1. Introduction
The field of total hip arthroplasty (THA) is undergoing rapid transformation due to several factors, including the increasing age of the population, advancements in surgical methodologies, and the emergence of novel implant materials. Nevertheless, this advancement is not without its own set of obstacles, primarily the rising prevalence of periprosthetic femoral fractures (PFFs) [
1,
2]. Fractures, whether they occur during surgery or after surgery, impose a considerable clinical burden, frequently resulting in unfavorable outcomes, elevated reoperation rates, and heightened mortality. The objective of this article is to explore the intricacies surrounding PFFs, encompassing their epidemiology and classification systems, as well as the most recent treatment approaches and risk factors. By doing so, this article provides healthcare professionals with a comprehensive resource for effectively managing this complex complication [
1,
3].
The prevalence of periprosthetic femoral fractures (PFFs) exhibits considerable variation, with estimates ranging from 1% to 11% for primary total hip arthroplasty (THA) and up to 18% for revised hip femoral stems. The variability is further compounded by the expanding indications for total hip arthroplasty (THA), which currently encompass not only younger patients with elevated functional demands but also older patients with concurrent medical conditions [
4,
5]. The phenomenon of an aging population has resulted in a notable increase in total hip arthroplasty (THA) surgeries, which in turn has led to a rise in postoperative periprosthetic femoral fractures (PFFs). Research indicates that individuals who are 85 years of age or older are especially susceptible to adverse effects following a hip fracture, including diminished functional outcomes and elevated mortality rates [
6,
7].
The utilization of classification systems such as the Vancouver classification, along with its more recent incorporation into the Unified Classification System for Periprosthetic Fractures (UCS-PF), has played a crucial role in providing guidance for treatment strategies. Nevertheless, it is important to acknowledge that these systems do have certain limitations. For example, there is a frequent failure to accurately document fractures that are treated without surgery or those that undergo open reduction and internal fixation (ORIF), resulting in an underestimation of the actual occurrence of proximal femoral fractures (PFFs) [
8,
9,
10].
The selection of implants also significantly influences the incidence of periprosthetic femoral fractures (PFFs). Cementless stems exhibit a significantly elevated incidence of intraoperative fractures, approximately 14 times greater than that observed in cemented stems [
3,
12]. Moreover, the design characteristics of cemented stems, such as the choice between taper-slip and composite beam designs, have been demonstrated to have a substantial influence on the likelihood of periprosthetic femoral fractures (PFFs), although there is a scarcity of data available on this particular topic [
8,
10,
13].
An additional crucial factor to consider is the influence of sarcopenia and osteoporosis on the elderly population, rendering them more prone to falls and less capable of withstanding impact. Consequently, this elevates the likelihood of experiencing proximal femoral fractures (PFFs) [
7,
14]. This article aims to examine the present understanding of PFFs, taking into account their growing prevalence, the developing classification systems, the influence of implant selection, and the significance of patient-specific risk factors. The objective of this study is to present a comprehensive perspective on proximal femoral fractures (PFFs), equipping healthcare professionals with the necessary resources to effectively address this complex and frequently debilitating condition.
2. Materials and Methods
This article presents a retrospective analysis of periprosthetic femoral fractures (PFFs) that were treated at clinic of the Bucharest University Emergency Hospital. The duration of the study spanned from August 2022 to August 2023.
This study comprised a cohort of nine patients diagnosed with Vancouver B2 and B3 fractures. The selection of these cases was deliberate, as they effectively exemplify the intricacies and difficulties inherent in PFFs. The study included a cohort of patients who possessed comprehensive clinical and radiographic records, which were examined retrospectively. The study population consisted of individuals of both genders, encompassing a wide range of ages, which is consistent with the main focus of this article. All surgical procedures were conducted by highly experienced senior surgeons at our clinic, possessing extensive expertise in the fields of orthopedics and traumatology.
Although not explicitly mentioned in the original text, it is pertinent to consider the specific arthroplasty procedure that each patient had undergone prior to the occurrence of the fracture, as well as the characteristics of the trauma that caused the fracture (low-energy versus high-energy), as these variables have the potential to impact the outcomes of treatment.
The selection between general anesthesia and lumbar anesthesia was determined by considering the patient's personal preference and the complexity of the case. The patients in the study underwent treatment via a lateral approach involving open reduction and internal fixation (ORIF) utilizing a locking compression plate (LCP) that was secured in place using screws and cerclage cables.
The fractures were categorized based on the Vancouver classification system. In the most recent follow-up, the assessment of clinical outcomes was conducted utilizing the Harris Hip Score (NHS), while the evaluation of radiographic outcomes was performed based on specific criteria aimed at determining the degree of fracture healing and the stability of the implant.
The initiation of physical rehabilitation for patients commenced on the day following the surgical procedure, with the initial focus being on assuming sitting positions. Partial weight-bearing was authorized at the end of a two-week period, with a gradual transition to full weight-bearing by the conclusion of six weeks.
