Submitted:
26 September 2023
Posted:
27 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
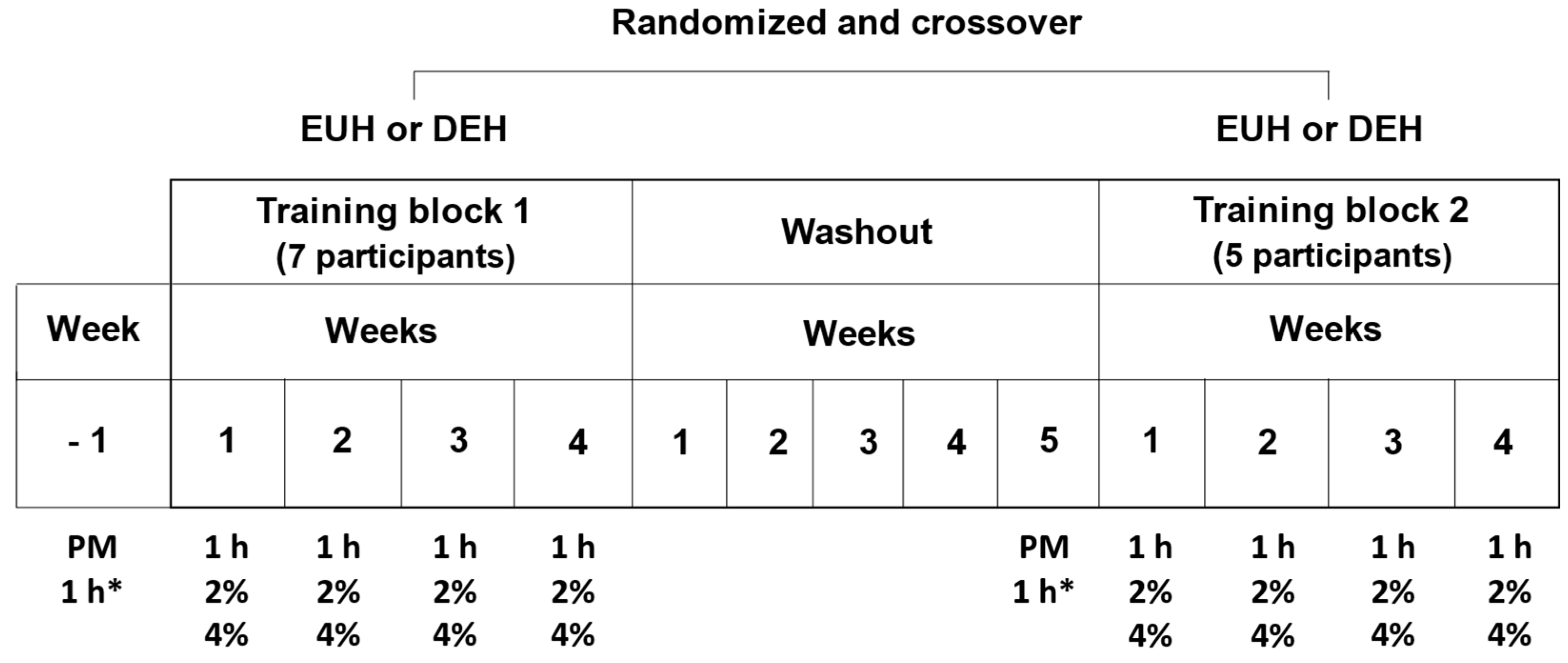
2. Materials and Methods
2.1. Participants
2.2. Context of the study
2.3. Preliminary measurements
2.4. Pre-exercise protocol
2.6. Measurements
2.7. Statistical analyses
3. Results
3.1. Pre-exercise hydration and ambient temperature and relative humidity
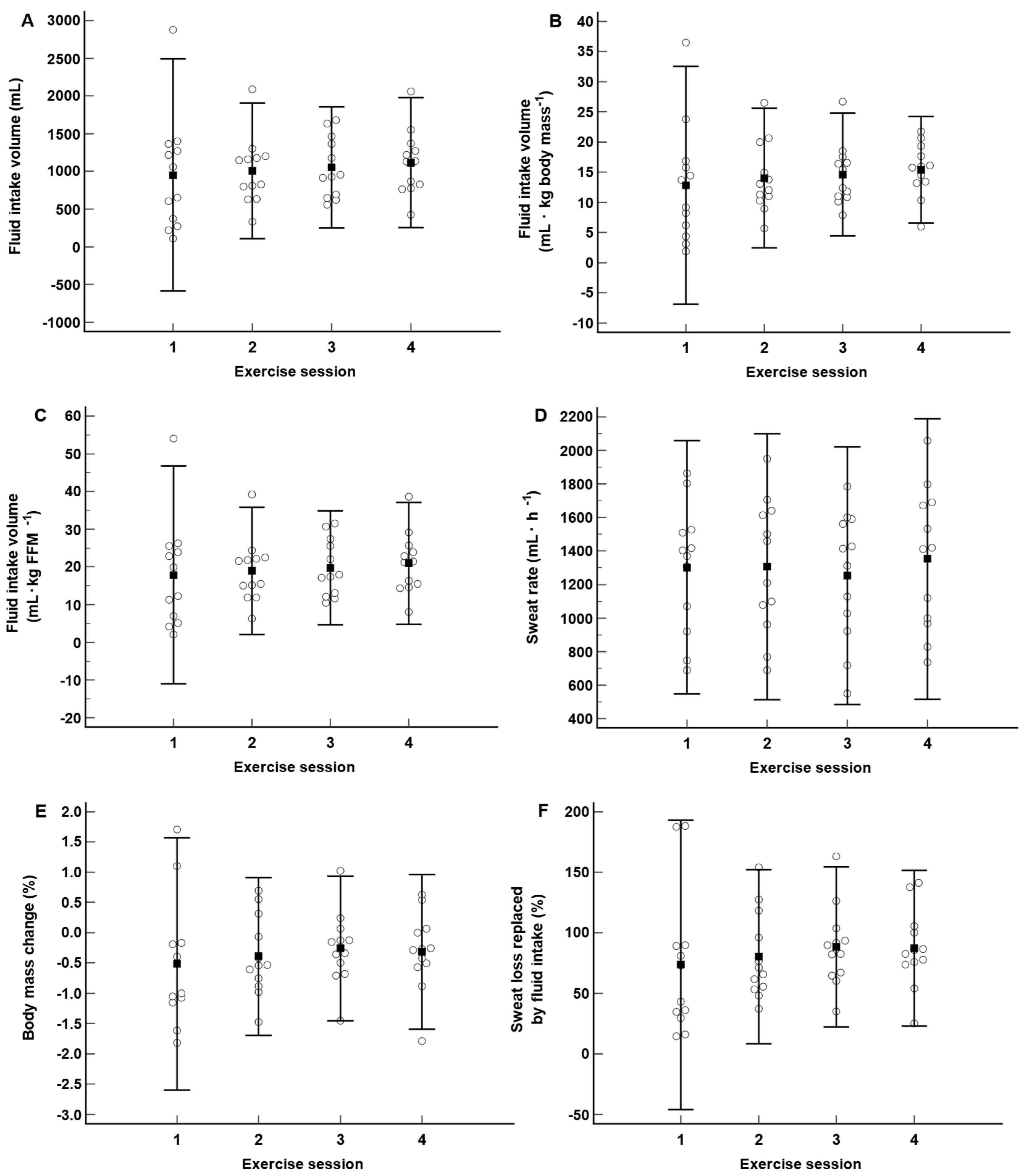
3.2. Fluid balance
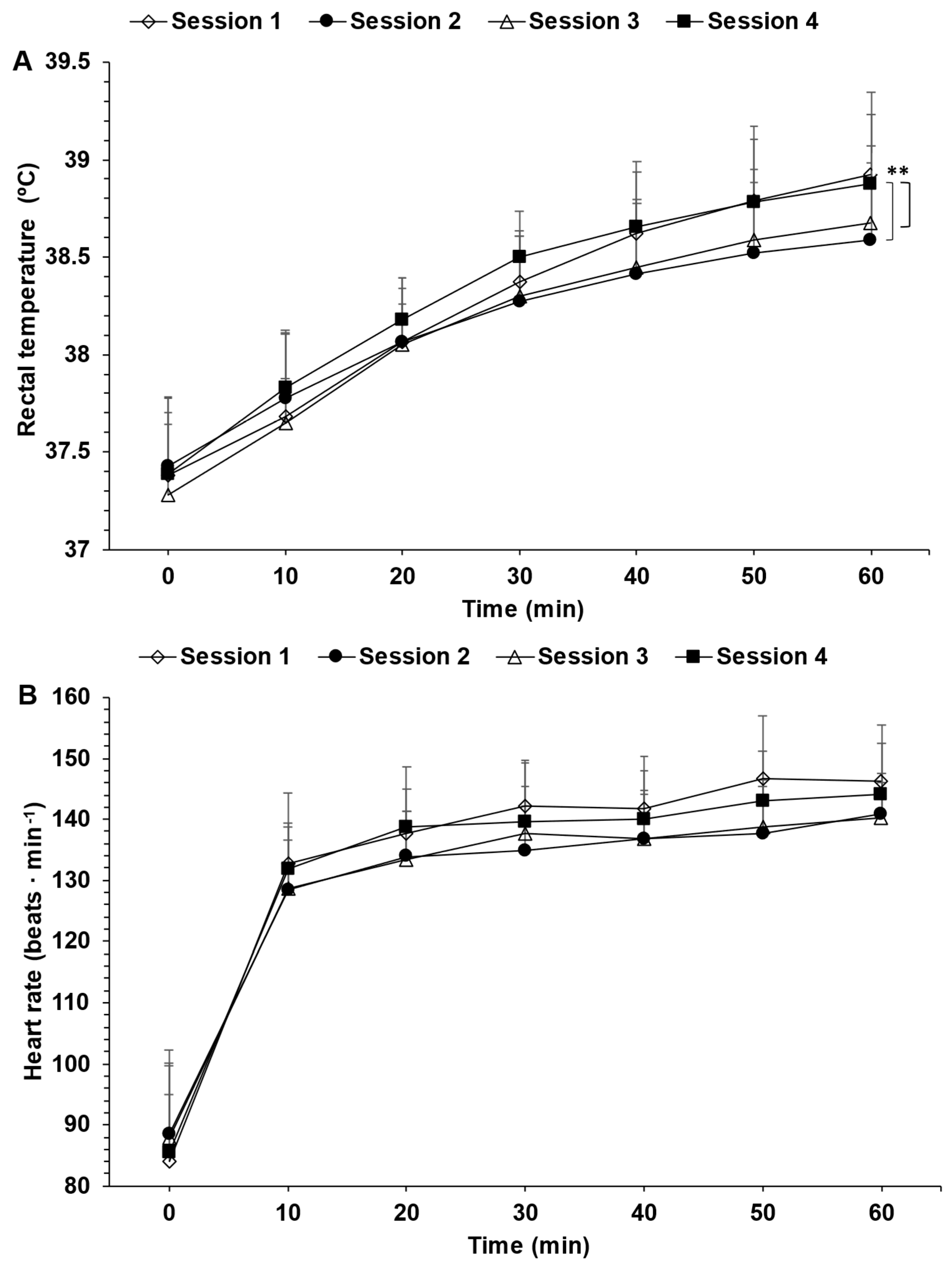
3.3. Rectal temperature and heart rate
3.4. Perceived thirst, exertion and heat stress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
References
- Cramer, M.N.; Gagnon, D.; Laitano, O.; Crandall, C.G. Human temperature regulation under heat stress in health, disease, and injury. Physiol Rev 2022, 102, 1907–1989. [Google Scholar] [CrossRef] [PubMed]
- Cheuvront, S.N.; Carter Iii, R.; Sawka, M.N. Fluid Balance and Endurance Exercise Performance. Current Sports Medicine Reports (Lippincott Williams & Wilkins) 2003, 2, 202–208. [Google Scholar]
- Cheuvront, S.N.; Kenefick, R.W. Dehydration: physiology, assessment, and performance effects. Compr Physiol 2014, 4, 257–285. [Google Scholar] [PubMed]
- James, L.J.; Funnell, M.P.; James, R.M.; Mears, S.A. Does Hypohydration Really Impair Endurance Performance? Methodological Considerations for Interpreting Hydration Research. Sports Med 2019, 49, 103–114. [Google Scholar] [CrossRef] [PubMed]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.E.; Casa, D.J.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O. National Athletic Trainers’ Association Position Statement: Fluid Replacement for the Physically Active. J Athl Train 2017, 52, 877–895. [Google Scholar] [CrossRef] [PubMed]
- Garth, A.K.; Burke, L.M. What do athletes drink during competitive sporting activities? Sports Med 2013, 43, 539–564. [Google Scholar] [CrossRef]
