Submitted:
26 September 2023
Posted:
27 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
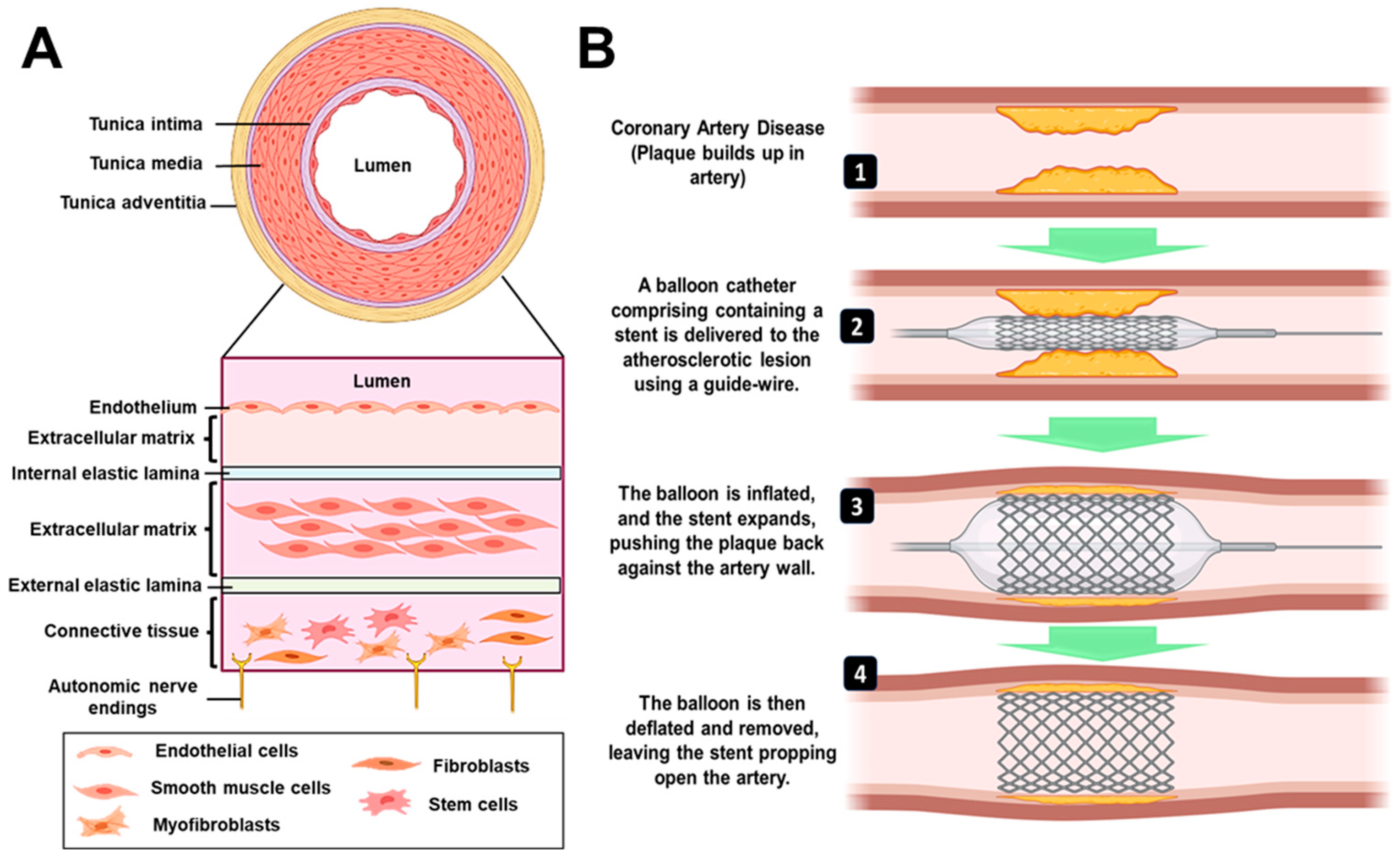
2. Clinical Perspective of Stents
2.1. Metal Stents
2.2. Drug-Eluting Stents
2.3. Bio-Resorbable Vascular Scaffold
3. Limitations
4. Fabrication Technologies
4.1. 3D Printing
4.1.1. Extrusion Based 3D Printing
4.1.1.1. Fused Deposition Modelling
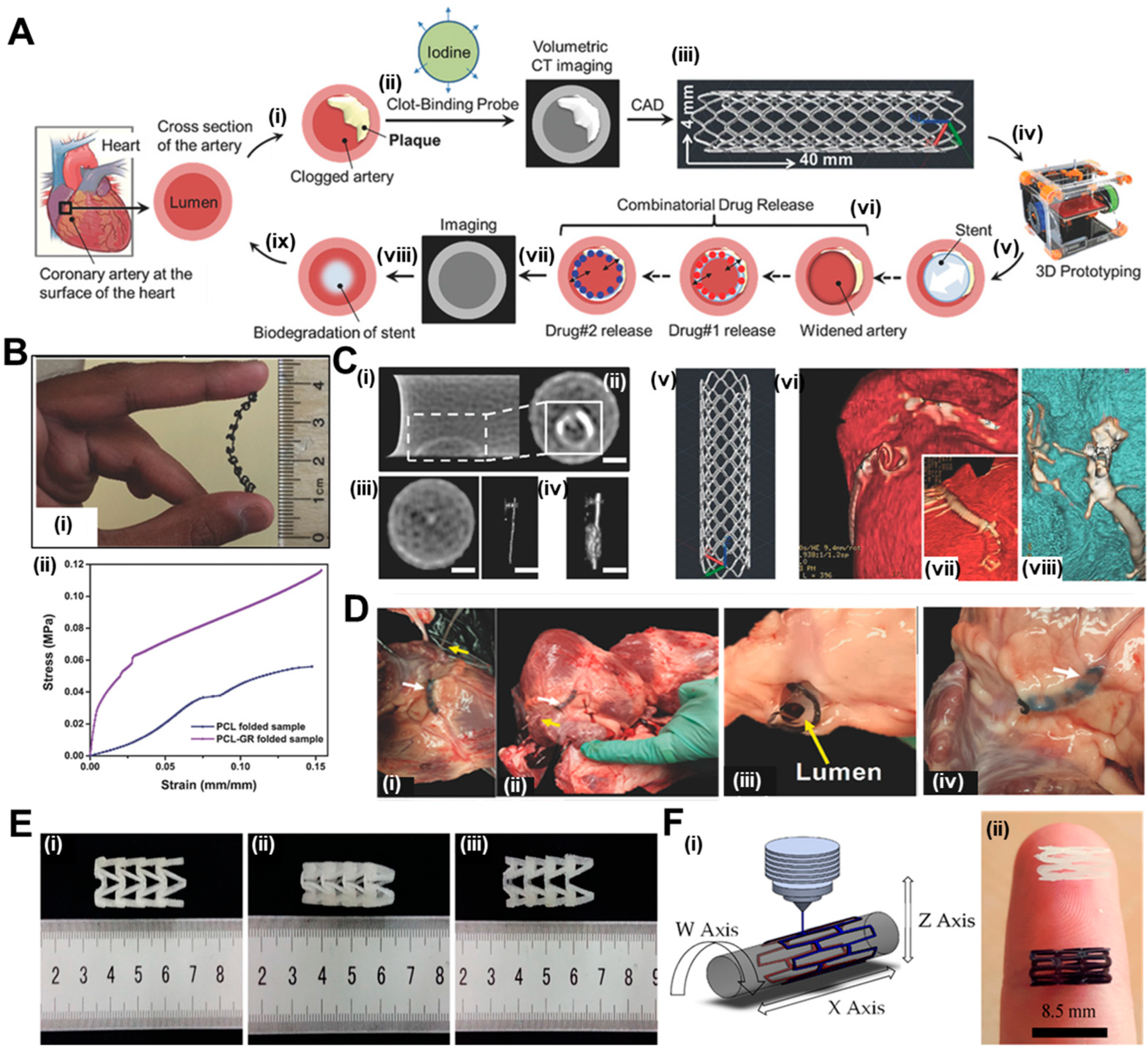
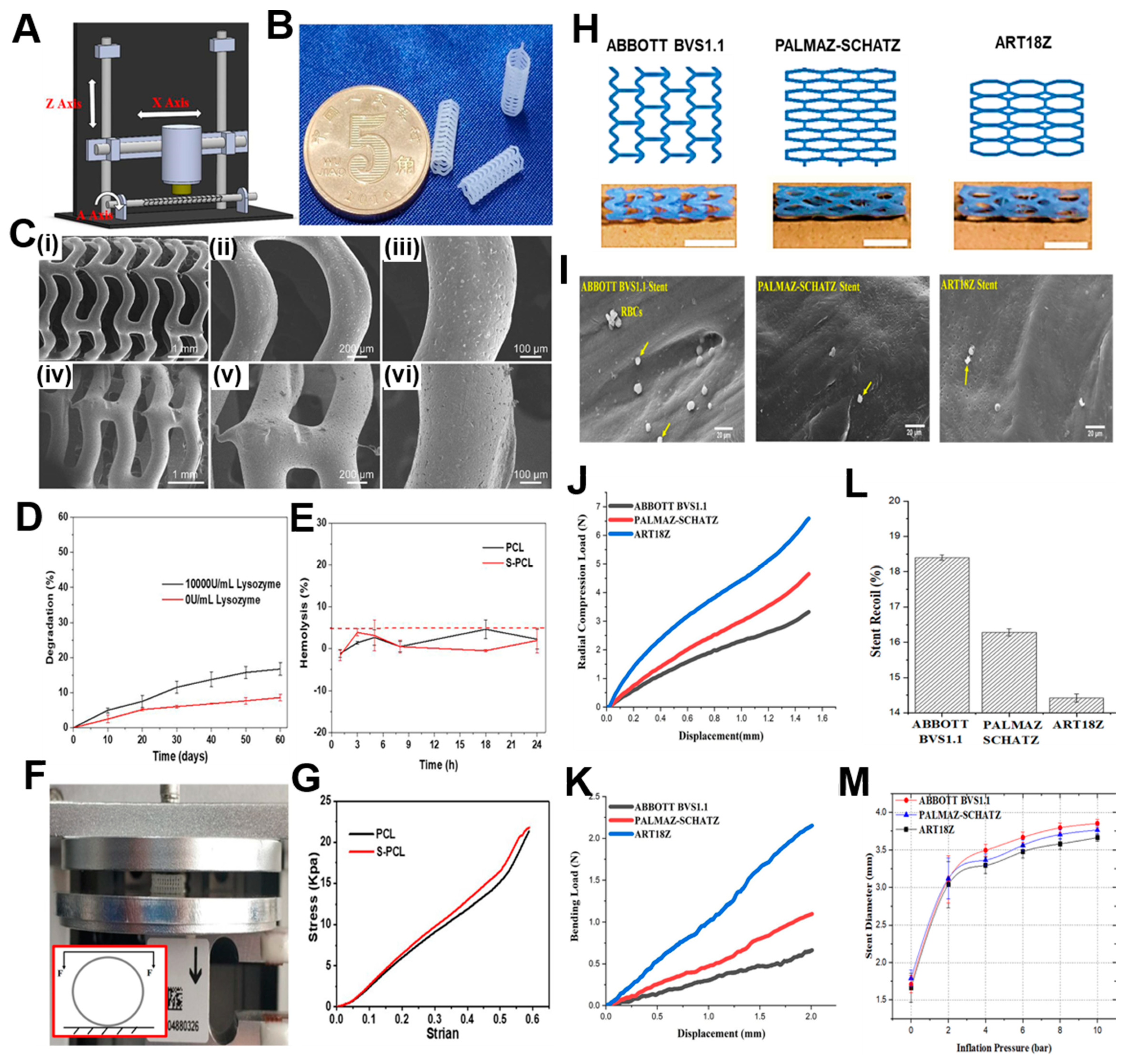
4.1.1.2. Solvent Cast 3D Printing
4.1.2. Light-Based Printing
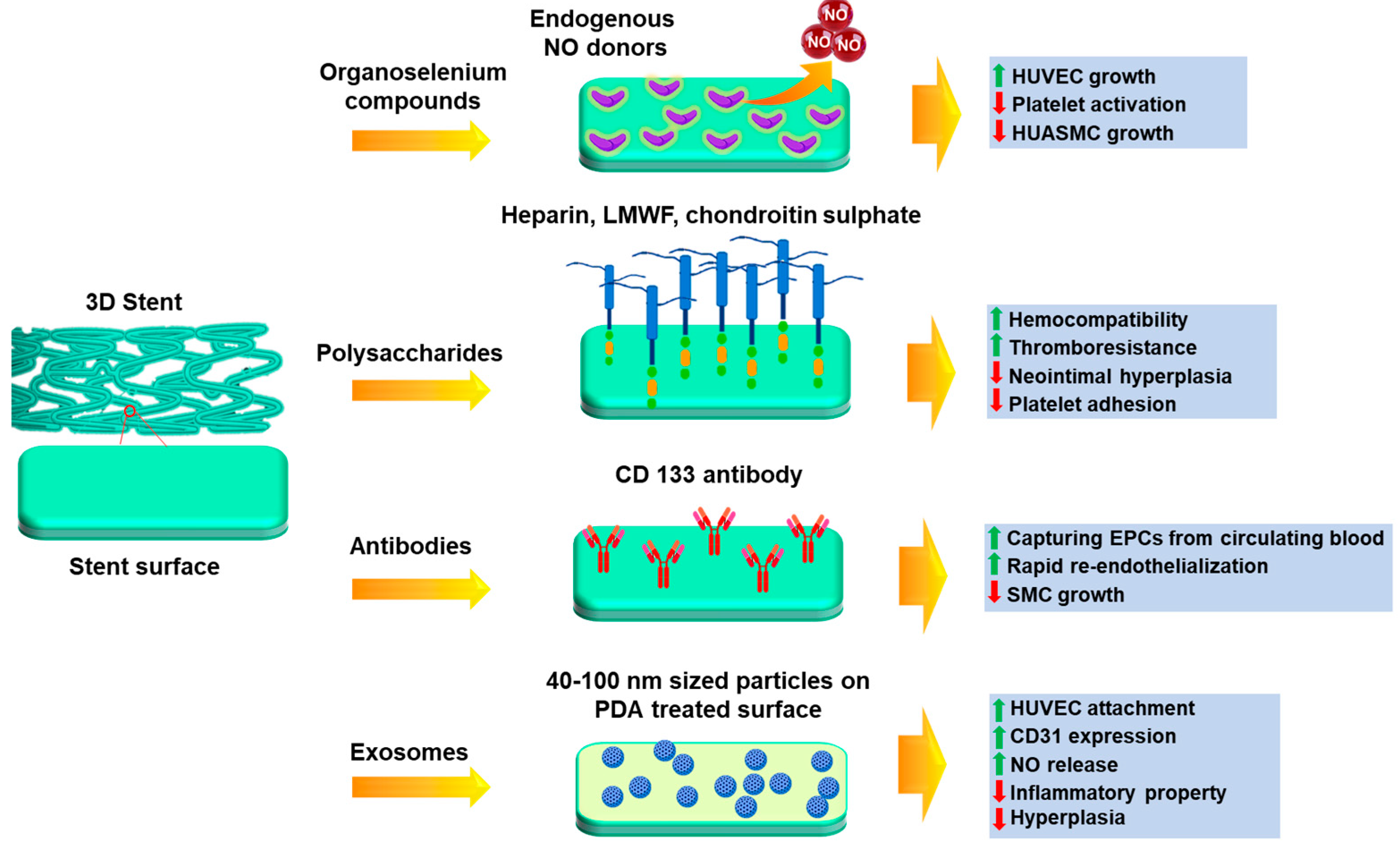
5. Functionalization with Bioactive Molecules
6. Conclusions
7. Future Perspectives
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fox, K.A.A.; Metra, M.; Morais, J.; Atar, D. The Myth of ‘Stable’ coronary artery disease. Nat Rev Cardiol 2020, 17, 9–21. [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R. Heart Disease and Stroke Statistics—2019 Update: A Report from the American Heart Association. Circulation 2019, 139, e56–e528.
- Iqbal, J.; Gunn, J.; Serruys, P.W. Coronary Stents: Historical Development, Current Status and Future Directions. Br Med Bull 2013, 106, 193–211. [CrossRef]