Through the implementation of this rigorous methodology, our objective is to make a meaningful contribution to the understanding and management of PFFs. This will ultimately assist clinicians in navigating the intricate and frequently catastrophic nature of this condition, enhancing their decision-making capabilities.
3. Case series presentation and results
Periprosthetic fractures occurring at the femoral stem level, specifically classified as Vancouver B fractures, present a multifaceted and demanding clinical situation that frequently requires surgical intervention. Fractures in the vicinity of a prosthetic implant are classified into B1, B2, and B3 subtypes, which are determined by the stability of the implant and the condition of the surrounding bone tissue. The management of these fractures presents a complex challenge due to the presence of a pre-existing implant, which introduces complications in both the diagnostic process and the formulation of an appropriate treatment plan.
The Vancouver B fractures pose a variety of risks that encompass both immediate and long-term consequences. Immediate concerns include pain and immobility, while long-term complications may involve implant failure, non-union, and potentially sepsis. The inclusion of a prosthetic implant introduces an additional level of intricacy, as it can exhibit either stability or looseness, necessitating distinct surgical methodologies. Furthermore, it is important to consider the patient's general health status, age, and presence of other medical conditions, as these factors can have a substantial impact on the results of surgical interventions. Consequently, adopting a uniform treatment strategy that applies to all patients becomes unfeasible.
Due to the significant consequences involved, surgical intervention frequently emerges as the most feasible course of action for the restoration of function and alleviation of pain. The selection of surgical technique for treating Vancouver B fractures is contingent upon the particular type of fracture, and may involve internal fixation utilizing plates and screws, cerclages, or revision arthroplasty with an extended prosthesis. Hence, it is imperative to possess a comprehensive comprehension of these fractures, which should be substantiated by radiographic assessment and in accordance with contemporary medical literature, in order to achieve the most effective patient care.
3.1. Vancouver B1
Periprosthetic femoral fractures (PFFs) in Vancouver Bl classification pose distinct challenges that frequently require surgical intervention. Fractures of this nature manifest in the vicinity of a stable stem and can exhibit either displacement or lack thereof. Although conservative management may be an option for certain undisplaced fractures, surgical intervention is typically the preferred approach when the patient is deemed eligible for surgery. There exists a wide array of surgical options, encompassing a spectrum of techniques such as minimally invasive plate osteosynthesis (MIPO) and open reduction and internal fixation (ORIF). The selection of these methods is contingent upon several factors, such as the imperative for achieving anatomical reduction, the need for cerclaging around the stem, and the potential necessity for structural graft augmentation.
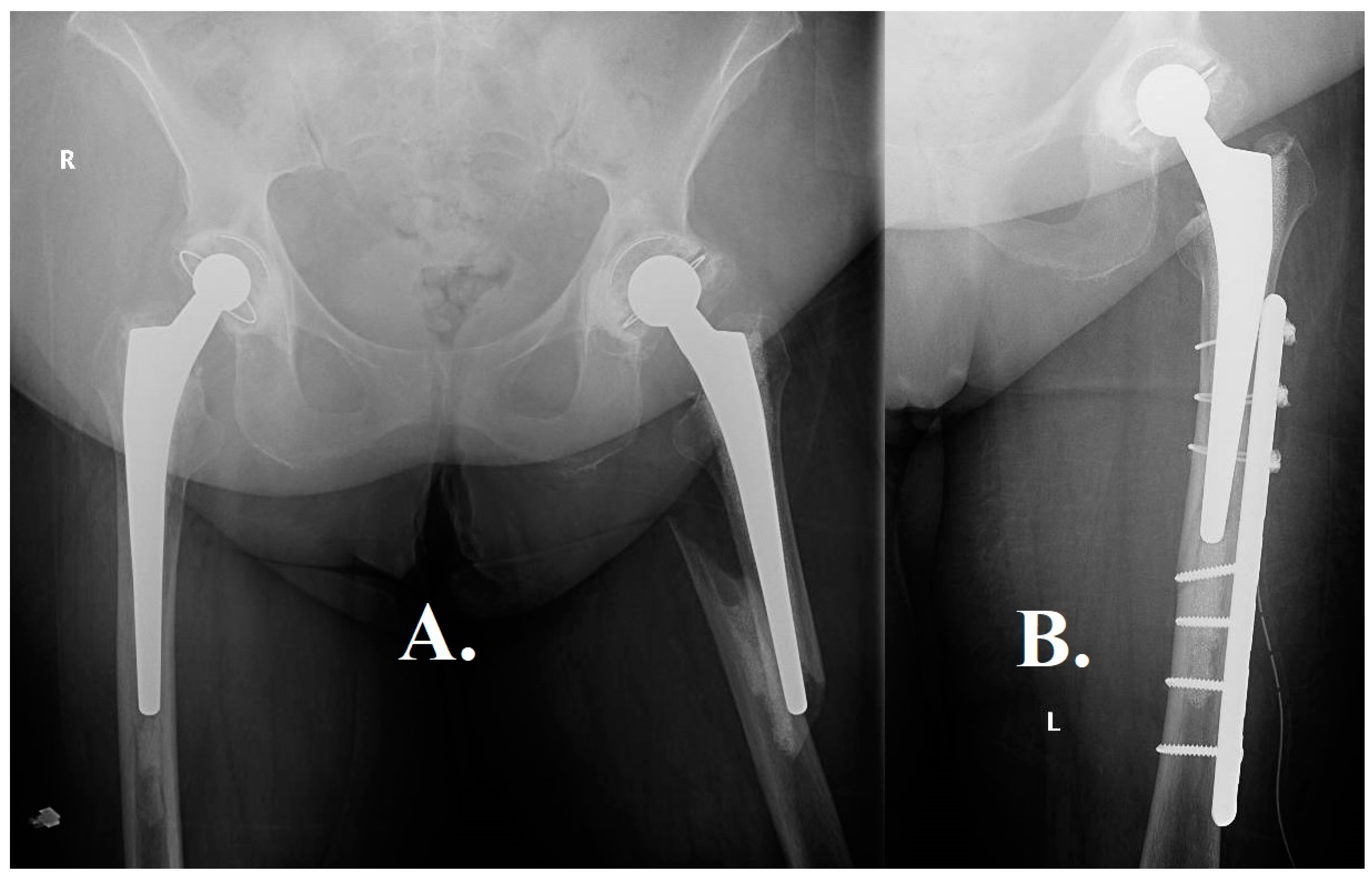
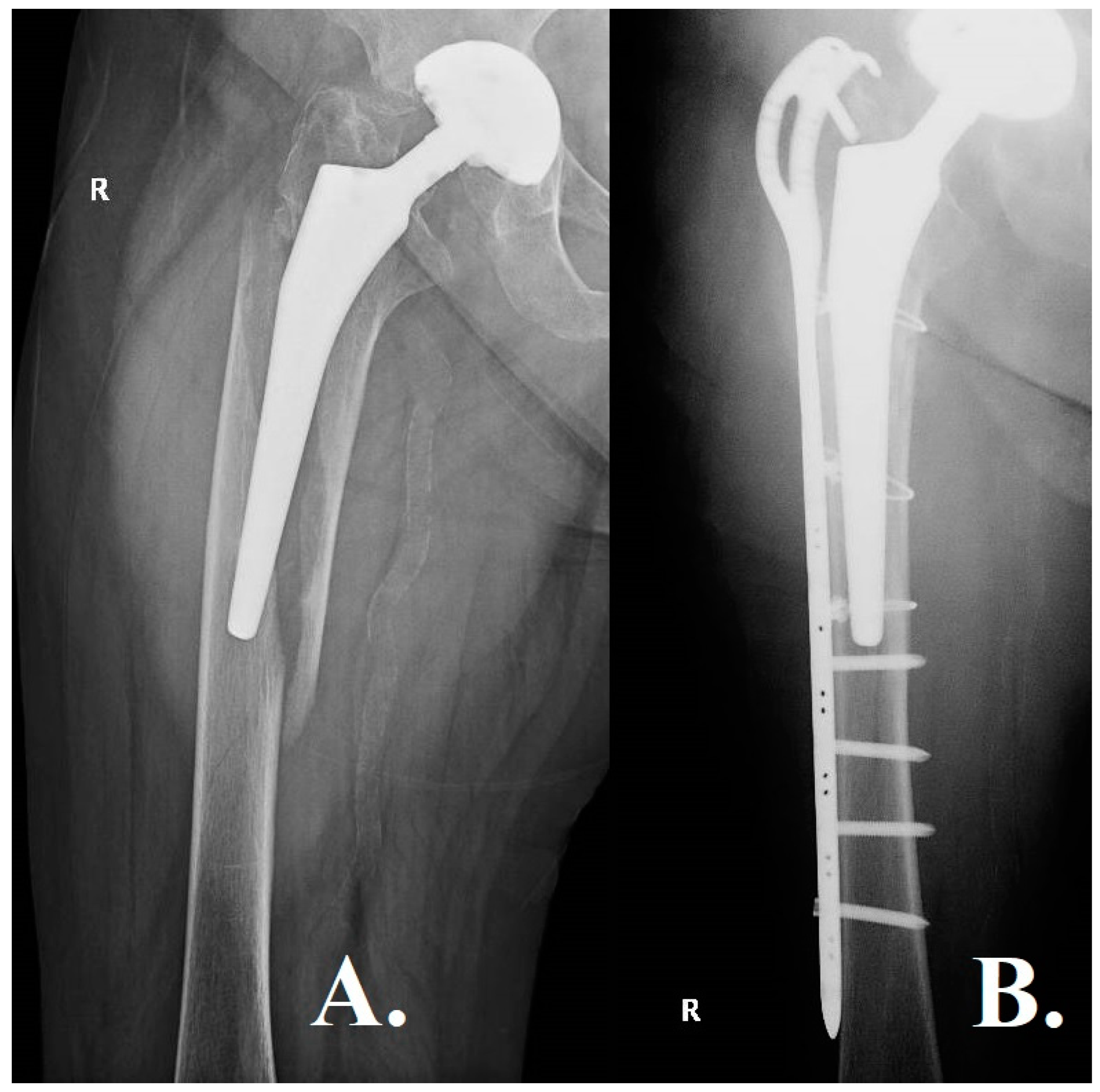
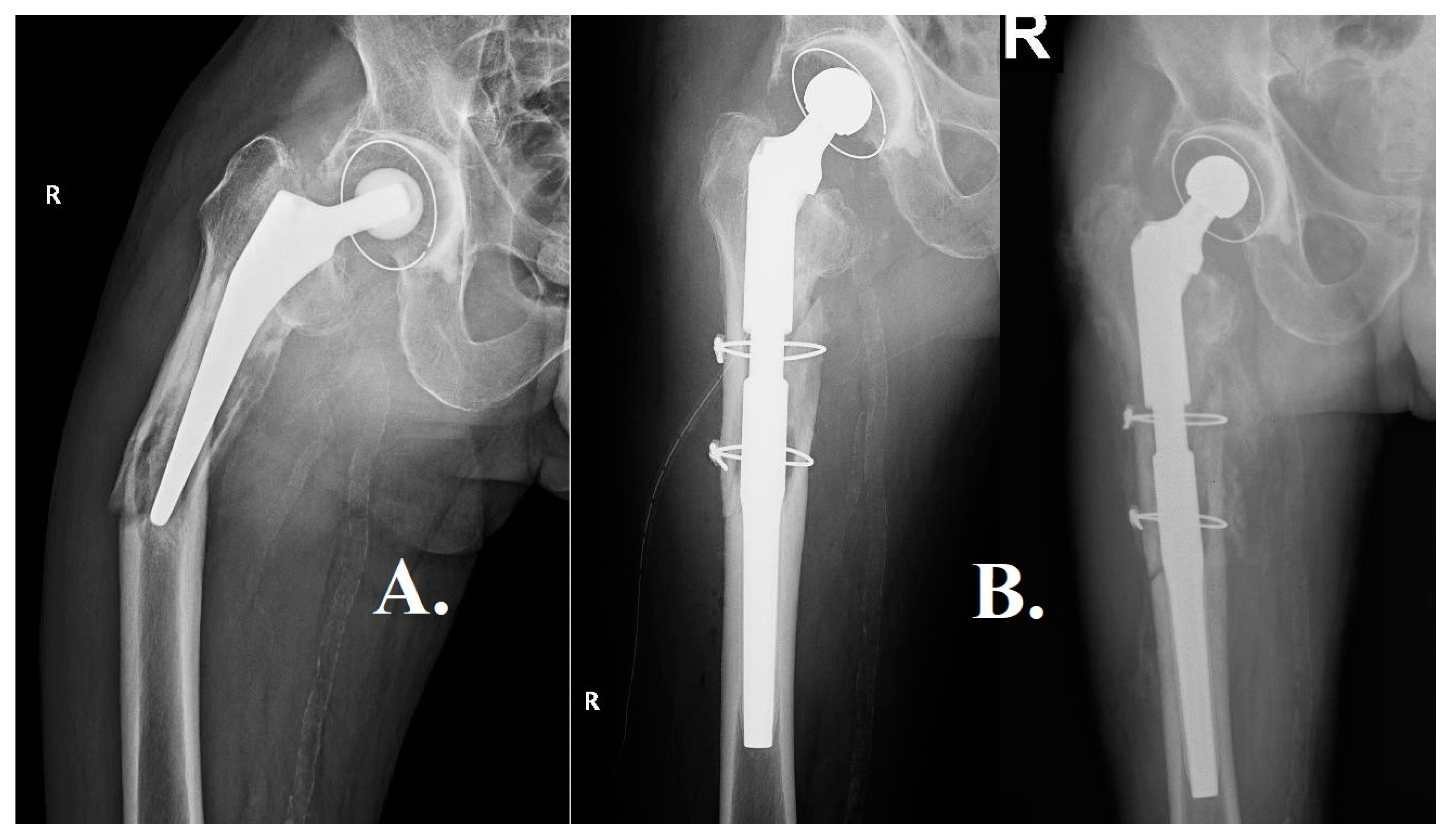
The selection of a plate fixation approach (
Figure 1) was made due to the stability of the cemented stem in a case concerning a 76-year-old patient with a total hip prosthesis that had been cemented. This decision is consistent with the prevailing literature, which suggests a predilection for plate fixation in approximately 90% of similar instances. The postoperative outcomes of the patient were in line with anticipated results, highlighting the effectiveness of this method for older patients with stable, cemented prostheses.
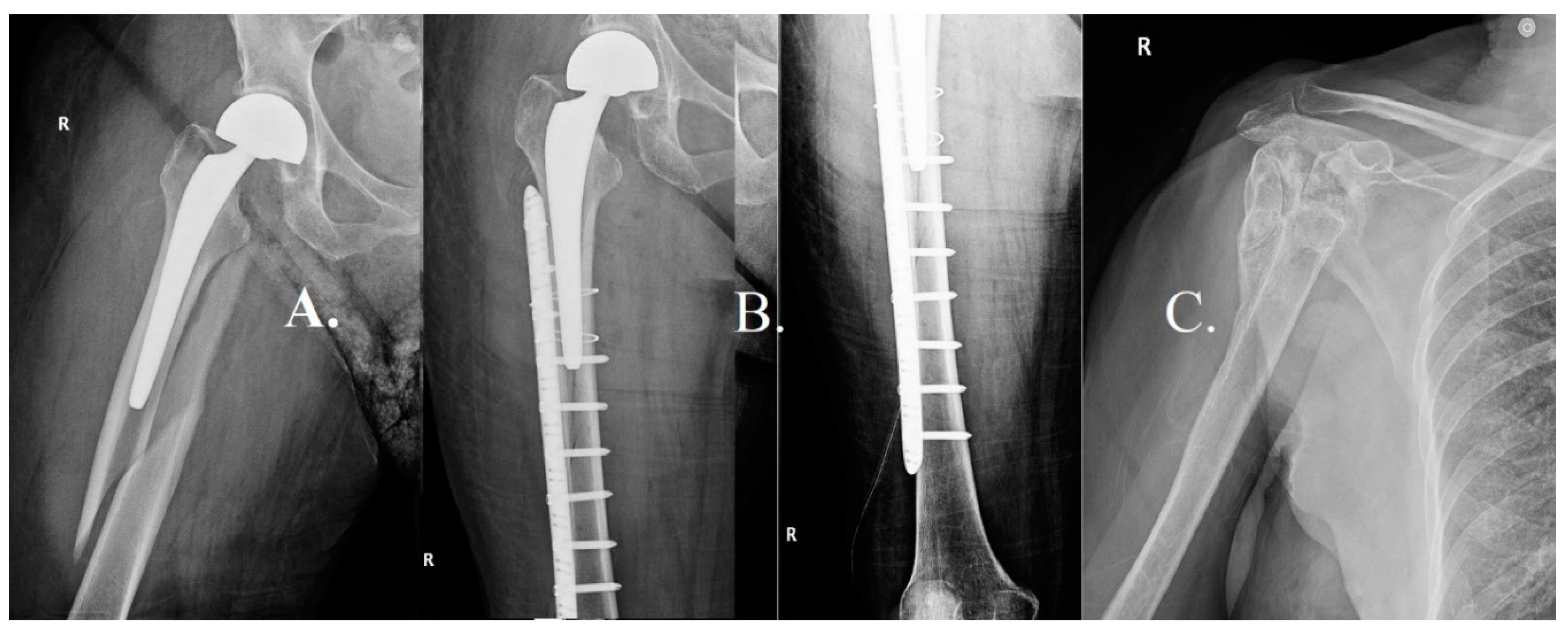
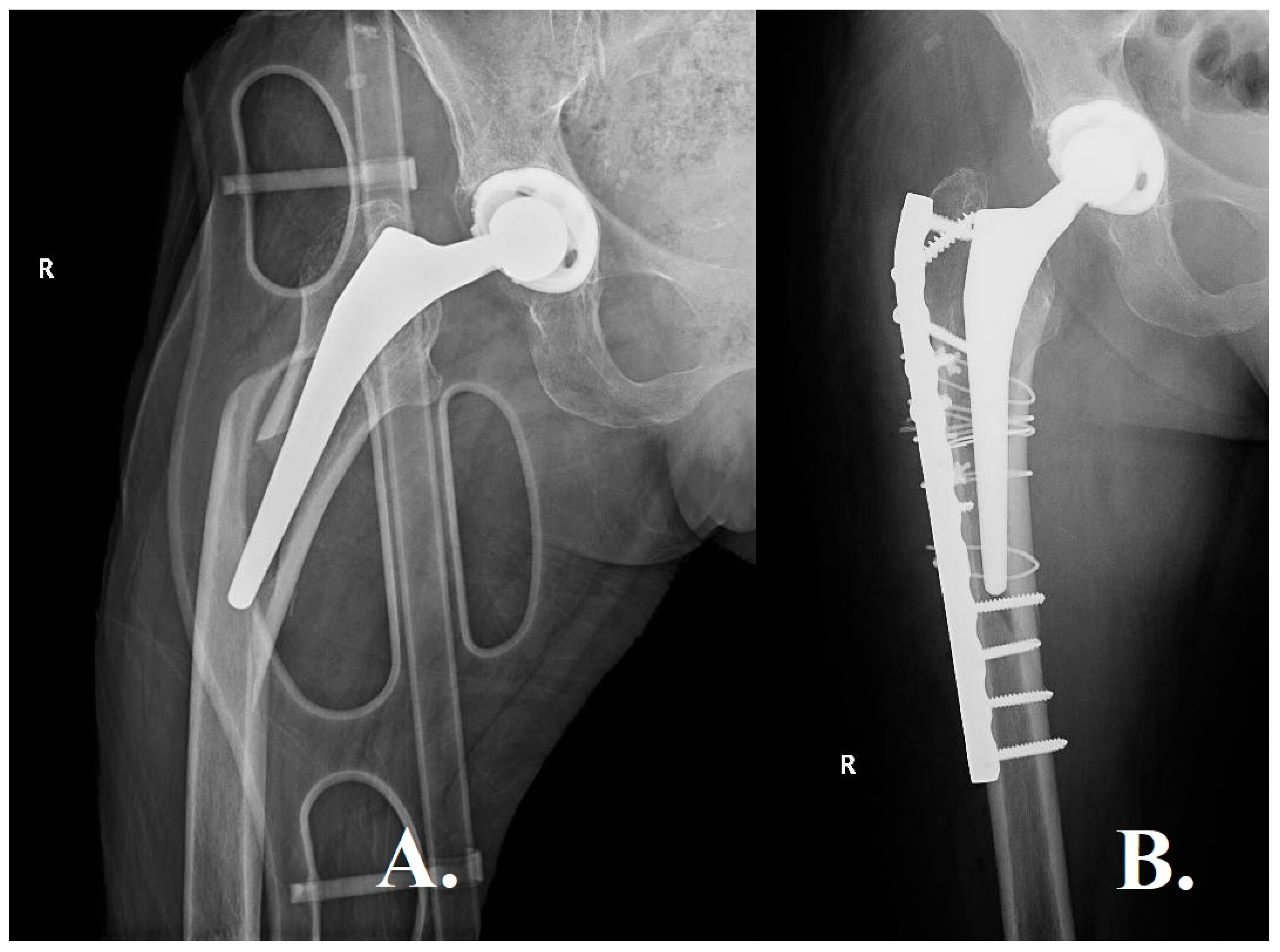
Another case study involved an octogenarian patient with a bipolar prosthesis. Due to the patient's advanced age and the specific characteristics of the prosthesis, a meticulous customization of the surgical approach was necessary. The case presented in
Figure 2 highlights the evident complexities associated with managing B1 fractures in patients who have various types of prostheses, including a bipolar prosthesis.
The aforementioned case serves as an illustration of the intricate nature of handling Vancouver B1 fractures in older individuals who have multiple comorbidities, such as cognitive impairments. The statement underscores the importance of adopting a nuanced and personalized treatment strategy that carefully considers the potential risks associated with surgery while also prioritizing the effective management of fractures.
A notably arduous circumstance emerged in a patient who underwent a B1 fracture while undergoing the revision of a preexisting prosthesis. The fracture that occurred during the revision procedure introduced an additional level of intricacy, necessitating careful surgical strategizing in order to mitigate the risk of subsequent complications (see
Figure 3). This particular case serves as an instructive example, underscoring the potential hazards inherent in prosthesis revision surgeries.
Several fracture characteristics, such as transverse or short oblique patterns, medial comminution, or occurrence over a cemented stem, have the potential to diminish both the mechanical and biological healing capabilities. In these particular cases, the suggestion has been made to consider a revision procedure involving the elongation of the stem, potentially combined with the use of a structural allograft, as a means to decrease the likelihood of fixation failure.
3.2. Vancouver B2
Orthopedic surgery encounters distinctive challenges when dealing with Vancouver B2 fractures. In contrast to B1 fractures, which typically present in the vicinity of a secure femoral stem, B2 fractures are characterized by their occurrence in the presence of an unstable stem, often necessitating a more complex surgical intervention. The intricacy of these fractures is additionally amplified by the requirement for both fracture fixation and prosthesis revision, underscoring the importance of preoperative planning in achieving favorable results.
