1. Introduction
Temporomandibular disorders (TMD) are a heterogeneous group of pathologies affecting either the temporomandibular joint (TMJ), masticatory muscles, or associated structures.[
1] The prevalence of TMD is approximately 31% for adults/elderly [
2] and in children and adolescence varies between 20% and 60%.[
3] TMJ clicking sounds, pain, limitation of mandibular movements, and headache are the most common signs and symptoms of TMD.[
4,
5,
6] In children and adolescents, signs and symptoms of TMD seem to increase with age with a higher incidence in middle age. [
2,
3,
7,
8,
9]
The TMD have been classified into two majors categories, pain-related disorders (e.g., myalgia, headache attributed to TMD, and arthralgia) and disorders associated with the TMJ (primarily disc displacements and degenerative diseases). [
1]
Disc displacement (DD) is one of the disorders associated with the TMJ that can occur also in the children and adolescent population with click sound as the most frequent sign [
6,
7,
10]
DD is a frequent finding among adults, children, and adolescents who search for an orthodontic clinical examination [
11]
with a higher incidence of symptomatic TMJ DD in late teenager years. [
12]
Several studies have investigated the etiopathogenesis of DD, including macro and microtrauma in the joint, lack of muscle coordination, changes in TMJ lubrication, postural disorders, stress and depression
. [
10,
13,
14,
15] Likewise, the anatomical and functional changes of the osseous structures of the TMJ have been associated with disc displacement
. [
16,
17,
18,
19,
20] Joint hypermobility has also been associated with DD. [
21,
22,
23] Joint hypermobility (JH) is a term that describes the ability of a singular or multiple joints to move beyond the normal physiological limits and it is considered more as a descriptor rather than a diagnosis; it can be observed as localized joint hypermobility (LJH) or as GJH when it affects multiple joints. [
24]
The most common method used for assessing GJH is the Beighton Score (BS), a set of tests in a nine-point scoring system. It was initially developed as an epidemiological tool used for screening large populations, but later it has been utilized as a clinical tool for diagnosis of GJH. [
25,
26]
Some author suggested that adolescents with GJH have a greater risk of developing TMJ disc displacement, especially disc displacement without reduction. [
21] To the knowledge of the authors, there aren’t studies in the literature on the correlation between different degrees of severity of DD and GJH in growing patients.
It would be interesting to know if the severity of disc displacement assessed on MRI
is associated with the presence of GJH in patients in growth.
The aims of the present study, therefore, were (1) to assess if there is an association between internal derangements of TMJ, in particular the severity of DD, and the presence of GJH in pre-orthodontic growing patients evaluated on MRI and, (2) to determine the relationship between the severity stages of DD and the age in growing patients.
2. Materials and Methods
2.1. Study Population
This observational cross-sectional study has been conducted on pre-orthodontic patients visiting an Orthodontics Operational Unit of the Department of Odontostomatological and Maxillofacial Sciences of the University "La Sapienza" of Rome for an initial examination. Patients aged between 8 and 16 years, both sexes, diagnosed with TMD by DC/TMD and with indications for further diagnosis by MRI by the treating clinician and not as part of this study, were included after informed consent of all the subjects or their parents was obtained. Patients with systemic pathologies, clinical history of craniofacial traumas, syndromic patients, history of orthodontic or gnathological treatment, history of surgical operations of TMJ or maxillofacial, inflammatory TMJ pathologies, and, finally, motion artifacts in MRIs that were avoiding a proper evaluation of the MRI were excluded. The patients were divided into three age groups: Group I from 8 to 9 years (GR-I), Group II from 10 to 12 years (GR-II), and Group III from 13 to 16 years (GR-III). The study followed the Helsinki Declaration on medical protocol and recommendations for research in humans.
2.2. GJH Evaluation
Beighton score [
27] was applied to determine the presence of GJH, it consists of 5 tests, of which four are bilateral: (1) passive abduction of the thumb towards the front of the forearm; (2) passive dorsiflexion of the metacarpophalangeal joint of the 5th finger> 90 °; (3) hyperextension of the elbow joint> 10 °; (4) hyperextension of the knee joint > 10 °; (5) contact of the palms of the hands on the floor with the extended lower limbs. For each positive test, it was assigned 1 point.
Considering a cut-off value of ≥ 4 in Beighton score [
25,
26] the final sample was divided into two groups: a Study Group (SG), subjects with GJH, and a Control Group (CG), subjects without GJH.
2.3. MRI Evaluation
The TMJ MRIs were acquired with a bilateral 7.5 cm TMJ antenna on an MRI scanner OpticaMR360® GE 1.5-Tesla model (General Electric Medical System®). The images were obtained in maximum intercuspation and in maximum mouth opening in both the sagittal and coronal projection (parallel to the long axis of the condyle) with a 3 mm thick sections. For each TMJ (right and left) oblique sagittal T1-w, oblique sagittal T2-w, and oblique coronal T1-w in closed- mouth position and oblique sagittal PD in opened-mouth sequences were obtained.
