1. Introduction
Abdominal wall hernia is the most frequently encountered surgical condition that affects all age groups regardless of sex. Globally, the prevalence of abdominal wall hernia was 1.7% for all ages. Abdominal wall hernias are accounting for 15%–18% of all surgical procedures, and annually more than 20 million hernias are operated worldwide (1).
The hernia can also be characterized as a rupture in smooth tissue through which an organ protrudes or pushes through. It is mainly common in the abdomen, groin regions, navel area and upper thigh. Common types include inguinal, hiatal and umbilical hernias. The most frequent hernia is the inguinal hernia (73% of cases) (2-5).
Hernia is a common surgical condition whose frequency is estimated at five percent of the total male population (6-7).
Knowledge of the prevalence, pattern and management of hernia disease locally will highlight local surgical needs and inform health resource allocation (8).
For such circumstances, hernias should be studied more to have the most advanced knowledge about it. We performed a cross-sectional study about the prevalence and associated risk factors of hernias.
2. Materials and Methods
We conducted a descriptive cross-sectional study among patients who admitted to the department of surgery in a tertiary care center. Data were collected from 1 August 2023 to 20 September 2023. Inclusion criteria were patients who are 18 years old and older and visiting the department of surgery. Exclusion criteria were those who were pregnant women and children.
Patients with missed details were excluded for the study. Age, sex, types of hernia, and comorbidities were studied. Full clinical examination was performed for all the patients. All data were saved on excel sheet for statistics. Data were processed on SPSS Statistics version 23.
Analysis was done using descriptive statistics.
3. Results
patients was 37.28 ± 11.55 years (19-77) years.
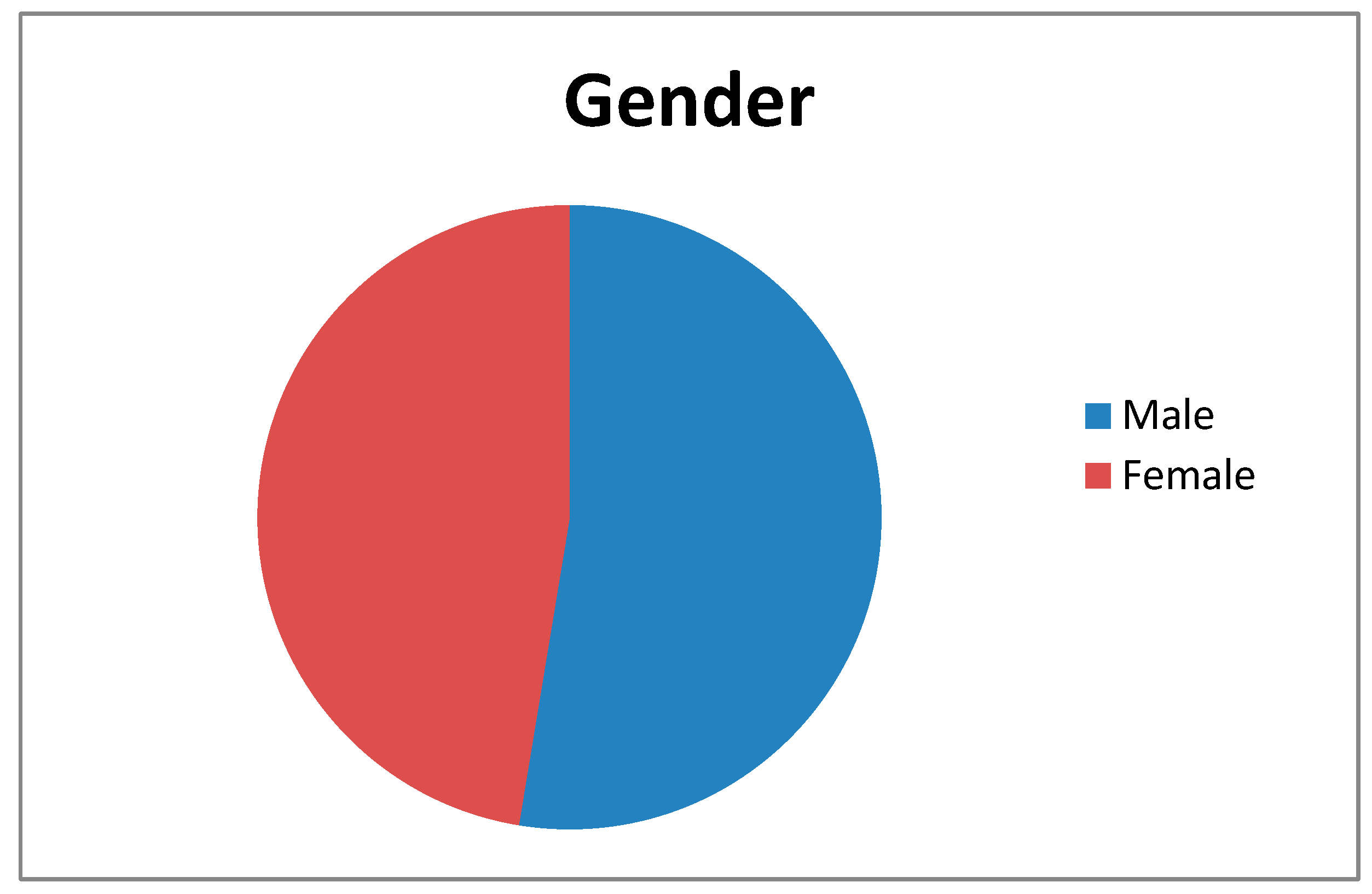
We found 143(52.6 %) patients were males and the rest 129 (47.4 %) patients were female (
Figure A1).
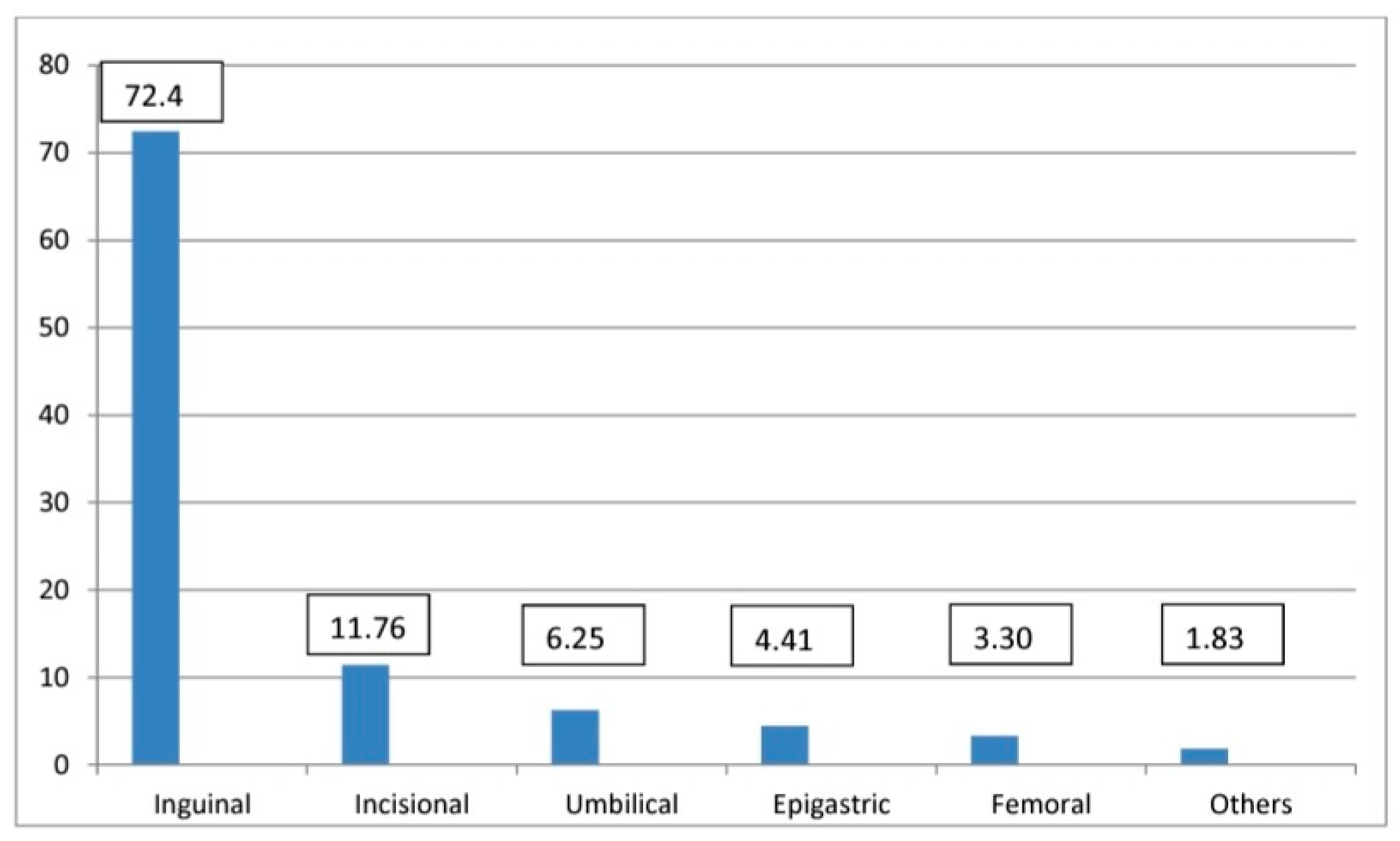
In our study, inguinal hernias were 72.4 %, incisional hernias were 11.76 %, umbilical hernias were 6.25 %, Epigastric hernias were 4.41 %, and femoral hernias were 3.30 % (
Figure A2).
