1. Introduction
Even with advances in medical technology, medical errors due to human error still prone to be occur. According to a research report [To Err is Human- Built a Healthy and Safety System] published by the U.S. National Institute of Medicine in 2000, the rate of medical errors caused by human negligence is as high as 2.9%, of which over 50% Medical errors are preventable. Hence, how to avoid medical errors caused by human negligence has always been an important research topic in the medical field. Among all medical behaviours, surgery has always been the riskiest medical behaviours in the medical process. Among the types of surgical medical negligence, incorrect surgical site is among the top proportion of surgical medical negligence. The wrong surgical site here refers to the wrong position or wrong location of the incision.
For example, the original incision was on the right hand, but after anesthesia, the incision was changed to the left hand; or, the incision was originally on the left hand. The surgery was performed on the right elbow, but after anesthesia, the surgery was performed on the right wrist. Such wrong surgical site often causes an originally simple operation to cause serious harm to the patient. Since surgical site errors are often caused by human negligence, in addition to causing serious injuries to patients, their medical teams often have to face huge compensation and legal proceedings, and their medical institutions must withstand public opinion and pressure from society [
1]. Therefore, how to avoid medical errors caused by human negligence is still a primary research topic in the medical field until now.
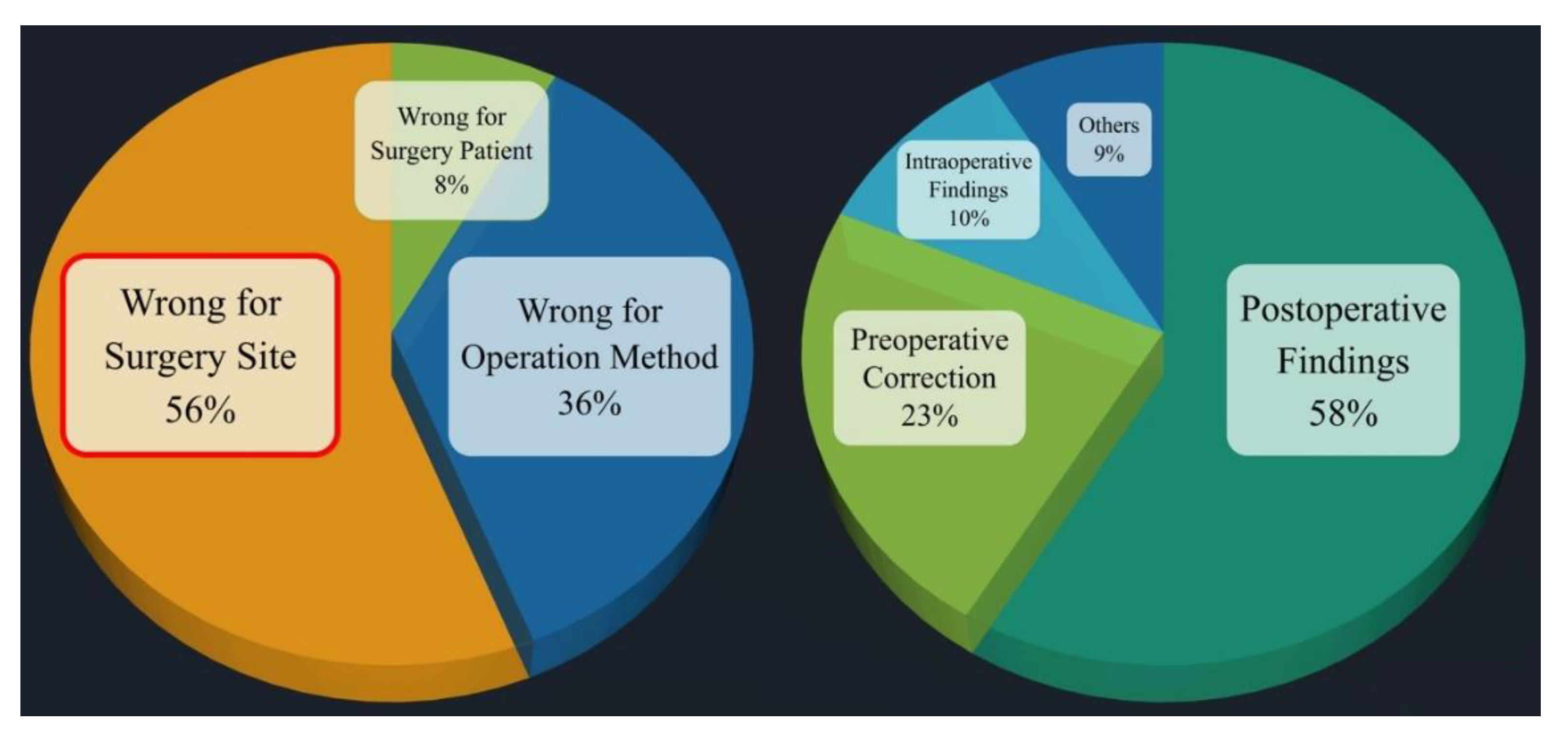
Among all medical errors, surgical medical errors often cause huge injuries and losses to patients and medical institutions, since surgery is the most prevalent medical action. Medical negligence in surgery is divided into several categories. Among them, in the 2019 annual report of the Taiwan Patient Safety Reporting System [
2], it was pointed out that the incidence of surgical site errors reached the second place among the types of surgical event errors. Therefore, how to avoid surgical site errors is an important issue for surgery research topics in medical malpractice. Among all surgical specialties, the orthopedic surgery is the most common category in surgical site errors, as high as 56%, and only 5.4% can be found to be corrected before surgery, because orthopedic surgery needs to deal with skeletal and muscular injuries of the extremities, as shown in Fig. 1 [
3]. Therefore, how to avoid surgical site errors is definitely the primary research topic in medical errors of orthopedic surgery.
Figure 1.
Category in surgical site errors [
3].
Figure 1.
Category in surgical site errors [
3].
In orthopedic surgery, the wrong site of surgery includes the wrong position of the operation and the wrong site of the operation. Taking the wrong incision position as an example, assume that the patient’s original incision was on the right limb, but due to human error, the incision was performed on the left limb. The original incision was on the right elbow, but after anesthesia, it was changed to the right wrist. Such operations are often simple operations, but the wrong surgical site causes more serious injuries to the patient, and makes the medical team and the hospital face huge compensation and pressure from public opinion, and even legal proceedings. In view of this, after discussing with the supervisor and the cooperating orthopedic surgeon, this project will first take the upper limb orthopedic surgery as the main surgical site, and propose a smart image recognition system that can prevent the error of the left and right parts of the upper limb orthopedic surgery, and assist the orthopedic surgeon to prevent upper limb surgery left-right misalignment occurs.
According to paper survey and relevant information obtained from medical institutions, the current methods to prevent the wrong location of surgery are still mainly marked by marking or barcode scanning, as shown in Fig. 2. However, regardless of marking or barcode scanning, it is still easy to cause errors at the surgical site due to many human factors, such as unusual time pressure, unusual instrument settings or handling in the operating room, more than one surgeon involved, the patient being taken transfer to another physician, and multidisciplinary physicians to participate in the operation. Therefore, this paper aims to integrate medical and artificial intelligence technologies to develop an intelligent image recognition system to replace the marking and barcode scanning methods to avoid the error of the left and right parts of upper limb orthopedic surgery caused by the above-mentioned human factors.
Figure 2.
Marking and barcode scanning.
Figure 2.
Marking and barcode scanning.
Susanne Hempel published a systemic review on the wrong surgical site in JAMA Surgery in 2015. It pointed out that the incidence of surgical site errors is about 1 in 100,000. The major reason for the occurrence is poor communication to be prone to make the medical personnel mistakes. The poor communication included Miscommunications among staff, Missing information that should have been available to the operating room staff, surgical team members not speaking up when they noticed that a procedure targeted the wrong side, and a surgeon ignoring surgical team members who questioned laterality [
3]. Therefore, the medical team must communicate fully and raise any questions bravely. The chief surgeon must also respect everyone's opinions to avoid medical negligence in the wrong surgical site.
Research published by Mark A Palumbo in 2013 pointed out that it is not only the limbs that can be operated on in the wrong place. In spinal surgery, the wrong joint often occurs. Once the wrong part is prescribed, it will be a devastating disaster for both the patient and the doctor. The author suggested that in order to prevent the wrong surgical site, in addition to the strict regulation of the medical system, it is also necessary to develop a customized process (patient specific protocol) in order to avoid the wrong surgical site [
4].
Omid Moshtaghi published the results of the study in 2017, analyzing the surgical site errors in California from 2007 to 2014. The authors pointed out that although California introduced the universal surgical safety protocol in 2004 to ensure the safety of patients during surgery, the wrong site of surgery still continues to occur. Occurrence of the disciplines, orthopedics as the largest was accounted for 35% [
5].
Ambe P.C.'s research report in 2015 also pointed out that orthopedics is the department with the most frequent surgical site errors. The most common causes included breakdown in communication, time pressure, emergency procedures, multiple procedures on the same patient by different surgeons, and obesity. The author recommends doing check lists and checking carefully before surgery, which is an effective solution [
6].
