Submitted:
01 October 2023
Posted:
02 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
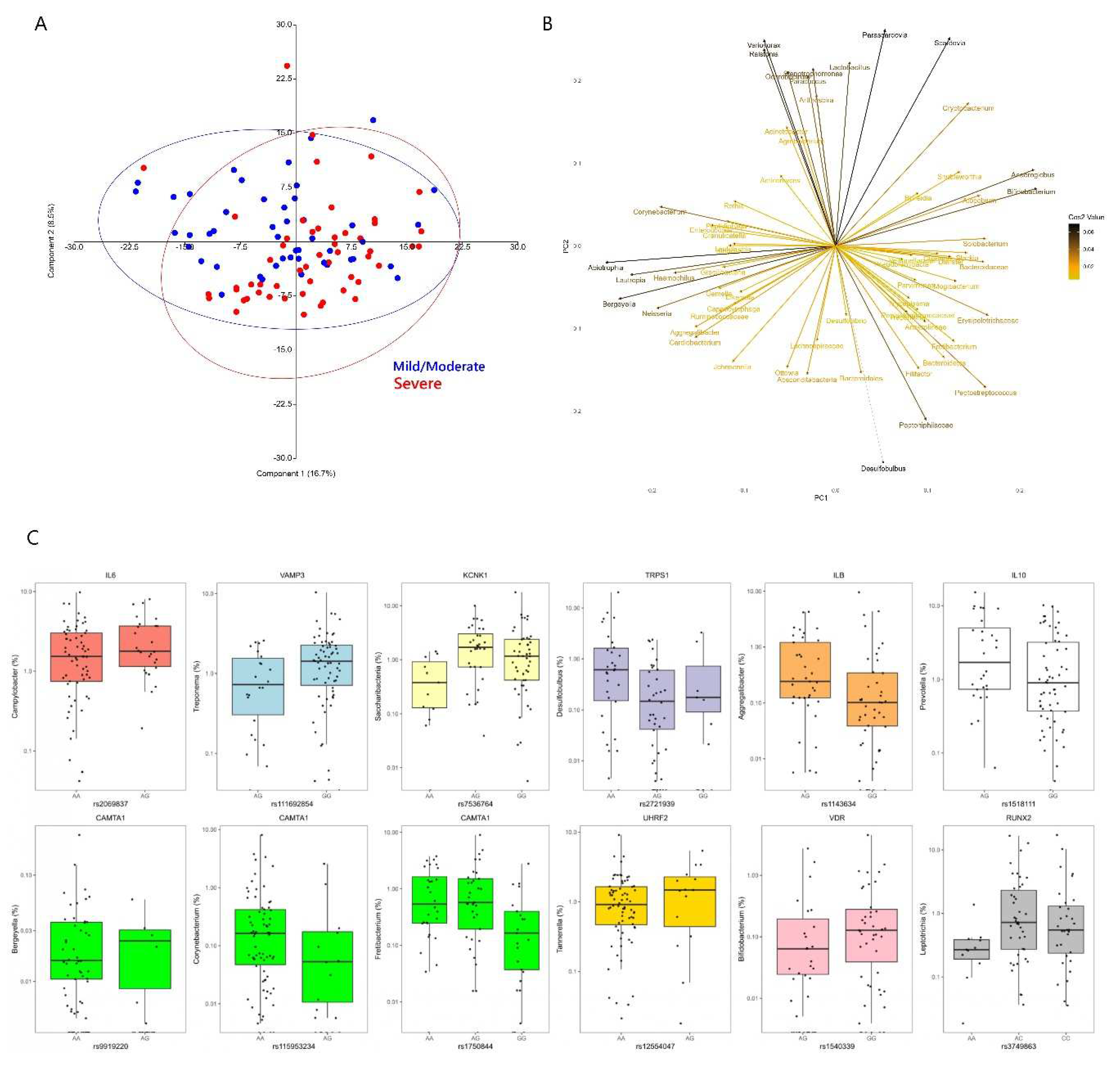
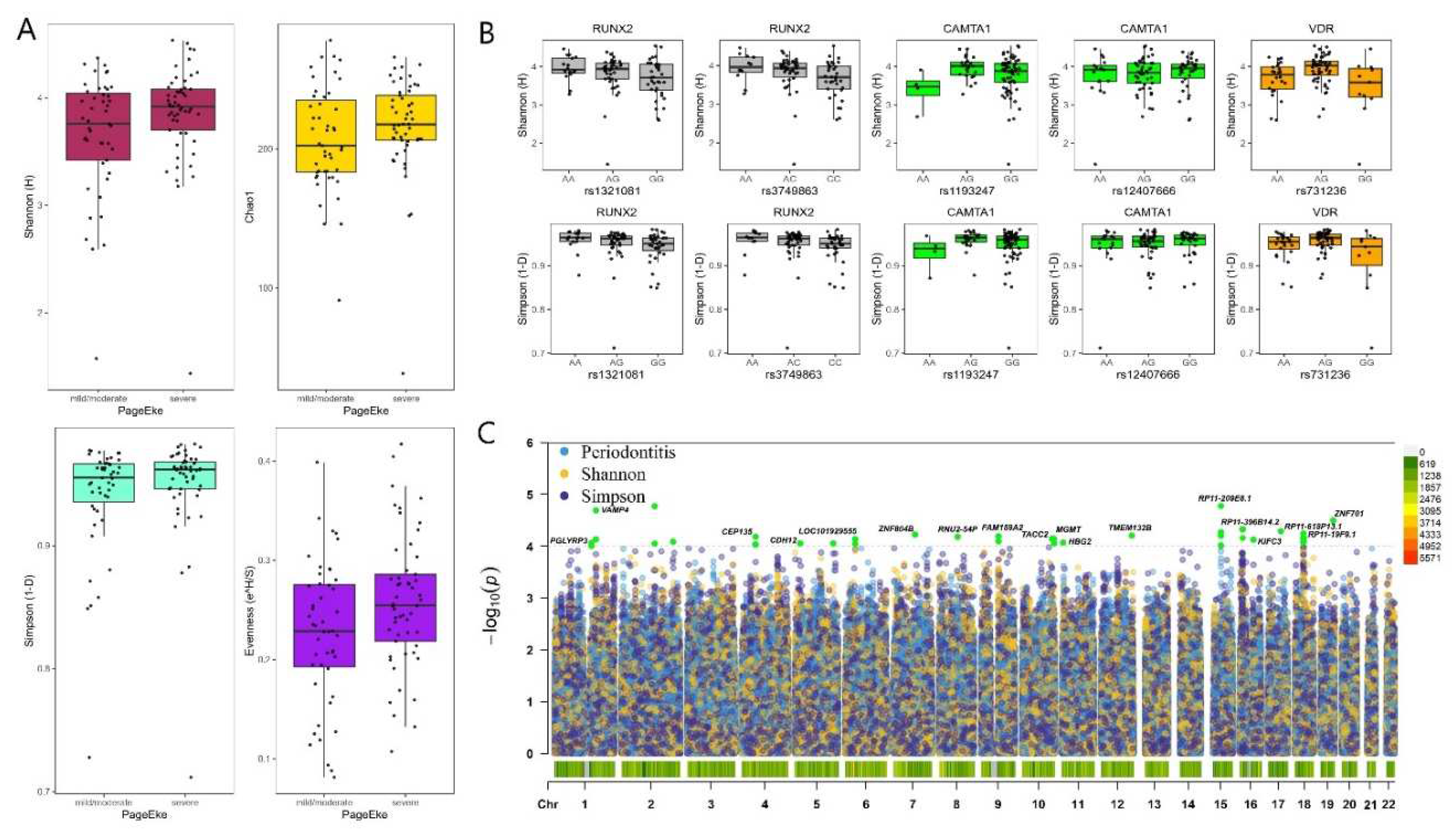
2.1. Microbial diversity and metabolic syndrome