- Ueda, P.; Gulayin, P.; Danaei, G. Long-Term Moderately Elevated LDL-Cholesterol and Blood Pressure and Risk of Coronary Heart Disease. PLoS One 2018, 13, e0200017.
- Kloc, M.; Ghobrial, R.M. Chronic Allograft Rejection: A Significant Hurdle to Transplant Success. Burns Trauma 2014, 2, 2321–3868.
- Madamanchi, N.R.; Vendrov, A.; Runge, M.S. Oxidative Stress and Vascular Disease. Arterioscler Thromb Vasc Biol 2005, 25, 29–38. [CrossRef]
- Braun, M.M.; Stevens, W.A. P376-1. 2018, 97, 376–384.
- Burgess, S.N.; John, J.; Juergens, C.P.; French, J.K. Coronary Artery Bypass Grafting versus Percutaneous Intervention in Coronary Revascularization: A Historical Perspective and Review. Research Reports in Clinical Cardiology 2015, 6, 57–71.
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur Heart J 2019, 40, 87–165. [CrossRef]
- Lobato, E.B. Chapter 3 - Care of the Patient with Coronary Stents Undergoing Noncardiac Surgery. In Essentials of Cardiac Anesthesia for Noncardiac Surgery; Kaplan, J.A., Cronin, B., Maus, T.M., Eds.; Elsevier: New York, 2019; pp. 33–69 ISBN 978-0-323-56716-9.
