1. Introduction
Obstructive sleep apnea (OSA) is a common disorder causing daytime sleepiness. In the general population, the prevalence of sleep apnea defined by AHI≥5 has ranged from 9-38 % in men and 1-17 % in women.1,2 It is even more prevalent among professional truck drivers. In recent studies prevalence figures as high as 28-78% have been reported.3–7 Daytime sleepiness increases the risk of traffic accidents. In Finland, driver sleepiness/fatigue is a contributing factor in 17-19% of fatal vehicle accidents.8,9 In 2013 European driving license committees working group estimated that sleep apnea and narcolepsy together cause a relative risk elevation of 271 % (RR = 3.71) for traffic accidents, and most of it is due to sleep apnea.10
OSA is classified as mild, moderate, or severe according to apnea-hypopnea-index (AHI). European Union directives rule to assess daytime sleepiness yearly in professional drivers with at least moderate sleep apnea (AHI≥15). Obstructive sleep apnea syndrome is a treatable condition, e.g., by continuous positive airway pressure (CPAP).11,12 That is why it is important to detect the possibility of OSA in occupational health care. Also, evidence shows that CPAP treatment reduces the risk of motor vehicle accidents. 13,14
Previously different tools for predicting sleep apnea have been described. Some of those require oximetry data,15–17 some require clinical evaluations of anatomy (for example Mallampati score) 18 among them DES-OSA Score. 19 Also automatic detection of OSA by speech signals has been studied.20 Different prediction tools with questionnaires and some measurements, for example neck circumference or systolic blood pressure, but no clinical evaluation, have emerged. Among these are SAS Score, 21 No-Apnea, 22 STOP questionnaire, 23 STOP-Bang,24,25 NoSAS score 26,27 and Four-Variable Screening Tool (Four-V). 28
Of the prediction tools presented before, Berlin Questionnaire, 29–31 a clinical prediction rule presented by Miranda Serrano et al. 32 and Multivariable Apnea Prediction (MAP) Index 33 are more easily accomplished since they include only questions to be answered by the patient and the only measurement is body mass index (BMI).
Also Epworth Sleepiness Scale (ESS) has been suggested to predict the probability of sleep apnea and several studies with different outcomes have been published before. 34,35 However, ESS did not appear to correlate with sleep-disordered breathing (SDB) in women, and prediction value in men was modest at best with an average ESS score of 9,1 for no SDB, and 10,1 for severe SDB. 36 Several studies have compared the accuracy of different predictive tools and also meta-analysis has been done. 37–39
There is still a need for an easy and cheap method to recognize the ones that should undergo sleep studies, especially in occupational health care. In this study we wanted to estimate the usefulness of various screening tools in detecting OSA and to establish a new, simple measure that does not require any clinical examination by a clinician, for screening of OSA.
2. Methods
A structured questionnaire was sent to 2066 professional truck drivers living in Southern Finland as described earlier.7 We selected the subjects from the Finnish Truck Drivers’ (Rahtarit ry) registry. 175 of these drivers had a clinical examination. The sleep studies included cardiorespiratory polygraphy as well as tests of daytime sleepiness, also maintenance of wakefulness test (MWT). Sleep studies were done successfully in 172 drivers. From these drivers we included in this BAMSA study only those, who had complete information so that we could compute also STOP-Bang, NoSAS, ESS and the BERLINscore for everyone. Altogether 160 men remained.
2.1. Questionnaire
Demographic variables, including age, weight, height and neck circumference, were asked. They were measured also during the medical visit. BMI-values were highly correlated (r = 0.9675). The BMI during the visit was a bit higher than BMI derived from the questionnaire (BMI(visit) = 2.36 + 0.913*BMI(questionnaire); R2=0.9386). The correlation of neck circumference (NC) was less good (r=0.733; NC(visit) = 18.47 + 0.548*NC(questionnaire); R2=0.537). We used BMI and neck circumference as they were measured because they were always available. Age at the time of visit was used.
All subjects filled in the questionnaire modified from the Basic Nordic Sleep Questionnaire (BNSQ). 40 In addition, they answered questions about their driving history, sleepiness while driving and other driving related items.
The question on snoring (from the BNSQ) was: “Do you snore while sleeping (ask other people if you are not sure)?” History of subjective sleep apnea (from the BNSQ) was asked as: Have you had breathing pauses (sleep apnea) at sleep (have other people noticed that you have pauses in respiration when you sleep)?
