Submitted:
30 September 2023
Posted:
01 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
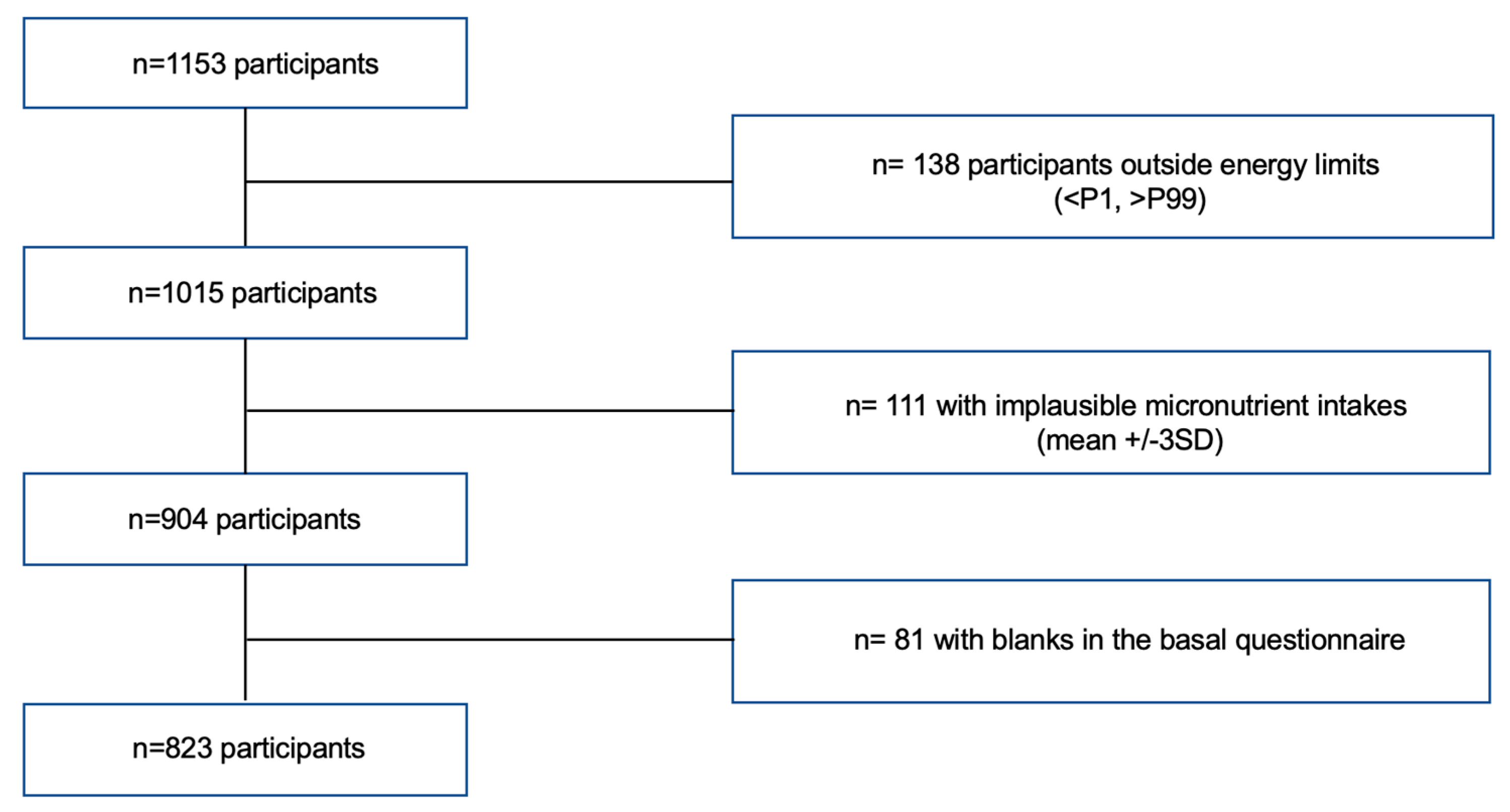
Study Population
Dietary Assessment
Assessment of Covariates
Outcome assessment
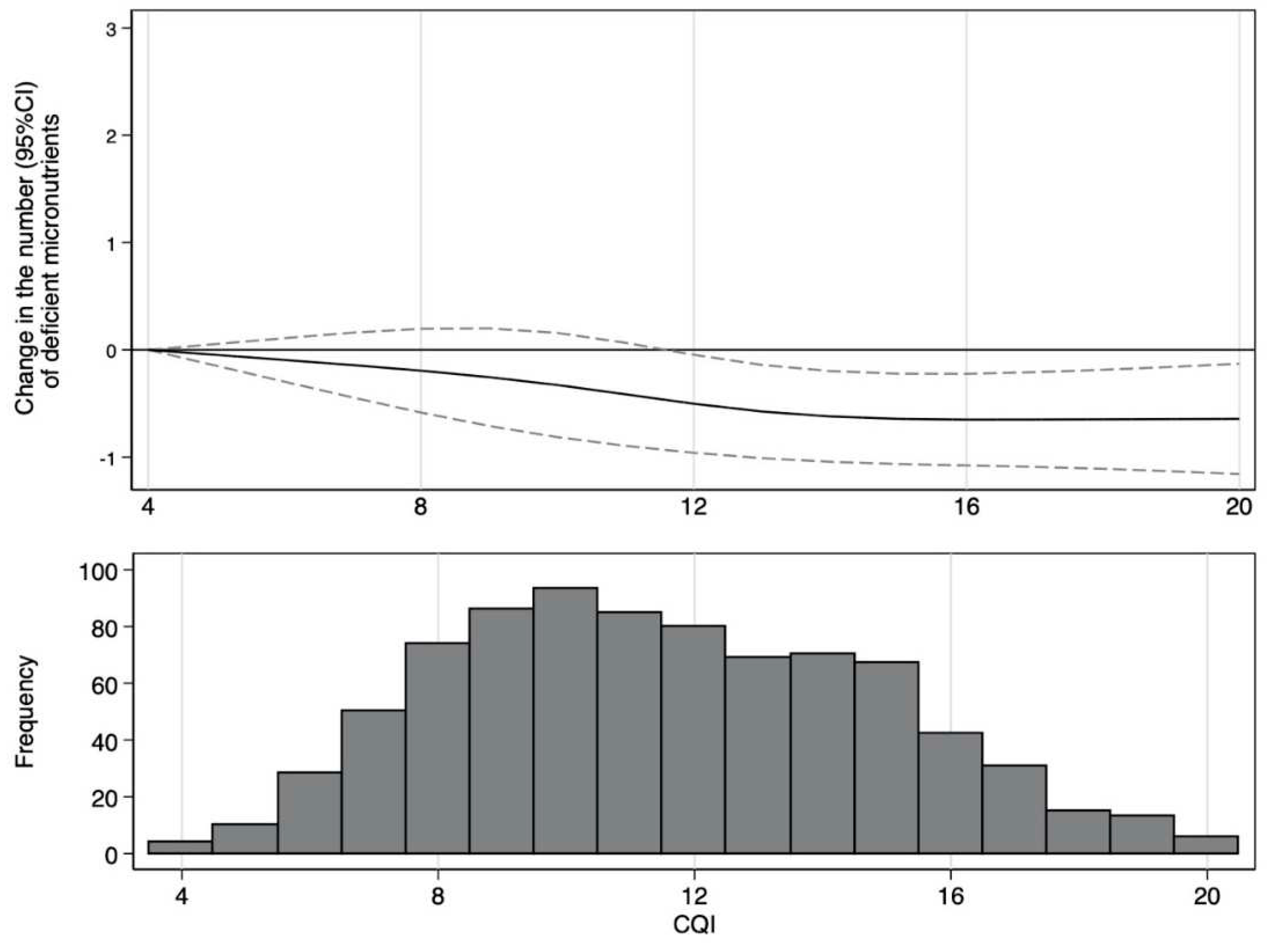
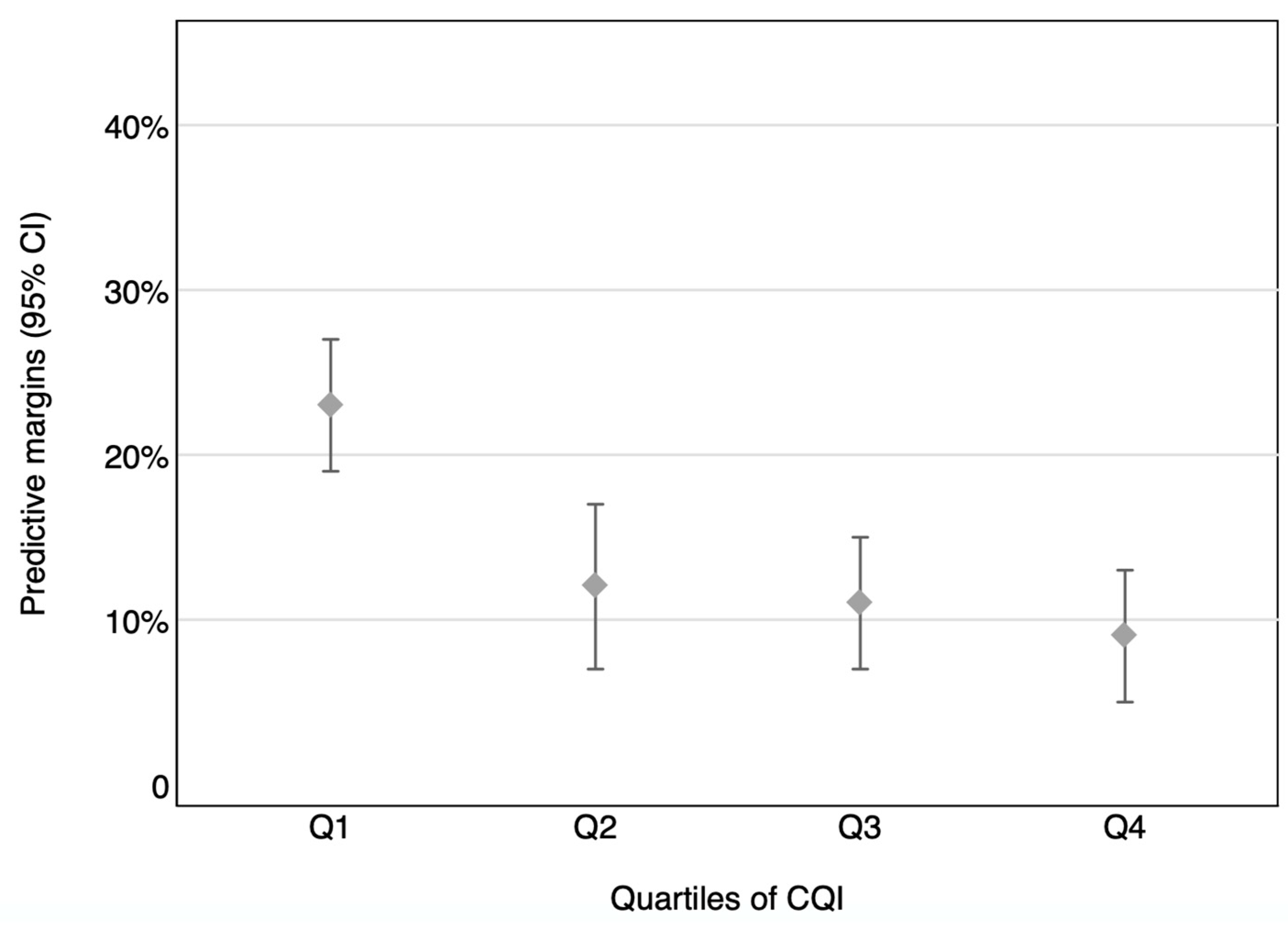
Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gil Hernández Ángel, Sanchez de Medína Contreras Fermín. Tratado de Nutrición. 3rd ed. Gil Hernández Ángel, editor. Vol. 1. España: Editorial Médica Panamericana; 2017. 4 p.