After visiting the operation process, it can be found that in the current orthopedic surgery, before the operation is disinfected and draped, a mark is drawn on the site where the patient intends to be operated on, so as to remind the surgeon whether to draw the wrong knife. At present, the position of orthopedic surgery is mostly marked by using a colored pen to draw a mark on the site to be operated on, as shown in Fig. 2. In modern times, some hospitals adopt the barcode scanning method, that is, paste a barcode on the site to be operated on, and then scan it through a barcode machine to confirm whether the position is correct, as shown in Fig. 2. However, regardless of marking or barcode marking, it is still easy to cause wrong surgical site due to the following factors, such as initiate or complete surgery under unusual time pressure, instrument settings or handling that are not commonly used in the operating room, such as left-handed surgery, more than one surgeon is involved, the patient is referred to another physician, physicians from multiple disciplines participate in the operation, and unusual physical features require special positioning.
Based on the above literature review, the main research methods in the world to prevent incorrect surgical sites currently still use traditional methods, such as strengthening communication, identifying patients, marking the surgical site, time-out before surgery, and using check lists and so on. They all hope that through stricter inspections and checks, the occurrence of surgical site errors can be prevented.
Among the intelligence image recognition technologies, the most commonly used one is deep learning image recognition. This type of image recognition method mainly uses a large number of training data sets and learning training methods to find the characteristics of the image to be recognized, and then completes image recognition through these image characteristics. However, the current deep learning image recognition technology cannot be applied to the above-mentioned intelligent image recognition system for the left and right parts of upper limb orthopedic surgery. The main reason is that the human body itself has a left-right symmetry of the golden ratio. Taking the left and right parts of the upper limbs to be identified in this project as an example, if there are no special marks, birthmarks, or scars on the left or right upper limbs, the left and right upper limbs will have the same image features.
This is an innovative research. We plan to develop an upper and lower limb surgical site identification system based on deep learning. In the first stage, a simulated dummy will be used as the test object. After the deep learning model training is mature, we will apply for IRB approval and conduct the second stage human trials. It is hoped that the research results can be actually applied to the clinical treatment of the hospital to achieve the purpose of smart medical treatment, which can truly benefit patients and reduce surgical site errors.
Therefore, after discussing with the orthopedic surgeon (co-host), it is absolutely necessary to develop an upper limb orthopedic intelligent image recognition system to replace the above-mentioned marking and barcode machine scanning methods before surgical disinfection and draping. From the background and purpose of the research project, it can be found that orthopedic surgery accounts for 41% of wrong site surgery, ranking first. Among them, the part where position errors occur most frequently is the left and right position errors. However, in current research at home and abroad, most of the related research on upper limb surgery focuses on rehabilitation, lymph, and nerve [7-29], and no research results have been proposed on distinguishing between left and right upper limbs to prevent dislocation surgery image recognition. Therefore, how to develop a new type of intelligent image recognition system to help surgeons distinguish the left and right upper limbs to prevent dislocation surgery, and avoid the problem of wrong left and right surgical positions during orthopedic upper limb surgery will be of considerable benefit and research value.
Therefore, an artificial intelligent image recognition system (AIIRS) for preventing wrong side upper limb surgery, was proposed to address the above issues in this paper. In order not to violate academic theory and human body research ethics, this paper will first use laboratory students to simulate orthopedic surgery patients as the object of system experimental testing to establish a training data set and a test data set. After the proto type of deep learning model training is completed, the IRB application approval is completed. The industry-university cooperation with the hospital and the second phase of human trials are carried out. Hence, the research results are actually applied to orthopedic clinical treatment to achieve the purpose of smart medical treatment.
2. Materials and Methods
The current position marking of orthopedic surgery is mainly based on mark marking or barcode scanning. However, such an approach is still prone to surgical site errors due to time pressure, unfamiliar instrument setup or handling, participation of multiple surgeons, patient being referred to another physician, and other factors. Therefore, how to prevent the wrong surgical site is absolutely the top priority of orthopedic surgery.