- Li, X.; Zhang, W.; Lin, W.; Qiu, H.; Qi, Y.; Ma, X.; Qi, H.; He, Y.; Zhang, H.; Qian, J.; et al. Long-Term Efficacy of Biodegradable Metal-Polymer Composite Stents After the First and the Second Implantations into Porcine Coronary Arteries. ACS Appl Mater Interfaces 2020, 12, 15703–15715. [CrossRef]
- Garg, S.; Serruys, P.W. Coronary Stents: Current Status. J Am Coll Cardiol 2010, 56, S1–S42. [CrossRef]
- Joner, M.; Finn, A. V; Farb, A.; Mont, E.K.; Kolodgie, F.D.; Ladich, E.; Kutys, R.; Skorija, K.; Gold, H.K.; Virmani, R. Pathology of Drug-Eluting Stents in Humans: Delayed Healing and Late Thrombotic Risk. J Am Coll Cardiol 2006, 48, 193–202.
- Bates, E.R.; Lau, W.C.; Angiolillo, D.J. Clopidogrel–Drug Interactions. J Am Coll Cardiol 2011, 57, 1251–1263.
- Menown, I.; Noad, R.; Garcia, E.; Meredith AM, P.I. The Platinum Chromium Element Stent Platform: From Alloy, to Design, to Clinical Practice. Adv Ther 2010, 27, 129–141. [CrossRef]
- McMahon, S.; Bertollo, N.; Cearbhaill, E.D.O.; Salber, J.; Pierucci, L.; Duffy, P.; Dürig, T.; Bi, V.; Wang, W. Bio-Resorbable Polymer Stents: A Review of Material Progress and Prospects. Prog Polym Sci 2018, 83, 79–96. [CrossRef]
- Garg, S.; Serruys, P.W. Coronary Stents: Looking Forward. J Am Coll Cardiol 2010, 56, S43–S78.
- Windecker, S.; Meier, B. Late Coronary Stent Thrombosis. Circulation 2007, 116, 1952–1965.
- Finn, A. V; John, M.C.; Gold, H.K.; Newell, J.; Nakazawa, G.; Joner, M.; D. Kolodgie, F.; Virmani, R. Response to Letter Regarding Article,“Pathological Correlates of Late Drug-Eluting Stent Thrombosis: Strut Coverage as a Marker of Endothelialization.” Circulation 2007, 116, e550–e550.
- Pilgrim, T.; Windecker, S. Drug-Eluting Stent Thrombosis. Minerva Cardioangiol 2009, 57, 611–620.
- Sigwart, U.; Urban, P.; Golf, S.; Kaufmann, U.; Imbert, C.; Fischer, A.; Kappenberger, L. Emergency Stenting for Acute Occlusion after Coronary Balloon Angioplasty. Circulation 1988, 78, 1121–1127. [CrossRef]
- Sharma, U.; Concagh, D.; Core, L.; Kuang, Y.; You, C.; Pham, Q.; Zugates, G.; Busold, R.; Webber, S.; Merlo, J.; et al. The Development of Bioresorbable Composite Polymeric Implants with High Mechanical Strength. Nat Mater 2018, 17, 96–102. [CrossRef]
- Peuster, M.; Wohlsein, P.; Brügmann, M.; Ehlerding, M.; Seidler, K.; Fink, C.; Brauer, H.; Fischer, A.; Hausdorf, G. A Novel Approach to Temporary Stenting: Degradable Cardiovascular Stents Produced from Corrodible Metal-Results 6-18 Months after Implantation into New Zealand White Rabbits. Heart 2001, 86, 563–569. [CrossRef]
- Qi, Y.; Qi, H.; He, Y.; Lin, W.; Li, P.; Qin, L.; Hu, Y.; Chen, L.; Liu, Q.; Sun, H.; et al. Strategy of Metal–Polymer Composite Stent to Accelerate Biodegradation of Iron-Based Biomaterials. ACS Appl Mater Interfaces 2018, 10, 182–192. [CrossRef]
- Peuster, M.; Hesse, C.; Schloo, T.; Fink, C.; Beerbaum, P.; von Schnakenburg, C. Long-Term Biocompatibility of a Corrodible Peripheral Iron Stent in the Porcine Descending Aorta. Biomaterials 2006, 27, 4955–4962. [CrossRef]
- Colotti, G.; Ilari, A.; Boffi, A.; Morea, V. Metals and Metal Derivatives in Medicine. Mini-Reviews in Medicinal Chemistry 2013, 13, 211–221. [CrossRef]
- Onuma, Y.; Ormiston, J.; Serruys, P.W. Bioresorbable Scaffold Technologies. Circulation Journal 2011, 75, 509–520. [CrossRef]
- Garg, S.; Serruys, P. Biodegradable Stents and Non-Biodegradable Stents. Minerva Cardioangiol 2009, 57, 537—565.
- Morice, M.-C.; Serruys, P.W.; Sousa, J.E.; Fajadet, J.; Ban Hayashi, E.; Perin, M.; Colombo, A.; Schuler, G.; Barragan, P.; Guagliumi, G.; et al. A Randomized Comparison of a Sirolimus-Eluting Stent with a Standard Stent for Coronary Revascularization. N Engl J Med 2002, 346, 1773–1780. [CrossRef]
- Grube, E.; Silber, S.; Hauptmann, K.E.; Mueller, R.; Buellesfeld, L.; Gerckens, U.; Russell, M.E. Six- and Twelve-Month Results from a Randomized, Double-Blind Trial on a Slow-Release Paclitaxel-Eluting Stent for de Novo Coronary Lesions. Circulation 2003, 107, 38–42. [CrossRef]
- F., L.T.; Jan, S.; R., E.F.; Michael, J.; Gaku, N.; C., T.F.; Renu, V. Drug-Eluting Stent and Coronary Thrombosis. Circulation 2007, 115, 1051–1058. [CrossRef]
- Joost, D.; W., S.P. Drug-Eluting Stent Update 2007. Circulation 2007, 116, 316–328. [CrossRef]
- Lasala, J.M.; Stone, G.W.; Dawkins, K.D.; Serruys, P.W.; Colombo, A.; Grube, E.; Koglin, J.; Ellis, S. An Overview of the TAXUS® Express®, Paclitaxel-Eluting Stent Clinical Trial Program. J Interv Cardiol 2006, 19, 422–431. [CrossRef]
- Stone, G.W.; Ellis, S.G.; Cox, D.A.; Hermiller, J.; O’Shaughnessy, C.; Mann, J.T.; Turco, M.; Caputo, R.; Bergin, P.; Greenberg, J.; et al. A Polymer-Based, Paclitaxel-Eluting Stent in Patients with Coronary Artery Disease. New England Journal of Medicine 2004, 350, 221–231. [CrossRef]
- Beijk, M.A.M.; Klomp, M.; Verouden, N.J.W.; van Geloven, N.; Koch, K.T.; Henriques, J.P.S.; Baan, J.; Vis, M.M.; Scheunhage, E.; Piek, J.J.; et al. Genous Endothelial Progenitor Cell Capturing Stent vs. the Taxus Liberte Stent in Patients with de Novo Coronary Lesions with a High-Risk of Coronary Restenosis: A Randomized, Single-Centre, Pilot Study. Eur Heart J 2010, 31, 1055–1064. [CrossRef]
- Smits, P.C.; Vlachojannis, G.J.; McFadden, E.P.; Royaards, K.J.; Wassing, J.; Joesoef, K.S.; Van Mieghem, C.; Van De Ent, M. Final 5-Year Follow-Up of a Randomized Controlled Trial of Everolimus- and Paclitaxel-Eluting Stents for Coronary Revascularization in Daily Practice the COMPARE Trial (A Trial of Everolimus-Eluting Stents and Paclitaxel Stents for Coronary Revascularizat. JACC Cardiovasc Interv 2015, 8, 1157–1165. [CrossRef]
- Fajadet, J.; Wijns, W.; Laarman, G.-J.; Kuck, K.-H.; Ormiston, J.; Baldus, S.; Hauptmann, K.E.; Suttorp, M.J.; Drzewiecki, J.; Pieper, M.; et al. Long-Term Follow-up of the Randomised Controlled Trial to Evaluate the Safety and Efficacy of the Zotarolimus-Eluting Driver Coronary Stent in de Novo Native Coronary Artery Lesions: Five Year Outcomes in the ENDEAVOR II Study. EuroIntervention 2010, 6, 562–567. [CrossRef]
- Kirtane, A.J.; Leon, M.B.; Ball, M.W.; Bajwa, H.S.; Sketch, M.H.; Coleman, P.S.; Stoler, R.C.; Papadakos, S.; Cutlip, D.E.; Mauri, L.; et al. The “Final” 5-Year Follow-Up from the ENDEAVOR IV Trial Comparing a Zotarolimus-Eluting Stent With a Paclitaxel-Eluting Stent. JACC Cardiovasc Interv 2013, 6, 325–333. [CrossRef]
- Leon, M.B.; Mauri, L.; Popma, J.J.; Cutlip, D.E.; Nikolsky, E.; O’Shaughnessy, C.; Overlie, P.A.; McLaurin, B.T.; Solomon, S.L.; Douglas, J.S.; et al. A Randomized Comparison of the Endeavor Zotarolimus-Eluting Stent Versus the TAXUS Paclitaxel-Eluting Stent in De Novo Native Coronary Lesions: 12-Month Outcomes from the ENDEAVOR IV Trial. J Am Coll Cardiol 2010, 55, 543–554. [CrossRef]