Disc Position
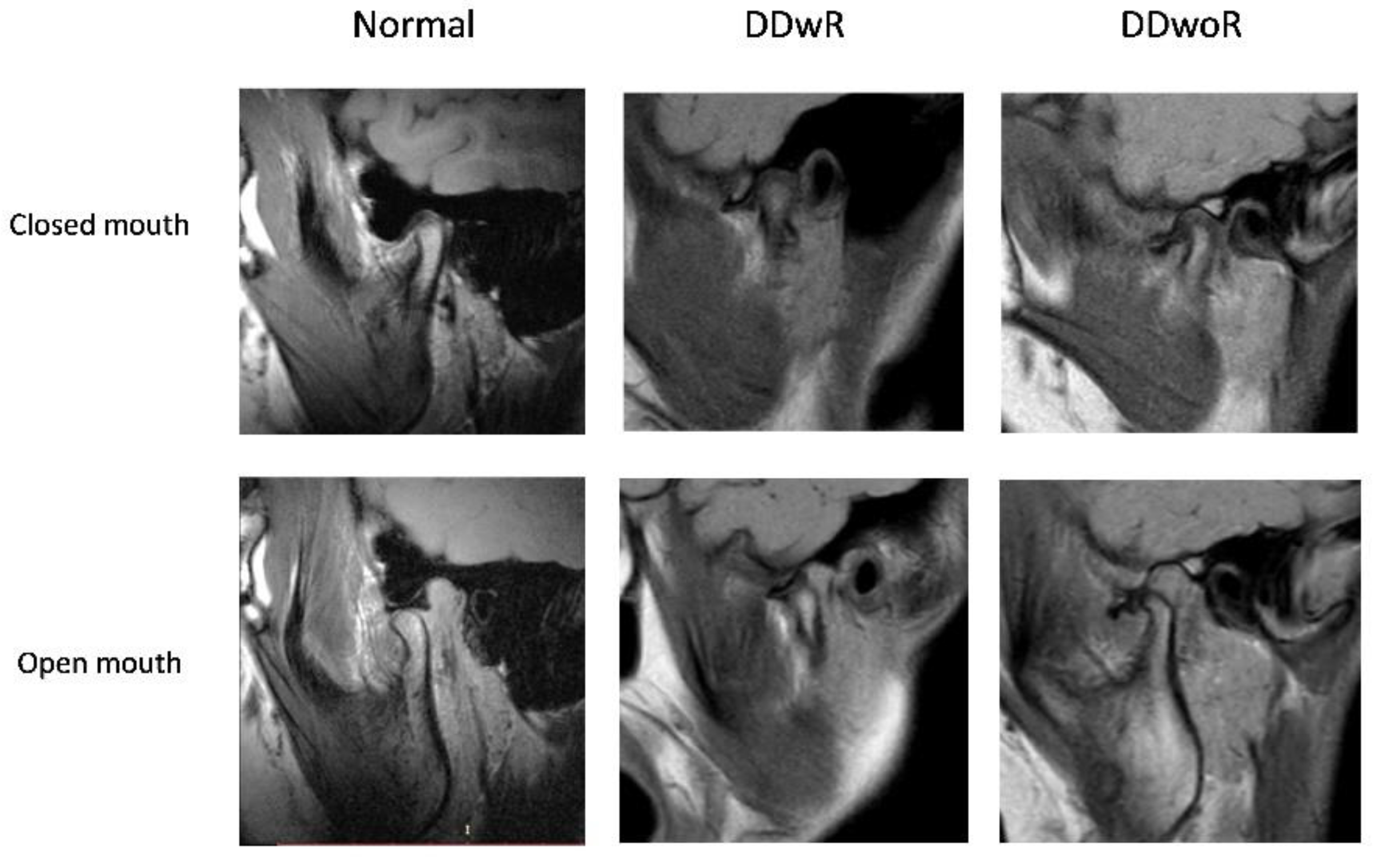
The disc position, evaluated in the sagittal and coronal projection of MRI, was classified into three categories:1,28,29
Normal disc position (N), when in closed-mouth position, the posterior band of the disc was positioned above the apex of the condylar head (in a 12 o'clock position), while in an open-mouth position the intermediate zone of the disc was interposed between the condyle and the articular eminence; in coronal projection, the disc was located over the head of the condyle; in open-mouth, the disc remained interposed between the condyle and the articular surface of the articular eminence.
Disc Displacement with reduction (DDwR), when in sagittal projection, in a closed-mouth position, the posterior band of the disc was anteriorly displaced relative to the head of the condyle and in coronal projection could appear in a normal position over the head of the condyle and/or displaced medially or laterally. However, the articular disc was reduced on mouth opening.