After discussions with orthopedic surgeons, this paper proposed an artificial intelligent image recognition system, AIIRS, combined with a deep learning neural network model to assist orthopedic surgeons to prevent left-right dislocation in upper limb surgery. In the internal survey of the members of the Orthopedic Medical Association of the Republic of China, it was also shown that 56% of the wrong parts were opened, and only 5.4% could be found to be corrected before the operation. Therefore, the artificial intelligent image recognition system (AIIRS) for the left and right parts of upper limb orthopedic surgery proposed in this paper will have considerable benefits and research value for upper limb orthopedic surgery.
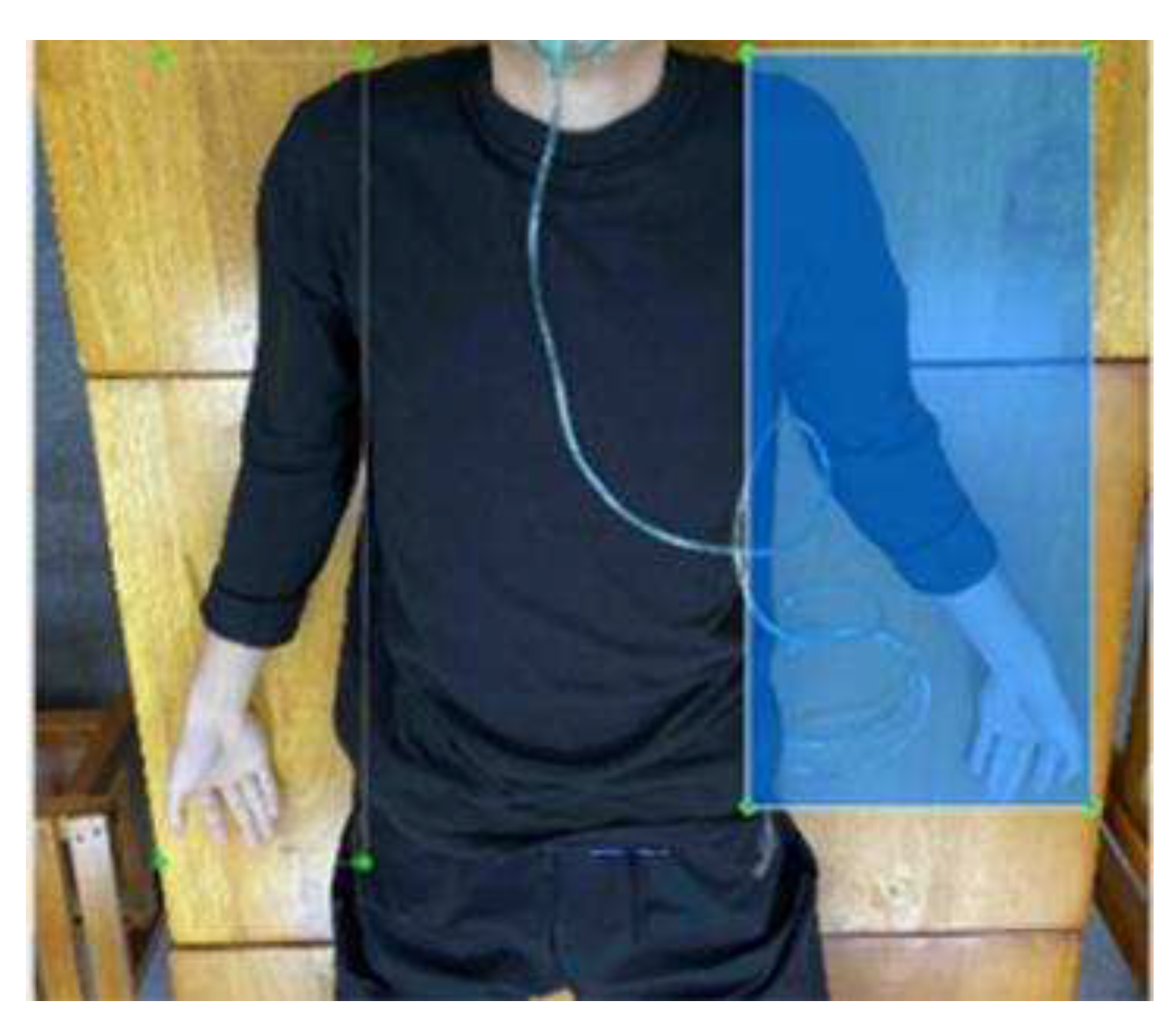
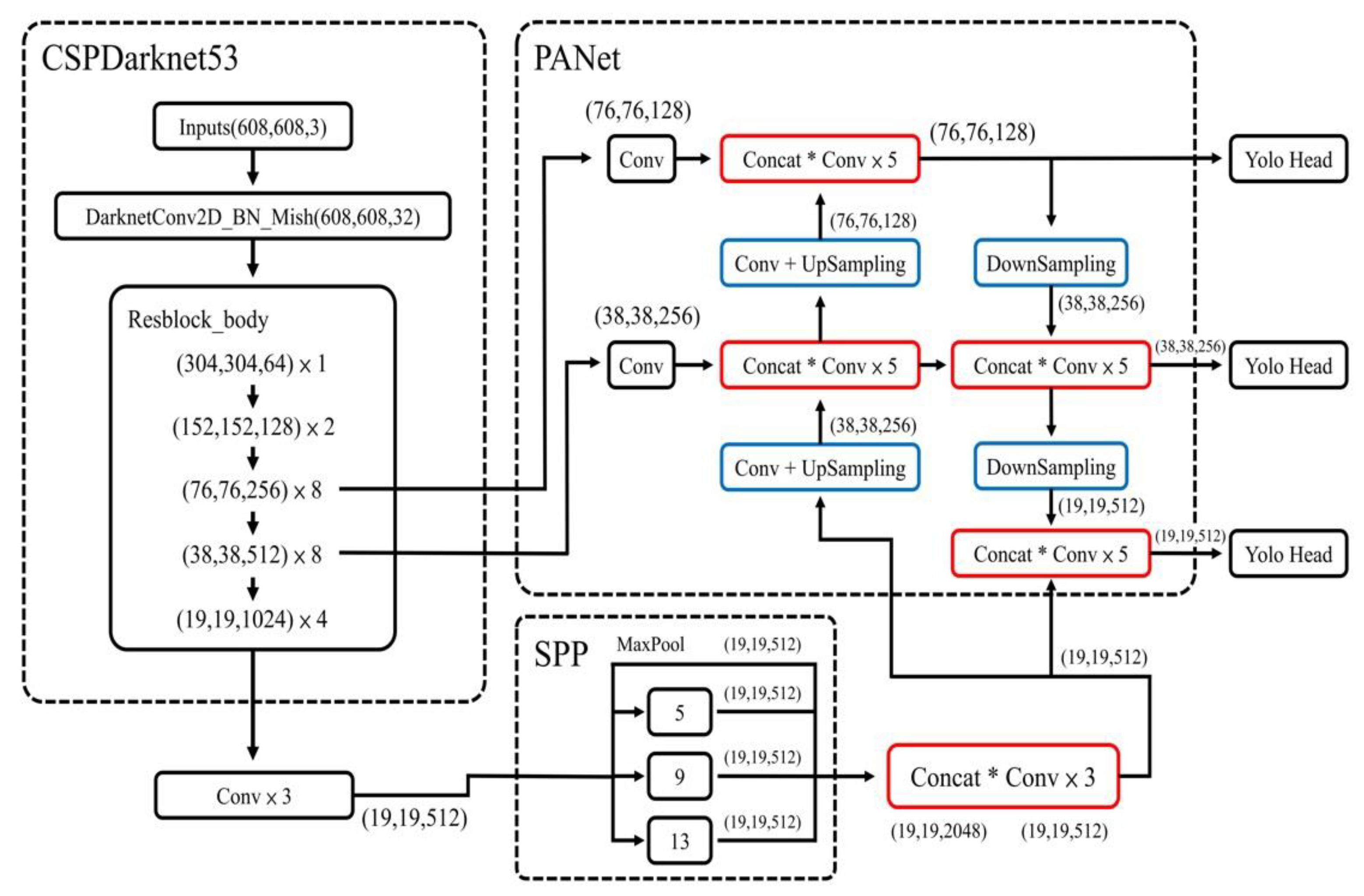
The main contribution of this paper is to combine the existing deep learning neural network model through appropriate data training sets and test sets with the coordination of model parameters to achieve intelligent image recognition of the left and right positions of upper limb orthopedic surgery limbs. In the existed deep learning neural network model, Yolo was proved to be used in most image recognition applications. Hence, the neural network model in this paper adopts the most commonly used YoloV4 model. Since CSPNet in YoloV4 is based on DarknNet53 neural network, and DarkNet53 is developed based on ResNet, two different models, such as ResNet50 and YoloV4, were used for simultaneous training. In the data set, total number of photos is 810. Among these data set, 122 photos are generated by data generation method. The ratio of the training set to the test set is 9:1. The labeling is used through the LabelImg software. The photos are labeled one by one for the training range, and divided into two parts, such as right-hand and left-hand for training, as shown in Fig. 3.
Figure 3.
Labeling through the LabelImg software.
Figure 3.
Labeling through the LabelImg software.
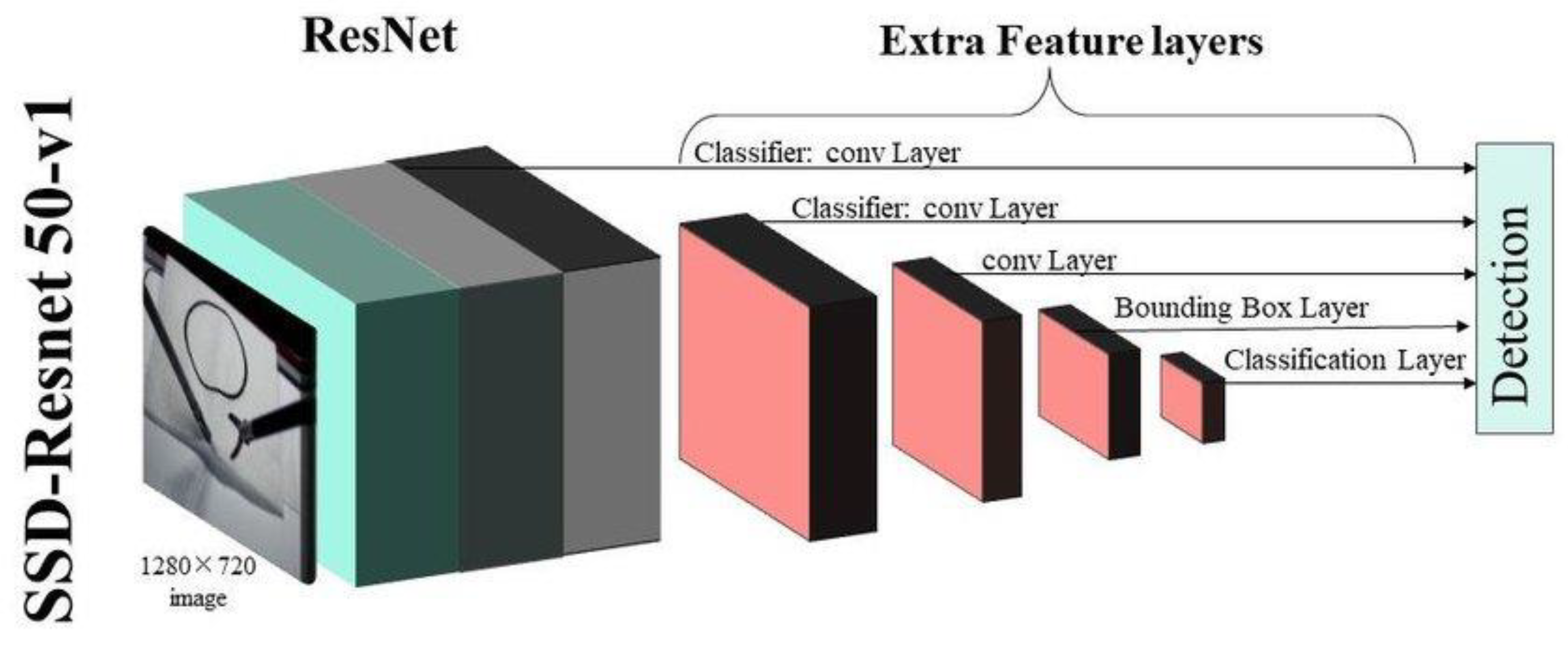
In ResNet50, the marked data set is classified into training set and test set in the two folders. The two folders are converted into the .record files to ensure that the model training process could process the image files with adding a pre-training model. This model is related to the final training results. If this pre-training model is replaced, it could be transformed into other models. ResNet50 was shown in Fig. 4. The parameter in pipeline.config of ResNet50 was listed in
Table 1 [
30]. In YoloV4, the parameters were listed in
Table 2. The YoloV4 model was shown in Fig. 5. We used the Mish function as the activation function and the CIOU function as the loss function in YoloV4 [
31].
In order not to violate academic theory and human research ethics, this project will first use laboratory students to simulate orthopedic surgery patients as the subjects of the system experimental test to establish a training data set and a test data set. After the deep learning model training matures, we will apply for IRB approval in the future, conduct industry-university cooperation with the hospital, conduct the second phase of human trials, and actually apply the research results to clinical medical treatment in orthopedics to achieve the purpose of smart medical care and implement the combination of theory and practice achieves real industry-university cooperation.
Figure 4.
ResNet50 model [
30].
Figure 4.
ResNet50 model [
30].
Figure 5.
YoloV4 model [
31].
Figure 5.
YoloV4 model [
31].
3. Results
Since this paper is a pilot study, the experimental results were executed by our lab members not the real patients to avoid the ethical permission. In addition, it was assumed that the lighting in the operating room is sufficient since image recognition for left and right in the upper limb was executed before the surgery. To ensure the number of training data is adequate, some data was generated by data generation method. The number of training data is 810. In the training data, the training data generated by data generation method is 122. The ratio of the test set to the training set is 1:9. In the pre-processing of data, each training data is labeled one by one through the LabelImg software. The training data set are divided into right-hand data and left-hand data.
In this paper, it focused on
Accuracy and
Recall, since the proportion of correct classifications and correct samples in overall model needed to be judged. Hence, the
Accuracy and
Recall are the main performance metrics in our experimental results.
Accuracy was defined as (1), where true positive (
TP) is an actual positive sample which is predicted to be a positive sample, false positive (
FP) is an actual negative sample which is predicted to be a positive sample, false negative (
FN) is an actual positive sample which is predicted to be a negative sample, and true negative (
TN) is an actual negative sample which is predicted to be a negative sample, respectively.
Recall was defined as (2)
The confidence value (Conf_threshold) close to the recognition frame is defined as the threshold value of object frame recognition and could be adjusted. It is also the important parameter in our proposal. For example, if the confidence value is set to 0.9, only the object frame which Conf_threshold of object frame recognition larger than 0.9 could be shown on the screen, as shown in Fig. 6.