- World Health Organization. Micronutrients [Internet]. 2022 [cited 2022 Jun 25]. Available from: https://www.who.int/health-topics/micronutrients#tab=tab_1.
- Centers for Disease Control and Prevention. Micronutrients Facts [Internet]. U.S. Department of Health & Human Services. 2022 [cited 2022 Jun 25]. Available from: https://www.cdc.gov/nutrition/micronutrient-malnutrition/micronutrients/index.html.
- Kim K, Melough MM, Kim D, Sakaki JR, Lee J, Choi K, et al. Nutritional Adequacy and Diet Quality Are Associated with Standardized Height-for-Age among U.S. Children. Nutrients. 2021 May 16;13(5):1689. [CrossRef]
- Reider CA, Chung RY, Devarshi PP, Grant RW, Hazels Mitmesser S. Inadequacy of Immune Health Nutrients: Intakes in US Adults, the 2005–2016 NHANES. Nutrients. 2020 Jun 10;12(6):1735. [CrossRef]
- UNICEF. The State of the World’s Children 2019. Children, Food and Nutrition: Growing well in a changing world. New York; 2019.
- Kaganov B, Caroli M, Mazur A, Singhal A, Vania A. Suboptimal Micronutrient Intake among Children in Europe. Nutrients. 2015 May 13;7(5):3524–35. [CrossRef]
- Agencia Española de Consumo SA y N. Estudio ENALIA 2012-2014: Encuesta Nacional de consumo de Alimentos en población Infantil y Adolescente. Madrid; 2017.