The question on quality of snoring was: “How do you snore (ask other people about the quality of your snoring)?” Response alternatives were: 1) “I don’t snore”, 2) “my snoring sounds regular and it is of low voice”, 3) “it sounds regular but rather loud”, 4) “it sounds regular but it is very loud (other people hear my snoring in the next room)”, 5) “I snore very loudly and intermittently (there are silent breathing pauses when snoring is not heard and at times very loud snorts with gasping”.
The question on witnessed apneas was: “Have you had breathing pauses (sleep apnea) at sleep (have other people noticed that you have pauses in respiration when you sleep)?” Response alternatives were: 1) “never or less than once per month”, 2) “less than once per week”, 3) “on 1-2 nights per week”, 4) “on 3-5 nights per week”, and 5) “every night or almost every night”.
We also asked about daytime fatigue, tiredness and sleepiness. In addition, Epworth Sleepiness Scale was filled by the responders.
2.2. The Berlin Score, STOP-BANG, NoSAS and ESS criteria
The Berlin Questionnaire includes questions of three categories.29 The first one includes questions of snoring and breathing pauses, the second one of tiredness and falling asleep while driving and the third one of high blood pressure and body mass index (BMI). The subject is categorized in high risk group when having at least two positive categories (this means answering positively in two questions of categories one and two, one question in category three or BMI>30).
The 8-item STOP-BANG score was computed. 24 It includes questions of snoring, tiredness, breathing pauses, high blood pressure, BMI, age, sex and neck circumference with the options yes or no and the risk for sleep apnea increases with the higher scores. We have computed the results with older STOP-Bang criteria and also with the new one, which has different neck circumference criteria for male and female. 41
The NoSAS score is one of the previously used screening tools. 26 It ranges from 0 to 17, includes questions on neck circumference, BMI, snoring, sex and age and with 8 points or more the individual is at high risk for OSA.
Epworth Sleepiness Scale (ESS) is also presented to be a possible predictor of OSA. 34 In that questionnaire the subject is asked to evaluate the probability of falling asleep in eight different situations and total score ranges from 0 to 24.
2.3. Design of the BAMSA criteria
First, we computed sensitivity, specificity and the receiver operating characteristic (ROC) for detecting sleep apnea using different screening tools. We used also our empirical experience, since late 1970′s, in diagnosing patients with sleep apnea. We wanted to design a tool that is as simple as possible, yet sensitive and especially specific enough. We also wanted to have a screening tool that is based mainly on anamnestic information using semi-quantitative questions instead of dichotomic yes/no alternatives for occurrence of snoring and occurrence of sleep apnea.40 The reason for this is that almost all humans snore at least sometimes if they are sleeping in supine position and if they have been drinking some alcohol. For this reason, “snoring - yes” differs from “snoring at least on one night per week”. For sleep apnea the cutpoint for “yes” was: having witnessed breathing pauses (apneas) at least on one night per month.
The new BAMSA screening tool consists of 5 questionnaire (interview) items: 1) BMI>30 kgm-2 (no=0, yes=1); 2) Age>50 years (no=0, yes=1); 3) Gender (female=0, Male=1); 4) Snoring at least on one night per week (from the BNSQ; no=0, yes=1); 5) Having had at least sometimes breathing pauses (Apneas) during sleep (BNSQ response >1; no=0, yes=1).
2.4. Clinical examination
All subjects who were monitored in the sleep laboratory underwent a thorough medical examination. Weight and height were measured. The shape of the hard and soft palate was tabulated as well as size and shape of tonsils, tongue, jaw (micrognathia, retrognathia) and bite (overjet, signs of bruxism etc.). The clinician measured the neck and waist circumferences and tabulated the cricomental space in three classes: normal, slightly abnormal and abnormal. Pulse rate and blood pressure were measured and a neurological examination was performed.
2.5. Sleep recordings
All 160 subjects underwent full-night cardiorespiratory polygraphic sleep recordings as described earlier. 7 We recorded nasal airflow and thoracic and abdominal respiratory movements as well as snoring sounds, sleep position, pulse and oxygen saturation. We used a limit of ≥ 4% from pre-event baseline for oxygen desaturations as defined by AASM 1999 Type A definition / AASM 2.2 Criteria 1B for the detection of hypopnea. 42,43 The 1999 rules with the 4% desaturation criteria has been reported to give essentially similar results as the current AASM rules. 43 We categorized the severity of obstructive sleep apnea (OSA) into four groups by apnea-hypopnea index (AHI): AHI <5/h (normal/no sleep apnea), 5≤ AHI <15 (mild), 15≤ AHI <30 (moderate) and AHI≥30 (severe).