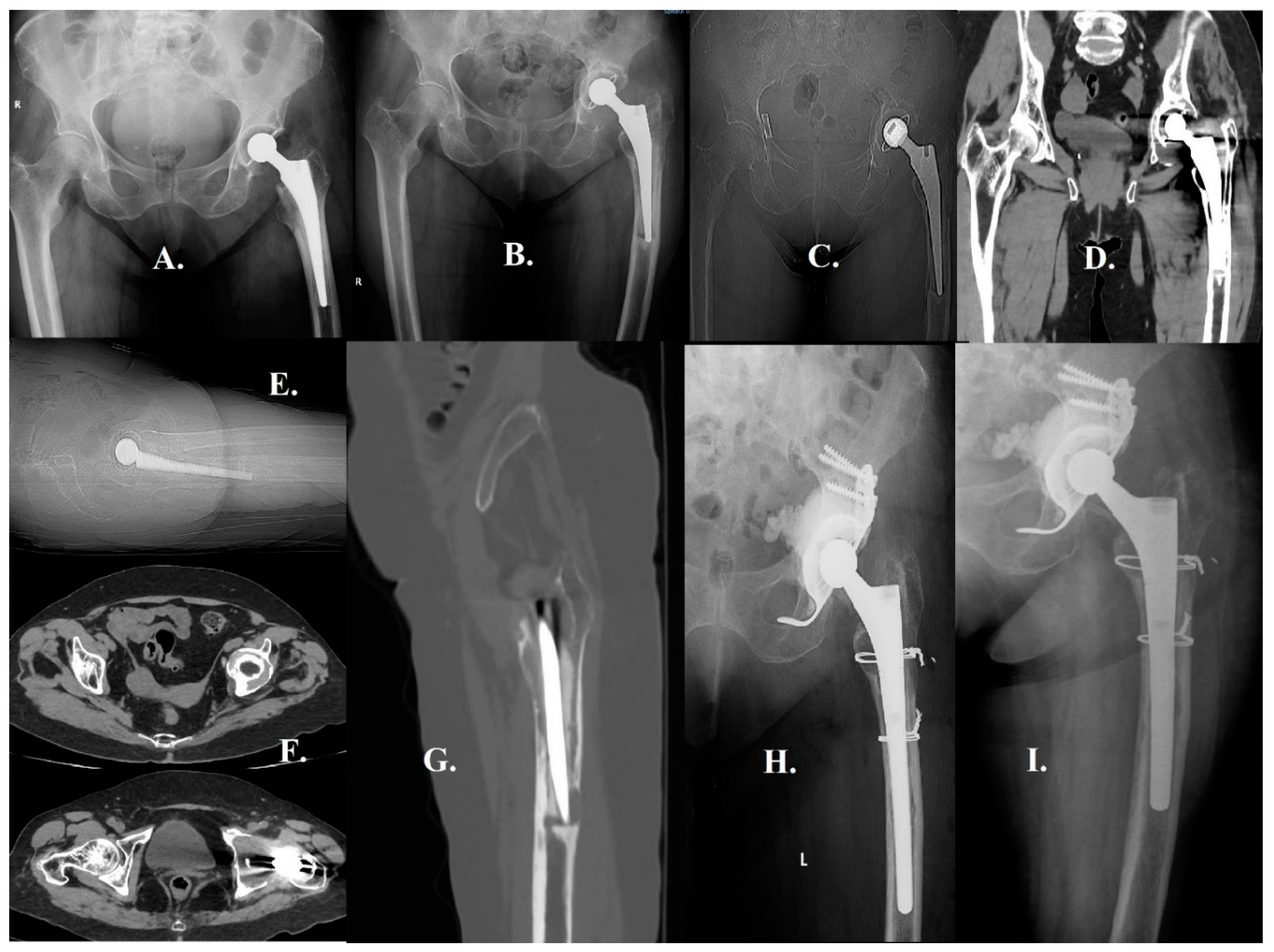
Within the framework of our ongoing discourse regarding Vancouver B2 fractures in Vancouver, we analyze the instance of a 56-year-old individual with a medical background of chronic renal pathology since early life, which has required prolonged administration of corticosteroids. As a result of the presence of comorbidities, the patient experienced the onset of advanced coxarthrosis at the relatively young age of 48, leading to the necessity of undergoing an uncemented total hip arthroplasty procedure. Notwithstanding medical counsel advising otherwise, the individual persisted in participating in athletic endeavors, taking into consideration his comparatively youthful age and vigorous physiological state. The patient, experienced a spiroid fracture during a skiing activity, as illustrated in
Figure 4.
The treatment of Vancouver B2 periprosthetic femoral fractures in the Vancouver classification system is frequently complicated by the presence of comorbidities in the patient and the mechanical stability of the current implant. In this study, we investigate the case of an octogenarian female patient who, approximately twelve years ago, underwent a cemented total hip arthroplasty procedure to address coxarthrosis. Subsequently, the patient's medical background has become more intricate due to the presence of hypertension, diabetes mellitus, New York Heart Association (NYHA) Class 3 chronic heart failure, and notable cerebrovascular stenosis affecting her carotid arteries. After experiencing an episode of lipothymia, the patient exhibited a multifaceted, lengthy spiral fracture that spanned from the greater trochanter to a location roughly 2 cm below the femoral stem (as depicted in
Figure 5). Typically, the femoral artery is not discernible on conventional radiographic imaging of the hip and femur. The observed visibility indicates the presence of notable vascular pathology. After carefully considering the patient's complex medical history and the unstable nature of the fracture as observed through radiological imaging, it was deemed prudent to exclude the option of a high-risk surgical revision of the femoral component. Alternatively, a surgical approach that was both conservative and efficacious was implemented. The significance of tailoring treatment plans to the specific needs of patients with Vancouver B2 fractures, especially in geriatric individuals with multiple medical comorbidities, is emphasized by this approach. The postoperative course of the patient has demonstrated positive outcomes, thereby confirming the effectiveness of this individualized approach.
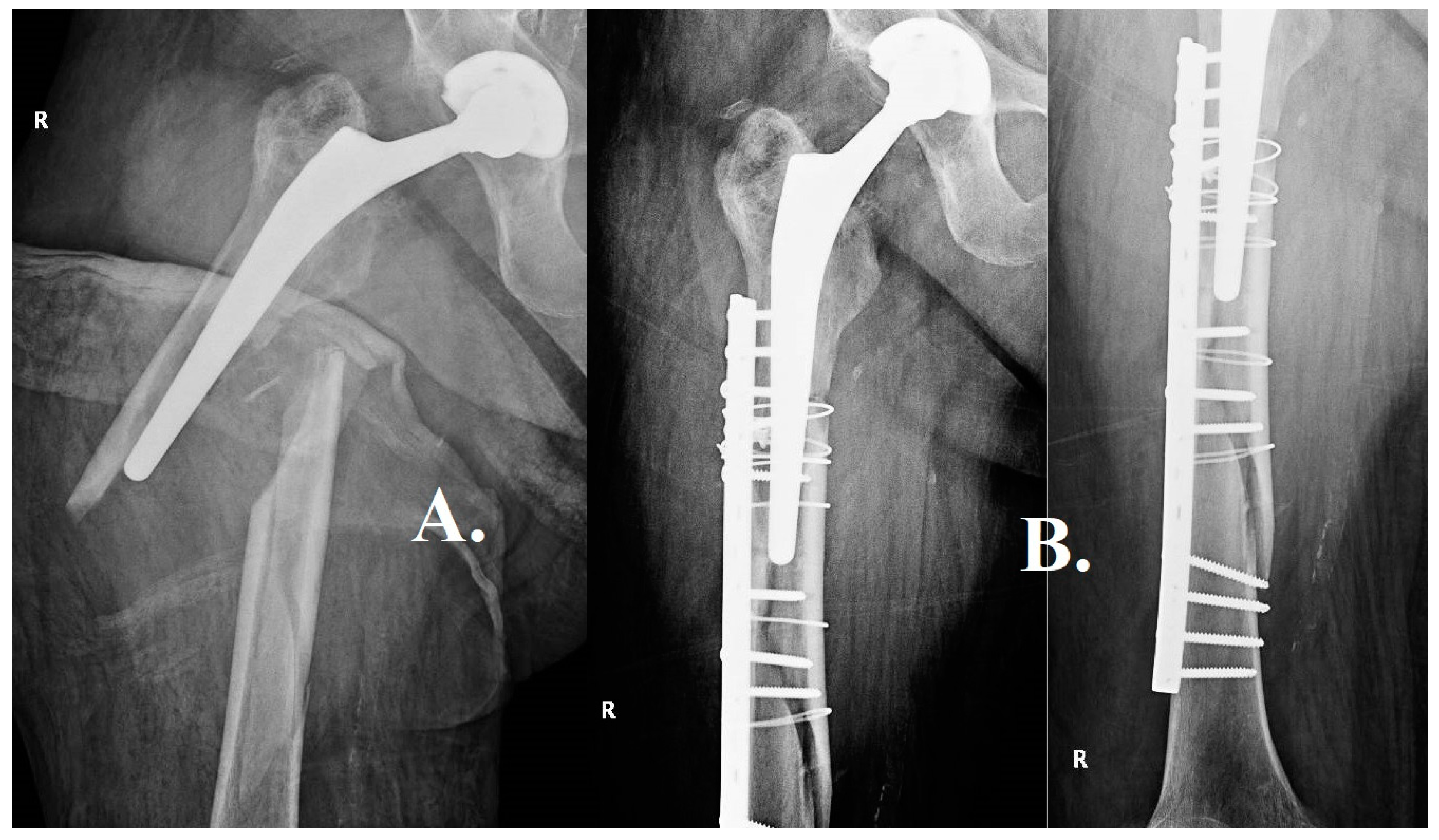
The case of septuagenarian individual of 77 years of age, presenting with a seven-year-old unsecured total hip prosthesis. The individual experienced a periprosthetic femoral fracture subsequent to a descent down a set of stairs. The fracture exhibited a spiral pattern and encompassed an intricate "butterfly wing" element, thereby introducing an extra level of intricacy to the already demanding clinical situation (
Figure 6). In the specific context of Vancouver B2 fractures, this particular case holds significant importance due to various reasons. The presence of a spiral configuration in the fracture, along with the inclusion of a butterfly wing component, indicates a considerable degree of instability. Consequently, the successful management of such a fracture necessitates meticulous surgical planning and precise execution. Furthermore, the age of the patient and the length of time since the initial hip replacement introduce an additional level of intricacy. Although the uncemented prosthesis has presumably attained satisfactory biological fixation over time, the integrity of the adjacent bone stock may be compromised as a result of osteoporosis associated with aging. Therefore, it is imperative to conduct a meticulous assessment of bone quality during the process of surgical planning in order to guarantee that the selected method of fixation will offer sufficient stability.
3.3. Vancouver B3
Vancouver B3 periprosthetic femoral fractures (PFFs) pose significant challenges within the field of orthopedic surgery. These fractures exhibit an unstable stem and insufficient bone quality, which pose challenges for surgical planning and postoperative recuperation. The limited bone supply frequently hinders the use of simple fixation techniques, leading to the need for more intricate surgical procedures like long stem revision, allograft-prosthetic composites (APCs), or even proximal femoral replacement. Other fixation techniques, such as the use of extramedullary cortical strut grafts, have been recommended to improve stability and facilitate bone healing, especially in situations where there is insufficient bone supply. These grafts are a valuable addition to intramedullary fixation systems, particularly due to the extended duration required for the incorporation and remodeling of such grafts, which can span up to one year. In patients with low demand, the utilization of a distally locked stem could be considered as a potential salvage intervention. Double mobility implants are frequently employed in conjunction with these constructs in order to enhance joint stability. Successfully managing Vancouver B3 fractures necessitates employing a sophisticated strategy that encompasses an in-depth analysis of not only the fracture's specific attributes but also the patient's comprehensive health condition, coexisting medical conditions, and way of life.