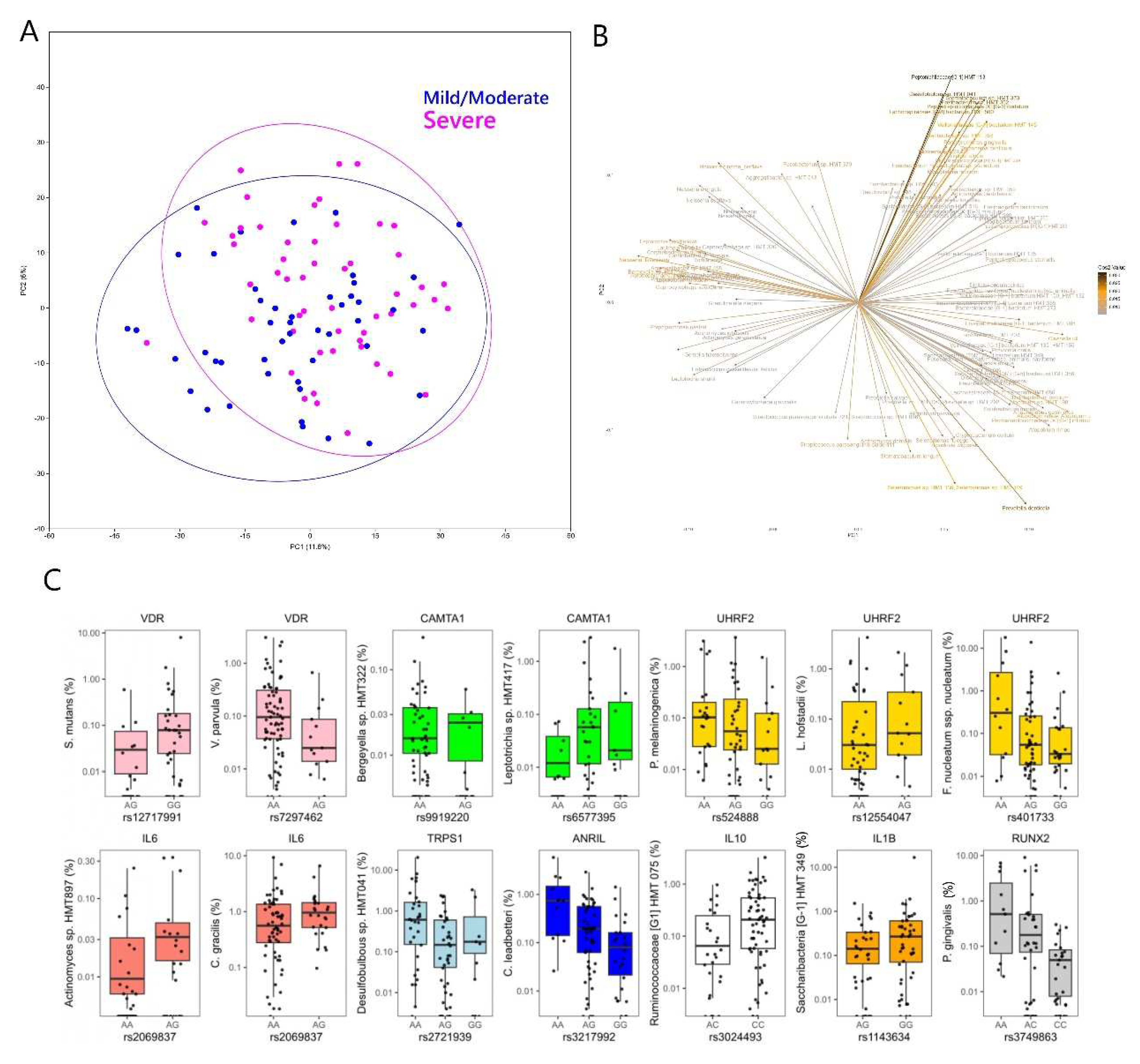
2.2. Genotype associations with microbial taxa
2.2.1. Genotype associations at the Genus level
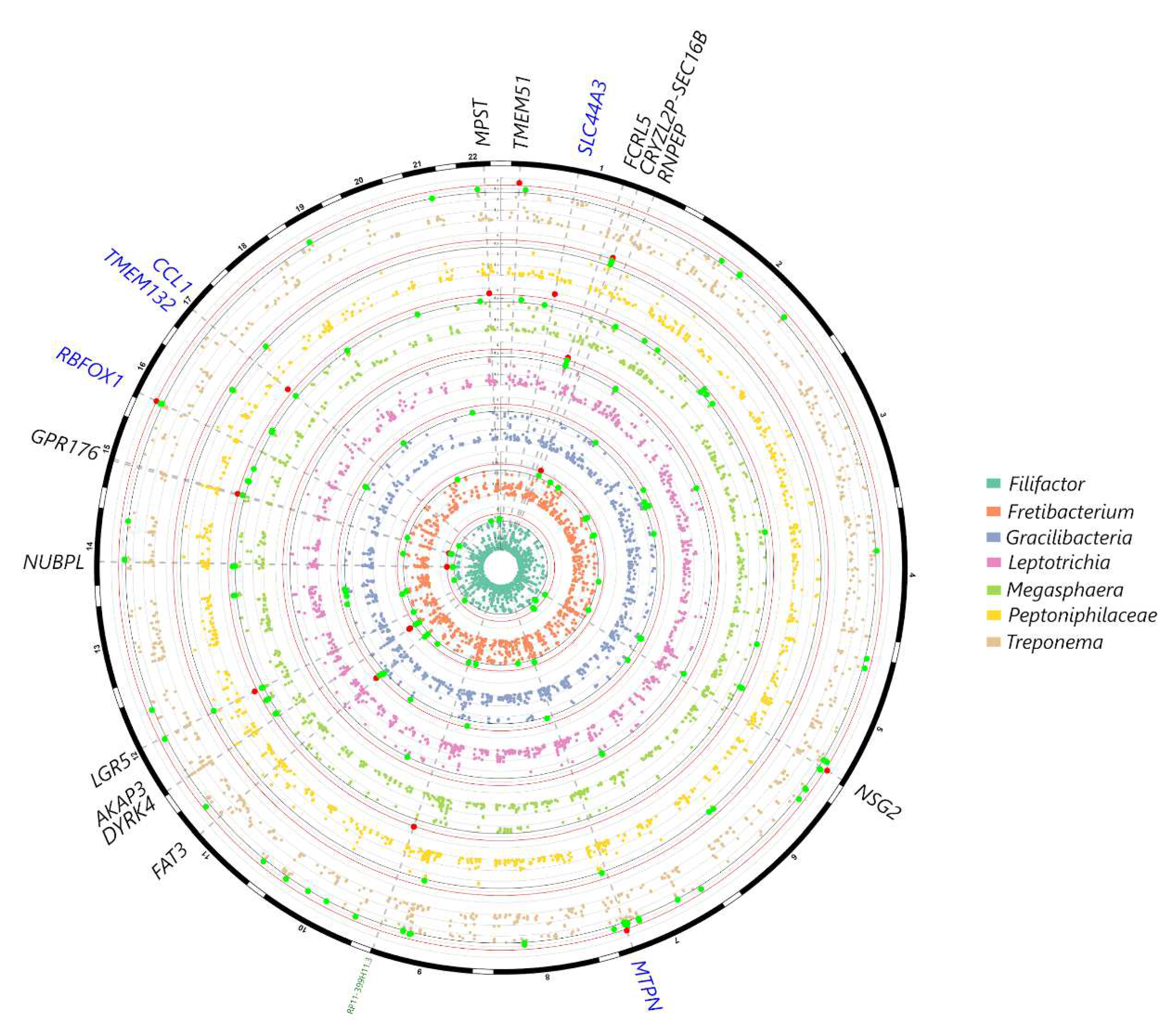
2.2.2. Genotype associations at the Species level

3. Discussion
4. Materials and Methods
4.1. Study population
- Caucasian ethnicity;
- Age 25- 75;
- Diagnosis of metabolic syndrome as defined by the revised NCEP ATP III (e.g. the presence of at least 3 of the following factors)[47]:
- 1.