- Kandzari, D.E.; Mauri, L.; Popma, J.J.; Turco, M.A.; Gurbel, P.A.; Fitzgerald, P.J.; Leon, M.B. Late-Term Clinical Outcomes with Zotarolimus- and Sirolimus-Eluting Stents: 5-Year Follow-up of the ENDEAVOR III (a Randomized Controlled Trial of the Medtronic Endeavor Drug [ABT-578] Eluting Coronary Stent System versus the Cypher Sirolimus-Eluting Coro. JACC Cardiovasc Interv 2011, 4, 543–550. [CrossRef]
- von Birgelen, C.; Basalus, M.W.Z.; Tandjung, K.; van Houwelingen, K.G.; Stoel, M.G.; Louwerenburg, J. (Hans) W.; Linssen, G.C.M.; Saïd, S.A.M.; Kleijne, M.A.W.J.; Sen, H.; et al. A Randomized Controlled Trial in Second-Generation Zotarolimus-Eluting Resolute Stents Versus Everolimus-Eluting Xience V Stents in Real-World Patients: The TWENTE Trial. J Am Coll Cardiol 2012, 59, 1350–1361. [CrossRef]
- Gada, H.; Kirtane, A.J.; Newman, W.; Sanz, M.; Hermiller, J.B.; Mahaffey, K.W.; Cutlip, D.E.; Sudhir, K.; Hou, L.; Koo, K.; et al. 5-Year Results of a Randomized Comparison of XIENCE V Everolimus-Eluting and TAXUS Paclitaxel-Eluting Stents: Final Results From the SPIRIT III Trial (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Patient. JACC Cardiovasc Interv 2013, 6, 1263–1266. [CrossRef]
- Stone, G.W.; Rizvi, A.; Sudhir, K.; Newman, W.; Applegate, R.J.; Cannon, L.A.; Maddux, J.T.; Cutlip, D.E.; Simonton, C.A.; Sood, P.; et al. Randomized Comparison of Everolimus- and Paclitaxel-Eluting Stents: 2-Year Follow-Up from the SPIRIT (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System) IV Trial. J Am Coll Cardiol 2011, 58, 19–25. [CrossRef]
- Grube, E.; Chevalier, B.; Guagliumi, G.; Smits, P.C.; Stuteville, M.; Dorange, C.; Papeleu, P.; Kaul, U.; Džavík, V. The SPIRIT V Diabetic Study: A Randomized Clinical Evaluation of the XIENCE V Everolimus-Eluting Stent vs the TAXUS Liberté Paclitaxel-Eluting Stent in Diabetic Patients with de Novo Coronary Artery Lesions. Am Heart J 2012, 163, 867-875.e1. [CrossRef]
- Park, K.W.; Lee, J.M.; Kang, S.-H.; Ahn, H.-S.; Kang, H.-J.; Koo, B.-K.; Rhew, J.Y.; Hwang, S.H.; Lee, S.Y.; Kang, T.S.; et al. Everolimus-Eluting Xience V/Promus Versus Zotarolimus-Eluting Resolute Stents in Patients with Diabetes Mellitus. JACC Cardiovasc Interv 2014, 7, 471–481. [CrossRef]
- Planer, D.; Smits, P.C.; Kereiakes, D.J.; Kedhi, E.; Fahy, M.; Xu, K.; Serruys, P.W.; Stone, G.W. Comparison of Everolimus- and Paclitaxel-Eluting Stents in Patients with Acute and Stable Coronary Syndromes: Pooled Results from the SPIRIT (A Clinical Evaluation of the XIENCE v Everolimus Eluting Coronary Stent System) and COMPARE (A Trial of Everolimu. JACC Cardiovasc Interv 2011, 4, 1104–1115. [CrossRef]
- Liu, S.-J.; Chiang, F.-J.; Hsiao, C.-Y.; Kau, Y.-C.; Liu, K.-S. Fabrication of Balloon-Expandable Self-Lock Drug-Eluting Polycaprolactone Stents Using Micro-Injection Molding and Spray Coating Techniques. Ann Biomed Eng 2010, 38, 3185–3194. [CrossRef]
- Chen, M.C.; Liu, C.T.; Tsai, H.W.; Lai, W.Y.; Chang, Y.; Sung, H.W. Mechanical Properties, Drug Eluting Characteristics, and in Vivo Performance of a Genipin-Crosslinked Chitosan Polymeric Stent. Biomaterials 2009, 30, 5560–5571. [CrossRef]
- Bleier, B.S.; Paulson, D.P.; O’Malley, B.W.; Li, D.; Palmer, J.N.; Chiu, A.G.; Cohen, N.A. Chitosan Glycerophosphate-Based Semirigid Dexamethasone Eluting Biodegradable Stent. Am J Rhinol Allergy 2009, 23, 76–79. [CrossRef]
- Gogas, B.D.; Farooq, V.; Onuma, Y.; Serruys, P.W. The ABSORB Bioresorbable Vascular Scaffold: An Evolution or Revolution in Interventional Cardiology? Hellenic J Cardiol 2012, 53, 301–309.
- Gogas, B.D. Bioresorbable Scaffolds for Percutaneous Coronary Interventions. Glob Cardiol Sci Pract 2014, 2014, 409–427. [CrossRef]
- Mattesini, A.; Bartolini, S.; Sorini Dini, C.; Valente, S.; Parodi, G.; Stolcova, M.; Meucci, F.; Di Mario, C. The DESolve Novolimus Bioresorbable Scaffold: From Bench to Bedside. J Thorac Dis 2017, 9, S950—S958. [CrossRef]
- Verheye, S.; Ormiston, J.A.; Stewart, J.; Webster, M.; Sanidas, E.; Costa, R.; Costa, J.R.J.; Chamie, D.; Abizaid, A.S.; Pinto, I.; et al. A Next-Generation Bioresorbable Coronary Scaffold System: From Bench to First Clinical Evaluation: 6- and 12-Month Clinical and Multimodality Imaging Results. JACC Cardiovasc Interv 2014, 7, 89–99. [CrossRef]
- Iqbal, J.; Onuma, Y.; Ormiston, J.; Abizaid, A.; Waksman, R.; Serruys, P. Bioresorbable Scaffolds: Rationale, Current Status, Challenges, and Future. Eur Heart J 2014, 35, 765–776. [CrossRef]
- Iqbal, J.; Verheye, S.; Abizaid, A.; Ormiston, J.; de Vries, T.; Morrison, L.; Toyloy, S.; Fitzgerald, P.; Windecker, S.; Serruys, P.W. DESyne Novolimus-Eluting Coronary Stent Is Superior to Endeavor Zotarolimus-Eluting Coronary Stent at Five-Year Follow-up: Final Results of the Multicentre EXCELLA II Randomised Controlled Trial. EuroIntervention 2016, 12, e1336–e1342. [CrossRef]
- Boeder, N.F.; Dorr, O.; Bauer, T.; Mattesini, A.; Elsasser, A.; Liebetrau, C.; Achenbach, S.; Hamm, C.W.; Nef, H.M. Impact of Strut Thickness on Acute Mechanical Performance: A Comparison Study Using Optical Coherence Tomography between DESolve 150 and DESolve 100. Int J Cardiol 2017, 246, 74–79. [CrossRef]
- Ramcharitar, S.; Serruys, P.W. Fully Biodegradable Coronary Stents: Progress to Date. Am J Cardiovasc Drugs 2008, 8, 305–314. [CrossRef]
- Abizaid, A.; Carrie, D.; Frey, N.; Lutz, M.; Weber-Albers, J.; Dudek, D.; Chevalier, B.; Weng, S.-C.; Costa, R.A.; Anderson, J.; et al. 6-Month Clinical and Angiographic Outcomes of a Novel Radiopaque Sirolimus-Eluting Bioresorbable Vascular Scaffold: The FANTOM II Study. JACC Cardiovasc Interv 2017, 10, 1832–1838. [CrossRef]
- Zhang, Y.; Bourantas, C. V; Farooq, V.; Muramatsu, T.; Diletti, R.; Onuma, Y.; Garcia-Garcia, H.M.; Serruys, P.W. Bioresorbable Scaffolds in the Treatment of Coronary Artery Disease. Med Devices (Auckl) 2013, 6, 37–48. [CrossRef]
- Rao, A.S.; Makaroun, M.S.; Marone, L.K.; Cho, J.S.; Rhee, R.; Chaer, R.A. Long-Term Outcomes of Internal Carotid Artery Dissection. J Vasc Surg 2011, 54, 370–375. [CrossRef]
- Kumar, A.S.; Hariram, V. Indigenous Stents: Examining the Clinical Data on New Technologies. Interventional Cardiology (London) 2014, 6, 319–333. [CrossRef]
- Yanping, C.; Pawel, G.; Masahiko, S.; Kamal, R.; Chang, L.; A., E.E.; Daniell, D.; C., M.J.; B., C.G.; L., K.G.; et al. Comparative Characterization of Biomechanical Behavior and Healing Profile of a Novel Ultra-High-Molecular-Weight Amorphous Poly-l-Lactic Acid Sirolimus-Eluting Bioresorbable Coronary Scaffold. Circ Cardiovasc Interv 2016, 9, e004253. [CrossRef]
- Indolfi, C.; De Rosa, S.; Colombo, A. Bioresorbable Vascular Scaffolds - Basic Concepts and Clinical Outcome. Nat Rev Cardiol 2016, 13, 719–729. [CrossRef]