Disc displacement without reduction (DDwoR), when in sagittal and/or coronal planes, in both closed-mouth position and open-mouth position, the posterior band of the disc was displaced relative to the head of the condyle and in an open-mouth position, the correct relationship of the condyle-disc complex was not restored. (
Figure 1)
Disc Displacement Severity
According to the method developed by Ikeda et al.[
29], the severity of DD was assessed in MRI sagittal and coronal planes, to classify the disc position into four different severity stages of DD, from stage 0 to stage 4. In the
sagittal plane the position of the disc in each joint was evaluated in three sagittal MRI slices (medial, middle, and lateral) and based on the location of the posterior band (PB) of the articular disc related to the condyle apex was and rated as
level 0 (normal), level 1, level 2, and level 3 when PB is at 12 o’clock, 11 o’clock, 10 o’clock, and 9 o’clock or below, respectively. In the
coronal plane the mediolateral DD was assessed and assigned the rating of
Level 0 when was not present mediolateral disc displacement and
Level 1 when the disc was wider on the medial or lateral side or when the disc was displaced until one-sixth of its mediolateral breadth;
Level 2 when the disc was displaced till one-third of its mediolateral breadth with a drop-like form; and, finally,
Level 3 when the disc was displaced half or more of its mediolateral breadth.
Based on the assessment of the emerged data from the sagittal and coronal plane, it was assigned a
severity stage to the DD [
29] :
Stage 0 (normal): disc in a normal position, both in a sagittal and coronal plane
Stage 1: the position of the disc in the sagittal planes and the coronal plane up to level 1.
Stage 2: the disc position in sagittal planes of level 2 or sagittal planes of level 1 and the coronal plane up to level 2
Stage 3: disc position in sagittal planes of level 3 and the coronal plane of level up to 3 with disc reduction in mouth opening.
Stage 4: sagittal planes of level 3 and the coronal plane of level up to 3 without disc reduction in mouth opening.
2.4. Statistical Analysis
For statistical descriptive purposes, each TMJ was considered as a statistical unit. The statistical analysis was conducted using the IBM SPSS version 24 software and Pearson's χ2 Test was performed for the analysis of the statistical correlation to compare the frequency of events of the two groups. The statistical significance level of the correlations was set at 5% (p ≤ 0.05).
3. Results
The final sample was composed of 56 individuals, of which 36 females (64.3%) and 20 males (35.7%), ranging in age from 8 to 16 years with a mean age of 12.46 ± 2.28 years.
The sample was divided, based on the presence or absence of GJH, in a Study Group of 30 subjects with GHJ, 22 females (39.3%) and 8 males (14.3%), and a Control Group without GHJ composed of 26 subjects, 14 females (25%) and 12 males (21.4%). No statistically significant association was observed between the presence of GHJ and sex (p> 0.05).
Furthermore, the sample was divided into three age groups: group I (GR-I) from 8 to 9 years, composed of 7 subjects (12.5%), group II (GR-II) from 10 to 12 years, were 23 subjects (41.1%), and group III (GR-III) from 13 to 16 years of 26 subjects (46.4%). No statistical association between age groups and the presence of GHJ was evident (p>0.05).
3.1. MRI Assessment
A total of one hundred twelve (112) TMJs were examined and each TMJ was treated as a single statistical unit.