Figure 6.
Example with Conf_threshold larger than 0.9.
Figure 6.
Example with Conf_threshold larger than 0.9.
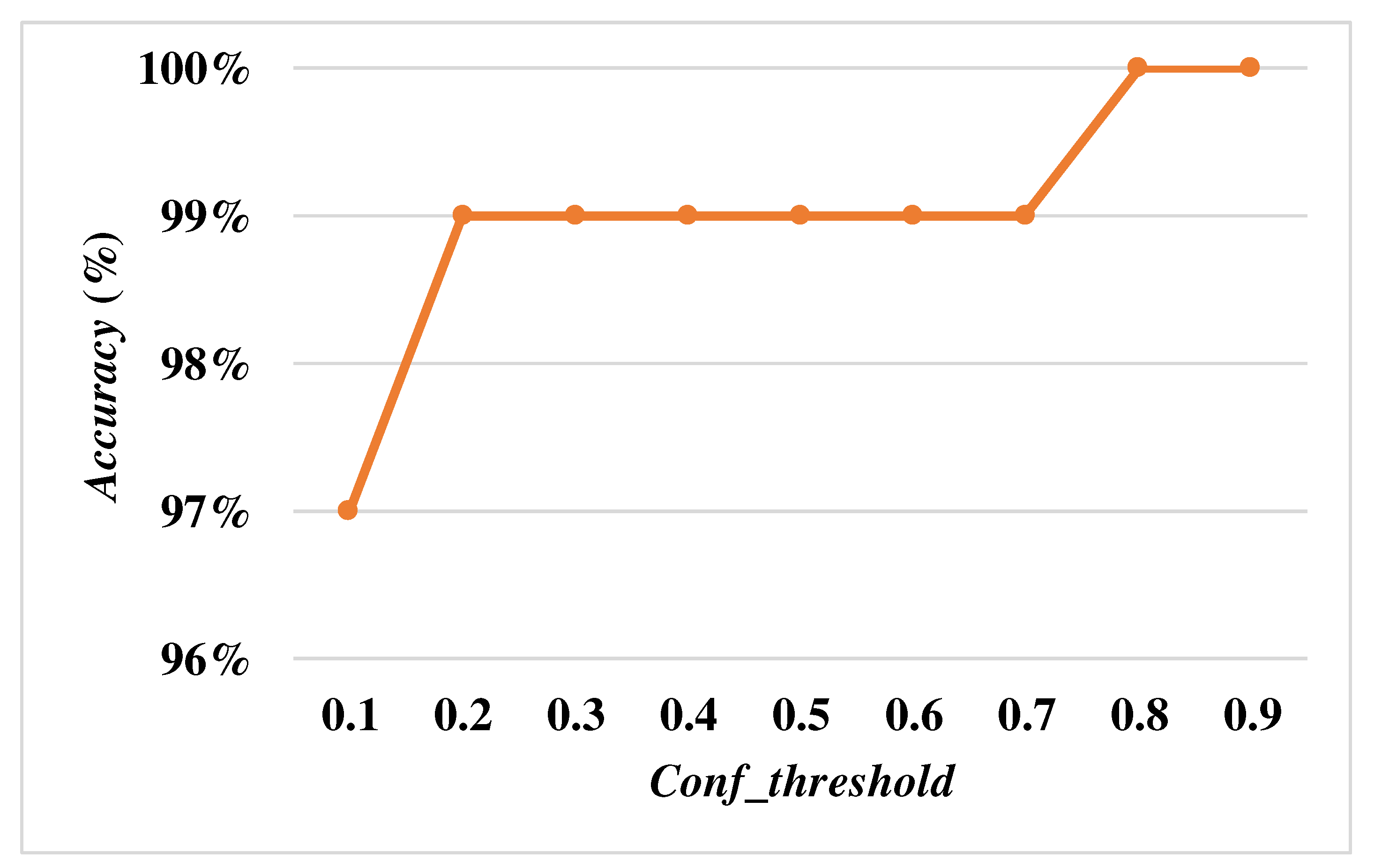
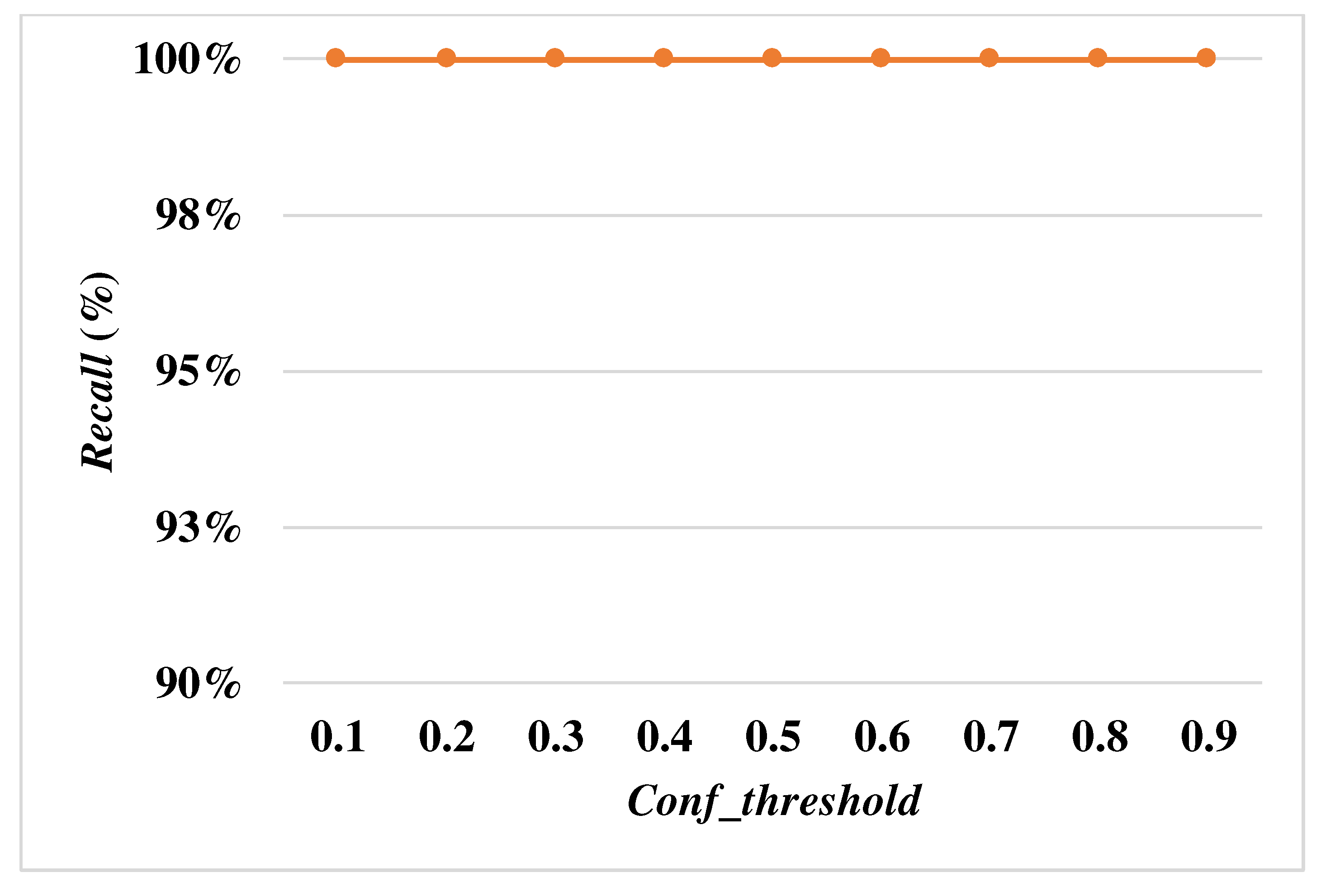
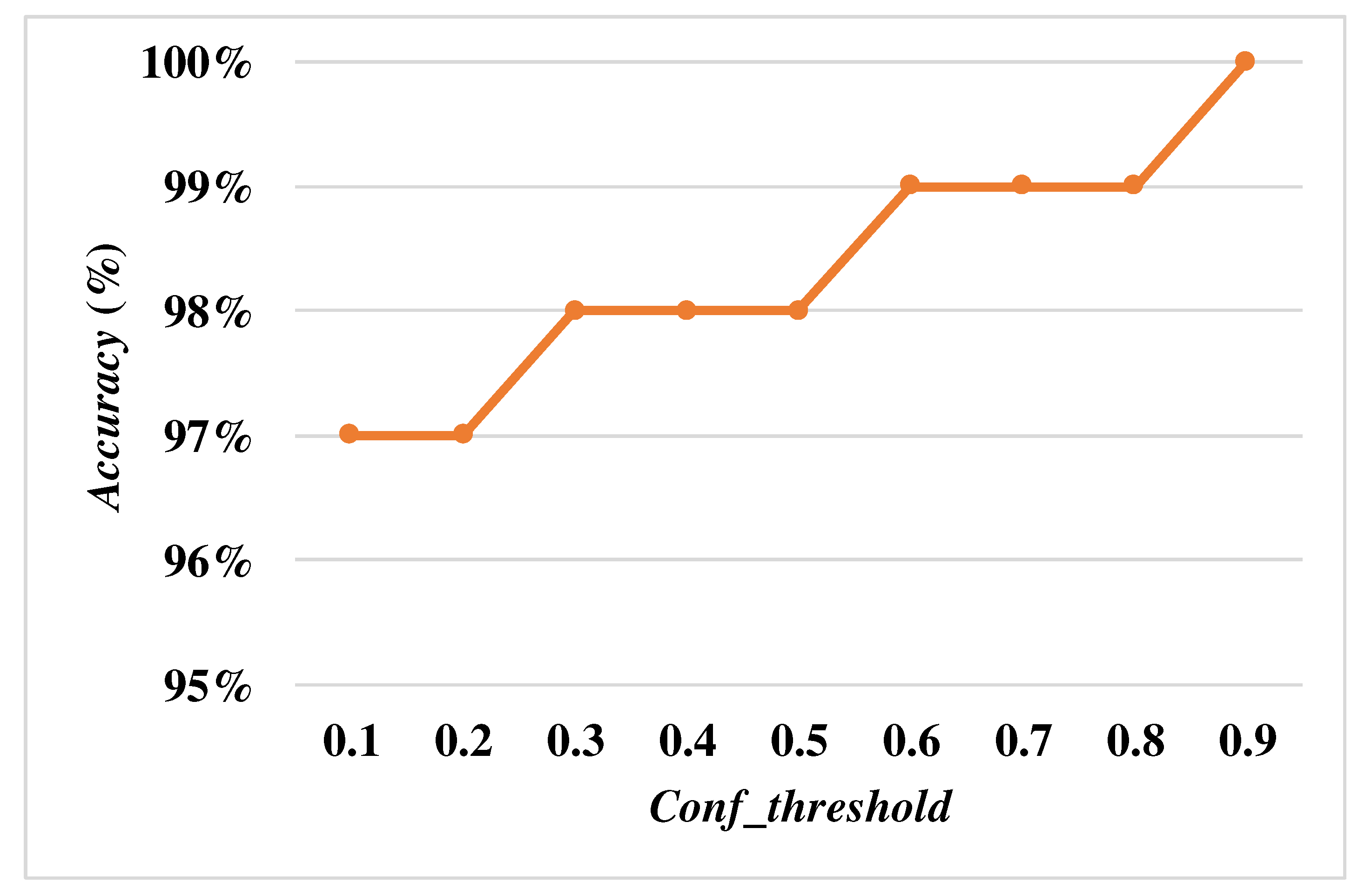
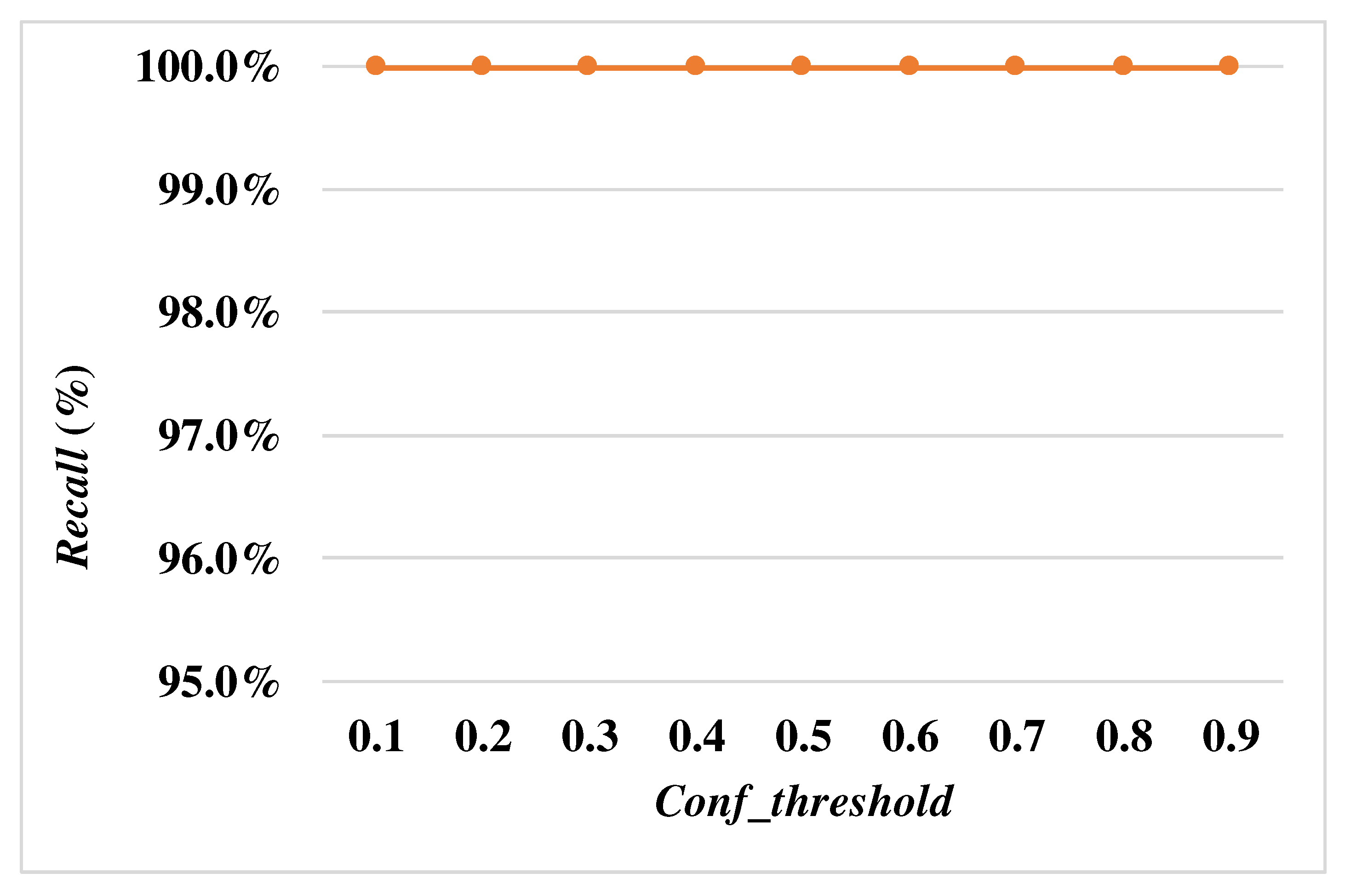
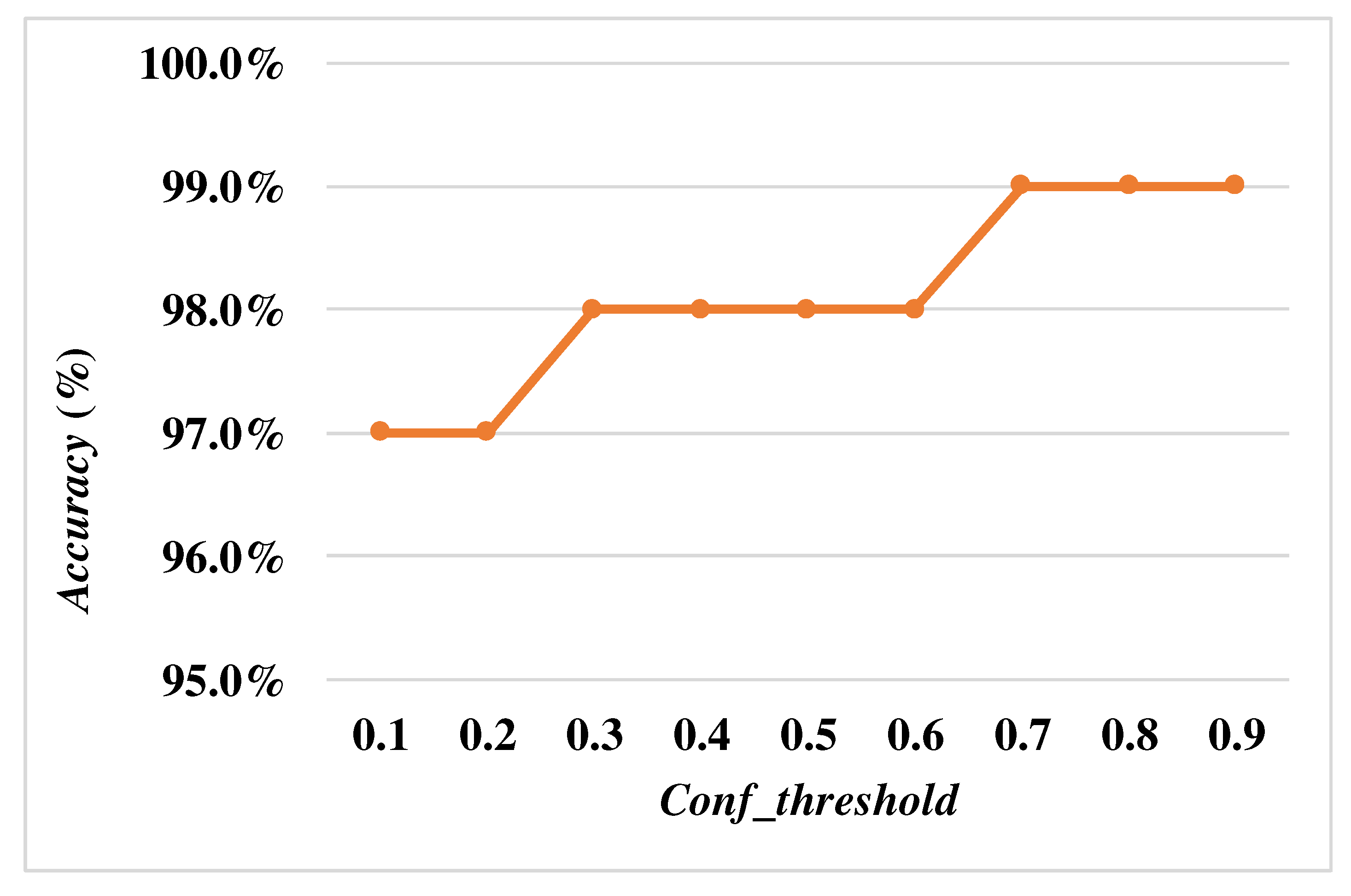
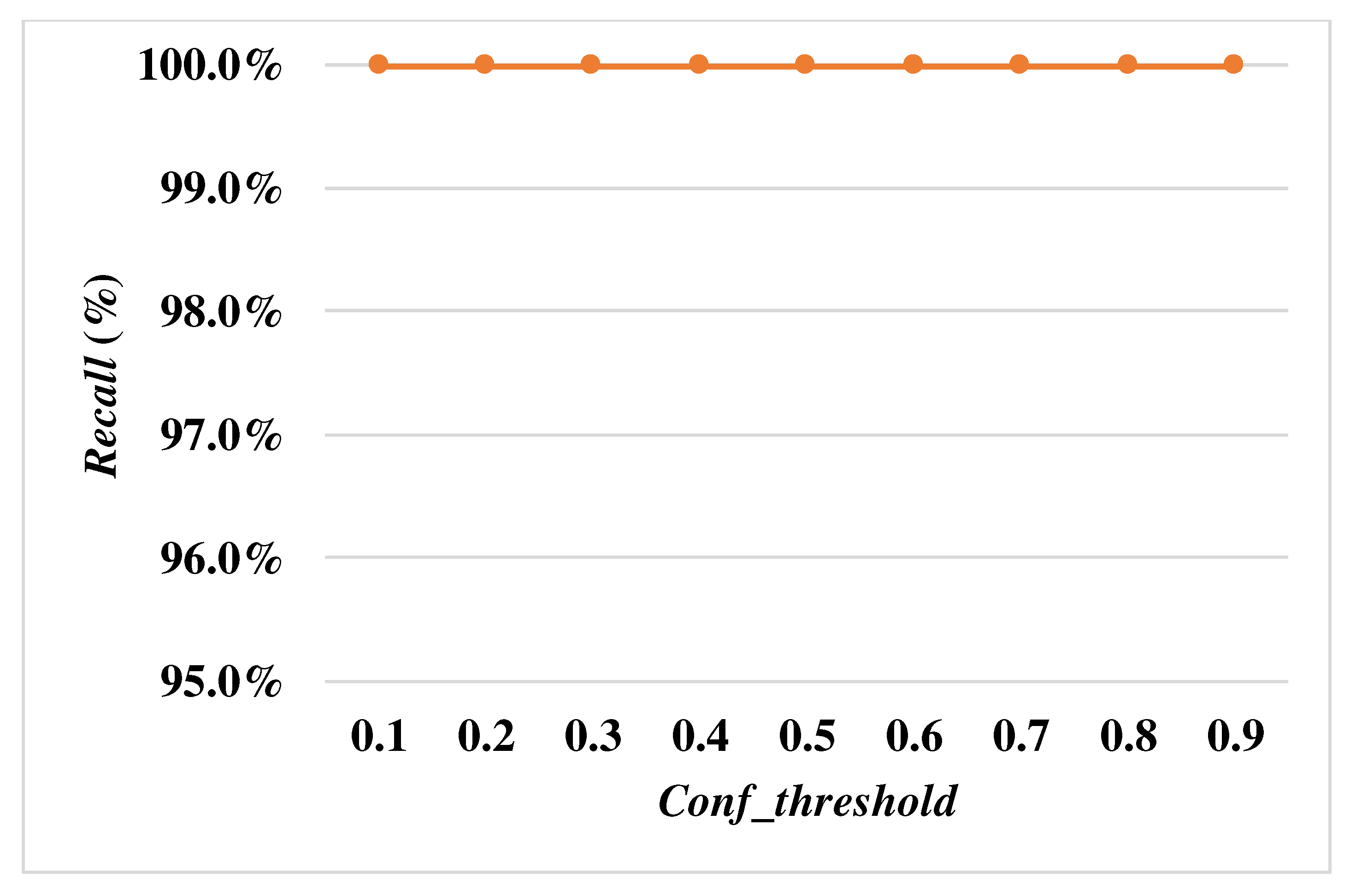
When the size of the input image is the same, the lower Conf_threshold will lead to FP in a decrease of the overall accuracy. In order to determine the optimal Conf_threshold, the Conf_threshold is increased by 0.1 each time to calculate Accuracy and Recall with the input size is,, and, respectively.
In Figs. 7 and 8, they showed Accuracy and Recall with the input size is when the Conf_threshold is increased by 0.1 each time. In Figs. 9 and 10, they showed Accuracy and Recall with the input size is when the Conf_threshold is increased by 0.1 each time. In Figs. 11 and 12, it showed Accuracy and Recall with the input size is when the Conf_threshold is increased by 0.1 each time. Through the experimental results in Figs. 7-12, they showed that the optimal Conf_threshold is 0.9.
Figure 7.
Accuracy with the input size.
Figure 7.
Accuracy with the input size.
Figure 8.
Recall with the input size.
Figure 8.
Recall with the input size.
Figure 9.
Accuracy with the input size.
Figure 9.
Accuracy with the input size.
Figure 10.
Recall with the input size.
Figure 10.
Recall with the input size.
Figure 11.
Accuracy with the input size.
Figure 11.
Accuracy with the input size.
Figure 12.
Recall with the input size.
Figure 12.
Recall with the input size.
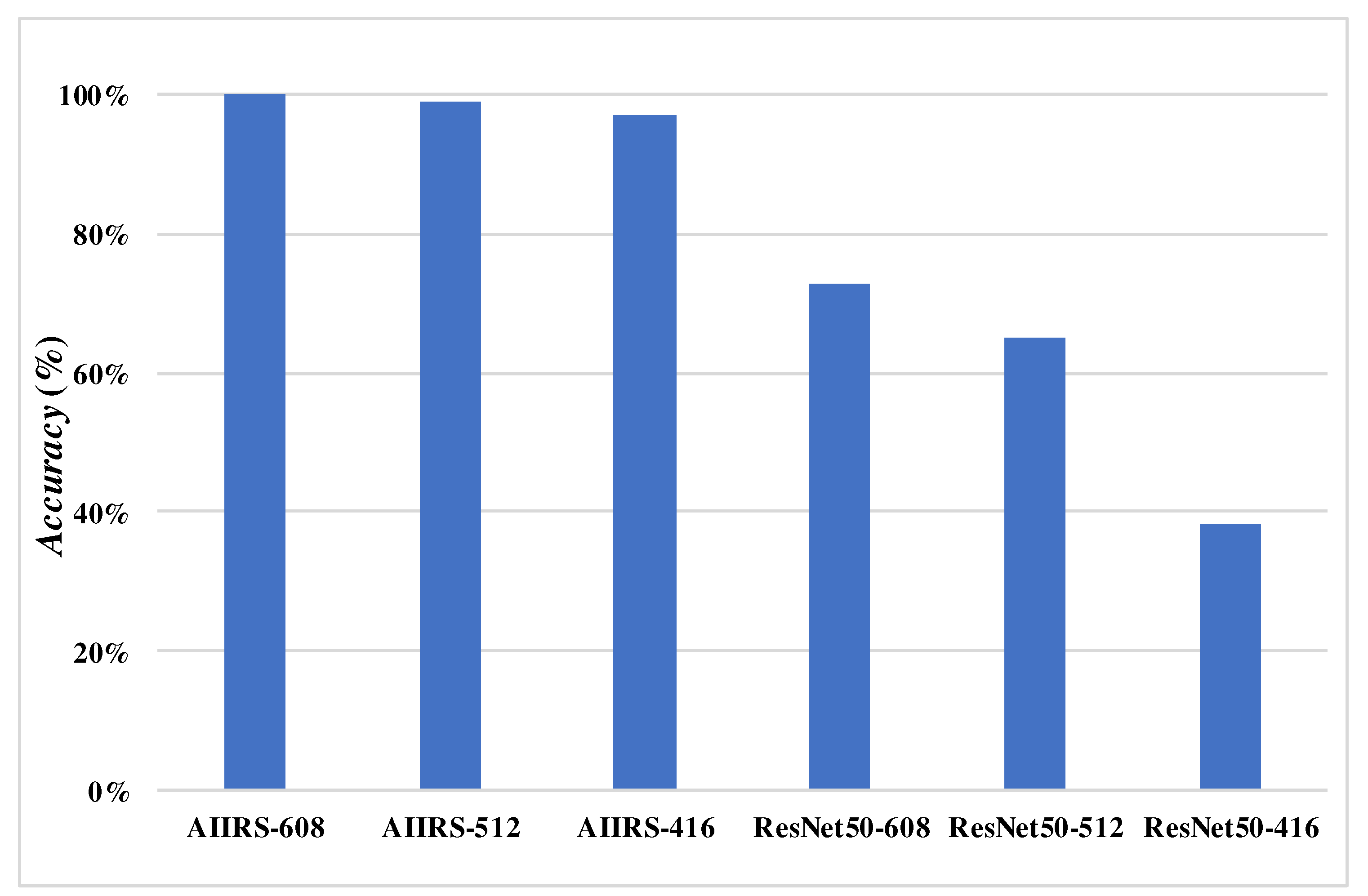
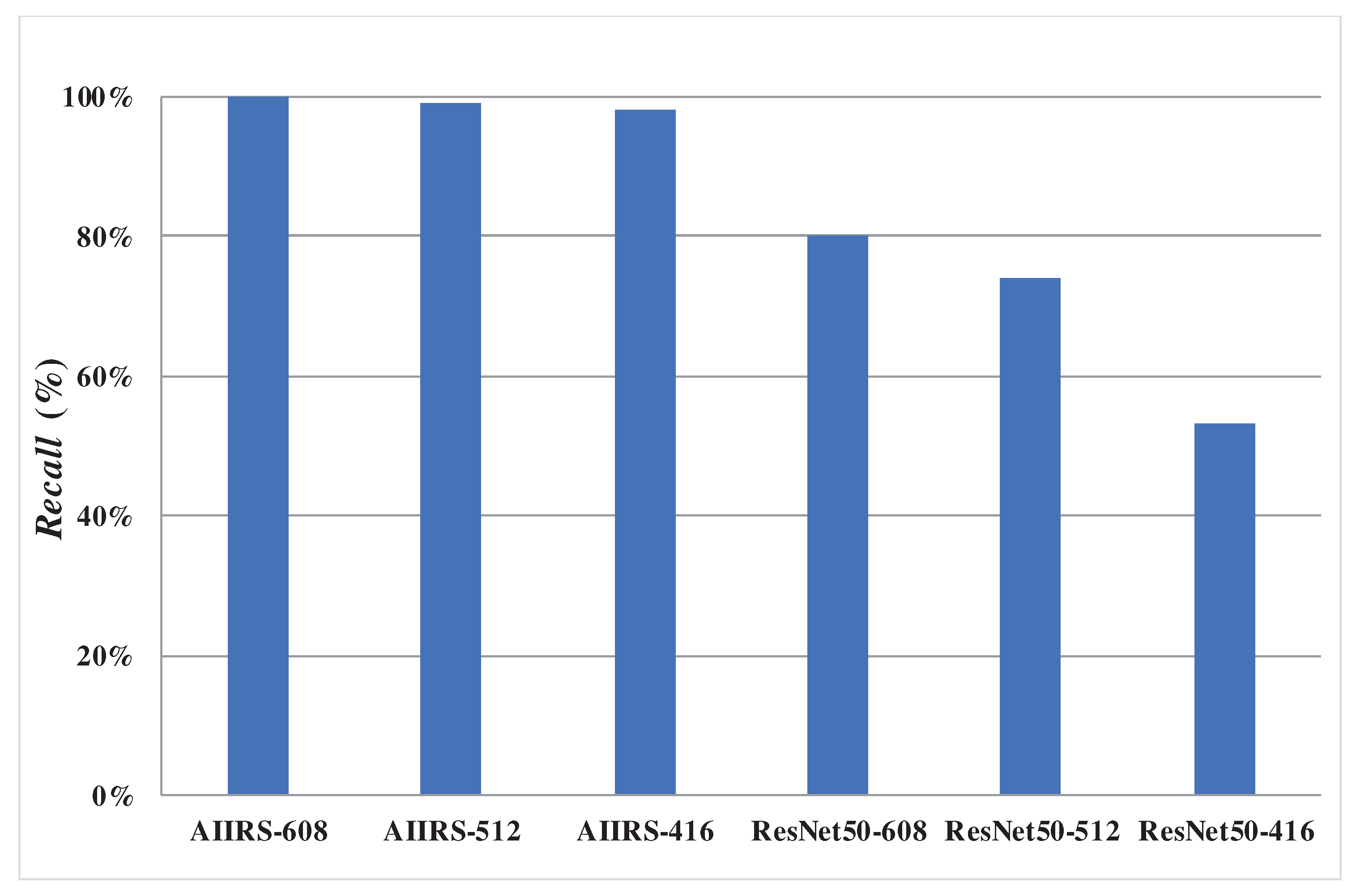
The following experimental results are based on the comparison of Accuracy and Recall while the Conf_threshold is 0.9 and input size is, as shown in Figs. 7 and 8, since AIIRS had the optimal Accuracy and Recall with 0.9 of Conf_threshold and of input size. AIIRS-608 was defined as AIIRS with input size and others are followed in the same way. Hence, the optimal value of Conf_threshold is set to 0.9 in the experiment under AIIRS and ResNet50, where ResNet50-608 is defined as ResNet50 with input size and others are followed in the same way.