2.6. Statistics
We did statistical analyses with the STATA versions 15.1 and 17.0 (StataCorp, USA). We used medians, means, standard deviations (SD) and range to describe distributions. We tested statistical differences between groups using Student’s t-test, Mann-Whitney’s U-test or the Kruskall-Wallis test depending on the number of groups and nature of the distribution. We tested the normality of the distribution by the Shapiro-Wilk test 44. Pearson’s chi-square test was computed from the cross-tabulations. Receiver operating characteristic (ROC) analysis and the area under the curve were computed when applicable. Sensitivity, specificity, positive predictive values (PPV) and negative predictive value (NPV), positive likelihood ratio (LR+) and negative likelihood ratio (LR-) were computed using the .diagt command of STATA. 45 Odds ratios (OR) of a test with a specific cutpoint (LR+/LR-) were computed.
2.7. Ethical considerations
The ethical committee of Helsinki University Hospital approved this study. This study obeyed guidelines and instructions of the Declaration of Helsinki. Every subject fulfilled a written informed consent. All information was strictly confidential and the access to all the data required being an investigator in this study. If moderate or severe sleep apnea was diagnosed, the subjects had the opportunity to give permission to send the data to the public health care to receive the treatment for sleep apnea. The employers of the truck drivers did not get any data.
3. Results
3.1. Characteristics of the drivers
Altogether 160 subjects were men. Their mean age was 42.0 years (SD 9.3, median 41.4, range 20-58). 39 men (24.4%) were over 50 years old. Mean BMI was 28.3 kgm-2 (SD 5.1, median 27.3, range 19.4 – 46.2). 49 men (30.6%) were obese with BMI>30 kgm-2. Mean neck circumference was 41.2 cm (SD 3.1, median 41, range 35-52). 31 men (19.4%) had neck circumference >43 cm. The mean waist circumference was 101.4 cm (SD 15.2; median 99.5 cm, range 67.5-160). In 74 men (46.25%) waist circumference was >100 cm, and it was >110 cm in 36 men (23.1%). 27 men (16.9%) used antihypertensive medication and/or had a diagnosis of arterial hypertension.
Snoring at least on 3 nights per week was reported by 83 men (51.9%) and this also includes habitual, almost every night snoring, which was reported by 70 men (43.75%). 27 men (16.9%) reported that they never snore. Loudness (quality) of snoring associated with frequency of snoring history. All men reporting very loud and intermittent snoring (n=69) snored at least on 3 nights per week. 60 of them (87%) were habitual snorers.
Breathing pauses (apneas) at least sometimes were reported by 86 men (53.75%). Apneas at least on 3 nights per week were reported by 53 men (33.1%) and this also included those 36 men (22.5%) who reported having apneas almost every night. 34 (94.4%) of these 36 men reported snoring almost every night. 74 men (46.3%) reported that they have never had witnessed apneas.
Apnea-hypopnea index (AHI) was ≥ 5 in 70 drivers (43.75%), ≥15 in 17.5% (n=28), and ≥30 in 7.5% (n=12) of these 160 subjects. 53.9% of those snoring at least on three nights per week had AHI≥5. Only one of the drivers without any prior history of snoring had AHI≥30. His BMI was 32.7kg/m2 and he was 57 years old. On the other hand, 33.3% of them had AHI≥5 and 7.4% (n=2) had AHI≥15 (one had AHI=52 and the other had AHI=18). In other words, a simple absence of snoring did not completely exclude severe sleep apnea.
Altogether 33 men (20.6%) reported tiredness on at least three days per week. The mean ESS was 8.7 (SD 3.8, median 9, range 1-19). ESS was >10 in 47 (29.4%) and >15 in 8 (5.0%). 28.6% of those who had AHI≥15 had ESS>10 and 29.6% of those who had AHI<15 had ESS>10. ESS was over 10 points in 31.4% of those who had AHI≥5 and in 27.8% of those who had AHI<5. ESS was on average 8.6 (SD 3.7, median 8) among those who had AHI≥5 and 8.7 (SD 3.8, median 8.5) among those who had AHI<15.