The study of MRI images revealed the following percentages of disc position in the total sample: normal disc position 41%, DDwR 51%, DDwoR 20%. Was observed, therefore, a higher prevalence of DDwR. There wasn’t a statistically significant association between disc position and sex (p>0.05) or age groups (p>0.05). However, DDwoR did not occur in age group I, but were more frequent in GR-III. (
Table 1)
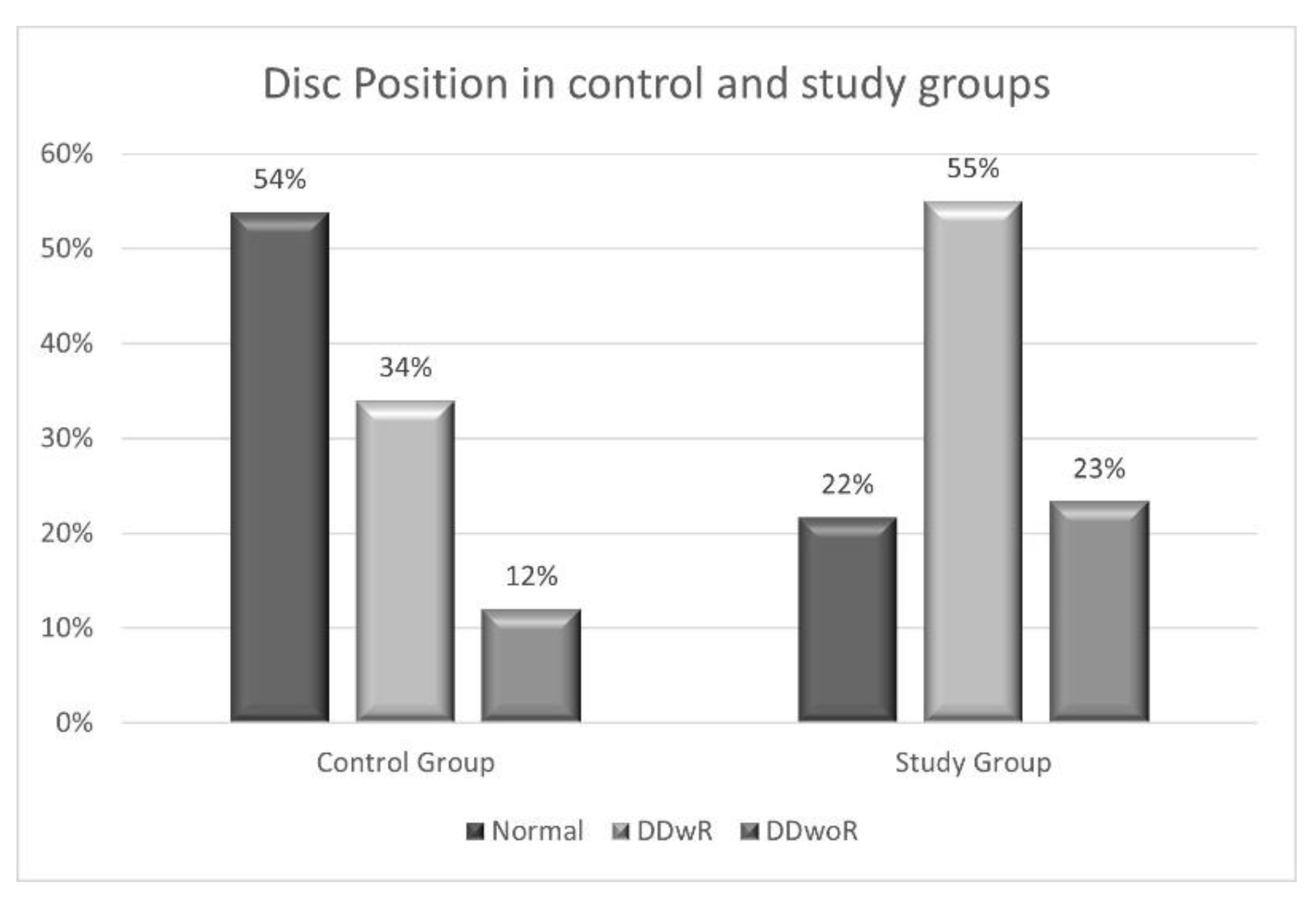
A statistically significant association emerged between
GHJ and disc position, in the study group 78% of patients showed a DD, compared to 46% of the control group (p=0.00; χ2 = 12.431; OR=4.218). DDwR and DDwoR showed a higher presence in the study group (55% and 23% respectively) compared to the control group (34% and 12% respectively) (p=0.002; χ2 = 12.592). (
Figure 2)
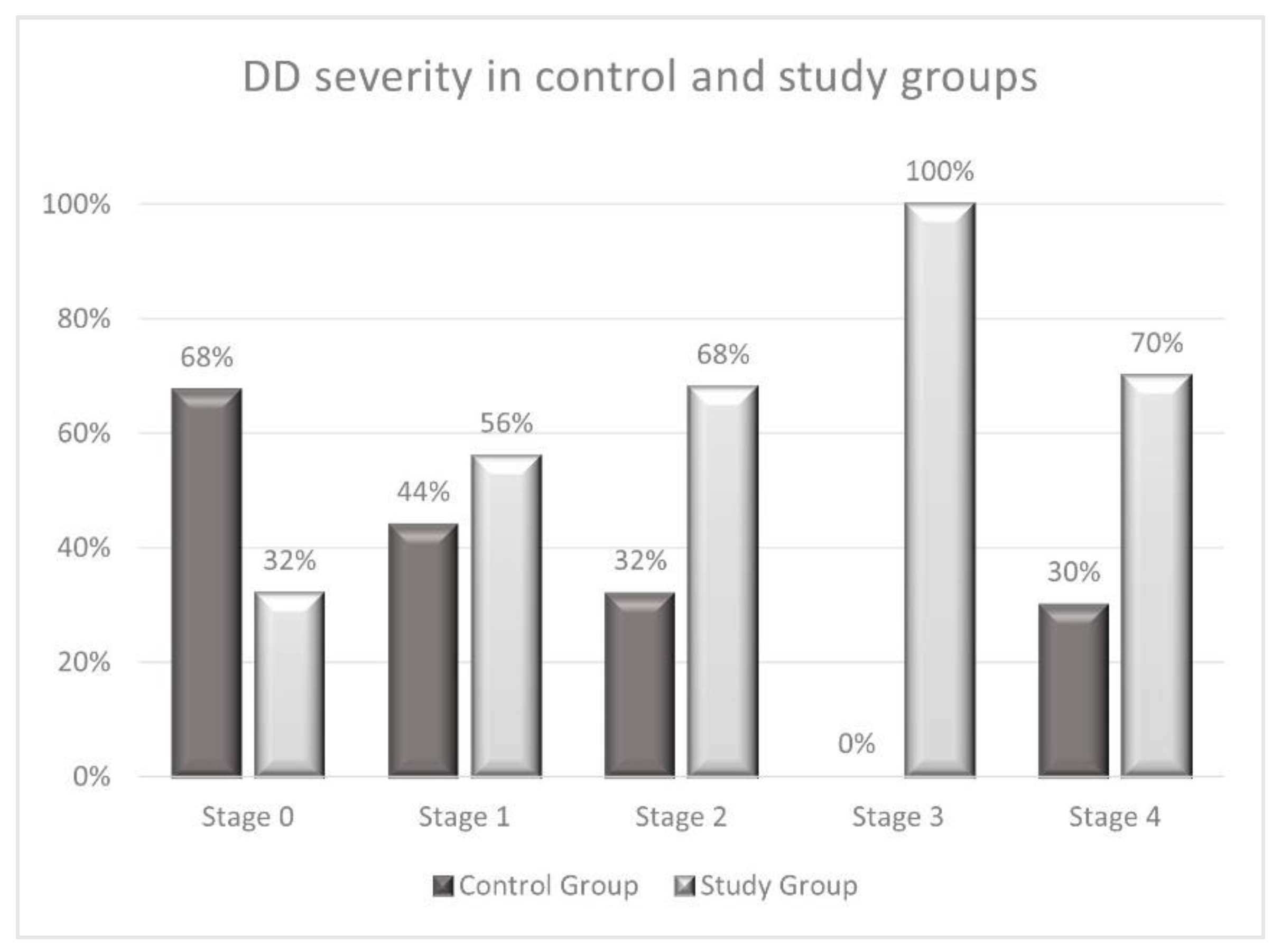
The analysis of the association between the
GJH and DD severity, showed statistically significant results (p < 0.010; χ2 = 13.196), the most severe DD showed a frequency of 70% in the study group compared to 30% in the control group. The specific percentages of each stage are illustrated in
Figure 3.
Regarding the severity of DD and sex, there was no statistical correlation (p>0,05) but stage 3 and 4 of severity DD was mostly frequent in the female.
A statistically significant association was observed between
DD severity and age groups (p=0.017; χ2 = 18.707), with a higher frequency of stages 2, 3 and 4 severity in age groups II and III, showing that with increasing age, the greater the severity of DD. The specific percentages of each stage are represented in
Table 2.
4. Discussion
This cross-sectional study was conducted to investigate the association between the severity of DD and the presence of GJH in pre-orthodontic growing patients evaluated on MRI, and to investigate the relationship between the stages of DD and age.
MRI is an important tool for the imaging diagnosis of TMD and has been considered the gold standard for the evaluation of the TMJ, because provides detailed images of soft tissues and anatomical structures of the TMJ, especially of the articular disc and its position. [
30,
31,
32] MRI can identify disc displacements in their early stages, enabling early and preventive treatment. [
30,
33] In growing patients, it is crucial to detect issues in the TMJ as early as possible to address them effectively. Unlike other imaging techniques like computed tomography (CT), MRI does not use ionizing radiation, this makes it safe for use in young patients and avoids unnecessary radiation exposure. [
34,
35]
The DD is the most common TMJ internal damage condition., it was diagnosed in the general population and also present in children and adolescents. [
6,
36,
37,
38,
39,
40] In the present study the most common DD was DDwR, a result that is in agreement with several authors. Valesan
et al. [
2] in their systematic review reported a higher prevalence of DDwR than DDwoR in developmental individuals of the general population. While Nebbe
et al. [41] evaluated pre-orthodontic adolescents with a high prevalence of DDwR.