Figure 13 showed that
Accuracy with input size
in both AIIRS and ResNet50 was higher than
Accuracy with the other input size while
Conf_threshold is set to 0.9. It also showed that
Accuracy in AIIRS was higher than
Accuracy in ResNet50. In the same way,
Recall with input size
in both AIIRS and ResNet50 was higher than
Recall with the other input size in Fig. 14 while
Conf_threshold is set to 0.9.
Figure 14 also showed that
Recall in AIIRS was higher than
Accuracy in ResNet50.
4. Discussion
Since
Conf_threshold will affect the performance metrics, such as
Accuracy and
Recall, how to determine the suitable
Conf_threshold was the first goal in the experimental results. From Figs. 7 to 12, they showed that the optimal
Conf_threshold could be set to 0.9 in AIIRS. In Figs. 7-12, it also showed that the optimal input size could be set to
in AIIRS.
Figure 13 and
Figure 14 showed that
Accuracy and
Recall, in AIIRS were higher than
Accuracy and
Recall, in ResNet50.
Figure 13 and
Figure 14 also showed that the optimal input size could be set to
in ResNet50. The experimental results proved that our designed intelligent image recognition system, IIRS, with YoloV4 could be applied for preventing wrong side upper limb surgery. Based on the pilot experimental results, the IRB for this our designed artificial intelligent image recognition system, AIIRS, to prevent wrong side upper limb surgery has been applied and passed. Hence, the experimental results will be closer to perfection and consistent with actual left and right position identification in upper limb orthopedic surgery in the future.
5. Conclusions