- USDA ARS. Usual Nutrient Intake from Food and Beverages, by Gender and Age, What We Eat in America, NHANES 2013-2016 [Internet]. 2019 [cited 2022 Jun 16]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/usual/Usual_Intake_gender_WWEIA_2013_2016.pdf.
- Hilger J, Goerig T, Weber P, Hoeft B, Eggersdorfer M, Carvalho N, et al. Micronutrient Intake in Healthy Toddlers: A Multinational Perspective. Nutrients. 2015 Aug 18;7(8):6938–55. [CrossRef]
- Sievenpiper JL. Low-carbohydrate diets and cardiometabolic health: the importance of carbohydrate quality over quantity. Nutr Rev. 2020 Aug 1;78(Supplement_1):69–77. [CrossRef]
- Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe and Asia: A dose–response meta-analysis. Nutrition, Metabolism and Cardiovascular Diseases. 2020 Jun;30(6):853–71. [CrossRef]
- Reynolds A, Mann J, Cummings J, Winter N, Mete E, te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet. 2019 Feb;393(10170):434–45. [CrossRef]
- Willett WC, Liu S. Carbohydrate quality and health: distilling simple truths from complexity. Am J Clin Nutr. 2019 Oct 1;110(4):803–4. [CrossRef]
- AlEssa HB, Cohen R, Malik VS, Adebamowo SN, Rimm EB, Manson JE, et al. Carbohydrate quality and quantity and risk of coronary heart disease among US women and men. Am J Clin Nutr. 2018 Feb 1;107(2):257–67. [CrossRef]
- Hashimoto Y, Tanaka M, Miki A, Kobayashi Y, Wada S, Kuwahata M, et al. Intake of Carbohydrate to Fiber Ratio Is a Useful Marker for Metabolic Syndrome in Patients with Type 2 Diabetes: A Cross-Sectional Study. Ann Nutr Metab. 2018;72(4):329–35. [CrossRef]
- Zazpe I, Sánchez-Taínta A, Santiago S, de la Fuente-Arrillaga C, Bes-Rastrollo M, Martínez JA, et al. Association between dietary carbohydrate intake quality and micronutrient intake adequacy in a Mediterranean cohort: the SUN (Seguimiento Universidad de Navarra) Project. British Journal of Nutrition. 2014 Jun 14;111(11):2000–9. [CrossRef]
- Martínez-González MA, Fernandez-Lazaro CI, Toledo E, Díaz-López A, Corella D, Goday A, et al. Carbohydrate quality changes and concurrent changes in cardiovascular risk factors: a longitudinal analysis in the PREDIMED-Plus randomized trial. Am J Clin Nutr. 2020 Feb 1;111(2):291–306. [CrossRef]
- Santiago S, Zazpe I, Bes-Rastrollo M, Sánchez-Tainta A, Sayón-Orea C, de la Fuente-Arrillaga C, et al. Carbohydrate quality, weight change and incident obesity in a Mediterranean cohort: the SUN Project. Eur J Clin Nutr. 2015 Mar 17;69(3):297–302. [CrossRef]
- Zazpe I, Santiago S, Gea A, Ruiz-Canela M, Carlos S, Bes-Rastrollo M, et al. Association between a dietary carbohydrate index and cardiovascular disease in the SUN (Seguimiento Universidad de Navarra) Project. Nutrition, Metabolism and Cardiovascular Diseases. 2016 Nov;26(11):1048–56. [CrossRef]
- Romanos-Nanclares A, Gea A, Martínez-González MÁ, Zazpe I, Gardeazabal I, Fernandez-Lazaro CI, et al. Carbohydrate quality index and breast cancer risk in a Mediterranean cohort: The SUN project. Clinical Nutrition. 2021 Jan;40(1):137–45.. [CrossRef]
- Sánchez-Tainta A, Zazpe I, Bes-Rastrollo M, Salas-Salvadó J, Bullo M, Sorlí JV, et al. Nutritional adequacy according to carbohydrates and fat quality. Eur J Nutr. 2016 Feb 24;55(1):93–106. [CrossRef]
- Zazpe I, Santiago S, de la O V, Romanos-Nanclares A, Rico-Campà A, Álvarez-zallo N, et al. Validity and reproducibility of a semi-quantitative food frequency questionnaire in Spanish preschoolers — The SENDO project. Nutr Hosp. 2020. [CrossRef]
- Moreiras Tuni Olga, Carbajal Angel. Tablas de composición de alimentos. Madrid: Pirámide; 2019.