- Goulet, E.D.B.; Hoffman, M.D. Impact of Ad Libitum Versus Programmed Drinking on Endurance Performance: A Systematic Review with Meta-Analysis. Sports Med 2019, 49, 221–232. [Google Scholar] [CrossRef]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 2007, 39, 377–390. [Google Scholar]
- Baker, L.B. Sweating rate and sweat sodium concentration in athletes: a review of methodology and intra/interindividual variability. Sports Med 2017, 47, 111–128. [Google Scholar] [CrossRef]
- Claveau, P.; Deshayes, T.A.; Jeker, D.; Pancrate, T.; Goulet, E.D.B. Provision of instructions to drink ad libitum or according to thirst sensation: impact during 120 km of cycling in the heat in men. Appl Physiol Nutr Metab 2021, 1–8. [Google Scholar]
- Kenefick, R.W. Drinking Strategies: Planned Drinking Versus Drinking to Thirst. Sports Med 2018, 48, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Maresh, C.M.; Gabaree-Boulant, C.L.; Armstrong, L.E.; Judelson, D.A.; Hoffman, J.R.; Castellani, J.W.; Kenefick, R.W.; Bergeron, M.F.; Casa, D.J. Effect of hydration status on thirst, drinking, and related hormonal responses during low-intensity exercise in the heat. J Appl Physiol (1985) 2004, 97, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Gizowski, C.; Bourque, C.W. The neural basis of homeostatic and anticipatory thirst. Nat Rev Nephrol 2018, 14, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Freemas, J.A.; Goss, C.S.; Ables, R.; Baker, T.B.; Bruinvels, G.; Mündel, T.; Martin, B.J.; Carter, S.J.; Chapman, R.F.; Schlader, Z.J. Fluid balance during physical work in the heat is not modified by the menstrual cycle when fluids are freely available. J Appl Physiol (1985) 2023, 134, 1376–1389. [Google Scholar] [CrossRef]
- Sekiguchi, Y.; Benjamin, C.L.; Dion, S.O.; Manning, C.N.; Struder, J.F.; Dierickx, E.E.; Morrissey, M.C.; Filep, E.M.; Casa, D.J. Changes in Hydration Factors Over the Course of Heat Acclimation in Endurance Athletes. Int J Sport Nutr Exerc Metab 2021, 31, 406–411. [Google Scholar] [CrossRef]