- Wu, Y.; Shen, L.; Wang, Q.; Ge, L.; Xie, J.; Hu, X.; Sun, A.; Qian, J.; Ge, J. Comparison of Acute Recoil between Bioabsorbable Poly-L-Lactic Acid XINSORB Stent and Metallic Stent in Porcine Model. J Biomed Biotechnol 2012, 2012, 413956. [CrossRef]
- Shen, L.; Wu, Y.; Ge, L.; Zhang, Y.; Wang, Q.; Qian, J.; Qiu, Z.; Ge, J. A Head-to-Head Comparison of XINSORB Bioresorbable Sirolimus-Eluting Scaffold versus Metallic Sirolimus-Eluting Stent: 180 Days Follow-up in a Porcine Model. Int J Cardiovasc Imaging 2017, 33, 1473–1481. [CrossRef]
- Wang, Y.; Zhang, X. Vascular Restoration Therapy and Bioresorbable Vascular Scaffold. Regen Biomater 2014, 1, 49–55. [CrossRef]
- Muramatsu, T.; Onuma, Y.; Zhang, Y.-J.; Bourantas, C. V; Kharlamov, A.; Diletti, R.; Farooq, V.; Gogas, B.D.; Garg, S.; Garcia-Garcia, H.M.; et al. Progress in Treatment by Percutaneous Coronary Intervention: The Stent of the Future. Rev Esp Cardiol (Engl Ed) 2013, 66, 483–496. [CrossRef]
- Jabara, R.; Pendyala, L.; Geva, S.; Chen, J.; Chronos, N.; Robinson, K. Novel Fully Bioabsorbable Salicylate-Based Sirolimus-Eluting Stent. EuroIntervention 2009, 5 Suppl F, F58-64. [CrossRef]
- Tenekecioglu, E.; Farooq, V.; Bourantas, C. V; Silva, R.C.; Onuma, Y.; Yilmaz, M.; Serruys, P.W. Bioresorbable Scaffolds: A New Paradigm in Percutaneous Coronary Intervention. BMC Cardiovasc Disord 2016, 16, 38. [CrossRef]
- Costa, R.A.; Liew, H.-B.; Abizaid, A.; de Ribamar Costa, J.; Chamié, D.; Abizaid, A.; Castro, J.P.; Serruys, P.W.; Santoso, T. TCT-546 6-Month Angiographic Results of the Novel MIRAGE Microfiber Sirolimus-Eluting Bioresorbable Vascular Scaffold - A Quantitative Coronary Angiography Analysis from the Prospective, Randomized MIRAGE Clinical Trial. J Am Coll Cardiol 2015, 66, B223. [CrossRef]
- Hideo, T.; Keiji, I.; Eisho, K.; Kunihiko, K.; Akiyoshi, K.; Shigeo, M.; Hidenori, K.; Takafumi, T.; Seiichiro, M.; Hiromu, U. Initial and 6-Month Results of Biodegradable Poly-l-Lactic Acid Coronary Stents in Humans. Circulation 2000, 102, 399–404. [CrossRef]
- Nishio, S.; Kosuga, K.; Igaki, K.; Okada, M.; Kyo, E.; Tsuji, T.; Takeuchi, E.; Inuzuka, Y.; Takeda, S.; Hata, T.; et al. Long-Term (>10 Years) Clinical Outcomes of First-in-Human Biodegradable Poly-l-Lactic Acid Coronary Stents: Igaki-Tamai Stents. Circulation 2012, 125, 2343–2353. [CrossRef]
- Yahagi, K.; Yang, Y.; Torii, S.; Mensah, J.; White, R.M.; Mathieu, M.; Pacheco, E.; Nakano, M.; Barakat, A.; Sharkawi, T.; et al. Comparison of a Drug-Free Early Programmed Dismantling PDLLA Bioresorbable Scaffold and a Metallic Stent in a Porcine Coronary Artery Model at 3-Year Follow-Up. J Am Heart Assoc 2017, 6, e005693. [CrossRef]
- Durand, E.; Sharkawi, T.; Leclerc, G.; Raveleau, M.; van der Leest, M.; Vert, M.; Lafont, A. Head-to-Head Comparison of a Drug-Free Early Programmed Dismantling Polylactic Acid Bioresorbable Scaffold and a Metallic Stent in the Porcine Coronary Artery: Six-Month Angiography and Optical Coherence Tomographic Follow-up Study. Circ Cardiovasc Interv 2014, 7, 70–79. [CrossRef]
- Ielasi, A.; Tespili, M. Current and Future Perspectives on Drug-Eluting Bioresorbable Coronary Scaffolds. Future Cardiol 2014, 10, 409–420.
- Kenny, D.; Hijazi, Z.M. Bioresorbable Stents for Pediatric Practice: Where Are We Now? Interv Cardiol (Lond) 2015, 7, 245–255. [CrossRef]
- Hoffmann, R.; Mintz, G.S.; Dussaillant, G.R.; Popma, J.J.; Pichard, A.D.; Satler, L.F.; Kent, K.M.; Griffin, J.; Leon, M.B. Patterns and Mechanisms of In-Stent Restenosis. Circulation 1996, 94, 1247–1254. [CrossRef]
- Haude, M.; Ince, H.; Abizaid, A.; Toelg, R.; Lemos, P.A.; von Birgelen, C.; Christiansen, E.H.; Wijns, W.; Neumann, F.-J.; Kaiser, C.; et al. Safety and Performance of the Second-Generation Drug-Eluting Absorbable Metal Scaffold in Patients with de-Novo Coronary Artery Lesions (BIOSOLVE-II): 6 Month Results of a Prospective, Multicentre, Non-Randomised, First-in-Man Trial. The Lancet 2016, 387, 31–39. [CrossRef]
- Haude, M.; Erbel, R.; Erne, P.; Verheye, S.; Degen, H.; Vermeersch, P.; Weissman, N.; Prati, F.; Bruining, N.; Waksman, R.; et al. Safety and Performance of the DRug-Eluting Absorbable Metal Scaffold (DREAMS) in Patients with de Novo Coronary Lesions: 3-Year Results of the Prospective, Multicentre, First-in-Man BIOSOLVE-I Trial. EuroIntervention 2016, 12, e160-6. [CrossRef]
- Haddad, R.N.; Adel Hassan, A.; AL Soufi, M.; Kasem, M. A Word of Caution: Early Failure of Magmaris® Bioresorbable Stent after Pulmonary Artery Stenting. Catheterization and Cardiovascular Interventions 2023, 101, 131–134. [CrossRef]
- He, Y.; Wang, J.; Yan, W.; Huang, N. Gallic Acid and Gallic Acid-Loaded Coating Involved in Selective Regulation of Platelet, Endothelial and Smooth Muscle Cell Fate. RSC Adv 2014, 4, 212–221. [CrossRef]
- Toyota, T.; Morimoto, T.; Shiomi, H.; Yoshikawa, Y.; Yaku, H.; Yamashita, Y.; Kimura, T. Very Late Scaffold Thrombosis of Bioresorbable Vascular Scaffold: Systematic Review and a Meta-Analysis. JACC Cardiovasc Interv 2017, 10, 27–37. [CrossRef]
- Verschuur, E.M.L.; Steyerberg, E.W.; Kuipers, E.J.; Siersema, P.D. Effect of Stent Size on Complications and Recurrent Dysphagia in Patients with Esophageal or Gastric Cardia Cancer. Gastrointest Endosc 2007, 65, 592–601.
- Alexy, R.D.; Levi, D.S. Materials and Manufacturing Technologies Available for Production of a Pediatric Bioabsorbable Stent. Biomed Res Int 2013, 2013. [CrossRef]
- Martinez, A.W.; Chaikof, E.L. Microfabrication and Nanotechnology in Stent Design. WIREs Nanomedicine and Nanobiotechnology 2011, 3, 256–268. [CrossRef]
- Ballyns, J.J.; Gleghorn, J.P.; Niebrzydowski, V.; Rawlinson, J.J.; Potter, H.G.; Maher, S.A.; Wright, T.M.; Bonassar, L.J. Image-Guided Tissue Engineering of Anatomically Shaped Implants via MRI and Micro-CT Using Injection Molding. Tissue Eng Part A 2008, 14, 1195–1202. [CrossRef]
- Bartolo, P.; Kruth, J.P.; Silva, J.; Levy, G.; Malshe, A.; Rajurkar, K.; Mitsuishi, M.; Ciurana, J.; Leu, M. Biomedical Production of Implants by Additive Electro-Chemical and Physical Processes. CIRP Ann Manuf Technol 2012, 61, 635–655. [CrossRef]
- Hung, K.C.; Tseng, C.S.; Hsu, S.H. Synthesis and 3D Printing of Biodegradable Polyurethane Elastomer by a Water-Based Process for Cartilage Tissue Engineering Applications. Adv Healthc Mater 2014, 3, 1578–1587. [CrossRef]
- De Leon, A.C.; Chen, Q.; Palaganas, N.B.; Palaganas, J.O.; Manapat, J.; Advincula, R.C. High Performance Polymer Nanocomposites for Additive Manufacturing Applications. React Funct Polym 2016, 103, 141–155. [CrossRef]
- Wong, K. V; Hernandez, A. A Review of Additive Manufacturing. ISRN Mech. Eng. 2012, 1–10 (2012).