3.2. Performance of different screening tools
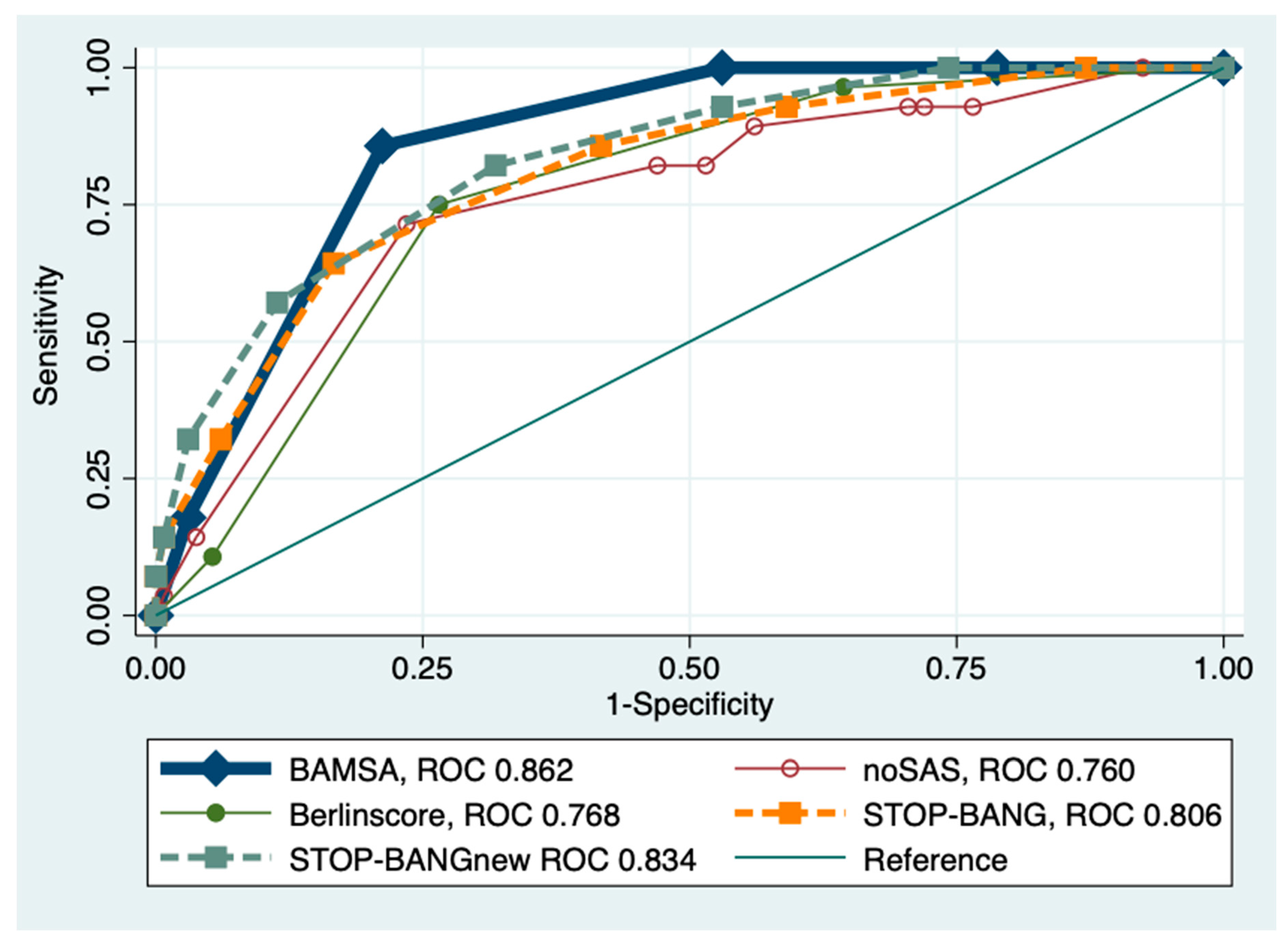
For presence of sleep apnea (AHI≥5) the ROC area for the BERLIN score was 0.660. The ROC area of the original STOP-BANG score was 0.724. The ROC area of the STOP-BANG score with the new neck circumference criteria (STOP-BANGnew) was 0.734. The ROC area for the NoSAS score was 0.698. The ROC area for ESS was 0.524 (for ESS≥11 the ROC area was 0.518). The ROC area of BAMSA for AHI≥5 was 0.741. The results for BAMSA were the best for detecting AHI≥5 (see
Table 1). The ROC area of Epworth sleepiness score was close to 0.5.
For detecting AHI≥15 the sensitivity and specificity of BAMSA with a cutpoint of 3 were 100% and 47%, respectively. With a BAMSA cutpoint of 4 they were 85.7% and 78.8%, respectively (see
Table 2).
Using AHI≥15 the overall ROC area for BAMSA was 0.862. The ROC area of the BAMSA score was statistically significantly better than that of the original STOP-BANG (P=0.085), the Berlin score (P=0.0005), ESS (P<0.0001) and NoSAS (P=0.027). There was no statistically significant difference between BAMSA and the modified STOP-BANGnew score with the new neck circumference criteria (P=0.342) (see
Figure 1).