Various hypotheses have been put forward to explain the etiopathogenesis of abnormal disc position, including ligamentous hypermobility. [
42] The TMJ can be affected by GJH, receiving an overload, and as a consequence suffers degenerative changes which can produce internal derangements. [
43] Some studies show that in the TMJ of GHJ subjects there is an increased risk of articular disc displacement and a lower risk of reduced mouth opening capacity. [
44,
45] These data agree with the results of this research, subjects with GHJ, compared to the control group, have a higher percentage of DD, with a 4-fold increased risk of presenting DD for patients with GHJ. Other authors suggest that there is no such correlation between GHJ and DD, however, they did not study growing patients. [
43,
46]
The DDwR was the most frequent DD in the whole sample, as reported also by other authors. [
6,
7,
8,
14] However, in the age distribution it is important to note that DDwR occurred only in age group III from 12 to 14 years. This result could be explained by the suggestion of some authors who propose that DDwR would be the first stage of disk displacement, which could evolve into DDwoR. [
10,
14,
37]. However, the literature is controversial on this aspect, as some authors report that this evolution is not evident. In the systematic review conducted by Naeije
et al. [
47] it emerges that the DDwR is usually a stable, painless condition and accompanies the patient throughout life depending on the adaptive physiological processes that may occur.
Regarding the severity of DD patients with GHJ had a 2-fold higher frequency of DD of greater severity (stage 3 and 4) than patients in the control group. Furthermore, there was a higher frequency of 2, 3 and 4 severity stages in age groups II and III, while the group I showed the presence stage 1 of DD, considered incipient, showing that with increasing age, the greater the severity of DD. These results, which are consistent with those reported by Ikeda et al [
29], suggest that it is possible that intra-articular disorder may begin before the age of 10 years and that it is clinically desirable to check the condition of the articular disc at an early age.
Despite the limitations of this study, the results obtained provide an insight into the aetiology and mechanism of DD development in children and adolescents. Future studies should be conducted to study the presence of DD in growing patients by studying correlating factors.
5. Conclusions
The results of this study suggest that growing patients with GJH have a higher risk of developing DD and with more severe stages. The risk of developing DD and having a more advanced stage of severity increases with increasing age.
Author Contributions
Conceptualization, AM.B. and AA.DS.; methodology, M.H.; software, AM.B.; validation, AA.DS. and M.H.; formal analysis, A.I.; investigation, E.S.; data curation, AM.B.; writing—original draft preparation, AM.B., AA.DS; writing—review and editing, M.H.; visualization and supervision, G.G.; project administration, G.G.; funding acquisition, AA.DS. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Policlinico Umberto I (N.47/19/0001155).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral. Facial Pain. Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; et al. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: A systematic review with meta-analysis. J. Oral. Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef]
- Bonjardim, L.R.; Gavião, M.B.D.; Pereira, L.J.; Castelo, P.M.; Garcia, R.C.M.R. Signs and symptoms of temporomandibular disorders in adolescents. Braz. Oral. Res. 2005, 19, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Kohler, A.; Helkimo, N.; Magnusson, T.; Hugoson, A. Prevalence of symptoms and signs indicative of temporomandibular disorders in children and adolescents. A Cross-Sect. Epidemiol. Investig. Cover. Two Decades. Eur. Arch. Paediatr. Dent. 2009, 10, 16–25. [Google Scholar]
- Da Silva, C.G.; Pachêco-Pereira, C.; Porporatti, A.L.; Savi, M.G.; Peres, M.A.; Flores-Mir, C.; et al. Prevalence of clinical signs of intra-articular temporomandibular disorders in children and adolescents A systematic review and meta-analysis. J. Am. Dent. Assoc. 2015, 147, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Christidis, N.; Lindström Ndanshau, E.; Sandberg, A.; Tsilingaridis, G. Prevalence and treatment strategies regarding temporomandibular disorders in children and adolescents-A systematic review. J. Oral. Rehabil. 2019, 46, 291–301. [Google Scholar] [CrossRef]