- Atkinson FS, Brand-Miller JC, Foster-Powell K, Buyken AE, Goletzke J. International tables of glycemic index and glycemic load values 2021: a systematic review. Am J Clin Nutr. 2021 Nov 8;114(5):1625–32. [CrossRef]
- Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C, Aranceta J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004 Oct;7(7):931-5. PMID: 15482620. [CrossRef]
- Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012 Aug;7(4):284–94. [CrossRef]
- Santiago S, Benítez-Borja A, Martín Calvo N, Romanos-Nanclares A, Moreno-Galarraga L, Zazpe I. Association between parental attitudes towards their offspring's diet and children's actual dietary habits - The SENDO project. Nutr Hosp. 2021 Oct 13;38(5):961-970. English. PMID: 34304576. [CrossRef]
- Romanos-Nanclares A, Zazpe I, Santiago S, Marín L, Rico-Campà A, Martín-Calvo N. Influence of Parental Healthy-Eating Attitudes and Nutritional Knowledge on Nutritional Adequacy and Diet Quality among Preschoolers: The SENDO Project. Nutrients. 2018 Dec 3;10(12):1875. PMID: 30513857; PMCID: PMC6316633. [CrossRef]
- Institute of Medicine Food Nutrition. Dietary reference intakes: applications in dietary assessment [Internet]. Washington DC: National Academy Press; 2000 [cited 2022 Jul 10]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222890/pdf/Bookshelf_NBK222890.pdf.
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate OBV and C. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. National Academies Press (US); 1998.
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for Calcium and Vitamin D. Ross AC TCYA et al., editor. Washington, D.C.: National Academies Press; 2011.
- Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. National Academies Press (US); 2000.
- National Academies of Sciences E and MH and MDF and NBC to R the DRI for S and P. Reference Intakes for Sodium and Potassium. Oria M HMSV, editor. Washington (DC): National Academies Press (US); 2019.
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, D.C.: National Academies Press; 1997.
- Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington (DC): National Academies Press (US); 2001.
- Norton EC, Dowd BE, Maciejewski ML. Marginal Effects-Quantifying the Effect of Changes in Risk Factors in Logistic Regression Models. JAMA. 2019 Apr 2;321(13):1304-1305. PMID: 30848814. [CrossRef]
- VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med. 2017 Aug 15;167(4):268. [CrossRef]
- Libuda L, Alexy U, Buyken AE, Sichert-Hellert W, Stehle P, Kersting M. Consumption of sugar-sweetened beverages and its association with nutrient intakes and diet quality in German children and adolescents. British Journal of Nutrition. 2009 May 16;101(10):1549. [CrossRef]
- Louie JCY, Buyken AE, Brand-Miller JC, Flood VM. The link between dietary glycemic index and nutrient adequacy. Am J Clin Nutr. 2012 Mar 1;95(3):694–702. [CrossRef]
- Sette S, D’Addezio L, Piccinelli R, Hopkins S, le Donne C, Ferrari M, et al. Intakes of whole grain in an Italian sample of children, adolescents and adults. Eur J Nutr. 2017 Mar 20;56(2):521–33. [CrossRef]
- Madrigal C, Soto-Méndez MJ, Hernández-Ruiz Á, Ruiz-López MD, Samaniego-Vaesken ML, Partearroyo T, Varela-Moreiras G, Gil Á. Dietary Intake, Nutritional Adequacy, and Food Sources of Selected Antioxidant Minerals and Vitamins; and Their Relationship with Personal and Family Factors in Spanish Children Aged 1 to <10 Years: Results from the EsNuPI Study. Nutrients. 2022 Oct 5;14(19):4132. PMID: 36235784; PMCID: PMC9573671. [CrossRef]
- Willett W. Nutritional Epidemiology. New York: Oxford University Press; 2012. p.9.
- Willett W. Nutritional Epidemiology. New York: Oxford University Press; 2012. P.86.
- Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013 Aug 1;42(4):1012–4. [CrossRef]
| CQI | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p for trend | |
| N | 252 | 178 | 219 | 174 | |
| Range of CQI | 4 to 9 | 10 to 11 | 12 to 14 | 15 to 20 | |
| Mother’s characteristics | |||||
| Maternal age (years) | 39.58 (4.81) | 39.93 (4.10) | 40.32 (4.19) | 39.86 (4.13) | 0.32 |
| Maternal age (years), % | 0.65 | ||||
| <35 | 33 (13.10) | 16 (8.99) | 23 (10.50) | 24 (13.79) | |
| 35-40 | 107 (42.46) | 74 (41.57) | 80 (36,53) | 64 (36.78) | |
| 40-45 | 81 (32.14) | 67 (37.64) | 92 (42.01) | 69 (39.66) | |
| >45 | 31 (12.30) | 21 (11,80) | 24 (10,96) | 17 (9.77) | |
| Maternal high education, % | 199 (78.97) | 144 (80.90) | 181 (82,65) | 145 (83.33) | 0.20 |
| Number of children, % | <0.001 | ||||
| 1 | 32 (12.70) | 17 (9.55) | 25 (11,42) | 33 (18.97) | |
| 2 | 123 (48.81) | 85 (47.75) | 125 (57.08) | 101 (58.05) | |
| 3-4 | 79 (31.35) | 63 (35.39) | 62 (28.31) | 36 (20.69) | |
| 5 or more | 18 (7.14) | 13 (7.30) | 7 (3.20) | 4 (2.30) | |
| Family of history of obesity, % | 51 (20.40) | 37 (21.02) | 45 (20.64) | 24 (14.04) | 0.16 |
| Parental attitudes towards child’s dietary habits, % | <0.001 | ||||
| Low score (<40%) | 29 (11.51) | 7 (3.93) | 3 (1.37) | 4 (2.30) | |
| Medium score (40-70%) | 116 (46.03) | 60 (33.71) | 62 (28.31) | 30 (17.24) | |
| High score (>70%) | 107 (42.46) | 111 (62.36) | 154 (70.32) | 140 (80.46) | |
| Parental knowledge about the child’s nutritional recommendations, % | <0.001 | ||||
| Low score (<40%) | 71 (28.17) | 50 (28.09) | 41 (18.72) | 24 (13.79) | |
| Medium score (40-70%) | 157 (62.30) | 110 (61.80) | 144 (65.75) | 115 (66.09) | |
| High score (>70%) | 24 (9.52) | 18 (10.11) | 34 (15.53) | 35 (20.11) | |
| Children’s characteristics | |||||
| Sex (female), % | 124 (49.21) | 93 (52.25) | 103 (47.03) | 84 (48.28) | 0.64 |
| Age (years) | 5.08 (0.86) | 5.13 (0.90) | 4.93 (0.82) | 4.83 (0.76) | <0.001 |
| Race (white), % | 242 (96.03) | 171 (96.07) | 216 (99.08) | 165 (94.83) | 0.99 |
| Gestational age (weeks), % | 0.04 | ||||
| <38 | 36 (14.34) | 25 (14.12) | 35 (16.06) | 17 (9.88) | |
| 38 to 40 | 109 (43.43) | 77 (43.50) | 81 (37.16) | 64 (37.21) | |
| >40 | 106 (42.23) | 75 (42.37) | 102 (46.79) | 91 (52.91) | |
| Birthweight (g) | 3216 (568,72) | 3211 (570,72) | 3273 (477,50) | 3250 (475.23) | 0.24 |
| Birthweight (g), % | 0.23 | ||||
| <2500 | 27 (10.76) | 20 (11.30) | 17 (7.80) | 12 (6.98) | |
| 2500-3000 | 59 (23.51) | 35 (19.77) | 43 (19.72) | 39 (22.67) | |
| 3000-3500 | 92 (36.65) | 69 (38.98) | 94 (43.12) | 70 (40.70) | |
| 3500-4000 | 60 (23.90) | 48 (27.12) | 48 (22.02) | 43 (25.00) | |
| >4000 | 13 (5.18) | 5 (2.82) | 16 (7.34) | 8 (4.65) | |
| Breastfeeding duration (months), % | <0.001 | ||||
| No breastfeeding | 49 (19.44) | 37 (20.79) | 34 (15.53) | 17 (9.77) | |