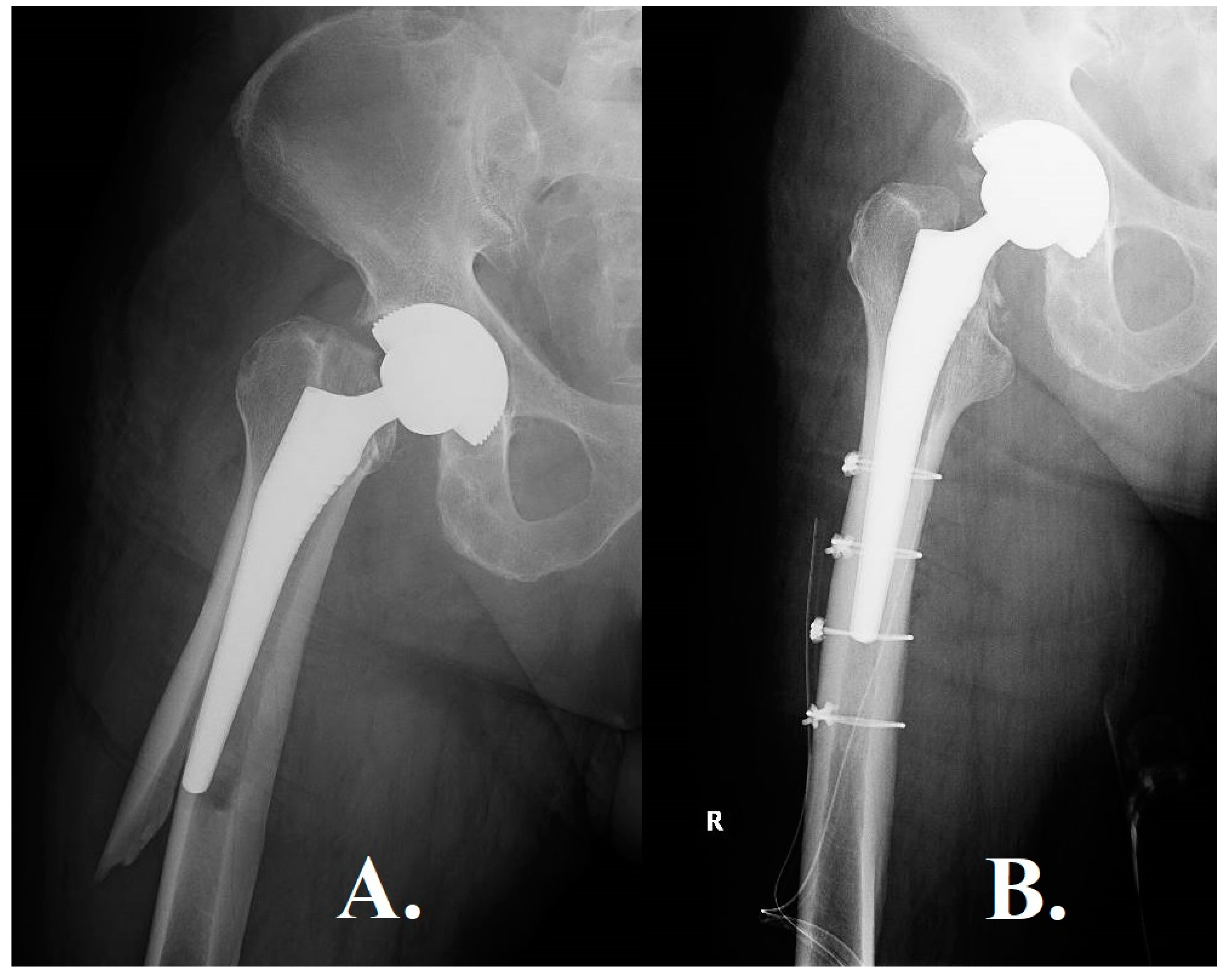
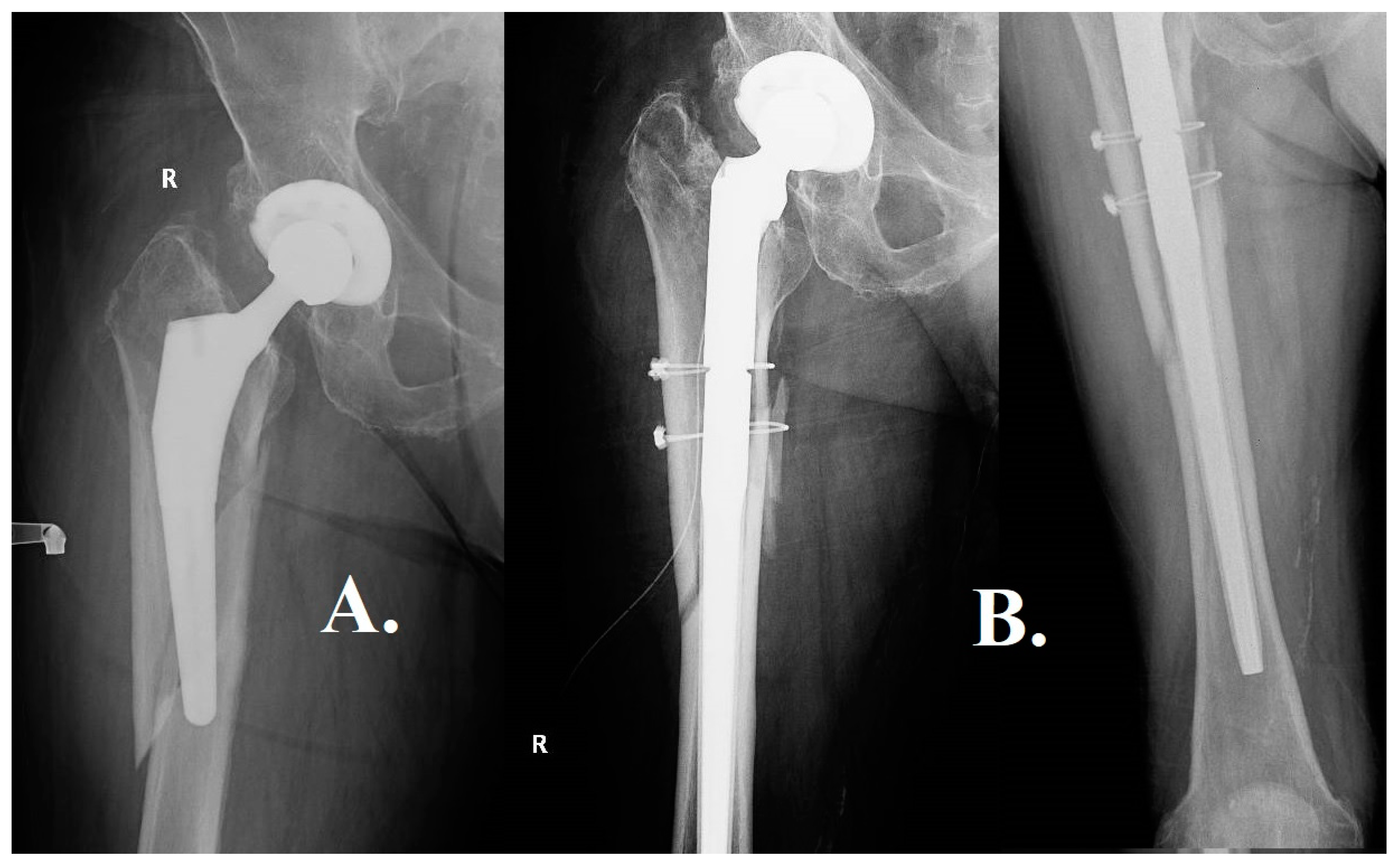
The initial case involves a patient who is 90 years old and has a medical background of undergoing an uncemented total hip arthroplasty procedure 15 years ago. The presence of morbid obesity in the patient, as evidenced by a body mass index (BMI) of 33, introduces an additional level of intricacy in the process of making surgical decisions. The radiographic results demonstrate a lengthy, fragmented spiral fracture with a butterfly fragment, suggesting substantial instability and a reduction in bone density (
Figure 7). Based on the patient's age and obesity, the surgical team made the decision to perform fracture reduction and fixation utilizing a plate and screws, without modifying the femoral component. The objective of this approach was to reduce the potential hazards associated with surgery while ensuring sufficient stabilization.
The second case pertains to an individual of comparatively younger age, specifically a 74-year-old patient, who maintains an active lifestyle and does not exhibit any notable coexisting medical conditions. The individual in question had previously undergone surgical intervention for coxarthrosis approximately ten years ago and has since maintained a physically active lifestyle without experiencing any notable issues (
Figure 8). The traumatic incident transpired when the individual was in pursuit of public transportation, leading to a fall from their own level. This particular case serves as a compelling illustration of the complex surgical planning that is necessary for effectively managing Vancouver B3 fractures. The decision to modify the femoral component demonstrates an awareness of the necessity for strong mechanical stability, considering the fragmented and displaced characteristics of the fracture. Cerclages are employed to enhance stability, thereby augmenting the probability of achieving successful union of fractures.
The third case involves an octogenarian patient who underwent cemented total hip arthroplasty approximately nine years ago. The patient possesses a notable medical background characterized by the presence of atrial fibrillation (AF) and deep vein thrombosis (DVT). The radiographic evidence reveals the presence of peri-implant lysis surrounding the femoral component, which is further supported by the patient's reported experience of mild pain during movement (
Figure 9). The occurrence of the fracture transpired when the patient experienced a loss of consciousness during the act of rising from a seated position. The presented case serves as an illustration of the intricate decision-making process involved in the management of complex Vancouver B3 fractures in the context of peri-implant lysis. The surgical approach needed to consider the concurrent issues of acute mechanical instability and compromised bone quality, leading to the requirement for a revision of the femoral component. The implementation of a thicker, uncemented modular stem and the incorporation of supplementary cerclages exemplify a holistic strategy designed to enhance both initial stability and the eventual healing of fractures over an extended period.
4. Discussion
The management of periprosthetic femoral fractures (PFFs) following total hip arthroplasty (THA) continues to present a multifaceted dilemma within the field of orthopedic surgery. This research, carried out at Bucharest University Emergency Hospital, examines a sample of nine cases in order to gain insights into the complexities of PFFs. The study primarily focuses on the epidemiology, classification, treatment modalities, and patient-specific risk factors associated with these fractures. The absence of algorithms that are universally accepted for the management of PFFs adds further complexity to the clinical environment [
10,
15].
Our study substantiates the increasing incidence of proximal femoral fractures (PFFs), particularly among individuals belonging to an aging demographic. The study additionally emphasizes the growing prevalence of "type B fractures," which constitute 90% of fractures occurring after surgery and 70% of fractures occurring during surgery. The Vancouver classification system, which is commonly employed to guide treatment choices, demonstrated a satisfactory degree of agreement among observers for UCS type B fractures (k=0.76). Nonetheless, the differentiation between B1 and B2 fractures presents difficulties as a result of constraints in preoperative X-ray assessments (k=0.64) [
16].
The research highlights the significance of patient-specific factors, such as sarcopenia and osteoporosis, in augmenting the susceptibility of older individuals to proximal femoral fractures (PFFs). The study found that elderly patients with Vancouver B type fractures who underwent open reduction and internal fixation (ORIF) had decreased mortality rates and similar hospital stays, regardless of whether the initial stem was press-fit or cemented [
17]. This observation is consistent with prior research that has documented an increasing incidence of proximal femoral fractures (PFFs) in the elderly population.
Our study makes a valuable contribution to the ongoing discourse surrounding the effectiveness of open reduction internal fixation (OR1F) compared to revision arthroplasty in the treatment of Vancouver B2 and B3 fractures. The primary variables assessed encompassed implant subsidence, subsequent revision surgeries, estimated blood loss (EBL), and one-year mortality rates. There were no statistically significant differences observed between the groups that received cemented implants and those that received press-fit implants [
3,
10,
17]. Furthermore, the research findings suggest an upward trajectory in the utilization of cemented and hybrid prostheses, while the adoption of uncemented implants remains consistent [
18].
According to Quah et al. (6), the authors propose that open reduction and internal fixation (ORIF) with anatomic alignment is a viable treatment option for B type fractures, provided that the cement mantle remains intact and there is an adequate amount of bone stock available. Nevertheless, there is a presence of contradictory evidence regarding the effects of cemented and uncemented stems on outcomes [
17,
19].
The Vancouver classification system, despite its widespread recognition, possesses certain limitations, notably its incapacity to encompass fractures that are managed without surgical intervention. Additional research is warranted in order to establish a more comprehensive classification system that has the potential to enhance the effectiveness of treatment. Recent research has indicated that ORIF (open reduction and internal fixation) may yield positive outcomes, particularly in older populations or individuals with comorbidities [
20,
21]. As an example, a comprehensive analysis revealed that out of a total of 343 B2 fractures, 86.8% of cases were subjected to revision arthroplasty, while 12.6% were treated solely with open reduction and internal fixation (ORIF). Similarly, among 167 B3 fractures, revision arthroplasty was performed in 95.8% of cases, whereas 4.8% were managed using ORIF [
10,
22].
The present study provides a comprehensive examination of treatment modalities, specifically focusing on the utilization of cerclage wires and locking compression plates (LCP), which have demonstrated efficacy in particular contexts [
10,
17]. Customized treatment approaches are of utmost importance in the management of Vancouver B3 fractures, as they necessitate a comprehensive strategy that takes into account both mechanical and biological factors. A noteworthy discovery pertains to the efficacy of cortical strut allografts in the treatment of proximal femoral fractures (PFFs). The utilization of allografts serves the dual purpose of enhancing mechanical stability and facilitating the process of fracture healing, thereby diminishing the duration necessary for bone union [
23,
24]. The utilization of these allografts was found to be linked with a relatively low infection rate of 2.0%, underscoring the notion that the complexity of the surgical procedure plays a significant role in determining infection rates [
24]. The investigation also documented a notable survival rate of 95.8% for cortical strut allografts during the ultimate follow-up, consistent with prior research that has reported survival rates ranging from 93% to 100% [
23,
25].
The analysis provided in
Table 1 is a valuable resource within the dynamic domain of orthopedic surgery. It effectively consolidates various studies that investigate the efficacy of diverse arthroplasty and fixation methods for the treatment of hip fractures. Over a period of multiple years and involving a variety of research approaches and cohorts, the table consolidates essential information regarding surgical variables, functional results, and possible adverse events, providing a comprehensive perspective on the present state of investigation in this field. The table elucidates the subtle distinctions among different treatment methodologies, emphasizing factors such as duration of surgery, amount of blood loss, and level of post-operative mobility, which play a crucial role in determining the efficacy of the surgical intervention. Furthermore, this study illuminates the rates of survival and complications, offering a well-rounded viewpoint that can inform subsequent research endeavors and clinical judgments.
This research offers a thorough examination of PFFs, highlighting the intricacies involved in their administration. This emphasizes the necessity of individualized treatment approaches, particlarly for Vancouver B3 fractures, and advocates for additional research to enhance classification systems and investigate the possibilities offered by emerging technologies. The findings of this study make a substantial contribution to the current body of knowledge and carry significant implications for future research and clinical practice.
5. Conclusions
Our research, conducted at Bucharest University Emergency Hospital, explored the management of periprosthetic femoral fractures (PFFs), specifically focusing on the complexities associated with Vancouver B type fractures. The present study brings attention to the increasing prevalence of these fractures, primarily observed among the elderly demographic, and emphasizes the significant influence of patient-specific factors, such as sarcopenia and osteoporosis, in augmenting the vulnerability of older individuals to proximal femoral fractures (PFFs).
Our research underscores the importance of implementing personalized treatment approaches, specifically when managing Vancouver fractures. The results of our study support the implementation of a comprehensive strategy that considers the distinct medical and lifestyle characteristics of individual patients, with the aim of enhancing outcomes and potentially mitigating mortality rates.