- De Stefano, A.; Guercio-Mónaco, E.; Uzcátegui, A.; Boboc, A.M.; Barbato, E.; Galluccio, G. Temporomandibular disorders in Venezuelan and Italian adolescents. CRANIO® 2022, 40, 517–523. [Google Scholar] [CrossRef]
- Song, Y.L.; Yap, A.U.; Türp, J.C. Association between temporomandibular disorders and pubertal development: A systematic review. J. Oral. Rehabil. 2018, 45, 1007–1015. [Google Scholar] [CrossRef]
- Impellizzeri, A.; Di Benedetto, S.; De Stefano, A.; Monaco Guercio, E.; Barbato, E.; Galluccio, G. General health & psychological distress in children with temporomandibular disorder. Clin. Ter. 2019, 170, e321–7. [Google Scholar]
- Lai, Y.C.; Yap, A.U.; Türp, J.C. Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J. Oral Rehabil. 2020, 47, 270–280. [Google Scholar] [CrossRef] [PubMed]
- LeResche, L.; Mancl, L.A.; Drangsholt, M.T.; Saunders, K.; Von Korff, M. Relationship of pain and symptoms to pubertal development in adolescents. Pain 2005, 118, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D. Etiopathogenesis of disk displacement of the temporomandibular joint: A review of the mechanisms. Indian. J. Dent. Res. 2009, 20, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Romani, V.; Di Giorgio, R.; Castellano, M.; Barbato, E.; Galluccio, G. Prevalence of craniomandibular disorders in orthodontic pediatric population and possible interactions with anxiety and stress. Eur. J. Paediatr. Dent. 2018, 19, 317–323. [Google Scholar] [PubMed]
- Impellizzeri, A.; Serritella, E.; Putrino, A.; Vizzielli, G.; Polimeni, A.; Galluccio, G. Assessment of masticatory and cervical muscles’ thickness by ultrasonography in patients with facial asymmetry. Clin. Ter. 2019, 170, e272–e277. [Google Scholar]
- De-Stefano, A.A.; Di-Chicco, A.; Impellizzeri, A.; Serritella, E.; Guercio-Mónaco, E.; Galluccio, G. Unilateral Condylar Hyperplasia: A Thee-Dimensional CBCT Morphometric and Volumetric Evaluation of Mandibular Condyle by Open-Source Softwares. Int. J. Morphol. 2021, 39, 1164–1170. [Google Scholar] [CrossRef]
- De Stefano, A.; Guercio-Monaco, E.; Hernández-Andara, A.; Galluccio, G. Association between temporomandibular joint disc position evaluated by magnetic resonance imaging and mandibular condyle inclination evaluated by computed tomography. J. Oral. Rehabil. 2020, 47, 743–749. [Google Scholar] [CrossRef]
- Guercio-Monaco, E.; De Stefano, A.; Impellizzeri, A.; Galluccio, G. Association between the temporomandibular joint disc position on magnetic resonance imaging and the mandibular deviation on posteroanterior cephalogram: A cross-sectional study in adolescents. Clin. Ter. 2020, 171, e509–16. [Google Scholar]
- Vernucci, R.A.; Mazzoli, V.; Galluccio, G.; Silvestri, A.; Barbato, E. Unilateral hemimandibular hyperactivity: Clinical features of a population of 128 patients. J. Cranio-Maxillofac. Surg. 2018, 46, 1105–1110. [Google Scholar] [CrossRef]
- Guercio Monaco, E.; De Stefano, A.; Hernandez-Andara, A.; Galluccio, G. Correlation between condylar size on CT and position of the articular disc on MRI of the temporomandibular joint. CRANIO® 2022, 40, 64–71. [Google Scholar] [CrossRef]
- Boboc, A.M.; De Stefano, A.; Impellizzeri, A.; Barbato, E.; Galluccio, G. Correlation between generalized joint hypermobility and temporomandibular joint disc displacement in adolescent patients: Magnetic ResonanceImaging study. Eur. J. Paediatr. Dent. 2022, 23, 106–110. [Google Scholar] [PubMed]
- Bin Abd Razak, H.R.; Bin Ali, N.; Sen, H.T. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J. Sci. Med. Sport. 2014, 17, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.L.C.; Wang, D.D.H.; Yang, M.C.M.; Hsu, W.E.W.; Hsu, M.L.M. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J. Med. Sci. 2018, 34, 223–230. [Google Scholar] [CrossRef]
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A framework for the classification of joint hypermobility and related conditions. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Remvig, L.; Jensen, D.V.; Ward, R.C. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: Review of the literature. J. Rheumatol. 2007, 34, 804–809. [Google Scholar] [PubMed]
- Bockhorn, L.N.; Vera, A.M.; Dong, D.; Delgado, D.A.; Varner, K.E.; Harris, J.D. Interrater and Intrarater Reliability of the Beighton Score: A Systematic Review. Orthop. J. Sport. Med. 2021, 9, 2325967120968099. [Google Scholar] [CrossRef]
- Beighton, P.; Solomon, L.; Soskolne, C.L. Articular mobility in an African population. Ann. Rheum. Dis. 1973, 32, 413–418. [Google Scholar] [CrossRef]
- Tasaki, M.M.; Westesson, P.L.; Isberga, M.; Ren, Y.F.; Tallents, R.H. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 249–262. [Google Scholar] [CrossRef]