| <6 | 90 (35.71) | 50 (28.09) | 57 (26.03) | 40 (22.99) | |
| 6 to 12 | 64 (25.40) | 48 (26.97) | 58 (26.48) | 42 (24.14) | |
| >12 | 49 (19.44) | 43 (24.16) | 70 (31.96) | 75 (43.10) | |
| Child’s position among siblings, % | 0.09 | ||||
| The oldest/singletons | 70 (27.78) | 69 (38.76) | 87 (39.73) | 72 (41.38) | |
| 2nd/3, 2nd or 3rd/4 | 48 (19.05) | 36 (20.22) | 31 (14.16) | 11 (6.32) | |
| The youngest or beyond the fourth | 134 (53.17) | 73 (41.01) | 101 (46.12) | 91 (52.30) | |
| Z-score of the BMI | 0.18 (1.12) | (-)0.08 (1.14) | 0.12 (1.20) | (-)0.05 (1.10) | 0.16 |
| Nutritional Status, % | 0.08 | ||||
| Low weight | 32 (12.70) | 32 (17.98) | 34 (15.53) | 27 (15.52) | |
| Normal weight | 184 (73.02) | 123 (69.10) | 154 (70.32) | 136 (78.16) | |
| Overweight/obesity | 36 (14.29) | 23 (12.92) | 31 (14.16) | 11 (6.32) | |
| Moderate-vigorous physical activity (h/day) | 1.00 (0.70) | 1.02 (0.72) | 1.21 (0.84) | 1.26 (0.80) | <0.001 |
| Screen time (hours/day) | 1.19 (0.90) | 1.07 (0.89) | 1.14 (1.21) | 0.97 (0.70) | 0.05 |
| CQI | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p for trend | |
| n | 252 | 178 | 219 | 174 | |
| Total energy intake (Kcal/d) | 1923 (445.5) | 2143 (469.9) | 2072 (501.0) | 2042 (436.2) | 0.01 |
| Carbohydrate intake (% of TEI) | 42.84 (4.94) | 42.47 (5.11) | 43.76 (5.31) | 44.60 (5.38) | <0.001 |
| Protein intake (% of total energy) | 17.09 (1.96) | 17.09 (2.40) | 17.20 (2.18) | 16.84 (2.13) | 0.40 |
| Fat intake (% of total energy) | 40.06 (5.00) | 40.44 (5.21) | 39.04 (5.40) | 38.56 (5.33) | <0.001 |
| SFA intake (% of total energy) | 11.73 (2.13) | 11.67 (2.07) | 10.87 (2.04) | 10.28 (2.02) | <0.001 |
| PUFA intake (% of total energy) | 4.72 (1.34) | 4.70 (0.94) | 4.68 (1.03) | 4.64 (1.03) | 0.40 |
| MUFA intake (% of total energy) | 15.25 (3.32) | 15.53 (3.60) | 15.08 (3.56) | 15.46 (3.50) | 0.90 |
| Fibre intake (g/d) | 15.91 (4.19) | 20.21 (3.87) | 22.51 (5.42) | 27.17 (6.10) | <0.001 |
| KIDMED score (p50 (IQR)) | 5 (4-6) | 6 (5-7) | 7 (6-8) | 7 (6-8) | <0.001 |
| Food groups | |||||
| Vegetables (g/d) | 132.1 (79.1) | 192.7 (95.3) | 209.7 (103.8) | 254.2 (116.3) | <0.001 |
| Fruits (g/d) | 266.3 (157.6) | 333.1 (155.0) | 415.9 (216.3) | 516.2 (247.2) | <0.001 |
| Legumes (g/d) | 24.42 (12.55) | 31.51 (13.99) | 22.59 (16.61) | 42.04 (24.93) | <0.001 |
| Dairy (g/d) | 528.5 (235.3) | 518.3 (260.6) | 471.4 (225.2) | 397.3 (225.0) | <0.001 |
| Cereals (g/d) | 77.28 (37.02) | 76.73 (40.67) | 78.41 (41.59) | 74.32 (34.31) | 0.59 |
| Potatoes (g/d) | 14.69 (15.13) | 18.82 (16.93) | 20.38 (24.17) | 21.90 (17.78) | <0.001 |
| Meat (g/d) | 133.43 (42.44) | 146.15 (44.36) | 133.2 (47.17) | 119.2 (46.20) | <0.001 |
| Fish (g/d) | 30.77 (15.06) | 36.18 (17.77) | 36.75 (16.83) | 38.45 (16.38) | <0.001 |
| Nuts (g/d) | 3.08 (4.40) | 4.46 (6.00) | 5.80 (6.53) | 8.98 (11.88) | <0.001 |