In the category of surgical medical negligence, the wrong surgical site caused by the wrong location of the operation or the wrong site of the operation has ranked the second among the wrong types of surgical events. Among the surgical site errors, orthopedic surgery is the most common discipline. Among them, the wrong part accounted for 56%, and only 5.4% could be found to be corrected before the operation. Since the surgical site errors are often caused by human negligence, 50% of medical errors could be prevented. Therefore, how to prevent surgical site errors is definitely a top priority in orthopedic surgery.
However, the current methods to prevent left and right dislocation in upper limb orthopedic surgery mainly use marking or barcode scanning. However, the above methods are still prone to many external factors. Therefore, this study, in cooperation with the orthopedic surgeons of the hospital, integrates medical and artificial intelligence technologies, and develops an intelligent image recognition system for the left and right parts of upper limb orthopedic surgery to replace the above-mentioned marking and barcode machine scanning methods.
In view of this, this study proposes an intelligent image recognition system for the left and right parts of upper limb orthopedic surgery. Through the image recognition of the upper limb in the image, it can be judged whether the left upper limb in the image is the left upper limb or the right upper limb. Through image recognition of the upper limbs and machine learning technology, the position of the left upper limb and the right upper limb can be judged, and then the doctor can be given the correct surgical position to help orthopedic surgeons prevent the occurrence of left and right dislocation in upper limb surgery. It is believed that the research results of this project will be considerable benefit and research value for upper limb orthopedic surgery.
