Tabel of Contents:
1. Introduction
My granddaughter who is 27 years old became severely ill with Long COVID following acute COVID-19 mid December 2022. When I saw her again after some time, I was shocked by her severe pallor. I had never seen anything like it in my 36 years as a general practitioner, and I initially thought of a serious case of anaemia. A few days later she presented blue nail beds which does not support the diagnosis of anaemia, as the blood apparently does not have a shortage of colour. This gave me the idea that flow of blood is squeezed as a response to a shortage of blood.
So the blood does not lack colour, the body does lack blood.
The symptoms of Long COVID present themselves as a form of chronic fatigue syndrome [1]. Decades ago, it was measured that this syndrome is associated with a shortage of blood in the body [9]. Because no good explanation for this blood shortage was found and no effective treatment was developed, this association fell into oblivion.
A chronic shortage of blood in Long COVID patients provides a therapeutic target for a treatment of this condition. Since the invention of aspirin, medical research is mainly focused on molecular enzymatic processes and compounds in the tissues, this has yielded good results, but diseases also take form at a higher level of organs and organ systems, which can also be the focus of therapy.
2. Long Covid pathophysiology: The emergence of the shortage of blood and the stagnation of its recovery
Which cells are prey to the virus?
During the haematogenous spread of the virus in the acute phase of COVID-19, virus particles are rapidly spread via the arteries through the entire body. They adhere to the endothelial cells that form the inner lining of all blood vessels. This adhering particularly occurs in those areas where the speed of the flow of blood is significantly reduced: in the capillaries of all tissues. As a result, many endothelial cells are destroyed in these areas and holes are formed in the blood vessel wall. Platelet activation leads to the formation of clots of erythrocytes and fibrin. Such a capillary is thus completely disabled. This impedes blood flow and, consequently, the function of the tissues and organs, including the haematopoietic organs [6].
Due to the many capillaries being disabled, the total flow capacity of the blood vessel network is greatly reduced, and the normal amount of blood has become too large, relative to this flow capacity. This leads to high pressure in all blood vessels, including the pulmonary artery and pulmonary capillaries. This can lead to pulmonary edema. Such congestion may be a significant contributing factor to the lethal course of acute COVID-19. Therefore, if a patient with acute COVID-19 becomes short of breath: have the patient sit up halfway with the legs as low as possible. The blood that is now superfluous can then sink down into the veins of the legs and thus relieve the pulmonary circulation.
Because the progressive decline in capillary function occurs at a slow enough rate during the initial development of Long COVID, there is enough time for the spleen to break down the now superfluous erythrocytes and to transfer the dangerous potassium and iron ions which are released
in this process to the liver via the hepatic portal vein. (In acute COVID-19, these dangerous breakdown products directly end up in the systemic circulation). Also the red bone marrow reduces the release of red blood cells, and the liver reduces the production of plasma. Old and worn out red blood cells are broken down daily in large quantities, also in healthy individuals. In the case of Long COVID, this breakdown is further increased as the cells are trapped in clots and may become damaged during their passage along damaged endothelial cells. And albumin leaks away through the damaged capillaries. Red blood cells have an average lifespan of approximately 120 days and albumin has a half-time of approximately two weeks.
The production of blood is thus reduced whereas the breakdown of blood continues, and is initially even increased. Finally, a new equilibrium between the production and breakdown of red blood cells and albumin is reached at a lower level with a reduced total blood volume. However, the long COVID patient now has a total volume of blood which is too small to meet the needs of all organs.
The emergency measure of distribution of the remaining blood (see below) impedes the recovery of the total amount of blood because it also causes a reduction in the flow of blood through the liver and the red bone marrow which are responsible for the production of new blood.
After the virus has run its course, the recovery process can begin. The production of new capillaries becomes greater than their loss. This creates space for more blood. The haematopoietic organs can resume their work, erythro- cytes can be released again and albumin production resumes. This leads to an increase in blood.