| Bakery and sweets (g/d) | 77.32 (44.67) | 95.75 (71.37) | 79.44 (49.02) | 79.44 (49.02) | 0.16 |
| Sugar-sweetened beverages (g/d) | 57.67 (95.31) | 52.24 (66.83) | 37.23 (70.77) | 23.93 (39.29) | <0.001 |
| Fast Food (g/d) | 58.72 (25.69) | 64.72 (28.46) | 59.84 (31.67) | 52.33 (25.32) | 0.01 |
| Eggs (g/d) | 18.24 (11.17) | 19.83 (7.18) | 20.96 (10.90) | 20.26 (7.86) | 0.01 |
| Olive oil (g/d) | 9.96 (11.99) | 13.08 (15.92) | 9.95 (12.40) | 8.21 (11.95) | 0.05 |
| Other fats (g/d) | 3.22 (4.55) | 2.52 (3.67) | 2.48 (3.13) | 2.22 (3.43) | 0.009 |
| CQI | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p for trend | |
| N | 252 | 178 | 219 | 174 | |
| Micronutrients | |||||
| Vitamin A (equiv Retinol) (µg/d) | 922 (26.7) | 1008 (31.7) | 1143 (28.4) | 1255 (31.8) | 0.001 |
| Vitamin C (mg/d) | 106 (3.37) | 124 (4.00) | 155 (3.59) | 184 (4.03) | 0.001 |
| Vitamin D (µg/d) | 2.98 (0.11) | 2.93 (0.13) | 3.27 (0.12) | 3.41 (0.13) | 0.002 |
| Vitamin E (mg/d) | 8.02 (0.17) | 7.83 (0.20) | 8.36 (0.18) | 9.36 (0.20) | 0.001 |
| Vitamin B1 (mg/d) | 1.40 (0.01) | 1.40 (0.02) | 1.47 (0.02) | 1.50 (0.02) | 0.001 |
| Vitamin B2 (mg/d) | 2.03 (0.03) | 2.05 (0.04) | 2.08 (0.03) | 2.02 (0.04) | 0.93 |
| Vitamin B3 (mg/d) | 33.6 (0.47) | 35.6 (0.55) | 36.6 (0.50) | 38.1 (0.55) | 0.001 |
| Vitamin B6 (mg/d) | 2.08 (0.26) | 2.21 (0.03) | 2.37 (0.03) | 2.58 (0.03) | 0.001 |
| Folic Acid (µg/d) | 262 (4.42) | 282 (5.25) | 318 (4.70) | 355 (5.27) | 0.001 |
| Vitamin B12 (µg/d) | 4.63 (0.08) | 4.63 (0.10) | 4.84 (0.88) | 4.60 (0.10) | 0.68 |
| Ca (mg/d) | 1205 (15.8) | 1155 (18.7) | 1165 (16.8) | 1137 (18.8) | 0.01 |
| I (µg/d) | 111 (1.45) | 109 (1.71) | 110 (1.54) | 107 (1.72) | 0.18 |
| Fe (mg/d) | 12.9 (0.12) | 13.6 (0.14) | 14.4 (0.13) | 15.3 (0.14) | 0.001 |
| P (mg/d) | 1667 (40.6) | 1655 (48.2) | 1788 (43.2) | 1841 (48.5) | 0.001 |
| Mg (mg/d) | 269 (2.37) | 289 (2.81) | 310 (2.52) | 341 (2.82) | <0.001 |
| Se (µg/d) | 71.0 (0.83) | 70.4 (0.99) | 73.6 (0.89) | 72.8 (0.99) | 0.03 |
| Zn (mg/d) | 9.02 (0.12) | 9.62 (0.15) | 9.95 (0.13) | 10.07 (0.15) | <0.001 |
| Cr (µg/d) | 62.3 (1.25) | 66.1 (1.49) | 67.0 (1.33) | 74.7 (1.50) | <0.001 |
| K (mg/d) | 3073 (34.4) | 3278 (40.8) | 3542 (36.6) | 3848 (41.0) | <0.001 |
| Na (mg/d) | 3060 (53.2) | 2994 (56.7) | 2886 (63.5) | 2886 (63.5) | 0.01 |
| CQI | p for trend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| n | 252 | 178 | 219 | 174 | |
| Crude | 1.00 (ref) | 0.29 (0.16-0.51) | 0.29 (0.17-0.51) | 0.27 (0.15-0.48) | <0.001 |
| Multivariate adjusted model 1 | 1.00 (ref) | 0.34 (0.17-0.67) | 0.30 (0.16-0.54) | 0.24 (0.12-0.48) | <0.001 |
| Multivariate adjusted model 2 | 1.00 (ref) | 0.33 (0.16-0.67) | 0.29 (0.15-0.54) | 0.22 (0.11-0.47) | <0.001 |
| Multivariate adjusted model 3 | 1.00 (ref) | 0.33 (0.16-0.66) | 0.28 (0.15-0.54) | 0.22 (0.10-0.48) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