Notwithstanding the perceptive discoveries, we acknowledge the constraints inherent in our investigation, which encompass the potential for selection bias due to its retrospective nature and the limited size of the sample. We advocate for additional prospective studies to substantiate these findings and investigate the potential applications of emerging technologies in the management of PFFs. In its entirety, our study represents a substantial addition to the current corpus of knowledge, thereby establishing a foundation for subsequent investigations and potentially bringing about transformative changes in clinical practice within the realm of orthopedics.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, MIHNEA GABRIEL POPA and CURSARU ADRIAN.; methodology, CRETU BOGDAN.; software, GEORGIAN IACOBESCU validation, MIHNEA GABRIEL POPA, CURSARU ADRIAN .; formal analysis, RAZVAN SPIRIDONICA.; investigation, ANGEL RASCU.; resources, SERGIU IORDACHE.; data curation, SERBAN BOGDAN.; writing—original draft preparation, MIHNEA GABRIEL POPA, SERBAN BOGDAN.; writing—review and editing, CURSARU ADRIAN.; supervision, CRETU BOGDAN.; project administration, CĂTĂLIN CÎRSTOIU.;. All authors have read and agreed to the published version of the manuscript.”
Funding
This research received no external funding
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Bucharest Emergency University Hospital (protocol code 586313 and date of approval : 09.09.2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest
References
- Baryeh K, Wang C, Sochart DH. Periprosthetic femoral fractures around the original cemented polished triple-tapered C-stem femoral implant: A consecutive series of 500 primary total hip arthroplasties with an average follow-up of 15 years. Arch Orthop Trauma Surg. 2023 Jul;143(7):4511-4518. Epub 2022 Nov 29. [CrossRef] [PubMed] [PubMed Central]
- Capone A, Congia S, Civinini R, Marongiu G. Periprosthetic fractures: Epidemiology and current treatment. Clin Cases Miner Bone Metab. 2017 May-Aug;14(2):189-196. Epub 2017 Oct 25. [CrossRef] [PubMed] [PubMed Central]
- Chatziagorou G, Lindahl H, Garellick G, Kärrholm J. Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int. 2019 May;29(3):282-288. Epub 2018 Jul 16. [CrossRef] [PubMed]
- Duncan CP, Haddad FS. The Unified Classification System (UCS): Improving our understanding of periprosthetic fractures. Bone Joint J. 2014 Jun;96-B(6):713-6. [CrossRef] [PubMed]
- Mondanelli N, Troiano E, Facchini A, Ghezzi R, Di Meglio M, Nuvoli N, Peri G, Aiuto P, Colasanti GB, Giannotti S. Treatment algorithm of periprosthetic femoral fractures. Geriatr Orthop Surg Rehabil. 2022 May 10;13:21514593221097608. [CrossRef] [PubMed] [PubMed Central]
- Quah C, Porteous M, Stephen A. Principles of managing Vancouver type B periprosthetic fractures around cemented polished tapered femoral stems. Eur J Orthop Surg Traumatol. 2017 May;27(4):477-482. Epub 2016 Nov 26. [CrossRef] [PubMed]
- Heu JY, Kim JY, Lee SW. Periprosthetic fracture around a cemented stem in total hip arthroplasty. Hip Pelvis. 2022 Sep;34(3):140-149. Epub 2022 Sep 30. [CrossRef] [PubMed] [PubMed Central]
- Karam J, Campbell P, Desai S, Hunter M. Periprosthetic proximal femoral fractures in cemented and uncemented stems according to Vancouver classification: Observation of a new fracture pattern. J Orthop Surg Res. 2020 Mar 10;15(1):100. [CrossRef] [PubMed] [PubMed Central]
- Jain S, Lamb J, Townsend O, Scott CEH, Kendrick B, Middleton R, Jones SA, Board T, West R, Pandit H. Risk factors influencing fracture characteristics in postoperative periprosthetic femoral fractures around cemented stems in total hip arthroplasty: A multicentre observational cohort study on 584 fractures. Bone Jt Open. 2021 Jul;2(7):466-475. [CrossRef] [PubMed] [PubMed Central]
- De Maio F, Caterini A, Cesaretti L, Ziranu A, De Luna V, Farsetti P. Vancouver B2 and B3 periprosthetic femoral fractures treated by ORIF: Mid to long-term follow-up study in 28 patients. Eur Rev Med Pharmacol Sci. 2022 Nov;26(1 Suppl):1-8. [CrossRef] [PubMed]
- Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32,644 primary total hip arthroplasties: A 40-year experience. Bone Joint J. 2016 Apr;98-B(4):461-7. Erratum in: Bone Joint J. 2020 Dec;102-B(12):1782. [CrossRef] [PubMed]
- Liu Y, Li C, Cao Z, Wang X, Wen J, Ping H, Kong X, Chai W. Undetected intraoperative periprosthetic femoral fractures in patients undergoing primary total hip arthroplasty: A retrospective case series and literature review. Orthop Surg. 2023 Mar;15(3):758-765. Epub 2023 Jan 17. [CrossRef] [PubMed] [PubMed Central]
- Konow T, Baetz J, Melsheimer O, Grimberg A, Morlock M. Factors influencing periprosthetic femoral fracture risk. Bone Joint J. 2021 Apr;103-B(4):650-658. [CrossRef] [PubMed]
- Lv H, Guo X, Wang YH, Zhang ZJ, Zou LF, Xue H, Huang DH, Tan MY. Open reduction and locked compression plate fixation, with or without allograft strut, for periprosthetic fractures in patients who had a well-fixed femoral stem: A retrospective study with an average 2-year follow-up. BMC Musculoskelet Disord. 2022 Jan 19;23(1):69. [CrossRef] [PubMed] [PubMed Central]
- Shah RP, Sheth NP, Gray C, Alosh H, Garino JP. Periprosthetic fractures around loose femoral components. J Am Acad Orthop Surg. 2014 Aug;22(8):482-90. [CrossRef] [PubMed]
- Capone A, Cavaliere P, Campacci A, Carulli C, Pignatti G, Randelli F, Marelli B, Esopi P, Congia S, Marongiu G. Current practice of Italian Association of Revision Surgery members in the treatment of Unified Classification System type B periprosthetic femoral fracture around hip arthroplasty: A cross-sectional survey. Geriatr Orthop Surg Rehabil. 2022 Mar 24;13:21514593221080341. [CrossRef] [PubMed] [PubMed Central]
- Barghi A, Hanna P, Merchan N, Weaver MJ, Wixted J, Appleton P, Rodriguez E. Outcomes of fixation of Vancouver B periprosthetic fractures around cemented versus uncemented stems. BMC Musculoskelet Disord. 2023 Apr 4;24(1):263. [CrossRef] [PubMed] [PubMed Central]
- Chatziagorou G, Lindahl H, Garellick G, Kärrholm J. Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int. 2019 May;29(3):282-288. Epub 2018 Jul 16. [CrossRef] [PubMed]
- Smitham PJ, Carbone TA, Bolam SM, Kim YS, Callary SA, Costi K, Howie DW, Munro JT, Solomon LB. Vancouver B2 peri-prosthetic fractures in cemented femoral implants can be treated with open reduction and internal fixation alone without revision. J Arthroplasty. 2019 Jul;34(7):1430-1434. Epub 2019 Mar 8. [CrossRef] [PubMed]
- Stoffel K, Blauth M, Joeris A, Blumenthal A, Rometsch E. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: A systematic review. Arch Orthop Trauma Surg. 2020 Oct;140(10):1381-1394. Epub 2020 Feb 21. [CrossRef] [PubMed] [PubMed Central]
- Barghi A, Hanna P, Merchan N, Lechtig A, Haggerty C, Weaver MJ, von Keudell A, Wixted J, Appleton P, Rodriguez E. Outcomes after operative fixation of Vancouver B2 and B3 type periprosthetic fractures. J Orthop Trauma. 2022 May 1;36(5):228-233. [CrossRef] [PubMed]
- Khan T, Grindlay D, Ollivere BJ, Scammell BE, Manktelow AR, Pearson RG. A systematic review of Vancouver B2 and B3 periprosthetic femoral fractures. Bone Joint J. 2017 Apr;99-B(4 Supple B):17-25. [CrossRef] [PubMed]
- Kwon DG, Park JS, Moon KH. Treatment of Vancouver type B periprosthetic femoral fractures using cortical strut allografts. Geriatr Orthop Surg Rehabil. 2022 Sep 6;13:21514593221125618. [CrossRef] [PubMed] [PubMed Central]
- Wu HB, Yan SG, Wu LD, He RX, Wang XH, Dai XS. Combined use of extensively porous coated femoral components with onlay cortical strut allografts in revision of Vancouver B2 and B3 periprosthetic femoral fractures. Chin Med J (Engl). 2009 Nov 5;122(21):2612-5. [PubMed]
- Barden B, Fitzek JG, Huttegger C, Löer F. Supportive strut grafts for diaphyseal bone defects in revision hip arthroplasty. Clin Orthop Relat Res. 2001 Jun;(387):148-55. [CrossRef] [PubMed]
- Solomon LB, Hussenbocus SM, Carbone TA, Callary SA, Howie DW. Is internal fixation alone advantageous in selected B2 periprosthetic fractures? ANZ J Surg. 2015;85:169–173. [CrossRef]
- Baum C, Leimbacher M, Kriechling P, Platz P, Cadosch D. Treatment of periprosthetic femoral fractures type Vancouver B2 - Revision arthroplasty vs. open reduction and internal fixation with Locking Compression Plate: A retrospective single-center study. Br J Surg. 2017;104:20.
- Wall B, Stambough JB, Cherney SM, Mears SC. Use of the Locking Attachment Plate for Internal Fixation of Periprosthetic Femur Fractures. Geriatr Orthop Surg Rehabil. 2022 May 3;13:21514593221100417. [CrossRef] [PubMed] [PubMed Central]
- Lunebourg A, Mouhsine E, Cherix S, Ollivier M, Chevalley F, Wettstein M. Treatment of type B periprosthetic femur fractures with curved non-locking plate with eccentric holes: Retrospective study of 43 patients with minimum 1-year follow-up. Orthop Traumatol Surg Res. 2015;101:277–282. [CrossRef]
- Spina M, Rocca G, Canella A, Scalvi A. Causes of failure in periprosthetic fractures of the hip at 1- to 14-year follow-up. Injury. 2014;45(Suppl 6):S85–S92. [CrossRef]
Figure 1.
One of the instances that exemplify the intricacy of Vancouver B1 periprosthetic femoral fractures involves a 76-year-old individual who had previously received cemented total hip arthroplasty eight years ago. The individual exhibited a positive result following arthroplasty; however, they have recently encountered a periprosthetic Vancouver type B1 fracture as a result of a fall from a standing position. The preoperative radiographic assessment confirmed the B1 categorization of the fracture, as illustrated in Figure A. Based on the patient's age, the stability of the cemented stem, and the characteristics of the fracture, it was determined that surgical intervention was required. An open reduction procedure was conducted to realign the fracture, followed by stabilization using a specialized plate that incorporated distal screws and was reinforced with proximal cerclage wires. The radiographs taken after the surgery, as depicted in Image B, verified that the reduction and fixation were successful. These results are consistent with the current recommended approach for treating fractures in older patients who have stable prostheses that are cemented in place.
Figure 1.
One of the instances that exemplify the intricacy of Vancouver B1 periprosthetic femoral fractures involves a 76-year-old individual who had previously received cemented total hip arthroplasty eight years ago. The individual exhibited a positive result following arthroplasty; however, they have recently encountered a periprosthetic Vancouver type B1 fracture as a result of a fall from a standing position. The preoperative radiographic assessment confirmed the B1 categorization of the fracture, as illustrated in Figure A. Based on the patient's age, the stability of the cemented stem, and the characteristics of the fracture, it was determined that surgical intervention was required. An open reduction procedure was conducted to realign the fracture, followed by stabilization using a specialized plate that incorporated distal screws and was reinforced with proximal cerclage wires. The radiographs taken after the surgery, as depicted in Image B, verified that the reduction and fixation were successful. These results are consistent with the current recommended approach for treating fractures in older patients who have stable prostheses that are cemented in place.
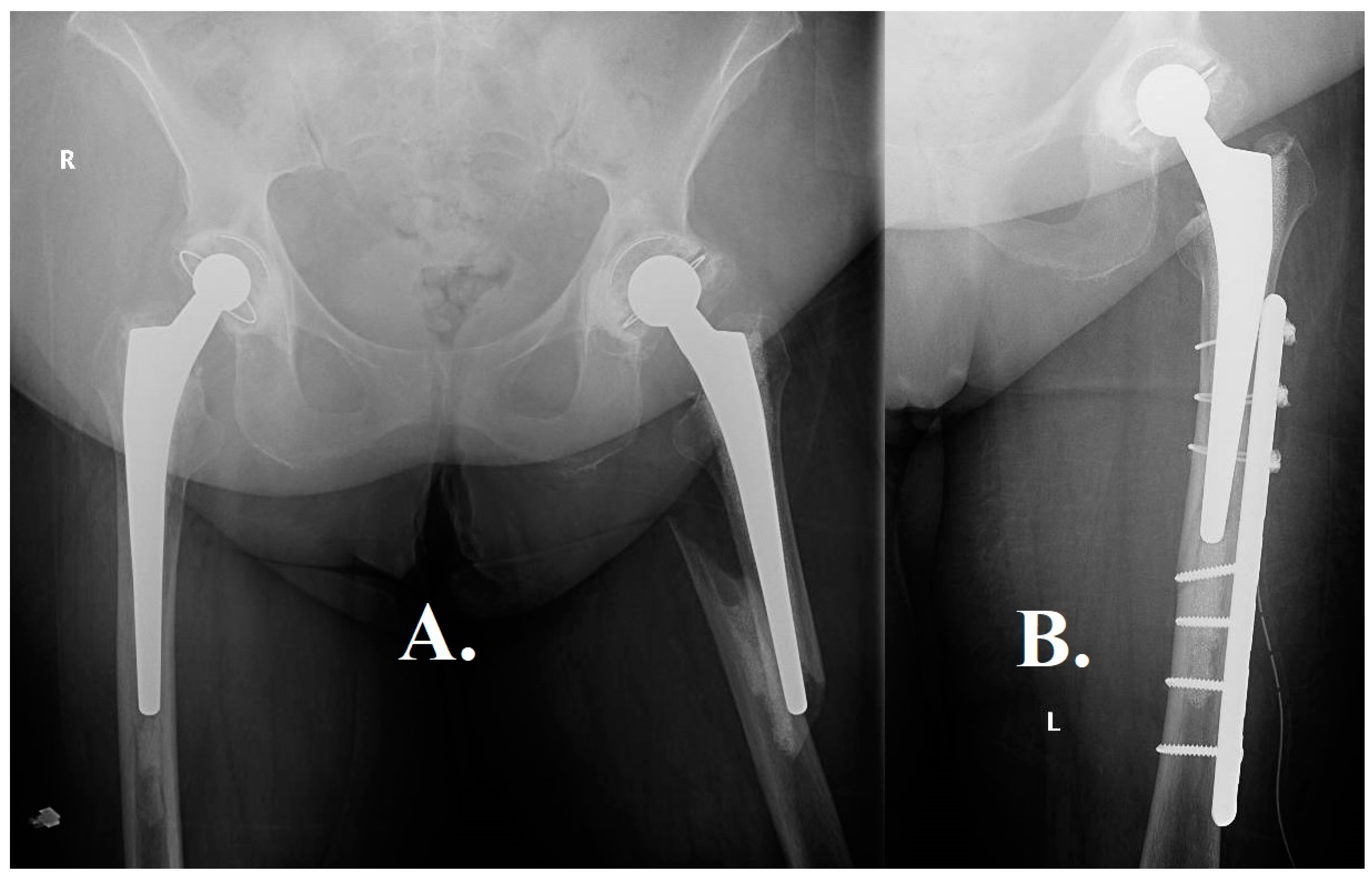
Figure 2.
