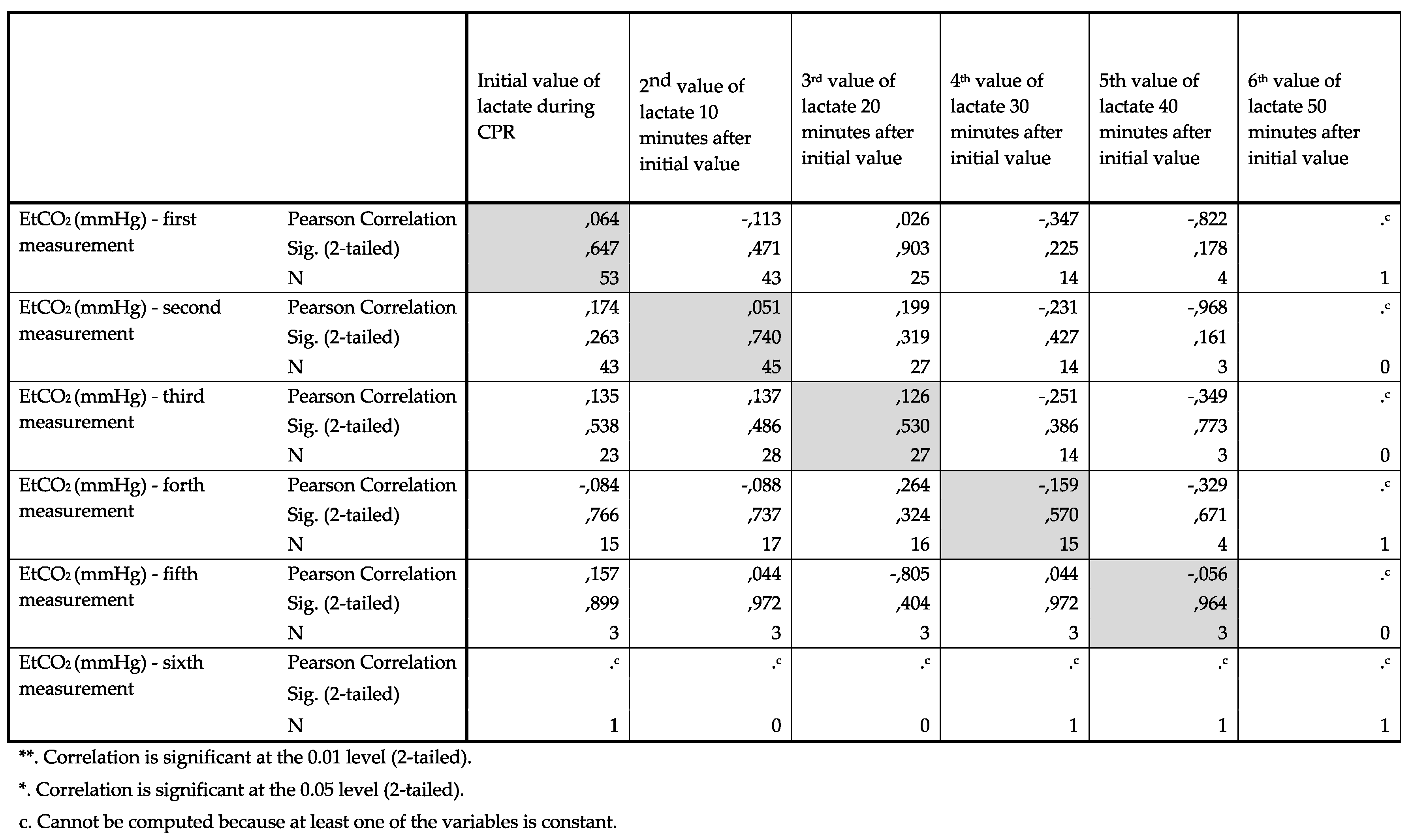
| Patients | N | Mean | Std. Deviation | p | |
| Initial value of lactate | Patients with first monitored shockable rhythm |
16 | 6,43 | 3,81 | 0,037 |
| Patients with first monitored non-shockable rhythm |
43 | 9,19 | 4,61 | ||
| Serial value of lactate after 10 minutes | Patients with first monitored shockable rhythm |
10 | 5,81 | 3,47 | 0,019 |
| Patients with first monitored non-shockable rhythm |
38 | 10,03 | 5,19 | ||
| Serial value of lactate after 20 minutes | Patients with first monitored shockable rhythm |
9 | 5,83 | 2,47 | 0,075 |
| Patients with first monitored non-shockable rhythm |
21 | 8,61 | 5,73 | ||
| Serial value of lactate after 30 minutes | Patients with first monitored shockable rhythm |
6 | 6,52 | 3,27 | 0,329 |
| Patients with first monitored non-shockable rhythm |
12 | 8,95 | 5,40 | ||