The spontaneous recovery that slowly starts comes to a halt if either one of these hematopoietic organs does not produce its blood components in pace with the other. If there is not enough plasma, the production of erythrocytes by the red bone marrow halts, and conversely, if there are not enough erythrocytes, the production of plasma by the liver is halted. The organism has to maintain both the albumin and the haematocrit values within the reference range. If the haematocrit drops too far, the oxygen-carrying capacity of the blood flowing through the tissues becomes too low, and if the haematocrit becomes too high, the blood becomes too viscous and its flow is impeded. The albumin level of the plasma regulates the colloidal osmotic pressure of the blood. If the albumin level becomes too low, the colloidal osmotic pressure of the blood decreases, resulting in (micro) oedema in the tissues and in the lungs. This hinders the gas transport of oxygen and carbon dioxide to and from the red blood cells in the tissues and the lungs.
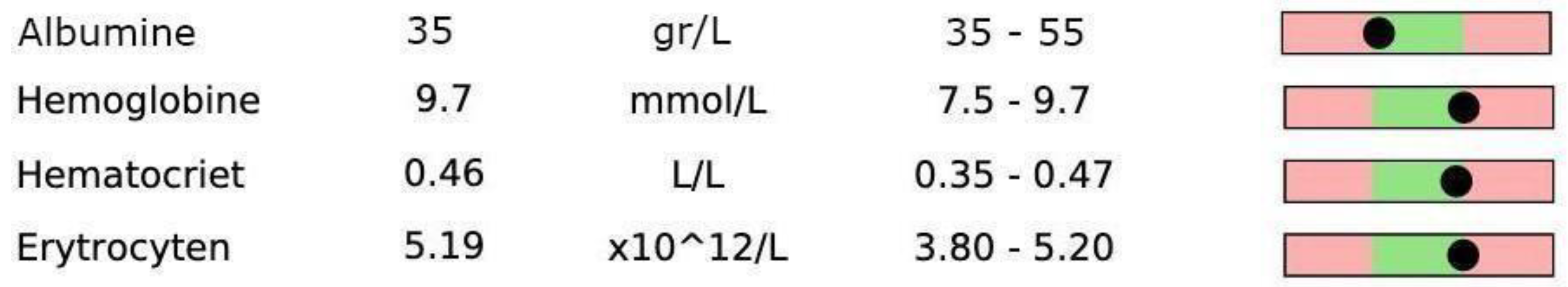
As an example of laboratory blood values with haematocrit at the extreme highest end of the reference ranges and albumin at the lowest end of the reference range, consider those of my granddaughter (
Figure 1).
This situation indicates that the production of albumin cannot keep up with the production of red blood cells. This causes both to stagnate.
If the red bone marrow recovers slightly and releases more red blood cells, the liver will respond by producing more plasma. The total blood volume will then increase again, but this process stops when the liver reaches its still small capacity to produce albumin. The liver is apparently unable to respond sufficiently to an increase in haematocrit, and can keep the amount of albumin at the required level only for a smaller volume of blood, and sometimes even only just with an albumin level in the plasma at the low end.
Due to a colloidal osmotic pressure that is low and is already being challenged by the leakage of albumin from the bloodstream through damaged vessels [2,3], too much tissue fluid is formed, causing the gas and food supply of the tissues, and therefore of the haematopoietic organs as well, to worsen.
An explanation of why the recovery of the liver lags behind the recovery of the red bone marrow is that the liver, in addition to arterial blood, is also perfused with blood from the portal vein coming from the intestinal mucosa, which contains less oxygen, more carbon dioxide and more viral particles [4]. The liver is thus attacked by the virus from two sides: not only from the primary foci in the lungs but also from the secondary foci in the capillaries of the intestinal mucosa. Therefore, the liver has (had) a greater viral load than the bone marrow.