- Waist circumference > 102 cm for men and > 88 cm for women;
- 2.
- High triglycerides: ≥ 150 mg/dL (1.7 mmol/L), or specific treatment for this lipid abnormality;
- 3.
- Low HDL cholesterol: < 40 mg/dL (1.03 mmol/L) in males, < 50 mg/dL (1.29 mmol/L) in females, or specific treatment for this lipid abnormality;
- 4.
- High blood pressure: systolic BP ≥ 130 or diastolic BP ≥85 mm Hg, or treatment of previously diagnosed hypertension;
- 5.
- High fasting plasma glucose: FPG ≥100 mg/dL (5.6 mmol/L), or previously diagnosed type 2 diabetes.
- Presence of at least 12 teeth.
- Pregnancy;
- Presence of infectious diseases such as hepatitis and HIV;
- Antibiotic pre-medication required for the performance of periodontal examination;
- Previous periodontal therapy within 6 months of the study visit.
4.2. Medical assessment and sampling
- healthy/mild periodontitis: < 2 sites on different teeth with CAL ≥ 4 mm or no sites with PPD ≥ 4 mm;
- moderate periodontitis: ≥ 2 sites on different teeth with CAL ≥ 4 mm or one site with PPD ≥ 4 mm;
- severe periodontitis: ≥ 2 sites on different teeth with CAL ≥ 6 mm and ≥ 1 site with PPD ≥ 4 mm.
4.3. Genotyping, Imputation and Genome-wide association analysis
4.4. Microbiome Profiling
4.5. Statistical analysis/power calculation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kellam, P.; Weiss, R. A. Infectogenomics: insights from the host genome into infectious diseases. Cell 2006 124(4), 695–697. [CrossRef]
- Nibali, L.; Henderson, B.; Sadiq, S. T.; Donos, N. Genetic dysbiosis: the role of microbial insults in chronic inflammatory diseases. Journal of oral microbiology 2014 6, 10.3402/jom.v6.22962. [CrossRef]
- Zoheir, N.; Kurushima, Y.; Lin, G. H.; Nibali, L. Periodontal infectogenomics: a systematic review update of associations between host genetic variants and subgingival microbial detection. Clinical oral investigations 2022 26(3), 2209–2221. [CrossRef]
- Hajishengallis, G.; Lamont, R. J. Beyond the red complex and into more complexity: the polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Molecular oral microbiology 2012 27(6), 409–419. [CrossRef]
- Socransky, S. S.; Haffajee, A. D. Periodontal microbial ecology. Periodontology 2000 2005 38, 135–187. [CrossRef]
- Nibali, L.; Ready, D. R.; Parkar, M.; Brett, P. M.; Wilson, M.; Tonetti, M. S.; Griffiths, G. S. Gene polymorphisms and the prevalence of key periodontal pathogens. Journal of dental research 2007 86(5), 416–420. [CrossRef]
- Nibali, L.; Donos, N.; Brett, P. M.; Parkar, M.; Ellinas, T.; Llorente, M.; Griffiths, G. S. A familial analysis of aggressive periodontitis - clinical and genetic findings. Journal of periodontal research 2008 43(6), 627–634. [CrossRef]
- Nibali, L.; Pometti, D.; Tu, Y. K.; Donos, N. Clinical and radiographic outcomes following non-surgical therapy of periodontal infrabony defects: a retrospective study. Journal of clinical periodontology 2011 38(1), 50–57. [CrossRef]
- Divaris, K.; Monda, K. L.; North, K. E.; Olshan, A. F.; Reynolds, L. M.; Hsueh, W. C.; Lange, E. M.; Moss, K.; Barros, S. P.; Weyant, R. J. et al. Exploring the genetic basis of chronic periodontitis: a genome-wide association study. Human molecular genetics 2013 22(11), 2312–2324. [CrossRef]
- Ye, Y.; Carlsson, G.; Wondimu, B.; Fahlén, A.; Karlsson-Sjöberg, J.; Andersson, M.; Engstrand, L.; Yucel-Lindberg, T.; Modéer, T.; Pütsep, K. Mutations in the ELANE gene are associated with development of periodontitis in patients with severe congenital neutropenia. Journal of clinical immunology 2011 31(6), 936–945. [CrossRef]
- Zhang, S.; Yu, N.; Arce, R. M. Periodontal inflammation: Integrating genes and dysbiosis. Periodontology 2000 2020 82(1), 129–142. [CrossRef]
- Nibali, L.; Sousa, V.; Davrandi, M.; Liu, L. S.; Spratt, D.; Donos, N. Patterns of subgingival microbiota in different periodontal phenotypes. Journal of dentistry 2022 117, 103912. [CrossRef]