- Mohamed, O.A.; Masood, S.H.; Bhowmik, J.L. Optimization of Fused Deposition Modeling Process Parameters: A Review of Current Research and Future Prospects. Adv Manuf 2015, 3, 42–53. [CrossRef]
- Korpela, J.; Kokkari, A.; Korhonen, H.; Malin, M.; Närhi, T.; Seppälä, J. Biodegradable and Bioactive Porous Scaffold Structures Prepared Using Fused Deposition Modeling. J Biomed Mater Res B Appl Biomater 2013, 101B, 610–619. [CrossRef]
- Konta, A.; García, M.; Serrano, D. Personalised 3D Printed Medicines: Which Techniques and Polymers Are More Successful? Bioengineering 2017, 4, 1–16. [CrossRef]
- Jakus, A.E.; Taylor, S.L.; Geisendorfer, N.R.; Dunand, D.C.; Shah, R.N. Metallic Architectures from 3D-Printed Powder-Based Liquid Inks. Adv Funct Mater 2015, 25, 6985–6995. [CrossRef]
- Olga, I.; Christopher, W.; Thomas, C. Additive Manufacturing (AM) and Nanotechnology: Promises and Challenges. Rapid Prototyp J 2013, 19, 353–364. [CrossRef]
- Misra, S.K.; Ostadhossein, F.; Babu, R.; Kus, J.; Tankasala, D.; Sutrisno, A.; Walsh, K.A.; Bromfield, C.R.; Pan, D. 3D-Printed Multidrug-Eluting Stent from Graphene-Nanoplatelet-Doped Biodegradable Polymer Composite. Adv Healthc Mater 2017, 6, 1–14. [CrossRef]
- Cui, J.; Li, J.; Mathison, M.; Tondato, F.; Mulkey, S.P.; Micko, C.; Chronos, N.A.F.; Robinson, K.A. A Clinically Relevant Large-Animal Model for Evaluation of Tissue-Engineered Cardiac Surgical Patch Materials. Cardiovascular Revascularization Medicine 2005, 6, 113–120. [CrossRef]
- Jia, H.; Gu, S.Y.; Chang, K. 3D Printed Self-Expandable Vascular Stents from Biodegradable Shape Memory Polymer. Advances in Polymer Technology 2018, 37, 3222–3228. [CrossRef]
- Alam, J.; Khan, A.; Alam, M.; Mohan, R. Electroactive Shape Memory Property of a Cu-Decorated CNT Dispersed PLA/ESO Nanocomposite. Materials 2015, 8, 6391–6400. [CrossRef]
- Wu, Z.; Zhao, J.; Wu, W.; Wang, P.; Wang, B.; Li, G.; Zhang, S. Radial Compressive Property and the Proof-of-Concept Study for Realizing Self-Expansion of 3D Printing Polylactic Acid Vascular Stents with Negative Poisson’s Ratio Structure. Materials 2018, 11. [CrossRef]
- Wang, W.-Q.; Liang, D.-K.; Yang, D.-Z.; Qi, M. Analysis of the Transient Expansion Behavior and Design Optimization of Coronary fStents by Finite Element Method. J Biomech 2006, 39, 21–32. [CrossRef]
- Wang, C.; Zhang, L.; Fang, Y.; Sun, W. Design, Characterization, and 3D Printing of Cardiovascular Stents with Zero Poisson’s Ratio in Longitudinal Deformation. Engineering 2020, 7, 979–990. [CrossRef]
- Guerra, A.; Roca, A.; de Ciurana, J. A Novel 3D Additive Manufacturing Machine to Biodegradable Stents. Procedia Manuf 2017, 13, 718–723. [CrossRef]
- Guerra, A.J.; Cano, P.; Rabionet, M.; Puig, T.; Ciurana, J. 3D-Printed PCL/PLA Composite Stents: Towards a New Solution to Cardiovascular Problems. Materials 2018, 11, 1–13. [CrossRef]
- Qiu, T.; Jiang, W.; Yan, P.; Jiao, L.; Wang, X. Development of 3D-Printed Sulfated Chitosan Modified Bioresorbable Stents for Coronary Artery Disease. Front Bioeng Biotechnol 2020, 8, 1–12. [CrossRef]
- Lutter, C.; Nothhaft, M.; Rzany, A.; Garlichs, C.D.; Cicha, I. Effect of Specific Surface Microstructures on Substrate Endothelialisation and Thrombogenicity: Importance for Stent Design. Clin Hemorheol Microcirc 2015, 59, 219–233.
- Vurugonda, U.; Rednam, P.; Sinha, M. Development of Biodegradable Scaffold Using Polylactic Acid and Polycaprolactone for Cardiovascular Application. International Journal of Polymeric Materials and Polymeric Biomaterials 2018, 67, 78–85. [CrossRef]
- Zamiri, P.; Kuang, Y.; Sharma, U.; Ng, T.F.; Busold, R.H.; Rago, A.P.; Core, L.A.; Palasis, M. The Biocompatibility of Rapidly Degrading Polymeric Stents in Porcine Carotid Arteries. Biomaterials 2010, 31, 7847–7855. [CrossRef]
- Martins, J.A.; Lach, A.A.; Morris, H.L.; Carr, A.J.; Mouthuy, P.-A. Polydioxanone Implants: A Systematic Review on Safety and Performance in Patients. J Biomater Appl 2020, 34, 902–916.
- Chen, E.; Xiong, Z.; Cai, X.; Liu, S.; Qin, X.; Sun, J.; Jin, X.; Sun, K. Bioresorbable PPDO Sliding-Lock Stents with Optimized FDM Parameters for Congenital Heart Disease Treatment. J Mech Behav Biomed Mater 2023, 138, 105609.
- Okereke, M.I.; Khalaj, R.; Tabriz, A.G.; Nandi, U.; Scoutaris, N.; Douroumis, D. Development of 3D Printable Bioresorbable Drug Eluting Coronary Stents: An Experimental and Computational Investigation. J Drug Deliv Sci Technol 2023, 79, 103952.