An additional noteworthy instance pertains to an octogenarian patient, aged 87, who presented with a multitude of concurrent medical conditions, including Alzheimer's disease, which exerted a substantial impact on the chosen therapeutic strategy. The patient experienced a femoral neck fracture at the age of 85. Due to the patient's advanced age and cognitive impairment, the decision was made to opt for a bipolar prosthesis instead of a total hip replacement. This choice was made with the aim of reducing surgical risks and the likelihood of postoperative dislocation. The patient recently encountered another incident of falling from a standing position, leading to a periprosthetic Vancouver type B1 fracture, as indicated in Image A. In light of the patient's diagnosis of Alzheimer's disease and the concomitant difficulties in providing postoperative care, an initial contemplation was made regarding the implementation of a non-surgical intervention. Nevertheless, given the gravity and specific anatomical site of the femoral fracture, surgical intervention was considered inevitable. The procedures of fracture reduction and osteosynthesis were effectively executed, as evidenced by the visual representations in Images B and C. It is noteworthy to mention that approximately ten years prior, the patient had also experienced a fracture in the proximal humerus region. During that period, the family chose to pursue conservative treatment as a result of the patient's mental condition. Nevertheless, in the case of a femoral fracture, non-operative management was deemed impractical, highlighting the crucial nature of such injuries and the imperative for surgical intervention, even in intricate medical scenarios.
Figure 2.
An additional noteworthy instance pertains to an octogenarian patient, aged 87, who presented with a multitude of concurrent medical conditions, including Alzheimer's disease, which exerted a substantial impact on the chosen therapeutic strategy. The patient experienced a femoral neck fracture at the age of 85. Due to the patient's advanced age and cognitive impairment, the decision was made to opt for a bipolar prosthesis instead of a total hip replacement. This choice was made with the aim of reducing surgical risks and the likelihood of postoperative dislocation. The patient recently encountered another incident of falling from a standing position, leading to a periprosthetic Vancouver type B1 fracture, as indicated in Image A. In light of the patient's diagnosis of Alzheimer's disease and the concomitant difficulties in providing postoperative care, an initial contemplation was made regarding the implementation of a non-surgical intervention. Nevertheless, given the gravity and specific anatomical site of the femoral fracture, surgical intervention was considered inevitable. The procedures of fracture reduction and osteosynthesis were effectively executed, as evidenced by the visual representations in Images B and C. It is noteworthy to mention that approximately ten years prior, the patient had also experienced a fracture in the proximal humerus region. During that period, the family chose to pursue conservative treatment as a result of the patient's mental condition. Nevertheless, in the case of a femoral fracture, non-operative management was deemed impractical, highlighting the crucial nature of such injuries and the imperative for surgical intervention, even in intricate medical scenarios.
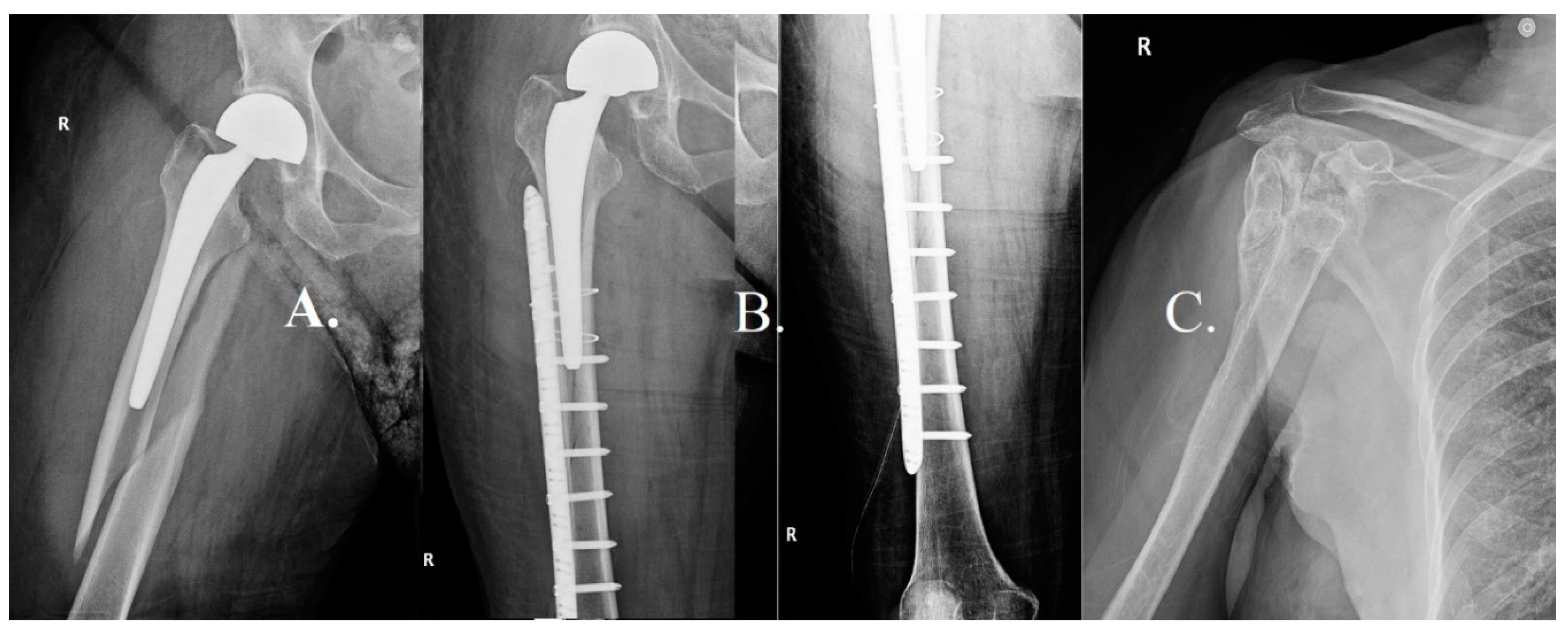
Figure 3.
An illustrative case pertains to a patient of 76 years old who underwent total hip arthroplasty at the age of 65. After a period of seven years following the operation, the radiographic examination revealed slight deteriorations without any notable clinical symptoms, as illustrated in Image A. Nevertheless, a span of 11 years subsequent to the primary arthroplasty, the patient exhibited significant discomfort in the hip region along with notable restrictions in functional abilities. The radiographic assessment conducted at this particular stage, as depicted in Image B, exhibited significant deterioration observed at both the femoral and acetabular levels. Additional imaging modalities, such as computed tomography scans illustrated in Figures C, D, F, and G, corroborated the presence of notable femoral lysis and considerable loss of acetabular substance. Due to the significant deterioration of the prosthetic device, it was determined that revision hip arthroplasty should be pursued. The patient experienced a Vancouver type B1 periprosthetic femoral fracture during the surgical procedure. In order to tackle this issue, a pair of cerclage wires were employed to provide stability to the extended revision stem, as depicted in Figure H. After one year following the revision procedure, the patient exhibited positive results, as indicated by radiographic evidence demonstrating successful healing of the fracture and integration of the prosthesis, as depicted in Image I. The present case serves as a prime illustration of the difficulties and intricacies associated with the management of Vancouver B1 fractures within the framework of revision hip arthroplasty. This highlights the significance of diligent and extended postoperative monitoring for individuals with hip prostheses, particularly in light of the possibility of substantial prosthetic deterioration that may require intricate surgical interventions.
Figure 3.
An illustrative case pertains to a patient of 76 years old who underwent total hip arthroplasty at the age of 65. After a period of seven years following the operation, the radiographic examination revealed slight deteriorations without any notable clinical symptoms, as illustrated in Image A. Nevertheless, a span of 11 years subsequent to the primary arthroplasty, the patient exhibited significant discomfort in the hip region along with notable restrictions in functional abilities. The radiographic assessment conducted at this particular stage, as depicted in Image B, exhibited significant deterioration observed at both the femoral and acetabular levels. Additional imaging modalities, such as computed tomography scans illustrated in Figures C, D, F, and G, corroborated the presence of notable femoral lysis and considerable loss of acetabular substance. Due to the significant deterioration of the prosthetic device, it was determined that revision hip arthroplasty should be pursued. The patient experienced a Vancouver type B1 periprosthetic femoral fracture during the surgical procedure. In order to tackle this issue, a pair of cerclage wires were employed to provide stability to the extended revision stem, as depicted in Figure H. After one year following the revision procedure, the patient exhibited positive results, as indicated by radiographic evidence demonstrating successful healing of the fracture and integration of the prosthesis, as depicted in Image I. The present case serves as a prime illustration of the difficulties and intricacies associated with the management of Vancouver B1 fractures within the framework of revision hip arthroplasty. This highlights the significance of diligent and extended postoperative monitoring for individuals with hip prostheses, particularly in light of the possibility of substantial prosthetic deterioration that may require intricate surgical interventions.
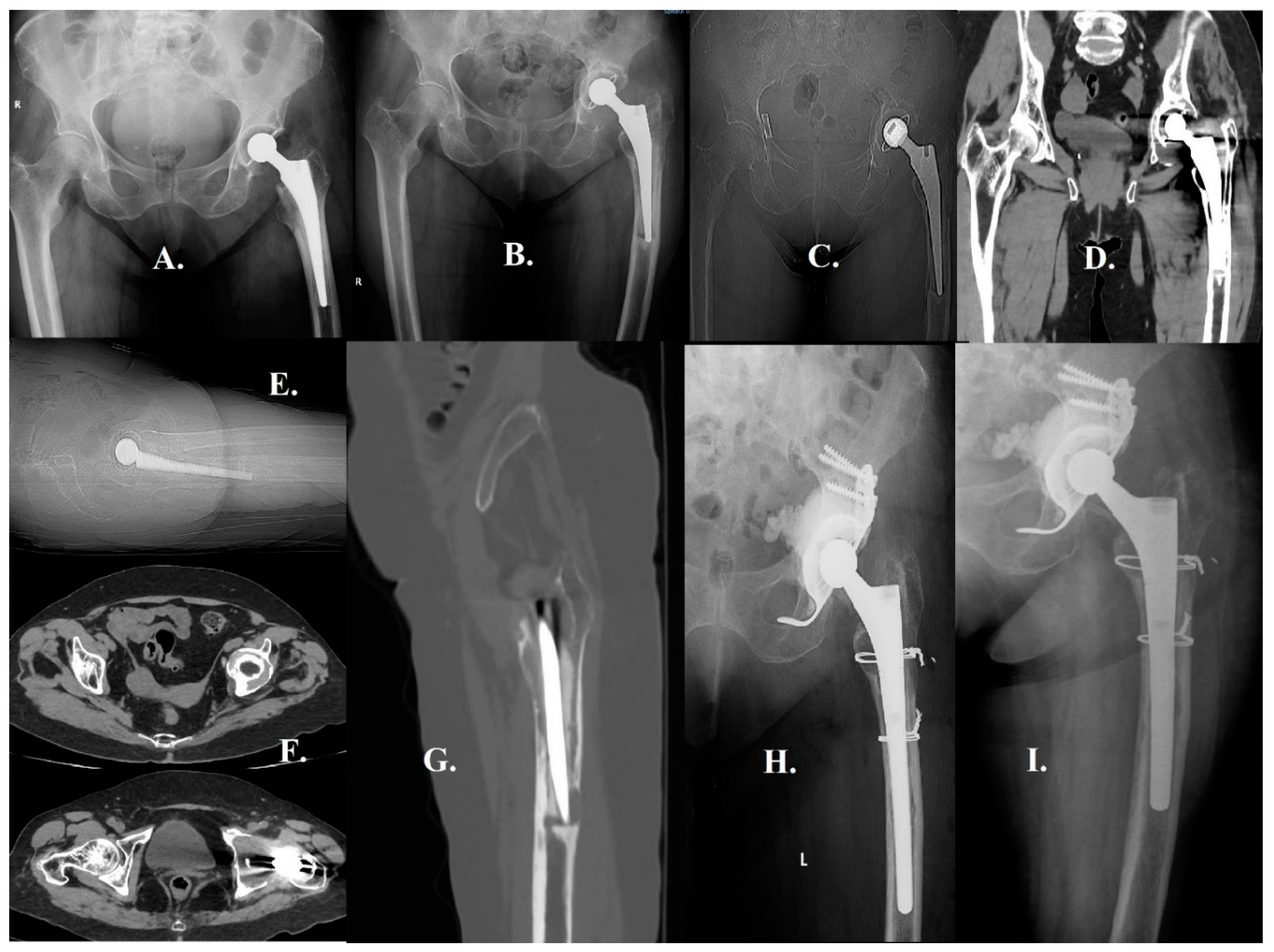
Figure 4.