I suspect that we will find a high haematocrit and a low albumin level in most Long COVID patients before the start of the treatment, because the liver cannot keep up with the recovery of the red bone marrow.
3. Long Covid pathophysiology: The consequences of the shortage of blood
In response to the shortage of blood, the vascular system reduces its calibre and decreases its metric volume. This is done by the veins which have to adapt daily to changes in requirements of circulating blood, for example in order to adapt to the differences between lying and standing, and a warm and a cold environment. The buffer capacity of the network of blood vessels lies mainly in the veins, which can shrink without initially increasing their pressure. It is only when the venous buffer capacity has been maximally used that there is not enough blood available to sufficiently perfuse all organs to their requirements at the same time, and a distribution of blood will be necessary. In order to sufficiently perfuse organs that are directly necessary for survival, the body takes the life saving emergency measure of diverting blood from other organs by opening their arteriolovenous anastomoses. Under normal circumstances, an organ autonomously regulates the flow of blood through its capillary networks according to the variable needs of the moment. In the case of a blood shortage, however, the organism as a whole overrides this mechanism.
The organ systems that are directly necessary for immediate survival of the organism need constant perfusion and are therefore spared as much as possible. These include:
The muscles necessary for breathing: the intercostal muscles and the muscles of the diaphragm.
The brainstem, spinal cord, and nerves that control the muscle groups mentioned above.
And of course the arterial blood supply to the heart muscle itself.
The blood flow to the lungs is a separate story because the total amount of blood that flows through the entire body in one minute must also flow through the lungs in its entirety within one minute. For an explanation of dyspnea, see below.
A seriously ill Long COVID patient cannot afford even minimal exertion [5] because the total amount of blood is quickly insufficient to maintain an acceptable level of central circulation. Additionally, there is not enough blood avail- able to clear the metabolic waste products after exertion.
Nearly all signs and symptoms of Long COVID patients can be explained by a shortage of blood and distribution of the remaining blood. As in the case of my granddaughter:
-
A heavy feeling in the arms and legs:
caused by insufficient blood flow to the muscles that require constant perfusion, even at rest, for the maintenance of motor end plates, tendon attachments, and muscle cells.
-
Fatigue and slow recovery after minimal exertion of muscles and brain (brainfog):
caused by inadequate removal of waste products due to insufficient flow of blood.
-
Hypersensitivity to light and sound:
caused by insufficient blood flow to the sensory organs.
-
Pain throughout the entire body:
caused by insufficient blood flow to peripheral nerves.
-
Periods of not being able to move at all:
caused by insufficient blood flow somewhere in the central nervous system.
-
Occasional extreme pallor:
caused by narrowing of the subcutaneous veins. This is a strong indication that the venous blood buffering capacity has been drained as an initial compensation for a shortage of blood.
-
Occasional blue nail beds:
caused by a fluctuating arterial blood flow to the skin.
-
Reduced tolerance to heat:
caused by insufficient blood flow causing a reduced ability to lose heat by radiation or sweating.
-
Dyspnea:
caused by the closing of the arteriolovenous anastomoses in the lungs, which are opened wide in non-affected people, particularly during rest, because there is a continuous supply of blood which is much larger than required for the gas exchange. In non-affected people the blood is directly diverted via the pulmonary veins to the left side of the heart. In the case of Long COVID patients, these anastomoses are closed for a large part, even at rest, in order to move the small supply of blood through the capillary networks of the lungs. The capillary networks in the lungs have also been damaged by the virus. The throughflow capacity of these capillary networks therefore has very little reserve, and the perfusion is also handicapped. If the heart rate increases, this causes a congestion in the pulmonary artery, which results in a feeling of dyspnea. Here, an extremely low arterial blood pressure (80/85 mmHg, in the case of my granddaughter) may also play a role: this is set to such a low level by the body to compensate for the low colloid osmotic pressure to prevent more fluids from leaking out of the blood vessels. In order to maintain a sufficient flow of blood in the case of this low blood pressure, the heart has to beat with many small pulses, so a high pulse rate. In this case even small fluctuations of the pulse rate can have large consequences for the blood pressure. In Long COVID patients, no lung abnormalities are generally found in either x-ray examination or spirometric examination, however, MRI scans do show abnormalities in the perfusion of pulmonary regions [10]. This indicates that capillaries have been disabled. Because of this a congestion of the pulmonary artery can occur.