We found 18 patients were 20 years age or less, 31 patients were between 21-30 years, 85 patients were between 31-45 years, 97 patients were between 46-60 years, and only 41 patients were more than 60 years old (Table A1). The male: female ratio of overall hernia patients was 2.8:1 and that for the inguinal hernia was 3.10:1, the incisional hernia was 2.2:1, the umbilical hernia was 2.4:1, the epigastric hernia was 2:1 and the femoral hernia was 3.5:1.
In our study, we had 29 (10.7 %) patients out of 272 who had comorbidity. Diabetes mellitus was found in 16 patients (5.8 %), hypertension was found in 7 patients (2.5 %), chronic obstructive pulmonary disease was found in 4 patients (1.4 %), and hydrocele was found in 3 patients (1.1 %) (
Table A2)
4. Discussion
Our study aimed to assess the prevalence of hernias among patients who admitted to a general surgery department. This study showed the prevalence of hernia was 27.9 %. Deo et al and Kibret AA, et al found the prevalence of hernias was 23.14%, 11.7% respectively (1, 9).
A retrospective analysis of the National Center for Health Statistics in the US showed a 15.6% baseline prevalence of abdominal inpatient emergent hernia repaired from
2001 to 2010 over 10 years (10).
In our study, we found the male-to-female ratio of inguinal hernia, incisional hernia, and umbilical hernia showed male preponderance whereas femoral hernia was found to be more in the female.
These findings resemble a study by Deo et al. (9) which they found male predominance of male gender except for femoral hernia (female predominance). In contrast, female preponderance was found in study by
This cross section study revealed that most cases were inguinal hernias (72.4 %), followed by incisional hernias (11.76 %), 6.25 % for umbilical hernias, 4.41 % epigastric hernias, and 3.30 % for femoral hernias.
Another study was done by Abdulmajeed Ahmed Alenazi et al. found that the most common site of abdominal hernias was para-umbilical, as they were found in 33.9% of cases followed by inguinal 27.3% then umbilical in 20.8% (11).
The distribution of hernias was found to be higher in age between 46- 60 years (97 cases). The less proportion of hernias was found in younger patients (less than 20 years).
These findings were declared in a study Kibret AA, et al (1).
Many studies showed the same finding regarding the correlation between hernias and advanced age (12-14)
The reason could be attributed to the degenerative weakness of abdominal muscles and fibrous tissue in the elderly age group. Loss of abdominal muscle strength and resistance to high intra-abdominal pressure can lead to herniation (15).
Many studies showed comorbidities accompanied with hernias.
Comorbidities associated with inguinal hernia are male gender, low body mass index, Ehlers-Danlos syndrome, prostatomegaly, smoking, COPD, etc (16-17).
In this study, we found diabetes mellitus was the most common in our patients (10.7 %), followed by hypertension (2.5 %), COPD was found in 4 patients (1.4 %), and hydrocele was found in 3 patients (1.1 %).
5. Conclusions
We conclude that the prevalence of hernias in our study was among the range of most previous studies. More studies and efforts are needed to make guidelines regarding early diagnosis of hernias and well management.