The fracture in question is categorized as Vancouver B2 owing to the radiological instability observed in the prosthesis stem as we see in image A. Nevertheless, the bone quality of the patient was remarkably high, enabling a precise anatomical realignment of the fracture during the surgical procedure. Considering the effective decrease in symptoms and the presence of concurrent medical conditions in the patient, it was determined that a more conservative surgical approach would be suitable. As depicted in Figure B, the conventional approach for managing these fractures frequently entails the utilization of plate and screw fixation. Nevertheless, in this particular instance, osteosynthesis was accomplished through the utilization of four cerclage wires, deviating from the customary treatment protocol. The patient's postoperative course was without any notable incidents, which serves to underscore the significance of tailoring treatment plans to address intricate Vancouver B2 fractures.
Figure 4.
The fracture in question is categorized as Vancouver B2 owing to the radiological instability observed in the prosthesis stem as we see in image A. Nevertheless, the bone quality of the patient was remarkably high, enabling a precise anatomical realignment of the fracture during the surgical procedure. Considering the effective decrease in symptoms and the presence of concurrent medical conditions in the patient, it was determined that a more conservative surgical approach would be suitable. As depicted in Figure B, the conventional approach for managing these fractures frequently entails the utilization of plate and screw fixation. Nevertheless, in this particular instance, osteosynthesis was accomplished through the utilization of four cerclage wires, deviating from the customary treatment protocol. The patient's postoperative course was without any notable incidents, which serves to underscore the significance of tailoring treatment plans to address intricate Vancouver B2 fractures.
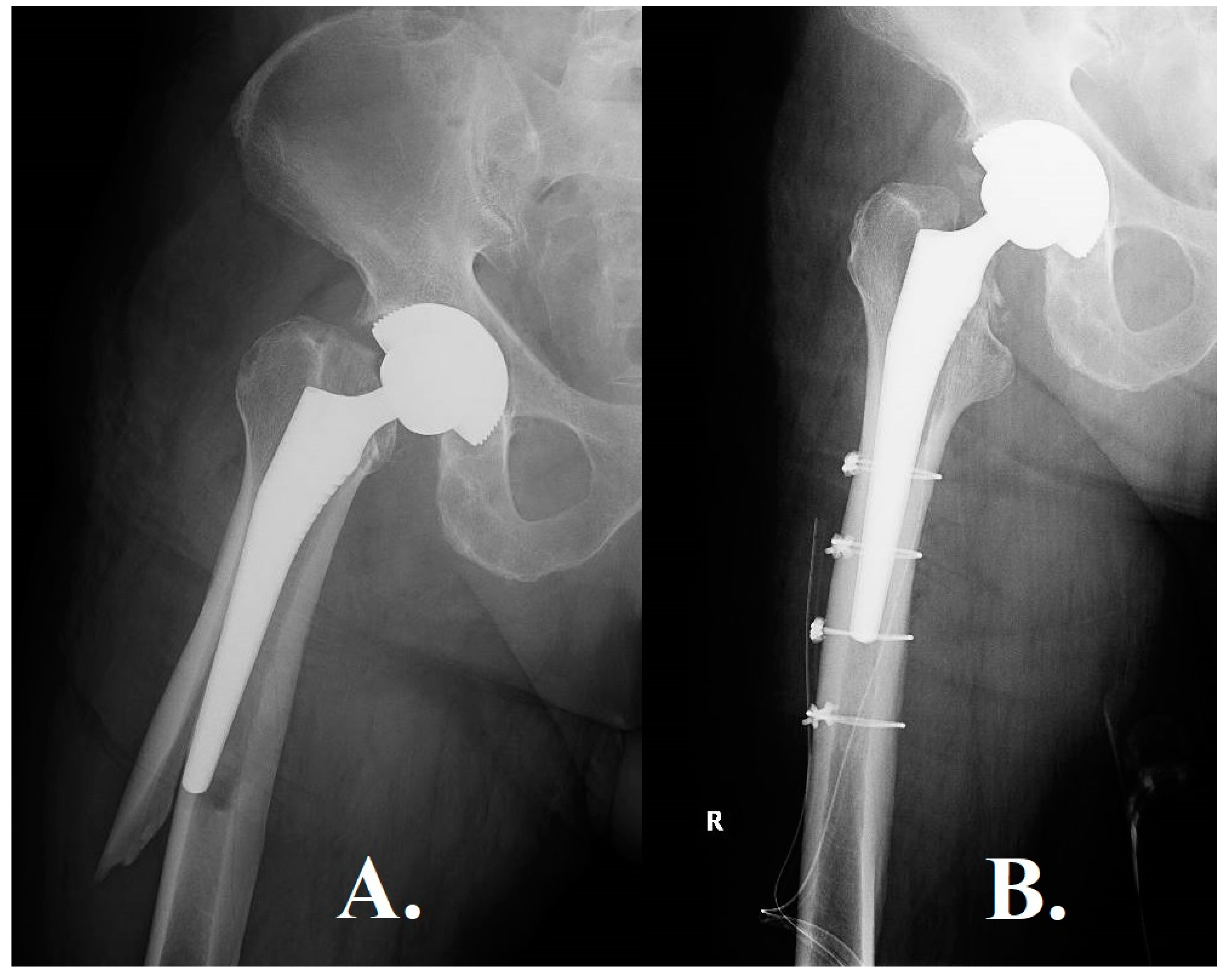
Figure 5.
Image A depicts the spiroid fracture as described in the accompanying text, while Image B illustrates the radiological assessment following open reduction and internal fixation (ORIF) using a proximal hook plate, cerclages, and self-locking screws.
Figure 5.
Image A depicts the spiroid fracture as described in the accompanying text, while Image B illustrates the radiological assessment following open reduction and internal fixation (ORIF) using a proximal hook plate, cerclages, and self-locking screws.
Figure 6.
Image A depicts a spiroid fracture located at the femur level, accompanied by an unstable femoral stem. Image B depicts the anatomical realignment of the periprosthetic fracture using proximal and distal screws in conjunction with plates to enhance its stability. Additionally, a relatively large number of cerclages have been employed at the plate level to maintain the fracture's position. While this approach does indeed enhance resistance, it also elevates the risk of compromising the vascularization of the bone at this particular site.
Figure 6.
Image A depicts a spiroid fracture located at the femur level, accompanied by an unstable femoral stem. Image B depicts the anatomical realignment of the periprosthetic fracture using proximal and distal screws in conjunction with plates to enhance its stability. Additionally, a relatively large number of cerclages have been employed at the plate level to maintain the fracture's position. While this approach does indeed enhance resistance, it also elevates the risk of compromising the vascularization of the bone at this particular site.
Figure 7.
The radiological observations in Image A pose a particularly complex situation. The visual representation depicts a spiroid fracture that originates from the trochanteric massif and extends approximately 5 centimeters below the distal end of the femoral stem. In this instance of a comminuted fracture, a butterfly fragment become detached, covering a span of approximately 2 thirds along the entire length of the fracture. The detachment of the fracture greatly intensifies its instability, presenting a challenging surgical predicament. On the other hand, Image B depicts a surgical intervention that has achieved a favorable outcome. The fracture was anatomically reduced and stabilized using Open Reduction and Internal Fixation (ORIF) technique, which involved the application of a self-locking plate supplemented with cables. The selection of this approach was likely made with the intention of optimizing the likelihood of achieving fracture union, while simultaneously minimizing the potential for exacerbating the already delicate nature of the fracture.
Figure 7.
The radiological observations in Image A pose a particularly complex situation. The visual representation depicts a spiroid fracture that originates from the trochanteric massif and extends approximately 5 centimeters below the distal end of the femoral stem. In this instance of a comminuted fracture, a butterfly fragment become detached, covering a span of approximately 2 thirds along the entire length of the fracture. The detachment of the fracture greatly intensifies its instability, presenting a challenging surgical predicament. On the other hand, Image B depicts a surgical intervention that has achieved a favorable outcome. The fracture was anatomically reduced and stabilized using Open Reduction and Internal Fixation (ORIF) technique, which involved the application of a self-locking plate supplemented with cables. The selection of this approach was likely made with the intention of optimizing the likelihood of achieving fracture union, while simultaneously minimizing the potential for exacerbating the already delicate nature of the fracture.
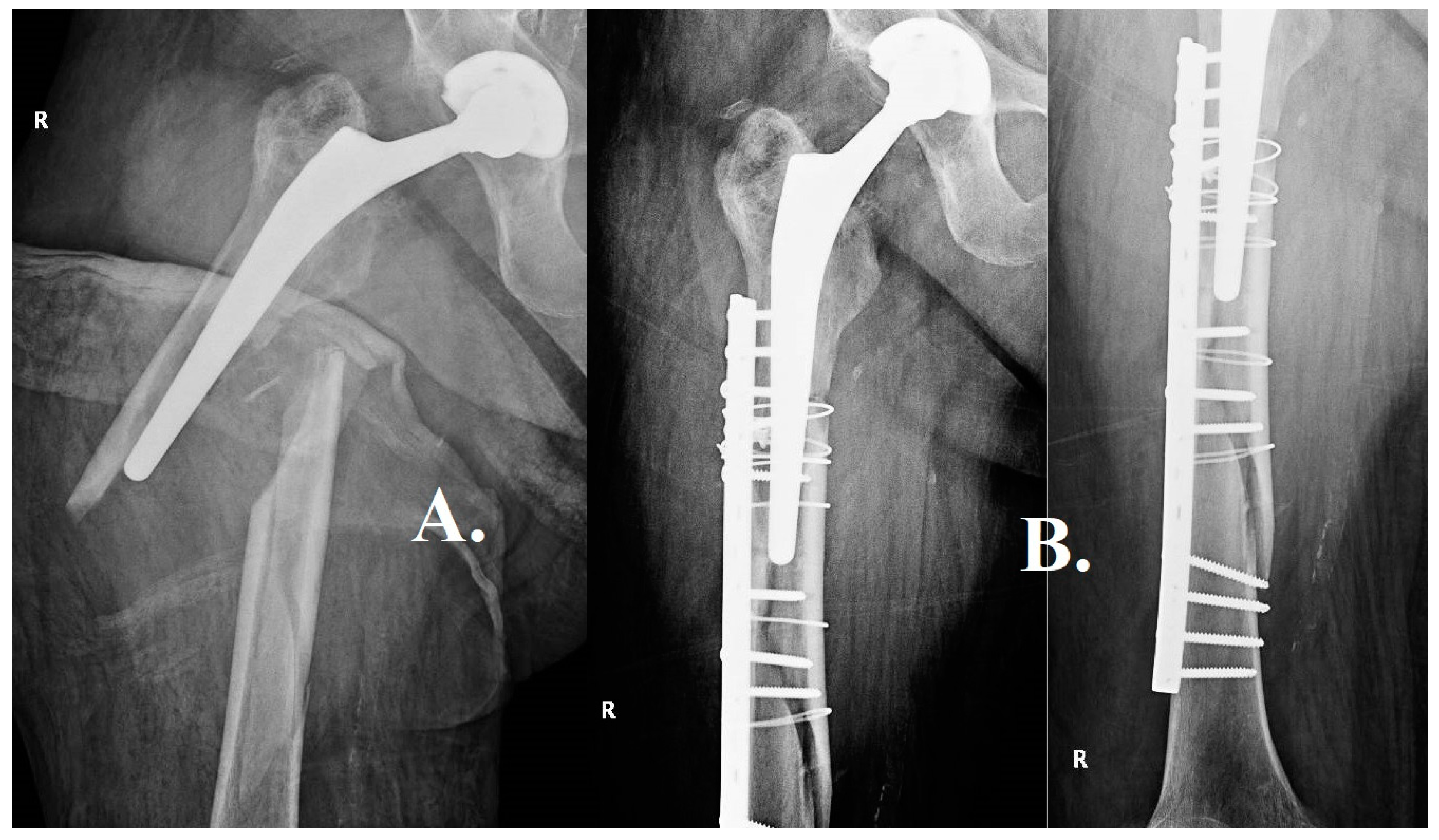
Figure 8.
Image A poses a significant clinical dilemma. The radiographic image demonstrates a comminuted fracture that affects the trochanteric massif and the proximal third of the femur. It is worth noting that there is a considerable degree of telescoping and shortening observed in the femur, which serves as an indication of pronounced instability and displacement. Due to the intricate nature of the fracture and its inherent instability, it is probable that a simple internal fixation would not provide adequate long-term stability and promote fracture union. Within this particular context, the surgical team made the decision to pursue a more assertive course of action, as illustrated in Image B. A modification was made to the femoral component by utilizing a longer revision stem in order to improve stability and promote the growth of bone tissue. In order to enhance the stability of the fracture in its anatomical alignment, two cerclages were employed. The utilization of a combined strategy involving the modification of the femoral component and the implementation of cerclages is intended to effectively tackle both the immediate mechanical instability and the enduring biological prerequisites for fracture healing.
Figure 8.
Image A poses a significant clinical dilemma. The radiographic image demonstrates a comminuted fracture that affects the trochanteric massif and the proximal third of the femur. It is worth noting that there is a considerable degree of telescoping and shortening observed in the femur, which serves as an indication of pronounced instability and displacement. Due to the intricate nature of the fracture and its inherent instability, it is probable that a simple internal fixation would not provide adequate long-term stability and promote fracture union. Within this particular context, the surgical team made the decision to pursue a more assertive course of action, as illustrated in Image B. A modification was made to the femoral component by utilizing a longer revision stem in order to improve stability and promote the growth of bone tissue. In order to enhance the stability of the fracture in its anatomical alignment, two cerclages were employed. The utilization of a combined strategy involving the modification of the femoral component and the implementation of cerclages is intended to effectively tackle both the immediate mechanical instability and the enduring biological prerequisites for fracture healing.
