1. Text and Figures
To differentiate between benign and malignant biliary strictures can be challenging when relying solely on cross-sectional imaging. SpyGlass peroral cholangioscopy (POCS) provides a valuable solution by enabling direct visualization and the acquisition of mucosal tissue samples from the biliary and pancreatic ducts. Data from a multinational registry indicate impressive success rates for POCS, with an 87.2% rate for visual diagnostic impressions and a 92.9% rate for obtaining adequate biopsies, all while maintaining a low procedure-related adverse event rate of 1.7% [
1]. A meta-analysis of 283 POCS procedures further revealed that the overall pooled sensitivity and specificity of visual interpretation for detecting biliary malignancies was 94% (95% CI 89~97%) and 95% (95% CI 90~98%), respectively [
2]. Primary sclerosing cholangitis (PSC), characterized by long-term chronic inflammation and scarring of the bile ducts, carries an elevated risk of biliary strictures and cholangiocarcinoma. POCS has emerged as a valuable tool for the diagnosis of PSC. Notably, Itoi et al. identified nine distinct POCS features, with scarring and pseudodiverticula indicating PSC, while partially enlarged vessels suggesting cholangiocarcinoma [
3]. Subsequently, Fujisawa et al. examined various endoscopic findings in the context of PSC. During the active phase, they noted features like mucosal erythema, ulceration, fibrinous white exudate and an irregular surface. In contrast, during the chronic phase, features such as scarring, pseudodiverticula and bile duct stenosis were observed. Moreover, there is a subgroup of PSC patients who present with nodular or mass formation regardless of the phase. Common endoscopic findings include friability, dilated vessels, tortuous vessels and mass formation. These findings should be carefully distinguished from indicators of cholangiocarcinoma [
4]. Furthermore, POCS-directed biopsy is instrumental in assessing inflammatory activity and malignant potential in PSC patients [5, 6]. Although research on the diagnostic utility of POCS for PSC is limited, it remains a critical tool for early diagnosis as well as detecting malignant transformations in PSC cases and may aid in predicting the timing of liver transplantation [