- Wilk, B.; Kriemler, S.; Keller, H.; Bar-Or, O. Consistency in preventing voluntary dehydration in boys who drink a flavored carbohydrate-NaCl beverage during exercise in the heat. Int J Sport Nutr 1998, 8, 1–9. [Google Scholar] [CrossRef]
- Greenleaf, J.E.; Brock, P.J.; Keil, L.C.; Morse, J.T. Drinking and water balance during exercise and heat acclimation. J Appl Physiol Respir Environ Exerc Physiol 1983, 54, 414–419. [Google Scholar] [CrossRef]
- Deshayes, T.A.; Daigle, N.; Jeker, D.; Lamontagne-Lacasse, M.; Perreault-Briere, M.; Claveau, P.; Simoneau, I.L.; Chamoux, E.; Goulet, E.D.B. Impact of Repeated Acute Exposures to Low and Moderate Exercise-Induced Hypohydration on Physiological and Subjective Responses and Endurance Performance. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Deshayes, T.A.; Daigle, N.; Jeker, D.; Lamontagne-Lacasse, M.; Perreault-Briere, M.; Claveau, P.; Simoneau, I.L.; Chamoux, E.; Goulet, E.D.B. Cognitive Performance Before and Following Habituation to Exercise-Induced Hypohydration of 2 and 4% Body Mass in Physically Active Individuals. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- American College of Sports, M.; Thompson, W.R. ACSM’s guidelines for exercise testing and prescription, 8th ed.; Lippincott Williams & Wilkins Philadelphia: Philadelphia, 2009. [Google Scholar]
- Gosselin, J.; Beliveau, J.; Hamel, M.; Casa, D.; Hosokawa, Y.; Morais, J.A.; Goulet, E.D.B. Wireless measurement of rectal temperature during exercise: Comparing an ingestible thermometric telemetric pill used as a suppository against a conventional rectal probe. J Therm Biol 2019, 83, 112–118. [Google Scholar] [CrossRef]