As all subjects were men, we analyzed the data by excluding gender from the formulas. The ROC areas of the different screening tools did not change. We wanted to keep the male gender in BAMSA questionnaire since it is a known risk factor for sleep apnea and common among professional truck drivers.
4. Discussion
Our aim was to create and validate a screening tool for professional drivers that is easy to use without any contact with the health care. We introduce BAMSA (0 to 5 points), a simple five-question tool that is shown to be at least as sensitive and more specific than the other tested screening tools to detect sleep apnea. It detects mild sleep apnea and especially moderate to severe sleep apnea very well. It includes four questions (no = 0 points, yes = 1 point) and measurement of BMI (> 30 kgm-2 = 1 point), which is easy to measure at home by the subject himself. With this prediction tool it is also easy for a clinician to determine which patients to send for sleep laboratory studies. The ROC area of BAMSA for AHI≥5 was 0.741. BAMSA did even better in detecting moderate and severe sleep apnea and the ROC area of BAMSA for AHI≥15 was 0.862. When using the cutpoint of 4 points, the sensitivity of BAMSA in detecting AHI≥15 was 85.7% and the specificity was 78.8%.
STOP-BANG is one of the best validated and most commonly used screening tools. 24Recently the criteria for STOP-BANG, particularly concerning the neck circumference criteria, have been updated. 41 It inquires about the measurement of neck circumference, and the criteria are different depending on the gender. The scoring of the original 24 and also the new STOP-BANG 41 are somewhat more complicated than the scoring of BAMSA, and it has different options for evaluating the subject in high-risk group. The NoSAS Score 26 includes sex, age, BMI, snoring and neck circumference and it also has a rather complicated scoring system. Berlin Questionnaire is another previously established screening tool, 29 which does not require any measurements but again, the scoring is complicated. Epworth sleepiness scale is a widely used questionnaire to test for subjective daytime sleepiness. It has been suggested to be an option for predicting the risk of sleep apnea, 34 but the results have not been promising. 36 In fact, Lee et al. have suggested that ESS should not be used in clinical settings. 46 Also, in our study ESS performed poorly and its predictive value for sleep apnea was close to tossing a coin.
A screening tool should be sensitive with a good negative predictive value to assure that there are not many false negatives. At the same time, it should be specific enough to avoid high rate of false positive suspicion of sleep apnea – to avoid unnecessary polygraphic sleep recordings, and to avoid causing unnecessary anxiety for the screened subjects. In this study, BAMSA showed a good sensitivity in detecting clinically relevant sleep apnea (AHI≥15), 86.2 % (cutpoint 4) or even 100 % (cutpoint 3). Specificity was also better than that of the other tested prediction tools (tables 1 and 2). This means that not only BAMSA detects almost all of the cases, but it also detects them more accurately than the other prediction tools.
The strengths of our study include the fact that our population of professional truck drivers consisted assumed healthy individuals as well as those with suspected sleep apnea. Our study population is rather large, which is a strength. The evaluation of occurrence of snoring is based on a quantitative time scale instead of purely subjective evaluation. 40 The words such as “sometimes” and “often” may mean different things for different people, while for example “on 3 nights per week” means exactly the same for everybody. Many of the populations presented in previous studies include only the ones that have been addressed to sleep studies with suspected sleep apnea or other sleep disorder. 19,27,47–49 Also, as far as we know, this is the first screening tool to be used in professional drivers.
There are also limitations in our study. Our study population consisted of male truck drivers only. Therefore, our results cannot be generalized neither into female populations nor other populations than professional drivers. We have started to validate BAMSA also in other populations, including women. We can already conclude that BAMSA can be used as a screening tool for clinically significant sleep apnea in male populations. We used respiratory polygraphy instead of full polysomnography, which might have found more subjects with mild sleep apnea. However, we are confident that all subjects with clinically relevant sleep apnea were found.
BAMSA is a valid tool that may be used instead of, or in combination with other screening tools, for example STOP-BANG, in making inferences on prior probability of sleep apnea. Anyway, although BAMSA is working well in male populations, we need larger populations including women and younger subjects before we can conclude that it works well in all clinical settings.
5. Conclusions
In conclusion, we have created a sensitive and specific screening tool for sleep apnea in male professional drivers. BAMSA is easy to use and more simple than the other screening tools established before. BAMSA only consists of five yes or no questions. The cutpoint of 3 seems to be able to find all of the cases and, if using a cutpoint of 4, the specificity is high. Using BAMSA can help find professional male truck drivers that are in risk of having sleep apnea and especially the ones that should be sent to sleep laboratory tests.