In order to apply the research results to the clinical treatment of the hospital and implement the combination of theory and practice, this study not only used laboratory students to simulate patients as test objects in the prototype stage to complete the deep learning model, but also passed the IRB human body test. Apply for the experimental plan, carry out the second phase of human trials, and will implement IRB experiments in the future, so that it can be actually applied to clinical medical treatment in hospitals to achieve the so-called smart medical treatment.
In the future, we will continue to optimize the model architecture used for training, hoping to achieve the same results with lower layers and fewer neurons (nodes), so that the system requirements will be reduced, and the recognition speed will be further improved to be closer to practical applications. The hardware facilities of the scene make it run smoothly.
Author Contributions
Y.-C.W. was responsible for Conceptualization, Methodology, Investigation, Writing - Original Draft, and Writing - Review & Editing. C.-Y.C. was responsible for Resources and Software. Y.-T.U. was responsible for Validation and Formal analysis. S.-Y.C and C.-H.C. were responsible for Data Curation and Visualization. H.-K.K. was responsible for Supervision and Project Administration. All authors read and approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This is an observational study. The IRB was approved by the Chang Gung Memorial Hospital at Linkou, Taiwan. The IRB number is 202202226B0.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
This paper was supported by the National Science and Technology Council (NSTC) of Taiwan to National Yunlin University of Science and Technology under 111-2221-E-143-002.
Conflicts of Interest
The authors declare no conflict of interest.
References
- In: To Err is Human: Building a Safer Health System. edn. Edited by Kohn LT, Corrigan JM, Donaldson MS. Washington DC: 2000 by the National Academy of Sciences; 2000.
- https://www.patientsafety.mohw.gov.tw/Content/Downloads/List01.aspx?SiteID=1&MmmID=621273303702500244.