- Pancrate, T.; Gosselin, J.; Deshayes, T.A.; Goulet, E.D.B. Validity and Reliability of the CorTemp(TM) Telemetric Pill during 50 h of Reuse in a Circulating Water Bath. J Therm Biol 2020, 93, 102737. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Dion, T.; Savoie, F.A.; Asselin, A.; Gariepy, C.; Goulet, E.D. Half-marathon running performance is not improved by a rate of fluid intake above that dictated by thirst sensation in trained distance runners. Eur J Appl Physiol 2013, 113, 3011–3020. [Google Scholar] [CrossRef] [PubMed]
- Jeker, D.; Claveau, P.; Abed, M.E.F.; Deshayes, T.A.; Lajoie, C.; Gendron, P.; Hoffman, M.D.; Goulet, E.D.B. Programmed vs. Thirst-Driven Drinking during Prolonged Cycling in a Warm Environment. Nutrients 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Schielzeth, H.; Dingemanse, N.J.; Nakagawa, S.; Westneat, D.F.; Allegue, H.; Teplitsky, C.; Réale, D.; Dochtermann, N.A.; Garamszegi, L.Z.; Araya-Ajoy, Y.G. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods in Ecology and Evolution 2020, 11, 1141–1152. [Google Scholar] [CrossRef]
- Bakdash, J.Z.; Marusich, L.R. Repeated Measures Correlation. Front Psychol 2017, 8, 456. [Google Scholar] [CrossRef]
- Hyslop, N.P.; White, W.H. Estimating precision using duplicate measurements. J Air Waste Manag Assoc 2009, 59, 1032–1039. [Google Scholar] [CrossRef]
- Perreault-Briere, M.; Beliveau, J.; Jeker, D.; Deshayes, T.A.; Duran, A.; Goulet, E.D.B. Effect of Thirst-Driven Fluid Intake on 1 H Cycling Time-Trial Performance in Trained Endurance Athletes. Sports (Basel) 2019, 7. [Google Scholar] [CrossRef]
- Périard, J.D.; Racinais, S.; Sawka, M.N. Adaptations and mechanisms of human heat acclimation: Applications for competitive athletes and sports. Scand J Med Sci Sports 2015, 25 (Suppl. 1), 20–38. [Google Scholar] [CrossRef]
- Engell, D.B.; Maller, O.; Sawka, M.N.; Francesconi, R.N.; Drolet, L.; Young, A.J. Thirst and fluid intake following graded hypohydration levels in humans. Physiol Behav 1987, 40, 229–236. [Google Scholar] [CrossRef]