Research has found small blood clots in the capillary networks of all organs [1]. However, the insufficient circulation can not solely be explained by permanent blockage of the capillaries because the severity of the symptoms varies throughout the day and from hour to hour, such as, in the case of periods of not being able to move at all. These varying symptoms can be explained by a varying blood flow to the associated capillary networks. The change in blood flow to these capillary networks can be regulated in two ways: Firstly in an autonomous manner by the organ itself through the closing and opening of the passage gates between the arterioles and the capillaries, and, secondly by signals from other organ systems that overrule this first mechanism, causing the arterial blood to be directly redirected to the draining veins via the arteriolovenous anastomoses, bypassing the capillary network.
The previously identified inflammation in the brain [7] can also be caused by insufficient perfusion. Blood flow is not only necessary for the supply of nutrients, oxygen and other compounds but also for the removal of protein breakdown products from normal cellular metabolism. The stagnation of this removal can trigger inflammatory processes.
A note on the meaning of serum ferritin levels for iron storage. In research on the blood laboratory values of Long COVID patients it was found that all patients had high serum ferritin levels [8]. This indicates that there is a reduced production of erythrocytes, because under normal circumstances the iron that is released by the breakdown of erythrocytes is immediately used in the production of new erythrocytes. If the production of erythrocytes stagnates, the iron released in the breakdown of erythrocytes is stored in ferritin, particularly in the cells of the liver, and also leads to an increased serum ferritin level.
Measurable symptoms that are characteristic of severely ill:
4. Treatment of Long COVID
The proposed treatment will focus on the recovery of the correct amount of blood in the body. This will also cause an improved perfusion of the red bone marrow and the liver which in turn improves the production of new red blood cells and albumin. By doing so, we break the equilibrium set at too low a level and initiate the healing process.
To initiate the recovery of the correct amount of blood we have at our disposal: donor blood products and red bone marrow stimulating agents. The choice between these is guided by the found blood values of haematocrit, albumin and ferritin. If the therapy is successful, the ferritin levels will decrease.
A trial treatment is easier to implement and less risky for the patient than analysing the total blood volume, which lies far outside daily medical practice, and requires the injection of a radioactive marker. Therefore, a diagnosis ex juvantibus, observing how the patient responds to treatment, is preferred.
This treatment can only take place in a facility that is equipped and qualified for blood transfusion, under the authority of a physician familiar with blood transfusion, such as a haematologist, gastroenterologist or anaesthesiologist.
When performing blood transfusions on Long COVID patients, we pay attention to the following:
The infusion must not be prepared with, at least the patient is not left with, a saline infusion because the colloidal osmotic pressure of the blood may be critically low, and the saline water could then flow directly into the lungs.
The infusion must be administered very slowly and with small amounts per day to allow the osmotic pressure to adjust and because the potentially stiff blood vessels cannot adapt quickly. The entire vascular system needs time to adapt. If it goes too fast, the blood circulation in the lungs will be overloaded.
There must be continuous supervision by a qualified physician or nurse to stop the infusion if the patient becomes short of breath.
The patient is advised to stop taking pain-relieving anti-inflammatory medications at least a week prior to the start of the treatment. These are the COX inhibitors and the prostaglandin inhibitors (such as aspirin, ibuprofen, diclofenac and even paracetamol), because they not only inhibit the dilation of blood vessels but also the growth of new capillaries.