- Nibali, L.; Donos, N.; Terranova, V.; Di Pino, A.; Di Marca, S.; Ferrara, V.; Pisano, M.; Scicali, R.; Rabuazzo, A. M.; Purrello, F.; Malatino, L. Left ventricular geometry and periodontitis in patients with the metabolic syndrome. Clinical oral investigations 2019 23(6), 2695–2703. [CrossRef]
- Zanoli, L.; Ozturk, K.; Cappello, M.; Inserra, G.; Geraci, G.; Tuttolomondo, A.; Torres, D.; Pinto, A.; Duminuco, A.; Riguccio, G. et al. Inflammation and Aortic Pulse Wave Velocity: A Multicenter Longitudinal Study in Patients With Inflammatory Bowel Disease. J Am Heart Assoc. 2019 8(3), e010942. [CrossRef]
- Nibali, L.; Tatarakis, N.; Needleman, I.; Tu, Y. K.; D'Aiuto, F.; Rizzo, M.; Donos, N. Clinical review: Association between metabolic syndrome and periodontitis: a systematic review and meta-analysis. The Journal of clinical endocrinology and metabolism 2013 98(3), 913–920. [CrossRef]
- Lourenςo, T. G. B.; Spencer, S. J.; Alm, E. J.; Colombo, A. P. V. Defining the gut microbiota in individuals with periodontal diseases: an exploratory study. Journal of oral microbiology 2018 10(1), 1487741. [CrossRef]
- Olsen, I.; Yamazaki, K. Can oral bacteria affect the microbiome of the gut? Journal of oral microbiology, 2019 11(1), 1586422. [CrossRef]
- Page, R. C.; Eke, P. I. Case definitions for use in population-based surveillance of periodontitis. Journal of periodontology 2007 78(7 Suppl), 1387–1399. [CrossRef]
- Tu, Y.; Ling, X.; Chen, Y.; Wang, Y;, Zhou, N.; Chen, H. Effect of S. Mutans and S. Sanguinis on Growth and Adhesion of P. Gingivalis and Their Ability to Adhere to Different Dental Materials. Medical science monitor: international medical journal of experimental and clinical research 2017 23, 4539–5445. [CrossRef]
- Luppens, S. B.; Kara, D.; Bandounas, L.; Jonker, M. J.; Wittink, F. R.; Bruning, O.; Breit, T. M.; Ten Cate, J. M.; Crielaard, W. Effect of Veillonella parvula on the antimicrobial resistance and gene expression of Streptococcus mutans grown in a dual-species biofilm. Oral microbiology and immunology 2008 23(3), 183–189. [CrossRef]
- Liu, S.; Chen, M.; Wang, Y.; Zhou, X.; Peng, X.; Ren, B.; Li, M.; Cheng, L. Effect of Veillonella parvula on the physiological activity of Streptococcus mutans. Archives of oral biology 2020 109, 104578. [CrossRef]
- Van Dyke, T. E.; Bartold, P. M.; Reynolds, E. C. The Nexus Between Periodontal Inflammation and Dysbiosis. Frontiers in immunology 2020 11, 511. [CrossRef]
- Kurushima, Y.; Wells, P. M.; Bowyer, R. C. E.; Zoheir, N.; Doran, S.; Richardson, J. P.; Sprockett, D. D.; Relman, D. A.; Steves, C. J.; Nibali, L. Host Genotype Links to Salivary and Gut Microbiota by Periodontal Status. Journal of dental research 2023 102(2), 146–156. [CrossRef]
- Torrungruang, K.; Chantarangsu, S.; Sura, T.; Thienpramuk, L. Interplay between vitamin D receptor FokI polymorphism and smoking influences Porphyromonas gingivalis proportions in subgingival plaque. Journal of clinical periodontology 2020 47(8), 912–920. [CrossRef]
- Nibali, L.; Madden, I.; Franch Chillida, F.; Heitz-Mayfield, L.; Brett, P.; Donos, N. IL6 -174 genotype associated with Aggregatibacter actinomycetemcomitans in Indians. Oral diseases 2011 17(2), 232–237. [CrossRef]
- Schaefer, A. S.; Bochenek, G.; Jochens, A.; Ellinghaus, D.; Dommisch, H.; Güzeldemir-Akçakanat, E.; Graetz, C.; Harks, I.; Jockel-Schneider, Y.; Weinspach, K. et al. Genetic evidence for PLASMINOGEN as a shared genetic risk factor of coronary artery disease and periodontitis. Circulation. Cardiovascular genetics 2005 8(1), 159–167. [CrossRef]
- Aarabi, G.; Zeller, T.; Seedorf, H.; Reissmann, D. R.; Heydecke, G.; Schaefer, A. S.; Seedorf, U. Genetic Susceptibility Contributing to Periodontal and Cardiovascular Disease. Journal of dental research 2017 96(6), 610–617. [CrossRef]