- Singh, J.; Pandey, P.M.; Kaur, T.; Singh, N. A Comparative Analysis of Solvent Cast 3D Printed Carbonyl Iron Powder Reinforced Polycaprolactone Polymeric Stents for Intravascular Applications. J Biomed Mater Res B Appl Biomater 2021, 109, 1344–1359. [CrossRef]
- Singh, J.; Kaur, T.; Singh, N.; Pandey, P.M. Biological and Mechanical Characterization of Biodegradable Carbonyl Iron Powder/Polycaprolactone Composite Material Fabricated Using Three-Dimensional Printing for Cardiovascular Stent Application. Proc Inst Mech Eng H 2020, 234, 975–987. [CrossRef]
- Singh, J.; Singh, G.; Pandey, P.M. Multi-Objective Optimization of Solvent Cast 3D Printing Process Parameters for Fabrication of Biodegradable Composite Stents. International Journal of Advanced Manufacturing Technology 2021, 115, 3945–3964. [CrossRef]
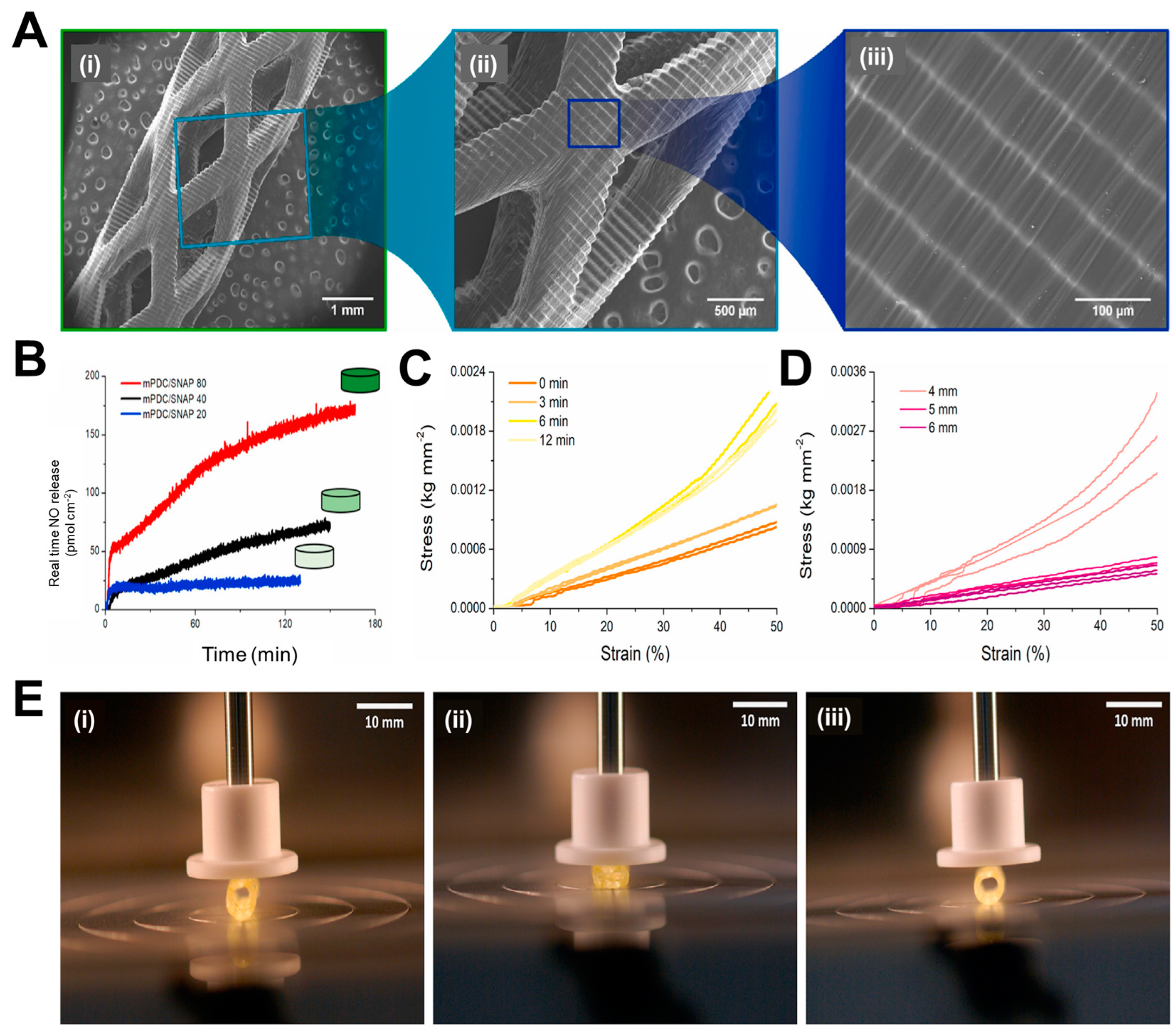
- van Lith, R.; Baker, E.; Ware, H.; Yang, J.; Farsheed, A.C.; Sun, C.; Ameer, G. 3D-Printing Strong High-Resolution Antioxidant Bioresorbable Vascular Stents. Adv Mater Technol 2016, 1, 1–7. [CrossRef]
- Tumbleston, J.R.; Shirvanyants, D.; Ermoshkin, N.; Janusziewicz, R.; Johnson, A.R.; Kelly, D.; Chen, K.; Pinschmidt, R.; Rolland, J.P.; Ermoshkin, A. Continuous Liquid Interface Production of 3D Objects. Science (1979) 2015, 347, 1349–1352. [CrossRef]
- Park, S.A.; Lee, S.J.; Lim, K.S.; Bae, I.H.; Lee, J.H.; Kim, W.D.; Jeong, M.H.; Park, J.K. In Vivo Evaluation and Characterization of a Bio-Absorbable Drug-Coated Stent Fabricated Using a 3D-Printing System. Mater Lett 2015, 141, 355–358. [CrossRef]
- Flege, C.; Vogt, F.; Höges, S.; Jauer, L.; Borinski, M.; Schulte, V.A.; Hoffmann, R.; Poprawe, R.; Meiners, W.; Jobmann, M.; et al. Development and Characterization of a Coronary Polylactic Acid Stent Prototype Generated by Selective Laser Melting. J Mater Sci Mater Med 2013, 24, 241–255. [CrossRef]
- Ware, H.O.T.; Farsheed, A.C.; van Lith, R.; Baker, E.; Ameer, G.; Sun, C. Process Development for High-Resolution 3D-Printing of Bioresorbable Vascular Stents. Advanced Fabrication Technologies for Micro/Nano Optics and Photonics X 2017, 10115, 101150N. [CrossRef]
- de Oliveira, M.F.; da Silva, L.C.E.; de Oliveira, M.G. 3D Printed Bioresorbable Nitric Oxide-Releasing Vascular Stents. Bioprinting 2021, 22, e00137. [CrossRef]
- Napoli, C.; Paolisso, G.; Casamassimi, A.; Al-Omran, M.; Barbieri, M.; Sommese, L.; Infante, T.; Ignarro, L.J. Effects of Nitric Oxide on Cell Proliferation: Novel Insights. J Am Coll Cardiol 2013, 62, 89–95. [CrossRef]
- Rajendran, P.; Rengarajan, T.; Thangavel, J.; Nishigaki, Y.; Sakthisekaran, D.; Sethi, G.; Nishigaki, I. The Vascular Endothelium and Human Diseases. Int J Biol Sci 2013, 9, 1057–1069.
- Xu, J.; Zou, M.-H. Molecular Insights and Therapeutic Targets for Diabetic Endothelial Dysfunction. Circulation 2009, 120, 1266–1286. [CrossRef]
- Böger, R.H. The Pharmacodynamics of L-Arginine. J Nutr 2007, 137, 1650S-1655S. [CrossRef]
- Lei, J.; Vodovotz, Y.; Tzeng, E.; Billiar, T.R. Nitric Oxide, a Protective Molecule in the Cardiovascular System. Nitric Oxide 2013, 35, 175–185. [CrossRef]
- Cha, W.; Meyerhoff, M.E. Catalytic Generation of Nitric Oxide from S-Nitrosothiols Using Immobilized Organoselenium Species. Biomaterials 2007, 28, 19–27. [CrossRef]
- Yang, Z.; Yang, Y.; Xiong, K.; Li, X.; Qi, P.; Tu, Q.; Jing, F.; Weng, Y.; Wang, J.; Huang, N. Nitric Oxide Producing Coating Mimicking Endothelium Function for Multifunctional Vascular Stents. Biomaterials 2015, 63, 80–92. [CrossRef]
- Deux, J.F.; Meddahi-Pellé, A.; Bree, F.; Bataille, I.; Michel, J.B.; Letourneur, D. Comparative Studies on the Mechanisms of Action of Four Polysaccharides on Arterial Restenosis. J Biomater Sci Polym Ed 2009, 20, 689–702. [CrossRef]
- Jean-François, D.; Anne, M.-P.; F., L.B.A.; J., F.L.; Sylvia, C.-J.; Françoise, B.; Frank, B.; Jean-Baptiste, M.; Didier, L. Low Molecular Weight Fucoidan Prevents Neointimal Hyperplasia in Rabbit Iliac Artery In-Stent Restenosis Model. Arterioscler Thromb Vasc Biol 2002, 22, 1604–1609. [CrossRef]
- Kim, J.M.; Bae, I.-H.; Lim, K.S.; Park, J.-K.; Park, D.S.; Lee, S.-Y.; Jang, E.-J.; Ji, M.S.; Sim, D.S.; Hong, Y.J.; et al. A Method for Coating Fucoidan onto Bare Metal Stent and in Vivo Evaluation. Prog Org Coat 2015, 78, 348–356. [CrossRef]
- Roux, N.; Brakenhielm, E.; Freguin-Bouillant, C.; Lallemand, F.; Henry, J.-P.; Boyer, O.; Thuillez, C.; Plissonnier, D. Progenitor Cell Mobilizing Treatments Prevent Experimental Transplant Arteriosclerosis. Journal of Surgical Research 2012, 176, 657–665. [CrossRef]
- Keuren, J.F.W.; Wielders, S.J.H.; Willems, G.M.; Morra, M.; Cahalan, L.; Cahalan, P.; Lindhout, T. Thrombogenicity of Polysaccharide-Coated Surfaces. Biomaterials 2003, 24, 1917–1924. [CrossRef]
- Thalla, P.K.; Fadlallah, H.; Liberelle, B.; Lequoy, P.; De Crescenzo, G.; Merhi, Y.; Lerouge, S. Chondroitin Sulfate Coatings Display Low Platelet but High Endothelial Cell Adhesive Properties Favorable for Vascular Implants. Biomacromolecules 2014, 15, 2512–2520. [CrossRef]
- Stefan, V.; P., M.C.; Y., S.M.; Barbara, W.; B., K.S.; A., R.K.; F., C.N.A.; R., H.S. Reduced Thrombus Formation by Hyaluronic Acid Coating of Endovascular Devices. Arterioscler Thromb Vasc Biol 2000, 20, 1168–1172. [CrossRef]
- Li, G.; Yang, P.; Qin, W.; Maitz, M.F.; Zhou, S.; Huang, N. The Effect of Coimmobilizing Heparin and Fibronectin on Titanium on Hemocompatibility and Endothelialization. Biomaterials 2011, 32, 4691–4703. [CrossRef]
- Boyle, J.P.; Smart, R.H.; Shirey, J.K. Heparin in the Treatment of Chronic Obstructive Bronchopulmonary Disease. American Journal of Cardiology 1964, 14, 25–28. [CrossRef]
- Lee, S.J.; Jo, H.H.; Lim, K.S.; Lim, D.; Lee, S.; Lee, J.H.; Kim, W.D.; Jeong, M.H.; Lim, J.Y.; Kwon, I.K.; et al. Heparin Coating on 3D Printed Poly (l-Lactic Acid) Biodegradable Cardiovascular Stent via Mild Surface Modification Approach for Coronary Artery Implantation. Chemical Engineering Journal 2019, 378, 122116. [CrossRef]
- Liu, Z.; Zheng, Z.; Chen, K.; Li, Y.; Wang, X.; Li, G. A Heparin-Functionalized Woven Stent Graft for Endovascular Exclusion. Colloids Surf B Biointerfaces 2019, 180, 118–126. [CrossRef]
- Luo, C.; Zheng, Y.; Diao, Z.; Qiu, J.; Wang, G. Review: Research Progress and Future Prospects for Promoting Endothelialization on Endovascular Stents and Preventing Restenosis. J Med Biol Eng 2011, 31, 307–316. [CrossRef]
- Wawrzyńska, M.; Duda, M.; Wysokińska, E.; Strządała, L.; Biały, D.; Ulatowska-Jarża, A.; Kałas, W.; Kraszewski, S.; Pasławski, R.; Biernat, P.; et al. Functionalized CD133 Antibody Coated Stent Surface Simultaneously Promotes EPCs Adhesion and Inhibits Smooth Muscle Cell Proliferation–A Novel Approach to Prevent in-Stent Restenosis. Colloids Surf B Biointerfaces 2019, 174, 587–597. [CrossRef]
- Wu, X.; Yin, T.; Tian, J.; Tang, C.; Huang, J.; Zhao, Y.; Zhang, X.; Deng, X.; Fan, Y.; Yu, D.; et al. Distinctive Effects of CD34- and CD133-Specific Antibody-Coated Stents on Re-Endothelialization and in-Stent Restenosis at the Early Phase of Vascular Injury. Regen Biomater 2015, 2, 87–96. [CrossRef]
- Xiao, L.; Wang, G.; Jiang, T.; Tang, C.; Wu, X.; Sun, T. Effects of Shear Stress on the Number and Function of Endothelial Progenitor Cells Adhered to Specific Matrices. Journal of Applied Biomaterials and Biomechanics 2011, 9, 193–198. [CrossRef]
- Chausse, V.; Mas-Moruno, C.; Martin-Gómez, H.; Pino, M.; Díaz-Ricart, M.; Escolar, G.; Ginebra, M.-P.; Pegueroles, M. Functionalization of 3D Printed Polymeric Bioresorbable Stents with a Dual Cell-Adhesive Peptidic Platform Combining RGDS and YIGSR Sequences. Biomater Sci 2023.