Author Contributions
Riikka Huhta: Conceptualization, Funding acquisition, Data curation, Methodology, Formal analysis, Writing - original draft, Writing - review & editing; Mariusz Sieminski: Writing - review & editing; Kari Hirvonen: Conceptualization, Funding acquisition, Data curation, Investigation, Formal analysis, Project administration, Writing - review & editing; Eemil Partinen: Writing - review & editing; Markku Partinen: Supervision, Conceptualization, Funding acquisition, Investigation, Methodology, Data curation, Formal analysis, Project administration, Writing - original draft, Writing - review & editing.
Funding
This study was funded by The Finnish Work Environment Fund “Unikuorma study”. Riikka Huhta has got grants and personal fees from The Finnish Work Environment Fund, grants from Henry Ford Foundation, grants from Maire Taponen Foundation, grants from The Finnish Sleep Research Society, grants from HES, The Research Foundation of the Pulmonary Diseases, grants from The Finnish Traffic Medicine Foundation and grants from Väinö ja Laina Kivi Foundation.
Acknowledgments
We thank all truck drivers that participated in the study. We thank the Rahtarit ry for the collaboration. We thank Anne Huutoniemi and other employees of the Helsinki Sleep Clinic. Parts of the results have been reported earlier in an abstract format in the virtual 25th Congress of the European Sleep Research Society in September 2020 and also in an oral presentation in The 19th Nordic Sleep Conference, organised by the Finnish Sleep Research Society, in May 2021
Conflicts of Interest
Dr. Huhta reports grants and personal fees from The Finnish Work Environment Fund, grants from Henry Ford Foundation, grants from Maire Taponen Foundation, grants from The Finnish Sleep Research Society, grants from HES, The Research Foundation of the Pulmonary Diseases, grants from The Finnish Traffic Medicine Foundation, grants from Väinö ja Laina Kivi Foundation, during the conduct of the study. Dr. Sieminski declare no conflicts of interest. Dr. Hirvonen reports other from Neurotest Tampere Oy, outside the submitted work. Dr. Eemil Partinen declare no conflicts of interest. Dr. Markku Partinen reports grants from Signe and Ane Gyllenberg Foundation, other from Takeda, other from Orion, other from Berlin Cures, other from Teva, outside the submitted work; . Open access funded by Helsinki University Library.
Abbreviations
| AHI |
Apnea-Hypopnea-Index |
| BNSQ |
Basic Nordic Sleep Questionnaire |
| CPAP |
Continuous Positive Airway Pressure |
| ESS |
Epworth Sleepiness Scale |
| LR |
Likelihood Ratio |
| NPV |
Negative Predictive Value |
| NS |
Statistically not Significant |
| OR |
Odds Ratio |
| OSA |
Obstructive Sleep Apnea |
| PPV |
Positive Predictive Value |
| ROC |
Area under the Receiver Operating Curve |
| SDB |
Sleep-Disordered Breathing |
| SENS |
Sensitivity |
| SPEC |
Specificity |
BAMSA
Questionnaire for screening sleep apnea
- 1)
Is your BMI (Body Mass Index) >30 kgm-2?
Yes □ (1point) No □ (0 points)
- 2)
Age: Are you over 50 years old?
Yes □ (1 point) No □ (0 points)
- 3)
What is you gender?
Male □ (1 point) Female □ (0 points)
- 4)
Do you Snore while sleeping (ask other people if you are not sure) at least on one night per week?
Yes □ (1 point) No □ (0 points)
- 5)
Have you had at least sometimes breathing pauses (sleep Apnea) at sleep (or have other people noticed that you have pauses in respiration when you sleep)?
Yes □ (1 point) No □ (0 points)
If you had at least 3 points, your risk of having sleep apnea is elevated.
Copyright® Riikka Huhta, Markku Partinen, Kari Hirvonen, Mariusz Sieminski, Eemil Partinen 15.5.2020
May be used with permission of the authors.