- Li, N.; Li, Y.; Hu, J.; Wu, Y.; Yang, J.; Fan, H.; Li, L.; Luo, D.; Ye, Y.; Gao, Y.; Xu, H.; Hai, W.; Jiang, L. A Link Between Mitochondrial Dysfunction and the Immune Microenvironment of Salivary Glands in Primary Sjogren's Syndrome. Frontiers in immunology 2022 13, 845209. [CrossRef]
- Xie, H.; Hong, J.; Sharma, A.; Wang, B. Y. Streptococcus cristatus ArcA interferes with Porphyromonas gingivalis pathogenicity in mice. Journal of periodontal research 2012 47(5), 578–583. [CrossRef]
- Ho, MH.; Lamont, R.J.; Xie, H. Identification of Streptococcus cristatus peptides that repress expression of virulence genes in Porphyromonas gingivalis . Sci Rep 2017 7, 1413. [CrossRef]
- Karched, M.; Bhardwaj, R.G.; Asikainen, S.E. Coaggregation and biofilm growth of Granulicatella spp. with Fusobacterium nucleatum and Aggregatibacter actinomycetemcomitans BMC Microbiol 2015 15, 114. [CrossRef]
- Haffajee, A. D.; Socransky, S. S.; Smith, C.; Dibart, S. Relation of baseline microbial parameters to future periodontal attachment loss. Journal of clinical periodontology 1991 18(10), 744–750. [CrossRef]
- Haffajee, A. D.; Socransky, S. S.; Dibart, S.; Kent, R. L., Jr.Response to periodontal therapy in patients with high or low levels of P. gingivalis, P. intermedia, P. nigrescens and B. forsythus. Journal of clinical periodontology 1996 23(4), 336–345. [CrossRef]
- Socransky, S. S.; Haffajee, A. D.; Cugini, M. A.; Smith, C.; Kent, R. L., Jr. Microbial complexes in subgingival plaque. Journal of clinical periodontology 1998 25(2), 134–144. [CrossRef]
- Oliveira, R. R.; Fermiano, D.; Feres, M.; Figueiredo, L. C.; Teles, F. R.; Soares, G. M.; Faveri, M. Levels of Candidate Periodontal Pathogens in Subgingival Biofilm. Journal of dental research 2016 95(6), 711–718. [CrossRef]
- Ghayoumi, N.; Chen, C.; Slots, J. Dialister pneumosintes, a new putative periodontal pathogen. Journal of periodontal research 2002 37(1), 75–78. [CrossRef]
- Aruni, A. W.; Mishra, A.; Dou, Y.; Chioma, O.; Hamilton, B. N.; Fletcher, H. M.Filifactor alocis--a new emerging periodontal pathogen. Microbes and infection 2015 17(7), 517–530. [CrossRef]
- Ozuna, H.; Snider, I.; Belibasakis, G. N.; Oscarsson, J.; Johansson, A.; Uriarte, S. M. Aggregatibacter actinomycetemcomitans and Filifactor alocis: Two exotoxin-producing oral pathogens. Frontiers in oral health 2022 3, 981343. [CrossRef]
- Razooqi, Z.; Höglund Åberg, C.; Kwamin, F.; Claesson, R.; Haubek, D.; Oscarsson, J.; Johansson, A. Aggregatibacter actinomycetemcomitans and Filifactor alocis as Associated with Periodontal Attachment Loss in a Cohort of Ghanaian Adolescents. Microorganisms 2022 10(12), 2511. [CrossRef]
- Peña-Chilet, M.; Esteban-Medina, M.; Falco, M. M.; Rian, K.; Hidalgo, M. R.; Loucera, C.; Dopazo, J. Using mechanistic models for the clinical interpretation of complex genomic variation. Scientific reports 2019 9(1), 18937. [CrossRef]
- Ke, J.; Gao, W.; Wang, B.; Cao, W.; Lv, J.; Yu, C.; Huang, T.; Sun, D.; Liao, C.; Pang, Y. et al. Exploring the Genetic Association between Obesity and Serum Lipid Levels Using Bivariate Methods. Twin research and human genetics: the official journal of the International Society for Twin Studies, 2022 25(6), 234–244. [CrossRef]
- de Vries, P. S.; van Herpt, T. T.; Ligthart, S.; Hofman, A.; Ikram, M. A.; van Hoek, M.; Sijbrands, E. J.; Franco, O. H.; de Maat, M. P.; Leebeek, F. W. et al. ADAMTS13 activity as a novel risk factor for incident type 2 diabetes mellitus: a population-based cohort study. Diabetologia 2017 60(2), 280–286. [CrossRef]
- Zillikens, M. C.; Demissie, S.; Hsu, Y. H.; Yerges-Armstrong, L. M.; Chou, W. C.; Stolk, L.; Livshits, G.; Broer, L.; Johnson, T.; Koller, D. L., Kutalik, Z., Luan, J., Malkin, I., Ried, J. S., Smith, A. V., Thorleifsson, G., Vandenput, L., Hua Zhao, J., Zhang, W., Aghdassi, A. et al. Large meta-analysis of genome-wide association studies identifies five loci for lean body mass. Nature communications 2017 8(1), 80. [CrossRef]