4]. Herein, we presented the SpyGlass POCS findings in a PSC patient with benign hilar biliary stricture.
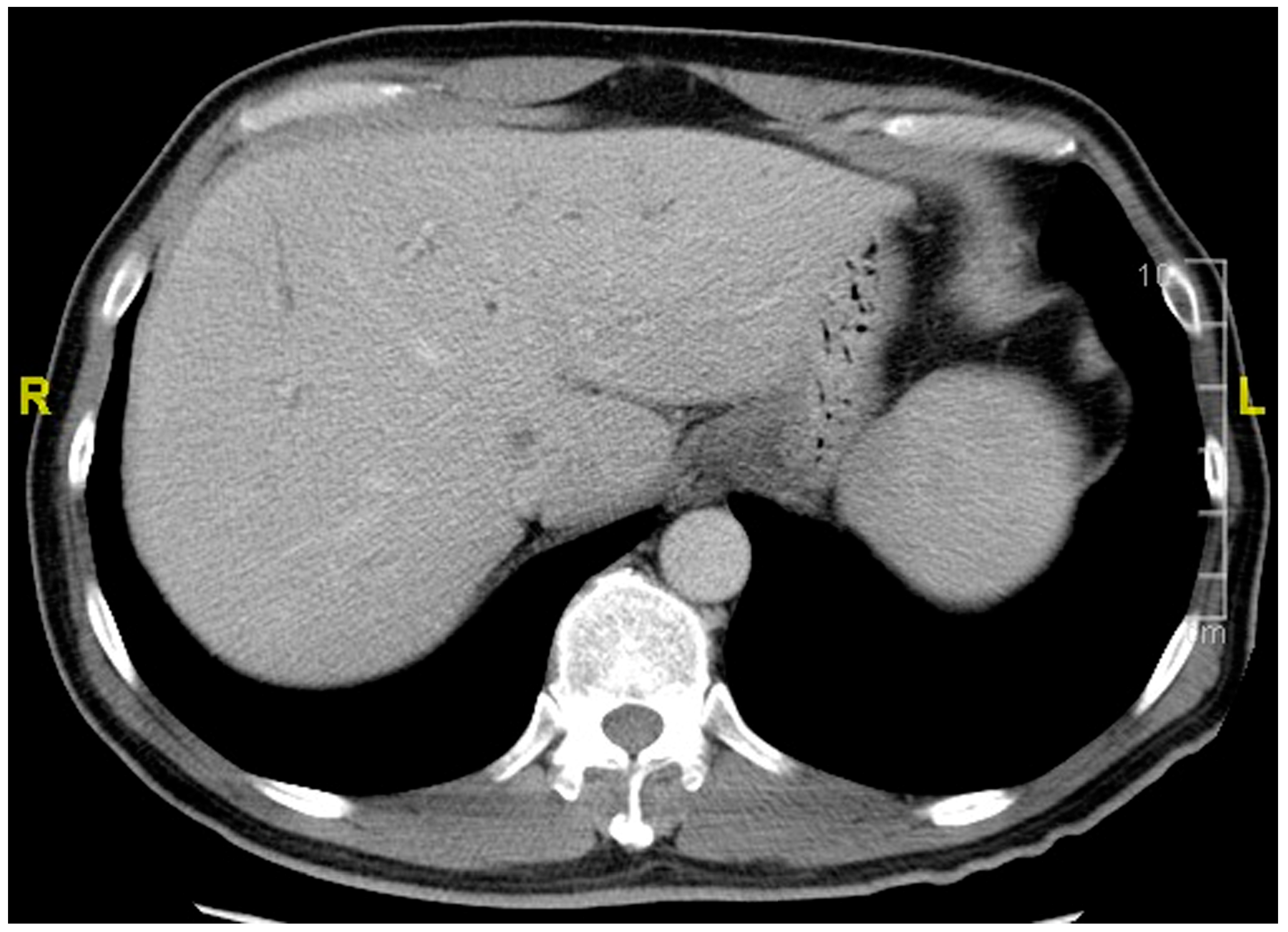
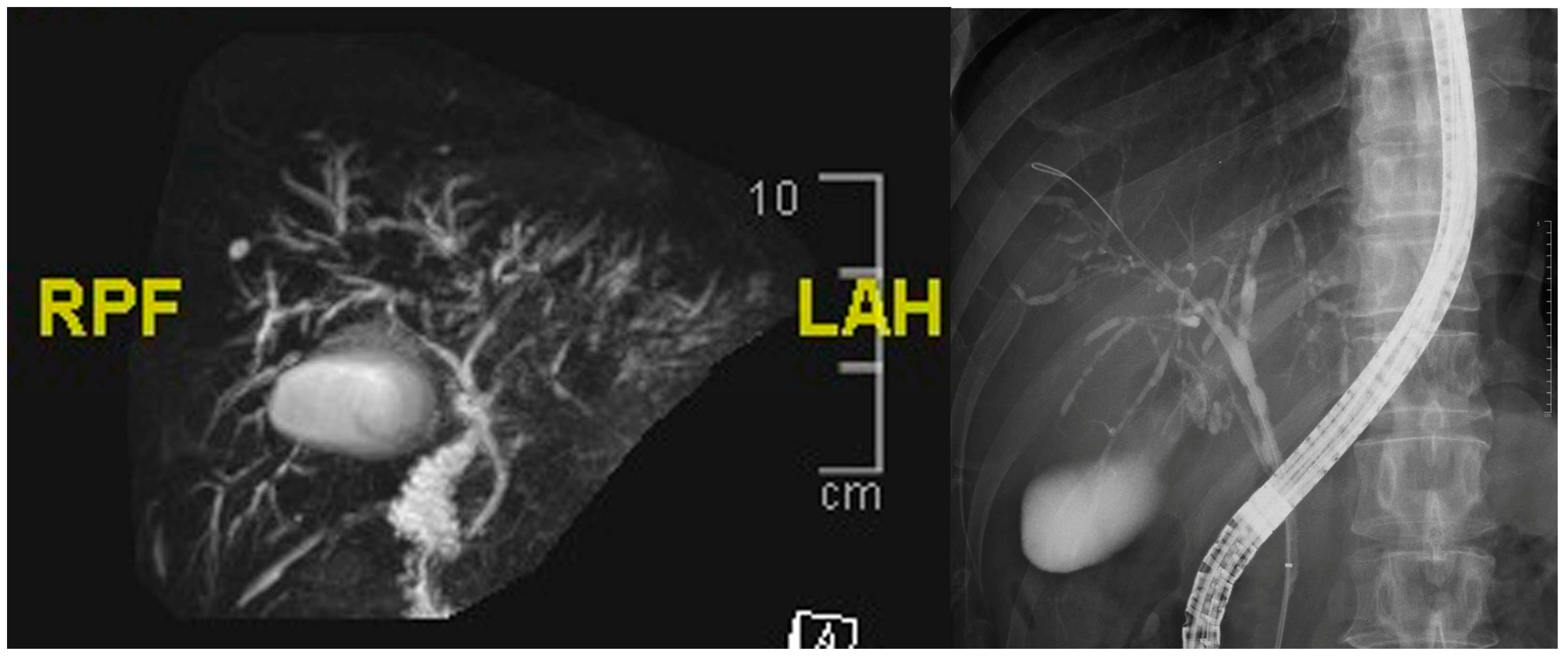
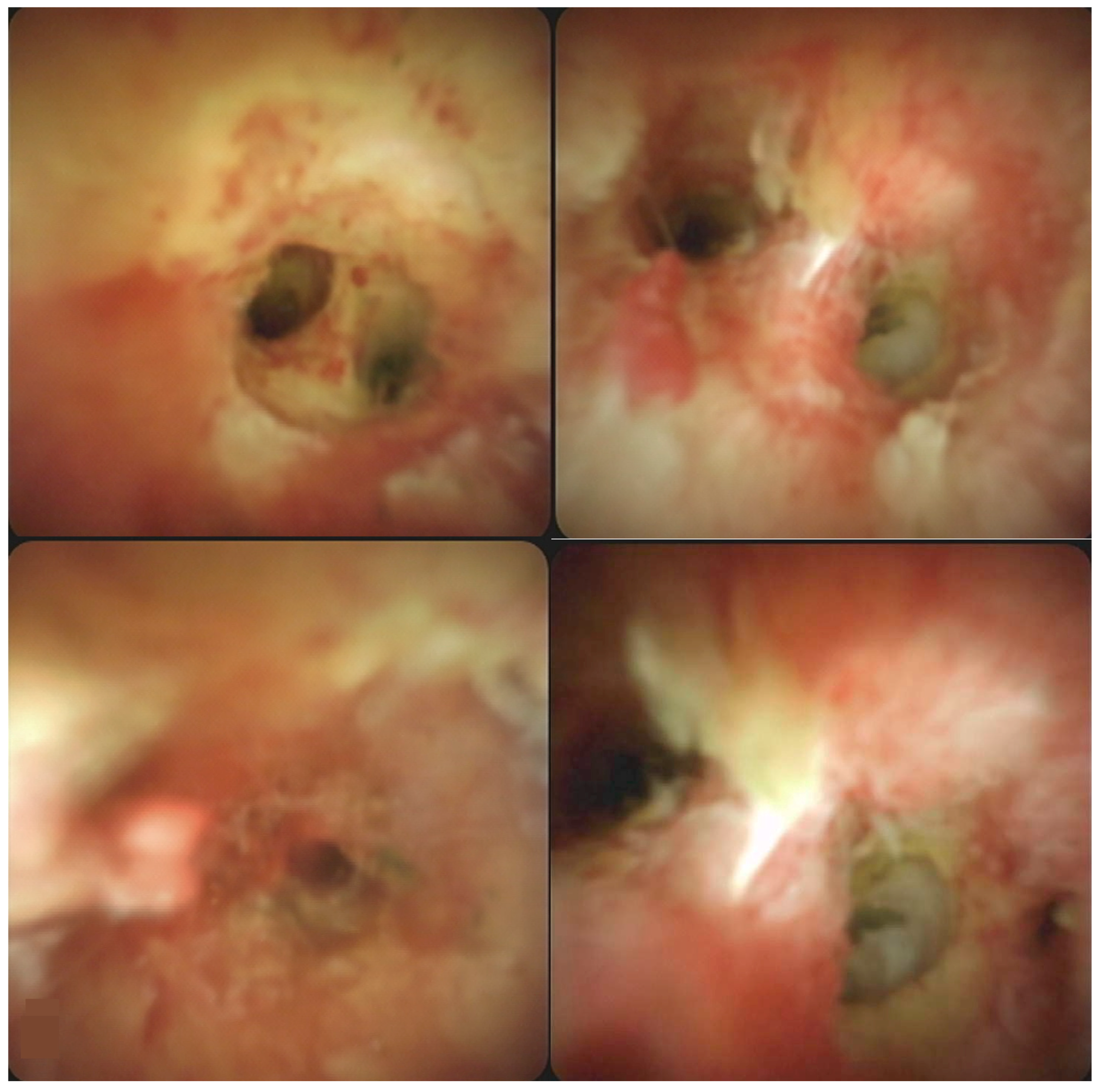
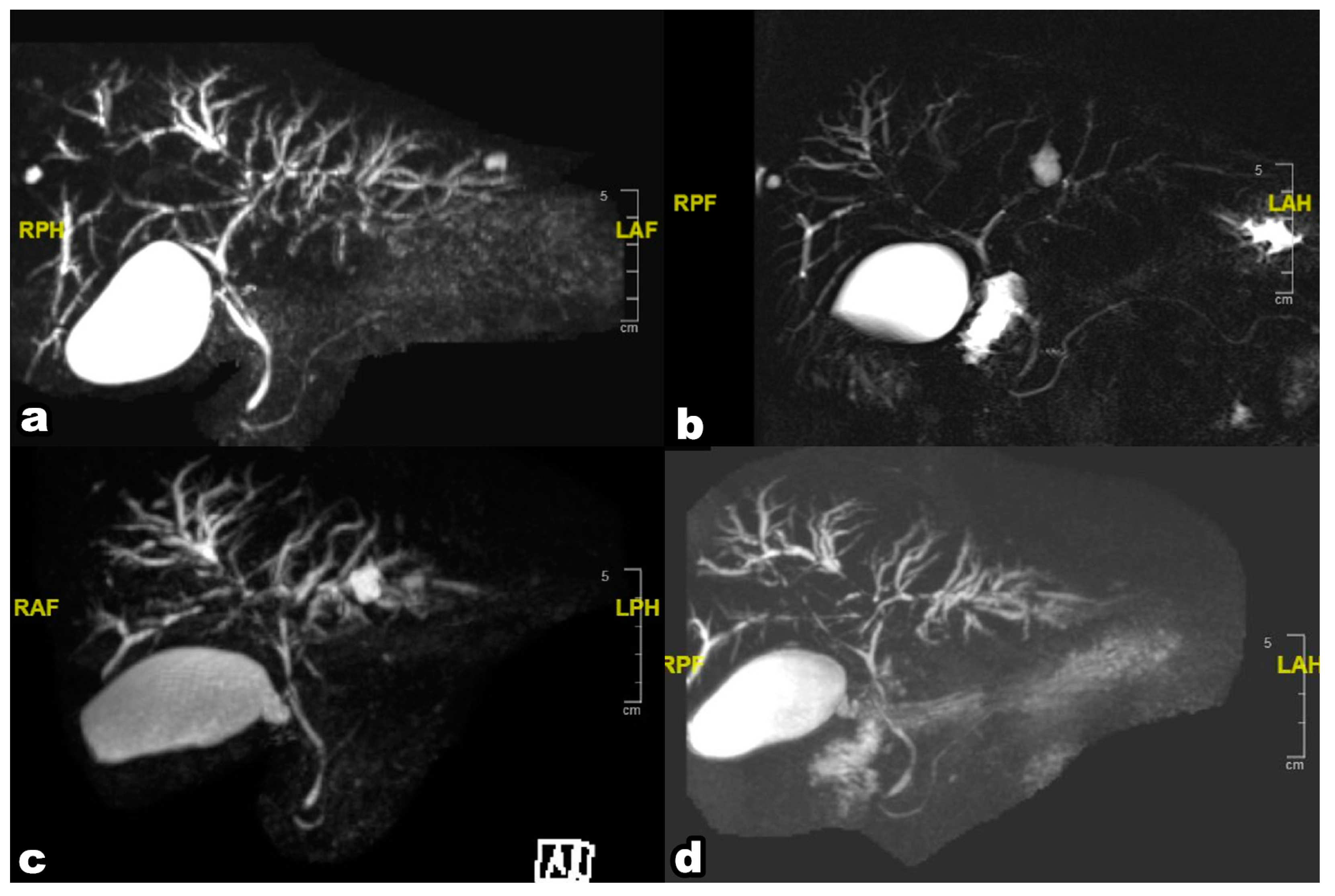
This 59-year-old man suffered from epigastralgia and progressive jaundice for 2 weeks. Tri-phase computer tomography showed diffuse dilatation of intrahepatic ducts (IHDs) with tapering at the hilum (Figure 1). Magnetic Resonance Cholangiopancreatography (MRCP) disclosed diffuse irregular sausage-like IHDs with minimal peri-ductal enhancement and endoscopic retrograde cholangiopancreaticography confirmed a hilar biliary stricture (Figure 2). The SpyGlass™ Direct Visualization System-II (Boston Scientific, Marlborough, MA, USA) demonstrated fibrinous exudates within an ulcerated and erythematous stenotic bile duct. No irregular dilated