- Hew-Butler, T.; Rosner, M.H.; Fowkes-Godek, S.; Dugas, J.P.; Hoffman, M.D.; Lewis, D.P.; Maughan, R.J.; Miller, K.C.; Montain, S.J.; et al. Statement of the 3rd International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Br J Sports Med 2015, 49, 1432–1446. [Google Scholar] [CrossRef] [PubMed]
- Nolte, H.; Noakes, T.D.; Van Vuuren, B. Ad libitum fluid replacement in military personnel during a 4-h route march. Med Sci Sports Exerc 2010, 42, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Nolte, H.W.; Noakes, T.D.; Nolte, K. Ad libitum vs. restricted fluid replacement on hydration and performance of military tasks. Aviat Space Environ Med 2013, 84, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Nolte, H.W.; Noakes, T.D.; van Vuuren, B. Protection of total body water content and absence of hyperthermia despite 2% body mass loss (‘voluntary dehydration’) in soldiers drinking ad libitum during prolonged exercise in cool environmental conditions. Br J Sports Med 2011, 45, 1106–1112. [Google Scholar] [CrossRef]
- Nolte, H.W.; Noakes, T.D.; Van Vuuren, B. Trained humans can exercise safely in extreme dry heat when drinking water ad libitum. J Sports Sci 2011, 29, 1233–1241. [Google Scholar] [CrossRef]
- Nolte, H.W.; Nolte, K.; Hew-Butler, T. Ad libitum water consumption prevents exercise-associated hyponatremia and protects against dehydration in soldiers performing a 40-km route-march. Mil Med Res 2019, 6, 1. [Google Scholar] [CrossRef]
- Montain, S.J.; Coyle, E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol (1985) 1992, 73, 1340–1350. [Google Scholar] [CrossRef]
- Armstrong, L.E. Hydration assessment techniques. Nutr Rev 2005, 63, S40–S54. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Ganio, M.S.; Klau, J.F.; Johnson, E.C.; Casa, D.J.; Maresh, C.M. Novel hydration assessment techniques employing thirst and a water intake challenge in healthy men. Appl Physiol Nutr Metab 2014, 39, 138–144. [Google Scholar] [CrossRef]