- H. Susanne, M.-G. Melinda, K. N. David, J. D. Aaron, M.-L. Isomi, M. B. Jessica, J. B. Marika, N. V. M. Jeremy, S. Roberta, and G. S. Paul, "Wrong-Site Surgery, Retained Surgical Items, and Surgical Fires : A Systematic Review of Surgical Never Events," JAMA Surgery, vol. 150, no. 8, pp. 796-805, 2015.
- P. Mark, J. B. Aaron, E. Sean, and H. D. Alan, "Wrong-site Spine Surgery," The Journal of the American Academy of Orthopaedic Surgeons, vol. 21, no. 5, pp. 312-320, 2013.
- O. Moshtaghi, Y. M. Haidar, R. Sahyouni, A. Moshtaghi, Y. Ghavami, H. W. Lin, and H. R. Djalilian, "Wrong-Site Surgery in California, 2007-2014," Otolaryngol Head Neck Surg., vol. 157, no. 1, pp. 48-52, 2017.
- C. Nunes and F. Pádua, "A Convolutional Neural Network for Learning Local Feature Descriptors on Multispectral Images," IEEE Latin America Transactions, Vol. 20, Issue 2, pp. 215-222, 2022. [CrossRef]
- Y. Qi, Y. Guo, and Y. Wang, "Image Quality Enhancement Using a Deep Neural Network for Plane Wave Medical Ultrasound Imaging," IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control, Vol. 68, Issue 4, pp. 926-934, 2021. [CrossRef]
- T. Hassanzadeh, D. Essam, and R. Sarker, "2D to 3D Evolutionary Deep Convolutional Neural Networks for Medical Image Segmentation," IEEE Transactions on Medical Imaging, Vol. 40, Issue 2, pp. 712-721, 2021. [CrossRef]
- Z. Duan, T. Zhang, J. Tan, and X. Luo "Non-Local Multi-Focus Image Fusion with Recurrent Neural Networks," IEEE Access, Vol. 8, pp. 135284-135295, 2020.
- Y. Tian, "Artificial Intelligence Image Recognition Method Based on Convolutional Neural Network Algorithm," IEEE Access, Vol. 8, pp. 125731-125744, 2020. [CrossRef]
- Y. Tan, M. Liu, W. Chen, X. Wang, H. Peng, and Y. Wang, "DeepBranch: Deep Neural Networks for Branch Point Detection in Biomedical Images," IEEE Transactions on Medical Imaging, Vol. 39, Issue 4, pp. 1195-1205, 2020. [CrossRef]
- A Waseem, M. David, and G. Andrea, "Limbs Detection and Tracking of Head-Fixed Mice for Behavioral Phenotyping Using Motion Tubes and Deep Learning," IEEE Access, vol. 8. pp. 37891-37901. 2020.
- Y. Zhang, S. Li, J. Liu, Q. Fan, and Y. Zhou, "A Combined Low-Rank Matrix Completion and CDBN-LSTM Based Classification Model for Lower Limb Motion Function," IEEE Access, vol. 8, pp. 205436-205443, 2020. [CrossRef]
- S. Javeed, C. F. Dibble, J. K. Greenberg, J. K. Zhang, J. M. Khalifeh, Y. Park, T. J. Wilson, E. L Zager, A. H Faraji, M. A. Mahan, L. J. Yang, R. Midha, N. Juknis, and W. Z. Ray, "Upper Limb Nerve Transfer Surgery in Patients With Tetraplegia", JAMA Network Open, Vol. 5, Issue 11, pp. 1-14, 2022. [CrossRef]
- M. Li, J. Guo, R. Zhao, J.-N. Gao, M. Li, and L.-Y. Wang, "Sun-Burn Induced Upper Limb Lymphedema 11 Years Following Breast Cancer Surgery: A Case Report", World Journal of Clinical Cases, Vol. 10, Issue 32, pp. 7-12, 2022. [CrossRef]
- W. Shi, J. Dong, J.-F. Chen, and H. Yu, "A Meta-Analysis Showing the Quantitative Evidence Base of Perineural Nalbuphine for Wound Pain From Upper-Limb Orthopaedic Trauma Surgery", International Wound Journal, pp. 1-15, 2022. [CrossRef]
- K. Chmelová and M. Nováčková, "Effect of manual lymphatic drainage on upper limb lymphedema after surgery for breast cancer”, Ceska Gynaecology, Vol. 87, Issue 5, pp. 317-323, 2022. [CrossRef]
- W. Johanna, R. Carina, and B.-K. Lina, "Linking Prioritized Occupational Performance in Patients Undergoing Spasticity-Correcting Upper Limb Surgery to the International Classification of Functioning, Disability, and Health", Occupational Therapy International, Vol. 2022, pp.1-11, 2022.
- T. Ramström, C. Reinholdt, J. Wangdell, and J. Strömberg, "Functional Outcomes 6 years After Spasticity Correcting Surgery with Regimen-Specific Rehabilitation in the Upper Limb", Vol. 48, Issue 1, Journal of Hand Surgery, pp. 54-55, 2022. [CrossRef]
- Y. Duan, G.-L. Wang, X. Guo, L.-L. Yang, and F. G. Tian, "Acute Pulmonary Embolism Originating from Upper Limb Venous Thrombosis Following Breast Cancer Surgery: Two Case Reports", World Journal of Clinical Cases, Vol. 10, Issue 21, pp. 8-13, 2022. [CrossRef]
- H.-Z. Zhang, Q.-L. Zhong, H.-T. Zhang, Q.-H. Luo, H.-L. Tang, and L.-J. Zhang, "Effectiveness of Six-Step Complex Decongestive Therapy for Treating Upper Limb Lymphedema After Breast Cancer Surgery", World Journal of Clinical Cases, Vol. 10, Issue 25, pp. 7-16, 2022. [CrossRef]
- E. A. Stanley, B. Hill, D. P. McKenzie, P. Chapuis, M. P. Galea, and N. V. Zyl, "Predicting Strength Outcomes for Upper Limb Nerve Transfer Surgery in Tetraplegia", Journal of Hand Surgery, Vol.47, Issue 11, pp.1114-1120, 2022.
- H. Alsajjan, N. Sidhoum, N. Assaf, C. Herlin, and R. Sinna, "The Contribution of the Late Dr. Musa Mateev to the Field of Upper Limb Surgery with the Shape-Modified Radial Forearm Flap", Annales de Chirurgie Plastique Esthétique, Vol. 67, Issue 4, pp.196-201, 2022.
- T. Redemski, D. G. Hamilton, S. Schuler, R. Liang, and Z. A. Michaleff, "Rehabilitation for Women Undergoing Breast Cancer Surgery: A Systematic Review and Meta-Analysis of the Effectiveness of Early, Unrestricted Exercise Programs on Upper Limb Function", Clinical Breast Cancer, Vol. 22, Issue 7, pp. 650-665, 2022.
- V. Meunier, O. Mares, Y. Gricourt, N. Simon, P. Kuoyoumdjian, and P. Cuvillon, "Patient Satisfaction After Distal Upper Limb Surgery Under WALANT Versus Axillary Block: A Propensity-Matched Comparative Cohort Study", Hand Surgery and Rehabilitation, Vol. 41, Issue 5, pp. 576-581, 2022. [CrossRef]
- Q. Luo, H. Liu, L. Deng, L. Nong, H. Li, Y. Cai, and J. Zheng, "Effects of Double vs Triple Injection on Block Dynamics for Ultrasound-Guided Intertruncal Approach to the Supraclavicular Brachial Plexus Block in Patients Undergoing Upper Limb Arteriovenous Access Surgery: Study Protocol for a Double-Blinded, Randomized Controlled Trial", Trials, Vol. 23, Issue 1, pp.295, 2022. [CrossRef]
- M. Manna, W. B. Mortenson, B. Kardeh, S. Douglas, C. Marks, E. M. Krauss, and M. J. Berger, "Patient Perspectives and Self-Rated Knowledge of Nerve Transfer Surgery for Restoring Upper Limb Function in Spinal Cord Injury", PM&R, Online Ahead of Print, 2022. [CrossRef]
- S. Beiranvand, M. Alvani, and M. M. Sorori, "The Effect of Ginger on Postoperative Nausea and Vomiting Among Patients Undergoing Upper and Lower Limb Surgery: A Randomized Controlled Trial", Journal of PeriAnesthesia Nursing, Vol. 37, Issue 3, pp.365-368, 2022. [CrossRef]
- Y. Gao, P. Dai, L. Shi, W. Chen, W. Bao, L. He, and Y. Tan, "Effects of Ultrasound-Guided Brachial Plexus Block Combined with Laryngeal Mask Sevoflurane General Anesthesia on Inflammation and Stress Response in Children Undergoing Upper Limb Fracture Surgery", Minerva Pediatrics, Vol. 74, Issue 3, pp.385-387, 2021. [CrossRef]
- A. ashidi, J. Grantner, I. Abdel-Qader, and S. A Shebrain, "Box-Trainer Assessment System with Real-Time Multi-Class Detection and Tracking of Laparoscopic Instruments, using CNN Box-Trainer Assessment System with Real-Time Multi-Class Detection and Tracking of Laparoscopic Instruments, using CNN", Acta Polytechnica Hungarica, Vol. 19, Issue 2, pp.2022-2029, 2022. [CrossRef]
- X. Zhang and H. Wang, "Research on YOLOv4 Detection Algorithm Based on Lightweight Network", Computer Science and Application, Vol. 11, Issue 9, pp.2333-2341, 2021.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).