vessels nor papillary projections were noted, favoring a benign mucosa (Figure 3). POCS-directed biopsy reported chronic inflammation with negative CK AE1/3 staining. Following a 2-month course of ursodeoxycholic acid (15mg/kg/day) for PSC, the patient’s cholestatic-type jaundice normalized. During a three-year follow-up, the patient has been free from recurrent jaundice, cholangitis, and abdominal pain. Notably, both total bilirubin and alkaline phosphatase levels have consistently remained within the normal range, and serial MRCP scans have shown stable results (Figure 4).
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Almadi MA, Itoi T, Moon JH et al. Using single-operator cholangioscopy for endoscopic evaluation of indeterminate biliary strictures: results from a large multinational registry. Endoscopy 2020, 52, 574–582. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira PVAG, de Moura DTH, Ribeiro IB et al. Efficacy of digital single-operator cholangioscopy in the visual interpretation of indeterminate biliary strictures: a systematic review and meta-analysis. Surg Endosc. 2020, 34, 3321–3329. [Google Scholar] [CrossRef] [PubMed]
- Itoi T, Kamisawa T, Igarashi Y, et al. The role of peroral video cholangioscopy in patients with IgG4-related sclerosing cholangitis. J. Gastroenterol. 2013, 48, 504–514. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa T, Ushio M, Takahashi S et al. Role of Peroral Cholangioscopy in the Diagnosis of Primary Sclerosing Cholangitis. Diagnostics (Basel). 2020, 10, 268. [Google Scholar] [CrossRef] [PubMed]
- Siiki A, Rinta-Kiikka I, Koivisto Tet al. Spyglass single-operator peroral cholangioscopy seems promising in the evaluation of primary sclerosing cholangitis-related biliary strictures. Scand J Gastroenterol. 2014, 49, 1385–1390. [Google Scholar] [CrossRef] [PubMed]
- Rey JW, Hansen T, Dümcke S et al. Efficacy of SpyGlass(TM)-directed biopsy compared to brush cytology in obtaining adequate tissue for diagnosis in patients with biliary strictures. World J Gastrointest Endosc. 2014, 6, 137–143. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).