References
- Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 2015, 7, 1311–22. [Google Scholar]
- Senaratna C, V. , Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Stoohs RA, Bingham LA, Itoi A, Guilleminault C, Dement WC. Sleep and sleep-disordered breathing in commercial long-haul truck drivers. Chest. 1995, 107, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Sanchez Armengol A, Cano Gomez S, Capote Gil F, Garcia Diaz E, Carmona Bernal C, Castillo Gomez J. [The detection of the sleep apnea syndrome in a population of professional drivers]. An Med Interna. 1997, 14, 547–553. [Google Scholar]
- Howard ME, Desai A V, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004, 170, 1014–1021. [Google Scholar] [CrossRef]
- Pack AI, Maislin G, Staley B, et al. Impaired performance in commercial drivers: role of sleep apnea and short sleep duration. Am J Respir Crit Care Med. 2006, 174, 446–454. [Google Scholar] [CrossRef]
- Huhta R, Hirvonen K, Partinen M. Prevalence of sleep apnea and daytime sleepiness in professional truck drivers. Sleep Med. 2021, 81, 136–143. [Google Scholar] [CrossRef]
- Partinen M, Sulander P. [Problems with alertness and perception as causes for traffic accidents]. Duodecim. 1999, 115, 709–16. [Google Scholar]
- Partinen, M. Väsymys ja nukahtaminen kuolemaan johtaneissa onnettomuuksissa. VALT. 2004.
- Mcnicholas W, Gilles M, Ms B, Kremer J, De Valck E, Franklin K. New Standards and Guidelines for Drivers with Obstructive Sleep Apnoea syndrome. Brussels; 2013.
- Jing J, Huang T, Cui W, Shen H. Effect on quality of life of continuous positive airway pressure in patients with obstructive sleep apnea syndrome: a meta-analysis. Lung. 2008, 186, 131–144. [Google Scholar] [CrossRef]
- McDaid C, Griffin S, Weatherly H, et al. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess. 2009, 13, iii–iv, xi. [Google Scholar]
- Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006, 2, 193–200. [Google Scholar]
- Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2010, 33, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Magalang UJ, Dmochowski J, Veeramachaneni S, et al. Prediction of the Apnea-Hypopnea Index From Overnight Pulse Oximetry *. Chest. 2003, 124, 1694–1701. [Google Scholar] [CrossRef]
- Poupard L, Philippe C, Goldman MD, Sartène R, Mathieu M. Novel mathematical processing method of nocturnal oximetry for screening patients with suspected sleep apnoea syndrome. Sleep Breath. 2012, 16, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Zou J, Guan J, Yi H, et al. An Effective Model for Screening Obstructive Sleep Apnea: A Large-Scale Diagnostic Study. Arias-Carrion O, ed. PLoS One. 2013, 8, e80704. [Google Scholar]
- Lee RWW, Petocz P, Prvan T, Chan ASL, Grunstein RR, Cistulli PA. Prediction of obstructive sleep apnea with craniofacial photographic analysis. Sleep. 2009, 32, 46–52. [Google Scholar]
- Deflandre E, Degey S, Brichant J-F, Poirrier R, Bonhomme V. Development and Validation of a Morphologic Obstructive Sleep Apnea Prediction Score: The DES-OSA Score. Anesth Analg. 2016, 122, 363–372. [Google Scholar] [CrossRef]
- Goldshtein E, Tarasiuk A, Zigel Y. Automatic Detection of Obstructive Sleep Apnea Using Speech Signals. IEEE Trans Biomed Eng. 2011, 58, 1373–1382. [Google Scholar] [CrossRef]
- Topîrceanu A, Udrescu M, Udrescu L, et al. SAS score: Targeting high-specificity for efficient population-wide monitoring of obstructive sleep apnea. Romigi A, ed. PLoS One. 2018, 13, e0202042. [Google Scholar]
- Duarte RLM, Rabahi MF, Magalhães-da-Silveira FJ, de Oliveira-e-Sá TS, Mello FCQ, Gozal D. Simplifying the Screening of Obstructive Sleep Apnea With a 2-Item Model, No-Apnea: A Cross-Sectional Study. J Clin Sleep Med. 2018, 14, 1097–1107. [Google Scholar] [CrossRef] [PubMed]
- Chung F, Yegneswaran B, Liao P, et al. STOP Questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008, 108, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest. 2016, 149, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012, 108, 768–775. [Google Scholar] [CrossRef]
- Marti-Soler H, Hirotsu C, Marques-Vidal P, et al. The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. Lancet Respir Med. 2016, 4, 742–748. [Google Scholar] [CrossRef]
- Coutinho Costa J, Rebelo-Marques A, Machado JN, et al. Validation of NoSAS (Neck, Obesity, Snoring, Age, Sex) score as a screening tool for obstructive sleep apnea: Analysis in a sleep clinic. Pulmonology. 2019, 25, 263–270. [Google Scholar] [CrossRef]
- Takegami M, Hayashino Y, Chin K, et al. Simple four-variable screening tool for identification of patients with sleep-disordered breathing. Sleep. 2009, 32, 939–48. [Google Scholar]
- Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999, 131, 485–491. [Google Scholar]
- Senaratna C, V. , Perret JL, Matheson MC, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2017, 36, 116–124. [Google Scholar] [CrossRef]
- Tan A, Yin JDC, Tan LWL, van Dam RM, Cheung YY, Lee C-H. Using the Berlin Questionnaire to Predict Obstructive Sleep Apnea in the General Population. J Clin Sleep Med. 2017, 13, 427–432. [Google Scholar] [CrossRef]
- Miranda Serrano E, Lopez-Picado A, Etxagibel A, et al. Derivation and validation of a clinical prediction rule for sleep apnoea syndrome for use in primary care. BJGP Open. 2018, 2, bjgpopen18X101481. [Google Scholar] [CrossRef] [PubMed]
- 33. Lyons MM, Keenan BT, Li J, et al. Symptomless Multi-Variable Apnea Prediction Index Assesses Obstructive Sleep Apnea Risk and Adverse Outcomes in Elective Surgery. Sleep 2017, 40.