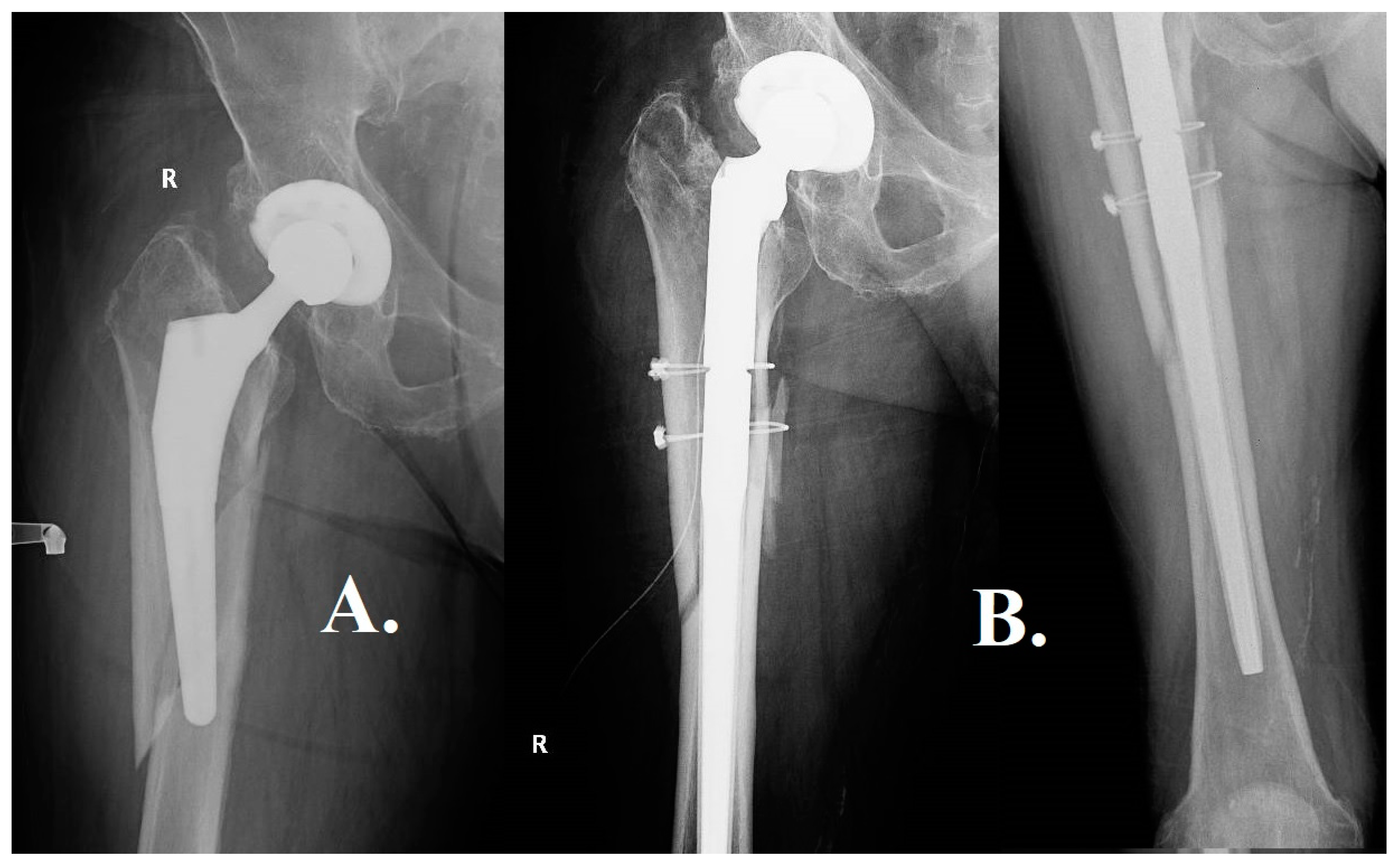
Figure 9.
Image A presents a distinctive and demanding clinical situation wherein a spiroid fracture is observed that extends to the apex of the femoral stem. Interestingly, the primary cause of instability in this particular scenario is not solely attributed to the fracture, but rather to the considerable peri-implant lysis that compromised the stability of the pre-existing femoral stem during the occurrence of the trauma. The occurrence of lysis, which refers to the pathological degradation of bone tissue surrounding the implant, further intensified the mechanical instability following the traumatic event. Due to the compromised quality of the tissue and the destabilizing effects caused by the lysis process, it was not feasible to preserve the original stem. As illustrated in Figure B, the surgical team made the decision to perform a revision arthroplasty utilizing a thicker, uncemented modular stem. The utilization of this method facilitated a comprehensive removal of fibrous tissue from the femoral canal until reaching a state of high-quality bone, thereby establishing a more robust base for the subsequent implantation. In order to augment stability and promote the process of fracture healing, two cerclages were administered at the site of the fracture. Every instance mentioned emphasizes the necessity of an individualized strategy for the management of Vancouver B3 fractures in Vancouver. This approach should consider the distinct difficulties and requirements posed by the medical and lifestyle factors of each patient.
Figure 9.
Image A presents a distinctive and demanding clinical situation wherein a spiroid fracture is observed that extends to the apex of the femoral stem. Interestingly, the primary cause of instability in this particular scenario is not solely attributed to the fracture, but rather to the considerable peri-implant lysis that compromised the stability of the pre-existing femoral stem during the occurrence of the trauma. The occurrence of lysis, which refers to the pathological degradation of bone tissue surrounding the implant, further intensified the mechanical instability following the traumatic event. Due to the compromised quality of the tissue and the destabilizing effects caused by the lysis process, it was not feasible to preserve the original stem. As illustrated in Figure B, the surgical team made the decision to perform a revision arthroplasty utilizing a thicker, uncemented modular stem. The utilization of this method facilitated a comprehensive removal of fibrous tissue from the femoral canal until reaching a state of high-quality bone, thereby establishing a more robust base for the subsequent implantation. In order to augment stability and promote the process of fracture healing, two cerclages were administered at the site of the fracture. Every instance mentioned emphasizes the necessity of an individualized strategy for the management of Vancouver B3 fractures in Vancouver. This approach should consider the distinct difficulties and requirements posed by the medical and lifestyle factors of each patient.
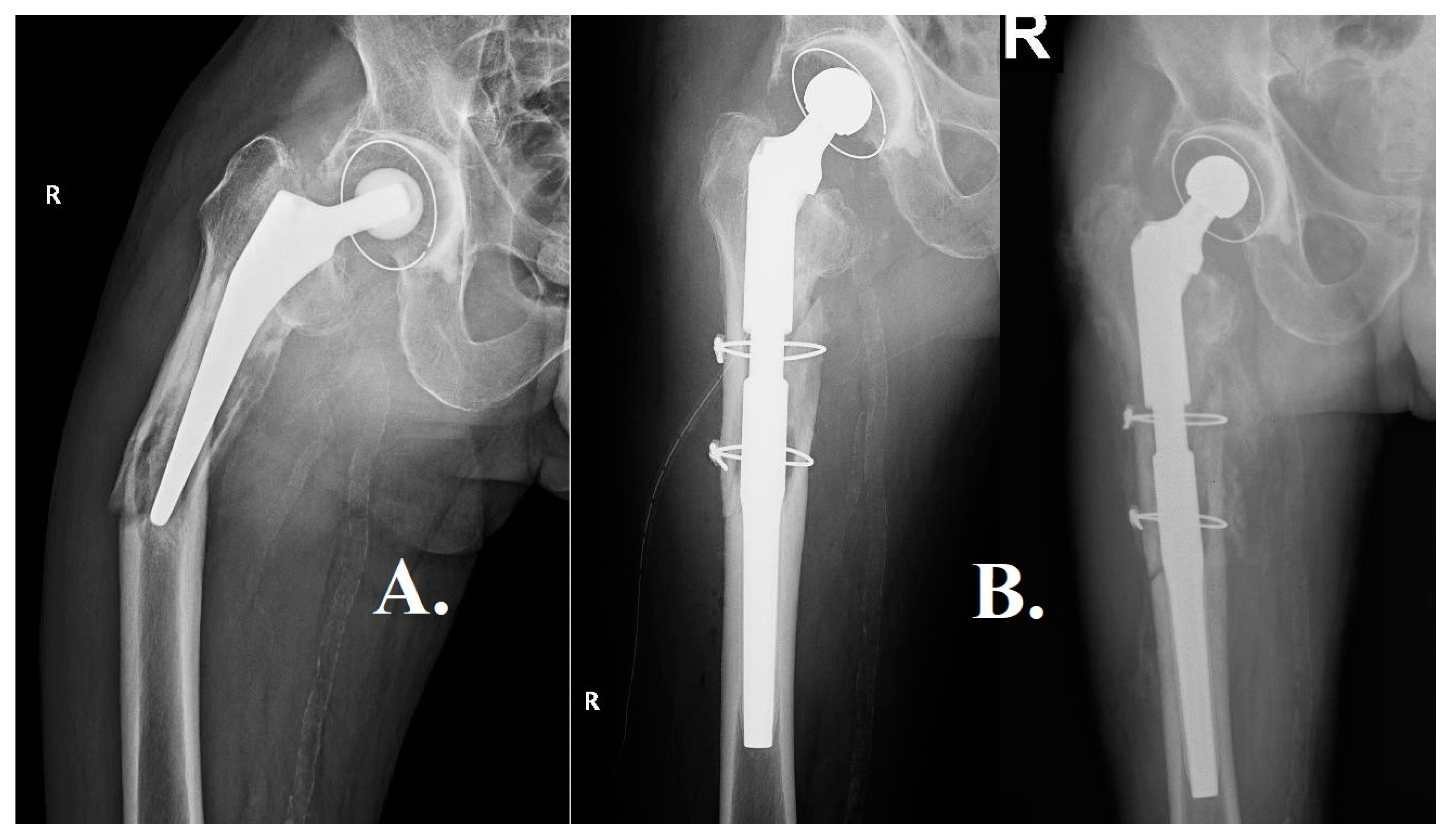
Table 1.
The research conducted possesses certain limitations. The retrospective nature of its design and the small size of its sample may potentially introduce selection bias. Subsequent investigations should strive to conduct comprehensive and forward-looking studies in order to corroborate the aforementioned findings. Moreover, the influence of nascent technologies such as 3D printing on PFF (proximal femoral fractures) management has yet to be thoroughly examined, thus necessitating additional research.
Table 1.
The research conducted possesses certain limitations. The retrospective nature of its design and the small size of its sample may potentially introduce selection bias. Subsequent investigations should strive to conduct comprehensive and forward-looking studies in order to corroborate the aforementioned findings. Moreover, the influence of nascent technologies such as 3D printing on PFF (proximal femoral fractures) management has yet to be thoroughly examined, thus necessitating additional research.
| Pub. Year |
2022 |
2022 |
2015 |
2017 |
2022 |
2015 |
2014 |
| Authors |
Lv et al.(14) |
Maio et al.(10) |
Solomn et al.(26) |
Baum et al. (27) |
Wall et al.(28) |
Lunebourg et al.(29) |
Spina et al.(30) |
| Initial Medical Diagnosis |
B1: 15, B2: 66, B3: 106 |
B2+B3:28 |
B2: 21 |
B2: 57 |
B1: 12, B2: 2, C: 11, other:3 |
B1: 18, B2: 23, B3: 2 |
B1: 30, B2: 7, B3: 11 |
| Type of Arthroplasty |
All THA |
Total hip arthroplasty, hemiarthroplasty, or revision arthroplasty. |
ORIF: 12, Stem Revision: 9 |
THA: 53, HHA: 4 |
All THA |
Primary THA or HA |
Not specified |
| Type of Fixation |
Group A-ORIF(B1:15,C:2)/Group B- ORIF+cortical strut allografting(B1:15,C:1) |
ORIF using screws and cerclage;bone grafting |
N/A |
N/A |
LCP-LAP construct |
N/A |
N/A |
| Hospital and Surgery Outcomes |
Mean time to fracture healing: Group A - 5.3 months, Group B - 5.1 months. |
Clinical and radiographic results were good; patients returned to ambulation. |
ORIF mean 390 g, Stem Revision mean: 1502.5 g |
ORIF: 21, Revision: 36 |
Averae age at surgery: 73.3y; BMI:28.4Gender: 20f, 8m
Average: follow-up: 9.8 months |
ORIF: 35, Revision and ORIF: 8 |
ORIF: 54, Revision: 7 |
| Union Rate and Radiological Results |
Overall union rate: 96.9%. Group A had one nonunion and one malunion case. |
Post-ORIF B2 fractures scored higher than B3 fractures. |
Bony union in all patients |
ORIF non-union: 1, Revision non-union: 8 |
Non-union cases: 3 (10.7%)
Non-union plate breakage: 2 |
Union achieved in all patients |
ORIF B2 straight stem: 4, anatomic stem: 1 |
| Functional, Mobility, and Disability Outcomes |
N/A |
N/A |
ORIF 1 pt: Before fx 5, latest fu 5 |
N/A |
N/A |
ORIF: varied, Revision: varied |
ORIF: varied, Revision: varied |
| Complications and Reoperations |
Group A had one nonunion and one malunion case. |
satisfactory ORIF results without stem revision |
ORIF: No infection |
ORIF: 6, Revision: 9 |
Overall complications: 17.9%
Three non-unions, one deep infection, and one revision femoral stem loosening required reoperations. |
ORIF: 0, Revision: 3 |
ORIF: 4, Revision: 3 |
| Survival Rates |
N/A |
N/A |
96.7% (1-year) |
N/A |
N/A |
N/A |
96.7% (1-year), 88.5% (2-year) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).