A therapeutic period could consist of ten sessions spread over ten consecutive days (plus any eventual break days).
- -
The treatment is stopped earlier if the patient feels healed.
- -
The well-being of the patient is always the guiding principle.
- -
If symptoms worsen, the following sessions are cancelled.
Prior to each session, haemoglobin, haematocrit, albumin and serum ferritin must be measured. The values found are evaluated with consideration of the patient's stature and sex.
- -
Patients with a low serum ferritin level have to be examined for occult blood loss.
The following is an example treatment for a patient with a high normal value of haematocrit and a low normal value of albumin.
We will start with an infusion of albumin concentrate to address the deficiency in albumin production by the liver.
- -
Dose of albumin concentrate per day: equivalent to 100 mL of plasma (as in a vial of 100 mL with an albumin concentrate of 40 g/L).
- -
Infusion rate: 1 mL per minute.
If the next day the haematocrit level is not on the low side we can continue giving albumin concentrate because the red bone marrow has responded by releasing more red blood cells. If, on the other hand, the haematocrit is on the low side the next day, we wait for one to several days to see if it will rise. Otherwise, a cautious administration of erythropoietin may be considered to stimulate the red bone marrow. If the serum ferritin becomes too low (for example, below 80 micrograms per litre) and the hematocrit does not rise, erythrocyte concentrate or whole blood from a donor may be considered.
Everything based on the clinical picture, the well-being of the patient and the common sense of the doctor.
This treatment proposal does not (yet) claim to be based on clinical evidence but is based on reasoned speculation: the projection of the symptoms of Long Covid onto the structure and functions of the human body.
Selection criteria for the pilot with several patients:
Patients who volunteer for this treatment with general symptoms of Long COVID and the following laboratory blood values:
Counterindication: people with severe heart, lung or blood diseases.
The treatment can eventually be extended to Long COVID patients with haematocrit at the low extreme of the reference range. In this case the treatment should start with erythrocyte concentrate.
Conflicts of Interest
The author of this paper is a family member of the patient described in this report. This relation- ship may influence the author's perspective and interpretation of the case.
References
- Davis, H. E., McCorkell, L., Vogel, J. M., & Topol, E. J. (2023). Long COVID: major findings, mechanisms and recommendations. Nature Reviews Microbiology, 21(3), 133-146. [CrossRef] [PubMed]
- Acharya R., et al. (2021) Low Serum Albumin Predicts Severe Outcomes in COVID-19 Infection: A Single-Cen- ter Retrospective Case-Control Study. J Clin Med Res. 13(5): 258-267. [CrossRef] [PubMed]
- Viana-Llamas, M. C., et al. (2021) Hypoalbuminemia on admission in COVID-19 infection: An early predictor of mortality and adverse events. A retrospective observational study. Medicina clinica, 156(9), 428-436. [CrossRef] [PubMed]
- Natarajan, A., et al. (2022) Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med, 3(6), 371-387. [CrossRef] [PubMed]
- Davis, H. E., et al. (2021) Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38. [CrossRef] [PubMed]
- Dennis, A., et al. (2021). Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ open, 11(3), e048391. [CrossRef] [PubMed]
- Visser D., et al. (2022) Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET. Medrxiv, Jun 04, 2022. [CrossRef]
- Pasini, Evasio, et al. (2021) Serum metabolic profile in patients with long-Covid (PASC) syndrome: clinical implications. Frontiers in Medicine, 8, 714426. [CrossRef] [PubMed]
- Bell, D. On Low Blood Volume in Chronic Fatigue Syndrome. Healthrising.org, Sep 30, 2015.
- Yu, J.Z., et al. (2022) Perfusion disturbances in nonhospitalized post-COVID with dyspnea-A magnetic resonance imaging feasibility study. J Intern Med. 2022 Dec;292(6):941-956. Epub 2022 Aug 26. [CrossRef] [PubMed] [PubMed Central]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).