- Ikeda, K.; Kawamura, A.; Ikeda, R. Prevalence of Disc Displacement of Various Severities among Young Preorthodontic Population: A Magnetic Resonance Imaging Study. J. Prosthodont. 2014, 23, 397–401. [Google Scholar] [CrossRef]
- Ahmad, M.; Hollender, L.; Anderson, Q.; Kartha, K.; Ohrbach, R.; Truelove, E.L.; et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): Development of image analysis criteria and examiner reliability for image analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, 844–860. [Google Scholar] [CrossRef]
- Pupo, Y.M.; Pantoja, L.L.Q.; Veiga, F.F.; Stechman-neto, J.; Zwir, L.F.F.; Farago, P.V.; et al. Diagnostic validity of clinical protocols to assess temporomandibular disk displacement disorders: A meta-analysis. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2016, 122, 572–586. [Google Scholar] [CrossRef] [PubMed]
- Vogl, T.J.; Lauer, H.C.; Lehnert, T.; Naguib, N.N.N.; Ottl, P.; Filmann, N.; et al. The value of MRI in patients with temporomandibular joint dysfunction: Correlation of MRI and clinical findings. Eur. J. Radiol. 2016, 85, 714–719. [Google Scholar] [CrossRef]
- Talmaceanu, D.; Lenghel, L.M.; Bolog, N.; Hedesiu, M.; Buduru, S.; Rotar, H.; et al. Imaging modalities for temporomandibular joint disorders: An update. Dent. Med. 2018, 91, 280–287. [Google Scholar] [CrossRef]
- Shen, S.; Ye, M.; Wu, M.; Zhou, W.; Xu, S. MRI and DC/TMD Methods Analyze the Diagnostic Accuracy of the Change in Articular Disc of Temporomandibular Joint. Comput. Math. Methods Med. 2022, 2022, 1770810. [Google Scholar] [CrossRef] [PubMed]
- Whyte, A.; Boeddinghaus, R.; Bartley, A.; Vijeyaendra, R. Imaging of the temporomandibular joint. Clin. Radiol. 2021, 76, e21–e35. [Google Scholar] [CrossRef]
- Paesani, D.; Salas, E.; Martinez, A.; Isberg, A. Prevalence of temporomandibular joint disk displacement in infants and young children. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1999, 87, 15–19. [Google Scholar] [CrossRef]
- De Melo, D.P.; Sousa Melo, S.L.; De Andrade Freitas Oliveira, L.S.; Ramos-Perez, F.M.D.M.; Campos, P.S.F. Evaluation of temporomandibular joint disk displacement and its correlation with pain and osseous abnormalities in symptomatic young patients with magnetic resonance imaging. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2015, 119, 107–112. [Google Scholar] [CrossRef]
- Marpaung, C.; van Selms, M.K.A.; Lobbezoo, F. Temporomandibular joint anterior disc displacement with reduction in a young population: Prevalence and risk indicators. Int. J. Paediatr. Dent. 2019, 29, 66–73. [Google Scholar] [CrossRef]
- Kellenberger, C.J.; Bucheli, J.; Schroeder-Kohler, S.; Saurenmann, R.K.; Colombo, V.; Ettlin, D.A. Temporomandibular joint magnetic resonance imaging findings in adolescents with anterior disk displacement compared to those with juvenile idiopathic arthritis. J. Oral. Rehabil. 2019, 46, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.D. . Internal Derangement of Temporomandibular Joint - A Review\n. IOSR J. Dent. Med. Sci. 2014, 13, 66–73. [Google Scholar] [CrossRef]
- Nebbe, B.; Major, P.W. Prevalence of TMJ Disc Displacement in a Pre-Orthodontic Adolescent Sample. Angle Orthod. 2000, 70, 454–463. [Google Scholar] [PubMed]
- Chiodelli, L.; Pacheco, A.B.; Missau, T.S.; Silva, A.M.; Corrêa, E.C. Influence of generalized joint hypermobility on temporomandibular joint and dental occlusion: A cross-sectional study. Codas 2016, 28, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Sáez-Yuguero, R.; Linares-Tovar, E.; Calvo-Guirado, J.L.J.L.; Bermejo-Fenoll, A.; Rodríguez-Lozano, F.J.; Sáez-Yuguero, R.; et al. Joint hypermobility and disk displacement confirmed by magnetic resonance imaging: A study of women with temporomandibular disorders. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2009, 107, e54–e57. [Google Scholar] [CrossRef]
- Kavuncu V, Sahin S, Kamanli A, Karan, A. , Aksoy, C. The role of systemic hypermobility and condylar hypermobility in temporomandibular joint dysfunction syndrome. Rheumatol. Int. 2006, 26, 257–260. [Google Scholar] [CrossRef]
- Hirsch, C.; John, M.T.; Stang, A. Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur. J. Oral. Sci. 2008, 116, 525–530. [Google Scholar] [CrossRef]
- Berger, M.; Szkutnik, J.; Szalewski, L.; Wójcik, D.; Bakalczuk, M.; Ginszt, M. Correlation between generalized joint laxity and symptoms of temporomandibular disorders. Pol. Merkur. Lek. 2016, 40, 248–251. [Google Scholar]
- Naeije, M.; te Veldhuis, A.H.; te Veldhuis, E.C.; Visscher, C.M.; Lobbezoo, F. Disc displacement within the human temporomandibular joint: A systematic review of a “noisy annoyance. J. Oral. Rehabil. 2013, 40, 139–158. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).