| Serial value of lactate after 40 minutes | Patients with first monitored shockable rhythm |
2 | 8,90 | 1,13 | 0,259 |
| Patients with first monitored non-shockable rhythm |
3 | 15,90 | 6,71 | ||
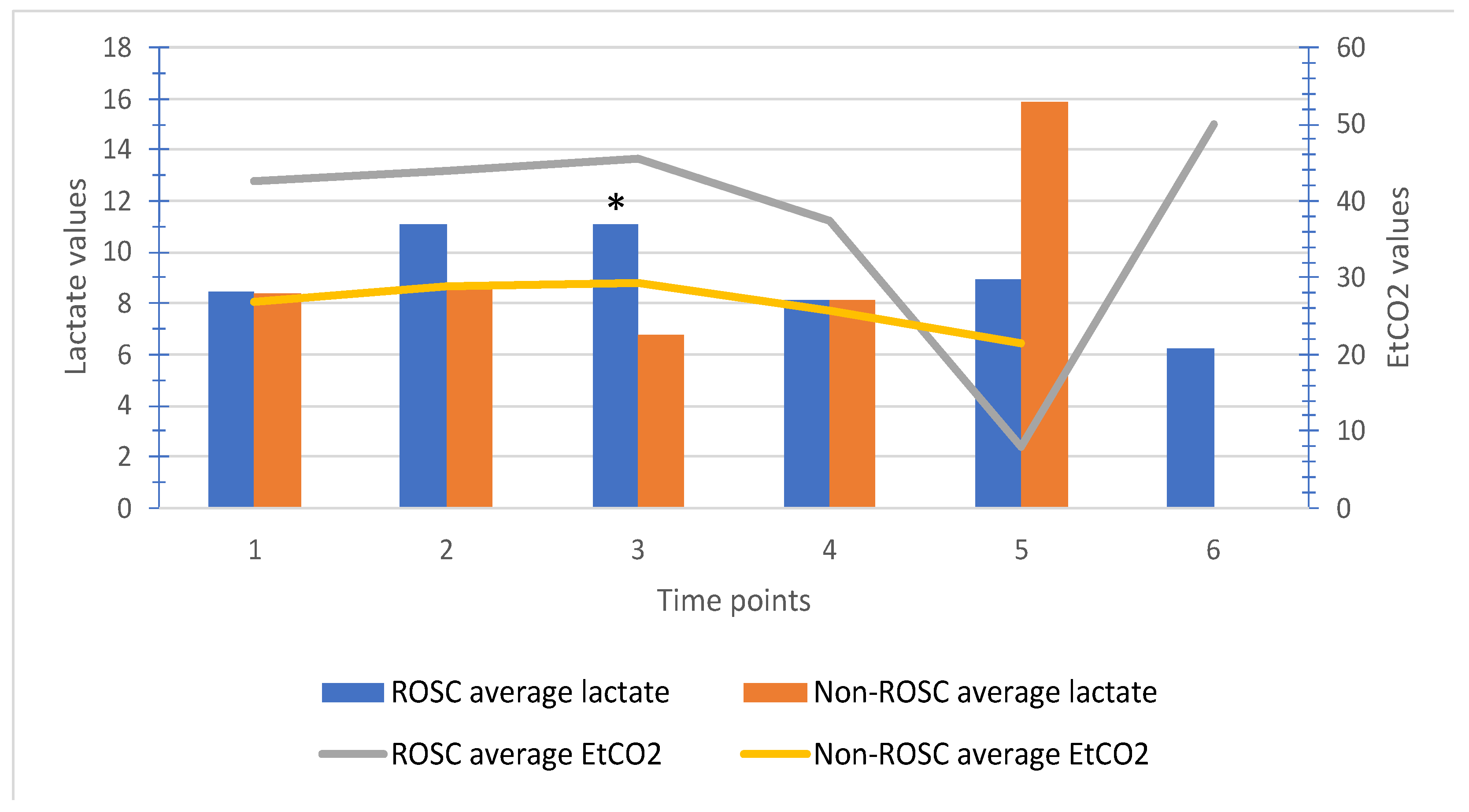
| ROSC | N | Mean | Std. Deviation | p | |
|---|---|---|---|---|---|
| Initial value of lactate during CPR | Yes | 21 | 8,48 | 4,86 | 0,959 |
| No | 38 | 8,42 | 4,43 | ||
| 2nd value of lactate after 10 min | Yes | 11 | 11,09 | 5,17 | 0,156 |
| No | 37 | 8,57 | 5,06 | ||
| 3rd value of lactate after 20 min | Yes | 7 | 11,10 | 6,59 | 0,047 |
| No | 23 | 6,77 | 4,23 | ||
| 4th value of lactate after 30 min | Yes | 3 | 8,13 | 0,95 | 0,998 |
| No | 15 | 8,14 | 5,32 | ||
| 5th value of lactate after 40 min | Yes | 2 | 8,90 | 1,13 | 0,259 |
| No | 3 | 15,90 | 6,71 | ||
| 6th value of lactate after 50 min | Yes | 1 | 6,20 | ||
| No | 0a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