- Zhu, Z.; Guo, Y.; Shi, H.; Liu, C. L.; Panganiban, R. A.; Chung, W.; O'Connor, L. J.; Himes, B. E.; Gazal, S.; Hasegawa, K. et al. Shared genetic and experimental links between obesity-related traits and asthma subtypes in UK Biobank. The Journal of allergy and clinical immunology 2020 145(2), 537–549. [CrossRef]
- Baca, P.; Barajas-Olmos, F.; Mirzaeicheshmeh, E. et al. DNA methylation and gene expression analysis in adipose tissue to identify new loci associated with T2D development in obesity. Nutr. Diabetes 12, 50 (2022). [CrossRef]
- Nibali, L.; Stephen, A.; Hagi-Pavli, E.; Allaker, R.; Pino, A. D.; Terranova, V.; Pisano, M.; Marca, S. D.; Ferrara, V.; Scicali, R.; et al. Analysis of gingival crevicular fluid biomarkers in patients with metabolic syndrome. Journal of dentistry 2022 118, 104065. [CrossRef]
- Grundy, S. M.; Brewer, H. B.; Jr, Cleeman, J. I.; Smith, S. C., Jr; Lenfant, C.; American Heart Association; National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004 109(3), 433–438. [CrossRef]
- Guerrero, A.; Griffiths, G. S.; Nibali, L.; Suvan, J.; Moles, D. R.; Laurell, L.; Tonetti, M. S. Adjunctive benefits of systemic amoxicillin and metronidazole in non-surgical treatment of generalized aggressive periodontitis: a randomized placebo-controlled clinical trial. Journal of clinical periodontology 2005 32(10), 1096–1107. [CrossRef]
- Chang, C. C.; Chow, C. C.; Tellier, L. C.; Vattikuti, S.; Purcell, S. M.; Lee, J. J. Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScience 2015 4, 7. [CrossRef]
- Loh, P. R.; Danecek, P.; Palamara, P. F.; Fuchsberger, C.; A Reshef, Y.; K Finucane, H.; Schoenherr, S.; Forer, L.; McCarthy, S.; Abecasis, G. R. et al. Reference-based phasing using the Haplotype Reference Consortium panel. Nature genetics 2016 48(11), 1443–1448. [CrossRef]
- Durbin R. Efficient haplotype matching and storage using the positional Burrows-Wheeler transform (PBWT). Bioinformatics (Oxford, England) 2014 30(9), 1266–1272. [CrossRef]
- McCarthy, S.; Das, S.; Kretzschmar, W.; Delaneau, O.; Wood, A. R.; Teumer, A.; Kang, H. M.; Fuchsberger, C.; Danecek, P.; Sharp, K. et al. A reference panel of 64,976 haplotypes for genotype imputation. Nature genetics 2016 48(10), 1279–1283. [CrossRef]
- Yin, L.; Zhang, H.; Tang, Z.; Xu, J.; Yin, D.; Zhang, Z.; Yuan, X.; Zhu, M.; Zhao, S.; Li, X. et al. rMVP: A Memory-efficient, Visualization-enhanced, and Parallel-accelerated Tool for Genome-wide Association Study. Genomics, proteomics & bioinformatics 2021 19(4), 619–628. [CrossRef]
- Oscanoa, J.; Sivapalan, L.; Gadaleta, E.; Dayem Ullah, A. Z.; Lemoine, N. R.; Chelala, C. SNPnexus: a web server for functional annotation of human genome sequence variation (2020 update). Nucleic acids research 2020 48(W1), W185–W192. [CrossRef]
- Eren, A. M.; Vineis, J. H.; Morrison, H. G.; Sogin, M. L. A filtering method to generate high quality short reads using illumina paired-end technology. PloS one 2013 8(6), e66643. [CrossRef]
- Schloss, P. D.; Westcott, S. L.; Ryabin, T.; Hall, J. R.; Hartmann, M.; Hollister, E. B.; Lesniewski, R. A.; Oakley, B. B.; Parks, D. H.; Robinson, C. J. et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Applied and environmental microbiology 2009 75(23), 7537–7541. [CrossRef]
- Eren, A. M.; Morrison, H. G.; Lescault, P. J.; Reveillaud, J.; Vineis, J. H.; Sogin, M. L. Minimum entropy decomposition: unsupervised oligotyping for sensitive partitioning of high-throughput marker gene sequences. The ISME journal 2015 9(4), 968–979. [CrossRef]
- Chen, T.; Yu, W. H.; Izard, J.; Baranova, O. V.; Lakshmanan, A.; Dewhirst, F. E. The Human Oral Microbiome Database: a web accessible resource for investigating oral microbe taxonomic and genomic information. Database: the journal of biological databases and curation 2010, baq013. [CrossRef]
- Hammer, Ø.; Harper, D. A. Past: paleontological statistics software package for educaton and data anlysis. Palaeontologia electronica 2001 4(1), 1.