Author Contributions
Conceptualization, Mahmoud M.Abokhsab.; Maher Al-Hajjaj; software, Husam Matalqah.; validation, Lina E.Matalkeh. formal analysis Razan Yaseen; investigation, Mohammad Matalkeh.; resources, Husni Alswalha7; data curation, Maher Al-Hajjaj.; writing—original draft preparation, Maher Al-Hajjaj.; writing—review and editing, Mahmoud M.Abokhsab, Lina E.Matalkeh.; visualization, Basil Al Taani.; supervision, Maher Al-hajjaj.; project administration, Mahmoud M.Abokhsab; funding acquisition, None. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Data are available and it could be reached through the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kibret AA, Tekle SY, H/ Mariam MM, et al. Prevalence and associated factors of external hernia among adult patients visiting the surgical outpatient department at the University of Gondar Comprehensive Specialised Hospital, Northwest Ethiopia: a cross-sectional study. BMJ Open 2022, 12, 056488. [CrossRef]
- Rains AJH, Capper WM. Bailey & Love’s Short Practice of Surgery. 15th ed. London: Lewis; 1971.
- Kingnorth A, LeBlanc KA. Management of abdominal hernias. 3rd Edition. London: Edward Arnold, 2003.
- Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet 2003, 362, 1561–1571. [CrossRef] [PubMed]
- Townsend C, Beauchamp D, Evers M, Mattox KL, Sabiston DC. In Sabiston Textbook of Surgery: The biological basis of modern surgical practice; WB Saunders: Philadelphia, PA, USA, 2001.
- Zendejas B, Ramirez T, Jones T, et al. Incidence of inguinal hernia repairs in Olmsted County, Minnesota: A population-based study. Ann Surg 2013, 257, 520–526. [CrossRef] [PubMed]
- Odula PO, Kakande IM. Groin hernia in Mulago hospital, Kampala. East Cent Afr J Surg 2004, 9, 48–52.
- Odula PO, Kakande IM. Groin hernia in Mulago hospital, Kampala. East Cent Afr J Surg 2004, 9, 48–52.
- Waweru, J. , Barasa, M., Mwenda, A., & Mwago, J.K. (2014). Hernia Surgery in Nyeri Provincial General Hospital, Kenya: Our 6 Year Experience. The Annals of African Surgery, 11.
- Deo KK, Shrestha R, Gc S, Maharjan S, Shrestha A, Neupane A. Hernia among Patients Admitted to the Department of Surgery of a Tertiary Care Centre: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2023, 61, 200–203. [CrossRef] [PubMed]
- Beadles CA, Meagher AD, Charles AG. Trends in emergent hernia repair in the United States. JAMA Surg 2015, 150, 194–200. [CrossRef]
- AhmedAlenazi A, Alsharif MM, Hussain MA, Alenezi NG, Alenazi AA, Almadani SA, et al. Prevalence, risk factors and character of abdominal hernia in Arar City, Northern Saudi Arabia in 2017. Electron Physician. Electron Physician 2017, 9, 4806–4811. [CrossRef]
- Sazhin A, Zolotukhin I, Seliverstov E, et al. Prevalence and risk factors for abdominal wall hernia in the general Russian population. Hernia 2019, 23, 1237–1242. [CrossRef]
- Iqbal MN, Akhter S, Irfan M. Prevalence of hernia in relation to various risk factors in Narowal, Pakistan. Sci Lett 2015, 3, 29–32.
- van der Rest M, Garrone R. Collagen family of proteins. Faseb J 1991, 5, 2814–2823. [CrossRef]
- Lauscher JC, Loh JC, Rieck S, et al. Long-term follow-up After Bincisional hernia repair: are there only benefits for symptomatic patients? Hernia 2013;17:203–9.van der Rest M, Garrone R. Collagen family of proteins. Faseb J 1991, 5, 2814–2823. [Google Scholar]
- Abebe MS, Tareke AA, Alem A, Debebe W, Beyene A. Worldwide magnitude of inguinal hernia: Systematic review and meta-analysis of population-based studies. SAGE Open Med 2022, 10, 20503121221139150.
- Jensen KK, Henriksen NA, Jorgensen LN. Inguinal hernia epidemiology. In: Hope WW, Cobb WS, Adrales GL, editors. Textbook of Hernia. Cham: Springer International Publishing; 2017. p. 23–7. Available online: https://doi. org/10.1007/978-3-319-43045-4_4.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).