- Rosenthal LD, Dolan DC, D Rosenthal L, C Dolan D, Rosenthal LD, Dolan DC. The Epworth sleepiness scale in the identification of obstructive sleep apnea. J Nerv Ment Dis. 2008, 196, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Lee SJ, Kang HW, Lee LH. The relationship between the Epworth Sleepiness Scale and polysomnographic parameters in obstructive sleep apnea patients. Eur Arch Oto-Rhino-Laryngology. 2012, 269, 1143–1147. [Google Scholar] [CrossRef] [PubMed]
- Lipford MC, Wahner-Roedler DL, Welsh GA, Mandrekar J, Thapa P, Olson EJ. Correlation of the Epworth Sleepiness Scale and Sleep-Disordered Breathing in Men and Women. J Clin Sleep Med. 2019, 15, 33–38. [Google Scholar] [CrossRef]
- Chiu H-Y, Chen P-Y, Chuang L-P, et al. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Sleep Med Rev. 2017, 36, 57–70. [Google Scholar] [CrossRef]
- Prasad KT, Sehgal IS, Agarwal R, Nath Aggarwal A, Behera D, Dhooria S. Assessing the likelihood of obstructive sleep apnea: a comparison of nine screening questionnaires. Sleep Breath. 2017, 21, 909–917. [Google Scholar] [CrossRef]
- Amra B, Rahmati B, Soltaninejad F, Feizi A. Screening Questionnaires for Obstructive Sleep Apnea: An Updated Systematic Review. Oman Med J. 2018, 33, 184–192. [Google Scholar] [CrossRef]
- Partinen M, Gislason T. Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res. 1995, 4, 150–155. [Google Scholar] [CrossRef]
- The Official STOP-Bang Questionnaire Website. Available online: http://www.stopbang.ca/osa/screening.php.
- Tsai WH, Flemons WW, Whitelaw WA, Remmers JE. A comparison of apnea-hypopnea indices derived from different definitions of hypopnea. Am J Respir Crit Care Med. 1999, 159, 43–8. [Google Scholar] [CrossRef]
- Duce B, Milosavljevic J, Hukins C. The 2012 AASM Respiratory Event Criteria Increase the Incidence of Hypopneas in an Adult Sleep Center Population. J Clin Sleep Med. 2015, 11, 1425–31. [Google Scholar] [CrossRef] [PubMed]
- Shapiro S, Wilk M. An analysis of variance test for normality (complete samples). Biometrika, Vol 52, No. 3/4. Available online: http://www.jstor.org/discover/10.2307/2333709?uid=3737976&uid=2129&uid=2&uid=70&uid=4&sid=21104540051127.
- (PDF) DIAGT: Stata module to report summary statistics for diagnostic tests compared to true disease status. Available online: https://www.researchgate.net/publication/4794291_DIAGT_Stata_module_to_report_summary_statistics_for_diagnostic_tests_compared_to_true_disease_status.
- 46. Lee JL, Chung Y, Waters E, Vedam H. The Epworth sleepiness scale: Reliably unreliable in a sleep clinic population. J Sleep Res 2020, 29.
- Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu AAL. Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath. 2010, 14, 371–6. [Google Scholar] [CrossRef] [PubMed]
- Yang H, Watach A, Varrasse M, King TS, Sawyer AM. Clinical Trial Enrollment Enrichment in Resource-Constrained Research Environments: Multivariable Apnea Prediction (MAP) Index in SCIP-PA Trial. J Clin Sleep Med. 2018, 14, 173–181. [Google Scholar] [CrossRef]
- Peng M, Chen R, Cheng J, Li J, Liu W, Hong C. Application value of the NoSAS score for screening sleep-disordered breathing. J Thorac Dis. 2018, 10, 4774–4781. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).