- Nibali, L.; Zavattini, A.; Nagata, K.; Di Iorio, A.; Lin, G. H.; Needleman, I.; Donos, N. Tooth loss in molars with and without furcation involvement - a systematic review and meta-analysis. Journal of clinical periodontology 2016 43(2), 156–166. [CrossRef]
- Nibali, L.; Bayliss-Chapman, J.; Almofareh, S. A.; Zhou, Y.; Divaris, K.; Vieira, A. R. What Is the Heritability of Periodontitis? A Systematic Review. Journal of dental research 2019 98(6), 632–641. [CrossRef]
- Cavalla, F.; Biguetti, C. C.; Melchiades, J. L.; Tabanez, A. P.; Azevedo, M. C. S.; Trombone, A. P. F.; Faveri, M.; Feres, M.; Garlet, G. P. Genetic Association with Subgingival Bacterial Colonization in Chronic Periodontitis. Genes 2018 9(6), 271. [CrossRef]
- Rhodin, K.; Divaris, K.; North, K. E.; Barros, S. P.; Moss, K.; Beck, J. D.; Offenbacher, S. Chronic periodontitis genome-wide association studies: gene-centric and gene set enrichment analyses. Journal of dental research 2014 93(9), 882–890. [CrossRef]
- Shusterman, A.; Durrant, C.; Mott, R.; Polak, D.; Schaefer, A.; Weiss, E. I.; Iraqi, F. A.; Houri-Haddad, Y. Host susceptibility to periodontitis: mapping murine genomic regions. Journal of dental research 2013 92(5), 438–443. [CrossRef]
- Shusterman, A.; Munz, M.; Richter, G.; Jepsen, S.; Lieb, W.; Krone, B.; Hoffman, P.; Laudes, M.; Wellmann, J.; Berger, K. et al. The PF4/PPBP/CXCL5 Gene Cluster Is Associated with Periodontitis. Journal of dental research 2017 96(8), 945–952. [CrossRef]
- Munz, M.; Richter, G. M.; Loos, B. G.; Jepsen, S.; Divaris, K.; Offenbacher, S.; Teumer, A.; Holtfreter, B.; Kocher, T.; Bruckmann, C. et al. Meta-analysis of genome-wide association studies of aggressive and chronic periodontitis identifies two novel risk loci. European journal of human genetics: EJHG 2019 27(1), 102–113. [CrossRef]
- Munz, M.; Willenborg, C.; Richter, G. M.; Jockel-Schneider, Y.; Graetz, C.; Staufenbiel, I.; Wellmann, J.; Berger, K.; Krone, B.; Hoffmann, P. et al. A genome-wide association study identifies nucleotide variants at SIGLEC5 and DEFA1A3 as risk loci for periodontitis. Human molecular genetics 2017 26(13), 2577–2588. [CrossRef]
- Divaris, K.; Monda, K. L.; North, K. E.; Olshan, A. F.; Lange, E. M.; Moss, K.; Barros, S. P.; Beck, J. D.; Offenbacher, S. Genome-wide association study of periodontal pathogen colonization. Journal of dental research 2012 91(7 Suppl), 21S–28S. [CrossRef]
| Average | ||
| Age | 58.12 ± 9.89 | |
| BMI | 31.88 ± 4.37 | |
| Frequency | ||
| Gender | Male | 65 (63.1%) |
| Female | 48 (36.9%) | |
| Smoking status | Non smoker | 67 (65.0%) |
| Current smoker | 28 (27.2%) | |
| Former smoker | 8 (7.8%) | |
| Frequency of dental visits | Never been | 2 (1.9%) |
| Only in case of problems | 79 (76.7%) | |
| 1/year | 12 (11.7%) | |
| >1/year | 10 (9.7%) | |
| Previous periodontal treatment | Yes | 3 (2.9%) |
| No | 100 (97.1%) | |
| Last dental visit | Never been | 2 (1.9%) |
| >10 years ago | 7 (6.8%) | |
| 1-10 years ago | 60 (58.3%) | |
| <1 year ago | 34 (33.0%) | |
| Tooth brushing frequency | <1/day | 6 (5.9%) |
| 1/day | 34 (33.0%) | |
| At least 2/day | 63 (61.1%) | |
| Type of toothbrush | None | 1 (1.0%) |
| Manual | 92 (89.3%) | |
| Electric | 10 (9.7%) | |
|
Use of interdental cleaning tools |
Daily-weekly | 14 (13.6%) |
| Never | 89 (86.4%) | |
| Average | Number | |
| Number of teeth (excluding third molars) | 22.77 ± 4.19 | 2345 |
| DMFT | 12.58 ± 6.07 | - |
| Decayed teeth | 0.63 ± 0.96 | 65 |
| Patients with caries detected | - | 38 (36.89%) |
| FMPS | 72.11 ± 22.51 | - |
| FMBS | 23.92 ± 19.62 | - |
| Average PPD | 2.44 ± 0.73 | - |
| Average CAL | 3.05 ± 1.12 | - |
| % PPDs 1-4mm | 93.17 ± 0.88% | - |
| % PPDs 5-6mm | 5.92 ± 0.75% | - |
| % of PPDs >6mm | 0.94 ± 0.23% | - |
| No-Mild periodontitis | - | 10 (9.7%) |
| Moderate periodontitis | - | 38 (36.9%) |
| Severe periodontitis | - | 55 (53.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