| Physical characteristics | Mean ± SD |
|---|---|
| Age (years) | 23 ± 5 |
| Body mass (kg) | 71.7 ± 12.7 |
| Height (cm) | 173.8 ± 8.5 |
| Body mass index (kg · m2) | 23.7 ± 3.7 |
| Fat-free mass (kg) | 57.9 ± 10.4 |
|
Relative maximal O2 consumption (mL· kg body mass · min-1) |
52.7 ± 7.1 |
| Resting heart rate (beats · min-1) | 70 ± 13 |
| Resting systolic blood pressure (mmHg) | 119 ± 10 |
| Resting diastolic blood pressure (mmHg) | 73 ± 4 |
| Variables |
Exercise session 1 |
Exercise session 2 | Exercise session 3 | Exercise session 4 | pvalue | ||
|
Urine specific gravity (g · mL-1) |
1.011 ± 0.007 | 1.016 ± 0.009 | 1.018 ± 0.008 | 1.021 ± 0.005 | 0.001 | ||
| Body mass (kg) | 72.1 ± 12.6 | 72.3 ± 12.7 | 72.3 ± 12.9 | 71.7 ± 12.8 | 0.18 | ||
| Thirst (AU) | 2.2 ± 0.8 | 2.3 ± 0.8 | 2.3 ± 0.8 | 2.7 ± 0.9 | 0.66 | ||
|
Exercise session 1 to 2 |
Exercise session 1 to 3 |
Exercise session 1 to 4 |
|||||
| Change in body mass (%) | 0.35 ± 1.32 | 0.21 ± 1.55 | - 0.55 ± 1.45 | 0.046 | |||
| Participants | Exercise session 1 (mL) * | Exercise session 2 (mL) * | Exercise session 3 (mL) * | Exercise session 4 (mL) * | Total accumulated fluid intake volume (mL) - total accumulated sweat loss (mL) * |
|---|---|---|---|---|---|
| 1 | - 650 | - 332 | - 303 | - 175 | - 1460 |
| 2 | - 1286 | - 1070 | - 1042 | - 1264 | - 4662 |
| 3 | - 580 | - 357 | - 72 | + 39 | - 970 |
| 4 | - 150 | - 50 | + 50 | - 200 | - 350 |
| 5 | - 500 | - 750 | - 150 | 0 | - 1400 |
| 6 | - 145 | - 466 | - 635 | - 245 | - 1491 |
| 7 | + 654 | + 414 | + 144 | + 312 | + 1524 |
| 8 | - 250 | + 200 | + 650 | + 400 | + 1000 |
| 9 | - 1150 | - 700 | - 250 | - 400 | - 2500 |
| 10 | - 800 | - 650 | - 500 | - 650 | - 2600 |
| 11 | - 700 | - 250 | - 200 | - 250 | - 1400 |
| 12 | + 1350 | + 450 | - 100 | - 400 | + 1300 |
| Mean ± SD | - 350 ± 738 | - 297 ± 435 | - 201 ± 419 | - 236 ± 439 | - 1084 ± 1783 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