- Valadi, H.; Ekström, K.; Bossios, A.; Sjöstrand, M.; Lee, J.J.; Lötvall, J.O. Exosome-Mediated Transfer of MRNAs and MicroRNAs Is a Novel Mechanism of Genetic Exchange between Cells. Nat Cell Biol 2007, 9, 654–659. [CrossRef]
- Hou, Y. chen; Li, J. an; Zhu, S. jie; Cao, C.; Tang, J. nan; Zhang, J. ying; Guan, S. kang Tailoring of Cardiovascular Stent Material Surface by Immobilizing Exosomes for Better Pro-Endothelialization Function. Colloids Surf B Biointerfaces 2020, 189, 110831. [CrossRef]
- Luo, L.; Tang, J.; Nishi, K.; Yan, C.; Dinh, P.-U.; Cores, J.; Kudo, T.; Zhang, J.; Li, T.-S.; Cheng, K. Fabrication of Synthetic Mesenchymal Stem Cells for the Treatment of Acute Myocardial Infarction in Mice. Circ Res 2017, 120, 1768—1775. [CrossRef]
- Gong, M.; Yu, B.; Wang, J.; Wang, Y.; Liu, M.; Paul, C.; Millard, R.W.; Xiao, D.S.; Ashraf, M.; Xu, M. Mesenchymal Stem Cells Release Exosomes That Transfer MiRNAs to Endothelial Cells and Promote Angiogenesis. Oncotarget 2017, 8, 45200–45212. [CrossRef]
| Stent | Manufacturer | Base Material | Strut Thickness (µm) | Drug Name and Conc. (µg/cm2) | Polymer for Drug Coating | Polymer Thickness (µm) | Drug Release | Ref. |
|---|---|---|---|---|---|---|---|---|
|
Cypher (1st Gen) |
Cordis Corporation | SS | 140 | Sirolimus (140) | PEVA and PBMA | 12.6 | 80% | [31,32] |
| Taxus Express (1st Gen) | Boston Scientific Corporation, | SS | 132 | Paclitaxel (100) | SIBS | 16.0 | <10% | [33,34] |
| Taxus Liberté (1st Gen) | Boston Scientific Corporation | SS | 97 | Paclitaxel (100) |
SIBS | 16.0 | <10% | [35,36] |
|
Endeavour (2nd Gen) |
Medtronic | CoCr | 91 | Zotarolimus (100) |
PC | 4.1 | 95% | [12,37,38,39,40] |
|
Xience V (2nd Gen) |
Abbott Laboratories | CoCr | 81 | Everolimus (100) |
PVDF-HFP and PBMA | 7.6 | 80% | [41,42,43,44,45,46] |
| Drug | Description |
|---|---|
| Sirolimus (previously called rapamycin) | Macrolide antibiotic having immunosuppressant functions |
| Zotarolimus | Semisynthetic (made by substituting a tetrazole ring for the native hydroxyl group at position 42 in rapamycin) |
| Everolimus | Synthetic derivative of sirolimus (40-O-[2-hydroxyethyl]-rapamycin) |
| Paclitaxel | Antineoplastic agent |
| Stent | Manufacturer | Base Material | Strut Thickness (µm) |
Drug Name | Polymer for Drug Coating | Resorption Time (Months) |
Ref. |
|---|---|---|---|---|---|---|---|
| ABSORB 1.0 | Abbott Vascular | PLLA | 150 | Everolimus | PDLLA | 24 | [50] |
| ABSORB 1.1 | Abbott Vascular | PLLA | 150 | Everolimus | PDLLA | 24 | [3,51] |
|
DESolve150/ DESolve Nx |
Elixir Medical | PLLA | 150 | Myolimus | PLLA | 12 | [52,53,54] |
| DESolve 100 | Elixir Medical | PLLA | 100 | Novolimus | DESyne BD | - | [55,56] |
| DESolve Cx | Elixir Medical | - | 120 | Novolimus | - | [56] | |
| REVA | Reva Medical Inc. | Tyrosine derived polycarbonate |
200 | None | - | 24 | [54] |
| ReZolve | Reva Medical Inc. | ReZorbTM polymer |
115–230 | Sirolimus | - | 4-6 | [54,57] |
| ReZolve 2 | Reva Medical Inc. | ReZorbTM polymer |
- | Sirolimus | - | - | - |
| Fantom | Reva Medical Inc. | Desaminotyrosine polycarbonate | 125 | Sirolimus | ReZorbTM polymer | - | [58] |
| MeRes | Meril Life Sciences | PLA | >200 | Sirolimus | Non-inflammatory biodegradable polymer | - | [59,60,61] |
| MeRes 100 | Meril Life Sciences | PLLA | 100 | Sirolimus | PDLLA | [60] | |
| FORTITUDE | Amaranth Medical, Inc. | high MW PLLA | 150–200 | Sirolimus | - | 10 | [54,62] |
| APTITUDE | Amaranth Medical, Inc. | Amorphous PLLA | 115 | Sirolimus | - | 3–6 | [63] |
| MAGNITUDE | Amaranth Medical, Inc. | PLLA | <100 | - | - | 24-36 | - |
| XINSORB | Huaan Biotechnology Group Co., Ltd | PLLA | 160 | Sirolimus | PDLLA/PLLA | - | [64,65,66,67] |
|
IDEAL (1st Gen) |
Bioabsorbable Therapeutics Inc. | Poly (anhydride ester) salicylic acid (SA) | 200 | Sirolimus | SA linked with adipic acid |
9–12 | [51] |
|
IDEAL (2nd Gen) |
Xenogenics Corporation | Poly (anhydride ester) salicylic acid (SA) | 175 | Sirolimus | - | >12 | [50,68] |
| Mirage BRMS | Manli Cardiology | PLLA | 125, 150 | Sirolimus | PLA | 14 | [69,70] |
| Igaki-Tamai | Kyoto Medical Planning Co., Ltd | PLLA | 170 | None | - | 24 | [3,71,72] |
| ArterioSorb | Arterius Ltd. | PLLA | 95, 120 | Sirolimus | PDLA | [72] | |
| ART Pure | Arterial Remodelling Technologies Inc. | PLA | - | None | - | 24 | [73,74] |
| ON-AVS | OrbusNeich | PDLA | 150 | Sirolimus and CD34+ | - | >6 | [54,75] |
| Stanza BRS | 480 Biomedical | PLGA | - | - | Polyester/ Poly-urethane elastomer |
12 | [22,76] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





